Abstract
Purpose
To investigate the correlation between hysteroscopic findings of chronic endometritis and CD138 immunohistochemistry positive in endometritis and to analyze the pregnancy outcomes and associated risk factors following embryo transfer in women diagnosed with chronic endometritis via hysteroscopy.
Methods
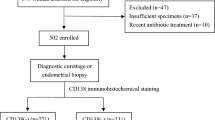
A retrospective observational study carried out at the Reproductive Medicine Center of Tangdu Hospital of Air Force Medical University, from January 2021 to December 2021, was performed by obtaining data from 194 medical records of women who underwent hysteroscopies for infertility and were diagnosed with chronic endometritis based on Delphi criteria. Spearman correlation analysis was used to evaluate the correlation between hysteroscopic findings and endometrial CD138 immunohistochemistry. The study also observed the differences in relevant indexes between the CD138-positive and CD138-negative groups after embryo transfer and analyzed factors influencing implantation failure using logistic regression analysis.
Results
The correlation analysis between hysteroscopic findings and CD138 immunohistochemistry showed that micropolyps were correlated with CD138 immunohistochemistry positivity. The correlation coefficient was 0.32 (P < 0.01). After embryo transfer, the clinical pregnancy rate of the CD138-positive group was lower compared to that of the CD138-negative group [64.79% (46/71) vs. 81.30% (100/123), P < 0.05]. The results of the multivariate logistic regression analysis revealed that age (P = 0.43) and CD138 immunohistochemistry positivity (P = 0.008) were the independent risk factors for predicting whether or not embryo implantation was successful.
Conclusion
Hysteroscopic findings do not correlate strongly with endometrial CD138 immunohistochemistry, and chronic endometritis cannot be diagnosed by hysteroscopy alone. CD138 immunohistochemistry positivity is an independent factor contributing to the decrease in clinical pregnancy rate following embryo transfer.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Chronic endometritis (CE) is a persistent, focal, or diffuse inflammation of the endometrium, characterized by plasma cells penetrating the endometrial stroma [1]. CE is often asymptomatic or mild, such as abnormal uterine bleeding (AUB), pelvic discomfort, dyspareunia, and leucorrhea, making it easy to overlook the diagnosis of the disease in the clinic. In recent years, there has been increasing evidence suggesting that CE is associated with poor reproductive outcomes [2, 3], such as infertility, repeated implantation failure (RIF), and recurrent pregnancy loss (RPL). CE has gained increasing attention in reproductive medicine, and the treatment of CE can improve patients’ pregnancy outcomes; oral antibiotics are commonly used to treat CE [4, 5]. To date, numerous studies on CE have been published; however, there is no consensus regarding diagnostic criteria for CE, which is mostly diagnosed via hysteroscopy, endometrial biopsy, and microbial detection. Clinically, the diagnosis generally relies on identifying endometrial stromal plasma cells using two methodologies: hematoxylin and eosin (HE) staining and immunohistochemistry (IHC) staining for plasma cell-specific surface antigen CD138. Recent studies have shown that CD138 immunohistochemistry positivity has a high sensitivity for the diagnosis of CE [6]. The sensitivity of the diagnosis of CE via hysteroscopy may be dependent upon the physician’s experience [5, 7]. Bacterial culture is limited in clinical practice due to its long-time requirement, high false-positive rate, and susceptibility to contamination by vaginal secretions.
Materials and methods
Study population and study design
This was a retrospective study conducted between January 2021 and December 2021; the study collected the medical records of 194 patients who underwent hysteroscopies for infertility at the Reproductive Medicine Center of Tangdu Hospital, Air Force Medical University. These patients were diagnosed with CE based on Delphi criteria, which include strawberry aspect, focal hyperemia, hemorrhagic spots, micropolyps, and stromal edema (see Figs. 1, 2, 3, and 4). In this study, all patients were diagnosed with CE by hysteroscopy and at least 5 CD138-positive cells in one HPF were visible in the endometrial stroma as the diagnostic criteria for CE. This study was approved by the Ethics Committee of Tangdu Hospital of Air Force Medical University (Assigned No. TDLL-202403–05).
