Abstract
In Germany it is common practice to use pulse oximetry and supplementary oxygen only on request in patients breathing spontaneously transferred to the post-anaesthesia care unit (PACU) following surgery under general anaesthesia. The main aim was to study the influence of medical training and clinical experience on assessing SpO2 and detecting hypoxaemia in these patients. The second aim was to do a preliminary assessment whether this practice can be found in countries other than Germany. Anaesthetists, nurses and medical students estimated SpO2 in patients breathing room air at the end of transfer to the PACU following surgery (including all major surgical fields) under general anaesthesia. Estimated SpO2 was compared to SpO2 measured by pulse oximetry. A survey was carried out among European anaesthesists concerning the use of pulse oximetry and supplementary oxygen during patient transfer to the PACU. Hypoxaemia (SpO2 < 90 %) occurred in 154 (13.5 %) out of 1,138 patients. Anaesthetists, nurses, and medical students identified only 25, 23, and 21 patients of those as being hypoxaemic, respectively. Clinical experience did not improve detection of hypoxaemia both in anaesthetists (p = 0.63) and nurses (p = 0.18). Use of pulse oximetry and supplemental oxygen during patient transfer to the PACU in European countries differs to a large extent. It seems to be applied only on request in many hospitals. Considering the uncertainty about deleterious effects of transient, short lasting hypoxaemia routine use of pulse oximetry is advocated for patient transfer to the PACU.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1 Introduction
Analysis of anaesthetic-related closed malpractice claims demonstrated that hypoxaemia, resulting in desaturation, was a major cause for morbidity and mortality during and following procedures under general anaesthesia [1, 2]. More recent data confirm the deleterious effects hypoxaemia may have on patient outcome [3, 4]. Accordingly, the use of pulse oximetry has become a compulsory part of the standard monitoring during general anaesthesia in Europe as reflected by the guidelines of the national anaesthesia societies [e.g. 5, 6]. In contrast, as for the period of immediate postanaesthetic recovery [i.e. during transfer from the operating room (OR) to the post-anaesthesia care unit (PACU)], guidelines and recommendations concerning anaesthetic care including instructions on when to use pulse oximetry and supplemental oxygen are inconsistent within Europe.
We recently demonstrated that 17 % of patients breathing room air in the period immediately following general anaesthesia during transfer from the OR to the PACU were hypoxaemic (SpO2 < 90 %) and that hypoxaemia was not detected based on clinical signs in 82 % of these patients [7]. However, despite these results it is not uncommon to encounter the opinion that more experienced anaesthesia providers are better at detecting hypoxaemia on clinical grounds only. To date, it has not been studied whether the level of medical education and clinical experience have any influence on either the accuracy of estimating the SpO2, or most importantly, on clinically detecting hypoxaemia.
In addition, results of a survey among anaesthesia departments of all German university hospitals revealed that at the vast majority of German university hospitals, it is not common practice to use pulse oximetry and supplementary oxygen in every patient breathing spontaneously during transfer to the PACU following surgery under general anaesthesia. Instead, pulse oximetry and supplementary oxygen are only used on request in selected patients [7].
Therefore, the main aims of this follow-up study were to investigate the influence of clinical experience on the accuracy of estimating the SpO2 in general and above all to determine the reliability of detecting hypoxaemic patients based only on clinical criteria. Moreover, in order to discern whether the findings of our previous [7] and present study may be of any relevance for anaesthesia providers in countries other than Germany, we sought to find out whether the practice to use pulse oximetry and supplemental oxygen only on request in selected patients breathing room air during their transfer to PACU following general anaesthesia can be encountered in other European countries.
2 Methods
Approval for this study was obtained from the local ethics committee (Ethics committee of the University Hospital of Marburg, Germany, AZ 3709, Chairperson Prof. G. Richter. According to the decision of the local ethics committee, no individual patient consent was required for this prospective observational study carried out at Marburg University Hospital (UKGM—Marburg campus). It was intended to include a minimum of 1,000 patients within 1 year.
2.1 Study protocol
Patients who do not require post-operative care on an intensive care unit (ICU) are commonly transferred from the OR to the adjacent PACU by the assigned anaesthetist and nurse without supplemental oxygen and without any monitoring of the vital signs unless requested by the anaesthetist. At the end of patient transfer to PACU on a mobile operating table, patients are moved onto the ward bed by means of a mechanical transfer table in an area separating the OR and the PACU (see Supplemental Digital Content 1 and 2: photographs of the mechanical transfer table). During that final stage of patient transfer (while the patient was on the mechanical transfer table) a PACU nurse, the assigned anaesthetist, and a medical student performed a clinical evaluation of the patient’s SpO2. Assessments of the patient’s SpO2 were performed at the discretion of the study subjects (most likely by looking for cyanosis). Participation of PACU nurses and anaesthetists in this study was by chance, depending on who happened to take care of the patient. Two medical students who also participated in this study took turns estimating the SpO2 in all patients. The latter did not have any previous training in assessing patients’ SpO2 neither as part of their medical education (3rd year medical students at the beginning of the clinical studies), nor as part of this investigation. This lack of experience made them good candidates to investigate whether any improvement of clinically assessing patient’s SpO2 can be achieved over time. Results of the estimations were taken down separately (first the students’, next the nurse’s, and last the anaesthetist’s evaluation) to exclude any influence by the results of the other persons’ estimations. Osram L38W/840 fluorescent tubes were used during the whole study period for illumination of the area where the mechanical transfer table was located. According to the manufacturer’s information, these tubes have a discontinuous spectrum including the whole visible range with significant power output in only three regions based around wavelengths at 440 nm (blue), 540 nm (green) and 610 nm (orange to light red).
