Abstract
This study was a replication of Mazefsky et al.’s (Journal of Autism and Developmental Disabilities 43:1236–1242, 2013) investigation among a sample of 45 high ability children and adolescents diagnosed with ASD under DSM-IV-TR. Items from the ADOS and ADI-R were mapped onto DSM-5 diagnostic criteria for ASD and SCD to determine whether participants would meet either diagnosis under DSM-5. If the ADOS were administered alone, 62% of individuals diagnosed with ASD would no longer meet criteria under DSM-5; however, when the ADI-R and ADOS scores were combined, 100% of individuals would continue to meet ASD diagnosis. The ADOS was determined to be an insufficient measure for SCD due to the small number of algorithm items measuring SCD diagnostic criteria, suggesting the development of SCD measures is required.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The Autism Diagnostic Interview, Revised (ADI-R; Rutter et al. 2003) and the Autism Diagnostic Observation Schedule (ADOS; Lord et al. 2002), which was recently revised (ADOS-2; Lord et al. 2012), are considered the gold standards in autism research and clinical identification. These instruments have generally good sensitivity (true positive rate), specificity (true negative rate), and clinical utility (Lord et al. 2000). Less is known about their utility among high functioning populations, and no studies have specifically examined diagnostic effectiveness among high ability children (i.e., children with ability scores of 120 [92nd percentile] or above) with autism spectrum disorder (ASD). Furthermore, with the advent of the new diagnostic category, Social Communication Disorder (SCD; American Psychiatric Association [APA] 2013), it is unclear whether existing ASD diagnostic instruments suffice in identifying children who may no longer meet criteria for ASD under the DSM-5 diagnostic guidelines. This is an important question because of similarities between SCD and ASD (APA 2013), the lack of diagnostic instruments specifically for SCD (van Steensel et al. 2015), and the opinion that some individuals previously diagnosed with ASD under DSM-IV-TR would now meet criteria for SCD under DSM-5 (Gibson et al. 2013; Norbury 2014; Swineford et al. 2014). The purpose of the current study is to examine the ADOS and ADIR profiles among a sample of high ability youth diagnosed with ASD under the DSM-IV to determine their diagnostic profiles in light of the DSM-5 criteria for ASD and SCD.
In the DSM-5, one set of criteria for ASD is offered, with three levels to indicate symptom severity. Social and communication symptoms are combined into one domain where all three criteria must be met currently or by history, and two symptoms must manifest currently or by history under the restrictive, repetitive patterns of behavior, interests, or activities domain. SCD requires four criteria be present, including deficits in social communication within social contexts, altering communication depending on context, following rules of conversations, and understanding inferences, idioms, and other forms of ambiguous language (APA 2013). Because SCD focuses on higher-level language skills, it should not be diagnosed until a child is 4–5 years old and it cannot be diagnosed in conjunction with ASD (Swineford et al. 2014).
Some scholars are concerned about the DSM-5 changes, particularly given findings suggesting 25–68% of those previously diagnosed with ASD would no longer meet criteria under the new guidelines (Kulage et al. 2014; McPartland et al. 2012). In one investigation, missed diagnosed was more likely among those with average or above cognitive ability, where only 46% continued to meet criteria, however a major limitation of this study was that original diagnoses were based on DSM-III-R criteria (McPartland et al. 2012). In a similar study of 90 children with ASD, 30% (most with PDD-NOS) no longer met ASD criteria under DSM-5 largely because of failing to reach criteria in the restricted interests domain (Criteria B; van Steensel et al. 2015). In their meta-analytic review of 14 studies, Kulage et al. (2014) concluded the number of children diagnosed with ASD under DSM-5 will be significantly reduced and this reduction would mainly affect those previously diagnosed with PDD-NOS.
