Abstract
Antimicrobial peptides (AMPs) offer a potent and effective alternative for treatment of antibiotic resistant microbes. Mastoparans or mastoparan like peptides are the most abundant peptides reported in vespid/social wasp venoms with potent antimicrobial activity. Polybia MP-1 is an amphipathic tetradecapeptide isolated from the venom of the vespid wasp Polybia paulista with potent antimicrobial activity and high selectivity for bacterial membranes. In the present study, the antimicrobial activity of Polybia MP-1 was evaluated against antibiotic resistant Pseudomonas aeruginosa isolated from mastitic cow milk samples. The isolates (n = 20) were obtained from mastitic milk samples and screened for sensitivity to antibiotics (Amikacin, Ciprofloxacin, Gentamycin, Imipenem, Ceftazidime, Colistin, Ceftriaxone and Aztreonam) by disc diffusion assay. The isolates were also characterized for the presence of different genes (n = 27) by polymerase chain reaction (PCR). These genes encoded for virulence factors, biofilm formation and antibiotic resistance. A correlation study was carried out to establish the significance of presence of antibiotic resistant genes i.e. blaTEM, blaCTX−M, blaSHV and blaOXA and resistance against different antibiotics for the bacterial isolates. Out of twenty, 7 isolates were found to be multiple drug resistant (MDR). We determined the minimum inhibitory concentration (MIC) of synthetic peptide, Polybia MP-1 against P. aeruginosa (ATCC 27853) and it was found to be 75 µM (124 µg/mL) whereas its minimum bactericidal concentration (MBC) was found to be 150 µM (2 X MIC). The Polybia MP-1 was able to effectively inhibit the growth of 5 out of 7 (71 %) MDR isolates at 6 X MIC (450 µM). The Polybia MP-1 was highly membrane selective and hence showed very low to moderate haemolytic activity against cattle, buffalo and goat red blood cells (RBCs). It further showed potent anti-biofilm activity against P. aeruginosa ATCC 27853 at 8 X MIC (600 µM). Thus, synthetic Polybia MP-1 has potent antimicrobial activity against antibiotic resistant P. aeruginosa and can be explored as an alternative to antibiotics for the management of disease conditions like mastitis in cattle.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
An opportunistic pathogen, Pseudomonas aeruginosa is often responsible for many life-threatening infections in humans and animals alike. It is a Gram negative; rod shaped, aerobic bacterium belonging to the family Pseudomonadaceae and is found almost in all environments like soil, water and sediment (Meng 2020). P. aeruginosa is often responsible for several nosocomial infections in humans especially in cystic fibrosis, burn wounds and immunocompromised patients. It has also been identified as an animal pathogen and as a frequent cause of mastitis in cattle (Daly et al. 1999). Mastitis is the inflammation of the udder leading to a reduction of both quality and quantity of milk. Besides the losses in production, the cost incurred on treatment, result in great economic losses to the dairy industry (Yang et al. 2019). Mastitis is an economic problem of dairy farms affecting all milk-producing ruminants all over the world and especially in India, the largest milk-producing country in the world. In India, annual economic loss incurred by dairy industry on account of udder infections is estimated to be Rs. 6053.21 crores and out of which loss of Rs. 4365.32 crore (70–80 per cent) has been attributed to sub-clinical mastitis (NAAS 2013). The P. aeruginosa can cause severe clinical mastitis, as well as, subclinical chronic mastitis. It causes the disease through contamination of the environment or when the host immunity is compromised due to stress, disease, or nutritional imbalances. In case of mastitis the bacterium has been reported in sources such as soil and water (like hoses used in the milking parlour, water and spray nozzles, damp bedding, and muddy pastures). Contaminated antibiotic solutions, teat dip and wipes, and intra-mammary treatment tubes can also be the cause of acute and sub-acute mastitis in dairy animals (Kelly and Wilson 2016).
The P. aeruginosa possesses a genome of 6–7 Mb encoding around 6000 genes and many of these encode a range of virulence factors that render it pathogenic (Cao et al. 2017). These factors can be either extracellular or cell associated. The extracellular factors may include exotoxin A, proteases like elastase and biofilm related proteins. Factors associated with cells may include lipopolysaccharide, pili, flagella, alginate, type III secretion system (T3SS), effector proteins for type III system, and pigment production (Finnan et al. 2004).
Antimicrobials are used widely for the treatment and prevention of mastitis. Often, excessive, prolonged and imprudent usage of antibiotics has led to the development of antimicrobial resistance (AMR) in many mastitis causing micro-organisms like Staphylococcus aureus, Klebsiella pneumoniae, Escherichia coli and P. aeruginosa (Saini et al. 2012; Boireau et al. 2018; Ameen et al. 2019). The AMR in P. aeruginosa has become a challenge for both human and animal health care professionals. The bacterium possesses intrinsic resistance because of natural low membrane permeability, production of antibiotic inactivating enzymes and expression of efflux pumps to expel antibiotics. Being a potent biofilm former, it has adaptive resistance against antibiotics whereby biofilm formation results in difficult accessibility of antibiotics to the bacterial cells. The P. aeruginosa can also acquire resistance through horizontal gene transfer or mutations (Pang 2019).
Antimicrobial peptides (AMPs) offer a viable alternative to overcome the menace of AMR. These are short cationic peptides ubiquitously found in various organisms as an important part of the innate immune system. They possess antimicrobial activity through diverse mechanisms which basically involve direct interaction with the bacterial membrane but can act indirectly through interaction with DNA, RNA or protein and modulating the host defense system as well. As a result of diverse mechanisms of action and multiple targets, AMPs can evade development of resistance by bacteria (Mahlapuu et al. 2016). As a result of their high antimicrobial efficacy AMPs can be used for the treatment of multiple drug resistant (MDR) microbes (Gupta et al. 2021). AMPs are obtained both from natural sequences as well as recent advances in computer aided design and advanced Artificial Intelligence (AI) based algorithms have made it easier to develop newer synthetic sequences of immense antimicrobial potential. AI based Deep ABPpred classifier has recently been developed to identify novel AMPs in protein sequences (Sharma et al. 2021a). In another study, an AI based model AniAMPpred has been developed to search for novel AMPs in the genome of animals (Sharma et al. 2021b). The antimicrobial activity of linear peptides can be further enhanced by multimerization (Gogoi et al. 2021), or glycosylation and lipidation (Li et al. 2021).
Wasp venoms have been rigorously searched for the presence of bioactive peptides especially AMPs. Mastoparans or mastoparan like peptides are the most abundant peptides reported in vespid/social wasp venoms with mast cell degranulating and histamine releasing principles (Palma 2013). First Mastoparan was obtained from the venom of the vespid wasp P. lewisii (Hirai et al. 1979). The mastoparans are generally tetradecapeptides i.e. 14 amino acids long with abundant hydrophobic residues such as leucine, isoleucine, valine and alanine. They mostly attain random coiled structure in water but assume α- helical structure on interaction with appropriate environments such as lipids and methanol. The abundance of hydrophobic and basic residues render them amphipathic and is thus responsible for their various biological activities like mast cell degranulation and histamine release, interactions with the plasma membrane and hemolysis (Konno et al. 2019).