Immediately after the clinical evaluation, the patient’s SpO2 was measured using a pulse oximeter (Massimo® RAD7; Massimo Corporation: Irvine CA, USA). In addition to the SpO2, the perfusion index (range 0.02–20 %; considered as a quality marker if >0.25 %) of the measured SpO2 was also detected. The measurement of the patient’s SpO2 was considered valid if the reading was stable for 10 s. Moreover, clinical experience of the anaesthetist and the nurse executing the estimation of the patient’s SpO2 were recorded.
2.2 Inclusion and exclusion criteria
All adult patients who were transferred to the PACU breathing room air following an elective operation under general anaesthesia were eligible for this study. There were neither restrictions concerning the type of surgery performed nor regarding drugs administered for induction and maintenance of anaesthesia. Departmental standards that applied included: (1) relaxometry when non depolarising relaxants were used, (2) monitoring depth of anaesthesia in patients that underwent surgery expected to last at least 15 min, and (3) measuring patients’ temperature and warming them if procedures were expected to last at least 30 min. FiO2 was changed to 1.0 for emergence of anaesthesia.
Patients who were transferred with supplemental oxygen from the OR to the PACU were not included in the study. Patients, whose SpO2 measurements were associated with a perfusion index <0.25 % or with a bad signal quality (as indicated on the display) were also excluded from the study.
2.3 Patient data
The following data of patients enrolled into the study were recorded:
Sex, age, height, weight, physical status according to ASA, pulmonary disease, smoking, and SpO2 prior to induction of anaesthesia, type of surgery, type of general anaesthesia, anaesthetics used for maintenance, duration of anaesthesia, type of airway, distance between OR and the mechanical transfer table, waiting time at the mechanical transfer table, perfusion index, and SpO2.
2.4 Preparatory data analysis
Hypoxaemia was defined as mild (SpO2 < 90 %), moderate (SpO2 < 85 %) and severe (SpO2 < 80 %) [8, 9]. Readings of the pulse oximetry were classified accordingly. Physicians’ clinical experience in anaesthesia was dichotomised as follows: ≤5 and >5 years.
2.5 Statistical analysis
Statistical analysis was performed using SPSS for windows, version 19.0 (SPSS Inc., Chicago IL, USA). Discrete variables are presented as number and proportion. Continuous variables are presented as mean with their standard deviation (SD) and confidence interval (CI) or minimum and maximum. The Kolmogorov–Smirnov test was used to explore normality of distribution of continuous variables. As for dichotomised data, Fisher’s exact test was applied for bivariate analysis and Wilcoxon–Mann–Whitney-test was used for continuous data. Spearman’s rank correlation coefficient (Spearman’s rho) was calculated to study associations between two continuous variables: measured SpO2 and difference between estimated and measured SpO2; running patient number as a surrogate for increasing experience of the medical students and difference between estimated and measured SpO2. Spearman’s rho regarding the latter association was used to investigate if a learning curve can be found concerning the accuracy of assessing the patient’s SpO2.
2.6 Survey concerning the use of pulse oximetry and supplemental oxygen immediately after general anaesthesia
The survey was carried out by means of a questionnaire containing seven questions that addressed the following aspects: use of pulse oximetry and supplemental oxygen (in all patients vs. on request), transfer time from the OR to the PACU (i.e. from disconnecting the patient from the vital sign monitor in the OR until reconnecting the patient to the vital sign monitor in the PACU), and use of supplemental oxygen in the PACU (routinely vs. on request depending on the SpO2). (See the original questionnaire at: Supplemental Digital Content 3) The survey was executed using 3 different approaches:
-
1.
One questionnaire each was sent to a senior member (chosen at the discretion of one of the authors working in the Netherlands—F.W.) of the anaesthesia department of each Dutch university hospital.
-
2.
One questionnaire was sent to one staff anaesthetist (chosen at the discretion of one of the authors working in Denmark—A.A.) of the anaesthesia departments of the 21 largest public hospitals that have an ICU and a PACU.
-
3.
Attendees of the 2013 Euroanaesthesia meeting were invited to take part in the survey carried out as an interview by two of the authors (D.R., L.E.). In order to get a better insight into the habits of the different European countries, the aim was to get as many participants as possible from different hospitals from a few selected countries rather than inviting attendees from all countries. The countries chosen include Austria, Belgium, France, Greece, Italy, Poland, Portugal, Romania, Slovenia, and Spain. In order to be able to identify participants from the same institution, data recorded also included name and location of the hospital at which attendees work. In addition to analysing the use of pulse oximetry and supplemental oxygen, a detailed analysis of the estimated average, minimal, and maximal patient transfer times (presented as mean, standard deviation and range) from the OR to the PACU was done if at least 3 anaesthetists working in different hospitals of the same country were participating in the survey.
