Abstract
Objectives Some injured workers with work-related, compensated back pain experience a troubling course in return to work. A prediction tool was developed in an earlier study, using administrative data only. This study explored the added value of worker reported data in identifying those workers with back pain at higher risk of being on benefits for a longer period of time. Methods This was a cohort study of workers with compensated back pain in 2005 in Ontario. Workplace Safety and Insurance Board (WSIB) data was used. As well, we examined the added value of patient-reported prognostic factors obtained from a prospective cohort study. Improvement of model fit was determined by comparing area under the curve (AUC) statistics. The outcome measure was time on benefits during a first workers’ compensation claim for back pain. Follow-up was 2 years. Results Among 1442 workers with WSIB data still on full benefits at 4 weeks, 113 were also part of the prospective cohort study. Model fit of an established rule in the smaller dataset of 113 workers was comparable to the fit previously established in the larger dataset. Adding worker rating of pain at baseline improved the rule substantially (AUC = 0.80, 95 % CI 0.68, 0.91 compared to benefit status at 180 days, AUC = 0.88, 95 % CI 0.74, 1.00 compared to benefits status at 360 days). Conclusion Although data routinely collected by workers’ compensation boards show some ability to predict prolonged time on benefits, adding information on experienced pain reported by the worker improves the predictive ability of the model from ‘fairly good’ to ‘good’. In this study, a combination of prognostic factors, reported by multiple stakeholders, including the worker, could identify those at high risk of extended duration on disability benefits and in potentially in need of additional support at the individual level.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Work disability due to back pain is a multidimensional problem [1] associated with high compensation and treatment costs. In 2012, a low back injury was the most common reason for injured workers to claim workers’ compensation benefits in Ontario [2]. Workers at low risk for chronic disability will most likely return to work with limited assistance [3]. Those at high risk for chronic disability may benefit from interventions [4]. Therefore, correct classification of those at high risk is important.
This paper describes the further development of a predictive rule [5] for identifying those at high risk of chronic disability due to back pain. In an earlier paper, we showed that a prognostic model for time on benefits during a first back-pain-related wage-replacement claim, based on data readily available from a workers’ compensation board, had fair predictive accuracy. The predictive rule was based on information provided to the board by employers, workers and healthcare providers, combined with the board’s administrative data on opioid prescriptions and use of healthcare services. In our final predictive model age, physical demands, opioid prescription, employer doubt about work-relatedness of injury, and healthcare provider’s poor recovery expectations were associated with increased time on benefits, while union membership, availability of a return-to-work program, participation in a rehabilitation program, and communication of functional ability between the healthcare provider and workers’ compensation board were associated with shorter time on benefits. The model was able to identify prolonged claims to a fair degree (area under the curve [AUC] = 0.79, 95 % confidence interval [CI] 0.74–0.84).
To further develop the prediction rule, we wanted to find out if adding information on some well-known prognostic factors that was unavailable in routinely collected data would improve the accuracy of the earlier developed predictive rule. A subsample of the dataset described above had more elaborate information available because subjects participated in the Readiness for Return to Work (R-RTW) cohort study [6]. We added the individual-level injured worker data collected in the R-RTW cohort study to the scores of the predictive tool developed in the larger dataset [7]. The aim was to find out which, if selected, worker-reported factors measured in the first 4 weeks post-injury improved the accuracy of the earlier tool in predicting the length of a first back-pain-related episode of wage-replacement benefits.
Methods
Study Sample
A random sample of 6665 workers was taken from the population of all (n = 18,974) workers in Ontario, Canada, who had a lost-time claim (LTC) for an uncomplicated back injury (strain or sprain) approved by the Workplace Safety and Insurance Board (WSIB) of Ontario. The date of injury was between January 1 and June 30, 2005. Participants (n = 332) from the R-RTW cohort study [7] who received benefits for back pain during the same period were added to the cohort. Our study sample included the 113 of workers in the WSIB dataset who were also in the R-RTW cohort and were still on 100 % benefits 4 weeks post-injury. We excluded workers whose claims were initially registered as no-lost-time claims (NLTC) but later transitioned to LTC status, and workers for whom the number of days between accident date and registration date of the claim was greater than 30 days. We used the information available in the first 4 weeks of work disability to build our predictive models. The Health Sciences Research Ethics Board of the University of Toronto approved the study protocol.
Sources of Data
The earlier prediction model was based on data from three WSIB databases: (1) the electronic claim file database (2) the healthcare billings database, and (3) the database of imaged files showing forms filled out by the employer, worker and healthcare provider. An experienced analyst extracted and assembled data elements kept in the WSIB’s electronic databases (both the claim file and healthcare billings databases).
