Abstract
Purpose
Cardiologists are among the health professionals that are most exposed to ionizing radiation, but there is no study comparing the level of exposure of physicians during different electrophysiology procedures. We aimed to measure and compare cardiologists’ exposure to radiation during different electrophysiology procedures.
Methods
The study population comprised all electrophysiology procedures performed over a 6-month period in a large referral centre. The endpoint was operator radiation exposure, assessed using a personal electronic dosimeter located on the operator’s left arm.
Results
In total, 150 electrophysiology procedures were analyzed. Compared with electrophysiology studies (reference category), physician radiation exposure was 3-fold greater during ablation of atrial fibrillation, 9-fold greater during ablation of atrioventricular nodal reentrant tachycardia (AVNRT)/atrioventricular reentrant tachycardia (AVNT), and 10-fold greater during ablation of atrial flutter (p < 0.001). Physician exposure was mainly related to X-ray time (R2 = 0.28).
Conclusions
Our study showed significant differences in cardiologists’ exposure to ionizing radiation depending on the type of electrophysiology procedure. Atrial flutter and AVNRT/AVNT ablations are the procedures in which operators are most exposed to ionizing radiation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Cardiologists are among the health professionals that are most exposed to ionizing radiation [1]. Recent publications have suggested that through deterministic effects, there may be an increased risk of radiation-induced cataracts in personnel working in catheterisation laboratories (cathlabs) [2,3,4,5], while stochastic effects may contribute to an increased frequency of left-hemisphere brain tumours in this population [6].
Radiation exposure of physicians working in cathlabs has been studied in the past, with a reported mean dose per procedure of 2 to 7 μSv [7]. In the field of electrophysiology, patient exposure has previously been studied [8,9,10,11], but the only available data regarding operator exposure are either outdated [12,13,14], or in vitro data (anthropomorphic phantom) [15]. To the best of our knowledge, there is no study comparing the level of exposure of physicians during different electrophysiology procedures.
The aim of our study was thus to measure and compare operator exposure to radiation during different types of electrophysiology procedure.
2 Methods
2.1 Study population
This was a prospective, analytical, epidemiological single-centre cohort study carried out in a large university hospital in France. The population for analysis included all consecutive electrophysiology procedures performed in our centre from November 2017 to May 2018. Diagnostic electrophysiology studies and radiofrequency ablation procedures (atrioventricular nodal reentrant tachycardia (AVNRT), atrioventricular reentrant tachycardia (AVRT), common atrial flutter and atrial fibrillation) were included. Atrioventricular node and ventricular tachycardia ablations were not included because of the small number of procedures.
2.2 Electrophysiology procedures
During electrophysiology procedures, 1 to 3 venous femoral sheaths of 6 to 8.5 Fr were implanted. Electrophysiology studies, AVNRT, AVNT and flutter ablations were performed under local anaesthesia without electroanatomical mapping. Atrial fibrillation ablation procedures were preceded by a cardiac angio-CT to use the CARTO 3 software (Biosense Webster, Johnson & Johnson, Irvine, CA, USA). They were performed under general anaesthesia, and trans-septal puncture was performed under trans-oesophageal echocardiographic and fluoroscopic control.
Three cardiologists with 8 or more years’ experience in electrophysiology and who were permanent, full-time practitioners in the Department during the study period performed the procedures in a single electrophysiology laboratory, equipped with the Arcadis Avantic system (Siemens Healthcare, Erlangen, Germany), in service since January 2011, with an image intensifier with a frame rate of 4 fps, and 33 cm size of field. The equipment undergoes half-yearly control by the manufacturer, and annual external quality control. The electrophysiology laboratory is equipped with lead screens and table drapes with 0.5-mm Pb equivalent used consistently. All operators wear a leaded apron and a thyroid shield with 0.5-mm Pb equivalent. They also have a passive dosimeter with quarterly statements (Landauer, Glenwood, USA) and an active dosimeter (APVL, Saint-Cyr-sur-Loire, France). A nurse was present for all procedures.