3 Results
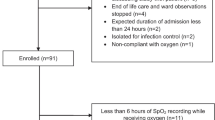
This study was performed on 1,187 patients over a period of 9 months. Forty-nine of those were excluded from data analysis leaving 1,138 patients for analysis (Fig. 1).
Flow diagram of the enrollment process. All data of analysed patients including biometric data, variables related to anaesthesia and surgery are summarised in Table 1
All data of analysed patients including biometric data, variables related to anaesthesia and surgery are summarised in Table 1.
3.1 SpO2 at the end of patient transfer to the PACU
The average SpO2 of the 984 (86.5 %) normoxaemic patients was 95 % (SD ± 2.6 %). The mean SpO2 of the 154 (13.5 %) hypoxaemic patients (SpO2 < 90 %) was 86 % (SD ± 4 %). Among those, 118 (10.4 %) had a mild (SpO2 85–89 %), 26 (2.3 %) a moderate (SpO2 80–84 %), and 10 (0.9 %) a severe hypoxaemia (SpO2 < 80 %). The lowest SpO2 measured was 60 %.
3.2 Hypoxaemia and anaesthetists’ clinical experience
Differences regarding the incidences of hypoxaemia between patients anaesthetised by colleagues with clinical experience up to 5 years compared to those with more than 5 years of clinical experience were not significant (p = 0.069; Fig. 2).
SpO2 and anaesthetists’ clinical experience. Incidences of mild, moderate and severe hypoxaemia in patients anaesthetised by colleagues with ≤5 years (blue columns) or more than 5 years (red columns) of clinical practice. Sixty-three (11.6 %) of the 544 patients taken care of by anaesthetists with ≤5 years of clinical practice were hypoxaemic compared to 91 (15.9 %) of the 594 patients taken care of anaesthetists with more than 5 years of clinical practice (p = 0.069). Differences in patients with mild (p = 0.1) and moderate (p = 0.3) hypoxaemia were not different either
3.3 Clinical assessment of SpO2
Sixty-four anaesthetists and 26 nurses participated in the study. The two medical students who also took part in the study estimated about 50 % of the patients each (student A: 582, student B: 556). Results of the estimations of SpO2 in hypoxaemic patients on clinical grounds are summarised in Table 2. In general, patients’ SpO2 was primarily overestimated in patients with a low SpO2 by anaesthetists, nurses and medical students. Details of the results of the clinical assessment of patients’ SpO2 by anaesthetists, nurses, and medical students are presented separately in the following sections with an emphasis on hypoxaemic patients.
3.4 Anaesthetists’ clinical assessment of patients’ SpO2
The mean estimated SpO2 in all patients was 94.5 % (±2.5) compared to an average measured SpO2 of 93.7 % (±4.2) with a mean difference of 0.9 % (±3.8; 95 % CI 0.7/1.1).
There was a correlation between the measured SpO2 and the difference between estimated versus measured SpO2 (Spearman’s rho −0.7453, p < 0.001, Fig. 3). Twenty-five (16.2 %) of the 154 hypoxaemic patients were correctly identified as being hypoxaemic. The mean estimated SpO2 in hypoxaemic patients was 92.3 % (±3.4) whereas the average measured SpO2 was 85.8 % (±4.0) with a mean difference of 6.5 % (±4.8). Results of the individual estimations of patients’ SpO2 by anaesthetists in hypoxaemic patients are shown in Fig. 4. Whereas in hypoxaemic patients who were anaesthetised by colleagues with ≤5 years of clinical experience the mean difference between the estimated SpO2 [mean 92.7 % (±2.7)] and the measured SpO2 [mean 85.4 % (±4.8)] was 7.3 % (±4.8) the corresponding results in hypoxaemic patients who were taken care of by anaesthetists with >5 years of clinical experience were 92.0 % (±3.8), 86.0 % (±3.3) and 5.9 % (±4.7), respectively. Estimation errors of patients’ SpO2 were not different between these two groups of anaesthetists (p = 0.63).
Difference between measured SpO2 and anaesthetists’ estimations of SpO2—all patients. SpO2 measured by pulse oximetry (abscissa) plotted against the difference between the anaesthetists’ estimation of the patients’ SpO2 and the measured SpO2 (ordinate) in all patients (modified Bland–Altman plot). Data points under the blue line represent patients whose SpO2 was underestimated and data points above the blue line represent patients whose SpO2 was overestimated. A point may represent multiple data with the same value
Difference between measured SpO2 and anaesthetists’ estimations of SpO2. SpO2 measured by pulse oximetry (abscissa) plotted against the difference between the anaesthetists’ estimation of the patients’ SpO2 and the measured SpO2 (ordinate) in hypoxaemic patients (modified Bland–Altman plot). Data points under the blue line represent patients whose SpO2 was underestimated and data points above the blue line represent patients whose SpO2 was overestimated. A point may represent multiple data with the same value
3.5 Nurses’ clinical assessment of patients’ SpO2
Twenty-three (14.9 %) of the 154 hypoxaemic patients were correctly identified as being hypoxaemic. In those hypoxaemic patients, the estimated SpO2 [mean 92.4 % (±2.9)] was off on average by 6.6 % (±4.0) compared to the measured SpO2 [mean 85.8 % (±4.0)]. Results of the individual estimations of patients’ SpO2 by nurses in hypoxaemic patients are presented in Fig. 5. The average clinical experience of the nurses who participated in this study was 15 years (±8.6, range 0.5–40 years). Clinical experience did not have a positive impact on the accuracy of clinically assessing the SpO2 in hypoxaemic patients (p = 0.18).
