Abstract
Milk contains elements of numerous proteolytic systems (zymogens, active proteases, protease inhibitors and protease activators) produced in part from blood, in part by mammary epithelial cells and in part by immune cell secretion. Researchers have examined milk proteases for decades, as they can cause major defects in milk quality and cheese production. Most previous research has examined these proteases with the aim to eliminate or control their actions. However, our recent peptidomics research demonstrates that these milk proteases produce specific peptides in healthy milk and continue to function within the infant’s gastrointestinal tract. These findings suggest that milk proteases have an evolutionary function in aiding the infant’s digestion or releasing functional peptides. In other words, the mother provides the infant with not only dietary proteins but also the means to digest them. However, proteolysis in the milk is controlled by a balance of protease inhibitors and protease activators so that only a small portion of milk proteins are digested within the mammary gland. This regulation presents a question: If proteolysis is beneficial to the infant, what benefits are gained by preventing complete proteolysis through the presence of protease inhibitors? In addition to summarizing what is known about milk proteolytic systems, we explore possible evolutionary explanations for this proteolytic balance.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Milk is a product of more than 200 million years of evolution that is hypothesized to have originated as a simple watery secretion to keep pre-mammalian’s papery eggs moist [1, 2]. Milk has remained under strong evolutionary pressures: every milk component costs energy for the mother and, therefore, must have positive effects on the neonate. The primary functional role of milk is feeding the neonate with high nutritional value proteins and adequate lipids and carbohydrates, as well as a minerals, vitamins and water. Milk also has important biological functions. Milk contains hundreds of intact proteins, many of them known to have biological actions, from antibacterial to immunomodulatory. But milk also contains a complex mixture of proteases, zymogens, protease activators and protease inhibitors. This array of proteolytic systems allows a small degree of proteolytic activity within the mammary gland. These components derive from mammary epithelial cell (MEC) expression, active or passive transport from blood or secretion by host immune cells, as will be discussed in a later section.
Proteolytic enzymes in bovine milk have received considerable research attention because these proteases strongly affect dairy product quality [3, 4]: overly high protease activity in milk causes casein degradation, which leads to lower cheese yields [5] and proteolysis in sterilized milk is involved in age gelation of milk proteins [6]. Milk proteases also impact flavor development during cheese ripening [7]. Driven by dairy industry concerns, many studies have characterized the protease systems in bovine milk, examined the proteolytic activities under different conditions and determined their interaction with other milk components. With the express purpose of examining milk proteases as a means of controlling their activity to improve consumer products, identifying the evolutionary advantage of these complex proteolytic systems has been neglected. Milk is, of course, more than just a food product: it is a unique evolutionary biological product optimized for mammals to survive and thrive. The balanced, simultaneous secretion of milk proteases, zymogens, inhibitors and activators hints at the biological significance of the milk protease system.
We showed recently that many human milk proteases act not only within the mammary gland, but also within the infant’s stomach [8, 9]. These findings provoked our hypothesis that milk enzymes are more than a defect: rather, that they are an evolutionarily driven, beneficial component. We hypothesized that the activity of these proteases within the infant is an important component of the infant’s digestive capacity. Infants have a lower digestive capacity than adults [10], therefore, human milk enzymes may serve as a compensatory factor for this digestive insufficiency. However, proteases are only moderately active in the mammary gland. These proteases are not all activated, and milk contains not just proteases and protease activators, but protease inhibitors. This finding suggests there is a benefit to balancing between too little and too much proteolytic activity. The central question of this review is: what evolutionary purpose can these proteolytic systems and their careful balance serve? We propose several hypotheses, evidence to support them and guidelines to test them. This review examines the origins, presence, activity, interactions, micro-locations and changes across lactation, gestational maturation and health status of these proteolytic system components.
Proteolytic Systems in Milk
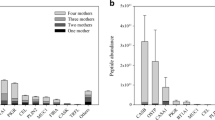
Milk contains numerous complex and interconnected proteolytic systems, including zymogens, active proteases, protease inhibitors and protease activators (Fig. 1). The balance of these system components controls the overall proteolytic activity of milk. Research demonstrates that human milk contains plasmin [11], anionic trypsin (now known as trypsin-2) [12], anionic elastase (now known as neutrophil elastase, ELANE) [12], cathepsin D [11, 13], thrombin and kallikrein [11] and carboxy- and aminopeptidases [13]. Human milk may also contain cathepsin B, as demonstrated by transcriptomic analysis of milk [14]. Bovine milk contains many of the same proteases, including plasmin [15], elastase [3], cathepsin D [16], cathepsin B [17, 18], kallikrein [19] and several carboxy- and aminopeptidases [17]. These proteases are typically secreted in their inactive form (as zymogens) and must be cleaved at a specific peptidic bond by a protease activator to become the active enzyme. Milk also provides many protease activators; for example human and bovine milk contain two plasmin activators: tissue-type plasminogen activator (t-PA) and urokinase-type activator (u-PA) [17, 20–22]. However, the presence of milk protease activators does not mean that all milk proteases are active. Milk counterbalances the effect of the protease activators by providing a variety of antiproteases [23–25] (e.g., α1-antitrypsin).
An overview of the proteolytic system network in milk. Protease activator activity is depicted in green. Inhibitory activity is highlighted in red. Protein names in italics represent components of the proteolytic system not yet found in milk. u-PA urokinase-type plasminogen activator, t-PA tissue-type plasminogen activator
We demonstrated recently via mass spectrometry-based peptidomic sequencing that milk proteases release hundreds of peptides from proteins within the human and bovine mammary gland [25–28]. The sequences of these peptides in term and preterm milk were analyzed with bioinformatic approaches. These searches suggested that plasmin, cathepsin D, elastase, cytosol aminopeptidase and carboxypeptidase B2 are active in human milk throughout lactation [25, 29, 30]. This combination of peptidomics and bioinformatic analysis shows with sequence-specific detail that even milk from healthy mammals milk begins to digest itself within the mammary gland [9, 30]. However, in both human and bovine milk, the digested peptides represent only a minority of the total protein component, and only specific proteins are digested [25, 31]. Certain proteins and fractions of proteins remain intact (e.g., lactoferrin, immunoglobulins, β-lactoglobulin (for bovine milk)), while others are partially digested (e.g., caseins, osteopontin, polymeric immunoglobulin receptor). This finding raises the question: what purpose might this minimal, controlled degradation serve? The following summarizes what is known about the major proteolytic systems in milk.
Plasmin System
Plasmin, which cleaves on the C-terminal side of lysine or arginine residues [32], is active in human and bovine milk [15, 33]. In fact, plasmin is likely the most active protease in human and bovine milk [15, 21, 33, 34]. Plasmin in bovine milk is known to degrade β-, αs1- and αs2-caseins to peptides [35].
The complete plasmin system is present in both human and bovine milk, including the zymogen (plasminogen), the active enzyme (plasmin), activators and inhibitors. In order to create active plasmin, its inactive form plasminogen must be cleaved at a specific peptide bond by plasmin activators [36]. Two serine proteases in both bovine and human milk perform this task: urokinase-type plasminogen activator and tissue-type plasminogen activator [15, 19–21].
Both human and bovine milk contains inhibitors that block the activators’ conversion of plasminogen to active plasmin, including type-1 plasminogen activator inhibitor (PAI-1) [19, 21, 37] and α1-antitrypsin (also known as α1-antiproteinase, SERPINA1) [17, 38, 39]. Proteomics revealed that bovine milk [17], but not human milk [39], contains plasma serine protease inhibitor (SERPINA5), which inhibits both tissue-type and urinary-type plasminogen activators [40]. Bovine milk contains additional protease inhibitors that inhibit the activated plasmin by directly binding, including α2-macroglobulin [41], α2-antiplasmin (SERPINF2) [37, 41], inter-α-trypsin inhibitor (cleaved from protein AMBP) [17, 42] and α1-antitrypsin [17, 38]. Human milk contains AMBP [39] and α1-antitrypsin [39] which directly inhibit plasmin.
This mixture of proteolytic system components in milk causes a mixture of active and inactive plasmin to exist in milk. At 6–7 days postpartum, bovine milk contains 4.8 (±4.2) Units/mL of plasmin activity and 12.4 (±9.9) Units/mL of plasminogen-derived activity [15]. Plasmin activity appears to increase across lactation in bovine milk [43]. Conversely, plasmin activity appears to decrease across lactation in human milk [29]. α1-Antitrypsin concentrations decrease across human lactation [22]. Both plasmin and plasminogen activator activity increase during bovine mammary gland involution [44]. Presumably, this increase in protease activity during involution is important in breaking down the mammary gland tissues.
Plasminogen in milk exists both free and in association with casein micelles [19, 21]. Tissue-type plasminogen activators, which converts plasminogen into the active plasmin, also binds to casein micelles and is present at much higher concentrations in the casein fraction than in whey (42 times higher in casein than whey in human milk) [21]. The majority of milk’s active plasmin is casein micelle-bound [45], most likely because of the physical proximity of the plasminogen and plasminogen activator. In vitro experiments show that plasmin activity for a mixture of plasminogen and plasminogen activator is effectively increased by the addition of casein micelles [21, 46, 47]. Both human and bovine caseins accelerate the rate of plasminogen activation by tissue-type plasminogen activator [47], likely due to the proximity between the plasminogen and the plasmin activator [21]. Interestingly, some of the plasminogen activator inhibitors, which inhibit the activator’s conversion of plasminogen to plasmin, are bound to tissue-type plasminogen activators in casein micelles [19]. Ostensibly, the presence of the plasminogen activator inhibitors on the micelle prevents more extensive casein micelle degradation in the mammary gland. The other main type of plasminogen activator in milk, urokinase-type plasminogen activator is associated only with the human milk somatic cell fraction [48], specifically the neutrophils [49, 50].