In Ontario, the employer, worker and healthcare provider complete a number of WSIB forms after claim filing. The employer form (Form 7) is mandatory and is submitted within 3 days of a work-related injury. Late or incomplete reporting can lead to a fine. The worker fills out a form (Form 6) if the worker has expenses related to the workplace injury and/or expects that the employer has not sent in Form 7. The healthcare provider fills out a form (Form 8) when a patient’s injury is work-related. The healthcare provider is reimbursed when a completed form is processed. In our study, data extractors accessed the WSIB’s imaged files and moved the information selected from these forms into an Access database.
The Readiness for Return to Work cohort study is a prospective study of Ontario workers with a back or upper extremity musculoskeletal disorder who filed a lost-time injury claim with the WSIB. Data was collected via self-reports from participants. The participants were interviewed by phone at baseline (on average 1 month post-injury) and at 6 and 12 months post-injury. The analysis in this paper is based on baseline data. The R-RTW study has been described in detail elsewhere [6, 7]. We added candidate predictors from the R-RTW cohort study, that were unavailable in the WSIB data, to the scores of the earlier developed predictive rule to our statistical model.
Candidate Predictors
Use of subject-matter knowledge is essential to selecting candidate predictors when building a prediction rule [8, 9]. Candidate predictors were identified in a review of studies in comparable settings and through stakeholder input [10]. In the prediction rule built from the WSIB data [5], age, physical demands at work [11, 12], opioid prescription [11, 13–15], employer doubt about work-relatedness of injury [16], poor recovery expectations as reported by healthcare provider, were associated with longer time on benefits. Union membership [17], availability of a return-to-work program [12, 18], participation in a work rehabilitation program and communication of functional ability [19, 20] were associated with shorter time on benefits. Some important prognostic factors [10] were unavailable in the WSIB databases but were collected in the R-RTW cohort study: self-report of pain with a 10 point Visual Analog Scale [10, 21], functional status with the Roland Morris Disability Questionnaire [10, 22], job satisfaction from the Job Content Questionaire [10, 23] and depression with the CES-D [10, 24]. Workplace accommodations were identified as an important prognostic factor in the R-RTW cohort [7], but this construct was already part of the WSIB prediction rule through the item on the availability of a return to work program. See Table 1 for an overview of the factors and the information source for each one.
Outcome Measures
Benefit status was ascertained from the workers’ compensation administrative databases over a 2 years period after first day of injury [25].The outcome was length of time, which is a continuous variable, with censoring at 2 years post accident. We defined time on benefits during a first claim for back pain as the length in calendar days of the first continuous episode of any wage replacement [26].
Statistical Analyses
We examined Pearson correlations between the factors from the developed rule and the new factors added from the R-RTW cohort study. The previously developed predictive tool was validated in the smaller dataset from the prospective cohort study. The area under the curve was calculated, comparing the predicted score with benefit status (yes/no on 100 % benefits) at 6 months.
The new model was built by taking the score from the earlier developed prediction rule as established in the larger dataset (xβ) for each individual worker and adding it to the R-RTW cohort dataset. A backward automated procedure determined which of the following factors would remain in the final model: score on the prediction rule, pain score [21], functional disability [22], depression score [27], and job satisfaction [28]. Variables with the lowest predictive value were deleted from the model until further elimination of variables resulted in a statistically significant lower model fit as indicated by the log-likelihood ratio test. The following factors were entered into the backward automated procedure: score on the prediction rule, pain score, functional disability, depression score, and job satisfaction. Factors that were removed by the automated procedure were forced back into the model that resulted from the automated procedure to examine possible improvements of the overall model. Statistical significance of individual variables was ignored since we aimed for the most parsimonious model.
We used Cox semi-parametric modeling to examine the relationship between multiple predictors and outcome. The proportional hazards assumption was checked [29]. An HRR smaller than one indicates longer time until end of benefits. We examined predictive validity of the score on this ‘improved’ prediction rule (xβ2) by calculating the area under the receiver-operating characteristic curve (ROC), c-statistic [30] comparing estimated probability of RTW as determined by the improved prediction rule with actual benefit status at 180 days on benefits. The following criteria were used to evaluate the AUC: 0.90–1.00 = excellent, 0.80–0.90 = good, 0.70–0.80 = fair, 0.60–0.70 = poor, <.50–0.60 = fail [30].
Analyses were performed using IBM SPSS Statistics for Windows, Version 19.0 (IBM Corp., Armonk, NY, 2010).