Difference between measured SpO2 and nurses’ estimations of SpO2. SpO2 measured by pulse oximetry (abscissa) plotted against the difference between the nurses’ estimation of the patients’ SpO2 and the measured SpO2 (ordinate) in hypoxaemic patients (modified Bland–Altman plot). Data points under the blue line represent patients whose SpO2 was underestimated and data points above the blue line represent patients whose SpO2 was overestimated. A point may represent multiple data with the same value
3.6 Medical students’ clinical assessment of patients’ SpO2
Twenty-one (13.6 %) of the 154 hypoxaemic patients were correctly identified as being hypoxaemic. The average difference between the measured SpO2 [mean 85.8 % (±4.0)] and the estimated SpO2 [mean 92.1 % (±2.6)] was 6.4 % (±3.7). Results of the individual estimations of patients’ SpO2 by the two medical students in hypoxaemic patients are shown in Fig. 6. As illustrated in Figure 7 and 8 (see Supplemental Digital Content 4 and 5), neither of them improved over time concerning the accuracy of clinically estimating patients’ SpO2 (student A: Spearman’s rho −0.0206, p = 0.8527 and student B: Spearman’s rho −0.0299, p = 0.8058).
Difference between measured SpO2 and medical students’ estimations of SpO2. SpO2 measured by pulse oximetry (abscissa) plotted against the difference between the medical students’ estimation of the patients’ SpO2 and the measured SpO2 (ordinate) in hypoxaemic patients (modified Bland–Altman plot). Data points under the blue line represent patients whose SpO2 was underestimated and data points above the blue line represent patients whose SpO2 was overestimated. A point may represent multiple data with the same value
3.7 European survey
3.7.1 Results in the Netherlands
In most Dutch university hospitals, neither pulse oximetry (6 out of 8) nor supplemental oxygen (7 out of 8) is used routinely in all patients breathing spontaneously during transfer from the OR to the PACU. Estimated transfer times are relatively short (mean transfer time: 0.5–3 min; minimal transfer time: 0.5–2 min; maximal transfer time: 1–5 min).
3.7.2 Results in Denmark
Of the 21 hospitals that were contacted 18 returned the questionnaires. Among those, there were 10 major hospitals (including university hospitals). In all but two hospitals, patients who undergo a procedure under general anaesthesia are routinely transferred to the PACU using either pulse oximetry in all patients and supplemental oxygen on request (n = 2), or supplemental oxygen in all patients and pulse oximetry on request (n = 4), or pulse oximetry and supplemental oxygen in all patients (n = 10). In two hospitals, both pulse oximetry and supplemental oxygen is used on request. In the latter, average transfer times were estimated to be 1 and 5 min, respectively. The ranges of the transfer times were estimated from a minimum of 1 and 5 min to a maximum of 2 and 10 min, respectively.
3.7.3 Results at the 2013 Euroanaesthesia meeting
A total of 122 anaesthetists participated in the study. They work at 114 different institutions in 14 different European countries. Results of the survey are presented in detail in Table 3. Results of countries with one participant each (n = 3) are not shown.
In summary, results of the survey demonstrate that patient transfer to PACU regarding the use of pulse oximetry and supplemental oxygen differs a lot in Europe. Moreover, results of the survey clearly suggest that in several countries (e.g. Austria, Portugal, and Spain) the use of pulse oximetry and/or supplemental oxygen in all patients breathing spontaneously transferred to PACU is not standard of care.
4 Discussion
Shortly after the introduction of pulse oximetry into clinical practice, shortcomings of the assessment of patients’ oxygenation and the detection of hypoxaemia based on clinical signs were demonstrated both for the period during as well as for the period following general anaesthesia [8–10]. Results of a more recent study [7] confirmed the deficiencies of clinically assessing patients’ oxyhaemoglobin fraction and more importantly the unreliability of clinically detecting hypoxaemia. Even though there is a widespread assumption that anaesthesia providers who have been working in anaesthesia for many years are better at clinically assessing patient’s SpO2 and detecting hypoxaemic patients, there has been no systematic investigation as the validity of this assumption.
