Abstract
Helicobacter pylori (H. pylori) infection is prevalent all over the world, which may even cause gastric cancer. Unfortunately, current antibiotic therapy cannot completely eradicate drug-resistant H. pylori. HF-18 (GFFKKAWRKVKKAFRRVL-NH2), a novel cationic antimicrobial peptide, showed broad antimicrobial activities, low cytotoxicity toward mammalian cells and low drug tolerance during our previous research. In this paper, to investigate the antibacterial activities and possible mechanisms underlying HF-18 against drug-resistant H. pylori, cytotoxin associated protein (CagA)-carrying recombinant E. coli BL21 was constructed. Subsequently, Zeta potential detection, N-Phenyl-1-naphthylamine uptake, propidium iodide fluorescence uptake, transmission electron microscope, qRT-PCR and Western blot assays were performed. Consequently, we found that HF-18 had potent antibacterial effects on clarithromycin- and amoxicillin- resistant H. pylori. In terms of its mode of action, HF-18 could neutralize negative charges on the surface of H. pylori, penetrate into and disrupt the integrity of bacterial membranes, resulting in the death of drug-resistant H. pylori to reduce cells infection. In addition, HF-18 inhibited the transcription of adhesion gene alpA/alpB and the expression of virulence protein CagA under sub-inhibitory concentration, and ultimately decreased bacterial virulence. Therefore, HF-18 lays a foundation for the development and utilization of new antibiotics.
Graphical Abstract

Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
H. pylori is one of the most widespread pathogens that cause serious human diseases (Pellicano et al. 2016). It is reported that about half of the world’s population carries H. pylori in the stomach (Rothenbacher and Brenner 2003; Saadat et al. 2007; Stein et al. 2002). Infection induced by H. pylori may lead to gastritis, gastric ulcers, duodenal ulcers, and even gastric cancer (Bugaytsova et al. 2017). In addition, among the various toxins produced by H. pylori, CagA is one of the most pathogenic toxins which can induce inflammatory and immune responses after stable adhesion of H. pylori in the stomach.
Triple therapy (omeprazole, clarithromycin and amoxicillin) is now widely used in the clinic to treat H. pylori infection; however, the development of drug resistance of H. pylori in clinical greatly reduces the eradication rate of H. pylori (Theuretzbacher et al. 2020). In the face of this dilemma, researchers have to look for alternative antibiotic resources to combat the emergence of drug-resistant pathogens (Annunziato 2019; Hahn et al. 2016; Torres et al. 2019). Current researches on antimicrobial peptide are very extensive (Yeaman and Yount 2003), including physicochemical properties, structural features, biological activity and molecular design and synthesis, etc., which are of remarkable achievements. Therefore, antimicrobial peptide is expected to be a novel class of antimicrobial drug (Thapa et al. 2020).
Our previous study has confirmed that peptide HF-18, 18 amino acids intercepted from hagfish intestinal peptide HFIAP-1 and mutated 2 amino acids (His12 and Gly14 to Lys12 and Phe14) for increasing positive charges and hydrophobicity, had significant antibacterial effects on both Gram-negative bacteria (G−) and Gram-positive bacteria (G+) in vitro (MIC range of 4–32 μg/ml), including S. aureus, S. pneumoniae, S. pyogenes, P. aeruginosa, which are common aerobic pathogens in clinic, especially on clinical mupirocin- and norfloxacin- resistant S. aureus (MIC 4 μg/ml) (Jiang et al. 2020b). In vivo, HF-18 also displayed desirable anti-infection effects on mouse systemic infection model and local skin infection model induced by drug-resistant S. aureus (Ma et al. 2020; Otvos et al. 2018; Ryu et al. 2014). In addition, HF-18 showed low hemolytic activity and cytotoxicity toward mammalian cells. Interestingly, this peptide had high stability even under acid condition (pH 2.2–8) (Jiang et al. 2020b; Neshani et al. 2019). Therefore, we further studied its antibacterial activity against H. pylori, a common clinical microaerobic Gram-negative bacterium that colonizes the stomach (Lin et al. 2021), to expand the antibacterial spectrum of HF-18. Surprisingly, results demonstrated that HF-18 eradicated H. pylori, including clarithromycin- and amoxicillin- resistant H. pylori Sydney Strain-1 (SS1), and reduced bacterial virulence simultaneously.
In this paper, the antibacterial activities of HF-18 against clarithromycin- and amoxicillin- resistant H. pylori SS1 were determined in vitro. In addition, the effects of HF-18 on the genes associated with adhesion and virulence were investigated. Furthermore, we elucidated the potential mechanisms underlying the antibacterial activity and explored the effects of HF-18 at sub-inhibitory concentration on the virulence protein CagA.
Materials and Methods
Bacterial Strains and Cell Culture
H. pylori Sydney Strain-1 (SS1) was acquired from the National Centers for Disease Control. H. pylori 26695 and GES-1 cells were purchased from American Type Culture Collection (ATCC). Recombinant E. coli BL21 (DE3)-CagA strain was obtained by Nanjing Genewiz Biotechnology Co., Ltd.
Culture Conditions
H. pylori strains were cultured in Helicobacter Pylori Agar/Broth Medium (Qingdao Hope Bio-Technology Co., Ltd., Qingdao, China) supplemented with 7% FBS and antimicrobial agents (10 mg/l vancomycin, 5 mg/l trimethoprim, 5 mg/l cefclidine, 5 mg/l amphotericin B) at 37 °C under microaerobic condition created by sealing the plates or test tubes in an anaerobic box using by an AneroPak environment generator (Mitsubishi Gas Chemical) for 48–72 h. E. coli BL21 (DE3)-CagA was cultured with kanamycin (50 μg/ml) in nutrient agar/broth media. IPTG (1 mM) was added to induce the expression of CagA for subsequent experiments. GES-1 cells were cultured in DMEM medium supplemented with 10% FBS at 37 °C in humidified atmosphere of 5% CO2.