2.3 Endpoints
The primary endpoint was cardiologist radiation exposure, as assessed using personal electronic dosimeters (APVL, Saint-Cyr-sur-Loire, France) with a silicon diode (μSv) located on the operator’s left arm outside the apron (Fig. 1) in order to optimise angular response, with the ideal position placing the dosimeter at an angle of 0° in relation to the radiation source, namely, the patient’s body in this instance [16]. The dosimeter has an energy response between 15 keV and 1.5 MeV and a dose range displayed from 0 to 9999 mSv in increments of 0.1 μSv. Radiation doses were recorded at the end of each procedure. This measurement corresponds to the dose received at 10 mm under the site of the dosimeter (HP10), and represents the probability of stochastic health effects from radiation.
Patient radiation exposure was assessed by dose area product (DAP), as measured by an ionisation chamber on the radiology apparatus. DAP is related to the overall patient body dose for standard patient geometry (stochastic risk) [17, 18]. Other variables recorded were x-ray time, patient body mass index (BMI) and age and sex of the patient. Data were obtained using the Dosimetric Archiving and Communication System (DACS) Radiation Dose Monitor (Medsquare, Paris, France). All patients have given, at the time of their hospitalisation, their informed consent for an anonymous retrospective use of their medical data.
2.4 Statistical analyses
Quantitative variables are described as median and (interquartile range) and qualitative variables as number (percentage). Quantitative variables were compared using the Kruskal–Wallis test. Qualitative variables were compared using Fisher’s exact or the chi-square test as appropriate. Relations between quantitative variables were investigated using simple linear regression. Analyses were performed using SPSS version 21 (IBM SPSS Statistics, Chicago, USA). A p value < 0.05 was considered statistically significant; all tests were bilateral.
3 Results
During the study period, 150 electrophysiology procedures were included, namely, 29 electrophysiology studies, 46 atrial fibrillation ablations, 47 common atrial flutter ablations, 15 AVNRT ablations and 13 AVRT ablations.
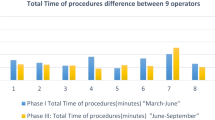
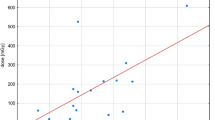
Characteristics of the procedures are shown in Table 1. Radiation exposure of operators and patients (as assessed by DAP) differed significantly according to the electrophysiology procedure (p < 0.001). Compared to electrophysiology studies, median physician radiation exposure was 3-fold greater during ablation of atrial fibrillation, 9-fold greater during ablation of AVNRT/AVNT and 10-fold greater during ablation of atrial flutter (Fig. 2). Median DAP was 3-fold higher during atrial fibrillation ablations, 5-fold higher during atrial flutter and 6-fold greater AVNRT and AVNT ablations (Fig. 3). Median X-ray time and BMI were on average 13.6 min and 28.1 kg/m2 during atrial flutter ablations and 21.3 min and 23.8 kg/m2 during AVNRT and AVNT ablations.
Both physician radiation exposure and dose area product were strongly related to X-ray time (R2 = 0.28 and R2 = 0.55 respectively).
4 Discussion
4.1 Operator radiation exposure
Our study found significant differences in cardiologists’ exposure to ionizing radiation depending on the type of procedure, and this variability is directly related to changes in X-ray time. Operators are significantly more exposed during ablation procedures, with the exception of atrial fibrillation ablation procedures in which X-ray time is low thanks to mapping systems.
We recently demonstrated with the same methodology that the average exposure of cardiologists to radiation in the cathlab ranged from 2 to 7 μSv per procedure, for an average X-ray time of 8 min [7], whereas in the present study, median exposure of cardiologists working in the electrophysiology laboratory ranged from 1 to 10 μSv, depending on the type of procedure. Operator exposure therefore appears to be similar in electrophysiology than in the cathlab.
4.2 Patient radiation exposure
The exposure of patients undergoing an electrophysiology procedure also varies significantly depending on the type of procedure, in the same manner as operator exposure. This is unsurprising, since the main source of operator exposure is the scattered radiation from the patient [17, 19]. In the cathlab, patients are exposed to a radiation dose ranging from 1900 to 3300 cGy cm2 [20], while in the present study, we found that patients were exposed to a median dose ranging from 148 to 884 cGy cm2. Patient exposure to radiation therefore seems to be considerably lower in the electrophysiology laboratory than in the cathlab, although operator exposure is similar. This could be explained by greater awareness among interventional cardiologists as compared to rhythmologists about the rules for reduce the dose of radiation (increasing table height at maximum, optimizing source-to-image distance, use of low frame rate, use of collimation and contour filters) and protecting against scattered radiation from patient (optimizing the use of lead screens and table drapes) [18], as reflected by the low number of publications pertaining to X-ray exposure of operators in the electrophysiology laboratory compared to the catheterisation laboratory.