Results of this work reconfirm the shortcomings of clinical signs to estimate patients’ SpO2 and, more importantly, to detect hypoxeamia. Given the clinical significance of hypoxeamia, data analysis focused on comparing estimated SpO2 to measured SpO2 in hypoxaemic patients. Hypoxaemia was not detected in 84 % by anaesthetists, 85 % by nurses, and 86 % by medical students. Even among the 10 patients with severe hypoxaemia (SpO2 < 80 %) 7, 5, and 4 patients were not considered to be hypoxaemic by anaesthetists, nurses and medical students, respectively (Table 2). Comparison of the scatter plots showing the difference between estimated and measured SpO2 in hypoxaemic patients of the three study groups clearly illustrates that all three study groups did similarly poor assessing the patients’ SpO2 and detecting hypoxaemia (Figs. 4, 5, 6). Likewise, the mean difference between estimated and measured SpO2 in hypoxaemic patients assessed by anaesthetists with more than 5 years of clinical experience [5.9 % (±4.7; 95 % CI 6.9/5.0)] was similar to corresponding data obtained by anaesthetists with up to 5 years of clinical experience [7.3 % (±4.8; 95 % CI 8.5/6.1)]. Estimation errors of patients’ SpO2 were not different between these two groups of anaesthetists (p = 0.63).
In line with that, estimation errors of hypoxaemic patients’ SpO2 by nurses demonstrated that clinical experience did not improve the nurses’ ability to correctly assess SpO2 in hypoxaemic patients (p = 0.176). Accordingly, neither of the medical students showed a significant improvement over time concerning their ability to correctly estimate SpO2 in hypoxaemic patients (p = 0.85 and 0.81).
Given these results, it is now evident that medical training and clinical experience do not improve the assessment of patients’ SpO2 and, more importantly, the clinical detection of hypoxaemia under conditions that this study was conducted.
In addition, given that hypoxaemia did not occur less frequently in patients anaesthetised by more experienced colleagues compared to those with less experience (see Fig. 2) results of this study strongly emphasize that the findings of this study may be relevant for both inexperienced and experienced anaesthetists.
4.1 Use of pulse oximetry and supplementary oxygen outside of Germany
In order to evaluate the clinical relevance of these results outside of Germany it is important to elucidate how pulse oximetry and supplementary oxygen are used in patients breathing spontaneously during transfer from OR to PACU in other countries. Findings of our survey demonstrate that the situation in this respect is not homogeneous in Europe. On the one hand, results of the enquiry in Denmark demonstrated that in the vast majority of hospitals either pulse oximetry, supplemental oxygen, or both are routinely applied to patients. This suggests that the knowledge of the inability to clinically detect hypoxaemia has already been incorporated to a large extent into clinical practice patterns. On the other hand, findings of the non-representative survey among anaesthetists from many other countries (e.g. Austria, Spain and Portugal) demonstrated that pulse oximetry and supplemental oxygen are not applied routinely but rather on request in many hospitals. In these hospitals that apply pulse oximetry and supplementary oxygen only on request, the estimated mean transfer times ranged from 0.5 to 10 min with an average from 3.2 to 4.3 min. These results are similar to the ones we recently obtained in a survey conducted at all German university hospitals [7]. Therefore, results of this study and of our previous study [7] might be relevant for anaesthesia providers in countries like Austria, Portugal and Spain. Results obtained from attendees from the other countries (Belgium, France, Greece, Italy, Lithuania, Poland, Romania, and Slovenia) were less conclusive given the smaller number of participants in the survey. However, even a conservative interpretation of those results suggests that patient transfer from the OR to the PACU (estimated transfer times also ranging from 0.5 to 10 min) without supplemental oxygen and pulse oximetry is not uncommon in these countries. In summary, given the similarities between Germany and many European countries concerning everyday practice of patient transfer from OR to PACU and transfer times it can be assumed that hypoxaemia during transfer from the OR to the PACU also occurs in countries other than Germany.
4.2 Recommendations of national anaesthesia societies
While the use of pulse oximetry during general anaesthesia to prevent hypoxaemia is mandatory throughout Europe according to the official recommendations of the national anaesthesia societies, the situation with respect to recommendations concerning post-anaesthesia care to prevent hypoxaemia during patient transfer to the PACU after general anaesthesia is inconsistent. Examples of that diversity are listed in detail online (supplemental digital content 6).
Taken together, guidelines don’t even exist (e.g. Austria), or (e.g. Germany, Denmark, Holland, Spain; ESA) do not require pulse oximetry or supplemental oxygen (except for the British guidelines) or both in all patients to prevent desaturation and hypoxaemia [11–15]. Hence, everyday practice throughout Europe seems to be by and large in accordance with both the national and the ESA safety guidelines of post-anaesthesia care as the use of pulse oximetry and supplemental oxygen during patient transfer are at the discretion of the anaesthetist, i.e. depending on the individual interpretation of the guidelines by the anaesthetist.
4.3 Patient safety and use of pulse oximetry on request
From a patient’s safety point of view decisions at the discretion of the anaesthetist concerning the use of pulse oximetry and supplemental oxygen are debatable for the following reasons. First, hypoxaemia cannot be predicted reliably despite the identification of risk factors [7]. Second, the detection of hypoxaemia using clinical signs has repeatedly been shown to be extremely unreliable [7, 8, 16]. Third, according to the results of this study, the shortcomings of clinically assessing patients’ SpO2 and more importantly of clinically detecting hypoxaemia are independent of clinical experience as well as medical education. Results also suggest that clinical experience does not result in lower incidences of hypoxaemia (Fig. 2). Finally, according to previous results [7] and results of this work estimated transfer times vary a lot with maxima ranging from 1 to 20 min in those hospitals that apply pulse oximetry and supplemental oxygen on request only. In addition, it cannot be excluded that transfer times take longer than planned in case of unexpected incidents.