Peptides and Reagents
HF-18 [Purity: ≥ 98.0% (HPLC); Peptide Content (N%): 78.5%] and FITC-HF-18 [Purity: ≥ 98.0% (HPLC)] were synthesized using the solid-phase method (GL Biochem Co., Ltd., Shanghai, China). Mouse anti-His monoclonal antibody and BCA protein assay kit were purchased from Nanjing Yifeixue Biotechnology Co., Ltd.; CagA antibody was purchased from Santa Co., Ltd.
Induction of Clarithromycin- and Amoxicillin- Resistance in H. pylori SS1
The experiment for induction of resistance was performed as previously described (Kalenić et al. 1998; Tenney et al. 1983). In brief, 100 µl of bacterial solution (1 × 1010 CFU/ml) was inoculated into Helicobacter Pylori Agar Medium plates containing antibiotics of 1/2 MIC concentration at 37 °C under microaerobic condition for 72 h based on the most recently observed MICs. The MICs of serial passaging were determined by agar plate dilution method (Suthisamphat et al. 2020; Wiegand et al. 2008; Yang et al. 2020). In brief, H. pylori were diluted to 1 × 109 CFU/ml and inoculated to Mueller–Hinton agar plates containing 5% sheep blood with different concentrations of antibiotics. Above steps were repeated until the drug-resistant H. pylori SS1 was successfully induced.
Antimicrobial Activity of HF-18
Minimal Inhibitory Concentration (MIC)
MICs were determined by using a standard micro-broth serial dilution assay as previously described (Moosazadeh Moghaddam et al. 2018). In brief, 50 μl of bacterial suspensions (1 × 105 CFU/ml) were inoculated with isovolumic drugs at serial diluted concentrations ranging from 128 to 0.0625 μg/ml, and then cultured in the corresponding condition for 24 h. MICs, the lowest concentrations that inhibited the visible growth of H. pylori after incubation, were obtained by recording optical density at 600 nm (OD600) using a microplate reader.
Minimum Bactericidal Concentration (MBC)
After MICs detection, 10 μl of mixture in which bacterial growth was visibly inhibited was cultured onto the Helicobacter Pylori Agar Medium supplemented with 7% FBS and placed at 37 °C under microaerobic condition for 72 h (Akhavan et al. 2019). The minimum drug concentration without visible bacterial colonies was considered as MBC.
Killing Curves (KCs)
3 ml of bacterial suspensions (2 × 105 CFU/ml) in Helicobacter Pylori Broth Medium supplemented with 7% FBS were incubated with isovolumic drugs at final concentration of 4 × MIC in the corresponding condition (Jiang et al. 2020a). At 0, 1, 2, 4, 8 and 12 h, samples were obtained for counting CFU of bacteria and KCs were constructed by plotting log10CFU/ml vs time.
Effects of Peptide HF-18 on the Cell Membrane of Resistant H. pylori SS1
Zeta Potential Detection
Zeta potential test was used to detect the variation of potential on bacterial membrane (Ma et al. 2016; Narayana et al. 2015). Drug-resistant H. pylori SS1 at logarithmic growth phase were washed by centrifugation at 8000 rpm for 10 min for 3 times and resuspended with sterile normal saline. Bacterial suspensions (1 × 107 CFU/ml) were co-incubated with the diluted peptides at final concentrations of 0.25, 0.5, 1, 2, 4 × MIC at 37 °C under microaerobic condition for 40 min. Then, potential changes could be measured by a ZetaPlus particle size analyser (Brookhaven Instruments Corporation, Holtsville, NY).
NPN Uptake
The alternation of bacterial membranes permeability caused by HF-18 was detected by N-Phenyl-1-naphthylamine (NPN) uptake assay (Helander and Mattila-Sandholm 2000; Narayana et al. 2015). In brief, drug-resistant H. pylori SS1 at logarithmic growth phase were washed by centrifugation at 8000 rpm for 10 min with PBS for three times and subsequently resuspended with Hepes (5 mM). Bacterial suspensions (1 × 107 CFU/ml) were treated with serial diluted HF-18 at final concentrations of 0.25, 0.5, 1, 2, 4 × MIC or 0.1% TritonX-100 at 37 °C under microaerobic condition for 8 h. NPN solution (10 μM) was added to a final volume of 250 μl and the fluorescence intensity was quantified at the excitation/emission of 350/420 nm.
PI Fluorescence Uptake
Propidium iodide (PI) fluorescence uptake assay was used to detect whether HF-18 could induce the rupture of bacterial inner membranes (Ma et al. 2016). In brief, bacterial suspensions (1 × 107 CFU/ml) were co-incubated with HF-18 (final concentrations: 0.25, 0.5, 1, 2, 4 × MIC) at 37 °C under microaerobic condition for 40 min. After centrifugation, cells were resuspended by PI solution (20 μg/ml) and detected by flow cytometry.
TEM
Transmission Electron Microscope (TEM) could be used to observe the integrity of bacterial membrane in the presence or absence of HF-18 intuitively (Pan et al. 2017). That is, drug-resistant H. pylori SS1 suspensions (1 × 107 CFU/ml) in Helicobacter Pylori Broth Medium supplemented with 7% FBS were mixed with HF-18 at a final concentration of 4 × MIC at 37 °C under microaerobic condition for 40 min. After centrifugation at 8000 rpm for 10 min for 3 times, the pellets were fixed with osmium tetroxide and then subjected to the routine process of TEM as previously described to observe the morphological changes of HF-18-treated bacteria (de Leeuw et al. 2010).
Anti-adhesion and Anti-inflammatory Activities of Peptide HF-18 In Vitro
Effects of FITC-HF-18 on the Adhesion of Drug-Resistant H. pylori SS1 to GES-1 cells by Fluorescence Detection
Drug-resistant H. pylori SS1 (1 × 108 CFU/ml) was pre-treated with HF-18 at final concentrations of 8, 4 and 2 μg/ml, respectively, in the corresponding condition for 1 h. After washing with PBS for 3 times, the precipitates were labeled with 1% FITC for 1 h in the dark (Jiang et al. 2020a). The FITC-labeled bacteria at a final concentration of 1 × 107 CFU/ml were resuspended in DMEM medium containing 10% FBS and used to infect GES-1 cells with multiplicity of infection (MOI: 100:1) at 37 °C. After 1 h post-infection, the non-adherent bacteria were washed with PBS for three times and the infected cells were observed by fluorescence microscopy.