The presence of β-casein-derived peptides as the major degradation products in human and bovine milk [25, 28, 31], despite not being the most abundant protein, suggests that the active casein-bound plasmin degrades proteins that associate with the micelle structure. We hypothesize further that a major reason whey proteins such as α-lactalbumin, secretory immunoglobulin A and lactoferrin do not yield digested peptides in milk [25] is because they do not associate with the micelles that contain the majority of active plasmin. Whey proteins’ globular structure and disulfide bonds also likely increase the resistance of these proteins to proteolysis in comparison with the looser structures of caseins.
Cathepsin Systems
A number of cathepsins are present in milk, including cathepsins B [17, 18], D [17] and Z [17] in bovine milk and cathepsins D [51], B [14], H [39] and S [39] in human milk. Other cathepsins, including cathepsin L and cathepsin G may be present in bovine milk, but their presence has not been confirmed [3]. This family is wide-ranging in functionality. Cathepsins, as a family, typically act within the lysosome at acid pH [52]. A defining feature of cathepsins is that they can be inactivated by oxidation and reactivated by reducing agents (e.g., glutathionine) [52]. The dozen members of the cathepsin family have different structures and catalytic mechanisms (some are aspartic proteases, some are serine proteases and some are cysteine proteases).
Unlike other cathepsins, cathepsin D seems to be active at neutral pH [53]. Cathepsin D, a soluble lysosomal aspartic endopeptidase—first synthesized as the zymogen procathepsin D in the rough endoplasmic reticulum [54]—cleaves predominantly between two hydrophobic amino acids, particularly when following Leu [32]. Although the active form of cathepsin D is found in the soluble component of bovine [55] and human milk [11, 51], the major form of this enzyme in milk is the inactive zymogen procathepsin D [51, 56]. Incubation of procathepsin D purified from bovine milk at pH 3.5 and 5.0 caused auto-activation to moderately active pseudocathepsin D, but apparently not into mature cathepsin D [57]. Activation of procathepsin D to cathepsin D requires cysteine proteases, but the specific activators are unknown [58]. Specific inhibitors of cathepsin D or activation of procathepsin D have not been found in milk. In addition to in vitro enzymatic assays which demonstrate that cathepsin D is active in bovine milk [59], our sequence-based bioinformatic study predicted that cathepsin D was active in bovine and human milk [30, 31]. Whether procathepsin D and cathepsin D in milk originate from secretion by MEC or milk immune cells remains unknown. Both MEC [60] and activated lymphocytes [61] can secrete procathepsin D. Cathepsin D activity in bovine milk is positively correlated with somatic cell count [59], but whether this reflects an increased amount of cathepsin D and/or procathepsin D and/or increased activation of the indigenous procathepsin D pool remains to be determined [62].
Cathepsin B, a cysteine protease, is also found in bovine milk [18] and may be present in human milk [14]. In vitro, cathepsin B actively cleaves β-casein and αs1-casein, with a preference for cleavage sites with Leu, Val, Gln, Pro and Ser [63]. Cathepsin B is most active at pH 6.0 and is inactivated at > pH 7.0 [64]. Whether cathepsin B is active in milk and whether the cathepsin B in milk is derived from MEC or milk immune cells remains unknown. Likewise, we are not aware of any inhibitors or activators of cathepsin B present in milk.
The degree to which cathepsins, their inhibitors and activators change in abundance across lactation in human and bovine milk remains unknown and deserves further research.
Elastase System
Elastase was found in human milk [12] but was not active within milk based on a succinyl-trialanine-p-nitroanilide substrate hydrolysis [12]. However, elastase was active in human milk based on hydrolysis of the substrate N-carbobenzoxy-alanine-napthylester [22]. The elastase zymogen proelastase has not been identified in milk. Elastase has not been identified in bovine milk, however it was present in polymorphonuclear neutrophils in bovine milk in experimentally-induced mastitis [65]. Elastase is a serine protease [66] that digests a wide variety of protein substrates [66], with a preferred specificity for bonds involving uncharged, non-aromatic amino acids (e.g., Ala, Val, Leu, Ile, Gly, Ser) [67]. Our peptidomics-based bioinformatic analysis predicted that elastase actively digests human milk proteins within the mammary gland [30]. To our knowledge, no elastase activators have been found in milk. However, several elastase inhibitors are found in milk. Antielastase was found in human milk from birth to 4 months postpartum [23], and plasma elastase inhibitor was found in bovine milk [41]. Inter-α-trypsin inhibitor, which is present in bovine milk [17, 41] but has not yet been detected in human milk, is also known to inhibit polymorphonuclear lysosomal granulocytic elastase [68]. α1-Antitrypsin (SERPINA1), found in bovine [17] and human [24] milk, also strongly inhibits elastase [38]. Some debate exists as to origins of elastase in milk: some suggest it originates from MECs [12], while others refer to it as a lysosomal protease (i.e., derived from milk immune cells) [3] as milk polymorphonuclear neutrophils produce elastase [69, 70]. Again, the answer to this question could be found in carefully designed transcriptomic analysis. How elastase, elastase inhibitors and elastase activators change across lactation remains unknown.
Trypsin System
Trypsin, which cleaves on the C-terminal side of lysine or arginine residues, is present in human milk [12, 17], but has not been identified in bovine milk. This milk trypsin, sometimes referred to as anionic trypsin, was detected in human milk by immunodiffusion and immunoelectrophoresis [71]. When comparing the amino acid sequences of anionic trypsin with that of trypsin 1 and 2 (using BLAST in Uniprot), we found that anionic trypsin has the same sequence as trypsin 2 (anionic trypsin is likely an older name). Radioimmunoassay showed that the concentration of trypsin in human milk is 2.9–5.6 μg/L.
Trypsinogen, the zymogen of trypsin, has not been identified in human milk. If present, this zymogen could be activated by thrombin [72] or enterokinase [73]. Thrombin has only been found as the zymogen form in human milk [13], and enterokinase has not been found in either bovine or human milk. However, enterokinase is secreted in the duodenum [74], so the milk trypsin could be activated once it reaches the small intestine. This hypothesis is discussed further in the “Role in Protein Digestion within the Infant” section.
Bovine milk contains inter-α-trypsin inhibitor (demonstrated by western blot and ELISA), which inhibits trypsin directly through binding [41]. Bovine milk also contains an unidentified bovine plasma trypsin inhibitor [41]. Based on a BLAST search against the sequence [75] in Uniprot, this protein appears to be SERPINA3-1, a known potent serine protease inhibitor with action against trypsin as well as elastase [42]. Proteomic studies show that bovine and human milk contains multiple inter-α-trypsin inhibitors, which are cleaved from a protein called AMBP [17, 39, 42]. Milk from women delivering at term and preterm contains the antiprotease α1-antitrypsin (SERPINA1) from the first day of lactation [22–24]. As previously mentioned, bovine milk also contains α1-antitrypsin [17]. α1-Antitrypsin is a serpin—a serine protease inhibitor—that inhibits a wide variety of proteases including trypsin [76]. α1-Antitrypsin inhibits trypsin through direct binding [77]. Trypsin inhibitory activity in human and bovine milk are similar [78].
When anionic trypsin (trypsin-2) is isolated from human milk, it is active (demonstrated by splitting the chromogenic substrate benzoyl-DL-arginine-p-nitroanilide) [71]. However, in the context of milk, trypsin seems to have no activity [71]. This lack of activity is likely due to effective blocking by the trypsin inhibitors present in milk. Though trypsin is inactive within human milk, it may be activated within the infant’s intestine after dissociation from the inhibitors.
As mentioned previously, α1-antitrypsin decreases across lactation [22]. The degree to which trypsin, trypsinogen, trypsin activators and other trypsin inhibitors change in abundance across lactation remains unknown.
Chymotrypsin System
To our knowledge, neither human nor bovine milk contain chymotrypsin or chymotrypsinogen. We found no antibody-based or proteomic evidence for the presence of this protein in either bovine or human milk. The main activator that converts inactive chymotrypsinogen to chymotrypsin is trypsin [79], which is present in human milk although apparently not active [71]. From the first day of lactation [22–24, 80] and at least up to 4 months postpartum [23], milk from women delivering at term and preterm contains the serpin antiprotease α1-antichymotrypsin (SERPINA3), which inhibits chymotrypsin through direct binding. Proteomics demonstrates that α1-antichymotrypsin is also present in bovine milk [17]. Bovine and human milk also contains α1-antitrypsin (SERPINA1) [17, 39, 81], which can inhibit chymotrypsin and actually has a higher specificity for chymotrypsin than α1-antichymotrypsin [81]. α1-Antichymotrypsin is not as versatile in its actions, as it does not bind to trypsin [81]. Bovine milk also contains plasma C1 protease inhibitor (SERPING1) [17, 41], which inhibits chymotrypsin. Why milk contains chymotrypsin inhibitors but not chymotrypsin remains unknown. These inhibitors may be present due to their overlapping inhibitory function for other serine proteases. Two chymotrypsin inhibitors, α1-antitrypsin and α1-antichymotrypsin decrease across lactation in human milk [22].
