Abstract
This article comprehensively reviews motor impairments in children with autism spectrum disorder (ASD) to: (1) determine the prevalence of motor problems in children with ASD; (2) understand the nature of motor difficulties in ASD and whether they are consistent with developmental coordination disorder (DCD); and (3) determine if the term DCD was used as a co-occurring diagnosis in children with ASD after publication of the DSM-5 in 2013. The following databases were systematically searched: MEDLINE, EMBASE, CINAHL, and PsycINFO from 2010 to December 2021. Articles were included if they: (1) were peer-reviewed and published in a scientific journal; (2) included children with ASD who were between 5 and 12 years; (3) used motor or function measures to assess motor abilities in children with ASD. Studies that included children with intellectual disabilities were excluded. Two independent reviewers reviewed titles, abstracts, and full-text articles for inclusion. Twenty-seven studies met the inclusion criteria and were assessed for quality by two independent reviewers using the Appraisal tool for Cross-Sectional Studies. The majority of articles (92.5%) indicated that 50–88% of children with ASD had significant motor impairments on standardized motor assessments and/or functional questionnaires. The nature of motor and function problems in ASD were consistent with DCD; however, only three out of 20 papers (15%) that were published from 2014 described the motor problems as DCD. One study reported that 15.1% of children with ASD with motor impairments had a co-occurring diagnosis of DCD, suggesting that DCD is under-recognized in this clinical population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Autism spectrum disorder (ASD) is a highly heterogenous and prevalent neurodevelopmental disorder characterized by permanent impairments in social interactions, communication skills, and restricted and repetitive behaviors (American Psychiatric Association, 2013). With the exception of stereotyped and repetitive movements, other motor impairments are not considered as a diagnostic criterion for ASD (American Psychiatric Association, 2013). However, research has shown the presence of motor deficits in 50–85% of children with ASD (American Psychiatric Association, 2013). Compared to typically developing (TD) children, children with ASD show a variety of motor impairments, including poor bilateral coordination (David et al., 2009), reduced grip strength (Hardan et al., 2003; Williams et al., 2006), impaired motor speed (Hardan et al., 2003; Takarae et al., 2004; Williams et al., 2006), gait abnormalities (Rinehart et al., 2006), and poor fine motor control (e.g., manual dexterity, handwriting, object control) (Berkeley et al., 2001; Kushki et al., 2011; McPhillips et al., 2014; Sacrey et al., 2014). Despite these various motor difficulties in children with ASD, motor problems are under-recognized and rarely addressed in therapy (Case-Smith & Arbesman, 2008). Motor problems in children with ASD can profoundly affect child’s development in academic, social, and communication domains (Dowd et al., 2010). A better understanding of the motor problems in children with ASD will help rehabilitation professionals to recognize the issue and provide evidence-based interventions.
ASD often co-occurs with other neurodevelopmental disorders, including intellectual disability (Charman et al., 2011) and attention deficit hyperactivity disorder (ADHD) (Simonoff et al., 2008). Recognizing that poor motor function was not a diagnostic criterion for ASD, but that prevalence of motor difficulties was high in this population, the Diagnostic and Statistical Manual of Mental Disorders—5th edition (DSM-5) published in 2013 allowed for dual diagnosis of ASD and developmental coordination disorder (DCD) (previously not permitted in DSM-IV). DSM-5 defines DCD as a neurodevelopmental disorder marked by significant impairment in the development of motor skills that interferes with academic achievement and/or activities of daily living. The onset of these difficulties is in early childhood and are not due to another medical condition (American Psychiatric Association, 2013). Several hypotheses have been raised as to whether the observed motor problems in ASD are specific to children with ASD or are in agreement with the diagnostic criteria of DCD. Some authors believe that children with ASD have discrete motor problems, particularly a praxis deficit, which is different from motor problems seen in DCD (MacNeil & Mostofsky, 2012); however, others believe that children with ASD showed motor difficulties consistent with DCD (Miyahara, 2013). Results from a systematic review showed that the motor coordination deficits is so prevalent in children with ASD that might be considered a cardinal feature in this children (Fournier et al., 2010). Another systematic review concluded that the children with ASD and DCD shared similar deficits in motor skills (Caçola et al., 2017).
In this systematic review, our primary research question was: In children with ASD, what is the nature and prevalence of motor problems consistent with DCD? We then asked: In children with ASD, did a co-occurring diagnosis of DCD increase after a dual diagnosis of ASD and DCD was permitted in the latest version of Diagnostic and Statistical Manual (DSM-5) in 2013?
Methods
In this systematic review [PROSPERO CRD42021237013] we applied the Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA) guidelines (Moher et al., 2010). Studies investigating motor or function capabilities that used any standardized motor or functional performance measures in children with autism spectrum disorder were considered for inclusion.
Search Strategy
We systematically searched databases including MEDLINE, EMBASE, CINAHL, and PsycINFO from 2010 to December 2021. We narrowed down the search to papers after 2010 since the last systematic review covered papers up to 2010 (Fournier et al., 2010), and also the DSM-5 published in 2013 allowed for dual diagnosis of ASD and developmental coordination disorder (DCD) (previously not permitted in DSM-IV). The librarian at the University of British Columbia assisted in designing the search strategies, including controlled vocabulary (e.g., Medical Subject Headings [MeSH]) and keywords, without setting limits on date or language. Keywords used in selected articles and systematic reviews were also searched in Google, including motor skills, motor skills disorders, and autism spectrum disorder. Terms in each group were linked with “OR” and groups were linked with “AND”. Supplementary Tables 1 and 2 show the keywords used in each category and an example of the search strategy in MEDLINE, respectively.
Criteria for Inclusion and Exclusion
Prior to the beginning of the study selection, inclusion and exclusion criteria were set by the two reviewers (MK, JZ). Studies of children between age 5–12 years old diagnosed with autism spectrum disorder were included, unless the sample included children with a co-occurring moderate/severe intellectual disability (IQ cut-off < 70). The papers with a wider age range were included if they separated results for the age range of interest. The focus was on the studies that measured motor skills (with or without function measure) in children with autism. Longitudinal studies were included only if they presented the baseline results; results related to the effect of maturation, medication, or intervention were not included in this review. Peer-reviewed studies, case reports, and papers written in English were included; systematic reviews, commentaries, conference proceedings, and animal studies were excluded. We included all papers that reported baseline results of motor or function measures, either compared to TD children or standardized measures. As we are interested in motor problems consistent with DCD, studies that solely focus on motor problems that are considered part of ASD, such as stereotyped or repetitive motor movements or difficulty using gestures, were excluded. Moreover, motor difficulties that can be explained by other conditions (e.g., genetic conditions affecting movement, cerebral palsy) were excluded.
Study Selection and Data Extraction
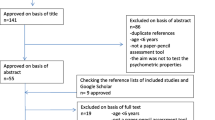
We imported the papers from all databases to the systematic review software called Covidence (Covidence—Better Systematic Review Management, n.d.). All papers were imported into Covidence, and duplications were removed automatically. Reviewers (MK and MM) ran two main stages in the Covidence independently: (a) title and abstract screening; and (b) full-text screening based on the inclusion and exclusion criteria. Conflicts were resolved by third reviewer (JZ) in both steps. Kappa statistics were used to calculate the level of agreement (Cohen, 1968) at each step and both reviewers agreed on including each paper in the systematic review. The level of agreement for title and abstract screening was almost perfect agreement (Kappa stat: 0.86), and for full-text screening was substantial (Kappa stat: 0.77). Figure 1 displays the selection process as per the PRISMA guideline (Moher et al., 2010).
Data extraction was completed by the first reviewer (MK) and confirmed by the second reviewer (MM). The extracted information was organized into two tables: Characteristics of studies (i.e., author, year, demographics of diagnosis group and control group(s), type of screening assessments, function and motor measures); and Results of studies (i.e., study design, effect size, multiple comparison type, function results (consistent with Criterion B of DCD), and motor results (consistent with Criterion A of DCD).
Quality Assessment
Twenty-seven met our inclusion criteria and were independently assessed for quality by two independent reviewers (MK and MM) using the Appraisal tool for Cross-Sectional Studies (AXIS) (Downes et al., 2016; Supplementary Table 3). The AXIS seemed to be the best fit for evaluation of the included papers, most of which were cross-sectional studies. This appraisal tool measures the appropriateness of the study (i.e., aim, study design, sample selection and justification, non-responders, measurement validity and reliability, statistics, results, confounding, conflict of interests, and limitations). The overall score classified into three categories of poor, moderate, and high based on the quality assessment of key points.
