Abstract
Purpose Our objective was to develop a clinical prediction model to identify workers with sustainable employment following an episode of work-related low back pain (LBP). Methods We used data from a cohort study of injured workers with incident LBP claims in the USA to predict employment patterns 1 and 6 months following a workers’ compensation claim. We developed three sequential models to determine the contribution of three domains of variables: (1) basic demographic/clinical variables; (2) health-related variables; and (3) work-related factors. Multivariable logistic regression was used to develop the predictive models. We constructed receiver operator curves and used the c-index to measure predictive accuracy. Results Seventy-nine percent and 77 % of workers had sustainable employment at 1 and 6 months, respectively. Sustainable employment at 1 month was predicted by initial back pain intensity, mental health-related quality of life, claim litigation and employer type (c-index = 0.77). At 6 months, sustainable employment was predicted by physical and mental health-related quality of life, claim litigation and employer type (c-index = 0.77). Adding health-related and work-related variables to models improved predictive accuracy by 8.5 and 10 % at 1 and 6 months respectively. Conclusion We developed clinically-relevant models to predict sustainable employment in injured workers who made a workers’ compensation claim for LBP. Inquiring about back pain intensity, physical and mental health-related quality of life, claim litigation and employer type may be beneficial in developing programs of care. Our models need to be validated in other populations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Low back pain (LBP) is the highest contributor of global disability worldwide [1]. In the UK in 2009, the direct health care costs of chronic back pain exceeded £1.5 billion [2]. Occupational back pain is associated with significant direct and indirect costs to employers, insurers, and injured workers [3]. In 2013 in the United States, the incidence of back pain injuries among full-time workers was 20 per 10,000 [4]. Additionally, back problems were ranked seventh for annual average cost of productivity loss (absenteeism and presenteeism) among employed workers with health reimbursement accounts [5]. A median of seven days away from work to recuperate from a back injury was reported in the United States in 2013 [4].
Previous studies suggest that back pain is episodic and is associated with recurrent work absenteeism [3, 6, 7]. Additionally, individuals with prevalent back pain are more likely to report future back injuries, work absences, and more comorbidities compared to workers with incident LBP [8]. Although we have gained knowledge about the outcomes experienced by injured workers with back pain, we still lack the ability to accurately predict who is more likely to regain sustainable employment. Therefore, it is important to develop clinical prediction models to predict outcome following a work-related back injury.
A challenging issue facing clinicians is to predict, shortly after the injury, the probability of returning to sustainable employment. Clinicians often rely on clinical experience and clinically relevant scientific evidence to determine the prognosis of a patient. Very few prediction models clearly identify who is likely to return to work and maintain sustainable employment following an occupational low back injury. Several studies have proposed prediction rules to identify workers at risk of chronic work disability; however, their predictive ability is low, ranging from 12 to 30 % [9–11]. Additionally, many models do not include important prognostic factors for work disability [12]. A literature review of predictive models and rules used to determine persisting functional restrictions in individuals with sub-acute LBP, reported the predictive ability of existing models was moderate at best (explained variance ranged from 28 % to 51 %) [13]. The objective of our study was to develop a clinical prediction model to identify individuals with sustainable patterns of employment 1 and 6 months after a low back work injury.
Methods
Design
We used data from the Arizona State University Healthy Back Study (ASU study) to develop clinical prediction models. The ASU study was a prospective inception cohort of workers who filed an incident claim for work-related back pain between January 1, 1999 and June 30, 2002 [3]. The individuals worked for one of five different employers across 37 American states.
Study Population
To be included in the ASU study, workers had to meet to following criteria: (1) back pain reported to the employer; (2) back injury occurred at work; and (3) diagnosis of LBP based on ICD-9 codes included in the following categories: 721 (spondylosis and allied disorders), 722 (intervertebral disc disorders), 724 (other and unspecified disorders of back), and 847 (sprains and strains of other and unspecified parts of the back) reported by the primary healthcare provider to the insurer. Workers with fractures, denied workers’ compensation claim, subsequent claim during the study period, or litigation related to the back injury that was initiated prior to study enrollment were excluded [3].