Effects of HF-18 on the Supernatant of Drug-Resistant H. pylori SS1 Infected Cells and the Number of Adherent Bacteria
Drug-resistant H. pylori SS1 at logarithmic growth phase were collected by centrifugation at 8000 rpm for 10 min and resuspended with DMEM medium supplemented with 10% FBS. After 1 h post addition of serial diluted HF-18 (final concentration: 64, 16 and 4 μg/ml), GES-1 cells were infected with drug-resistant H. pylori SS1 (MOI: 100:1) for 6 h at 37 °C in humidified atmosphere of 5% CO2 (Jiang et al. 2020a). The cell supernatant was collected and cells were lysed, respectively. Then the numbers of bacteria were determined by CFU enumeration.
qRT-PCR
Total RNA of drug-resistant H. pylori SS1 was extracted using bacteria RNA extraction Kit and cDNA was obtained with a HiScript Q RT SuperMix for qPCR kit. The qRT-PCR was performed according to a ChamQ SYBR qPCR Master Mix kit. The sequences of the forward and reverse primers were listed in Table 1. The relative mRNA expression was normalized to internal reference and determined using the comparative Cq method (2−ΔΔCq).
Effects of HF-18 on the Protein Virulence CagA
H. pylori SS1 and E. coli BL21 (DE3)-CagA suspensions at a final concentration of 1 × 107 CFU/ml were treated with serial diluted HF-18 (final concentrations: 8, 4 and 2 μg/ml or 2, 1 and 0.5 μg/ml) in Helicobacter Pylori Broth Medium supplemented with 7% FBS. After co-incubation for 8 h with H. pylori SS1 or 4 h with E. coli BL21 (DE3)-CagA, the washed bacteria were resuspended in 1 ml of PBS, broken using an ultrasonic cell crusher (model: SCIENT2-II D) followed by centrifugation at 12,000 rpm for 10 min and resuspension with PBS, subsequently mixed with 5 × loading buffer, and boiled at 100 °C for 10 min (Jafari and Mahmoodi 2021; Woo et al. 2020). After quantifying protein concentration using a BCA protein assay kit (Nanjing Yifeixue Biotechnology Co., Ltd., Nanjing, China), the protein samples were separated by SDS-PAGE, transferred into polyvinylidene fluoride membrane, and incubated with mouse anti-His monoclonal antibody followed by incubation with appropriate horseradish peroxidase-conjugated secondary antibody (goat anti-mouse IgG), and ultimately visualized using ECL reagents.
Statistical Analysis
Data were analysed by SPSS 22.0 software and presented as the mean ± SD. Comparison among groups was made by One-Way ANOVA Tukey Test of variance and Student t-test of unpaired data. P-value less than 0.05 was defined as significant differences. The graphs were made by GraphPad Prism software.
Results
Antibacterial Effects of HF-18 on Clarithromycin- and Amoxicillin- Resistant H. pylori SS1
The inhibitory activity of HF-18 against bacterial growth was evaluated by measuring MICs, MBCs and KCs values. As shown in Table 2, MICs of HF-18 against drug-resistant H. pylori SS1 and H. pylori 26695 were both 16 μg/ml, and MBCs were 32 μg/ml, respectively. Notably, the MIC and MBC of HF-18 against drug-resistant H. pylori were the same as positive control drug moxifloxacin, indicating that HF-18 had a potent antibacterial effect on H. pylori, especially for clinical drug-resistant H. pylori. In contrast, the MICs of amoxicillin and clarithromycin against drug-resistant H. pylori SS1 were more than 128 μg/ml, which were significantly bigger than those against H. pylori 26695. This result was consistent with the consequence after induction, suggesting that the antibacterial mechanism underlying HF-18 may be different from that of traditional antibiotics.
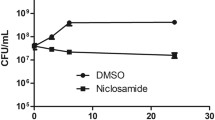
The KCs of HF-18 (4 × MIC, 64 μg/ml), moxifloxacin (4 × MIC, 64 μg/ml), amoxicillin (64 μg/ml) and clarithromycin (64 μg/ml) against clarithromycin- and amoxicillin- resistant H. pylori SS1 were performed using a standard inoculum of 1 × 105 CFU/ml. It can be seen (Fig. 1a) that HF-18 eliminated all H. pylori SS1 within 24 h, which was similar to that of moxifloxacin. Importantly, within 4–24 h, the bactericidal effect of peptide was significantly higher than that of moxifloxacin. Compared with the moxifloxacin, bacteria treated with HF-18 was decreased by nearly 2 log units during 8–12 h, indicating that this peptide was able to eliminate clarithromycin- and amoxicillin- resistant H. pylori SS1 rapidly. Consistently, inhibition zones (Fig. 1b) of HF-18 (0, 20, 40, 80 μg) also illustrated its antibacterial effects.
Bactericidal effect of HF-18 on clarithromycin- and amoxicillin- resistant H. pylori SS1 in vitro. The time-kill curves of HF-18 against clarithromycin- and amoxicillin- resistant H. pylori SS1 (a). Image of the inhibition zones of HF-18 (20, 40, 80 μg) against clarithromycin- and amoxicillin- resistant H. pylori SS1 (b). Growth curves of clarithromycin- and amoxicillin- resistant H. pylori SS1 under sub-inhibitory concentration of HF-18 treatment (c). Changes of urease reaction and hydrogen peroxide test under sub-inhibitory concentration of HF-18 stimulation (d)
In addition, as growth curves shown (Fig. 1c), 2, 4 and 8 μg/ml of HF-18 were sub-inhibitory against drug-resistant H. pylori SS1 (1 × 107 CFU/ml), and there was no growth inhibition among groups after 8 h. On the other hand, ureases and catalases are important virulence factors of H. pylori (Follmer 2010; Loewen et al. 2004), which can be determined by the changes of pH/color after decomposition of urea and bubble formation after incubating with 3% H2O2 (Fig. 1d). These results illustrated that HF-18 at sub-inhibitory concentration could reduce the activities of ureases and catalases without growth inhibitory effect.