The mastoparan peptide, Polybia MP-1 (NH2-IDWKKLLDAAKQIL-CONH2) obtained from the venom of the vespid wasp Polybia paulista is a potent AMP and intensively studied for its broad antimicrobial activity and low hemolytic activity (Souza et al. 2005; Dos Santos Cabrera 2008; Luong et al. 2017). In the present study, the isolates were assessed for antibiotic sensitivity and presence of different virulence factors. The antibacterial activity of Polybia MP-1 was evaluated against MDR P. aeruginosa isolated from mastitic milk samples. For any molecule to be effective as an intra-mammary infusion, the stability of active agent in the presence of milk is of utmost importance (Schmelcher et al. 2015; Li et al. 2017). The stability of the peptide was evaluated in different body fluids like serum and urine and also evaluated in milk. Further, the ability of synthetic Polybia MP-1 to disrupt P. aeruginosa biofilms and hemolysis of RBCs was also assessed.
Materials and Methods
Chemicals and Bacterial Strains
The chemicals for peptide synthesis viz. Rink amide MBHA resin (4-(2′,4′-Dimethoxyphenyl-Fmoc-aminomethyl)-phenoxyacetamido-norleucyl-Methylbenzhydrylamine hydrochloride resin, loading efficiency 0.8 mmol/gm), N, N′-Diisopropylcarbodiimide/ Hydroxybenzotriazole (DIPC/HOBt), and Fmoc protected aminoacid derivatives were purchased from NovaBiochem. The solvents like piperidine, Trifluoracetic acid (TFA), Triisopropylsilane (TIPS), Thioanisole, 1,2-Ethanedithiol (EDT), Phenol and HPLC grade water were from Merck, Germany.
Bacterial culture media like Mueller-Hinton Agar (MHA), Mueller-Hinton Broth (MHB), Brain Heart Infusion broth (BHI), Pseudomonas selective agar medium, Tryptone Soy Broth (TSB), standard antibiotic discs and standard isolate of P. aeruginosa (ATCC 27853) were purchased form HiMedia, India. Further, P. aeruginosa isolates were obtained from mastitic cow milk samples and used after phenotypic and genotypic characterization with regards to antibiotic sensitivity.
Synthesis and Purification of Peptide
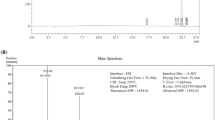
Polybia MP-1 (NH2-IDWKKLLDAAKQIL-CONH2) was synthesized by solid phase peptide synthesis methodology on Rink amide MBHA resin (loading efficiency 0.8 mmol/gm) using the standard 9-fluorenyl-methoxycarbonyl (Fmoc) coupling chemistry (Merrifield 1963). The DIPC/ HOBt method was used for activation of each aminoacid derivative and 20 % piperidine was used for removal of the Fmoc protecting group from the growing peptide chain. After completion of amino acid sequence, the peptide was cleaved by K reagent (85 % TFA, 1 % TIPS, 5 % Thioanisole, 2.5 % EDT, 1.5 % Phenol and 5 % HPLC grade water). The cleaved peptide was precipitated and washed several times with chilled diethyl ether and dried under vacuum. The peptide was reconstituted in HPLC grade water and desalted on ODS silica column to remove the salt impurities. The peptide was further purified by reverse phase high pressure liquid chromatography (RP-HPLC) (Shimadzu, Japan) on a C18 column (Shim-pack GIST C18 5 μm, 250 × 14 mm) using a linear acetonitrile: water gradient (95 to 5 %) in presence of 0.05 % TFA at a flow rate of 1.5 ml per minute.
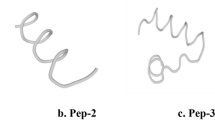
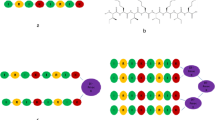
Physicochemical Analysis and Structure Prediction
In silico physicochemical analysis (molecular weight, net charge, hydrophobic ratio, theoretical PI) and structure prediction (two-dimensional (2-D) structure and helical wheel projection) of Polybia MP-1 was carried out by online available software PepCalc (https://pepcalc.com/ (Innovagen)-Peptide property calculator), PepFold3 (https://bioserv.rpbs.univ-paris-diderot.fr/services/PEP-FOLD3/) and Heliquest (http://heliquest.ipmc.cnrs.fr.).
Determination of Minimum Inhibitory Concentration (MIC) and Minimum Bactericidal Concentration (MBC)
MIC for Polybia MP-1 against P. aeruginosa ATCC 27853 was determined by the standard broth microdilution assay performed in a 96 well microtiter plate as per the method of Wiegand et al. 2008. The bacterial culture was grown overnight at 37 °C in MHB till mid log phase (OD600 0.3 approximately equivalent to 2 × 108 cells/mL) and used for the assay. These cells were further diluted to a final concentration of 106cells/mL in fresh MHB for seeding in wells. Two-fold serial dilutions of the peptide ranging from 25 µM to 300 µM were prepared in 50 µL of sterile water. To these dilutions 50 µL of 106 cells/mL in MHB were added. The final concentration of cells was 5 × 105cells/mL in total 100 µL of final mixture. Ciprofloxacin at the breakpoint of 1 µg/mL was used as the positive control and cells with no treatment were used as the normal control. This plate was incubated at 37 °C for 24 h in a humidified chamber and OD600 was taken in a microplate reader (Multiskan Go, Thermo Fischer Scientific, USA). MIC was defined as the minimum concentration of the peptide which inhibited more than 99 % visible growth of bacterial cells after incubation of 24 h at 37 °C.
For determining MBC, a microdilution assay plate was set up with predetermined concentrations i.e. half of MIC, MIC, 2X MIC, 4X MIC, 8X MIC and 16X MIC of the peptide similar to the method mentioned for MIC determination. After incubating the plate for 24 h at 37 °C, 10 µL was taken from each well and diluted 10,000 times in sterile PBS. This dilution was then spread plated on MHA plates and plates were incubated overnight at 37 °C. MBC was defined as the minimum concentration of the peptide which completely (> 99.9 %) eliminated bacterial growth on MHA plates.
Time Dependent Determination of Complete Elimination Concentration (CE Values) by Drop Plate Method
CE values were determined for Polybia MP-1 against P. aeruginosa ATCC 27853 based on the method described by Farkas et al. (2018) with some modifications. The bacterial culture was grown overnight at 37˚C in MHB till mid log phase (OD600 0.3 approximately equivalent to 2 × 108 cells/mL) and it was further diluted to 106 cells /mL in fresh MHB. To 50 µL of this culture, 50 µL of different two-fold peptide dilutions (0.5, 1, 2, 4 times of MIC), MIC of Amikacin (8 µg/mL) and MIC of Ciprofloxacin (1 µg/mL) made in sterile water, were added. The final concentration of cells in 100 µL corresponded to 5 × 105 cells/mL. These mixtures were incubated at 37 °C and 2 µL drops from them were placed on MHA plates after 0, 15, 30, 45, 60, 120 and 180 min of incubation. The drops were allowed to dry and the plates were incubated in an inverted position at 37 °C overnight. This experiment was carried out in triplicate.
Stability of Peptide in Serum, Urine and Milk
Antimicrobial activity of Polybia MP-1 at MIC and 5 × MIC was assessed in presence of different amounts (i.e. 6.25 %, 12.5 and 25 %) of bovine serum, urine and defatted raw cow milk by broth microdilution assay as stated in MIC determination section, against P. aeruginosa ATCC 27853. These concentrations of different fluids were selected to evaluate if the molecule is active in presence of different body fluids.