Thrombin System
A proteomics study identified peptides from the overall sequence of prothrombin in human colostrum [13], but these data cannot be applied to determine whether the fragments were derived from prothrombin or the activated form, thrombin. Thrombin activity has not been reported in human or bovine milk, and no thrombin activators (e.g., coagulation factor X) have been identified in proteomic analyses of human or bovine milk. α1-Antitrypsin (SERPINA1), which is present in bovine [17] and human [39] milk, inhibits thrombin activity [38]. Similar to α1-antitrypsin, inter-α-trypsin inhibitor found in bovine and human milk is likely to inhibit thrombin. Antithrombin III, which also inhibits thrombin activity, has been identified in bovine milk via western blot [41]. Proteomics confirms that bovine milk contains antithrombin III (SERPINC1) and also identifies thrombin inhibitor (SERPIND1) [17]. Proteomics demonstrate that human milk contain SERPINC1 but not SERPIND1 [39].
Kallikrein System
Plasma kallikrein (KLKB1) is an important blood serine protease [82] that has been found in human milk [11] and bovine milk [19]. Proteomics shows that human colostrum contains kallikrein 11 (Q9UBX7) and kallikrein 6 (Q92876) [11]; however, whether these proteases are present in the zymogen or active protease form is unknown. Active kallikrein has not been identified in human or bovine milk. In blood, kallikrein plays a key role in the contact phase activation of blood coagulation, fibrinolysis and kinin formation [82]. Proteomics shows that bovine milk contains kallistatin (SERPINA4), plasma serine protease inhibitor (SERPINA5) and plasma protease C1 inhibitor (SERPING1), which all inhibit kallikrein [17]. Plasma protease C1 inhibitor has also been found in bovine milk via western blot [41]. In blood, plasma protease C1 inhibitor is one of the major regulators of kallikrein and is important in the regulation of blood clot formation [82].
Amino- and Carboxypeptidase Systems
A recent proteomics study identified cytosol aminopeptidase (LAP3) and carboxypeptidase B2 (CPB2) in human milk [13]. The proteomic data cannot determine whether or not these enzymes were present as their active forms or as zymogens. Activation of carboxypeptidase B2 is performed by thrombin [83], which has been shown to be present but not active in human milk. Analysis of the cleavage sites of peptide sequences identified in human milk suggests that both cytosol aminopeptidase and carboxypeptidase B2 are active within the mammary gland [29]. Proteomics shows that bovine milk contains aminopeptidase Q (AQPEP), cytosol aminopeptidase (LAP3), carboxypeptidase B2 (CPB2) and glutamate carboxypeptidase 2 (FOLH1) [17]. Bovine milk also contains a lysosomal proteases called tripeptidyl peptidase I (TPP1), which releases tripeptides from the protein N-terminus [17].
Matrix Metalloproteinase System
Matrix metalloproteinases (also known as collagenases), which play a key role in extracellular matrix degradation and tissue remodeling, have been identified in human milk. Together, these proteases can degrade many kinds of extracellular matrix proteins. The collagen and gelatin-degrading metalloproteinases MMP-2 and MMP-9, both in the group called “gelatinases,” were detected in both term and preterm human milk [84, 85]. These two enzymes have a gelatinase-binding region not found in other MMPs, which allows them to degrade gelatin. The inhibitor of this enzyme, tissue inhibitor of MMP 4 (TIMP-4), was also detected in human milk. TIMP-1 has been identified in proteomic analysis of human milk [86] and was significantly more abundant in preterm milk compared to term milk [85]. Our literature search revealed no evidence for active MMPs in human milk.
Origins
Milk proteins generally are considered to be either expressed by MEC or derived from blood [87–89]. The majority of milk proteins (e.g., caseins) are synthesized in MEC and then secreted across the apical surface into the alveolar lumen, whereas some proteins including immunoglobulins and transferrin are derived from blood and transported into milk [88, 89]. For example, milk caseins are known to be synthesized in the MEC because the agglomeration into sub-micelles in the Golgi complex can be observed by microscopy and micelle formation can be observed in secretory vesicles [88]. Immunoglobulins secreted by plasma cells binds to receptors on the basolateral side of MEC, and the entire receptor-ligand complex is endocytosed and transferred across the cell [90]. Once it reaches the apical membrane, the complex is cleaved so that the IgA is secreted into the milk attached to a portion of the receptor called the secretory component [90]. Transferrin can be secreted into milk via MEC synthesis in some species, and also can be transferred from blood to the milk via transcytosis [91]. The transmission of transferrin from blood to milk was shown by measuring the transport of biotin and gold-labeled transferrin across rabbit MEC [91]. Milk proteases and inhibitors could be secreted via blood or MEC as well as by immune cells in the mammary gland (Fig. 2). Although researchers often postulate on the sources of milk proteolytic system components, their origins remain mostly unconfirmed. Determining the origins of different proteolytic system components could provide hints as to their biological functions and evolutionary role.
Using RNA sequencing technology to examine the genes expressed in target cells is a method to determine the sources of the proteins. Separating the target fraction from milk and then extracting the mRNA is the most common way to characterize the milk transcriptome, as collecting milk samples is non-invasive compared with collecting mammary tissue samples. The transcriptional profiling of milk can provide useful information. For example, Wickramasinghe et al. [20] demonstrated that the bovine somatic cells contained mRNA for most of the milk cathepsins and certain proteins in the plasmin system, which indicates that at least a portion of these proteins in milk originate from the somatic cells rather than from blood absorption. However, milk somatic cells represent a heterogeneous mixture, including immune cells, epithelial cells and stem cells [2, 92]. The transcripts thus represent the combination of cellular activity from these many cell types, and distinguishing which type of cell each transcript derived from is not possible. To our knowledge, no research has yet separated the different classes of cells in milk prior to transcriptional profiling, so we cannot determine which proteolytic system components are released from immune cells and which are from MEC. Further complicating this analysis, the mere presence of proteolytic system components in the mRNA extracted from a cell does not equate to knowledge that the component is secreted into the milk pool. Rather, many of the mRNA signals are for proteins that will remain within the cell. The application of milk somatic cell isolation followed by preparative-scale cell sorting technology could enable transcriptomic analyses that more clearly delineate which enzymes, zymogens, inhibitors and activators are produced in each cell type. However, even if these MEC are fully isolated, they still represent sloughed MEC, which are typically dying cells, therefore, the transcripts extracted may not represent that of a healthy MEC.
Lemay et al. [14] used an exciting new non-invasive technique to examine MEC transcriptomics in cytoplasmic crescents from milk fat globules. When milk fat globules are secreted, often a small crescent of MEC cytoplasm is caught within the globule. This source of transcripts represents the mRNA present in active MEC rather than sloughed, dying cells. This approach could provide a solution to understanding which proteases are produced by the MEC. The paper demonstrates that transcripts for both cathepsin D and B are present in the isolated fat fraction from human milk. Unfortunately, the time-point when these transcripts were seen in high abundance (colostrum samples) coincided with when the milk fat globules were most highly contaminated with milk immune cells. Therefore, we still cannot know whether these cathepsins originated in MEC or immune cells. That said, this approach is highly promising, and investigation of methods to more cleanly extract milk fat globules without cell contamination are highly warranted. To better sample healthy MEC transcriptomics, either a tissue collection and cell extraction or a cleaner cytoplasmic crescent extraction technique is necessary.
Expression by Mammary Epithelial Cells
Free amino acids in blood enter into mammary cells by amino acid transport systems with respective transporters for different groups of amino acids [89, 93]. After the uptake of amino acids from blood, the basic process for protein synthesis in the mammary gland is similar to that in other tissues. Initiated by factors that induce gene expression, proteins are synthesized in the rough endoplasmic reticulum and undergo post-translational modifications before exocytosis across the apical membrane into the lumen with other milk components [89, 94]. Therefore, the mRNA of specific proteases or inhibitors can indicate whether the proteases and inhibitors are synthesized in mammary cells.
Lemay et al. [95] used RNA sequencing to study the total RNA in mammary biopsies of lactating rhesus macaques. This technique can reveal the biosynthesis process that happens in the mammary gland. In addition to determining gene expression, detecting proteins from cell culture or tissue culture can show whether proteases would be synthesized in these cells. Lkhider et al. [53] conducted a study on lactating rat mammary gland fragments and acini. With immunoblotting and immunofluorescence, they showed that the active enzyme form of cathepsin D is released from endosomes or lysosomes of MEC.
Transport from Blood
As reviewed by Ollivier-Bousquet [96], during lactation, a healthy mammary gland can carry proteins originating from blood into milk by transcytosis (i.e., transport of macromolecules from one side of the epithelium to the other). The transcytosis process enables proteins such as transferrin and prolactin to be released into milk in intact and active forms [96]. Some proteolytic system components in milk may be transported from blood in this way. Absorbing proteins from blood rather than synthesizing them from amino acids within the MEC may be a strategy for conserving maternal energy.