Results
Description of Studies
Of the 4030 papers located in the search, 27 articles were included in the systematic review (Fig. 1 and Tables 1, 2). Most study designs were cross-sectional.
Of the 27 included articles, 14 studies compared children with ASD to TD children (Abu-Dahab et al., 2013; Alsaedi, 2020; Biffi et al., 2018; Bricout et al., 2019; Grace et al., 2017; Kaur et al., 2018; Mache & Todd, 2016; McPhillips et al., 2014; Odeh et al., 2020; Sansi et al., 2020; Schurink et al., 2012; Staples & Reid, 2010; Sumner et al., 2016; Whyatt & Craig, 2012) and 7 studies compared motor skills to standardized norms (Bhat, 2020; Bittner et al., 2018; Emck et al., 2011; Guest et al., 2017; Gustafsson et al., 2014; Henderson et al., 2016; Liu, 2013). Six studies divided children with ASD into two or three groups to investigate the effectiveness of an intervention; baseline data of the groups meeting our inclusion criteria were extracted (El Shemy & El-Sayed, 2018; Hassani et al., 2020; Pan et al., 2017; Rafiei Milajerdi et al., 2021; Sarabzadeh et al., 2019; Wuang et al., 2010). Three of these studies included other clinical groups, such as DCD (Sumner et al., 2016), behavioural disorder and emotional disorder (Emck et al., 2011), specific language impairment (McPhillips et al., 2014), and children with ASD with low IQ (< 70) (Kaur et al., 2018); these data were not extracted.
The range of sample size was wide, from 6 to 16,994 participants. The most frequently used motor measures were the Movement Assessment Battery for Children (MABC) (Schurink et al., 2012) and MABC-2 (n = 7) (Grace et al., 2017; Liu, 2013; McPhillips et al., 2014; Rafiei Milajerdi et al., 2021; Sarabzadeh et al., 2019; Sumner et al., 2016; Whyatt & Craig, 2012); Test of Goss Motor Development (TGMD-2) (n = 4) (Emck et al., 2011; Guest et al., 2017; Henderson et al., 2016; Staples & Reid, 2010); TGMD-3 (n = 2) (Bittner et al., 2018; Sansi et al., 2020); Bruininks-Oseretsky Test of Motor Proficiency (BOTMP) (n = 2) (Hassani et al., 2020; Wuang et al., 2010); and BOT-2 (n = 3) (Alsaedi, 2020; El Shemy & El-Sayed, 2018; Pan et al., 2017). Five studies used more than one measure: MABC-2 and BOT-2 (Odeh et al., 2020), TGMD-3 and postural sway condition (Mache & Todd, 2016), BOT-2 and sensory integration and praxis test (Kaur et al., 2018), MABC-2 and Gait Real-time Analysis Interactive Lab (GRAIL) (Biffi et al., 2018), and MABC, Physical and Neurological Exams for Subtle Signs (PANESS), and European Physical Fitness Test Battery (EUROFIT) (Bricout et al., 2019). Two studies used other specific motor assessments: Dynamometer, Finger Tapping Test, Grooved Pegboard, Luria-Nebraska test, and Reitan-Kolve test (Abu-Dahab et al., 2013), and Autism-Tics, ADHD and other Comorbidities inventory (A-TAC) (Gustafsson et al., 2014).
The most frequently used functional performance measures were the Vineland Adaptive Behavior Scale (VABS) (n = 4) (Bricout et al., 2019; Guest et al., 2017; Odeh et al., 2020; Sumner et al., 2016) and Developmental Coordination Disorder Questionnaire (DCDQ) (n = 2) (Bhat, 2020; Biffi et al., 2018). One study used the speed subtest of the Handwriting Performance Test as a functional measure (Grace et al., 2017).
Quality of Studies
The majority of papers (22 out of 27) had an overall rating of high quality (Alsaedi, 2020; Bhat, 2020; Biffi et al., 2018; Bricout et al., 2019; El Shemy & El-Sayed, 2018; Emck et al., 2011; Grace et al., 2017; Guest et al., 2017; Gustafsson et al., 2014; Hassani et al., 2020; Henderson et al., 2016; Kaur et al., 2018; Mache & Todd, 2016; McPhillips et al., 2014; Odeh et al., 2020; Pan et al., 2017; Rafiei Milajerdi et al., 2021; Sansi et al., 2020; Sarabzadeh et al., 2019; Schurink et al., 2012; Sumner et al., 2016; Wuang et al., 2010); and five papers were rated as a moderate-quality (Abu-Dahab et al., 2013; Bittner et al., 2018; Liu, 2013; Staples & Reid, 2010; Whyatt & Craig, 2012). All papers that measured functional performance in ASD were rated as high-quality papers.
Results of Studies
We reviewed and classified the results based on their agreement with two of the DSM-5 diagnostic criteria for DCD: criterion A states that motor difficulties are below age-expectations and criterion B is associated functional performance difficulties. Thus, in the first section of results, we discuss studies related to criterion A of DCD that used “Motor Assessments”. All studies except one (Bhat, 2020) evaluated motor skills in children with ASD. Bhat (2020) only used a function measure, so the results were reported in the function measure section.
The second section of results report “Functional Assessments” in children with ASD, consistent with criterion B of DCD (Alsaedi, 2020; Bhat, 2020; Biffi et al., 2018; Bricout et al., 2019; Grace et al., 2017; Guest et al., 2017; Kaur et al., 2018; Odeh et al., 2020; Sumner et al., 2016).
In the last section of results, we reported studies that used the term DCD in children with ASD (Bhat, 2020; Gustafsson et al., 2014; Sumner et al., 2016).
Motor Assessments
The most frequently used motor assessments were MABC (n = 8), TGMD (n = 6), and BOT (n = 5). Five studies used multi-measures (Biffi et al., 2018; Bricout et al., 2019; Kaur et al., 2018; Mache & Todd, 2016; Odeh et al., 2020), and two studies used other specific motor assessments (Abu-Dahab et al., 2013; Gustafsson et al., 2014). In what follows, we will summarize results based on the type of motor measures used. The standard scores of each test were compared to TD children if the study has TD sample; otherwise, these scores were compared to normative data.
Movement Assessment Battery for Children
The original Movement Assessment Battery for Children is a norm-referenced test designed to identify motor impairments in children aged from 4 to 12 years (Henderson & Sugden, 1992). The total score on the MABC is reported as a total impairment score, with higher scores indicating greater motor impairment.
The second edition of this test, called the MABC-2, was developed in 2007 and assesses fine and gross motor skills in 3–16-year-old children in three components (i.e., manual dexterity, ball skills, and balance) (Henderson et al., 2007). Raw scores are converted to standard scores (mean = 10; SD = 3). Standard scores are converted to percentile scores; scores in the bottom 5% (standard score of 5 or below) represent a definite motor problem placing in red zone, and scores between 5 and 15% suggest a degree of difficulty that is borderline (amber zone). Scores at the 16th % and above indicate no motor problem (green zone).
Six high quality papers (Grace et al., 2017; McPhillips et al., 2014; Rafiei Milajerdi et al., 2021; Sarabzadeh et al., 2019; Schurink et al., 2012; Sumner et al., 2016) and two moderate quality papers (Liu, 2013; Whyatt & Craig, 2012) used the MABC or MABC-2 to measure motor skills in children with ASD. Consistent across all of these studies, the scores of children with ASD were significantly lower than TD children or normative MABC data, indicating motor impairment in children with ASD.
Two of the above studies found significantly lower scores for total score and all three subtests of MABC-2 including dexterity, ball skills, and balance in children with ASD compared to TD children (Grace et al., 2017; McPhillips et al., 2014). Around 11% of children with ASD scored between 5th and 15th percentile on the MABC-2 (amber zone), suggesting borderline degree of motor difficulty; 50% of children with ASD scored below 5th percentile of a standardized MABC-2 score, indicating a definite motor problem (McPhillips et al., 2014). Sumner et al. (2016) stated that the total percentile score and all subtests’ scores were lower in children with ASD compared to TD children and 53% of children with ASD scored at or below 16th percentile.