Results
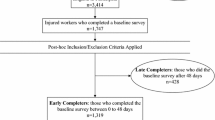
From the sample of 6657 WSIB cases, 1442 remained on full benefits at 4 weeks. From the sample of 332 R-RTW cases with LBP, 113 workers were on full benefits at 4 weeks. All 113 workers had complete data on predictive factors and outcomes. See Fig. 1 for a flowchart depicting the selection of cases for this study. None of the factors in the developed predictive rule was correlated with any of the selected factors from the R-RTW cohort study beyond 0.29 (between functional status and having an early RTW program). Table 2 shows the baseline characteristics of the full sample of 1442 injured workers and of the subsample of 113 workers form the R-RTW cohort. Results show that both samples are similar with respect to the distribution of the most important predictive factors.
Time on Benefits for First Back Pain Episode
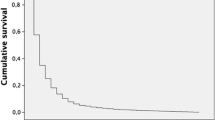
The median duration of time on disability benefits for the subsample was the same as for the full sample: 57 days (interquartile range 38–98) days (mean = 87 days, SD = 89). After 360 days, 94 % of workers had ended benefits (Fig. 2).
The prediction rule for time on benefits during a first claim episode had an AUC of 0.76 at 180 days when validated in the R-RTW cohort data (0.71 at 180 days in the full sample). An automated backward procedure testing all selected factors resulted in two factors remaining in the final model: the score on the prediction rule as derived from the main analysis and the score on the 10-point Likert Pain scale (Table 3). Adding the pain score from the baseline measurement improved the rule, raising it to the classification level of “good” (AUC = 0.80, 95 % CI 0.68, 0.91 at 180 days, AUC = 0.88, 95 % CI 0.74, 1.00 at 360 days). Figure 2 shows survival curves for the four risk categories of workers based on a division of predicted scores in quartiles.
This analysis shows that adding a single 10-point Likert Pain scale asking injured workers about their current pain could improve the predictive accuracy of the rule to the level where it can predict likely outcomes in individual cases. The Pain scale item was the following:
“How would you rate your back pain on a 0–10 scale at the present time, that is right now, where 0 is no pain and 10 is pain as bad as could be”
Discussion
Our findings highlighting the importance of the role of pain in understanding MSD-related work absence are consistent with findings of previous research [31–33].
The strength of our study was its use of routinely collected data from different stakeholders in the RTW process [1], compared to previous research that often relied on data collected from a single stakeholder perspective only, usually that of the injured worker or patient.
By using the score on the predictive rule derived from the larger dataset, we prevented overfitting of the model. Were we to have built the model within the R-RTW cohort only, using the variables identified in the larger data (age, physical demands, opioid prescription, employer doubt about work-relatedness of injury, and healthcare provider’s poor recovery expectations, union membership, availability of a return-to-work program, participation in a rehabilitation program, and communication of functional ability between the healthcare provider and workers’ compensation board), the model fit of the new “R-RTW” predictive rule would have had an AUC of 0.98 (95 % CI, 0.95, 1.00) at 360 days.
Both the model fit of the prediction rule (derived from the larger dataset) as validated in the smaller sample as well as the duration on benefits (median of 57 days) were comparable between the two samples, which confirms earlier analyses that the R-RTW is a representative sample of injured workers [7]. Still, a prediction rule developed in a small dataset is likely not applicable to the general population.The model fit of the improved prediction rule for time on benefits was better compared to the fit presented in studies in similar settings, which reported a discriminative ability of 0.80 [34] and 0.76 [35]. It was better compared to others reporting an AUC of 0.63 [36] and 0.69 when validating the Orebro Musculoskeletal Screening Questionnaire in a Canadian workers’ compensation setting [37].
Limitations of this study are of course the small sample size which limited the ability to add all predictors independently. We focused on workers that had a minimum of 1 month lost work time, meaning the sample is biased to claims that are more serious. However, in work compensation practice a prediction tool would most likely only be used close to the 4 week time point because of the good prognosis of LBP for RTW in the first 4 weeks. Earlier risk screening would be a substantial burden to the respondent and the person that is intended to apply the results of the screening. Screening can result in misclassification that would lead to potentially intervening in workers that would return to work regardless.