Data collection
Patients were retrospectively identified by querying the Tangdu Hospital electronic medical record system using the search term “chronic endometritis” (we used the Delphi standard to record patients with chronic endometritis in the electronic medical record system). The inclusion criteria were (1) infertile woman; (2) age 20 to 45 years; (3) in vitro fertilization and embryo transfer (IVF-ET)/intracytoplasmic sperm injection (ICSI) for fertility treatment; (4) complete preservation of hysteroscopic pictures and other clinical data; and (5) patients with hysteroscopy and endometrial biopsy signed informed consent. Exclusion criteria were (1) uterine adhesions; (2) congenital malformations of the uterus (unicornuate uterus, septate uterus, etc.); (3) untreated thyroid dysfunction, hyperprolactinemia, diabetes, etc.; (4) pelvic or genital tuberculosis; (5) chromosomal abnormalities in either male or female; (6) in preimplantation genetic testing (PGT) for fertility treatment; and (7) combined with submucosal myoma.
The patient underwent hysteroscopy under non-anesthesia at the Reproductive Medicine Clinic of Tangdu Hospital between 3 and 7 days after menstruation. The hysteroscopy and diagnosis were conducted by experienced medical professionals. The hysteroscopic outer sheath had a diameter of 4.5 mm, and 0.9% sodium chloride solution was used as the dilatation medium (a pressure between 80 and 110 mmHg and a flow rate between 100 and 200 mmHg). After hysteroscopy, a metal curette was used to obtain endometrial tissue for pathology. The specimens were fixed with formaldehyde solution and sent for HE staining and CD138 immunohistochemistry.
Referring to the diagnostic criteria in previous literature [8, 9], the diagnostic criteria for CE of hysteroscopy were mainly based on the Delphi standard in 2019: (1) endometrial strawberry aspect; (2) endometrial focal hyperemia; (3) endometrial hemorrhagic spots; (4) endometrial micropolyps; and (5) thick and pale appearance of the endometrium in the follicular phase owing to stromal edema (a normal finding during the secretory phase). Histopathological diagnostic criteria [10]: we used at least five CD138 + cells in the endometrial stroma per 400 × magnification as the criteria, and an experienced histopathologist examined the pathological findings. Patients with CD138 + endometrial biopsy were given doxycycline hydrochloride (100 mg, Bid, 14 days). Repeat hysteroscopy and endometrial biopsy between 3 and 7 days after menstruation, if CD138 remained positive, received metronidazole (500 mg, Bid, 14 days) and levofloxacin (200 mg, Bid, 14 days). Repeat hysteroscopy and endometrial biopsy between 3 and 7 days after menstruation, if CD138 remained positive, received azithromycin (500 mg, Bid, 14 days). All patients were treated with IVF-ET/ICSI for fertility treatment; blood HCG levels were checked on the 13th day after embryo transfer. If HCG levels were greater than 5 U/L, the implantation was considered successful. Intrauterine pregnancy confirmed by transvaginal ultrasound 42 days after embryo transfer was considered clinical pregnancy. According to this criterion, patients can be divided into the clinical pregnancy group and the non-pregnancy group.
Statistical analysis
SPSS v.23.0 software was used for statistical analysis. Normally distributed measurements were expressed as mean ± standard deviation (\(\overline{X}\pm S\)), and independent samples t-test was used for comparison between groups; count data were presented as frequency and constitutive ratios and the chi-square test was used for comparison between groups; the correlation between hysteroscopic findings and CD138 results was expressed using Spearman’s correlation coefficient; independent risk factors were screened using univariate and multivariate logistic regression analysis. Statistical significance for all tests was based on a P value < 0.05.
Result
The patients had an average age of 30.81 ± 3.72 years, an average BMI of 22.07 ± 2.91 kg/m2, and a mean duration of infertility of 3.55 ± 2.48 years (Table 1). Of the 194 patients enrolled, 71 (36.6%) were CD138 positive. Out of 194 patients, 129 had one hysteroscopic finding, 57 had two, and 8 had three. Micropolyps were found in 74 cases, strawberry aspect in 5 cases, focal hyperemia in 140 cases, hemorrhagic spots in 10 cases, and stromal edema in 37 cases. The correlation coefficient between micropolyps and CD138 immunohistochemical positivity was 0.320, which was statistically significant (P < 0.01). There was no significant correlation between the strawberry aspect, focal hyperemia, hemorrhagic spots, stromal edema, and CD138 immunohistochemical positivity (Table 2). It can be seen that endometrial micropolyps are most linked with CD138 immunohistochemical positivity.