Haemolytic Activity
Haemolytic activity of Polybia MP-1 was assessed as the amount of haemoglobin released by the lysis of red blood cells (RBCs). Polybia MP-1 was assessed for haemolytic activity against erythrocytes from different species viz., cattle, buffalo and goat, as per the procedure described by Bhagavathula et al. (2017) and Tan et al. (2017) with minor modifications. Blood from healthy animals was collected in EDTA vials and RBCs were collected by centrifugation at 1000 g for 5 min at 4 °C. The collected RBCs were washed in Alsever’s solution (pH 6.1) and stored overnight at 4 °C for ageing. Overnight-aged RBCs were washed with fresh sterile Alsever’s solution (pH 6.1), then resuspended to 4 % in the same buffer. 80 µL of 4 % RBC solution was incubated with 20 µL buffer containing various amounts of Polybia MP-1 i.e. 2.5, 5, 10, 25, 50, 75, 100, 150 and 200 µM in 0.6mL micro-centrifuge tubes. After incubation at 37 °C for 1 h, the mixtures were centrifuged (1000 g, 5 min, 4 °C) and the supernatants were transferred to a 96-well plate. The amount of haemoglobin released was assessed by measuring absorbance at 570 nm using a microplate reader. 4 % RBC suspension with buffer alone (Ablank) and 20 µL of 0.1 % Triton X-100 (Atriton) were used as control samples for 0 and 100 % hemolysis respectively. Hemolysis was calculated as per the equation:
Isolation, Identification and Characterization of P. aeruginosa isolates from mastitic cow milk samples
The P. aeruginosa isolates were obtained from mastitic cow milk samples collected from different dairy farms. 1 ml of the collected milk samples were added to 9 ml of sterile BHI broth for enrichment and incubated overnight at 37 °C. These overnight grown cultures were then streaked on Pseudomonas selective agar medium and the plates were further incubated in an inverted position at 37 °C. Single colonies were picked and transferred to BHI broth and mid log phase cultures (OD600 0.3 approximately equivalent to 2 × 108 cells/mL) were utilized for isolation of DNA by CTAB method as described by Minas et al. (2011). The isolates were further identified genotypically by setting up a multiplex polymerase chain reaction (PCR) for the genes 16SrDNA, oprL and gyrB at an annealing temperature of 60˚C. The confirmed isolates were assessed further for the presence and absence of virulence, biofilm formation and antibiotic resistance genes by PCR (Table 1). Primer sequences used were previously mentioned by Finnan et al. (2004), Dhanawade et al. (2010), Salman et al. (2013) and Fazeli and Momtaz (2014).
Antibiogram of P. aeruginosa Isolates From Mastitic Milk
Susceptibility of the isolates to different antibiotics was assessed by Kirby- Bauer disc diffusion assay (Bauer, 1966) for eight antibiotics namely Amikacin 30 µg (AK 30), Ciprofloxacin 5 µg (CIP 5), Gentamycin 10 µg (GEN 10), Imipenem 10 µg (IPM 10), Ceftazidime 30 µg (CAZ 30), Colistin (CL 10), Ceftriaxone 30 µg (CTR 30) and Aztreonam 30 µg (AT 30). These belonged to different classes of antibiotics such as aminoglycosides (AK 30 and GEN 10), fluoroquinolone (CIP 5), carbapenem (IMP 10), cephalosporin (CAZ 30 and CTR 30), Polymyxin E (CL 10) and new generation β-lactam (AT 30). An isolate resistant to three or more than three antimicrobial classes is defined as Multiple Drug Resistant (MDR) (Magiorakos et al. 2012).
Antimicrobial Activity of Polybia MP-1 Against P. aeruginosa Isolates From Mastitic Milk
The antimicrobial activity of Polybia MP-1 was assessed against P. aeruginosa isolates (n = 20) by broth micro-dilution assay as mentioned for MIC determination at a concentration of MIC, 2 × MIC, 4 × MIC and 6 × MIC i.e. 75, 150, 300 and 450 µM, respectively.
Crystal Violet Biofilm Reduction Assay
To examine the ability of Polybia MP-1 to disrupt Pseudomonas biofilms crystal violet biofilm reduction assay was performed in 96 well cell culture microtiter plate as described by Shukla and Rao (2017). For the formation of biofilms of P. aeruginosa ATCC 27853, 10 µl of bacterial cell suspension having an OD600 of 0.5 (approximately 2 × 109 cells/mL) was inoculated in 190 µl of TSB medium with 1 % glucose in each well of a 96 well flat bottom tissue culture plate and the plate was incubated at 37 °C for 24 h. Next day after aspiration of planktonic cells, different concentrations of Polybia MP-1 (1, 2, 4, 8 times of MIC) and Tetracycline (1 (16 µg/mL), 2, 4, 8 times of MIC) were added to wells in fresh TSB in triplicates. The plate was further incubated for 24 h at 37 °C and planktonic/detached cells were removed by flicking the plate. The biofilm was then fixed with 99 % methanol for 15 min. After fixing, the biofilms were washed twice with phosphate buffer saline (PBS) and air-dried. 200 µl of 0.2 % solution of crystal violet was added to all the wells and after an incubation of 15 min, the excess crystal violet was removed. Two washes with PBS were given and the plate was air dried. In the end, the crystal violet taken up by the cells was dissolved in 33 % acetic acid and biofilm mass was monitored in terms of OD570 using a microplate reader.
Statistical Analysis
All the results are reported as mean ± SEM and total variation present in between groups was determined by analysis of variance (ANOVA, one way or two way). Tukey’s multiple comparison test was used for post-test. Correlation between presence of antibiotic resistant genes viz., bla TEM, bla CTX-M, bla SHV, bla OXA and antibiotic resistance for AK 30, CIP 5, GEN 10, IPM 10, CAZ 30, CL 10, CTR 30 and AT 30 was determined by Pearson’s method and the correlation coefficients (r) and significance (P) were given, and the significant levels were defined at p < 0.05 (*) and p < 0.01 (**).
Results
Synthesis and Physicochemical Properties of Polybia MP-1
Polybia MP-1 was obtained with a free N terminal and a C terminal amide group after cleavage from Rink amide MBHA resin. After HPLC purification, the peptide had > 90 % purity. The physicochemical properties viz., molecular weight, net charge, isoelectric point, hydrophobic moment, hydrophobic residue %, GRAVY score and solubility of Polybia MP-1 are mentioned in Table 2. Helical wheel projection and three-dimensional (3D) structure of the peptide are mentioned in Fig. 1a and b.
Determination of MIC and MBC
On screening against a range of concentrations of Polybia MP-1 viz., 25 to 300 µM, the MIC was found to be 75 µM i.e. 124 µg/mL (Fig. 2). There was no increase at OD600 after incubation at 37 °C for 24 h at a concentration of 75 µM and above. 100 % inhibition of growth was observed for Ciprofloxacin, as positive control at a concentration of 1 µg/mL. The MBC for Polybia MP-1 was found to be twice of MIC i.e. 150 µM. At 2 × MIC of peptide, P. aeruginosa ATCC 27853 was completely eliminated and no growth was observed on MHA plates after overnight incubation at 37 °C.