Similarly, Liu (2013) used the MABC-2 to evaluate motor performance in children with ASD and found that 78% of these children were in the red zone, suggesting a definite motor problem; and 6% of them were in the amber zone. The total standard score and all subtests’ scores were lower than normative MABC-2 data, with the lowest scores for manual dexterity and ball skills, compared to balance subtest (Liu, 2013). Rafiei Milajerdi et al. (2021) reported the similar results that all subtests’ scores were lower than normative MABC-2 data (Rafiei Milajerdi et al., 2021). Another study revealed that the total standard score and all subtests’ scores in children with ASD were lower than TD children, and the lowest scores were for manual dexterity, ball skills, and static balance subtests, compared to dynamic balance (Whyatt & Craig, 2012).
There were two studies that reported the degree of motor difficulty based on motor impairment score (Sarabzadeh et al., 2019; Schurink et al., 2012). They used original version of MABC and reported the results based on the total motor impairment score. The total motor impairment score and all subtests’ scores of children with ASD were higher than normative MABC data, suggesting motor impairment in these children (Sarabzadeh et al., 2019). These total impairment score and all subtests’ scores were also higher in ASD relative to TD children such that 42.9% of children with ASD had definite motor problem (scored at red zone) and 21.4% of them were at risk of motor impairment (scored at amber zone) (Schurink et al., 2012).
Test of Goss Motor Development (TGMD)
Test of Gross Motor Development—2nd ed. (TGMD-2) is used to assess fundamental motor skills in locomotor (i.e., run, gallop, hop, leap, jump, and slide) and object control (i.e., strike, dribble, catch, kick, throw, and roll) (Ulrich, 2000). Scoring is based on the presence (1) or absence (0) of each performance criteria. Raw scores are converted to standard scores, with a mean of 10 and standard deviation of 3 for both locomotor skill and object control. The overall gross motor quotient (GMQ) ranges from 0 to 140 (mean:100, SD:15); higher scores indicate greater motor proficiency. The GMQ less than 89 is below average, indicating below 25th percentile and motor impairment.
Four high quality papers (Emck et al., 2011; Guest et al., 2017; H. Henderson et al., 2016; Sansi et al., 2020) and two moderate quality papers (Bittner et al., 2018; Staples & Reid, 2010) used the TGMD to assess motor difficulties in children with ASD. All studies except one (Sansi et al., 2020) showed that children with ASD scored lower than TD children or normative data.
Results from the TGMD-2 of 13 girls with ASD showed that all of the girls scored below 25th percentile, indicating significant motor difficulties (Guest et al., 2017). This study also found that girls with ASD had higher scores in the locomotor subtest compared to the object control subtest. Another study found that the overall gross motor quotient, locomotor, and object control subtests standard scores in children with ASD were lower than normative scores, suggesting motor impairment in children with ASD (Henderson et al., 2016); these results are in consistent with the results of the two other studies (Bittner et al., 2018; Emck et al., 2011) that used TGMD-3 and TGMD-2 respectively.
Staples and Reid (2010) compared 25 children with ASD with 25 TD children and found that the raw scores of locomotor and object control subtests in children with ASD were lower than TD children. Children with ASD had difficulty coordinating movements involving both sides of the body, or coordinating upper and lower limbs. The timing of movement was also uncoordinated, since there was no harmony between each segment of their body when performing locomotor subtest (Staples & Reid, 2010). They also found that children with ASD had difficulty controlling the force and direction of the ball and rotating their body when performing control object subtest.
Contrary to these results, a study investigated the effectiveness of specific physical activity program on children with ASD and TD children and did not find any significant differences in total scores and subtests’ score between children with ASD and their peers at baseline (Sansi et al., 2020).
Bruininks-Oseretsky Test of Motor Proficiency
The Bruininks-Oseretsky Test of Motor Proficiency is another standardized test for assessing gross and fine motor domains and consists of four main components—two assess fine motor skills (i.e., fine manual control and manual coordination) and two assess gross motor skills (i.e., body coordination, and strength and agility) (Bruininks, 1978). The second version of BOTMP (BOT-2) is suitable for children who do not speak English as a native language. The first and second versions have the same subtests and scoring. There are only slight differences between these two versions. For example, the complete version of BOT-2 has a total of 53 items, compared to 46 items in BOTMP. Therefore, a wider range of motor tasks can be evaluated using this tool, including gross motor, fine motor, and balance skills (Bruininks & Bruininks, 2005). In BOT-2, raw scores are converted to standard scores ranging from 20 to 80 with the mean of 50 and the standard deviation of 10. This total standard score can be reported as a categorical variable with five descriptive categories: well above average “ > 70”, above average “60–69”, average “41–59”, below average “31–40”, and well-below average “ < 30”. The total standard score under 40 indicates motor impairment (Bruininks & Bruininks, 2005).
Five high quality papers (Alsaedi, 2020; El Shemy & El-Sayed, 2018; Kaur et al., 2018; Odeh et al., 2020; Pan et al., 2017) reported motor performance in children with ASD using the BOTMP or BOT-2. All studies, except one (Pan et al., 2017) found that children with ASD had motor impairments compared to standardized norms. The study by Pan et al. (2017) only included boys with high-functioning autism.
Two studies found that all subtests and total standard composite scores of BOTMP were below the average (< 30) in children with ASD, suggesting motor impairment (Hassani et al., 2020; Wuang et al., 2010). Another study evaluated gross motor domain scores of BOTMP and found that children with ASD scored below the average (< 30) (El Shemy & El-Sayed, 2018).
Alsaedi (2020) found that children with ASD scored lower than TD children in the total standard composite score and both fine and motor domains. The majority of children (88%) scored below the average (31–40). The lowest subtest score in children with ASD was in strength, whereas the highest subtest score was in fine motor integration (Alsaedi, 2020). He also found that there was a positive correlation between age and overall motor performance; older children with ASD tend to perform better than younger children with ASD.
A study evaluating motor performance in 22 boys with high-functioning ASD found that all children scored in the average range (41–59) for total standard composite score and in all subtests of fine and gross motor domains (Pan et al., 2017).
Multi-measures
Five high quality papers used more than one measure to evaluate motor performance in children with ASD (Biffi et al., 2018; Bricout et al., 2019; Kaur et al., 2018; Mache & Todd, 2016; Odeh et al., 2020) and consistently reported that children with ASD had motor impairment.
One of these studies found that children with ASD scored lower in all subtests’ scores and total standard composite score on both the MABC-2 (Henderson et al., 2007), and BOT-2 (Bruininks & Bruininks, 2005) compared to TD children (Odeh et al., 2020). Mache and Todd (2016) found that children with ASD (compared to TD children) scored lower on the total score, and locomotor and object control subtest scores of TGMD-3, and had greater postural sway area in both solid and compliant conditions. Lower postural sway area in the solid condition is indicative of better gross motor skills; children with less postural sway area scored higher on the TGMD-3 (Mache & Todd, 2016).
Another study compared motor skills, praxis, and coordination in children with ASD compared to TD children (Kaur et al., 2018). They found that the total standard composite scores and three subtests of BOT-2 (body coordination, fine manual, and manual dexterity) of children with ASD were lower than TD children. Moreover, the scores from the bilateral motor coordination subtest of the Sensory Integration and Praxis Test showed that children with ASD had more praxis errors and needed more time to complete each action sequence compared to TD children (Kaur et al., 2018).
When compared to TD children, children with ASD had lower total standard scores and ball skills (aiming and catching) and balance scores on MABC-2 (Biffi et al., 2018). They also assessed the kinematics and kinetics gait features of children with ASD by using Gait Real-time Analysis Interactive Lab (GRAIL) and found that the steps in TD children tended to be faster and longer compared to children with ASD. The speed and length of steps, and range of motion of all joints in children with ASD were lower than TD children, meaning that the gait cycle took a bit longer than normal for of children with autism (Biffi et al., 2018).
The last study in this section used three measures to evaluate motor performance in children with ASD. Results from the MABC test showed that the total motor impairment score and all subtests’ scores were higher in ASD than TD children, suggesting definite motor problem in children with ASD, especially in manual dexterity and ball skills (Bricout et al., 2019). The Physical and Neurological Exam for Subtle Signs (PANESS) and the European Physical Fitness Test Battery also demonstrated poorer motor performance in children with ASD compared to TD children (Bricout et al., 2019).