4.3 Atrial flutter and AVNRT/AVNT ablation procedures
Surprisingly, operator exposure was similar during AVNRT/AVNT ablations and atrial flutter ablations, whereas the median X-ray time was 57% higher during AVNRT/AVNT ablations. This could be explained by the fact that median BMI of patients with AVNRT/AVNT ablations was 23.8 kg/m2 versus 28.1 kg/m2 for patients with atrial flutter ablation. Indeed, BMI is an important determinant of scattered radiation [18], and the main source of exposure for cardiologists is radiation scattered from the patient [17, 19]. In addition, the left anterior oblique (LAO) incidence is mostly used during atrial flutter ablation, and this incidence is known to be the most irradiating [18].
4.4 Study limitations
Our study has some limitations, namely, the single-centre design and the relatively low number of procedures. However, these findings are original and relevant since, to the best of our knowledge, there are no recent data on operator exposure to ionizing radiation in the electrophysiology laboratory, collected using a methodology that has already been proven to be valid.
Our study showed significant differences in cardiologists’ exposure to ionizing radiation depending on the type of electrophysiology procedure, and this is during ablation of atrial flutter and AVNRT/AVNT that operators are the most exposed.
Despite a considerably lower patient exposure to radiation in the electrophysiology laboratory than in the cathlab, operator exposure appears to be similar. It will therefore be necessary to reduce operator exposure in the future, and to this end, to develop new technologies as well as optimizing radiation protection practices in the electrophysiology laboratory.
References
Rehani MM, Ortiz-Lopez P. Radiation effects in fluoroscopically guided cardiac interventions—keeping them under control. Int J Cardiol. 2006;109:147–51. https://doi.org/10.1016/j.ijcard.2005.06.015.
Ciraj-Bjelac O, Rehani MM, Sim KH, Liew HB, Vano E, Kleiman NJ. Risk for radiation-induced cataract for staff in interventional cardiology: is there reason for concern? Catheter Cardiovasc Interv. 2010;76:826–34. https://doi.org/10.1002/ccd.22670.
Elmaraezy A, Ebraheem Morra M, Tarek Mohammed A, Al-Habaa A, Elgebaly A, Abdelmotaleb Ghazy A, et al. Risk of cataract among interventional cardiologists and catheterization lab staff: a systematic review and meta-analysis. Catheter Cardiovasc Interv. 2017;90:1–9. https://doi.org/10.1002/ccd.27114.
Brown NP. The lens is more sensitive to radiation that we had believed. Br J Ophtalmol. 1997;81:257.
Vano E, Gonzalez L, Fernandez JM, Haskal ZJ. Eye lens exposure to radiation in interventional suites: caution is warranted. Radiology. 2008;248:945–53. https://doi.org/10.1148/radiol.2482071800.
Roguin A, Goldstein J, Bar O. Brain tumours among interventional cardiologists: a cause for alarm? Report of four new cases from two cities and a review of the litterature. EuroIntervention. 2012;7:1081–6. https://doi.org/10.4244/EIJV7I9A172.
Faroux L, Blanpain T, Nazeyrollas P, Tassan-Mangina S, Heroguelle V, Tourneux C, et al. Effect of modern dose-reduction technology on the exposure of interventional cardiologists to radiation in the catheterization laboratory. J Am Coll Cardiol Interv. 2018;11:222–3. https://doi.org/10.1016/j.jcin.2017.10.022.
Perisinakis K, Damilakis J, Tcheocharopoulos N, Manios E, Vardas P, Gourtsoyiannis N. Accurate assessment of patient effective radiation dose and associated detriment risk from radiofrequency catheter ablation procedures. Circulation. 2001;104:58–62.
Nof E, Lane C, Cazalas M, Cuchet-Soubelet E, Michaud GF, John RM, et al. Reducing radiation exposure in the electrophysiology laboratory: it is more than just fluoroscopy times! Pacing Clin Electrophysiol. 2015;38:136–45. https://doi.org/10.1111/pace.12544.