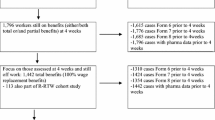
The intent of our clinical prediction models were to predict sustainable employment using data collected shortly after the onset of a workers’ compensation claim for LBP. Therefore, we restricted our sample to participants who completed the baseline questionnaire of the ASU study within 48 days post-claim initiation (early completers). Late completers were defined as those who completed the baseline questionnaire more than 48 days following the initiation of the claim. Furthermore, only participants who completed the second follow-up questionnaire between 130 and 230 days post-claim initiation were included in the final cohort (Fig. 1). These criteria were necessary to ensure the baseline data clearly preceded the collection of the outcome of interest and also optimize statistical power by capturing 90 % of the sample.
Outcome
The outcome was post-injury sustainable employment. Workers with sustainable employment had no work absence or an initial work absence followed by no future absences post-injury. Workers without sustainable employment were those who reported multiple episodes of work absences and those who had not returned to work. Sustainable employment at 1-month and 6-month post-claim initiation was determined by asking study participants the following questions: [1] “Did you have to take time off work because of your back injury?” [2] “Have you returned to work?” [3] “Between the time you returned to work and now (time of interview) did you have to take any additional time off work because of your back injury?”
Predictors
Predictive factor selection was based on evidence provided in the scientific literature and clinical judgment [9, 14–17]. These factors were then compared with those available in the ASU dataset. The final selected predictors included:
Demographics Age and sex.
Back and leg pain intensity Numeric Rating Scales for back pain and leg pain intensity (NRS-101), were used to rate pain from “0” (not bothersome at all) to “100” (pain is extremely bothersome). This scale is valid and reliable [18].
Type of occupation This was used as a basic clinical predictor since certain work activities may have an impact on recovery from back pain. Based on the ASU study coding, workers were grouped into the classifications of (1) professional/manager, (2) service, and (3) other.
Disability The Roland-Morris Disability Scale (24 item) was used to assess the functional abilities of individuals with LBP. It has high internal consistency, test–retest reliability (within a six-week period), criterion-based, construct and discriminant validity, and responsiveness [19–28].
Health related quality of life The SF-12 (second revision) was used to measure physical and mental health-related quality of life. The questionnaire was administered both at baseline and subsequent follow-up periods. This scale has good test–retest reliability over a two-week period and the SF-12 components are highly correlated with the same components of the SF-36 [29]. The SF-12 also has good internal consistency, validity and responsiveness [30].
Past history of LBP Workers were asked if they had LBP before this injury (yes/no).
Expectation of recovery This was assessed by asking “Do you think that your LBP will get better soon?” Available responses were: (1) “already fully recovered”; (2) “get better soon”; (3) “get better slowly”; (4) “never get better”; or (5) “get worse”.
Receiving care Workers were asked “Have you received care from a health care provider for your back pain (yes/no)?
Claim litigation This was determined by asking “Have you hired an attorney” (yes/no)? Litigation is directly related to the work injury and a result of the worker’s compensation claim.
Job tenure This was calculated by subtracting the hire date from the injury date and reported in years.
Job satisfaction Workers were asked “How satisfied are you with your job as a whole taking everything in consideration?” Responses ranged from very satisfied to very dissatisfied.
Employer Participants were recruited from five separate employers across the USA. To maintain anonymity of the employers, they are referred to as Employer 1 through 5.
Elapsed time to interview This was calculated by subtracting the interview date from the injury date and reported in days. Elapsed time to interview was grouped within the work-related domain due to the varying reporting procedures among employers.
Predictors were grouped into three different domains using a hierarchical approach evolving from a basic clinical assessment to a comprehensive review of factors collected during an in-depth clinical encounter.
Statistical Analysis
Description of Our Study Population
We examined the baseline characteristics of “early completers” (n = 1319) and “late completers” (n = 428) to ensure that they were from the same underlying population of workers with LBP. Differences between early and late responders were measured with Chi square and t-tests. Baseline characteristics of the final cohort and those lost to follow-up were also examined to determine if they differed systematically.