Although this prediction rule is intended for workers claiming for LBP all factors in this prediction rule apply to all conditions where pain is involved.Adding a simple Likert Pain scale to the form for workers, or including it in the routine Workers’ Compensation Case Manager’s intake interview, is a feasible step to take to improve identification of workers in need of early intervention. Pain is part of the experience of workers with disorders other than back pain, and consequently, the value of considering pain in early identification of workers at risk of prolonged work disability may be generalizable to a larger group of injured workers—this would need to be validated in further research. Musculoskeletal Disorders (MSD) associated with pain still account for a large proportion of all work disability cases in Ontario [2]. Pain scores are part of the mandatory assessment forms administered within the WSIB’s Program of Care (POC) for low-back pain. In recent years, the majority of low-back pain cases are referred to the WSIB’s POC within the first 4 weeks after the date of injury. Entry into the POC seems to be the ideal point at which to further assess the risk of prolonged disability for an injured worker. Temporal validation of the prediction rule established in this study could easily be done by data entry of assessment forms that are available in WSIB databases, since payment for service only occurs when assessment forms are sent in by the healthcare professional providing the POC.
Conclusion
The accuracy of our WSIB administrative data based predictive model was improved by adding information on worker reported pain rating [21]. A predictive tool, to be used by Workers’ Compensation Board staff, and possibly by other stakeholders, should be further developed and evaluated [9]. Such a tool would assist in identifying, early on in the life of claims, those workers who are at risk of prolonged work disability, and who may benefit from early intervention to assist them to return to work in a safe and sustainable fashion.
References
Loisel P, Durand MJ, Berthelette D, Vezina N, Baril R, Gagnon D, et al. Disability prevention—new paradigm for the management of occupational back pain. Dis Manag Health Outcomes. 2001;9(7):351–60.
WSIB. 2012 Schedule 1 statistical report. 2013. Toronto, WSIB. 9-11-2013. Ref Type: Online Source.
Indahl A, Velund L, Reikeraas O. Good prognosis for low back pain when left untampered. A randomized clinical trial. Spine. 1995;20(4):473–7.
Hill JC, Whitehurst DG, Lewis M, Bryan S, Dunn KM, Foster NE, et al. Comparison of stratified primary care management for low back pain with current best practice (STarT Back): a randomised controlled trial. Lancet. 2011;378(9802):1560–71.
Steenstra IA, Busse JW, Tolusso D, Davilmar A, Lee H, Furlan AD, et al. Predicting time on prolonged benefits for injured workers with acute back pain. J Occup Rehabil. 2015;25(2):267–78.
Bultmann U, Franche RL, Hogg-Johnson S, Cote P, Lee H, Severin C, et al. Health status, work limitations, and return-to-work trajectories in injured workers with musculoskeletal disorders. Qual Life Res. 2007;16(7):1167–78.
Franche RL, Severin CN, Hogg-Johnson S, Cote P, Vidmar M, Lee H. The impact of early workplace-based return-to-work strategies on work absence duration: a 6-month longitudinal study following an occupational musculoskeletal injury. J Occup Environ Med. 2007;49(9):960–74.
Steyerberg EW. Clinical prediction models. A practical approach to development, validation, and updating. New York: Springer; 2009.
McGinn TG, Guyatt GH, Wyer PC, Naylor CD, Stiell IG, Richardson WS. Users’ guides to the medical literature: XXII: how to use articles about clinical decision rules. Evid Based Med Work Group JAMA. 2000;284(1):79–84.
Steenstra IA, Busse JW, Hogg-Johnson S. Predicting return to work for workers with low-back pain. In: Loisel P, Anema JR, Pransky GS, editors. Work disability prevention handbook. New York: Springer Science + Business Media New York; 2013.
Du Bois M, Szpalski M, Donceel P. Patients at risk for long-term sick leave because of low back pain. Spine J. 2009;9(5):350–9.
Turner JA, Franklin G, Fulton-Kehoe D, Sheppard L, Stover B, Wu R, et al. ISSLS prize winner: early predictors of chronic work disability: a prospective, population-based study of workers with back injuries. Spine (Phila Pa 1976). 2008;33(25):2809–18.
Cifuentes M, Webster B, Genevay S, Pransky G. The course of opioid prescribing for a new episode of disabling low back pain: opioid features and dose escalation. Pain. 2010;151(1):22–9.
Franklin GM, Stover BD, Turner JA, Fulton-Kehoe D, Wickizer TM. Early opioid prescription and subsequent disability among workers with back injuries: the Disability Risk Identification Study Cohort. Spine. 2008;33(2):199–204.
Pransky GS, Verma SK, Okurowski L, Webster B. Length of disability prognosis in acute occupational low back pain: development and testing of a practical approach. Spine. 2006;31(6):690–7.