According to Kelly et al. [3], the major bovine milk proteases originate from blood. Plasmin enters milk in soluble form and lysosomal proteases, including cathepsins and elastase, enter in lysosomes of somatic cells. Here, we consider only protein components circulating freely in blood that enter into milk as being blood-derived. Proteins within somatic cells that migrate from the blood to the mammary gland are not considered as blood-derived. Kelly et al. [3] support this theory by stating that the amino acid sequence between proteases in milk and those in blood are identical. However, since genes coding the specific enzyme are the same within the individual genome, having an identical amino acid sequence is expected and does not prove that proteases in milk are derived from blood.
The absence of gene expression in mammary gland and milk somatic cells (e.g., sloughed MEC, immune cells, stem cells) provides a better support for the migration theory. The lack of mRNA in target cells indicates that protein is not synthesized in those cells. Wickramasinghe et al. [20] studied the mRNA expression profiles in bovine milk somatic cells. They showed that the plasminogen gene was not expressed in any of the milk somatic cell samples, which supports the theory that plasmin and plasminogen migrate from blood to milk. Although the absence of gene expression in milk somatic cells provides support that milk proteases are derived from blood, direct evidence, such as defining the transport pathways of specific proteases across the epithelium, is needed to confirm the blood origin theory.
How the proteases are transported from blood to milk remains unclear at the molecular level. Many interesting questions need to be answered, such as do the proteases pass the mammary epithelium by transcellular pathway or paracellular pathway, do respective receptors or transporters for specific proteases exist, and are the proteases modified during transportation? If receptor-mediated transport could be demonstrated, this finding would provide evidence for the evolutionary importance of these proteases in the milk.
Release from Immune Cells
Milk contains a heterogeneous population of somatic cells, which includes live immune cells [92, 97]. Immune cells such as macrophages, neutrophils and lymphocytes are present in human milk, and they actively express bioactive products [92, 97]. Lysosomal proteases (e.g., cathepsin D) can be expressed by immune cells. The major role of these lysosomal proteases within the immune cells is intracellular degradation of proteins [3, 62, 98]. Unless secreted, lysosomal proteases mostly do not interact with milk proteins. However, somatic cell count correlates with the activity of these proteases and total proteolysis in milk [99]. For example, cathepsin D can be secreted by macrophages into the extracellular space during inflammation [100]. Thus, these lysosomal proteases present in milk are likely released from immune cells by secretion or released with immune cell death and degradation, and then interact with milk proteins.
Specificity of Degradation
Digestion within milk seems targeted at specific proteins (e.g., the caseins, polymeric immunoglobulin receptor, osteopontin), whereas many abundant proteins are left intact (e.g., lactoferrin, immunoglobulins) [25, 28]. Likewise, in bovine milk, casein proteins release peptides within the mammary gland, whereas β-lactoglobulin, lactoferrin and immunoglobulins do not [31]. This specificity could provide a hint as to milk proteolytic systems evolutionary function. The lack of digestion of lactoferrin and immunoglobulin could be functional: by allowing these proteins to stay intact, they can continue to exert their well-known biological actions within the infant. In both humans and cows, the peptides released are highly similar across animals within the species and across lactation [25, 31].
Role within the Mammary Gland
Proteases are active within the mammary gland even in healthy mothers. This begs the question: what roles do these proteolytic systems play? One possibility is that milk proteases help to regulate casein micelle size. Alternatively, these proteases could be important for releasing functional peptides that are important for mammary gland health. For example, antimicrobial peptides released endogenously within the mammary gland by milk proteases are antimicrobial [25]. These antimicrobial endogenous peptides may have a role in the prevention of mastitis or recovery from the disease. Milk proteases may also be present to help with involution. Many milk enzymes increase during involution [101, 102], and these enzymes may be important in the cellular remodeling that occurs afterwards.
The protease inhibitors in milk could prevent proteolysis from destroying mammary gland tissue prior to involution. Overactive proteolysis by milk enzymes like matrix metalloproteinases could lead to major mammary tissue degradation. Likewise, inhibitors in milk could prevent overactive proteolysis within the mammary gland on milk proteins. As mentioned above, many bioactive milk proteins (e.g., lactoferrin, immunoglobulin) need to remain intact to function, and they appear to be protected within the mammary gland.
Role in Protein Digestion within the Infant
We showed via peptidomic and bioinformatic analysis that milk proteases actively break down protein within the human infant’s gastrointestinal tract [8, 9]. The question then becomes, why might the activity of milk proteases within the infant’s gut be evolutionarily advantageous? Our hypothesis is that these proteases are secreted by milk somatic cells or are transported into milk from the bloodstream to aid in protein digestion in the infant. This hypothesis makes sense in the context of the infant’s low digestive capacity. Infants produce low amounts of gastric acid in comparison with adults, and the buffering capacity of milk makes the postprandial pH more neutral than in adults [103]. The more neutral pH values in the infant’s stomach inhibits the acid protein denaturation that occurs in adults [10]. Because pepsin, the main gastric enzyme, performs optimally at low pH, this enzyme is likely less active in the stomach of infants than in the stomach of adults [10]. Intestinal digestive function is also lower in infants than adults. Enterokinase, which is secreted by duodenal epithelial cells in response to food stimulation [104], is essential for proteolysis in the small intestine as it is responsible for the activation of trypsinogen to trypsin [105], which activates chymotrypsinogen to chymotrypsin, proelastase to elastase and procarboxypeptidase to carboxypeptidase [106]. Enterokinase is present at birth and is active in infants, but the activity is less than 20 % of that in older children [107]. For the first month postpartum, the concentration of trypsin in the duodenum is also lower than in adults [108]. Chymotrypsin concentration in the pancreas is 10–60 % of that in adults [108]. Carboxypeptidase B concentration and activities were 10–25 % of those in 2-year-olds [108]. This lower digestive function in infants may be partially compensated for by milk enzymes.
Interestingly, some milk proteases increase in activity once they reach the stomach (e.g., cathepsin D) [8]. The question then becomes, what increases their activation? This increased activity could be due to the lowered pH (cathepsin D is activated at low pH [52]), removal of inhibitors or additional protease activators enabling the cleavage of zymogen to active protease. Likewise, trypsinogen has no identified activators in human milk. This enzyme could be activated by enterokinase once it enters the infant’s intestine.
The presence of antiproteases in milk could also partially limit protein degradation in the infant. The extent to which milk antiproteases inhibit proteolytic digestion within the infant’s stomach remains unknown. These antiproteases may help prevent degradation of bioactive proteins (e.g., lactoferrin, immunoglobulins) within the infant’s gastrointestinal system [109]. The balance of what is digested and what is protected from digestion in breast milk-fed infants merits further exploration.
If the purpose of proteases in human milk is to aid the infant’s digestion of proteins, it would, ostensibly, be counterproductive to synthesize protease inhibitors. The presence of inhibitors suggests that infants thrive best with a balance of proteolytic action because infants need some intact proteins. Gastric emptying can influence pancreatic secretion [110]. Hydrolyzed peptides and amino acids may pass through the stomach at a higher rate and thereby trigger less secretion of pancreatic enzymes to digest them. Kinouchi et al. [111] showed that rats fed protein hydrolysates had lower pancreas weight and lower pancreatic enzyme expression and secretion ability compared with those fed intact proteins. A lack of exposure to intact proteins can set infants up for lowered digestive function throughout life. This finding may present a problem for the strategy of feeding hydrolyzed formulas to infants with milk protein intolerance. To the best of our knowledge, no studies have investigated the long-term effects of hydrolyzed proteins on digestive function of the infant through to adulthood. Milk protease activity decreases across lactation, as the infant’s own protease production increases. This lowered proteolytic activity with continued lactation may be advantageous to the infant, as the higher amount of intact proteins may prepare the infant’s digestive system for the digestion of solid foods during the weaning process. Overactive milk proteases in the mammary gland and the infant’s gut can lead to the premature degradation of bioactive proteins (e.g., lactoferrin, immunoglobulins) and bioactive peptides (e.g., antimicrobials, opioids).
Low activity or absence of proteases in breast milk could lead to incomplete digestion of proteins in the infant’s small intestine. Ideally, dietary proteins are digested completely by host endogenous proteases and absorbed as amino acids or small peptides in the small intestine. Limited protein digestion in the small intestine can limit amino acid absorption of the infant. The large intestine has little to no ability to absorb amino acids [112]. Lower amino acid absorption means that the infant’s overall protein requirements increase.
When proteins or protein fragments reach the colon, they can serve as a food source for protein-fermenting (putrefactive) bacteria. This food source allows these bacterial species to grow in population size while leading to reduced counts of beneficial preferentially carbohydrate-consuming bacteria, such as bifidobacteria [113]. Bacteria whose growth is enhanced by excess protein in the colon include the potentially pathogenic Clostridium perfringens [113] and various Bacteroides species, especially B. fragilis [114]. Several colonic bacterial groups, including peptococci, acidaminococci, veillonella and some fusobacteria, eubacteria and clostridia, have only weak saccharolytic activity and preferably ferment amino acids [115]. These putrefactive bacteria produce metabolites such as hydrogen sulfide, ammonia, amines and phenols, which have negative effects on gut health. These microbial metabolites can increase epithelial permeability [116, 117], reduce colonic mucus layer thickness [118], lead to inflammatory reactions [119, 120], provoke colonic epithelial cell DNA damage [121] and reduce colonic epithelial cell viability [122]. These effects likely increase the infant’s risk of diarrhea and other inflammatory bowel conditions.