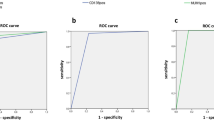
Based on CD138 immunohistochemistry, the patients were divided into CD138-positive and CD138-negative groups. There were no statistically significant differences in age, infertility years, and body mass index (BMI) between the two groups (P > 0.05), indicating comparability (Table 3). After embryo transfer, the clinical pregnancy rate in the CD138-positive group was found to be lower than that in the CD138-negative group (P < 0.05). However, there were no statistically significant differences observed between the two groups in terms of live birth rate, premature birth rate, and abortion rate (P > 0.05) (Table 4). Univariate analysis showed significant differences in age, luteinizing hormone (LH), and CD138 immunohistochemical positivity between the CD138-positive group and the CD138-negative group (P < 0.05). However, there were no significant differences in infertility type, infertility years, body mass index (BMI), anti-Müllerian hormone (AMH), follicle-making hormone (FSH), and hysteroscopic findings of CE (micropolyps, strawberry aspect, focal hyperemia, hemorrhagic spots, and stromal edema) between the two groups (P < 0.05). Age, LH, and CD138 immunohistochemical positivity with statistically significant differences in univariate analysis were included in multivariate logistic regression analysis, and the results showed that age [OR = 0.909, 95%CI (0.829, 0.997), P < 0.05] and CD138 immunohistochemical positivity [OR = 0.392, 95%CI (0.196, 0.784), P < 0.05] were independent risk factors for predicting whether embryo implantation was successful (Table 5).
Discussion
CE can adversely affect the immune microenvironment of endometrial, reduce the endometrial receptive, interfere with fertilized egg implantation and embryo implantation, is not conducive to the maintenance of pregnancy after implantation, and affect the reproductive health of women in their reproductive age. At present, most people believe that CE is mainly induced by intrauterine microbial infection [11]. Studies had conducted bacterial culture or microbial detection on the endometrium of patients with CE, showing that compared with broad-spectrum antibiotic treatment for CE patients with negative microbial culture, the cure rate was significantly improved and pregnancy outcome was improved when specific bacteria were found, and targeted therapy with antibiotics is performed [12, 13]. However, microbiological culture is not widely used in clinical practice due to its long-time requirement, high false-positive rate, and susceptibility to contamination by vaginal secretions.
Currently, there is no consensus on the diagnostic criteria for patients with CE; several domestic and international studies suggest that hysteroscopy combined with CD138 immunohistochemistry is more accurate and comprehensive for diagnosing CE [14]. Nevertheless, due to a lack of consensus on the hysteroscopic finding of CE and the differences in experience among inter-examiners, the accuracy of hysteroscopic diagnosis of CE is different in different studies. Therefore, the establishment of unified diagnostic criteria and the learning of diagnostic criteria can narrow the differences among observers and improve the accuracy of the diagnosis. In 2019, scholars from various countries jointly formulated the diagnostic criteria for CE hysteroscopy, which improved the consistency of clinical CE diagnosis [9]. To study the value of hysteroscopy in diagnosing CE, this paper retrospectively analyzed the correlation between the hysteroscopic findings of CE and the CD138 immunohistochemistry, and further observed the pregnancy outcomes after embryo transfer in both the CD138-positive group and CD138-negative group, analyzed the factors affecting the pregnancy outcomes, and expected to provide evidence-based medical evidence for the diagnosis, treatment, and prognosis of CE. One study showed that [15] hysteroscopic findings did not agree well with histopathological diagnosis. In our study, endometrial conditions were observed under direct vision by hysteroscopy, and HE staining routine histopathological examination combined with CD138 immunohistochemistry was performed by localization biopsy. The results showed that there was only a weak correlation (correlation coefficient of 0.320) between endometrial micropolyps and CD138 immunohistochemistry positivity, while strawberry aspect, focal hyperemia, hemorrhagic spots, and stromal edema were not correlated with CD138 immunohistochemistry positivity. It can be seen that there is a wide variability in the two methodologies. Cicinelli et al. [16, 17] found that endometrial micropolyps under hysteroscopy may be a reliable feature for the diagnosis of CE, and the histological changes were correlated with the results of hysteroscopy [18]. When one or more hysteroscopic findings are present on hysteroscopy, the diagnosis of CE should be vigilant; a concomitant endometrial biopsy should be performed to confirm or negate the diagnosis.
The histological diagnosis of CE is still subjective and may vary among different centers [9]. Although CD138 immunohistochemistry is considered a reliable method for diagnosing CE, recent literature suggests that the technique has some limitations.