Anti-inflammatory and Anti-adhesion Activities of Peptide HF-18 In Vitro
Results above showed that HF-18 had strong inhibitory effect on drug-resistant H. pylori SS1. Next, to further investigate the protection of HF-18 for GES-1 from drug-resistant H. pylori SS1 infection, the numbers of adherent colonies in the cell supernatant and intracellularly were counted after HF-18 treatment. Compared with the control group, HF-18 (64 μg/ml) could significantly reduce the number of bacteria in the cell culture supernatant (Fig. 2a) and intracellularly (Fig. 2b) by about 1.7 and 2.6 log units, respectively; however, moxifloxacin could only reduce the number of bacteria by about 1.4 and 1.5 log units, respectively. In contrast, clarithromycin and amoxicillin, to which H. pylori SS1 was resistant, had no significant antibacterial activity, manifesting that HF-18 could effectively scavenge the drug-resistant H. pylori SS1, thus reducing the number of bacteria in the supernatant and cells of GES-1.
Anti-inflammatory activities and anti-adhesion of HF-18 in vitro. Effects of HF-18 on the number of viable cells in the supernatant (a) and intracellularly (b) of GES-1 cells infected with clarithromycin- and amoxicillin- resistant H. pylori SS1. Effects of HF-18 on the mRNA transcription of inflammatory gene IL-8 of cells infected with drug-resistant H. pylori SS1 (c). Effects of HF-18 under sub-inhibitory concentrations on the adhesion of drug-resistant H. pylori SS1 towards GES-1 cells (d). Effects of HF-18 on the mRNA transcription of adhesion genes alpA (e) and alpB (f) of drug-resistant H. pylori SS1. Compared with the model group, *P < 0.05, **P < 0.01, ***P < 0.001. n = 3
In addition, bacterial infection can lead to the up-regulation of inflammatory factors (Yoshida and Yoshikawa 2002); thus, the influence of HF-18 on the transcription level of inflammatory genes IL-8 in GES-1 cells was also detected. After infection by drug-resistant H. pylori SS1, the transcription of IL-8 mRNA in GES-1 cells was significantly up-regulated (Fig. 2c). Comparatively, HF-18 (64 μg/ml) treatment down-regulated the expression of IL-8 mRNA by 1.5 times while positive drug moxifloxacin (16 μg/ml) reduced IL-8 mRNA by 1.3 times. In contrast, clarithromycin and amoxicillin had no effects on the transcription level of IL-8. It indicated that HF-18 may regulate the stress of immune systems induced by drug-resistant H. pylori SS1.
On the other hand, adhesins are proteins attached to the bacterial surface, with which bacteria can adhere to cells before intrusion into cells. Thus, adhesin of H. pylori is considered as an important virulence factor of bacteria, which is involved in many processes in the early and chronic stages of infection (Kalali et al. 2014). The effects of HF-18 on the adhesion of clarithromycin- and amoxicillin- resistant H. pylori SS1 to GES-1 cells were detected by counting of viable bacteria after co-incubation of cells with bacteria. Compared with the untreated group, HF-18 (4–8 μg/ml) reduced the adhesion of FITC-labeled H. pylori SS1 on the cells (Fig. 2d), reflecting as the significantly weakened green fluorescence. It indicated that this peptide had potent activities of anti-adhesion against drug-resistant H. pylori SS1. In order to further clarify the mechanism underlying HF-18 exerting anti-adhesion effect on drug-resistant H. pylori, HF-18 under sub-inhibitory concentrations (2, 4 and 8 μg/ml) were co-incubated with drug-resistant H. pylori and the influence of HF-18 on the transcription level of adhesion genes was explored. Consequently, HF-18 reduced the transcription of drug-resistant H. pylori SS1 adhesion gene (Fig. 2e, f) even under sub-inhibitory concentration. What's more, 8 μg/ml of peptide could down-regulate the mRNA transcription of adhesion genes alpA (Fig. 2e) and alpB (Fig. 2f) by 1.7 and 1.6 times respectively in a dose-dependent manner, indicating that this peptide not only killed bacteria quickly but also down-regulated the transcription of adhesion genes of drug-resistant H. pylori SS1.
HF-18 Destroyed the Membrane of Clarithromycin- and Amoxicillin- Resistant H. pylori SS1
To a certain extent, the bactericidal effects of antimicrobial peptides were positively correlated with the number of positive charges (Stone et al. 2019). Here, HF-18, carrying 8 positive charges, may interact with negatively charged bacterial membranes, thereby killing bacteria. Results from Zeta potential test (Fig. 3a) showed that the negative charges on the surface of drug-resistant H. pylori SS1 was − 24.7 ± 1.3 mV without peptide treatment. After incubating with HF-18 (4 × MIC), the negative charges were increased to − 14.4 ± 0.5 mV, indicating that HF-18 could neutralize the negative charges on the surface of clarithromycin- and amoxicillin- resistant H. pylori SS1. More intuitively, TEM was used to observe cell morphology in order to determine the effect of HF-18 on the integrity of bacterial membrane. The surface of bacteria in control group was smooth, and the structure was complete and curved (Fig. 3b). In HF-18 (4 × MIC) -treated group, H. pylori SS1 showed severe leakage of cytoplasmic contents with obvious morphological changes, including cytoplasmic aggregation and nuclear pyknosis, leading to substantial destruction of bacterial membrane. These results suggested that HF-18 could destroy the integrity of bacterial membrane to kill bacteria directly.