Development of the Clinical Prediction Models
The models were built in three different stages. First, we computed the correlations (Spearman) between predictors to determine whether they were highly correlated. A correlation > 0.7 was deemed too high for regression analysis, in which case the most clinically relevant and easily obtained (to minimize burden) predictor would be added to the model. Next, we used bivariate logistic regression to determine which predictors were associated with the outcome. Predictors associated with the outcome (p < 0.2 on the Wald Chi square test) were considered in the third stage of analysis. In the third stage, we built three sequential logistic regression models to derive our final clinical prediction model. This approach also allowed us to determine the contribution of each domain of variables to the final model. Separate prediction models were built for the 1-month and 6-month follow-up periods using a multi-stage approach.
-
Model 1: Basic clinical predictors (age, sex, previous episodes of back pain, intensity of back pain, intensity of leg pain, and type of occupation).
-
Model 2: Health-related clinical predictors - Model 1 plus a more elaborate set of clinical predictors (functional disability [RMDQ], health related quality of life [SF-12], previous care for the injury, and recovery expectations).
-
Model 3: Work-related predictors - Model 2 plus worker-related and job-related predictors (job tenure, job satisfaction, claim litigation, who one’s employer is, and elapsed time since baseline interview).
In Model 1, predictors associated with sustainable employment (Wald Chi square p < 0.1) were included. Model 2 included all predictors from Model 1 plus more elaborate health-related predictors associated with sustainable employment (Wald Chi square p < 0.1 using backward selection). Model 3 included the predictors from Model 2 plus work-related predictors associated with sustainable employment (Wald Chi square p < 0.1 using backward selection). We assessed the presence of multi-collinearity by computing the variance inflation factor (VIF); values exceeding 10 on the VIF indicated multi-collinearity [31].
Model accuracy The predictive accuracy of the models was measured using a receiver-operating characteristic curve (ROC) and the C-statistic. We interpreted our results following the proposed guideline for interpreting ROC curves: an AUC of ≥0.7 has acceptable discrimination, ≥0.8 is excellent, and ≥0.9 is outstanding [32]. This was performed for all models derived using multivariable logistic regression. All analyses were performed using SAS software (SAS Institute, version 9.1, Carry, NC, USA).
Internal validity of the prediction models We tested the internal validity of the final prediction models using bias corrected and accelerated confidence interval bootstrapping (2000 repetitions). All bootstrapping analyses were performed using Stata 9.2 (StataCorp, College Station, TX, USA).
Results
Cohort Characteristics
Of the 1747 who made a workers’ compensation claim for back pain and completed the baseline survey, 1319 completed it within 48 days of the onset of their claim (early completers) (Fig. 1). Compared to late responders, early responders were less likely to report recovery, but they were more likely to report favorable recovery expectations (Table 1). Early responders, also reported worse back and leg pain, functional limitations and health-related quality of life. A comparison of baseline characteristics between the final cohort (n = 736) and those who were lost to follow-up (n = 583) suggests that those in the final cohort had longer job tenure and were more likely to report previous back pain (Table 2). A further comparison to assess the effects of missing outcome data on baseline characteristics among respondents who completed both follow-up surveys did not identify any relevant differences between the groups.
Patterns of Employment
Data was used only for individuals who answered all return-to-work (RTW) questions at both follow-up periods (n = 461). Seventy-nine percent (365/461) of the study sample interviewed at the first follow-up had a sustainable employment pattern. This decreased to 77 % (354/461) at the second follow-up.
Prediction Models for the Final Cohort
Models from the 1-Month Follow-Up Period
The final clinical prediction model (Model 3) predicting sustainable employment included back pain intensity, mental health-related quality of life (SF-12 mental subscale), claim litigation and type of employer (Table 3). The predictive accuracy increased progressively across the models from a c-index = 0.71 for Model 1 to a c-index = 0.77 for Model 3. All three models had acceptable fit.
Models from the 6-Month Follow-Up Period
The final clinical prediction model (Model 3) for sustainable employment at the 6-month follow-up included physical and mental health-related quality of life (SF-12 physical and mental subscales), claim litigation and type of employer (Table 4). The predictive accuracy increased progressively across the models, from a c-index = 0.70 in Model 1 to a c-index = 0.77 in Model 3 (Table 4). The three models had acceptable fit.
The variance inflation factors tests indicated that no collinearity was present in our models.