Other Motor Measures
There was one high-quality (Gustafsson et al., 2014) and one moderate-quality (Abu-Dahab et al., 2013) paper that assessed motor competencies in children with ASD by different motor measures and confirmed motor impairment in these children. The first paper used the Autism-Tics, ADHD and other Comorbidities inventory (A-TAC) and found that 52.4% of children with ASD had motor impairment and might be at risk of DCD (Gustafsson et al., 2014).
The second study used the dynamometer, Finger Tapping Test, and Grooved Pegboard to measure grip strength, motor speed, and coordination in children with ASD, respectively (Abu-Dahab et al., 2013). Children with ASD scored significantly lower in all these three motor domains when compared to TD children. They also found that the coordination skill in ASD was positively correlated with age; however, the grip strength and motor speed did not significantly improve with increasing age in children with ASD (Abu-Dahab et al., 2013).
Functional Assessments
Seven papers used functional measures in addition to motor measures, with the majority of studies being of high quality (Biffi et al., 2018; Bricout et al., 2019; Grace et al., 2017; Guest et al., 2017; Kaur et al., 2018; Odeh et al., 2020; Sumner et al., 2016); only one paper assessed functional competencies in children with ASD that was ranked as high quality paper (Bhat, 2020).
Vineland Adaptive Behavior Scales
Four studies used the Vineland Adaptive Behavior Scales (VABS) to assess function in children with ASD compared to TD children. Children with ASD scored lower in all test domains (i.e., communication, daily living skills, and socialization) when compared to TD children (Bricout et al., 2019; Odeh et al., 2020; Sumner et al., 2016); lower scores in the daily living domain is more reflective of poor motor skills in children with ASD.
Another study found that children with ASD had lower composite score, compared to normative data of VABS, suggesting difficulties in day-to-day functioning, which may in part be due to motor challenges in this group of children (Guest et al., 2017). They also found that children with ASD scored lower than standard norms in Social Skills Improvement System, indicating impaired academic competence.
Developmental Coordination Disorder Questionnaire
Two studies measured function in children with ASD using the Developmental Coordination Disorder Questionnaire (DCDQ) (Wilson & Crawford, 2012), and reported poorer motor function in these children compared to TD children (Bhat, 2020; Biffi et al., 2018). Findings showed that 86.9% of children with ASD had definite motor impairment and were at risk of DCD, and the functional performance of 73% of children with ASD was lower than their TD peers (Bhat, 2020). She also found that the DCDQ performance is age related and the proportion of children between 5 and 7 years of age showed gradual improvement in motor performance, but the motor performance decreased by 10% at the 8-year mark, then remained unchanged until 15 years of age.
Other Function Measures
There was only one study used other function measures to evaluate functional performance in children with ASD. They used the speed subtest of the Handwriting Performance Test and found that children with ASD made more errors in both speeded and non-speeded conditions compared to TD children (Grace et al., 2017).
Meta-analysis
Using Review Manager 5.4.1 (The Cochrane Collaboration, 2020), we completed a meta-analysis to determine the potential prevalence of DCD in children with ASD. The forest plot of comparison for both analyses are shown in Figs. 2 and 3.
Meta-analytic Approach
The minimum number of studies to do a meta-analysis is three. These studies were similar in type and version of motor/function test and the results were reported in the same scale. Two separate meta-analysis were conducted comparing motor skills of children with ASD to TD children; one analysis included three studies that used MABC-2 (Grace et al., 2017; McPhillips et al., 2014; Odeh et al., 2020), and the second analysis included three studies used the BOT-2 (Alsaedi, 2020; Kaur et al., 2018; Odeh et al., 2020). One of the studies measured both MABC-2 and BOT-2 and included in both meta-analyses (Odeh et al., 2020).
We used a fixed-effect model with 95% confidence intervals. Overall, children with ASD had a standard score of 4.44 points lower than TD children on the MABC-2, and they had a standard score of 18.50 points lower than TD children on BOT-2, indicating significantly higher risk of DCD in children with ASD.
Dual Diagnosis of ASD and DCD
Despite significant motor and functional impairments in children with ASD reported by the majority of papers, only three out of 20 articles from 2014 (15%) used the term DCD to describe the motor impairments in children with ASD (Bhat, 2020; Gustafsson et al., 2014; Sumner et al., 2016). These findings suggest that DCD is under-diagnosed in this population.
Findings from one study showed that only 15.1% of children with ASD with motor impairments had been given a diagnosis of DCD, and 31.6% of whom were receiving rehabilitation services (Bhat, 2020).
Discussion
This systematic review synthesized findings from 27 studies of children with ASD to understand motor capabilities in these children relative to TD children. According to our findings, the majority of papers (n = 25) found that 50–88% of children with ASD had significant motor impairments on standardized motor assessments and/or functional measures consistent with DCD (Abu-Dahab et al., 2013; Alsaedi, 2020; Bhat, 2020; Biffi et al., 2018; Bittner et al., 2018; Bricout et al., 2019; El Shemy & El-Sayed, 2018; Emck et al., 2011; Grace et al., 2017; Guest et al., 2017; Gustafsson et al., 2014; Hassani et al., 2020; Henderson et al., 2016; Kaur et al., 2018; Liu, 2013; Mache & Todd, 2016; McPhillips et al., 2014; Odeh et al., 2020; Rafiei Milajerdi et al., 2021; Sarabzadeh et al., 2019; Schurink et al., 2012; Staples & Reid, 2010; Sumner et al., 2016; Whyatt & Craig, 2012; Wuang et al., 2010). However, only three articles from 2014 onwards had used the term DCD to refer to motor problems of children with ASD (Bhat, 2020; Gustafsson et al., 2014; Sumner et al., 2016).
Only two articles did not report any significant motor impairment in ASD and demonstrated that motor capabilities in these children were within the average range (Pan et al., 2017; Sansi et al., 2020). In one of the studies, the total score, locomotor subscales, and control objects subscales of the TGMD were lower in children with ASD than TD children, although it was still in the average range and not statistically different. This could be a result of sampling bias (e.g., geographical limitation to primary schools of one city in Turkey) (Sansi et al., 2020). The other study had a small sample size (n = 11) and only included boys with high-functioning autism, which reduced statistical power and generalizability of results (Pan et al., 2017).
Motor skills developing throughout childhood is vital for more advanced and complicated activities, such as self-care, leisure, social communication, and learning (Barnett et al., 2009; García‐Villamisar et al., 2017; Lubans et al., 2010). It is believed that motor deficits are highly correlated with intellectual quotient (IQ) (Westendorp et al., 2014). Some studies showed a significant positive correlation between IQ and motor performance in children with ASD (Green et al., 2009; Papadopoulos et al., 2012); however, findings from these 27 studies that were systematically reviewed are not in line with this idea, indicating the presence of motor impairment in children with ASD with IQs within or above the average range. The IQ cut-off in this review was above 70, so the motor impairment in children with ASD are not better explained by intellectual disability which is consistent with criterion D of DCD in DSM-5.
To further describe motor characteristics of ASD, we will explain the results in the context of fine and gross motor difficulties and functional motor problems as assessed by various motor assessments.
Fine Motor Skills in ASD
Fine motor deficits in children with ASD contribute to poorer participation at home and school (Barnett et al., 2009; García‐Villamisar et al., 2017). For example, at home, using a knife for cutting a sandwich, pouring a drink, and using a finger to complete a maze on a smartboard are more challenging due to weaker grip strength (Abu-Dahab et al., 2013), poorer upper limb coordination (Alsaedi, 2020; Grace et al., 2017; Hassani et al., 2020; Odeh et al., 2020; Schurink et al., 2012; Sumner et al., 2016; Whyatt & Craig, 2012; Wuang et al., 2010), and poorer manual dexterity (Alsaedi, 2020; Bricout et al., 2019; Grace et al., 2017; Hassani et al., 2020; Kaur et al., 2018; Liu, 2013; McPhillips et al., 2014; Odeh et al., 2020; Sarabzadeh et al., 2019; Schurink et al., 2012; Sumner et al., 2016; Whyatt & Craig, 2012; Wuang et al., 2010).