Effects of HF-18 on the membrane permeation of clarithromycin- and amoxicillin- resistant H. pylori SS1. Neutralization of negative charge on the surface of H. pylori SS1 by different concentrations of HF-18 (a). TEM was used to detect the morphological changes of drug-resistant H. pylori SS1 (yellow arrow: heterogeneous cytoplasm; red arrow: the leakage of intracellular components; green arrow: nuclear pyknosis) (b). NPN uptake assay for the permeability of H. pylori SS1 cell membrane after HF-18 treatment (c). Flow cytometry analysis of the destruction of bacterial membrane integrity under HF-18 stimulation (d). *P < 0.05, **P < 0.01, ***P < 0.001. n = 3 (Color figure online)
The activity of HF-18 on the permeability of H. pylori SS1 cell membrane was detected by NPN fluorescence uptake assay. It can be seen (Fig. 3c) that after treatment with HF-18, the fluorescence uptake of NPN was increased continuously. Compared with the control group, the NPN uptake rate in high dose group (4 × MIC) was increased by 5.2 times, manifesting that the bactericidal concentration of HF-18 rapidly disintegrated bacterial membrane. Because water-soluble staining PI can combine with nucleic acid (Akhavan et al. 2019; Riccardi and Nicoletti 2006), PI staining was used to further detect the permeability of HF-18 into bacterial cells. As can be seen (Fig. 3d), the positive staining rate of PI was as high as 95.8% after HF-18 treatment (4 × MIC), manifesting that HF-18 penetrated and disrupted the bacterial membrane, making PI enter bacterial cells and bind to nucleic acid. These results indicated that HF-18 with positive charges may interact with bacterial membrane to neutralize the negative charges and lysate bacterial cells.
HF-18 Down-regulates the Transcription cagA mRNA and the Expression of CagA Protein
CagA is one of the main virulence factors of H. pylori, which is injected into cells through T4SS secretion system (Tohidpour 2016). After tyrosine phosphorylation in cells, CagA interacts with multiple host signal molecules by tyrosine phosphorylation dependent/independent ways, and mediates intracellular signal transduction to promote the malignant transformation of gastric epithelial cells (Takahashi-Kanemitsu et al. 2020). In additon, at present, one of the reason why antimicrobial peptides are difficult to become clinical drugs is that it is difficult for antimicrobial peptides to reach bactericidal concentration under physiological conditions. Under this circumstances, the inhibitory effects on the transcription and expression of virulence proteins at sub-inhibitory concentration of peptides can lay a foundation for synergistic antimicrobial effects with other antibiotics in the future. Thus, the inhibition of CagA expression is beneficial to reduce the toxicity of H. pylori.
The recombinant E. coli BL21 (DE3)-CagA was constructed to explore the effects of HF-18 on CagA protein of H. pylori SS1. Firstly, as shown in Table 2, HF-18 had potent antibacterial activity against E. coli BL21 (DE3)-CagA (MIC: 2 μg/ml). In addition, HF-18 eradicated all the recombinant bacteria within 8 h (Fig. 4a) without recovering growth after 12 h and its bactericidal effect was similar to that of polymyxin; however, moxifloxacin killed all the recombinant bacteria after 8 h and its bactericidal effect was far less than that of HF-18, indicating that HF-18 exerted desirable activity against E. coli BL21 (DE3)-CagA. Then, the growth curve (Fig. 4b) showed that HF-18 with 0.25, 0.5 and 1 μg/ml had no growth inhibition on E. coli BL21 (DE3)-CagA. Furthermore, SDS-PAGE analysis showed that the expression level of CagA was the highest under 1 mM IPTG induction for 4 h (Fig. 4c).
HF-18 decreased the transcription of cagA mRNA and the expression of CagA protein in clarithromycin- and amoxicillin- resistant H. pylori SS1 and E. coli BL21 (DE3)-CagA. The KCs of HF-18 against E. coli BL21 (DE3)-CagA (a). Growth curves of E. coli BL21 (DE3)-CagA under sub-inhibitory concentration of HF-18 treatment (b). The changes of CagA protein expression at different time points and concentrations after IPTG induction (c). The effects of HF-18 at sub-inhibitory concentration (d) on the transcription of cagA mRNA and (e) on the expression of CagA protein in clarithromycin- and amoxicillin- resistant H. pylori SS1. The effects of HF-18 at sub-inhibitory concentration (f) on the transcription of cagA mRNA and (g) on the expression of CagA protein in E. coli BL21 (DE3)-CagA. *P < 0.05, **P < 0.01. n = 3
HF-18 at sub-inhibitory concentration could reduce the transcription of cagA mRNA and CagA protein of H. pylori SS1 and E. coli BL21 (DE3)-CagA. HF-18 at a concentration of 8 μg/ml could down-regulate cagA mRNA by 2.9 times (Fig. 4d) and CagA protein (Fig. 4e) in drug-resistant H. pylori SS1. Besides, HF-18 at the concentration of 1 μg/ml could down-regulate cagA mRNA (Fig. 4f) by 1.7 times and CagA protein (Fig. 4g), indicating that this peptide could reduce cagA mRNA and CagA protein of H. pylori SS1 and E. coli BL21 (DE3)-CagA. Data above suggest that HF-18 not only destroys bacterial membrane but also down-regulates virulence protein, which may provide new ideas for the treatment of H. pylori infection.
Discussion
H. pylori infection plays an important role in chronic gastritis, gastric ulcer and even gastric cancer. At present, the triple therapy is used in clinic. However, some side effects, such as abdominal pain, nausea, diarrhea, vomiting, etc., will also occur in the treatment, and the most serious problem is the emergence of a large number of drug-resistant strains, resulting in the gradual increase of treatment failure cases (Crosio et al. 2019; González et al. 2016; Knutson et al. 2005; Narayana et al. 2015). In such a dilemma, we urgently need to seek new treatments to improve or change the existing treatment.
Antibiotic based therapy has brought resistance of H. pylori in clinic. In this paper, to address problems of drug-resistance, clarithromycin- and amoxicillin- resistant H. pylori SS1 was successfully constructed to explore the antimicrobial activities of peptide HF-18 against drug-resistant H. pylori. Results showed that HF-18 could effectively resist H. pylori SS1 with MIC of 16 μg/ml and MBC of 32 μg/ml. Moreover, for CagA high expressed E. coli BL21 (DE3)-CagA, HF-18 also displayed a desirable antibacterial activity with MIC and MBC of 2 μg/ml and 8 μg/ml, respectively. In addition, E. coli BL21 (DE3)-CagA could be completely killed within 8 h after co-incubation with HF-18. Here, Zeta potential, NPN uptake and PI staining assays were used to confirm that HF-18 could penetrate into the inner and outer membranes of drug-resistant H. pylori SS1. Thus, the reason why HF-18 exerted a potently direct bactericidal efficiency against drug-resistant H. pylori was that HF-18 could penetrate into drug-resistant bacteria and consequently disrupted the integrity of bacterial membrane, resulting in the leakage of a large number of intracellular substances.