Internal Validation
Our models are internally valid. Following bootstrapping, the 95 % confidence intervals for the regression coefficients in the models did not change.
Discussion
To our knowledge, this is the first model available to clinicians to assist with the prediction of sustainable employment for occupational LBP based on a clinically-based conceptual framework. Furthermore, the ability to accurately predict sustainable employment improved with the addition of a few specific health- and work-related factors. Our work supports the concept that LBP prognosis is multifaceted and should include a variety of prognostic factors from several domains [33]. Considering factors such as health-related quality of life, claim litigation and type of employer may help predict an individual’s work status at both acute and sub-acute periods post-injury. According to Hosmer and Lemeshow, our final models had acceptable predictive accuracy (c-index = 0.77) at both follow-ups [32]. Although the predictive accuracy of our models is deemed acceptable, it could be improved. Specifically, future models need to consider psychosocial variables. Previous studies have illustrated the importance of factors such as poor work relations, personality disorders, and irritability/temper [10, 15, 34].
Our clinical prediction model was conceptually developed from the perspective of a clinician who treats patients with back pain. We asked two fundamental questions: “What does a clinician ask when seeing a patient with a recent back injury?” and “What information does the average clinician typically collect to determine the prognosis of a patient with a recent work-related back injury?”. Our focus was to identify subsets of key predictors that would be useful for clinicians to identify whether a patient is likely to have a sustainable employment pattern after his/her injury. We divided the factors considered in our models into three domains: 1) demographic and basic clinical factors; 2) health-related factors; and 3) work-related factors. From a clinical perspective, this approach was important to obtain a comprehensive information base from injured workers.
Our study suggests that measuring specific clinical, health-related and work-related variables (early after the injury) may assist clinicians to predict sustainable employment 1 month following the initiation of a claim for back pain. Back pain intensity is easy to collect and already part of a typical initial clinical encounter. Additional health-related and job-related factors, some of which can be asked using standardized questionnaires and done during history taking, include: mental health-related quality of life (SF-12), claim litigation and type of employer. To predict sustainable employment approximately 6-month post-claim initiation, clinicians should examine physical and mental health-related quality of life, claim litigation and employer type. Of note is the similarity in predictors at both follow-up periods; mental health-related quality of life, litigation and employer type may impact sustainable employment in both the short and long term post-injury. Our findings also provide a valid method to inform injured workers with back pain about their prognosis. This information may be used to help educate, reassure and manage a patient with an occupational back pain injury.
It is difficult to directly compare prediction models because of methodological differences in the predictive analytic methods, varying populations, and few consistently measured prognostic factors. One clinical prediction rule developed in a Quebec population used a similar outcome; however, they used different predictors compared to our study [15]. Variables included in the study by Dionne et al. included: radiating pain, previous back surgery, irritability/temper, sleep problems, and frequent positional changes due to discomfort [15]. Their model, which examined RTW two years after an occupational injury, explained approximately 30 % of the variance. However, the model had high negative predictive values ranging from 74 to 91 %. Another study, conducted in Ontario, identified a different set of predictors than our models [17]. The study by McIntosh et al. used a data-splitting technique to develop and test multivariable models. Multivariable Cox proportional hazards were used to predict duration on compensation benefits. The models included the following variables: (1) work in the construction industry; (2) older age; (3) elapsed time from injury to first treatment; (4) pain referral into the leg; (5) three or more Waddell signs; (6) low back questionnaire score; (7) previous episode of pain; and (8) and intermittent pain. The predictive accuracy in their confirmatory sample was 67.3 %.
The predictive accuracy of our clinical prediction models is similar to previously developed clinical prediction rules. A rule based on a biopsychosocial predictive model for sub-acute and chronic LBP sufferers had a similar predictive accuracy as our models for RTW [34]. The biopsychosocial model correctly classified 80.5 % of those returning to work and consisted of a number of variables from the biopsychosocial spectrum including SF-36 sub-scales, right leg sciatica, the perception of problem severity and guarding on physical exam. A more recently developed rule that examined risk prediction of prolonged sick leave 6 months post-LBP injury contained job satisfaction, fear avoidance beliefs, pain intensity, complaint duration and sex [35]. Despite including factors from a range of domains (clinical, work, psychosocial), the predictive accuracy was moderate (c-index = 0.63) and the explained variance was low. In another prediction rule, for shoulder pain related to sick leave, satisfactory discrimination was achieved (70 %) [36]. Variables associated with a higher risk of work absence 6 months post-initial consult included: prolonged work absence prior to the initial consult, higher shoulder pain intensity, overuse, and co-existing psychological complaints.