Schultz IZ, Crook J, Meloche GR, Berkowitz J, Milner R, Zuberbier OA, et al. Psychosocial factors predictive of occupational low back disability: towards development of a return-to-work model. Pain. 2004;107(1–2):77–85.
Johnson WG, Butler RJ, Baldwin ML. First spells of work absences among Ontario workers. In: Thomason T, Chaykowski RP, editors. Research in Canadian workers’ compensation. Kingston: IRC Press; 2005.
Steenstra IA, Verbeek JH, Heymans MW, Bongers PM. Prognostic factors for duration of sick leave in patients sick listed with acute low back pain: a systematic review of the literature. Occup Environ Med. 2005;62(12):851–60.
Pransky G, Shaw W, Franche RL, Clarke A. Disability prevention and communication among workers, physicians, employers, and insurers–current models and opportunities for improvement. Disabil Rehabil. 2004;26(11):625–34.
Franche RL, Cullen K, Clarke J, Irvin E, Sinclair S, Frank J. Workplace-based return-to-work interventions: a systematic review of the quantitative literature. J Occup Rehabil. 2005;15:607–31.
Von Korff M, Ormel J, Keefe FJ, Dworkin SF. Grading the severity of chronic pain. Pain. 1992;50(2):133–49.
Roland M, Morris R. A study of the natural history of back pain. Part I: development of a reliable and sensitive measure of disability in low-back pain. Spine. 1983;8(2):141–4.
Karasek R. Job Content Instrument Users Guide: revision 1.1. Los Angeles: University of Southern California; 1985.
Franche RL, Carnide N, Hogg-Johnson S, Cote P, Breslin FC, Bultmann U, et al. Course, diagnosis, and treatment of depressive symptomatology in workers following a workplace injury: a prospective cohort study. Can J Psychiatry. 2009;54(8):534–46.
Croft PR, Dunn KM, Raspe H. Course and prognosis of back pain in primary care: the epidemiological perspective. Pain. 2006;122(1–2):1–3.
Steenstra IA, Lee H, de Vroome EM, Busse JW, Hogg-Johnson SJ. Comparing current definitions of return to work: a measurement approach. J Occup Rehabil. 2012;22(3):394–400.
Radloff LS. The CES_D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401.
Karasek R, Brisson C, Kawakami N, Houtman I, Bongers PM, Amick B. The Job Content Questionnaire (JCQ): an instrument for internationally comparative assessments of psychosocial job characteristics. J Occup Health Psychol. 1998;3(4):322–55.
Collett D. Modelling survival data in medical research. London: Chapman & Hall; 1994.
Hanley JA, McNeil BJ. The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology. 1982;143(1):29–36.
Murray E, Franche RL, Ibrahim S, Smith P, Carnide N, Cote P, et al. Pain-related work interference is a key factor in a worker/workplace model of work absence duration due to musculoskeletal conditions in Canadian nurses. J Occup Rehabil. 2013;23(4):585–96.
Franche RL, Murray E, Ibrahim S, Smith P, Carnide N, Cote P, et al. Examining the impact of worker and workplace factors on prolonged work absences among Canadian nurses. J Occup Environ Med. 2011;53(8):919–27.
Shaw WS, Linton SJ, Pransky G. Reducing sickness absence from work due to low back pain: How well do intervention strategies match modifiable risk factors? J Occup Rehabil. 2006;16(4):591–605.
Heymans MW, van BS, Knol DL, Anema JR, van MW, de Vet HC. The prognosis of chronic low back pain is determined by changes in pain and disability in the initial period. Spine J. 2010;10(10):847–56.
Heymans MW, Ford JJ, McMeeken JM, Chan A, de Vet HC, van MW. Exploring the contribution of patient-reported and clinician based variables for the prediction of low back work status. J Occup Rehabil. 2007;17(3):383–97.
Heymans MW, Anema JR, van BS, Knol DL, van MW, de Vet HC. Return to work in a cohort of low back pain patients: development and validation of a clinical prediction rule. J Occup Rehabil. 2009;19(2):155–65.
Kirkwood R. External validation of the orebro musculoskeletal pain screening questionnaire within an injured worker population: a Retrospective Cohort Study Open Access Dissertations and Theses. 2011. https://macsphere.mcmaster.ca/handle/11375/11432
Conflict of interest
The authors have no competing interests.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Steenstra, I.A., Franche, RL., Furlan, A.D. et al. The Added Value of Collecting Information on Pain Experience When Predicting Time on Benefits for Injured Workers with Back Pain. J Occup Rehabil 26, 117–124 (2016). https://doi.org/10.1007/s10926-015-9592-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10926-015-9592-3