Sciahbasi A, Ferrante G, Fischetti D, Milin DJ, Sarandrea A, Schirripa V, et al. Radiation dose among different cardiac and vascular invasive procedures: the RODEO study. Int J Cardiol. 2017;240:92–6. https://doi.org/10.1016/j.ijcard.2017.03.031.
Casella M, Dello Russo A, Russo E, Catto V, Pizzamiglio F, Zucchetti M, et al. X-ray exposure in cardiac eletrophysiology: a retrospective analysis in 8150 patients over 7 years of activity in a modern, large-volume laboratory. J Am Heart Assoc. 2018;7:e008233. https://doi.org/10.1161/JAHA.117.008233.
Calkins H, Niklason L, Sousa J, El-Atassi R, Langberg J, Morday F. Radiation exposure during radiofrequency catheter ablation of accessory atrioventricular connections. Circulation. 1991;84:2376–82.
Macle L, Weerasooriya R, Jais P, Scavee C, Raybaud F, Choi KJ, et al. Radiation exposure during radiofrequency catheter ablation for atrial fibrillation. Pacing Clin Electrophysiol. 2003;26:288–91.
Efstathopoulos EP, Katritsis DG, Kottou S, Kalivas N, Tzanalaridou E, Giazitzoglou E, et al. Patient and staff radiation dosimetry during cardiac electrophysiology studies and catheter ablation procedures: a comprehensive analysis. Europace. 2006;8:443–8. https://doi.org/10.1093/europace/eul041.
Teocharopoulous N, Damilakis J, Perisinakis K, Manios E, Vardas P, Gourtsoyiannis N. Occupational exposure in the electrophysiology laboratory: quantifying and minimizing radiation burden. Br J Radiol. 2006;79:644–51. https://doi.org/10.1259/bjr/76128583.
Brasselet C, Blanpain T, Tassan-Mangina S, Deschildre A, Duval S, Vitry F, et al. Comparison of operator radiation exposure with optimized radiation protection devices during coronary angiograms and ad hoc percutaneous coronary interventions by radial and femoral routes. Eur Heart J. 2008;29:63–70. https://doi.org/10.1093/eurheartj/ehm508.
Agarwal S, Parashar A, Bajaj NS, Khan I, Ahmad I, Heypler FA Jr, et al. Relationship of beam angulation and radiation exposure in the cardiac catheterization laboratory. J Am Coll Cardiol Intv. 2014;7:558–66. https://doi.org/10.1016/j.jcin.2013.12.203.
Hirshfeld JW, Ferrari VA, Bengel FM, Bergersen L, Chambers CE, Einstein AJ, et al. ACC//HRS/NASCI/SCAI/SCCT expert consensus document on optimal use of ionizing radiation in cardiovascular imaging: best practices for safety and effectiveness: a report of the American College of Cardiology Task Force on Expert Consensus Decision Pathways. J Am Coll Cardiol. 2018;71:e283–351. https://doi.org/10.1016/j.jacc.2018.02.016.
Christopoulos G, Makke L, Christakopoulos G, Kotsia A, Rangan BV, Roesle M, et al. Optimizing radiation safety in the cardiac catheterization laboratory: a practical approach. Catheter Cardiovasc Interv. 2016;87:291–301. https://doi.org/10.1002/ccd.25959.
Faroux L, Blanpain T, Nazeyrollas P, Tassan-Mangina S, Herce B, Tourneux C, et al. Minimizing exposure to radiation in invasive cardiology using modern dose-reduction technology: evaluation of the real life effects. Catheter Cardiovasc Interv. 2018;91:1194–999. https://doi.org/10.1002/ccd.27245.
Acknowledgements
The authors would like to thank Camille Bardoux, Mélanie François, Annie Godebert, Aude Turban and Karine Deschars for their invaluable aid with data collection.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Informed consent
All patients have given, at the time of their hospitalisation, their informed consent for an anonymous retrospective use of their medical data.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Faroux, L., Daval, C., Lesaffre, F. et al. Physicians’ exposure to radiation during electrophysiology procedures. J Interv Card Electrophysiol 55, 233–237 (2019). https://doi.org/10.1007/s10840-019-00568-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-019-00568-1