Strengths and Limitations
Our study has several strengths. First, the models were based on a large prospective incident cohort of workers who made an insurance claim for work-related back pain. The employees worked for five large national employers, in both the private and public sectors, which encompassed a fairly representative overview of the U.S. employed population. One of the more innovative aspects of this dataset was that it enabled us to measure the sustainability of employment. Another distinct aspect of our work is that it is clinically grounded. The three models used to create the final prediction model were created from a clinician’s perspective. Therefore, the predictors considered in our models are clinically relevant.
Our study has some limitations. First, we could not consider the full range of possible predictors because they were not measured in the ASU study. These included co-morbidities, measures of social support, and the domain of physical job demands. These have all been previously reported as important predictors [9–12, 34]. Other variables including race or ethnicity may also be relevant in a biopsychosocial approach to managing back pain [37]. Second, it is possible that selection bias due to non-participation and attrition may have biased our results. Also, depending on either clinical or theoretical perspective, variables may be grouped under different domains than what was done by the current authors. This may alter the makeup of the final models presented. Given this is preliminary work, others may feel it necessary to test these models in other working populations while also regrouping the variables. Furthermore, clinician judgement required in choosing appropriate ICD-9 codes may lead to exclusion of some cases. Finally, advances in occupational injury management since the data sampling for this study are likely. This may ultimately impact the outcome of the final models if tested in other populations.
Although our study had limitations, our final models can adequately predict who is likely to return to sustainable employment following a back injury. Elapsed time between the injury and the initial interview may have impacted the predictive ability of the models. It is possible that some variables may have become less predictive as more time elapsed between the injury and the interview.
Our work suggests that employers could have important implications for recovery. The results from this study may have limited generalizability given the job sectors represented and that only one employer was significant in the final model at both follow-ups. Although the source population included workers from 37 American states and various industries, only five employers were used to derive our sample. Even so, the results alert us to the potential that there may be an employer effect on recovery patterns. This may be related to specific employer support and policies for managing injured workers. Other work with this cohort has identified superior employment outcomes among employers with more proactive RTW policies [38].
Furthermore, it is important that researchers develop predictions rules based on the principle of pragmatic application - these rules are ultimately useless if the clinician will not employ them in practice. To be adopted by clinicians, clinical prediction rules must be simple to use and of demonstrated additional benefit to patient outcomes.
Future Research
The first level of evidence has been met, with the development and initial validity testing of the models. Next steps include testing these models in another distinct population of workers and performing an impact analysis. Until then, these models should not be used to direct patient management. Also, we feel the predictive ability or our models could be improved if additional factors are considered. Future models could build on our conceptual framework but further expand the multidimensional domains by including variables examining co-morbidities, measures of social support, and physical job demands.
Conclusion
Our analysis suggests that using information gathered during the initial clinical encounter may assist health care practitioners to better predict an injured worker’s post-back injury employment pattern. We created a promising clinical prediction model to predict sustainable employment following a work-related back injury. Our models suggest that clinicians might gain insight about sustainable employment approximately 1 month after claim-initiation by measuring back pain intensity, mental health-related quality of life (SF-12), claim litigation and type of employer. Similarly, examining physical and mental health-related quality of life (SF-12), claim litigation, and type of employer are adequate for predicting those with a sustainable employment pattern approximately 6 months post-injury.
References
Hoy DG, Smith E, Cross M, Sanchez-Riera L, Buchbinder R, Blyth FM, et al. The global burden of musculoskeletal conditions for 2010: an overview of methods. Ann Rheum Dis. 2014;73(6):982–9.
Hong J, Reed C, Novick D, Happich M. Costs associated with treatment of chronic low back pain: an analysis of the UK General Practice Research Database. Spine. 2013;38(1):75–82.
Côté P, Baldwin ML, Johnson WG, Frank JW, Butler RJ. Patterns of sick-leave and health outcomes in injured workers with back pain. Eur Spine J. 2008;17(4):484–93.