4.4 Clinical relevance of transient hypoxaemia
In order to evaluate the impact of our findings on every day clinical work it is important to know if transient hypoxaemias are of any clinical relevance and therefore what the significance of detecting hypoxaemias by means of pulse oximetry is. To date, it is impossible to give an unambiguous answer to these questions.
Systematic reviews that explored the benefits of pulse oximetry for perioperative monitoring [17, 18] came to the conclusion that the value of perioperative monitoring with pulse oximetry is questionable in relation to improved reliable outcomes. However, data analyses were primarily (about 90 % of included patients) based on a study by Moller et al. [19] carried out over 20 years ago at a time when troponin as a marker of myocardial ischemia was not yet available and cardiovascular complications were only defined as angina or ST-segment changes. Therefore, it is not possible to draw any conclusions from this study concerning the incidence of silent myocardial events such as NSTEMI in hypoxaemic patients compared to normoxaemic patients. Moreover, since data collection in the study by Moller et al. [19] was only until the patient was discharged from hospital or the latest to the 7th postoperative day, no conclusions concerning long-term morbidity and mortality could be drawn. A further large prospective randomised study to prove a positive effect of pulse oximetry on the incidence of perioperative complications is very unlikely to be carried out as such a study is considered by most as unethical [20].
Despite the ambiguous evidence concerning a positive impact of pulse oximetry on patient outcome, the following reasons are in favour of considering a non-stop use of pulse oximetry during and after general anaesthesia. It is still unknown what extent of hypoxaemia (determined by the duration and degree of hypoxaemia) is deleterious when considered in relation to the individual condition of a patient. Hence, we cannot rule out that even short lasting drops of SpO2 induce a damage that does not have any immediate measurable negative effect on commonly measured outcome parameters (e.g. admission to ICU) but that cause over time in combination with previous and future deleterious events negative effects on patient outcome.
Therefore, unless transfer times less than 2–3 min can be guaranteed and the patient lungs are mostly denitrogenised, the authors of this study advocate to critically question the use of pulse oximetry and supplemental oxygen on request only. Accordingly, as a consequence of the study results department policies were changed in the authors’ (HA, LE, MB, JH, CA, DR) institution. Portable oxygen tanks are available for every patient transfer from the OR to the PACU following general anaesthesia. Supplemental oxygen is given if orders to the patient to take deep breaths do not result in normoxaemia. If portable pulse oximetry is not available supplemental oxygen is mandatory.
4.5 Limitations
A drawback to this study is that the methodology to carry out the survey was not consistent even though the same tool (questionnaire) was used for every participant. However, it is important to realize that the main purpose of conducting a survey was not to get a representative picture of how patient transfer from OR to PACU is done in all European countries, but rather to assess whether there is evidence that use of pulse oximetry and supplemental oxygen only on request in selected patients for transfer to PACU is constrained to Germany alone. The Netherlands and Denmark were chosen for practical reasons with authors of this study working in these countries. According to experience from a previous study [7], the rate of replies to questionnaires is increased when contacting participants directly and individually instead of sending questionnaires to participants without addressing them individually. Also for practical reasons, the survey among attendees of the Euroanaesthesia 2013 Meeting was conducted as an interview (using the same questionnaire that was used in the Netherlands and Denmark) in order to be able to contact anaesthesia providers from many European countries in person. Compared to simply filling in a questionnaire without any assistance the interview has the advantage of giving the interviewer the chance to clarify questions that are difficult to understand for the interviewee and to double-check on answers to make sure they are authentic. In particular the latter seems to be an important point as many interviewees answered they would use pulse oximetry or oxygen routinely. However, when asked explicitly, if this is really the case in every patient, the answer was corrected.
The authors are aware that the way the survey was carried out at the Euroanaesthesia 2013 meeting is not a suitable instrument to yield representative results. However, bearing the main purpose of the survey in mind, interviewing attendees of the meeting appears to be an adequate tool. In fact, the authors are convinced that the results of the interviews carried out at the Euroanaesthesia meeting may be more authentic than answers to questionnaires sent out (e.g. to heads of anaesthesia departments) as the latter might reflect the official local standards of care which may not always be in accordance with what anaesthetists really do in everyday practice [21, 22].
Even though FiO2 was changed to 1.0 in every patient we did not record the resulting FeO2 when the airway was removed and, therefore, couldn’t investigate any correlation between FeO2 and hypoxaemia. In addition, the exact time between removal of the airway and measurement of SpO2 was not recorded. Likewise, the exact waiting time in patients who had to wait at the mechanical transfer table resulting in a significant increase in the total transfer time was not recorded either. Presumably, results of this study would be more conclusive if the exact time between removal of the airway and measurement of SpO2 as well as the exact FeO2 at removal of the airway had been recorded. Analysis of such data might have enabled to justify what patients can be safely transferred to PACU without pulse oximetry and or supplemental oxygen.