For mother-infant pairs that wean gradually (as opposed to an abrupt switch from milk to weaning food), milk enzymes may have a role in breaking down weaning food proteins. Again, by helping to break down these proteins, milk proteases may help prevent the overgrowth of putrefactive bacteria in the colon. Aiding the digestion of proteins may help avoid development of allergies by eliminating protein epitopes.
Changes across Lactation
Milk protease activity decreases across human lactation [22, 78]. The mean total protease activity in term mother’s milk decreases from 1.38 μmol tyrosine/1,000 mL/min in colostrum to 0.76 μmol tyrosine/1,000 mL/min in 7–32 day postpartum milk. This change over time might suggest that the need for milk proteases is reduced as the infant develops an increasingly robust digestive system. However, at involution, milk protease activity increases (shown for both plasmin and plasminogen activator activity in bovine milk [44]). Presumably, this increase in protease activity during involution is important in breaking down the mammary gland tissues. In the second phase of involution (non-reversible), the superfluous lobuloalveolar cells, their supporting matrix and accumulated milk are cleared by the combined action of lysosomal enzymes and matrix metalloproteinases, and the gland resumes an almost pre-gestation status [123].
Inhibitor concentrations seem to change across lactation as well as protease activity. For example, α1-antitrypsin and α1-antichymotrypsin concentrations decline across human lactation from day one to 2 weeks postpartum in both term and preterm milk [22, 24], but they remain detectable up to 160 days postpartum [22]. Trypsin inhibitory capacity in human milk decreases from 70 μg trypsin/mL milk in the first 3 days of lactation to 38 μg trypsin/mL milk 1 week to 4 months postpartum [23]. This decrease in inhibitor concentration could have a purpose: the high concentration of α1-antitrypsin and α1-antichymotrypsin in colostrum may protect the immunological milk proteins from degradation. These intact immunoglobulins can be absorbed from milk across the infant’s gut [124]. The higher concentration of inhibitors in colostrum may help to protect these important immunoglobulins.
Difference between Term and Preterm Infants
Armaforte et al. [125] found via 2D-SDS-PAGE, in-gel trypsin digestion and mass spectrometry that low-molecular weight casein fragments were over-expressed in preterm human milk as compared with term milk, whereas intact αs1- and β-casein were present at lower concentrations in preterm than term milk. These findings suggested that more degradation of casein occurs in preterm human milk than term milk. Specifically, plasmin activity in human preterm milk is higher than in term milk as shown by chromogenic enzyme-substrate assays (0.147–0.397 7-amino-4-methylcoumarin/min preterm vs. 0.045–0.104 7-amino-4-methylcoumarin/min term) [126] and peptidomics-based bioinformatic analysis [29].
Tight junctions of the mammary gland are leaky during pregnancy and undergo closure around parturition [127]. A previous review suggested that the mammary glands of mothers at <37 weeks of gestation have leaky tight junctions due to immaturity of the gland [128]. We hypothesize that incomplete closure of tight junctions in the immature mammary gland of preterm mothers underlies increased leakage of proteases and protease activators into the milk, explaining the observed higher amounts of peptides and the higher predicted plasmin activity in preterm human milk compared with term milk [29]. The increased proteolytic activity in preterm milk could also be due to increased expression of activators or decreased expression of inhibitors in the immature preterm mammary gland.
Compared with the term infant, the preterm infant is thought to be poorly equipped for the task of protein digestion [10, 129]. One study showed that gastrointestinal trypsin activity is lower in preterm than in term infants in early life [129]. Another study showed that gut trypsin activity decreases with human milk feeding in premature infants [130]. The high protein degradation by milk proteases in preterm milk might attenuate this lowered overall proteolysis. Before the advances in feeding strategies and modern medicine, premature infants (<32 weeks) almost never survived [131, 132]. It seems unlikely that the high proteolytic activity in preterm milk evolved to benefit preterm infant health. However, some studies showed that preterm human milk may in fact be better suited to the premature infant [129]. The increased milk protease activity in the preterm infant may compensate for the lower digestive function in premature infants. This compensation could aid in complete protein digestion within the small intestine, preventing milk proteins from arriving intact or as peptides to the distal colon where they can act as a food source for potentially harmful putrefactive bacteria [29]. Alternatively, term milk could be the “gold standard” for all infants, both term and preterm, and the increased proteolysis in preterm milk is simply the consequence of inadequately regulation in the mammary gland of a preterm mother.
Changes with Disease State
Proteolytic activity in the mammary gland can change with disease state, specifically inflammation of the mammary gland. Mammary gland inflammation is called mastitis. By definition, mastitis is associated with increasing somatic cell count. Both plasmin and plasminogen increase with increasing somatic cell count in bovine milk [101]. In mastitis, the concentration of both urokinase-type plasminogen activator and tissue-type plasminogen activator in bovine milk is higher and this causes higher plasmin activity in mastitis [101]. The total proteolytic activity in bovine milk also increases with increased somatic cell count [27, 133]. We showed, with a peptidomics approach, that the number of peptides released is increased in mastitic quarters compared with healthy quarters of the same cow [27]. Bioinformatic analysis of enzyme cleavage revealed increases in activity of cathepsin D and elastase (p < 0.05) with subclinical mastitis [27]. Milk proteases including plasmin, cathepsins B and D and elastase are up-regulated in bovine milk samples from mastitic mammary glands [134, 135]. Procathepsin D is 250-fold higher in mastitic bovine milk than in milk with low somatic cell count [136]. The increased proteolytic activity in mastitis has been hypothesized to result from increased plasminogen transmission from blood to bovine milk due to increased barrier permeability [137, 138] and increased protease secretion from bovine milk immune cells [35]. Neutrophils enter the mammary gland as part of the inflammatory process to eliminate the bacterial infection [139]. These neutrophils release enzymes like elastase [3]. Likewise, macrophages can secrete cathepsin D. Though cathepsin D has no activity ≥pH 7, at sites of inflammation the pericellular pH may be low enough to activate cathepsin D [100]. Invading bacteria present in mastitis often release exogenous enzymes into the bovine milk, including elastase [140]. The increase in bacterial proteases may also contribute to milk protein degradation. This increased proteolysis during mastitis can damage the mammary tissue [141].
Problems with Current Detection Techniques
Some components of the proteolytic systems in milk may be unknown because of their low concentration and the limit of detection techniques. Detection of these proteolytic systems is limited by the sensitivity of detection techniques. Proteomics sensitivity clearly depends on wide range of factors, especially sample pre-fractionation strategies [27]. The lack of a finding cannot be confused with the fact that a particular component is absent. Transcriptomics techniques are more reliable than proteomics and less susceptible to detection level limitations. However, the presence of the transcript cannot provide a complete picture of the milk system, as some milk proteases (e.g., plasmin) may be incorporated from blood rather than the MEC. Transcriptomics can only tell us how much mRNA message is produced, which is poorly correlated with the level of protein in a system [142] and cannot determine the percentage in the zymogen versus the active state. Moreover, transcriptomics studies are problematic when trying to understand milk proteases because it is difficult to isolate MEC-only mRNA. The cellular fraction of milk contains not only sloughed MEC but lymphocytes, neutrophils and macrophages. Although studies examining the transcriptome of milk overall (e.g., [20]) make sense using this procedure, they do not allow us to parse whether proteases derive from MECs or other cells. An innovative approach to isolating active MEC mRNA used just the cytoplasmic crescent from milk fat globules [14]. However, the fat globules were contaminated with other somatic cells in the fat layer. A method with improved elimination of other somatic cells could allow this method to work for protease investigations. Likewise, the microlocation of the protease can be very important (i.e., the position of each proteolytic component within the milk: protein-protein proximity, cellularly bound, etc.) to the activity—and transcriptomics cannot provide this information. Therefore, more protein-protein interaction studies are needed.
Conclusion
Clearly, milk contains a wide variety of proteases, and their relevant inhibitors and activators, allowing for a tightly controlled level of digestion within the mammary gland. And, clearly, these enzymes continue to be active within the infant’s gastrointestinal tract. The balance of proteolytic action is likely important to allow some proteins to stay intact for bioactive functions and to prime the infant’s own protease production. It is also necessary to aid immature gut absorption of high levels of amino acids and prevent accumulation of proteins in the distal colon that leads to growth of putrefactive bacteria.
More precise tools are required to fully understand the activities of these proteolytic enzyme systems. Transcriptomics can show the complete expression profile of proteolytic system components that are produced by MEC and milk somatic cells. Proteomics can allow determination of all the proteolytic system components present in the milk, even those that have not been expressed within the mammary gland itself, however this is limited by level of detection issues. Peptidomics and bioinformatic prediction can provide insight into which proteases are active [27]. Chromogenic enzyme-substrate analysis can also help to determine protease activity levels. Advanced studies of intra-mammary gland position of the proteolytic components and protein-protein interactions are needed to better understand this complex system.
Though a great deal of work has explored the proteases in milk, the majority of that work is decades old and leaves many questions unanswered. The modern tools of biology can now be brought to bear on these questions. A revitalization of this research with transcriptomics, proteomics and protein-protein interaction studies will reveal new insights into the biology and control of this system. With new information, we can begin to understand better the biological role of these complex proteolytic systems in milk.