Bureau of Labor Statistics US Depatment of Labour. Nonfatal occupational injuries and illnesses requiring days away from work, 2013. Table 5. Number, incidence rate, and median days away from work for nonfatal occupational injuries and illnesses involving days away from work by injury or illness characteristics and ownership, 2013 2013 [cited 2014 December 16, 2014]. http://www.bls.gov/iif/oshcdnew.htm.
Mitchell RJ, Bates P. Measuring health-related productivity loss. Popul Health Manag. 2011;14(2):93–8.
Dunn KM, Jordan K, Croft PR. Characterizing the course of low back pain: a latent class analysis. Am J Epidemiol. 2006;163(8):754–61.
Hestbaek L, Leboeuf-Yde C, Manniche C. Low back pain: what is the long-term course? A review of studies of general patient populations. Eur Spine J. 2003;12(2):149–65.
Cassidy JD, Cote P, Carroll LJ, Kristman V. Incidence and course of low back pain episodes in the general population. Spine. 2005;30(24):2817–23.
Pransky GS, Verma SK, Okurowski L, Webster B. Length of disability prognosis in acute occupational low back pain: development and testing of a practical approach. Spine. 2006;31(6):690–7.
Shaw WS, Pransky G, Patterson W, Winters T. Early disability risk factors for low back pain assessed at outpatient occupational health clinics. Spine. 2005;30(5):572–80.
Steenstra IA, Koopman FS, Knol DL, Kat E, Bongers PM, de Vet HC, et al. Prognostic factors for duration of sick leave due to low-back pain in Dutch health care professionals. J Occup Rehabil. 2005;15(4):591–605.
Crook J, Milner R, Schultz IZ, Stringer B. Determinants of occupational disability following a low back injury: a critical review of the literature. J Occup Rehabil. 2002;12(4):277–95.
Hilfiker R, Bachmann LM, Heitz CA, Lorenz T, Joronen H, Klipstein A. Value of predictive instruments to determine persisting restriction of function in patients with subacute non-specific low back pain. Systematic review. Eur Spine J. 2007;16(11):1755–75.
Cairns D, Mooney V, Crane P. Spinal pain rehabilitation: inpatient and outpatient treatment results and development of predictors for outcome. Spine. 1984;9(1):91–5.
Dionne CE, Bourbonnais R, Fremont P, Rossignol M, Stock SR, Larocque I. A clinical return-to-work rule for patients with back pain. CMAJ. 2005;172(12):1559–67.
Hogg-Johnson S, Cole DC. Early prognostic factors for duration on temporary total benefits in the first year among workers with compensated occupational soft tissue injuries. Occup Environ Med. 2003;60(4):244–53.
McIntosh G, Frank J, Hogg-Johnson S, Bombardier C, Hall H. Prognostic factors for time receiving workers’ compensation benefits in a cohort of patients with low back pain. Spine. 2000;25(2):147–57.
Jensen MP, Karoly P, Braver S. The measurement of clinical pain intensity: a comparison of six methods. Pain. 1986;27(1):117–26.
Beurskens AJ, de Vet HC, Koke AJ. Responsiveness of functional status in low back pain: a comparison of different instruments. Pain. 1996;65(1):71–6.
Deyo RA, Centor RM. Assessing the responsiveness of functional scales to clinical change: an analogy to diagnostic test performance. J Chronic Dis. 1986;39(11):897–906.
Deyo RA, Phillips WR. Low back pain. A primary care challenge. Spine. 1996;21(24):2826–32.
Hsieh CY, Phillips RB, Adams AH, Pope MH. Functional outcomes of low back pain: comparison of four treatment groups in a randomized controlled trial. J Manipulative Physiol Ther. 1992;15(1):4–9.
Kopec JA, Esdaile JM, Abrahamowicz M, Abenhaim L, Wood-Dauphinee S, Lamping DL, et al. The Quebec Back Pain Disability Scale. Measurement properties. Spine. 1995;20(3):341–52.
Leclaire R, Blier F, Fortin L, Proulx R. A cross-sectional study comparing the Oswestry and Roland-Morris Functional Disability scales in two populations of patients with low back pain of different levels of severity. Spine. 1997;22(1):68–71.