The main reason for the pathogenicity of H. pylori is that the adhesin secreted by H. pylori can tightly adhere to gastric epithelial cells. And a large amount of cytotoxins (CagA, VacA, SecA etc.) lead to persistent inflammatory reaction, and even mutate into gastric cancer in severe cases (Amieva and Peek 2016; Hatakeyama 2014). In this process, adhesion gene of H. pylori, virulence gene and inflammatory gene are undoubtedly of importance. As HF-18 could permeate into bacterial membrane, subsequently, RT-qPCR showed that HF-18 (8 μg/ml) could significantly down-regulate the expression of adhesion gene alpA/alpB and virulence gene cagA at mRNA level. At the cellular level, the adhesion of drug-resistant H. pylori SS1 to GES-1 cells was obviously weakened after treatment with this peptide; at the protein level, HF-18 also reduced the expression level of CagA. In addition, to further clarify the effect of HF-18 on CagA, a cytotoxin associated protein, the recombinant E. coli BL21 (DE3)-CagA was constructed and we found that HF-18 at dosage of sub-inhibitory concentration could down-regulate the expression of CagA both at mRNA and protein levels without affecting the growth of bacteria, which verified the above results again: HF-18 could enter into bacterial cells through membrane permeation and played a key role in down-regulating the transcription level of virulence genes. While, virulence protein CagA is injected into cytoplasm of host cells through T4SS secretion system, which is another important virulence factor in H. pylori. More attention should be paid on T4SS secretion systems for further study using H. pylori pre-mouse Sydney strain 1 (PMSS1), rather than SS1 strains, which is deficient of T4SS secretion systems (Draper et al. 2017; Dyer et al. 2018).
In the process of tissue damage and inflammation caused by drug-resistant H. pylori SS1 infection, inflammatory cells can further release cytokines and produce a cascade amplification effect. The role of IL-8 is particularly important, which is a powerful factor of cell chemotaxis and activation. It can cause neutrophil chemotaxis and mucosal inflammation induced by degranulation, and further lead to the occurrence and development of gastric diseases (Wiedemann et al. 2009). In this study, we constructed a cell model of GES-1 cells infected by H. pylori SS1, and found that HF-18 significantly down-regulated the expression of IL-8 at mRNA level. These results manifested that HF-18 reduced the transcription of adhesion gene, virulence gene of clarithromycin- and amoxicillin- resistant H. pylori SS1 after membrane permeation, and thus down-regulated inflammatory gene of GES-1 cells. Undeniably, there are many differences between the drug-resistant H. pylori induced by multi-step resistance selection in vitro and clinical drug-resistant H. pylori due to the different evolution ways, including phenotype and genotype. Therefore, the antibacterial effects of peptide should be further confirmed in H. pylori-infected patients with failed eradication in the future.
In conclusion, in this study, we further investigated the antibacterial effects of HF-18 on drug-resistant H. pylori SS1 and recombinant E. coli BL21 (DE3)-CagA and found that HF-18 could kill bacteria by neutralizing negative charges on the surface of bacteria, penetrating bacterial membrane and down- regulating the expression of adhesion genes alpA/alpB and virulence gene cagA. Moreover, HF-18 reduced transcription of IL-8, an important inflammatory factor, induced by drug-resistant H. pylori SS1 in GES-1 cells. Therefore, it will lay a theoretical foundation for the treatment of drug-resistant H. pylori.
Abbreviations
- CFU:
-
Colony forming unit
- Glu:
-
Glutamic acid
- Lys:
-
Lysine
- IPTG:
-
Isopropyl β-d-1-thiogalactopyranoside
References
Akhavan M, Foroughifar N, Pasdar H, Bekhradnia A (2019) Green synthesis, biological activity evaluation, and molecular docking studies of aryl alkylidene 2, 4-thiazolidinedione and rhodanine derivatives as antimicrobial agents. Comb Chem High Throughput Screen 22(10):716–727. https://doi.org/10.2174/1386207322666191127103122
Amieva M, Peek RM Jr (2016) Pathobiology of helicobacter pylori-induced gastric cancer. Gastroenterology 150(1):64–78. https://doi.org/10.1053/j.gastro.2015.09.004
Annunziato G (2019) Strategies to overcome antimicrobial resistance (AMR) making use of non-essential target inhibitors: a review. Int J Mol Sci. https://doi.org/10.3390/ijms20235844
Bugaytsova JA, Björnham O, Chernov YA, Gideonsson P, Henriksson S, Mendez M et al (2017) Helicobacter pylori adapts to chronic infection and gastric disease via pH-responsive BabA-mediated adherence. Cell Host Microbe 21(3):376–389. https://doi.org/10.1016/j.chom.2017.02.013
Crosio MA, Via MA, Cámara CI, Mangiarotti A, Del Pópolo MG, Wilke N (2019) Interaction of a polyarginine peptide with membranes of different mechanical properties. Biomolecules. https://doi.org/10.3390/biom9100625
De Leeuw E, Li C, Zeng P, Li C, Diepeveen-de Buin M, Lu WY et al (2010) Functional interaction of human neutrophil peptide-1 with the cell wall precursor lipid II. FEBS Lett 584(8):1543–1548. https://doi.org/10.1016/j.febslet.2010.03.004
Draper JL, Hansen LM, Bernick DL, Abedrabbo S, Underwood JG, Kong N et al (2017) Fallacy of the unique genome: sequence diversity within single helicobacter pylori strains. Mbio. https://doi.org/10.1128/mBio.02321-16