Abbreviations
- MEC:
-
Mammary epithelial cell
References
Oftedal OT. The mammary gland and its origin during synapsid evolution. J Mammary Gland Biol Neoplasia. 2002;7(3):225–52.
Lefèvre CM, Sharp JA, Nicholas KR. Evolution of lactation: ancient origin and extreme adaptations of the lactation system. Annu Rev Genomics Hum Genet. 2010;11(1):219–38. doi:10.1146/annurev-genom-082509-141806.
Kelly AL, O’Flaherty F, Fox PF. Indigenous proteolytic enzymes in milk: a brief overview of the present state of knowledge. Int Dairy J. 2006;16(6):563–72. doi:10.1016/j.idairyj.2005.10.019.
Ismail B, Nielsen S. Invited review: plasmin protease in milk: current knowledge and relevance to dairy industry. J Dairy Sci. 2010;93(11):4999–5009.
Barbano D, Rasmussen R, Lynch J. Influence of milk somatic cell count and milk age on cheese yield. J Dairy Sci. 1991;74(2):369–88.
Datta N, Deeth H. Age gelation of UHT milk—a review. Food Bioprod Process. 2001;79(4):197–210.
Farkye N, Landkammer CF. Milk plasmin activity influence on cheddar cheese quality during ripening. J Food Sci. 1992;57(3):622–39.
Holton TA, Vijaykumar V, Dallas DC, et al. Following the digestion of milk proteins from mother to baby. J Proteome Res. 2014;13(12):5777–83.
Dallas DC, Guerrero A, Khaldi N, et al. A peptidomic analysis of human milk digestion in the infant stomach reveals protein-specific degradation patterns. J Nutr. 2014;144(6):815–20. doi:10.3945/jn.113.185793.
Dallas DC, Underwood MA, Zivkovic AM, German JB. Digestion of protein in premature and term infants. J Nutr Disord Ther. 2012;2(3):112–21.
Palmer DJ, Kelly VC, Smit AM, Kuy S, Knight CG, Cooper GJ. Human colostrum: identification of minor proteins in the aqueous phase by proteomics. Proteomics. 2006;6(7):2208–16.
Borulf S, Lindberg T, Mansson M. Immunoreactive anionic trypsin and anionic elastase in human milk. Acta Paediatr. 1987;76(1):11–5.
Molinari CE, Casadio YS, Hartmann BT, et al. Proteome mapping of human skim milk proteins in term and preterm milk. J Proteome Res. 2012;11(3):1696–714.
Lemay DG, Ballard OA, Hughes MA, Morrow AL, Horseman ND, Nommsen-Rivers LA. RNA sequencing of the human milk fat layer transcriptome reveals distinct gene expression profiles at three stages of lactation. PLoS One. 2013;8(7):e67531.
Korycha-Dahl M, Dumas BR, Chene N, Martal J. Plasmin activity in milk. J Dairy Sci. 1983;66(4):704–11.
Fox P. Proteinases in dairy technology. Neth Milk Dairy J. 1981;35:233.
D’Alessandro A, Zolla L, Scaloni A. The bovine milk proteome: cherishing, nourishing and fostering molecular complexity. An interactomics and functional overview. Mol BioSyst. 2011;7(3):579–97.
Magboul AA, Larsen LB, McSweeney PL, Kelly AL. Cysteine protease activity in bovine milk. Int Dairy J. 2001;11(11):865–72.
Heegaard CW, Rasmussen LK, Andreasen PA. The plasminogen activation system in bovine milk: differential localization of tissue-type plasminogen activator and urokinase in milk fractions is caused by binding to casein and urokinase receptor. Biochim Biophys Acta. 1994;1222(1):45–55. doi:10.1016/0167-4889(94)90023-X.
Wickramasinghe S, Rincon G, Islas-Trejo A, Medrano JF. Transcriptional profiling of bovine milk using RNA sequencing. BMC Genomics. 2012;13(1):45–58. doi:10.1186/1471-2164-13-45.
Heegaard CW, Larsen LB, Rasmussen LK, Højberg KE, Petersen TE, Andreasen PA. Plasminogen activation system in human milk. J Pediatr Gastroenterol Nutr. 1997;25(2):159–66.
Lindberg T, Ohlsson K, Westrom B. Protease inhibitors and their relation to protease activity in human milk. Pediatr Res. 1982;16(6):479–83.
Lindberg T. Protease inhibitors in human-milk. Pediatr Res. 1979;13(9):969–72.
McGilligan KM, Thomas DW, Eckhert CD. Alpha-1-antitrypsin concentration in human milk. Pediatr Res. 1987;22(3):268–70.
Dallas D, Guerrero A, Khaldi N, et al. Extensive in vivo human milk peptidomics reveals specific proteolysis yielding protective antimicrobial peptides. J Proteome Res. 2013;12(5):2295–304. doi:10.1021/pr400212z.
Dallas DC, Weinborn V, de Moura Bell JM, et al. Comprehensive peptidomic and glycomic evaluation reveals that sweet whey permeate from colostrum is a source of milk protein-derived peptides and oligosaccharides. Food Res Int. 2014;63(B):203–9. doi:10.1016/j.foodres.2014.03.021.
Guerrero A, Dallas DC, Contreras S, et al. Peptidomic analysis of healthy and subclinically mastitic bovine milk. Int Dairy J. 2014. doi:10.1016/j.idairyj.2014.09.006.
Guerrero A, Dallas DC, Contreras S, et al. Mechanistic peptidomics: factors that dictate the specificity on the formation of endogenous peptides in human milk. Mol Cell Proteomics. 2014;13(12):3343–51. doi:10.1074/mcp.M113.036194.
Dallas DC, Smink CJ, Robinson RC, et al. Endogenous human milk peptide release is greater following preterm birth than term birth. J Nutr. 2015;145(3):425–33.
Khaldi N, Vijayakumar V, Dallas DC, et al. Predicting the important enzyme players in human breast milk digestion. J Agric Food Chem. 2014;62(29):7225–32. doi:10.1021/jf405601e.
Dallas D, Guerrero A, Parker E, et al. Peptidomic profile of milk of Holstein cows at peak lactation. J Agric Food Chem. 2013;62(1):58–65.
Christensen B, Schack L, Kläning E, Sørensen ES. Osteopontin is cleaved at multiple sites close to its integrin-binding motifs in milk and is a novel substrate for plasmin and cathepsin D. J Biol Chem. 2010;285(11):7929–37.
Ferranti P, Traisci MV, Picariello G, et al. Casein proteolysis in human milk: tracing the pattern of casein breakdown and the formation of potential bioactive peptides. J Dairy Res. 2004;71(1):74–87. doi:10.1017/s0022029903006599.
Grufferty MB, Fox PF. Milk alkaline proteinase. J Dairy Res. 1988;55(04):609–30.
Bastian ED, Brown RJ. Plasmin in milk and dairy products: an update. Int Dairy J. 1996;6(5):435–57.
Okamoto U, Horie N, Nagamatsu Y, Yamamoto J. Plasminogen-activator in human early milk: its partial purification and characterization. Thromb Haemost-Stuttgart. 1981;45(2):121–6.
Precetti AS, Oria MP, Nielsen SS. Presence in bovine milk of two protease inhibitors of the plasmin system. J Dairy Sci. 1997;80(8):1490–6. doi:10.3168/jds.S0022-0302(97)76077-6.
Uniprot. P34955- A1AT_BOVIN. 2014.
D’Alessandro A, Scaloni A, Zolla L. Human milk proteins: an interactomics and updated functional overview. J Proteome Res. 2010;9(7):3339–73.
Uniprot. Q9N2I2- IPSP_BOVIN. 2014.
Christensen S, Wiegers T, Hermansen J, Sottrup-Jensen L. Plasma-derived protease inhibitors in bovine milk. Int Dairy J. 1995;5(5):439–49. doi:10.1016/0958-6946(95)00020-4.
Uniprot. Q9TTE1- SPA31_BOVIN. Uniprot, 2014.
Benslimane S, Dognin-Bergeret MJ, Berdague J-L, Gaudemer Y. Variation with season and lactation of plasmin and plasminogen concentrations in Montbeliard cows’ milk. J Dairy Res. 1990;57(04):423–35.
Politis I. Plasminogen activator system: Implications for mammary cell growth and involution. J Dairy Sci. 1996;79(6):1097–107. doi:10.3168/jds.S0022-0302(96)76463-9.
Eigel W, Hofmann C, Chibber B, Tomich J, Keenan T, Mertz E. Plasmin-mediated proteolysis of casein in bovine milk. Proc Natl Acad Sci. 1979;76(5):2244–8.
Politis I, White JH, Zavizion B, Goldberg JJ, Guo MR, Kindstedt P. Effect of individual caseins on plasminogen activation by bovine urokinase-type and tissue-type plasminogen activators. J Dairy Sci. 1995;78(3):484–90. doi:10.3168/jds.S0022-0302(95)76658-9.
Markus G, Hitt S, Harvey S, Tritsch G. Casein, a powerful enhancer of the rate of plasminogen activation. Fibrinolysis. 1993;7(4):229–36.
White JH, Zavizion B, O’Hare K, et al. Distribution of plasminogen activator in different fractions of bovine milk. J Dairy Res. 1995;62:115.