Determination of Minimum Inhibitory Concentration (MIC) for Polybia MP-1 against P. aeruginosa ATCC 27853. Cip (1) corresponds to Ciprofloxacin at a concentration of 1μg/mL. One-way ANOVA wasapplied and P value vs control (without any treatment) ***<0.0001, **< 0.001, *<0.05. All values represent mean ± SEM (n=2)
Time Dependent Determination of CE Values
CE study was carried out by drop plate method whereby the time dependent complete elimination of P. aeruginosa ATCC 27853 growth was monitored at half MIC, MIC, 2 × MIC and 4 × MIC of Polybia MP-1 after incubation with the peptide for 0,15,30,45,60,120 and 180 min. Results of the experiment are given in Table 3. The peptide at a higher concentration of 4 × MIC was able to completely eliminate bacterial growth after 60 min of incubation whereas half of MIC was unable to inhibit growth even after 180 min of incubation. The peptide at MIC (75 µM) was unable to eliminate the bacterial growth even after 180 min. 2 × MIC was effective after 120 min of incubation (Fig. 3).
Stability of Polybia MP-1 in Serum, Urine and Milk
Polybia MP-1 was found to inhibit the growth of P. aeruginosa ATCC 27853 effectively at a higher concentration of 5 × MIC (375 µM) without any significant effect of 6.25 %,12.5 and 25 % of serum and urine added whereas a slight decrease in activity was observed for all three percentages of milk added with a maximum decrease at 25 % i.e. 39.82 % reduction in activity in comparison to the untreated peptide. On the other hand, at a lower concentration of 1 MIC (75 µM) a significant (p < 0.001) decrease in antibacterial activity of the peptide was observed for all three concentrations viz. 6.25 %, 12.5 and 25 % of milk i.e. 82.3, 74.2 and 100 % decrease in activity respectively. Similarly, a decrease in antibacterial activity of 1 MIC of the peptide was observed at 12.5 and 25 % of both urine and serum (Fig. 4). Overall the peptide showed more stability at a higher concentration of 5 MIC when compared with 1 MIC.
Complete Elimination study for Polybia MP-1 on P. aeruginosa (ATCC 27853) using drop plate method. Different figures correspond to different incubation times i.e. a 0 min b 15 min c 30 min d 45 min e 60 min f 120 min g 180 min. 1 A and 1B represent 0.5 MIC (37.5 µM); 2 A and 2B represent MIC (75 µM); 3 A and 3B represent 2 X MIC (150 µM); 4 A and 4B represent 4X MIC (300 µM) for Polybia MP-1; 1 C and 1D represent Amikacin at MIC (8 µg/mL); 2 C and 2D represent Ciprofloxacin at MIC (1 µg/mL); 3 C and 3D represent untreated cells and 4 C and 4D represent blank (plain media)
Haemolytic Activity
The percent haemolysis was calculated in comparison to haemoglobin leakage from untreated erythrocytes and that from erythrocytes treated with 0.1 % Triton X-100 (Table 4). Polybia MP-1 was found to cause the lowest haemolysis of 2.8 % in buffalo erythrocytes whereas higher percent haemolysis of 19.5 and 16.7 % were observed in goat and cattle erythrocytes respectively, at a concentration of 200 µM.
Identification of P. aeruginosa Isolated From Milk
A total of 38 isolates were obtained for P. aeruginosa on Pseudomonas selective agar medium from 50 milk samples and were subjected to PCR based identification based on the presence and absence of three genes viz. 16SrDNA, oprL and gyrB (Fig. 5). 20 isolates showing the presence of all the three genes were confirmed as P. aeruginosa isolates and selected for the study.
Genotypic Characterization of P. aeruginosa Isolates
PCR based genotypic characterization for genes responsible for virulence, antibiotic resistance and biofilm formation was carried out for the 20 isolates (Fig. 6). The bla SHV gene was found present only in 5 % (n = 1) of the isolates whereas bla OXA, bla TEM, csgD and icaD genes were found present in 15 % of isolates. The genes plcH, plcN, phzI, pilA and algD were found present in 100 % (n = 20) isolates. The exo S and toxA genes were found in 95 % (n = 19) and 90 % (n = 18) of the isolates respectively. The apr gene was present in 70 % (n = 14) of the isolates. In antibiotic resistant genes, blaCTX−M was most prevalent and present in 60 % isolates (n = 12).
Heat map depicting the presence and absence of genes for identification i.e. 16SrDNA, oprL and gyrB; virulence i.e. exoS, exoY, toxA, plcH, plcN, PA431C, pvdA, phzH, phzS, phzM, phzI, phzII, pilA, apr; antibiotic resistance i.e. bla TEM, bla CTX−M, bla SHV, bla OXA and biofilm formation i.e. algU, algD, icaD, csgA, csgB, csgD of P. aeruginosa isolates (n = 20) from milk samples
Antibiogram of P. aeruginosa Isolates From Mastitic Milk
Antibiotic sensitivity pattern determination for the 20 isolates was carried out against standard 8 antibiotics (Fig. 7). A maximum of 55 % isolates (n = 11) were found resistant against CIP 5 and CTR 30 followed by 45 % (n = 9) of isolates resistant against AK 30 and GEN 10. 40 % (n = 8) of the isolates were found resistant against CAZ 30 whereas 25 % (n = 5) isolates were resistant against AT 30. Least resistance was found against the antibiotics CL 10 and IPM 10 i.e. 15 % (n = 3) and 10 % (n = 2) respectively. Overall, 7 isolates (Isolate number 2, 3, 4, 15, 16, 17, and 18) were found to be resistant to one antibiotic from ≥ 3 classes of antibiotics and were categorised as multiple drug resistant (MDR) isolates (Fig. 8).
Antimicrobial susceptibility patterns of P. aeruginosa isolates (n = 20) from milk against eight antibiotics- Amikacin 30 µg (AK 30), Ciprofloxacin 5 µg (CIP 5), Gentamycin 10 µg (GEN 10), Imipenem 10 µg (IPM 10), Ceftazidime 30 µg (CAZ 30), Colistin (CL 10), Ceftriaxone 30 µg (CTR 30) and Aztreonam 30 µg (AT 30). The percentage of isolates resistant, intermediate and sensitive to different antibiotics is depicted on the bars
Heat map depicting antibiogram for the 20 P. aeruginosa isolates against Amikacin 30 µg (AK 30), Ciprofloxacin 5 µg (CIP 5), Gentamycin 10 µg (GEN 10), Imipenem 10 µg (IPM 10), Ceftazidime 30 µg (CAZ 30), Colistin (CL 10), Ceftriaxone 30 µg (CTR 30) and Aztreonam 30 µg (AT 30). Isolate number 2, 3, 4, 15, 16, 17, and 18 showed resistance for antimicrobial agents from ≥ 3 antibiotic classes, hence are considered MDR strains
Correlation Between Antibiotic Resistant Genes and Antibiotic Resistance
Correlation between the presence of antibiotic resistant genes and antibiogram for the P. aeruginosa isolates was carried out by Pearson’s method (Table 5). Resistance to Amikacin (AK 30) showed a moderate positive correlation (p < 0.05) with presence of bla TEM and bla OXA having a Pearson coefficient of 0.514. Resistance to Imipenem (IPM 10) showed a strong positive correlation (p < 0.01) with the presence of bla TEM and bla OXA having a Pearson coefficient of 0.793. Antibiotic resistance to Colistin (CL 10) showed a positive correlation (p < 0.01) with the presence of bla TEM, bla CTX−M and bla OXA with Pearson’s coefficients as 0.608, 0.572 and 0.608, respectively. No significant negative correlation was found in between any of the variables. Similarly, resistance to Ceftriaxone (CTR 30) showed a significant (p < 0.01) positive correlation with the presence of bla CTX−M with a Pearson coefficient of 0.596.