A major shortcoming of this study are the suboptimal lighting conditions in the area where the assessments took place. According to Australian standards only lamps that have a cyanosis observation index (COI) below 3.3 and a correlated colour temperature (CCT) between 3,200 and 5,500 K are suitable for the reliable detection of cyanosis [23]. Osram L38W-840 have a COI of 15.2 and a CCT of 4000. Therefore, the lamps used in this study do not meet the Australian standards for a reliable clinical detection of cyanosis. Consequently, we cannot rule out that clinical experience will result in a better detection of cyanosis under optimal lighting (e.g. natural sun light). However, according to Midolo and Sergeyeva [23], earlier work by Dain and Hood [24] suggested that light sources, which will allow the reliable detection of cyanosis should have an appropriate power output in the red part of the visible range, particularly around 660 nm where the maximum difference in spectral absorption between oxyhaemoglobin and de-oxyhaemoglobin occurs. It was concluded, that a patient’s skin colour may appear darker and therefore the patient may be misdiagnosed with cyanosis if the output is too low. Accordingly, many of the patients of our study should have been misdiagnosed as cyanosed. Interestingly, this was not the case at all. In fact, many patients with hypoxaemia were assessed as being normoxaemic. Regardless of these inconsistencies, findings of this study clearly demonstrate that greater clinical experience does not result in a better clinical observation of cyanosis that might be concealed by suboptimal lighting. We don’t know how common the use of the lamps is that we use (and the many other lamps that don’t have a COI < 3.3 either). However, we assume that our institution is not the only one where lighting does not meet the Australian standards. Consequently the questions arise how well the COI of the different lighting systems is known among anaesthesia care providers and how familiar are those who know about the COI with the lighting of the place they work at in order to make a decision whether it is safe to monitor patient’s oxygenation by looking for cyanosis.
Accordingly, considering above limitations of the observational study, one could argue that results of this study are irrelevant. However, it is important to realise that factors such as anaemia (which makes cyanosis less unlikely to develop) and lighting in the OR and the PACU are usually not taken into consideration when making the decision not to use pulse oximetry and oxygen for patient transfer. Instead, such a decision is rather based on the opinion that it is safe to do so which is in part founded on the view one would detect if the patient’s oxygenation is insufficient. Therefore, the results of this observational study in combination with the results of the survey clearly reveal the failure to implement principles of respiratory physiology into clinical practice.
5 Conclusion
In the immediate post-anaesthesia period including transfer from OR to PACU the use of pulse oximetry in all patients to detect hypoxaemia is considered advantageous for patient safety. Oxygen should be applied immediately in hypoxaemic patients (if prompts to take deep breaths do not result in normoxaemia) as long as any negative effects of transient hypoxaemias on patient outcome cannot be ruled out.
Abbreviations
- AAGBI:
-
Association of Anaesthetists of Great Britain and Ireland
- ASA:
-
ASA physical status classification system (based on ASA = American Society of Anesthesiologists)
- AZ:
-
“Aktenzeichen” (file-number)
- BMI:
-
Body mass index
- CI:
-
Confidence interval
- ESA:
-
European Society of Anaesthesiology
- FiO2 :
-
Inspired oxygen fraction
- FeO2 :
-
Expired oxygen fraction
- ICU:
-
Intermediate care unit
- MH:
-
Major hospital
- N2O:
-
Nitrous oxide
- OR:
-
Operating room
- PACU:
-
Post-anaesthesia care unit
- P all:
-
Pulse oximetry is used in all patients
- P on request:
-
Pulse oximetry is used on request only
- SD:
-
Standard deviation
- SpO2 :
-
Saturation of hemoglobin with oxygen as measured by pulse oximetry
- TIVA:
-
Total intravenous anaesthesia
- UH:
-
University hospital
References
Tinker JH, Dull DL, Caplan RA, Ward RJ, Cheney FW. Role of monitoring devices in prevention of anesthetic mishaps: a closed claims analysis. Anesthesiology. 1989;71:541–6.
Cheney FW, Posner KL, Lee LA, Caplan RA, Domino KB. Trends in anesthesia-related death and brain damage: a closed claims analysis. Anesthesiology. 2006;105:1081–6.
Bass JL, Corwin M, Gozal D, Moore C, Nishida H, Parker S, Schonwald A, Wilker RE, Stehle S, Kinane TB. The effect of chronic or intermittent hypoxia on cognition in childhood: a review of the evidence. Pediatrics. 2004;114:805–16 Review.
Kazan R, Bracco D, Hemmerling TM. Reduced cerebral oxygen saturation measured by absolute cerebral oximetry during thoracic surgery correlates with postoperative complications. Br J Anaesth. 2009;103:811–6.
Birks RJS, McNicol LR, Chambers AW, Sawyer RS, Cartwright DP, Adams AP, Aitkenhead A, Morgan M, Wallace PGM, Wilkinson DJ, Ballance JHW, Buckland RW, Harmer M (2000) Recommendations for standards of monitoring during anaesthesia and recovery: AAGBI guidelines 2000: http://www.aagbi.org/sites/default/files/monitoring00.pdf. Accessed September 2013.
Richtlinie der Deutschen Gesellschaft für Anästhesiologie und Intensivmedizin: Ausstattung des anästhesiologischen Arbeitsplatzes. (Directive of the German Society of Anaesthesiology and Intensive Care Medicine: Required features of the anesthesia workplace.) (1995) Anaesth Intensivmed 36:250–254.