At school, using different utensils for writing (e.g., pencil, marker), printing on different surfaces (e.g., paper or blackboard), and zipping and buttoning jackets are more difficult due to lower motor speed of movements (Abu-Dahab et al., 2013; Grace et al., 2017; Sarabzadeh et al., 2019; Schurink et al., 2012), weaker fine motor precision (Alsaedi, 2020; Hassani et al., 2020; Kaur et al., 2018; Odeh et al., 2020; Wuang et al., 2010), poor eye-hand coordination (Abu-Dahab et al., 2013; Grace et al., 2017; Odeh et al., 2020; Sarabzadeh et al., 2019; Schurink et al., 2012; Sumner et al., 2016; Whyatt & Craig, 2012), and weaker fine motor integration (Alsaedi, 2020; Hassani et al., 2020; Kaur et al., 2018; Odeh et al., 2020; Wuang et al., 2010).
Gross Motor Skills in ASD
Gross motor deficits in children with ASD impact their social interaction, leisure, and school life (Lubans et al., 2010). They might experience more challenges in playing sports such as baseball, football, and swimming due to slower running speed, decreased agility, and poorer motor coordination (Alsaedi, 2020; Bittner et al., 2018; Bricout et al., 2019; El Shemy & El-Sayed, 2018; Emck et al., 2011; Guest et al., 2017; Hassani et al., 2020; Henderson et al., 2016; Mache & Todd, 2016; Odeh et al., 2020; Staples & Reid, 2010; Wuang et al., 2010), decreased strength (Alsaedi, 2020; Bricout et al., 2019; El Shemy & El-Sayed, 2018; Hassani et al., 2020; Odeh et al., 2020; Wuang et al., 2010), poor ability in horizontal jump (Bittner et al., 2018; Emck et al., 2011; Guest et al., 2017; Henderson et al., 2016; Mache & Todd, 2016; Staples & Reid, 2010), weakness in over/under hand throw, one/two hand strike, and two hand catch, dribble, and kick (Bittner et al., 2018; Emck et al., 2011; Guest et al., 2017; Henderson et al., 2016; Mache & Todd, 2016; Staples & Reid, 2010).
Riding a horse and a bike are more difficult for children with ASD because of poor bilateral coordination (Alsaedi, 2020; El Shemy & El-Sayed, 2018; Hassani et al., 2020; Kaur et al., 2018; Odeh et al., 2020; Wuang et al., 2010), poor balance (Alsaedi, 2020; Biffi et al., 2018; Bricout et al., 2019; El Shemy & El-Sayed, 2018; Grace et al., 2017; Hassani et al., 2020; Liu, 2013; Mache & Todd, 2016; McPhillips et al., 2014; Odeh et al., 2020; Sarabzadeh et al., 2019; Schurink et al., 2012; Sumner et al., 2016; Whyatt & Craig, 2012; Wuang et al., 2010), and weaker postural control (Mache & Todd, 2016).
Children with ASD also performed more poorly than TD children on the playground, for example in sliding, hopping, skipping (Bittner et al., 2018; Emck et al., 2011; Guest et al., 2017; Henderson et al., 2016; Mache & Todd, 2016; Staples & Reid, 2010), walking (Biffi et al., 2018; Bricout et al., 2019), and galloping (Bittner et al., 2018; Emck et al., 2011; Guest et al., 2017; Henderson et al., 2016; Mache & Todd, 2016; Staples & Reid, 2010).
Functional Motor Performance in ASD
Evidence suggested the presence of motor deficits (i.e., fine motor skills and/or gross.motor skills) in children with ASD. The poor motor performance in children with ASD might affect their functional performance as shown in several studies using Vineland Adaptive Behavior Scale (Bricout et al., 2019; Guest et al., 2017; Odeh et al., 2020; Sumner et al., 2016), Developmental Coordination Disorder Questionnaire (DCDQ) (Bhat, 2020; Biffi et al., 2018), Handwriting Performance Test (Grace et al., 2017). Motor problems in ASD will significantly impact their future social skills development, adaptive function, and quality of life (MacDonald et al., 2013a, 2013b).
For example, good grip strength is essential for independence in functional tasks in both early childhood (Häger‐Ross & Rösblad, 2002) and adulthood (Hyatt et al., 1990). The early diagnosis and implementing an appropriate therapeutic intervention for motor impairments in children with ASD may lead to greater independence in functional performance involving self-care, school, and socializing and communication. Furthermore, early diagnosis of motor problems in ASD and providing evidence-based rehabilitation methods may decrease risk of cardiorespiratory problems (Okely et al., 2001), anxiety and poor self-esteem (Pan et al., 2009), obesity (Okely et al., 2004), low physical fitness, and social isolation (Srinivasan et al., 2014) in these children and lead to enhance self-efficacy, self-perception (Babic et al., 2014), self-confidence, and motivation (Cairney et al., 2019). While this evidence is for children with DCD, it may also be applicable to children with ASD.
Relationship Between Motor Performance and Age
Age might be a critical factor in determining the nature of the motor deficits seen in children with ASD. One study that used BOT-2 as a motor measure in children with ASD demonstrated a linear pattern of impairment in fine and gross motor skills that decreased with age (Alsaedi, 2020). However, another study reported that motor and function problems in children with ASD decrease between 5 and 7 years of age and then increase by 10% from age 8 years and motor problems persist (Bhat, 2020). Findings from another study showed that motor speed and grip strength became worse in children with ASD as they got older, while motor coordination became better with the age (Abu-Dahab et al., 2013). However, the cross-sectional nature of these studies imply caution in the interpretation of age-related phenomena and the relationship between motor skills and age in children with ASD needs to be further investigated.
Early diagnosis of children with DCD leads to earlier and more effective intervention (Lee & Zwicker, 2021; Zwicker & Lee, 2021), which may also be applicable to children with ASD. Therefore, it is necessary to increase awareness about motor problems in children with ASD. Early diagnosis of these motor deficits and employing evidence-based interventions can shift the overall trajectories of motor development in children with ASD.
Addressing motor impairments can also improve core deficits of ASD. Findings suggest that there is a relationship between motor function and core symptoms of ASD (i.e., language skills, repetitive behaviors, social functioning, and cognitive skills) (Fulceri et al., 2018). More specifically, greater motor skill impairment in children with ASD is associated with more language deficits, higher rate of repetitive behavior, more impaired social skills, and higher cognitive deficits (Fulceri et al., 2018).
Dual Diagnosis of ASD and DCD
The proportion of children with ASD who showed significant motor deficits and who performed below-age in motor functioning were 50–88% and 73%, respectively (Bhat, 2020; McPhillips et al., 2014); however, few children with ASD (15.1%) had a co-occurring diagnosis of DCD and many of children with ASD remained undiagnosed (Bhat, 2020). Findings are consistent with results of another study that confirmed a high prevalence of motor impairments in children with ASD which were often over-looked (Licari et al., 2020). Licari et al. (2020) conducted a cohort study on 2,084 children with ASD aged ≤ 6 years and they found that over one-third of these children met the criteria for motor impairment; however, only 1.34% of these children were clinically diagnosed with motor deficit.
Only 3/19 studies published from 2014 identified motor impairments in children with ASD as DCD and discussed a dual diagnosis of ASD and DCD. Evidence suggests that children with ASD may not be receiving the care they need to address their motor skill deficits. Despite a large and vast degree of motor deficits in children with ASD, only 31.6% of these children with a DCD diagnosis were receiving rehabilitation services for their motor deficits (Bhat, 2020).
Clinical Implications
As there are currently very few studies that have used the term DCD in children with ASD, greater awareness of co-occurring DCD in ASD is critical. Motor intervention for children with ASD should be considered a priority in treatment planning due to the high prevalence of motor problems of ASD and their long-term effect on performance, self-efficacy (Babic et al., 2014), self-esteem (Pan et al., 2009), physical fitness (Srinivasan et al., 2014), and social interaction (Henderson et al., 2016).
Our findings have important implications for clinicians working with children with ASD—to recognize, assess, and treat motor deficits and provide assessment data to inform DCD diagnosis. Because motor difficulties in ASD are consistent with DCD diagnosis, standardized assessments like MABC-2 and DCDQ can be easily used to identify motor problems in ASD (Ip et al., 2021).
Recommendations for Research
Due to the lack of consistent evidence, further investigation about the effect of chronological age on the motor performance of children with ASD is recommended. More longitudinal studies that investigate the developmental trajectory of children with ASD would be helpful to better understand the role of age in motor development. As the literature suggests, motor problems are rarely the target of therapy for children with ASD. One of the recommended treatments for children with DCD is called CO-OP (Cognitive Orientation to Occupational Performance) (Blank et al., 2019), which has been shown to be beneficial in case studies of children with ASD (Phelan et al., 2009; Rodger & Brandenburg, 2009). A randomized controlled trial exploring the effectiveness of CO-OP intervention is currently underway (NCT04119492).