As SCD is a new diagnostic category in the DSM-5, there is little to no empirical literature outside of the speech and language domain, where similar symptoms are described as pragmatic language impairment (Gibson et al. 2013; Swineford et al. 2014). While its inclusion in the DSM-5 is controversial, Swineford and colleagues state, “the goal of the new DSM diagnostic categories is not to prevent the loss of previously diagnosed disorders, but instead to represent natural phenomena as accurately as possible” (p. 2). Many believe children previously diagnosed with PDD-NOS will now be diagnosed with SCD (Gibson et al. 2013; Norbury 2014; Swineford et al. 2014), and others have found support for SCD as independent from ASD, mainly because of the lack of restricted and repetitive patterns of behavior in this population (Gibson et al. 2013). Still others question whether the independence of the diagnoses poses a risk for those with SCD of no longer receiving public health, education, research, and employment benefits afforded to those with ASD (Brukner-Wertman et al. 2016). In their review of four studies examining prevalence of SCD among individuals no longer diagnosed with ASD under DSM-5, Kulage et al. (2014) found extremely variable results, with percentages as low as 1.5% (Huerta et al. 2012) to as high as 63.2% (Wilson et al. 2013). The ADI-R and ADOS have been regarded as “enlightening” tools in diagnosing SCD in addition to ASD, particularly for those who consider the “possibility of a continuous dimension of social impairment between SCD and autism” (Gibson et al. 2013, p. 1194).
ADI-R and ADOS
The ADI-R is a standardized, semi-structured parent/caregiver interview examining past and current functioning within communication, social development and play, and repetitive and restricted behavior domains. It is comprised of 111 items (Cicchetti et al. 2008), 34 of which contribute to the algorithm for diagnosis (Lecavalier et al. 2006). Of these 34, 16 pertain to reciprocal social interaction, 13 to communication, and 8 to restricted, repetitive behaviors (Lord et al. 1994; Rutter et al. 2003). Algorithm items are those that most closely align with DSM-IV and ICD-10 diagnostic criteria for autism, but they have not been revised according to DSM-5 criteria. To receive an ASD diagnosis, the participant must meet diagnostic criteria in each of the three content areas and exhibit abnormality in at least one area by 36 months of age (Lord et al. 1994; Rutter et al. 2003).
The Autism Diagnostic Observation Schedule (ADOS; Lord et al. 2002) is a semi-structured, interactive assessment that allows clinicians to observe the communication, social interaction, and play skills specific to ASD in a standardized manner. The revised diagnostic algorithm for the ADOS (ADOS-2; Lord et al. 2012) has been established as having good predictive value, and good specificity in distinguishing between autism versus non-spectrum (Module 3 sensitivity of 0.91, specificity of 0.84) and non-autism ASD versus non-spectrum individuals (Module 3 sensitivity of 0.72, specificity of 0.77; Gotham et al. 2007).
Risi et al. (2006) examined the diagnostic utility of administering ADOS and ADI-R together among various populations and proposed only the communication and/or social domain criteria be met to receive a diagnosis, while scores on the restricted interest and patterns of behavior domains would not be required. This, however, would make differentiation between DSM-5 ASD and SCD troublesome, since absence of restricted and repetitive patterns of behavior is essentially what differentiates the two diagnoses. Recent, similar findings suggest using the ADI-R and ADOS to identify a continuum of symptoms is more advantageous than to establish a strict diagnostic category classification (de Bildt et al. 2013). Both studies suggest using the ADOS and ADI-R together increases specificity and decreases sensitivity, but that the revised ADOS algorithm may increase sensitivity (de Bildt et al. 2013; Risi et al. 2006). Others conclude these tools are less useful with children with mild ASD (Kamp-Becker et al. 2013).