Aust H, Eberhart LH, Kranke P, Arndt C, Bleimüller C, Zoremba M, Rüsch D. Hypoxemia after general anesthesia. Anaesthesist. 2012;61:299–309.
Moller JT, Wittrup M, Johansen SH. Hypoxemia in the postanesthesia care unit: an observer study. Anesthesiology. 1990;73:890–5.
Moller JT, Johannessen NW, Berg H, Espersen K, Larsen LE. Hypoxaemia during anaesthesia—an observer study. Br J Anaesth. 1991;66:437–644.
Daley MD, Norman PH, Colmenares ME, Sandler AN. Hypoxaemia in adults in the post-anaesthesia care unit. Can J Anaesth. 1991;38:740–6.
Empfehlungen zur Überwachung nach Anästhesieverfahren. (Recommendations for monitoring of anesthetic procedures.) (2009) Anästh Intensivmed 50:485–488.
REKOMMANDATION FOR OVERVÅGNING EFTER ANÆSTESI 2012. (Recommendation for Monitoring for Anaesthesia 2012). http://dasaim.dk/images/stories/PDF/Rekommendationer/REKOMMANDATION_OVERVAGNING_EFTER_ANSTESI_2012_FINAL_170412.pdf. Accessed Sept 2013.
Verenigingsstandpunten; Richtlijnen - Nederlandse Vereniging voor Anesthesiologie. (Positions; Guidelines - DutchSociety of Anaesthesiologists). http://www.anesthesiologie.nl/kwaliteit/verenigingsstandpunt/verkoeverperiode-en-de-inrichting-en-de-organisatie-van-de-verkoeverafdeling. Accessed Sept 2013.
Vimlatia L, Gilsanzb F, Goldikc Z. Quality and safety guidelines of postanaesthesia care: working party on post anaesthesia care. Eur J Anaesthesiol. 2009;26:715–21.
Rowbotham DJ et al (2002) Immediate Postanaesthetic recovery. Recommendations of the Association of Anaesthesists of Great Britain and Ireland (Chap. 4): page 6 Published by: The Association of Anaesthetists of Great Britain and Ireland, 21 Portland Place, London W1B 1PY; Website: www.aagbi.org.
Meiklejohn BH, Smith G, Elling AE, Hindocha N. Arterial oxygen desaturation during postoperative transportation: the influence of operation site. Anaesthesia. 1987;42:1313–5.
Pedersen T, Dyrlund Pedersen B, Moller AM. Pulse oximetry for perioperative monitoring. Cochrane Database Syst Rev. 2003;3:CD002013.
Pedersen T, Moller AM, Hovhannisyan K. Pulse oximetry for perioperative monitoring. Cochrane Database Syst Rev. 2009;4:CD002013.
Moller JT, Johannessen NW, Espersen K, Ravlo O, Pedersen BD, Jensen PF, Rasmussen NH, Rasmussen LS, Pedersen T, Cooper JB, et al. Randomized evaluation of pulse oximetry in 20, 802 patients: II. Perioperative events and postoperative complications. Anesthesiology. 1993;78:445–53.
Birks RJS, Gemmell LW, O’Sullivan EP, Rowbotham DJ, Sneyd JR Standards of Monitoring during Anaesthesia and Recovery—The Association of Anaesthetists of Great Britain and Ireland: 4th Edition. http://www.aagbi.org/sites/default/files/standardsofmonitoring07.pdf. Accessed Sept 2013.
Aust H, Veltum B, Wächtershäuser T, Eberhart L, Wulf H, Rüsch D. On preoperative risk evaluation of adult patients before elective non-cardiac surgery: results of a survey on clinical practice in the Federal State of Hessen. Anaesthesist. 2013;62:365–79.
Böhmer AB, Defosse J, Geldner G, Mertens E, Zwissler B, Wappler F. Preoperative risk evaluation of adult patients for elective, noncardiac surgical interventions. Results of an on-line survey on the status in Germany. Anaesthesist. 2012;61:407–19.
Midolo NA, Sergeyeva L. Lighting for clinical observation of cyanosis. Aust Hosp Eng. 2007;30(2):38–46.
Dain SJ, Hood JW (1997) Lighting for cyanosis identification. In: Conference proceedings IES convention.
Acknowledgments
The authors thank all the colleagues in Denmark, the Netherlands, and at the 2013 Euroanaesthesia meeting who took part in the study and thereby helped to obtain important data for this study. The authors also thank all staff from Marburg university hospital, department of anaesthesia who helped to acquire data for the observational part of this study.
Conflict of interest
All authors declare that they have no conflict of interest.
Ethical standard
The study complies with the current laws of the country in which it was performed.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
10877_2014_9620_MOESM6_ESM.doc
doc-document (Examples of recommendations concerning the use of pulse oximetry and supplemental oxygen in selected European countries) (DOC 24 kb)
Rights and permissions
About this article
Cite this article
Aust, H., Kranke, P., Eberhart, L.H.J. et al. Impact of medical training and clinical experience on the assessment of oxygenation and hypoxaemia after general anaesthesia: an observational study. J Clin Monit Comput 29, 415–426 (2015). https://doi.org/10.1007/s10877-014-9620-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-014-9620-4