Study Limitations
ASD is a heterogeneous disorder, meaning that children will present with a varied range of motor and/or cognitive presentations. Having less homogenous samples may decrease generalizability of the results to all children with ASD (Abu-Dahab et al., 2013; Biffi et al., 2018; Bittner et al., 2018; Emck et al., 2011; Liu, 2013; Mache & Todd, 2016; McPhillips et al., 2014; Sansi et al., 2020), same as the studies who only worked with one sex (Bricout et al., 2019; Grace et al., 2017; Guest et al., 2017; Kaur et al., 2018; Pan et al., 2009), or had small sample sizes (Bittner et al., 2018; Hassani et al., 2020; Kaur et al., 2018; Sarabzadeh et al., 2019). Results of the meta-analyses were also heterogenous. As we did not include grey literature, protocols, or trials register records in our review, the risk of publication bias could not be ruled out.
Another limitation was the wide range of motor deficits ranging from a prevalence of 50% to 88%, which might be related to the various motor measures and functional questionnaires used, or the cut-off scores that were employed. The nature of cross-sectional studies limited our understanding about developmental trajectories in ASD. Findings from all included studies in this review are not generalizable to children with ASD with a co-occurring intellectual disability.
Lastly, we inferred from the articles if the children met criteria A and B for DCD and that criteria C and D were not explicitly described; thus, the prevalence of DCD we report may be inflated; however, the prevalence of motor impairments are well documented and need to be addressed.
Conclusion
The majority of children with ASD show motor impairments, including deficits in various fine and gross motor skills. Despite the consistent nature of motor problems in ASD and the significant impact of motor deficits on their personal, academic, and social life, most children with ASD were not diagnosed with co-occurring DCD and were not receiving adequate rehabilitation services for their motor deficits (Bhat, 2020). As motor skills impairment is not a core symptom of ASD, a dual diagnosis of DCD is important to increase awareness and understanding of the motor deficit for the child, parents, teachers, coaches, and others working with children with ASD. Therapists can add evidence-based motor interventions, such as CO-OP, to the child’s treatment plan to improve their overall functioning.
References
Abu-Dahab, S. M. N., Skidmore, E. R., Holm, M. B., Rogers, J. C., & Minshew, N. J. (2013). Motor and tactile-perceptual skill differences between individuals with high-functioning autism and typically developing individuals ages 5–21. Journal of Autism and Developmental Disorders, 43(10), 2241–2248. https://doi.org/10.1007/s10803-011-1439-y
Alsaedi, R. H. (2020). An assessment of the motor performance skills of children with autism spectrum disorder in the gulf region. Brain Sciences, 10(9), 607. https://doi.org/10.3390/brainsci10090607
American Psychiatric Association (Ed.). (2013). Diagnostic and statistical manual of mental disorders: DSM-5 (5th ed). American Psychiatric Association.
Babic, M. J., Morgan, P. J., Plotnikoff, R. C., Lonsdale, C., White, R. L., & Lubans, D. R. (2014). Physical activity and physical self-concept in youth: Systematic review and meta-analysis. Sports Medicine, 44(11), 1589–1601. https://doi.org/10.1007/s40279-014-0229-z
Barnett, L. M., van Beurden, E., Morgan, P. J., Brooks, L. O., & Beard, J. R. (2009). Childhood motor skill proficiency as a predictor of adolescent physical activity. Journal of Adolescent Health, 44(3), 252–259. https://doi.org/10.1016/j.jadohealth.2008.07.004
Berkeley, S. L., Zittel, L. L., Pitney, L. V., & Nichols, S. E. (2001). Locomotor and object control skills of children diagnosed with autism. Adapted Physical Activity Quarterly, 18(4), 405–416. https://doi.org/10.1123/apaq.18.4.405
Bhat. (2020). Is motor impairment in autism spectrum disorder distinct from developmental coordination disorder? A report from the Spark study. Physical Therapy, 100(4), 633–644. https://doi.org/10.1093/ptj/pzz190
Biffi, E., Costantini, C., Ceccarelli, S. B., Cesareo, A., Marzocchi, G. M., Nobile, M., Molteni, M., & Crippa, A. (2018). Gait pattern and motor performance during discrete gait perturbation in children with autism spectrum disorders. Frontiers in Psychology, 9, 2530. https://doi.org/10.3389/fpsyg.2018.02530
Bittner, M., Silliman-French, L., Myers, D., & Nichols, D. (2018). Effectiveness of instructional strategies on the motor performance of children with autism spectrum disorder. Palaestra, 32(2), 36.
Blank, R., Barnett, A. L., Cairney, J., Green, D., Kirby, A., Polatajko, H., Rosenblum, S., Smits-Engelsman, B., Sugden, D., Wilson, P., & Vinçon, S. (2019). International clinical practice recommendations on the definition, diagnosis, assessment, intervention, and psychosocial aspects of developmental coordination disorder. Developmental Medicine & Child Neurology, 61(3), 242–285. https://doi.org/10.1111/dmcn.14132
Bricout, V.-A., Pace, M., Dumortier, L., Miganeh, S., Mahistre, Y., & Guinot, M. (2019). Motor capacities in boys with high functioning autism: Which evaluations to choose? Journal of Clinical Medicine, 8(10), 1521. https://doi.org/10.3390/jcm8101521
Bruininks, R. H. (1978). Bruininks-Oseretsky test of motor proficiency: Examiner’s manual. American Guidance Service.
Bruininks, R. H., & Bruininks, B. D. (2005). Bruininks-oseretsky test of motor proficiency second edition manual. Pearson Assessments.