Antimicrobial Activity of Polybia MP-1 Against P. aeruginosa Isolates From Mastitic Milk
Polybia MP-1 at 1 MIC (75 µM) for P. aeruginosa ATCC 27853 was unable to inhibit the growth of the isolates from mastitic milk. Maximum antibacterial activity for Polybia MP-1 against the isolates was observed at 6 X MIC (450 µM). At this concentration, Polybia MP-1 was able to inhibit 90 % (18/20) of the isolates. Isolate 2 and 4 were highly resistant to the activity of the peptide as well as the different antibiotics (Fig. 9). Polybia MP-1 was able to inhibit the growth of 5 MDR isolates out of the total 7 MDR isolates (71 % inhibition).
Disruption of P. aeruginosa Biofilm by Polybia MP-1
Treatment of P. aeruginosa ATCC 27853 biofilms, showed a steady decrease in biomass after treatment with increasing concentrations of Polybia MP-1 and Tetracycline (Fig. 10). The peptide showed significant decrease in the biofilm mass percent with increasing MIC with a maximum decrease at 8 X MIC. Similar decrease in biofilm mass percent was observed for tetracycline treatment as well. The peptide showed more potent activity at 2 X MIC and 4 X MIC when compared with tetracycline at the same concentrations.
Efficacy of Polybia MP-1 on established biofilms of P. aeruginosa (ATCC 27853). The biofilms established after 24 h of growth were treated with different concentrations of Polybia MP-1 and Tetracycline for another 24 h at 37˚C. The reduction in biofilm mass was assessed by crystal violet staining. Each value represents mean ± SEM (n = 3). Two-way ANOVA was applied where P value versus control: * <0.05, **<0.01, ***<0.001, ns not significant
Discussion
Mastoparans are amphipathic tetradecapeptides obtained from the venom of vespid wasps (hornets and paper wasps) and have been reported to possess an extensive range of therapeutically important properties such as anticancerous and antimicrobial activities (Wang et al. 2009; Dos Santos Cabrera, 2011; Konno et al. 2019). Polybia MP-1 is a mastoparan peptide with 14 amino acids which assumes an α-helical structure on interacting with membranes with the long helical surface parallel to the membrane bilayer. The hydrophobic residues assemble on one face of the helix whereas hydrophilic ones on the other. This formation of helical structure is a major requirement for the antibacterial activity of the peptide by inducing membrane disruption by pore formation through ionic interactions among cationic residues of the peptide and anionic bacterial surface as well as hydrophobic interactions in between hydrophobic helix residues and membrane’s interior portion (Alvares et al. 2016; Luong et al. 2017).
Souza et al. 2005, reported the antimicrobial activity of Polybia MP-1 against B. subtilis (CCT 2576), E. coli (ATCC 25922), S. aureus (ATCC 6538), and P. aeruginosa (ATCC 15422) with MIC 8, 8, 4 and 15 µg/mL, respectively. In another study by Luong et al. 2017, the MIC of Polybia MP-1 against P. aeruginosa was found to be greater than 100 µg/mL. In our study, the MIC against P. aeruginosa (ATCC 27853) was 75 µM i.e.124 µg/mL (Fig. 2). This higher MIC in P. aeruginosa ATCC 27853 may be due its enhanced biofilm forming activity of the strain. This was proven by transcriptomic analysis whereby P. aeruginosa ATCC 27853 expresses higher levels of exopolysaccharide synthesis genes like psl and pel that play a defining role in forming the external polysaccharide matrix for bacterial adhesion. Pyocyanin (PYO) a redox active phenazine is also expressed in higher amounts along with remarkable higher expression of type III secretion system genes like n psc, pcr and exs gene clusters in P. aeruginosa ATCC 27853 (Cao et al. 2017).
Polybia MP-1 is highly selective for bacterial membranes and this selectivity is attributed to its differential interaction with different concentrations of lipid. The peptide and lipid concentration must reach a certain level to start the cooperative leakage process. In the case of bacteria, this is highly governed by the bilayer composition and as such follow different rates of leakage depending on peptide and lipid concentration (Dos Santos Cabrera et al. 2008). In the present study, CE value determination experiment proves that with increasing concentration of peptide the particular threshold required for interaction with the bacterial bilayer and cause intense leakage, is reached at an earlier time point i.e. 4 × MIC of the peptide was able to act and eliminate bacteria the earliest after 60 min of incubation (Table 3; Fig. 3).
Serum, plasma, saliva, sweat, urine and other bodily secretions can impair the activity of antibiotics and AMPs either through proteolytic degradation because of the presence of different proteases, or by binding to protein and lipid fractions (Mohamed et al. 2017). Similarly, a variety of components present in milk may impair the activity of antibiotics and AMPs. Having a high activity in milk is a foremost requirement for drugs administered through the intramammary route for treatment of mastitis (Schmelcher et al. 2015; Li et al. 2017). Hence, the activity of the peptide was assessed in the presence of various concentrations of milk, serum and urine. Activity of the peptide was most affected by the addition of milk in both MIC and 5 × MIC concentrations (Fig. 4). This maybe as a result of the fact that milk is rich in various intricate and interconnected proteolytic systems which include zymogens such as plasminogen, trypsinogen; active proteases like cathepsins, protease inhibitors like α1 anti-trypsin and activators like thrombin (Dallas et al. 2015).
Polybia MP-1 is a highly selective AMP with little to nil haemolytic activity. Results of the present study are in agreement with Souza et al., (2005) which stated no significant effect of different concentrations of Polybia MP-1on rat RBCs up to 100 µM concentration. Similar, low haemolytic activity was observed with buffalo RBCs in the present study (Table 4). High haemolytic activity observed with goat and cattle RBCs may be a result of selective interaction of the peptide due to differences in lipid composition of the membranes.
The presence of various virulence factors renders P. aeruginosa pathogenic. These factors include factors associated with cells like flagellum, pilus, alginate, lipopolysaccharide (LPS) and other adhesins along with exoenzymes or may be factors of secretory nature like phospholipase, protease, elastase, exotoxins, exoenzymes, pyocyanin, rhamnolipids and siderophores (Mittal et al. 2009). Screening for genes encoding these virulence factors thus helps us determine the different aspects of pathogenicity in the isolates. Apart from these, abundance of biofilm forming genes and antibiotic resistant genes gives an overall picture of the pathogenicity of the isolates. It was found that isolate number 2, 4, 11 and 12 which were highly resistant to different antibiotics as well as the peptide, had many of the virulence factor genes, antibiotic resistant genes and biofilm forming genes present (Fig. 7).
β-lactamas are the most widely used class of antibiotics because of their low toxicity, with 50 % of the present systemic antibiotics belonging to this class (Jena et al. 2017). Acquired antibiotic resistance in P. aeruginosa can be attributed to acquiring genes for Extended-Spectrum β-Lactamases (ESBLs) and Metallo-β-Lactamases (MBLs). As these enzymes are encoded by plasmids they can be easily acquired and spread through horizontal gene transfer (Hosu et al. 2021). ESBLs provide resistance to third generation cephalosporins, oxyimino-β-lactams, carbapenems and monobactams. As per the Ambler classification, ESBLs are categorized into two, class A and class D. Enzymes in class A include blaTEM, blaCTX−M and blaSHV, and have been found to be most prevalent in resistant P. aeruginosa strains (Laudy et al. 2017). Class D β-Lactamases, are also referred to oxacillinases (OXAs) blaOXA, and are responsible for resistance against carbapenems (Zong et al. 2020). In the present study 3 isolates i.e. 2, 3, and 4 showed the presence of both blaTEM and blaOXA. Seven isolates showed the presence of blaCTX−M and one isolate was found positive for blaSHV (Fig. 7). Strains producing ESBL are often found resistant not only to the general β-lactams but also to other antimicrobial agents such as tetracycline, fluoroquinolones like Ciprofloxacin, aminoglycosides like Amikacin and Gentamycin, and trimethoprim/sulfamethoxazole (Ojdana et al. 2014; Rezai et al. 2015).