Politis I, Voudouri A, Bizelis I, Zervas G. The effect of various vitamin E derivatives on the urokinase-plasminogen activator system of ovine macrophages and neutrophils. Br J Nutr. 2003;89(02):259–65.
Politis I, Zavizion B, Cheli F, Baldi A. Expression of urokinase plasminogen activator receptor in resting and activated bovine neutrophils. J Dairy Res. 2002;69(02):195–204.
Vĕtvicka V, Vagner J, Baudys M, Tang J, Foundling S, Fusek M. Human breast milk contains procathepsin D--detection by specific antibodies. Biochem Mol Biol Int. 1993;30(5):921–8.
Bergmann M, Fruton JS. Regarding the general nature of catheptic enzymes. Science. 1936;84(2169):89–90.
Lkhider M, Castino R, Bouguyon E, Isidoro C, Ollivier-Bousquet M. Cathepsin D released by lactating rat mammary epithelial cells is involved in prolactin cleavage under physiological conditions. J Cell Sci. 2004;117(21):5155–64. doi:10.1242/jcs.01396.
Benes P, Vetvicka V, Fusek M. Cathepsin D—many functions of one aspartic protease. Crit Rev Oncol Hematol. 2008;68(1):12–28. doi:10.1016/j.critrevonc.2008.02.008.
Kaminogawa S, Yamauchi K. Acid protease of bovine milk. Agric Biol Chem. 1972;36(13):2351–6.
Larsen LB, Petersen TE. Identification of five molecular forms of cathepsin D in bovine milk. In: Takahashi K, editor. Aspartic proteinases. Berlin: Springer; 1995. p. 279–83.
Larsen LB, Boisen A, Petersen TE. Procathepsin D cannot autoactivate to cathepsin D at acid pH. FEBS Lett. 1993;319(1):54–8.
Wittlin S, Rösel J, Hofmann F, Stover DR. Mechanisms and kinetics of procathepsin D activation. Eur J Biochem. 1999;265(1):384–93.
O’Driscoll B, Rattray F, McSweeney P, Kelly A. Protease activities in raw milk determined using a synthetic heptapeptide substrate. J Food Sci. 1999;64(4):606–11.
Capony F, Rougeot C, Montcourrier P, Cavailles V, Salazar G, Rochefort H. Increased secretion, altered processing, and glycosylation of pro-cathepsin D in human mammary cancer cells. Cancer Res. 1989;49(14):3904–9.
Hasilik A. Theearly andlate processing of lysosomal enzymes: proteolysis and compartmentation. Experientia. 1992;48(2):130–51.
Hurley MJ, Larsen LB, Kelly AL, McSweeney PLH. The milk acid proteinase cathepsin D: a review. Int Dairy J. 2000;10:673–81.
Considine T, Healy A, Kelly A, McSweeney P. Hydrolysis of bovine caseins by cathepsin B, a cysteine proteinase indigenous to milk. Int Dairy J. 2004;14(2):117–24.
Kirschke H, Barrett AJ, Rawlings ND. Lysosomal cysteine proteases. Oxford: Oxford University Press; 1998.
Prin-Mathieu C, Le Roux Y, Faure G, Laurent F, Béné M, Moussaoui F. Enzymatic activities of bovine peripheral blood leukocytes and milk polymorphonuclear neutrophils during intramammary inflammation caused by lipopolysaccharide. Clin Diagn Lab Immunol. 2002;9(4):812–7.
Lewis UJ, Williams DE, Brink NG. Pancreatic elastase: purification, properties, and function. J Biol Chem. 1956;222(2):705–20.
Naughton M, Sanger F. Purification and specificity of pancreatic elastase. Biochem J. 1961;78(1):156–63.
Jochum M, Bittner A. Inter-alpha-trypsin inhibitor of human serum: an inhibitor of polymorphonuclear granulocyte elastase. Hoppe Seylers Z Physiol Chem. 1983;364(12):1709–15.
Travis J, Fritz H. Potential problems in designing elastase inhibitors for therapy. Am Rev Respir Dis. 1991;143(6):1412–5. doi:10.1164/ajrccm/143.6.1412.
Li N, Richoux R, Boutinaud M, Martin P, Gagnaire V. Role of somatic cells on dairy processes and products: a review. Dairy Sci Technol. 2014;94(6):517–38. doi:10.1007/s13594-014-0176-3.
Monti J, Mermoud A-F, Jolles P. Trypsin in human milk. Experientia. 1986;42(1):39–41.
Engel A, Alexander B, Pechet L. Activation of trypsinogen and plasminogen by thrombin preparations. Biochemistry. 1966;5(5):1543–51.
Yamashina I. The action of enterokinase on trypsinogen. Biochim Biophys Acta. 1956;20:433–4.
Hadorn B, Steiner N, Sumida C, Peters T. Intestinal enterokinase: mechanisms of its secretion into the lumen of the small intestine. Lancet. 1971;297(7691):165–6.
Christensen S, Sottrup-Jensen L. Characterization of two serpins from bovine plasma and milk. Biochem J. 1994;303:383–90.
Gettins PGW. Serpin structure, mechanism, and function. Chem Rev. 2002;102(12):4751–804.
Kalsheker N. Alpha 1-antitrypsin: structure, function and molecular biology of the gene. Biosci Rep. 1989;9(2):129–38.
Heyndrickx G. Further investigations on the enzymes in human milk. Pediatrics. 1963;31(6):1019–23.
Wilcox PE. Chymotrypsinogens—chymotrypsins. In: Gertrude E, Perlmann LL, editors. Methods Enzymol. Academic; 1970. p. 64–108.
Uruena C, Telleria JJ, Blanco-Quiros A, Arranz E, Gomez-Carrasco JA. Alpha-1 antichymotrypsin levels are actively increased in normal colostrum. J Pediatr Gastroenterol Nutr. 1998;26(4):376–9.
Beatty K, Bieth J, Travis J. Kinetics of association of serine proteinases with native and oxidized alpha-1-proteinase inhibitor and alpha-1-antichymotrypsin. J Biol Chem. 1980;255(9):3931–4.
Schapira M, Scott CF, Colman RW. Contribution of plasma protease inhibitors to the inactivation of kallikrein in plasma. J Clin Invest. 1982;69(2):462–8.
Zhao L, Morser J, Bajzar L, Nesheim M, Nagashima M. Identification and characterization of two thrombin-activatable fibrinolysis inhibitor isoforms. Thromb Haemost-Stuttgart. 1998;80:949–55.
Cheung P, Sawicki G, Gross S, Van Aerde J, Radomski M. Differential expression of matrix metalloproteinases and the tissue inhibitor in human milk. Proc West Pharmacol Soc: West Pharmacol Soc 2001;97–8.
Lubetzky R, Mandel D, Mimouni FB, Herman L, Reich R, Reif S. MMP-2 and MMP-9 and their tissue inhibitor in preterm human milk. J Pediatr Gastroenterol Nutr. 2010;51(2):210–2.
Picariello G, Ferranti P, Mamone G, et al. Gel-free shotgun proteomic analysis of human milk. J Chromatogr A. 2012;1227:219–33. doi:10.1016/j.chroma.2012.01.014.
Folley SJ. Biochemical aspects of mammary gland function. Biol Rev. 1949;24(3):316–54. doi:10.1111/j.1469-185X.1949.tb00579.x.
Burgoyne RD, Duncan JS. Secretion of milk proteins. J Mammary Gland Biol Neoplasia. 1998;3(3):275–86. doi:10.1023/a:1018763427108.
Stelwagen K. Mammary gland, milk biosynthesis and secretion | milk protein. In: Fuquay JW, editor. Encyclopedia of Dairy Sciences (Second Edition). San Diego: Academic; 2011. p. 359–66.
Mostov KE, Kraehenbuhl JP, Blobel G. Receptor-mediated transcellular transport of immunoglobulin: synthesis of secretory component as multiple and larger transmembrane forms. Proc Natl Acad Sci. 1980;77(12):7257–61.
Seddiki T, Delpal S, Ollivier-Bousquet M. Endocytosis and intracellular transport of transferrin across the lactating rabbit mammary epithelial cell. J Histochem Cytochem. 1992;40(10):1501–10.
Hassiotou F, Geddes DT, Hartmann PE. Cells in human milk: state of the science. J Hum Lact. 2013;29(2):171–82. doi:10.1177/0890334413477242.
Manjarin R, Bequette BJ, Wu G, Trottier NL. Linking our understanding of mammary gland metabolism to amino acid nutrition. Amino Acids. 2014;46(11):2447–62. doi:10.1007/s00726-014-1818-8.
Larson BL. Biosynthesis and secretion of milk proteins - review. J Dairy Res. 1979;46(2):161–74.
Lemay DG, Hovey RC, Hartono SR, et al. Sequencing the transcriptome of milk production: milk trumps mammary tissue. BMC Genomics. 2013;14(872):1–17. doi:10.1186/1471-2164-14-872.
Ollivier-Bousquet M. Transferrin and prolactin transcytosis in the lactating mammary epithelial cell. J Mammary Gland Biol Neoplasia. 1998;3(3):303–13.
Field CJ. The immunological components of human milk and their effect on immune development in infants. J Nutr. 2005;135(1):1–4.