Caçola, P., Miller, H. L., & Williamson, P. O. (2017). Behavioral comparisons in autism spectrum disorder and developmental coordination disorder: A systematic literature review. Research in Autism Spectrum Disorders, 38, 6–18. https://doi.org/10.1016/j.rasd.2017.03.004
Cairney, J., Dudley, D., Kwan, M., Bulten, R., & Kriellaars, D. (2019). Physical literacy, physical activity and health: Toward an evidence-informed conceptual model. Sports Medicine, 49(3), 371–383. https://doi.org/10.1007/s40279-019-01063-3
Case-Smith, J., & Arbesman, M. (2008). Evidence-based review of interventions for autism used in or of relevance to occupational therapy. American Journal of Occupational Therapy, 62(4), 416–429. https://doi.org/10.5014/ajot.62.4.416
Charman, T., Pickles, A., Simonoff, E., Chandler, S., Loucas, T., & Baird, G. (2011). IQ in children with autism spectrum disorders: Data from the Special Needs and Autism Project (SNAP). Psychological Medicine, 41(3), 619–627. https://doi.org/10.1017/S0033291710000991
Cohen, J. (1968). Weighted kappa: Nominal scale agreement provision for scaled disagreement or partial credit. Psychological Bulletin, 70(4), 213–220. https://doi.org/10.1037/h0026256
Covidence—Better systematic review management. (n.d.). Covidence - better systematic review management. Retrieved March 22, 2021, from https://get.covidence.org/systematic-review
David, F. J., Baranek, G. T., Giuliani, C. A., Mercer, V. S., Poe, M. D., & Thorpe, D. E. (2009). A pilot study: Coordination of precision grip in children and adolescents with high functioning autism. Pediatric Physical Therapy, 21(2), 205–211. https://doi.org/10.1097/PEP.0b013e3181a3afc2
Dowd, A. M., Rinehart, N. J., & McGinley, J. (2010). Motor function in children with autism: Why is this relevant to psychologists? Clinical Psychologist, 14(3), 90–96. https://doi.org/10.1080/13284207.2010.525532
Downes, M. J., Brennan, M. L., Williams, H. C., & Dean, R. S. (2016). Development of a critical appraisal tool to assess the quality of cross-sectional studies (AXIS). British Medical Journal Open, 6(12), e011458–e011458. https://doi.org/10.1136/bmjopen-2016-011458
El Shemy, S. A., & El-Sayed, M. S. (2018). The impact of auditory rhythmic cueing on gross motor skills in children with autism. Journal of Physical Therapy Science, 30(8), 1063–1068. https://doi.org/10.1589/jpts.30.1063
Emck, C., Bosscher, R. J., Van Wieringen, P. C., Doreleijers, T., & Beek, P. J. (2011). Gross motor performance and physical fitness in children with psychiatric disorders: Gross motor performance in child psychiatry. Developmental Medicine & Child Neurology, 53(2), 150–155. https://doi.org/10.1111/j.1469-8749.2010.03806.x
Fournier, K. A., Hass, C. J., Naik, S. K., Lodha, N., & Cauraugh, J. H. (2010). Motor coordination in autism spectrum disorders: A synthesis and meta-analysis. Journal of Autism and Developmental Disorders, 40(10), 1227–1240. https://doi.org/10.1007/s10803-010-0981-3
Fulceri, F., Grossi, E., Contaldo, A., Narzisi, A., Apicella, F., Parrini, I., Tancredi, R., Calderoni, S., & Muratori, F. (2018). Motor skills as moderators of core symptoms in autism spectrum disorders: Preliminary data from an exploratory analysis with artificial neural networks. Frontiers in Psychology, 9, 2683–2683. https://doi.org/10.3389/fpsyg.2018.02683
García-Villamisar, D., Dattilo, J., & Muela, C. (2017). Effects of therapeutic recreation on adults with ASD and ID: A preliminary randomized control trial. Journal of Intellectual Disability Research, 61(4), 325–340. https://doi.org/10.1111/jir.12320
Grace, N., Rinehart, N. J., Enticott, P. G., & Johnson, B. P. (2017). Do children with ASD have difficulty handwriting under time pressure? Research in Autism Spectrum Disorders, 37, 21–30. https://doi.org/10.1016/j.rasd.2017.02.001
Green, D., Charman, T., Pickles, A., Chandler, S., Loucas, T., Simonoff, E., & Baird, G. (2009). Impairment in movement skills of children with autistic spectrum disorders. Developmental Medicine & Child Neurology, 51(4), 311–316. https://doi.org/10.1111/j.1469-8749.2008.03242.x
Guest, L., Balogh, R., Dogra, S., & Lloyd, M. (2017). Examining the impact of a multi-sport camp for girls ages 8–11 with autism spectrum disorder. Therapeutic Recreation Journal, 51(2), 109–126. https://doi.org/10.18666/TRJ-2017-V51-I2-7383
Gustafsson, P., Kerekes, N., Anckarsäter, H., Lichtenstein, P., Gillberg, C., & Råstam, M. (2014). Motor function and perception in children with neuropsychiatric and conduct problems: Results from a population-based twin study. Journal of Neurodevelopmental Disorders, 6(1), 11. https://doi.org/10.1186/1866-1955-6-11
Häger-Ross, C., & Rösblad, B. (2002). Norms for grip strength in children aged 4–16 years. Acta Pædiatrica, 91(6), 617–625. https://doi.org/10.1111/j.1651-2227.2002.tb03290.x
Hardan, A. Y., Kilpatrick, M., Keshavan, M. S., & Minshew, N. J. (2003). Motor performance and anatomic magnetic resonance imaging (MRI) of the basal ganglia in autism. Journal of Child Neurology, 18(5), 317–324. https://doi.org/10.1177/08830738030180050801
Hassani, F., Shahrbanian, S., Shahidi, S. H., & Sheikh, M. (2020). Playing games can improve physical performance in children with autism. International Journal of Developmental Disabilities. https://doi.org/10.1080/20473869.2020.1752995
Henderson, H., Fuller, A., Noren, S., Stout, V. M., & Williams, D. (2016). The effects of a physical education program on the motor skill performance of children with autism spectrum disorder. Palaestra, 30(3), 41.
Henderson, S., Sudgen, D., & Barnett, A. (2007). Movement assessment battery for children (2nd ed.). Psychological Corporation.
Henderson, S., & Sugden, D. (1992). Movement assessment battery for children. Psychological Corporation.
Hyatt, R. H., Whitelaw, M. N., Bhat, A., Scott, S., & Maxwell, J. D. (1990). Association of muscle strength with functional status of elderly people. Age and Ageing, 19(5), 330–336. https://doi.org/10.1093/ageing/19.5.330
Ip, A., Mickelson, E. C. R., & Zwicker, J. G. (2021). Assessment, diagnosis, and management of developmental coordination disorder. Paediatrics & Child Health, 26(6), 375–378. https://doi.org/10.1093/pch/pxab047
Kaur, M., Srinivasan, S. M., & Bhat, A. N. (2018). Comparing motor performance, praxis, coordination, and interpersonal synchrony between children with and without autism spectrum disorder (ASD). Research in Developmental Disabilities, 72, 79–95. https://doi.org/10.1016/j.ridd.2017.10.025
Kushki, A., Chau, T., & Anagnostou, E. (2011). Handwriting difficulties in children with autism spectrum disorders: A scoping review. Journal of Autism and Developmental Disorders, 41(12), 1706–1716. https://doi.org/10.1007/s10803-011-1206-0
Lee, E. J., & Zwicker, J. G. (2021). Early identification of children with/at risk of developmental coordination disorder: A scoping review. Developmental Medicine & Child Neurology, 63(6), 649–658. https://doi.org/10.1111/dmcn.14803
Licari, M. K., Alvares, G. A., Varcin, K., Evans, K. L., Cleary, D., Reid, S. L., Glasson, E. J., Bebbington, K., Reynolds, J. E., Wray, J., & Whitehouse, A. J. O. (2020). Prevalence of motor difficulties in autism spectrum disorder: Analysis of a population-based cohort. Autism Research, 13(2), 298–306. https://doi.org/10.1002/aur.2230
Liu, T. (2013). Sensory processing and motor skill performance in elementary school children with autism spectrum disorder. Perceptual and Motor Skills, 116(1), 197–209. https://doi.org/10.2466/10.25.PMS.116.1.197-209
Lubans, D. R., Morgan, P. J., Cliff, D. P., Barnett, L. M., & Okely, A. D. (2010). Fundamental movement skills in children and adolescents: Review of associated health benefits. Sports Medicine, 40(12), 1019–1035. https://doi.org/10.2165/11536850-000000000-00000
MacDonald, M., Lord, C., & Ulrich, D. (2013a). The relationship of motor skills and adaptive behavior skills in young children with autism spectrum disorders. Research in Autism Spectrum Disorders, 7(11), 1383–1390. https://doi.org/10.1016/j.rasd.2013.07.020
MacDonald, M., Lord, C., & Ulrich, D. A. (2013b). The relationship of motor skills and social communicative skills in school-aged children with autism spectrum disorder. Adapted Physical Activity Quarterly, 30(3), 271–282. https://doi.org/10.1123/apaq.30.3.271
Mache, M. A., & Todd, T. A. (2016). Gross motor skills are related to postural stability and age in children with autism spectrum disorder. Research in Autism Spectrum Disorders, 23, 179–187. https://doi.org/10.1016/j.rasd.2016.01.001
MacNeil, L. K., & Mostofsky, S. H. (2012). Specificity of dyspraxia in children with autism. Neuropsychology, 26(2), 165–171. https://doi.org/10.1037/a0026955