Correlation data (Table 5) represent a strong positive correlation between the presence of blaTEM and blaOXA and resistance against Imipenem. This was in agreement with the reports that blaOXA −23 provides resistance against carbapenems like imipenem, meropenem and ertapenem in Acinetobacter johnsonii M19 (Zong et al. 2020). Similar, positive correlation was found between the presence of blaOXA and resistance against the aminoglycoside, Amikacin. Previous reports have mentioned the coexistence of carbapenem and aminoglycoside resistant genes in clinical strains of Acinetobacter baumannii. The genes, blaOXA−40 like and aac(3)- Ia/aph(3′)-VI were the most coexistent for acquiring carbapenem and aminoglycoside resistance in A. baumannii (Nowak et al. 2014). bla TEM, bla CTX−M and bla OXA presence was positively correlated with (polymyxin E) Colistin resistance in this study. Previous work has reported that carbapenem resistant isolates of P. aeruginosa (CRPA) having the blaOXA−10 gene were all resistant to colistin as well (Farajzadeh Sheikh et al. 2019). In the present study Ceftriaxone (cephalosporin) resistance showed a significant positive correlation with the presence of bla CTX−M. Wong et al. (2016) have shown that dissemination of the IncI1 plasmids carrying various bla CTX−M genes contributes to Ceftriaxone resistance in Salmonella enterica. Significant amplification of bla CTX−M genes on exposure to Ceftriaxone was reported in the gut flora of patients treated with it by Meletiadis et al. (2017).
Polybia MP-1 was able to effectively inhibit the growth of 18 of the isolates of the total 20. The peptide inhibited the growth of 5 MDR isolates out of 7 except for isolates 2 and 4. This high efficiency (71 %) of the peptide to inhibit MDR isolates proves its immense antimicrobial potential for the treatment of resistant P. aeruginosa.
P. aeruginosa is a potent biofilm former and when organized into biofilms it becomes more resistant to antibiotics due to increase in the complexity of the microbial community, expression of different biofilm forming genes, and the increase in the amounts of the extracellular matrix material, including DNA and carbohydrate polymers (Hirt and Gorr, 2013). When biofilm disruptive activity of Polybia MP-1 was evaluated against P. aeruginosa ATCC 27853 biofilms it was found to be equally effective to Tetracycline. Previously done work has established the effectivity of several cationic antimicrobial peptides against P. aeruginosa biofilms and proved their potential as valuable alternatives to antibiotics for treatment of resistant biofilm forming bacteria (Hirt and Gorr, 2013; Mohamed et al. 2017; Beaudoin et al. 2018; Park et al. 2019; Yin et al. 2020).
Conclusion
Mastitis causes major economic losses to the dairy industry and its prevention and treatment also adds to the economic burden. A wide range of antibiotics are used for treatment of mastitis, both as parenteral and also as intra-mammary infusions. Increasing use and misuse of antibiotics in dairy industry has led to tremendous rise in antimicrobial resistant bacteria and also the menace of antibiotic residues in the milk and milk products. The AMR issue not only risks human life through transfer of resistant bacteria to humans but also makes the treatment of mastitis difficult and is therefore economically not a viable option. The AMPs offer a valuable alternative to antibiotics to overcome the increasing threat of AMR. The Polybia MP-1 is a potent antimicrobial peptide with effective antimicrobial activity against antibiotic resistant P. aeruginosa isolates obtained from mastitic milk samples. It showed low hemolytic activity against RBCs and effectively inhibited the growth of 71 % (5/7) of resistant isolates. It showed potent biofilm disruptive activity against P. aeruginosa ATCC 27853 biofilms. The isolates showed the presence of numerous genes encoding different virulence factors, biofilm formation and antibiotic resistance. Correlation studies established the relationship between presence of the antibiotic resistant genes and antibiotic resistance. Overall study emphasised the ever-increasing problem of AMR in P. aeruginosa and how AMPs like Polybia MP-1 provide an effective alternative for the treatment of MDR isolates. Future prospects include detailed study of the combination of this peptide along with different antibiotics to achieve a synergistic action on MDR bacteria.
Data Availability
All data related to this work are presented in the MS hence, no supplementary data is provided.
References
Alvares DS, Fanani ML, Ruggiero Neto J, Wilke N (2016) The interfacial properties of the peptide Polybia-MP1 and its interaction with DPPC are modulated by lateral electrostatic attractions. Biochim Biophys Acta - Biomembr 1858:393–402. https://doi.org/10.1016/j.bbamem.2015.12.010
Ameen F, Reda SA, El-Shatoury SA et al (2019) Prevalence of antibiotic resistant mastitis pathogens in dairy cows in Egypt and potential biological control agents produced from plant endophytic actinobacteria. Saudi J Biol Sci 26:1492–1498. https://doi.org/10.1016/j.sjbs.2019.09.008
Bauer AW, Kirby WM, Sherris JC, Turck M (1966) Antibiotic susceptibility testing by a standardized single disk method. Am J Clin Pathol 45(4):493–496. PMID: 5325707
Beaudoin T, Stone TA, Glibowicka M et al (2018) Activity of a novel antimicrobial peptide against Pseudomonas aeruginosa biofilms. Sci Rep 8:1–12. https://doi.org/10.1038/s41598-018-33016-7
Bhagavathula N, Meedidoddi V, Bourque S, Vimaladevi R, Kesavakurup S, Selvadurai D, ShrivastavaS Krishnappa C (2017) Characterization of two novel antimicrobial peptidesfrom the cuticular extracts of the ant emopenTrichomyrmex crinicepsemclose (Mayr), (Hymenoptera: Formicidae). Arch Insect Biochem and Physiol. https://doi.org/10.1002/arch.21381
Boireau C, Cazeau G, Jarrige N et al (2018) Antimicrobial resistance in bacteria isolated from mastitis in dairy cattle in France, 2006–2016. J Dairy Sci 101:9451–9462. https://doi.org/10.3168/jds.2018-14835
Cao H, Lai Y, Bougouffa S, Xu Z, Yan A (2017) Comparative genome and transcriptome analysis reveals distinctive surface characteristics and unique physiological potentials of Pseudomonas aeruginosa ATCC 27853. BMC Genom 18:1–17. https://doi.org/10.1186/s12864-017-3842-z
Dallas DC, Murray NM, Gan J (2015) Proteolytic systems in milk: perspectives on the evolutionary function within the mammary gland and the infant. J Mammary Gland Biol Neoplasia 20(3–4):133–147. https://doi.org/10.1007/s10911-015-9334-3 (Epub 2015 Jul 16. PMID: 26179272; PMCID: PMC4637187)