Silanikove N, Merin U, Leitner G. Physiological role of indigenous milk enzymes: an overview of an evolving picture. Int Dairy J. 2006;16(6):533–45.
Somers JS, O’Brien B, Meaney WJ, Kelly AL. Heterogeneity of proteolytic enzyme activities in milk samples of different somatic cell count. J Dairy Res. 2003;70:45–50.
Owen CA, Campbell EJ. The cell biology of leukocyte-mediated proteolysis. J Leukoc Biol. 1999;65(2):137–50.
Heegaard CW, Christensen T, Rasmussen MD, et al. Plasminogen activators in bovine milk during mastitis, an inflammatory disease. Fibrinolysis. 1994;8(1):22–30.
Politis I, Ng Kwai Hang K, Giroux R. Environmental factors affecting plasmin activity in milk. J Dairy Sci. 1989;72(7):1713–8.
Mason S. Some aspects of gastric function in the newborn. Arch Dis Child. 1962;37(194):387–91.
Neu J. Gastrointestinal maturation and implications for infant feeding. Early Hum Dev. 2007;83(12):767–75.
Britton J, Koldovsky O. Development of luminal protein digestion: implications for biologically active dietary polypeptides. J Pediatr Gastroenterol Nutr. 1989;9(2):144–62.
Hadorn B. Development aspects of intraluminal protein digestion. In: Lebenthal E, editor. Textbook of gastroenterology and nutrition in infancy. New York: Raven; 1981. p. 365–73.
Antonowicz I, Lebenthal E. Developmental pattern of small intestinal enterokinase and disaccharidase activities in the human fetus. Gastroenterology. 1977;72(6):1299.
Lebenthal E, Lee P. Development of functional response in human exocrine pancreas. Pediatrics. 1980;66(4):556–60.
Chowanadisai W, Lonnerdal B. Alpha-1-antitrypsin and antichymotrypsin in human milk: origin, concentrations, and stability. Am J Clin Nutr. 2002;76(4):828–33.
Keller J, Layer P. Human pancreatic exocrine response to nutrients in health and disease. Gut. 2005;54 suppl 6:1–28. doi:10.1136/gut.2005.065946.
Kinouchi T, Koyama S, Harada E, Yajima T. Large molecule protein feeding during the suckling period is required for the development of pancreatic digestive functions in rats. Am J Physiol Regul Integr Comp Physiol. 2012;303(12):R1268–76. doi:10.1152/ajpregu.00064.2012.
Davila A-M, Blachier F, Gotteland M, et al. Intestinal luminal nitrogen metabolism: role of the gut microbiota and consequences for the host. Pharmacol Res. 2013;68(1):95–107. doi:10.1016/j.phrs.2012.11.005.
Rist VTS, Weiss E, Eklund M, Mosenthin R. Impact of dietary protein on microbiota composition and activity in the gastrointestinal tract of piglets in relation to gut health: a review. Animal. 2013;7(07):1067–78. doi:10.1017/S1751731113000062.
Macfarlane S, Macfarlane GT. Proteolysis and amino acid fermentation. In: Gibson GR, Macfarlane GT, editors. Human colonic bacteria--role in nutrition, physiology and pathology. CRC Press Inc.; 1995. p. 75–100.
Macfarlane GT, Macfarlane S. Human colonic microbiota: ecology, physiology and metabolic potential of intestinal bacteria. Scand J Gastroenterol Suppl. 1997;32(222):3–9.
Hughes R, Kurth MJ, McGilligan V, McGlynn H, Rowland I. Effect of colonic bacterial metabolites on Caco-2 cell paracellular permeability in vitro. Nutr Cancer. 2008;60(2):259–66. doi:10.1080/01635580701649644.
McCall IC, Betanzos A, Weber DA, Nava P, Miller GW, Parkos CA. Effects of phenol on barrier function of a human intestinal epithelial cell line correlate with altered tight junction protein localization. Toxicol Appl Pharmacol. 2009;241(1):61–70. doi:10.1016/j.taap.2009.08.002.
Toden S, Bird AR, Topping DL, Conlon MA. Differential effects of dietary whey, casein and soya on colonic DNA damage and large bowel SCFA in rats fed diets low and high in resistant starch. Br J Nutr. 2007;97(3):535–43. doi:10.1017/s0007114507336817.
Windey K, De Preter V, Verbeke K. Relevance of protein fermentation to gut health. Mol Nutr Food Res. 2012;56(1):184–96. doi:10.1002/mnfr.201100542.
Hamer HM, De Preter V, Windey K, Verbeke K. Functional analysis of colonic bacterial metabolism: relevant to health? Am J Physiol Gastrointestinal Liver Physiol. 2012;302(1):G1–9.
Attene-Ramos MS, Wagner ED, Plewa MJ, Gaskins HR. Evidence that hydrogen sulfide is a genotoxic agent. Mol Cancer Res. 2006;4(1):9–14. doi:10.1158/1541-7786.mcr-05-0126.
Pedersen G, Brynskov J, Saermark T. Phenol toxicity and conjugation in human colonic epithelial cells. Scand J Gastroenterol. 2002;37(1):74–9.
Khalkhali-Ellis Z, Goossens W, Margaryan NV, Hendrix MJC. Cleavage of histone 3 by cathepsin D in the involuting mammary gland. PLoS One. 2014;9(7):1–9.
Hurley WL, Theil PK. Perspectives on immunoglobulins in colostrum and milk. Nutrients. 2011;3(4):442–74.
Armaforte E, Curran E, Huppertz T, et al. Proteins and proteolysis in pre-term and term human milk and possible implications for infant formulae. Int Dairy J. 2010;20(10):715–23.
Greenberg R, Groves ML, Dower HJ. Human beta-casein - amino acid sequence and identification of phosphorylation sites. J Biol Chem. 1984;259(8):5132–8.
Nguyen D-AD, Neville MC. Tight junction regulation in the mammary gland. J Mammary Gland Biol Neoplasia. 1998;3(3):233–46.
Anderson G. The effect of prematurity on milk composition and its physiological basis. Fed Proc. 1984;43(9):2438–42.
Borgström B, Lindquist B, Lundh G. Enzyme concentration and absorption of protein and glucose in duodenum of premature infants. Am J Dis Child. 1960;99(3):338–43.
Engberg S, Mansson M, Andersson Y, Jakobsson I, Lindberg T. Trypsin and elastase activity in duodenal juice from preterm infants before and after a meal of human milk. Prenat Neonatal Med. 1999;4(6):466–71.
Arslanoglu S, Moro GE, Ziegler EE. Optimization of human milk fortification for preterm infants: new concepts and recommendations. J Perinat Med. 2010;38:233–8.
Beck S, Wojdyla D, Say L, et al. The worldwide incidence of preterm birth: a systematic review of maternal mortality and morbidity. Bull World Health Organ. 2010;88(1):31–8.
Mansor R, Mullen W, Albalat A, et al. A peptidomic approach to biomarker discovery for bovine mastitis. J Proteomics. 2013;85:89–98.
Saeman AI, Verdi R, Galton D, Barbano D. Effect of mastitis on proteolytic activity in bovine milk. J Dairy Sci. 1988;71(2):505–12.
Kirschke H, Barrett A, Glaumann H, Ballard F. Lysosomes: their role in protein breakdown. London: Academic; 1987.
Larsen LB, Rasmussen MD, Bjerring M, Nielsen JH. Proteases and protein degradation in milk from cows infected with Streptococcus uberis. Int Dairy J. 2004;14(10):899–907.
Kaartinen L, Sandholm M. Regulation of plasmin activation in mastitic milk: correlation with inflammatory markers and growth of Streptococcus agalactiae. J Vet Med B Infect Dis Vet Public Health. 1987;34(1–10):42–50.
Fang W, Sandholm M. Inhibition of the proteinase activity in mastitic milk. J Dairy Res. 1995;62(01):61–8.
Hogan J, Smith KL. Coliform mastitis. Vet Res. 2003;34(5):507–19.
Fleminger G, Heftsi R, Uzi M, Nissim S, Gabriel L. Chemical and structural characterization of bacterially-derived casein peptides that impair milk clotting. Int Dairy J. 2011;21(12):914–20.
Le Roux Y, Laurent F, Moussaoui F. Polymorphonuclear proteolytic activity and milk composition change. Vet Res. 2003;34(5):629–45.
Ning K, Fermin D, Nesvizhskii AI. Comparative analysis of different label-free mass spectrometry based protein abundance estimates and their correlation with RNA-Seq gene expression data. J Proteome Res. 2012;11(4):2261–71.
Acknowledgments
The authors thank Cora J. Dillard for editing this manuscript. D.C.D., N.M.M. and J.G. wrote the paper, and D.C.D. had primary responsibility for the final content. All authors read and approved the final manuscript. This project was funded in part by the K99/R00 Pathway to Independence Career Award, Eunice Kennedy Shriver Institute of Child Health & Development of the National Institutes of Health (K99HD079561) (D.C. D.).
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dallas, D.C., Murray, N.M. & Gan, J. Proteolytic Systems in Milk: Perspectives on the Evolutionary Function within the Mammary Gland and the Infant. J Mammary Gland Biol Neoplasia 20, 133–147 (2015). https://doi.org/10.1007/s10911-015-9334-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10911-015-9334-3