Firstly, some studies used different methodologies to quantify CD138-positive cells. Secondly, it should be noted that CD138-positive cells can also be detected in epithelial cells, fibroblasts, and B cells, so CD138-positive cells in endometrial specimens may not always be accurately identified [19]. Additionally, plasma cells can also be found in the endometrium of healthy women without any association with inflammation [20]. Therefore, the results may be different or inconsistent in the same patient. At present, there is a lack of standardized pathological diagnostic criteria. At least 7 histological diagnostic criteria for CE have been reported in the literature. However, there is no agreement on the minimum number of plasma cells required to diagnose CE [21]. The establishment of diagnostic criteria should take into account whether they contribute to improving pregnancy outcomes, and thus the pathological diagnostic criteria for CE should have a strong correlation with pregnancy outcomes to be valuable. The presence of CD138 cells has been found to be associated with the outcomes of embryo transfer in certain studies [22]; however, contrasting findings have been reported by another study [23]. Some studies have indicated that 5 CD138 + cells per 10 HPF are sufficient. This study used at least 5 CD138 + cells in one HPF as a diagnostic criterion. We found that CD138 immunohistochemical positivity was an independent influence on the reduction of the clinical pregnancy rate after embryo transfer, but more studies are needed to further confirm this finding.
The use of stricter diagnostic criteria in this study may reduce the sensitivity, leading to the possibility of missing many cases of CE. As a result, there may be some patients diagnosed by hysteroscopy as CE but with a negative CD138 result, indicating the possibility of false negative cases (only 36.6% of CD138 positive cases were identified in this study). Based on the low concordance rate between hysteroscopic findings and histopathological findings, as well as the limitations of the CD138 technique, it can be speculated that micropolyps and CD138-positive may indicate more severe cases. On the other hand, other findings at hysteroscopy but CD138-negative may be mild or moderate cases. One study showed that embryo transfer after antibiotic treatment in patients with hysteroscopic findings of CE and CD138-negative achieved better clinical pregnancy and full-term live birth rates [24]. Yang et al. came to a similar conclusion [25]. Therefore, we should pay attention to patients with hysteroscopic findings of CE but CD138 negative, which can be appropriately considered for interventional therapy to improve clinical pregnancy rates.
In summary, hysteroscopy, as a diagnostic method for CE, exhibits a certain degree of correlation between hysteroscopic findings and pathological results; however, the correlation is weak. Attention should be paid to the diagnosis of CE when there are characteristic findings in hysteroscopy. This study is a single-center retrospective study, and prospective randomized controlled studies or multi-center clinical trials are needed to further confirm and provide more convincing evidence for the diagnosis and treatment of patients with CE.
Conclusions
Studies on chronic endometritis (CE) and its relation to adverse pregnancy outcomes have been increasing and deepening over time, which has gained significant attention from gynecologists and reproductive doctors. However, the diagnosis rate of CE varies greatly due to variations in diagnostic methods and standards. The current gold standard for diagnosing CE is the detection of plasma cells in the endometrial tissue. Hysteroscopy can improve the detection rate of CE, but it cannot substitute pathology as the gold standard for the diagnosis of CE.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Klimaszyk K, Svarre H, Nielsen, Wender-Ozegowska E, et al. Chronic endometritis - is it time to clarify diagnostic criteria? Ginekol Polska. 2023;94:152–7.
Li J, Li X, Ding J, et al. Analysis of pregnancy outcomes in patients with recurrent implantation failure complicated with chronic endometritis. Front Cell Dev Biol. 2023;11:1088586.
Kitaya K, Tanaka SE, Sakuraba Y, et al. Multi-drug-resistant chronic endometritis in infertile women with repeated implantation failure: trend over the decade and pilot study for third-line oral antibiotic treatment. J Assist Reprod Genet. 2022;39:1839–48.
Xiong Y, Chen Q, Chen C, et al. Impact of oral antibiotic treatment for chronic endometritis on pregnancy outcomes in the following frozen-thawed embryo transfer cycles of infertile women: a cohort study of 640 embryo transfer cycles. Fertil Steril. 2021;116:413–21.
Kimura F, Takebayashi A, Ishida M, et al. Review: chronic endometritis and its effect on reproduction. J Obstet Gynaecol Res. 2019;45:951–60.
Xu Y, Mei J, Diao L, et al. Chronic endometritis and reproductive failure: role of syndecan-1. Am J Reprod Immunol (New York, N.Y. : 1989). 2020;84:e13255.
Cicinelli E, Trojano G, Mastromauro M, et al. Higher prevalence of chronic endometritis in women with endometriosis: a possible etiopathogenetic link. Fertil Steril. 2017;108:289-95.e1.
Liu L, Yang H, Guo Y, et al. The impact of chronic endometritis on endometrial fibrosis and reproductive prognosis in patients with moderate and severe intrauterine adhesions: a prospective cohort study. Fertil Steril. 2019;111:1002-10.e2.