Daly M, Power E, Björkroth J, Sheehan P, O’Connell A, Colgan M, Korkeala H, Fanning S (1999) Molecular analysis of Pseudomonas aeruginosa: epidemiological investigation of mastitis outbreaks in Irish dairy herds. Appl Environ Microbiol 65:2723–2729. https://doi.org/10.1128/aem.65.6.2723-2729.1999
Dhanawade NB, Kalorey DR, Srinivasan R, Barbuddhe SB, Kurkure NV (2010) Detection of intercellular adhesion genes and biofilm production in Staphylococcus aureus isolated from bovine subclinical mastitis. Vet Res Commun 34:81–89. https://doi.org/10.1007/s11259-009-9326-0
Dos Santos Cabrera MP, Costa STB, De Souza BM et al (2008) Selectivity in the mechanism of action of antimicrobial mastoparan peptide Polybia-MP1. Eur Biophys J 37:879–891. https://doi.org/10.1007/s00249-008-0299-7
Dos Santos Cabrera MP, Alvares DS, Leite NB et al (2011) New insight into the mechanism of action of wasp mastoparan peptides: lytic activity and clustering observed with giant vesicles. Langmuir 27:10805–10813. https://doi.org/10.1021/la202608r
Farajzadeh Sheikh A, Shahin M, Shokoohizadeh L et al (2019) Molecular epidemiology of colistin-resistant Pseudomonas aeruginosa producing NDM-1 from hospitalized patients in Iran. Iran J Basic Med Sci 22:38–42. https://doi.org/10.22038/ijbms.2018.29264.7096
Farkas A, Pap B, Kondorosi É, Maróti G (2018) Antimicrobial activity of NCR plant peptides strongly depends on the test assays. Front Microbiol 9:1–10. https://doi.org/10.3389/fmicb.2018.02600
Fazeli N, Momtaz H (2014) Virulence gene profiles of multidrug-resistant Pseudomonas aeruginosa isolated from Iranian hospital infections. Iran Red Crescent Med JDoi. https://doi.org/10.5812/ircmj.15722
Finnan S, Morrissey JP, O’Gara F, Boyd EF (2004) Genome diversity of Pseudomonas aeruginosa isolates from cystic fibrosis patients and the hospital environment. J Clin Microbiol 42:5783–5792. https://doi.org/10.1128/JCM.42.12
Gogoi P, Shrivastava S, Shah P, Saxena S, Srivastava S, Gaur GK (2021) Linear and branched forms of short antimicrobial peptide-IRK inhibit growth of multi drug resistant Staphylococcus aureus isolates from Mastitic cow milk. Int J Pept Res Ther. https://doi.org/10.1007/s10989-021-10243-7
Gupta S, Abhishek Shrivastava S, Singh RJ, Gogoi P, Kumar B (2021) Evaluation of antibacterial activity of Magainin and Mastoparan and its novel hybrid against MDR E. coli isolates of neonatal calves. Int J Pept Res Ther. https://doi.org/10.1007/s10989-020-10154-z
Hirai Y, Yasuhara T, Yoshida H et al (1979) A new mast cell degranulating peptide "Mastoparan” in the venom of Vespula lewisii. Chem Pharm Bull (Tokyo) 27:1942–1944. https://doi.org/10.1248/cpb.27.1942
Hirt H, Gorr S-U (2013) Antimicrobial peptide GL13K is effective in reducing biofilms of Pseudomonas aeruginosa. Antimicrob Agents Chemother 57:4903–4910. https://doi.org/10.1128/aac.00311-13
Hosu MC, Vasaikar SD, Okuthe GE, Apalata T (2021) Detection of extended spectrum beta-lactamase genes in Pseudomonas aeruginosa isolated from patients in rural Eastern Cape Province, South Africa. Sci Rep 11:1–8. https://doi.org/10.1038/s41598-021-86570-y
Jena J, Sahoo RK, Debata NK, Subudhi E (2017) Prevalence of TEM, SHV, and CTX-M genes of extended-spectrum β-lactamase-producing Escherichia coli strains isolated from urinary tract infections in adults. 3 Biotech 7:1–7. https://doi.org/10.1007/s13205-017-0879-2
Kelly EJ, Wilson DJ (2016) Pseudomonas aeruginosa mastitis in two goats associated with an essential oil–based teat dip. J Vet Diagnostic Investig 28:760–762. https://doi.org/10.1177/1040638716672255
Konno K, Kazuma K, Rangel M et al (2019) New mastoparan peptides in the venom of the solitary eumenine wasp eumenes micado. Toxins (Basel) 11:1–15. https://doi.org/10.3390/toxins11030155
Laudy AE, Róg P, Smolińska-Król K, Ćmiel M, Słoczyńska A, Patzer J et al (2017) Prevalence of ESBL-producing Pseudomonas aeruginosa isolates in Warsaw, Poland, detected by various phenotypic and genotypic methods. PLoS One 12(6):e0180121. https://doi.org/10.1371/journal.pone.0180121
Li L, Wang L, Gao Y, Wang J, Zhao X (2017) Effective antimicrobial activity of Plectasin-derived antimicrobial peptides against Staphylococcus aureus infection in mammary glands. Front Microbiol 8:1–8. https://doi.org/10.3389/fmicb.2017.02386
Li W, Separovic F, O’Brien-Simpson NM, Wade JD (2021) Chemically modified and conjugated antimicrobial peptides against superbugs. Chem Soc Rev. https://doi.org/10.1039/D0CS01026J
Luong HX, Kim DH, Lee BJ, Kim YW (2017) Antimicrobial activity and stability of stapled helices of polybia-MP1. Arch Pharm Res 40:1414–1419. https://doi.org/10.1007/s12272-017-0963-5
Magiorakos AP, Srinivasan A, Carey RB et al (2012) Multidrug-resistant, extensively drug-resistant and Pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect 18:268–281. https://doi.org/10.1111/j.1469-0691.2011.03570.x
Mahlapuu M, Håkansson J, Ringstad L, Björn C (2016) Antimicrobial peptides: an emerging category of therapeutic agents. Front Cell Infect Microbiol 6:194. https://doi.org/10.3389/fcimb.2016.00194
Meletiadis J, Turlej-Rogacka A, Lerner A, Adler A, Taconelli E, Mouton JW (2017) Amplification of antimicrobial resistance in gut flora of patients treated with ceftriaxone. Antimicrob Agents Chemother 61:1–10. https://doi.org/10.1128/AAC.00473-17
Meng L, Liu H, Lan T, Dong L, Hu H, Zhao S, Zhang Y, Zheng N, Wang J (2020) Antibiotic resistance patterns of Pseudomonas spp. isolated from raw milk revealed by whole genome sequencing. Front MicrobiolDoi. https://doi.org/10.3389/fmicb.2020.01005
Merrifield RB (1963) Solid phase peptide synthesis. I. The synthesis of a tetrapeptide. J Am Chem Soc 85(14):2149–2154. https://doi.org/10.1021/ja00897a025
Minas K, McEwan NR, Newbold CJ, Scott KP (2011) Optimization of a high-throughput CTAB-based protocol for the extraction of qPCR-grade DNA from rumen fluid, plant and bacterial pure cultures. FEMS Microbiol Lett 325(2):162–9. https://doi.org/10.1111/j.1574-6968.2011.02424.x (PMID: 22029887)
Mittal R, Aggarwal S, Sharma S, Chhibber S, Harjai K (2009) Urinary tract infections caused by Pseudomonas aeruginosa: a minireview. J Infect Public Health 2:101–111. https://doi.org/10.1016/j.jiph.2009.08.003
Mohamed MF, Brezden A, Mohammad H, Chmielewski J, Seleem MN (2017) A short D-enantiomeric antimicrobial peptide with potent immunomodulatory and antibiofilm activity against multidrug-resistant Pseudomonas aeruginosa and Acinetobacter baumannii. Sci Rep 7:1–13. https://doi.org/10.1038/s41598-017-07440-0