McPhillips, M., Finlay, J., Bejerot, S., & Hanley, M. (2014). Motor deficits in children with autism spectrum disorder: A cross-syndrome study: Motor deficits in children with ASD. Autism Research, 7(6), 664–676. https://doi.org/10.1002/aur.1408
Miyahara, M. (2013). Meta review of systematic and meta-analytic reviews on movement differences, effect of movement-based interventions, and the underlying neural mechanisms in autism spectrum disorder. Frontiers in Integrative Neuroscience, 7, 16–16. https://doi.org/10.3389/fnint.2013.00016
Moher, D., Liberati, A., Tetzlaff, J., & Altman, D. G. (2010). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. International Journal of Surgery, 8(5), 336–341. https://doi.org/10.1016/j.ijsu.2010.02.007
Odeh, C. E., Gladfelter, A. L., Stoesser, C., & Roth, S. (2020). Comprehensive motor skills assessment in children with autism spectrum disorder yields global deficits. International Journal of Developmental Disabilities. https://doi.org/10.1080/20473869.2020.1764241
Okely, A. D., Booth, M. L., & Chey, T. (2004). Relationships between body composition and fundamental movement skills among children and adolescents. Research Quarterly for Exercise and Sport, 75(3), 238–247. https://doi.org/10.1080/02701367.2004.10609157
Okely, A. D., Booth, M. L., & Patterson, J. W. (2001). Relationship of cardiorespiratory endurance to fundamental movement skill proficiency among adolescents. Pediatric Exercise Science, 13(4), 380–391. https://doi.org/10.1123/pes.13.4.380
Pan, C.-Y., Chu, C.-H., Tsai, C.-L., Sung, M.-C., Huang, C.-Y., & Ma, W.-Y. (2017). The impacts of physical activity intervention on physical and cognitive outcomes in children with autism spectrum disorder. Autism, 21(2), 190–202. https://doi.org/10.1177/1362361316633562
Pan, C.-Y., Tsai, C.-L., & Chu, C.-H. (2009). Fundamental movement skills in children diagnosed with autism spectrum disorders and attention deficit hyperactivity disorder. Journal of Autism and Developmental Disorders, 39(12), 1694–1705. https://doi.org/10.1007/s10803-009-0813-5
Papadopoulos, N., McGinley, J., Tonge, B. J., Bradshaw, J. L., Saunders, K., & Rinehart, N. J. (2012). An investigation of upper limb motor function in high functioning autism and Asperger’s disorder using a repetitive Fitts’ aiming task. Research in Autism Spectrum Disorders, 6(1), 286–292. https://doi.org/10.1016/j.rasd.2011.05.010
Phelan, S., Steinke, L., & Mandich, A. (2009). Exploring a cognitive intervention for children with pervasive developmental disorder. Canadian Journal of Occupational Therapy, 76(1), 23–28. https://doi.org/10.1177/000841740907600107
Rafiei Milajerdi, H., Sheikh, M., Najafabadi, M. G., Saghaei, B., Naghdi, N., & Dewey, D. (2021). The effects of physical activity and exergaming on motor skills and executive functions in children with autism spectrum disorder. Games for Health Journal, 10(1), 33–42. https://doi.org/10.1089/g4h.2019.0180
Rinehart, N. J., Tonge, B. J., Iansek, R., McGinley, J., Brereton, A. V., Enticott, P. G., & Bradshaw, J. L. (2006). Gait function in newly diagnosed children with autism: Cerebellar and basal ganglia related motor disorder. Developmental Medicine & Child Neurology, 48(10), 819–824. https://doi.org/10.1017/S0012162206001769
Rodger, S., & Brandenburg, J. (2009). Cognitive Orientation to (daily) Occupational Performance (CO-OP) with children with Asperger’s syndrome who have motor-based occupational performance goals. Australian Occupational Therapy Journal, 56(1), 41–50. https://doi.org/10.1111/j.1440-1630.2008.00739.x
Sacrey, L.-A.R., Germani, T., Bryson, S. E., & Zwaigenbaum, L. (2014). Reaching and grasping in autism spectrum disorder: A review of recent literature. Frontiers in Neurology, 5, 6–6. https://doi.org/10.3389/fneur.2014.00006
Sansi, A., Nalbant, S., & Ozer, D. (2020). Effects of an inclusive physical activity program on the motor skills, social skills and attitudes of students with and without autism spectrum disorder. Journal of Autism and Developmental Disorders. https://doi.org/10.1007/s10803-020-04693-z
Sarabzadeh, M., Azari, B. B., & Helalizadeh, M. (2019). The effect of six weeks of tai chi chuan training on the motor skills of children with autism spectrum disorder. Journal of Bodywork and Movement Therapies, 23(2), 284–290. https://doi.org/10.1016/j.jbmt.2019.01.007
Schurink, J., Hartman, E., Scherder, E. J. A., Houwen, S., & Visscher, C. (2012). Relationship between motor and executive functioning in school-age children with pervasive developmental disorder not otherwise specified. Research in Autism Spectrum Disorders, 6(2), 726–732. https://doi.org/10.1016/j.rasd.2011.10.013
Simonoff, E., Pickles, A., Charman, T., Chandler, S., Loucas, T., & Baird, G. (2008). Psychiatric disorders in children with autism spectrum disorders: Prevalence, comorbidity, and associated factors in a population-derived sample. Journal of the American Academy of Child and Adolescent Psychiatry, 47(8), 921–929. https://doi.org/10.1097/CHI.0b013e318179964f
Srinivasan, S. M., Pescatello, L. S., & Bhat, A. N. (2014). Current perspectives on physical activity and exercise recommendations for children and adolescents with autism spectrum disorders. Physical Therapy, 94(6), 875–889. https://doi.org/10.2522/ptj.20130157
Staples, K. L., & Reid, G. (2010). Fundamental movement skills and autism spectrum disorders. Journal of Autism and Developmental Disorders, 40(2), 209–217. https://doi.org/10.1007/s10803-009-0854-9
Sumner, E., Leonard, H. C., & Hill, E. L. (2016). Overlapping phenotypes in autism spectrum disorder and developmental coordination disorder: A cross-syndrome comparison of motor and social skills. Journal of Autism and Developmental Disorders, 46(8), 2609–2620. https://doi.org/10.1007/s10803-016-2794-5
Takarae, Y., Minshew, N. J., Luna, B., Krisky, C. M., & Sweeney, J. A. (2004). Pursuit eye movement deficits in autism. Brain, 127(Pt 12), 2584–2594. https://doi.org/10.1093/brain/awh307
Ulrich, D. A. (2000). Test of gross motor development (2nd ed.). Pro-Ed.
Westendorp, M., Hartman, E., Houwen, S., Huijgen, B. C. H., Smith, J., & Visscher, C. (2014). A longitudinal study on gross motor development in children with learning disorders. Research in Developmental Disabilities, 35(2), 357–363. https://doi.org/10.1016/j.ridd.2013.11.018
Whyatt, C. P., & Craig, C. M. (2012). Motor skills in children aged 7–10 years, diagnosed with autism spectrum disorder. Journal of Autism and Developmental Disorders, 42(9), 1799–1809. https://doi.org/10.1007/s10803-011-1421-8
Williams, D. L., Goldstein, G., & Minshew, N. J. (2006). Neuropsychologic functioning in children with autism: Further evidence for disordered complex information-processing. Child Neuropsychology, 12(4–5), 279–298. https://doi.org/10.1080/09297040600681190
Wilson, B. N., & Crawford, S. G. (2012). Parent questionnaire designed to screen for coordination disorders in children—DCDQ—The Developmental Coordination Disorder Questionnaire. https://www.dcdq.ca/
Wuang, Y.-P., Wang, C.-C., Huang, M.-H., & Su, C.-Y. (2010). The effectiveness of simulated developmental horse-riding program in children with autism. Adapted Physical Activity Quarterly, 27(2), 113–126. https://doi.org/10.1123/apaq.27.2.113
Zwicker, J. G., & Lee, E. J. (2021). Early intervention for children with/at risk of developmental coordination disorder: A scoping review. Developmental Medicine & Child Neurology, 63(6), 659–667. https://doi.org/10.1111/dmcn.14804
Funding
Melika Kangarani-Farahani received support from the University of British Columbia Faculty of Medicine Graduate Award (#6442), Effie I. Lefeaux Scholarship in Intellectual Disability, and Margaret Hood Scholarship in Occupational Therapy Myrah Malik was supported by a University of British Columbia Faculty of Medicine Graduate Award (#6442) and Syd Vernon Graduate Student Award. Jill Zwicker is funded by the Canadian Institutes of Health Research (Grant No. CIHR 201512MSH-360883-141638), BC Children’s Hospital Research Institute, and Canada Excellence Research Chairs Program (Grant No. 950-233161).
Author information
Authors and Affiliations
Contributions
Melika Kangarani-Farahani and Jill Zwicker contributed to study conception and design. Data collection and data extraction were completed by Melika Kangarani-Farahani and Myrah Malik. Data analysis was conducted by Melika Kangarani-Farahani and Jill Zwicker. The first draft of the manuscript was written by Melika Kangarani-Farahani and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interests to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kangarani-Farahani, M., Malik, M.A. & Zwicker, J.G. Motor Impairments in Children with Autism Spectrum Disorder: A Systematic Review and Meta-analysis. J Autism Dev Disord 54, 1977–1997 (2024). https://doi.org/10.1007/s10803-023-05948-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10803-023-05948-1