Dyer V, Brüggemann H, Sörensen M, Kühl AA, Hoffman K, Brinkmann V et al (2018) Genomic features of the helicobacter pylori strain PMSS1 and its virulence attributes as deduced from its in vivo colonisation patterns. Mol Microbiol 110(5):761–776. https://doi.org/10.1111/mmi.14123
Follmer C (2010) Ureases as a target for the treatment of gastric and urinary infections. J Clin Pathol 63(5):424–430. https://doi.org/10.1136/jcp.2009.072595
González R, Mendive-Tapia L, Pastrian MB, Albericio F, Lavilla R, Cascone O, Iannucci NB (2016) Enhanced antimicrobial activity of a peptide derived from human lysozyme by arylation of its tryptophan residues. J Pept Sci 22(2):123–128. https://doi.org/10.1002/psc.2850
Hahn AW, Jain R, Spach DH (2016) New approaches to antibiotic use and review of recently approved antimicrobial agents. Med Clin North Am 100(4):911–926. https://doi.org/10.1016/j.mcna.2016.03.012
Hatakeyama M (2014) Helicobacter pylori CagA and gastric cancer: a paradigm for hit-and-run carcinogenesis. Cell Host Microbe 15(3):306–316. https://doi.org/10.1016/j.chom.2014.02.008
Helander IM, Mattila-Sandholm T (2000) Fluorometric assessment of gram-negative bacterial permeabilization. J Appl Microbiol 88(2):213–219. https://doi.org/10.1046/j.1365-2672.2000.00971.x
Jafari E, Mahmoodi S (2021) Design, expression, and purification of a multi-epitope vaccine against helicobacter pylori based on melittin as an adjuvant. Microb Pathog 157:104970. https://doi.org/10.1016/j.micpath.2021.104970
Jiang M, Ma L, Huang Y, Wu H, Dou J, Zhou C (2020a) Antimicrobial activities of peptide Cbf-K(16) against drug-resistant helicobacter pylori infection in vitro and in vivo. Microb Pathog 138:103847. https://doi.org/10.1016/j.micpath.2019.103847
Jiang M, Yang X, Wu H, Huang Y, Dou J, Zhou C, Ma L (2020b) An active domain HF-18 derived from hagfish intestinal peptide effectively inhibited drug-resistant bacteria in vitro/vivo. Biochem Pharmacol 172:113746. https://doi.org/10.1016/j.bcp.2019.113746
Kalali B, Mejías-Luque R, Javaheri A, Gerhard M (2014) H. pylori virulence factors: influence on immune system and pathology. Mediators Inflamm 2014:426309. https://doi.org/10.1155/2014/426309
Kalenić S, Plecko V, Kresić S, Presecki V, Tripković V, Zele-Stracević L et al (1998) Helicobacter pylori: in vitro induction of resistance to azithromycin. Chemotherapy 44(1):17–20. https://doi.org/10.1159/000007085
Knutson MD, Oukka M, Koss LM, Aydemir F, Wessling-Resnick M (2005) Iron release from macrophages after erythrophagocytosis is up-regulated by ferroportin 1 overexpression and down-regulated by hepcidin. Proc Natl Acad Sci USA 102(5):1324–1328. https://doi.org/10.1073/pnas.0409409102
Lin Y, Kawai S, Sasakabe T, Nagata C, Naito M, Tanaka K et al (2021) Effects of Helicobacter pylori eradication on gastric cancer incidence in the Japanese population: a systematic evidence review. Jpn J Clin Oncol 51(7):1158–1170. https://doi.org/10.1093/jjco/hyab055
Loewen PC, Carpena X, Rovira C, Ivancich A, Perez-Luque R, Haas R et al (2004) Structure of helicobacter pylori catalase, with and without formic acid bound, at 1.6 A resolution. Biochemistry 43(11):3089–3103. https://doi.org/10.1021/bi035663i
Ma L, Wang Y, Wang M, Tian Y, Kang W, Liu H et al (2016) Effective antimicrobial activity of Cbf-14, derived from a cathelin-like domain, against penicillin-resistant bacteria. Biomaterials 87:32–45. https://doi.org/10.1016/j.biomaterials.2016.02.011
Ma L, Xie X, Liu H, Huang Y, Wu H, Jiang M et al (2020) Potent antibacterial activity of MSI-1 derived from the magainin 2 peptide against drug-resistant bacteria. Theranostics 10(3):1373–1390. https://doi.org/10.7150/thno.39157
Moosazadeh Moghaddam M, Eftekhary M, Erfanimanesh S, Hashemi A, Fallah Omrani V, Farhadihosseinabadi B et al (2018) Comparison of the antibacterial effects of a short cationic peptide and 1% silver bioactive glass against extensively drug-resistant bacteria, Pseudomonas aeruginosa and Acinetobacter baumannii, isolated from burn patients. Amino Acids 50(11):1617–1628. https://doi.org/10.1007/s00726-018-2638-z
Narayana JL, Huang HN, Wu CJ, Chen JY (2015) Epinecidin-1 antimicrobial activity: in vitro membrane lysis and In vivo efficacy against helicobacter pylori infection in a mouse model. Biomaterials 61:41–51. https://doi.org/10.1016/j.biomaterials.2015.05.014
Neshani A, Zare H, Akbari Eidgahi MR, Hooshyar Chichaklu A, Movaqar A, Ghazvini K (2019) Review of antimicrobial peptides with anti-helicobacter pylori activity. Helicobacter 24(1):e12555. https://doi.org/10.1111/hel.12555
Otvos L Jr, Ostorhazi E, Szabo D, Zumbrun SD, Miller LL, Halasohoris SA et al (2018) Synergy between proline-rich antimicrobial peptides and small molecule antibiotics against selected gram-negative pathogens in vitro and in vivo. Front Chem 6:309. https://doi.org/10.3389/fchem.2018.00309
Pan CY, Tsai TY, Su BC, Hui CF, Chen JY (2017) Study of the antimicrobial activity of tilapia piscidin 3 (TP3) and TP4 and their effects on immune functions in hybrid tilapia (Oreochromis spp.). PLoS ONE 12(1):e0169678. https://doi.org/10.1371/journal.pone.0169678
Pellicano R, Ribaldone DG, Fagoonee S, Astegiano M, Saracco GM, Mégraud F (2016) A 2016 panorama of helicobacter pylori infection: key messages for clinicians. Panminerva Med 58:304–317