NAAS (2013) Mastitis Management in Dairy Animals. Policy Paper No. 61, National Academy of Agricultural Sciences, New Delhi, 12 p
Nowak P, Paluchowska PM, Budak A (2014) Co-occurrence of carbapenem and aminoglycoside resistance genes among multidrug-resistant clinical isolates of Acinetobacter baumannii from Cracow, Poland. Med Sci Monit Basic Res 20:9–14. https://doi.org/10.12659/MSMBR.889811
Ojdana D, Sacha P, Wieczorek P et al (2014) The occurrence of blaCTX-M, blaSHV, and blaTEM genes in extended-spectrum β-lactamase-positive strains of Klebsiella pneumoniae, Escherichia coli, and Proteus mirabilis in Poland. Int J Antibiot 2014:935842. https://doi.org/10.1155/2014/935842
Palma MS (2013) Hymenoptera insect peptides, 2nd edn. Elsevier Inc, Amsterdam
Pang Z, Raudonis R, Glick BR, Lin TJ, Cheng Z (2019) Antibiotic resistance in Pseudomonas aeruginosa: mechanisms and alternative therapeutic strategies. Biotechnol Adv 37:177–192. https://doi.org/10.1016/j.biotechadv.2018.11.013
Park SC, Lee MY, Kim JY et al (2019) Anti-biofilm effects of synthetic antimicrobial peptides against drug-resistant Pseudomonas aeruginosa and Staphylococcus aureus planktonic cells and biofilm. Molecules 24:1–13. https://doi.org/10.3390/molecules24244560
Rezai MS, Salehifar E, Rafiei A et al (2015) Characterization of multidrug resistant extended-spectrum beta-lactamase-producing Escherichia coli among uropathogens of pediatrics in North of Iran. Biomed Res IntDoi. https://doi.org/10.1155/2015/309478
Saini V, McClure JT, Léger D et al (2012) Antimicrobial resistance profiles of common mastitis pathogens on Canadian dairy farms. J Dairy Sci 95:4319–4332. https://doi.org/10.3168/jds.2012-5373
Salman M, Ali A, Haque A (2013) A novel multiplex PCR for detection of Pseudomonas aeruginosa: a major cause of wound infections. Pakistan J Med Sci 29:957–961. https://doi.org/10.12669/pjms.294.3652
Schmelcher M, Powell AM, Camp MJ, Pohl CS, Donovan DM (2015) Synergistic streptococcal phage λSA2 and B30 endolysins kill streptococci in cow milk and in a mouse model of mastitis. Appl Microbiol Biotechnol 99:8475–8486. https://doi.org/10.1007/s00253-015-6579-0
Sharma R, Shrivastava S, Singh SK, Kumar A, Saxena S, Singh RK (2021) Deep-ABPpred: identifying antibacterial peptides in protein sequences using bidirectional LSTM with word2vec. Brief Bioinformatics. https://doi.org/10.1093/bib/bbab065
Sharma R, Shrivastava S, Singh SK, Kumar A, Saxena S, Singh RK (2021) AniAMPpred: artificial intelligence guided discovery of novel antimicrobial peptides in animal kingdom. Brief Bioinformatics. https://doi.org/10.1093/bib/bbab242
Shukla SK, Rao TS (2017) Staphylococcus aureus biofilm removal by targeting biofilm-associated extracellular proteins. Indian J Med Res 146:1–8. https://doi.org/10.4103/ijmr.IJMR_410_15
Souza BM, Mendes MA, Santos LD, Lilian MMC, Almeida RNA, Pagnocca FC, Konno K, Palma MS (2005) Structural and functional characterization of two novel peptide toxins isolated from the venom of the social wasp Polybia paulista. Peptides 26:2157–2164. https://doi.org/10.1016/j.peptides.2005.04.026
Tan T, Wu D, Li W, Zheng X, Li W, Shan A (2017) High specific selectivity and membrane-active mechanism of synthetic cationic hybrid antimicrobial peptides based on the peptide FV7. Int J Mol Sci 18(2):339. https://doi.org/10.3390/ijms18020339
Wang KR, Yan JX, Zhang BZ, Song JJ, Jia PF, Wang R (2009) Novel mode of action of Polybia-MPI, a novel antimicrobial peptide, in multi-drug resistant leukemic cells. Cancer Lett 278:65–72. https://doi.org/10.1016/j.canlet.2008.12.027
Wiegand I, Hilpert K, Hancock REW (2008) Agar and broth dilution methods to determine the minimal inhibitory concentration (MIC) of antimicrobial substances. Nat Protoc 3:163–175. https://doi.org/10.1038/nprot.2007.521
Wong MHY, Kan B, Chan EWC et al (2016) IncI1 plasmids carrying various blaCTX-M genes contribute to ceftriaxone resistance in Salmonella enterica serovar enteritidis in China. Antimicrob Agents Chemother 60:982–989. https://doi.org/10.1128/AAC.02746-15
Yang W-T, Ke C-Y, Wu W-T et al (2019) Effective treatment of bovine mastitis with Intramammary infusion of Angelica dahurica and Rheum officinale extracts. Evid Based Complement Altern Med. https://doi.org/10.1155/2019/7242705
Yin Q, Wu S, Wu L et al (2020) A novel in silico antimicrobial peptide DP7 combats MDR Pseudomonas aeruginosa and related biofilm infections. J Antimicrob Chemother 75:3248–3259. https://doi.org/10.1093/jac/dkaa308
Zong G, Zhong C, Fu J et al (2020) The carbapenem resistance gene bla OXA-23 is disseminated by a conjugative plasmid containing the novel transposon Tn6681 in Acinetobacter johnsonii M19. Antimicrob Resist Infect Control 9:1–11. https://doi.org/10.1186/s13756-020-00832-4
Acknowledgements
The present study was carried out behest National Agricultural Science Fund (NASF) project entitled “Detection of peptide biomarkers and development of synthetic antimicrobial peptide hydrogels for bovine mastitis (Project grant No. NASF/ABA-6014/2016-17/367). The peptide synthesis and other infrastructure created under the ICAR-Niche Area Excellence Programme on Biosensors at Division of Veterinary Biotechnology, ICAR-IVRI were utilized for this work and is thankfully acknowledged.
Funding
This study was funded by National Agricultural Science Fund (NASF) under the project entitled “Detection of peptide biomarkers and development of synthetic antimicrobial peptide hydrogels for bovine mastitis” (Project Grant No. NASF/ABA-6014/2016-17/367).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Research Involving Human and Animal Participants
In this work, no invasive procedure was performed on humans or any other animal species. The necessary permission from Institute Animal Ethics Committee was obtained vide reference no. F.26 − 1/2018-19/JD (R) dated 7th October 2019 for work related to testing of synthetic antimicrobial peptide hydrogels in bovine mastitis cases.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Shah, P., Shrivastava, S., Singh, R.J. et al. Synthetic Antimicrobial Peptide Polybia MP-1 (Mastoparan) Inhibits Growth of Antibiotic Resistant Pseudomonas aeruginosa Isolates From Mastitic Cow Milk. Int J Pept Res Ther 27, 2471–2486 (2021). https://doi.org/10.1007/s10989-021-10266-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10989-021-10266-0