Patrick DL, Deyo RA, Atlas SJ, Singer DE, Chapin A, Keller RB. Assessing health-related quality of life in patients with sciatica. Spine. 1995;20(17):1899–908.
Roland M, Morris R. A study of the natural history of back pain. Part I: development of a reliable and sensitive measure of disability in low-back pain. Spine. 1983;8(2):141–4.
Stratford PW, Binkley J, Solomon P, Finch E, Gill C, Moreland J. Defining the minimum level of detectable change for the Roland-Morris questionnaire. Phys Ther. 1996;76(4):359–65.
Stratford PW, Binkley J, Solomon P, Gill C, Finch E. Assessing change over time in patients with low back pain. Phys Ther. 1994;74(6):528–33.
Ware J Jr, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34(3):220–33.
Luo X, Lynn George M, Kakouras I, Edwards CL, Pietrobon R, Richardson W, et al. Reliability, validity, and responsiveness of the short form 12-item survey (SF-12) in patients with back pain. Spine. 2003;28(15):1739–45.
Cody RP, Smith JK. Chapter 9: multiple regression analysis. Applied Statistics and the SAS programming language. 5th ed. Upper Saddle River, NJ: Pearson Prentice Hall; 2006. p. 282–319.
Hosmer DW, Lemeshow S. Applied logistic regression. 2nd ed. London: Wiley; 2000.
Hayden JA, Dunn KM, van der Windt DA, Shaw WS. What is the prognosis of back pain? Best Pract Res Clin Rheumatol. 2010;24(2):167–79.
Schultz IZ, Crook JM, Berkowitz J, Meloche GR, Milner R, Zuberbier OA, et al. Biopsychosocial multivariate predictive model of occupational low back disability. Spine. 2002;27(23):2720–5.
Heymans MW, Anema JR, van Buuren S, Knol DL, van Mechelen W, de Vet HC. Return to work in a cohort of low back pain patients: development and validation of a clinical prediction rule. J Occup Rehabil. 2009;19(2):155–65.
Kuijpers T, van der Windt DA, van der Heijden GJ, Twisk JW, Vergouwe Y, Bouter LM. A prediction rule for shoulder pain related sick leave: a prospective cohort study. BMC Musculoskelet Disord. 2006;7:97.
Turner JA, Franklin G, Fulton-Kehoe D, Sheppard L, Wickizer TM, Wu R, et al. Worker recovery expectations and fear-avoidance predict work disability in a population-based workers’ compensation back pain sample. Spine. 2006;31(6):682–9.
Johnson WG, Butler RJ, Baldwin ML, Côté P. Diasability risk management and postinjury employment patterns of workers with back pain. Risk Manag Insur Rev. 2012;15(1):35–55.
Acknowledgments
This research was supported by the Graduate Education and Research Department at the Canadian Memorial Chiropractic College. The Arizona State University Healthy Back Study was supported by a grant from the National Chiropractic Insurance Company (NCMIC). Neither funding agency was involved in the collection of data, data analysis, interpretation of data, or drafting of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Shearer, Dr. Côté, Dr. Frank, & Professor Johnson declare they have no conflict of interest. Dr. Boyle has received research grants payable to the University Health Network from the Workplace Safety and Insurance Board and the Canadian Chiropractic Protective Association. She has received a grant payable to the University of Southern Denmark from the Fonden til fremme af Kiropraktisk forskning og postgraduate uddannelse. Dr. Hayden has received funding for a research professorship at Dalhousie University from the Canadian Chiropractic Research Foundation.
Ethical Approval
The study protocol for the secondary analysis was approved by the University Health Network and the University of Toronto Research Ethics Boards. The ASU study protocol was approved by the Institutional Review Boards at Arizona State University and East Carolina University. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Rights and permissions
About this article
Cite this article
Shearer, H.M., Côté, P., Boyle, E. et al. Who will have Sustainable Employment After a Back Injury? The Development of a Clinical Prediction Model in a Cohort of Injured Workers. J Occup Rehabil 27, 445–455 (2017). https://doi.org/10.1007/s10926-016-9678-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10926-016-9678-6