Riccardi C, Nicoletti I (2006) Analysis of apoptosis by propidium iodide staining and flow cytometry. Nat Protoc 1(3):1458–1461. https://doi.org/10.1038/nprot.2006.238
Rothenbacher D, Brenner H (2003) Burden of helicobacter pylori and H. pylori-related diseases in developed countries: recent developments and future implications. Microbes Infect 5(8):693–703. https://doi.org/10.1016/s1286-4579(03)00111-4
Ryu S, Song PI, Seo CH, Cheong H, Park Y (2014) Colonization and infection of the skin by S. aureus: immune system evasion and the response to cationic antimicrobial peptides. Int J Mol Sci 15(5):8753–8772. https://doi.org/10.3390/ijms15058753
Saadat I, Higashi H, Obuse C, Umeda M, Murata-Kamiya N, Saito Y et al (2007) Helicobacter pylori CagA targets PAR1/MARK kinase to disrupt epithelial cell polarity. Nature 447(7142):330–333. https://doi.org/10.1038/nature05765
Stein M, Bagnoli F, Halenbeck R, Rappuoli R, Fantl WJ, Covacci A (2002) c-Src/Lyn kinases activate helicobacter pylori CagA through tyrosine phosphorylation of the EPIYA motifs. Mol Microbiol 43(4):971–980. https://doi.org/10.1046/j.1365-2958.2002.02781.x
Stone TA, Cole GB, Ravamehr-Lake D, Nguyen HQ, Khan F, Sharpe S, Deber CM (2019) Positive charge patterning and hydrophobicity of membrane-active antimicrobial peptides as determinants of activity, toxicity, and pharmacokinetic stability. J Med Chem 62(13):6276–6286. https://doi.org/10.1021/acs.jmedchem.9b00657
Suthisamphat N, Dechayont B, Phuaklee P, Prajuabjinda O, Vilaichone RK, Itharat A et al (2020) Anti-helicobacter pylori, anti-inflammatory, cytotoxic, and antioxidant activities of mace extracts from Myristica fragrans. Evid Based Complement Alternat Med 2020:7576818. https://doi.org/10.1155/2020/7576818
Takahashi-Kanemitsu A, Knight CT, Hatakeyama M (2020) Molecular anatomy and pathogenic actions of helicobacter pylori CagA that underpin gastric carcinogenesis. Cell Mol Immunol 17(1):50–63. https://doi.org/10.1038/s41423-019-0339-5
Tenney JH, Maack RW, Chippendale GR (1983) Rapid selection of organisms with increasing resistance on subinhibitory concentrations of norfloxacin in agar. Antimicrob Agents Chemother 23(1):188–189. https://doi.org/10.1128/aac.23.1.188
Thapa RK, Diep DB, Tønnesen HH (2020) Topical antimicrobial peptide formulations for wound healing: current developments and future prospects. Acta Biomater 103:52–67. https://doi.org/10.1016/j.actbio.2019.12.025
Theuretzbacher U, Outterson K, Engel A, Karlén A (2020) The global preclinical antibacterial pipeline. Nat Rev Microbiol 18(5):275–285. https://doi.org/10.1038/s41579-019-0288-0
Tohidpour A (2016) CagA-mediated pathogenesis of helicobacter pylori. Microb Pathog 93:44–55. https://doi.org/10.1016/j.micpath.2016.01.005
Torres MDT, Sothiselvam S, Lu TK, de la Fuente-Nunez C (2019) Peptide design principles for antimicrobial applications. J Mol Biol 431(18):3547–3567. https://doi.org/10.1016/j.jmb.2018.12.015
Wiedemann T, Loell E, Mueller S, Stoeckelhuber M, Stolte M, Haas R, Rieder G (2009) Helicobacter pylori cag-pathogenicity island-dependent early immunological response triggers later precancerous gastric changes in Mongolian gerbils. PLoS ONE 4(3):e4754. https://doi.org/10.1371/journal.pone.0004754
Wiegand I, Hilpert K, Hancock RE (2008) Agar and broth dilution methods to determine the minimal inhibitory concentration (MIC) of antimicrobial substances. Nat Protoc 3(2):163–175. https://doi.org/10.1038/nprot.2007.521
Woo HJ, Yang JY, Lee MH, Kim HW, Kwon HJ, Park M et al (2020) Inhibitory effects of β-caryophyllene on helicobacter pylori Infection in vitro and in vivo. Int J Mol Sci. https://doi.org/10.3390/ijms21031008
Yang Y, Bian L, Hang X, Yan C, Huang Y, Ye F et al (2020) In vitro activity of new tetracycline analogues omadacycline and eravacycline against clinical isolates of helicobacter pylori collected in China. Diagn Microbiol Infect Dis 98(3):115129. https://doi.org/10.1016/j.diagmicrobio.2020.115129
Yeaman MR, Yount NY (2003) Mechanisms of antimicrobial peptide action and resistance. Pharmacol Rev 55(1):27–55. https://doi.org/10.1124/pr.55.1.2
Yoshida N, Yoshikawa T (2002) Effect of helicobacter pylori-mediated inflammation on nonsteroidal anti-inflammatory drugs-induced gastric mucosal injury. Keio J Med 51(Suppl 2):45–50. https://doi.org/10.2302/kjm.51.supplement2_45
Acknowledgements
This work was funded by the National Natural Science Foundation of China (Grant No. 82173863; No.81803591); National Key Research and Development Program of China (Grant No. 2018YFA0902000); the fellowship of China postdoctoral science foundation (Grant No. 2020T130723); Natural Science Foundation of Jiangsu Province of China (Grant No. BK20201327); the Basic Scientific Research Business Expense Project of China Pharmaceutical University (Grant No. 2632021ZD07)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there are no competing interests in this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zhou, C., Jiang, M., Ye, X. et al. Antibacterial Activities of Peptide HF-18 Against Helicobacter pylori and its Virulence Protein CagA. Int J Pept Res Ther 28, 63 (2022). https://doi.org/10.1007/s10989-022-10372-7
Accepted:
Published:
DOI: https://doi.org/10.1007/s10989-022-10372-7