Cicinelli E, Vitagliano A, Kumar A, et al. Unified diagnostic criteria for chronic endometritis at fluid hysteroscopy: proposal and reliability evaluation through an international randomized-controlled observer study. Fertil Steril. 2019;112:162-73.e2.
Bouet PE, El Hachem H, Monceau E, et al. Chronic endometritis in women with recurrent pregnancy loss and recurrent implantation failure: prevalence and role of office hysteroscopy and immunohistochemistry in diagnosis. Fertil Steril. 2016;105:106–10.
Liu Y, Ko EY, Wong KK, et al. Endometrial microbiota in infertile women with and without chronic endometritis as diagnosed using a quantitative and reference range-based method. Fertil Steril. 2019;112:707-17.e1.
Cicinelli E, Matteo M, Trojano G, et al. Chronic endometritis in patients with unexplained infertility: prevalence and effects of antibiotic treatment on spontaneous conception. Am J Reprod Immunol. 2018;79. https://doi.org/10.1111/aji.12782.
Cicinelli E, Matteo M, Tinelli R, et al. Chronic endometritis due to common bacteria is prevalent in women with recurrent miscarriage as confirmed by improved pregnancy outcome after antibiotic treatment. Reprod Sci (Thousand Oaks, Calif). 2014;21:640–7.
Zargar M, Ghafourian M, Nikbakht R, et al. Evaluating chronic endometritis in women with recurrent implantation failure and recurrent pregnancy loss by hysteroscopy and immunohistochemistry. J Minim Invasive Gynecol. 2020;27:116–21.
Song D, Li TC, Zhang Y, et al. Correlation between hysteroscopy findings and chronic endometritis. Fertil Steril. 2019;111:772–9.
Cicinelli E, Resta L, Nicoletti R, et al. Endometrial micropolyps at fluid hysteroscopy suggest the existence of chronic endometritis. Human Reprod (Oxford, England). 2005;20:1386–9.
Cicinelli E, Resta L, Nicoletti R, et al. Detection of chronic endometritis at fluid hysteroscopy. J Minim Invasive Gynecol. 2005;12:514–8.
Cicinelli E, Tinelli R, Lepera A, et al. Correspondence between hysteroscopic and histologic findings in women with chronic endometritis. Acta Obstet Gynecol Scand. 2010;89:1061–5.
Hue HJ, Choi H, Lee HK, et al. Prevalence and confounders of chronic endometritis diagnosed using CD138 in patients with recurrent implantation failure. Clin Exp Reprod Med. 2024;51(2):163–9.
Pérez-Cejuela BA, Vitale SG, Pérez-Medina T, et al. Hysteroscopic versus histopathological agreement in the diagnosis of chronic endometritis: results from a retrospective observational study. Arch Gynecol Obstet. 2023;308:1817–22.
Liu Y, Chen X, Huang J, et al. Comparison of the prevalence of chronic endometritis as determined by means of different diagnostic methods in women with and without reproductive failure. Fertil Steril. 2018;109:832–9.
Fan X, Li X, Li Y, et al. Endometrial CD138 count appears to be a negative prognostic indicator for patients who have experienced previous embryo transfer failure. Fertil Steril. 2019;112:1103–11.
Herlihy NS, Klimczak AM, Titus S, et al. The role of endometrial staining for CD138 as a marker of chronic endometritis in predicting live birth. J Assist Reprod Genet. 2022;39:473–9.
Tang C, Yue Y, Liu Y. Value of intervention in embryo transfer for CD138-negative patients with chronic endometritis. Lab Med Clin. 2022;19:1982–5 (in Chinese).
Yang R, Du X, Wang Y, et al. The hysteroscopy and histological diagnosis and treatment value of chronic endometritis in recurrent implantation failure patients. Arch Gynecol Obstet. 2014;289:1363–9.
Author information
Authors and Affiliations
Contributions
Conception and design: Xifeng Xiao, Mao Li. Analysis and/or interpretation of the data: all authors. Drafting of the article: all authors. Critical revision of the article for important intellectual content: all authors. All authors read and approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Ethics approval
This study was approved by the Ethics Committee of Tangdu Hospital of Air Force Medical University (TDLL-202403–05).
Consent for publication
All authors consent to publication.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Dang, J., Xiao, X. & Li, M. Correlation of hysteroscopic findings of chronic endometritis with CD138 immunohistochemistry and their correlation with pregnancy outcomes. J Assist Reprod Genet 41, 2477–2483 (2024). https://doi.org/10.1007/s10815-024-03204-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-024-03204-8