DSM-5 Diagnostic Changes
Most scholars advocate merging the previously distinct neurodevelopmental disorders in DSM-IV-TR into one autism spectrum disorder in DSM-5 (Lord et al. 2012) because the distinctions between the three diagnoses are frequently artificial (e.g., Brennan et al. 2014; Cholemkery et al. 2016) or related to varying diagnostic practices within clinics (Lord and Bishop 2015). Early research supported the diagnostic changes in the DSM-5 and that increased specificity may reduce false positives, yet miss as many as 12% of those with less severe symptoms (Frazier et al. 2012). Others too have expressed concerns about whether the revised criteria for ASD may miss some children previously diagnosed with PDD-NOS or Asperger Syndrome (Gibbs et al. 2012; Worley and Matson 2012) and apply less to cognitively able students (McPartland et al. 2012). In studies that documented percentages of individuals who no longer met ASD diagnostic criteria in the DSM-5, results showed it was mainly because they lacked two symptoms within the restricted and repetitive interests, activities, and behaviors category (Gibbs et al. 2012; McPartland et al. 2012) or did not meet all four social-communication criteria (McPartland et al. 2012). Whether these children would fit under the SCD category is unclear (van Steensel et al. 2015). Recent work suggests that when the ADOS and ADI-R are administered in combination, diagnostic applicability for the DSM-5 remains among higher functioning individuals, but administration of the ADOS alone may miss many children (McPartland et al. 2012; Mazefsky et al. 2013). However, including non-algorithm items from the restricted interests and repetitive behaviors domain increased the likelihood that children would continue to be identified under the DSM-5 (Mazefsky et al. 2013).
The purpose of the current study is to examine the ADI-R and ADOS scores among a group of high ability children diagnosed with ASD under the DSM-IV. It is a replication of the Mazefsky et al. 2013 study with two important differences. First, the sample consisted of high ability children (cognitive ability score of greater than or equal to 120 [92nd percentile]). Less is known about the applicability of these tools among gifted youth; it may be that ASD manifests uniquely among this population (Assouline et al. 2009, 2011; Foley Nicpon et al. 2010), but empirical research examining this possibility is limited. Second, the authors determined whether those who no longer met criteria for ASD under the DSM-5 did meet criteria for SCD. To date, the ADI-R and ADOS have not been examined in terms of efficacy in diagnosing SCD. Specifically, the following research questions were proposed:
-
a.
What percentage of high ability youth diagnosed with an autism spectrum disorder under DSM-IV-TR would still meet criteria under DSM-5, based on scores from the ADI-R and ADOS?
-
b.
Based on scores from the ADIR-R and ADOS, what percentage of students who no longer met criteria for ASD under DSM-5 would now meet diagnostic criteria for SCD?
Method
Sample
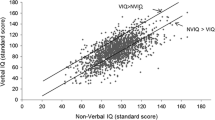
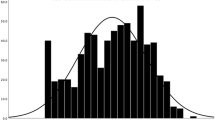
Forty-five children and adolescents ages 5 years, 6 months to 17 years, 10 months (grades kindergarten through 12) participated. Participants were evaluated at a psychology clinic within a university center for gifted and talented students. Children were either recruited through a US Department of Education grant seeking to provide evaluations for high ability students with suspected ASD or specific learning disability or they were self-referred to the clinic by parents for an ASD evaluation. Licensed psychologists with research-level ADOS and ADI-R certification administered the instruments as a part of a comprehensive evaluation to assess for ASD, which included clinical interviews, record review, behavioral observations, and administration of ability, achievement, executive, developmental, adaptive behavior, and psychosocial functioning. Eleven (24.4%) were girls and 34 (75.6%) were boys. Based on DSM-IV criteria, 16 were diagnosed with Autistic Disorder, 17 with Asperger’s Disorder, and 12 with PDD-NOS. High ability was determined through scores from an age-appropriate Wechsler intelligence test. Individuals were considered high ability if one or more index score was 120 or above (within a 95% confidence interval), which is considered the superior range. Index scores were used in favor of full scale scores given high ability youth with ASD typically score lower in processing speed, which contributes to the full scale index (Assouline et al. 2009; Doobay et al.2014; Calhoun and Mayes 2005; Foley Nicpon et al. 2012; Mayes and Calhoun 2007, 2008; Oliveras-Rentas et al. 2012) Similar criteria for identifying high ability among children with ASD have been used elsewhere (e.g., Assouline et al. 2011; Foley Nicpon et al. 2010). High ability among this population is typically within the higher order reasoning domains (e.g., verbal, nonverbal), rather than the lower order domains (e.g., short-term memory and processing speed; Foley Nicpon et al. 2010) but high ability children demonstrate strengths in both/or verbal and nonverbal domains (Reis et al. 2014).
Procedure
This study used the methodology of the Mazefsky et al. (2013) comparison of DSM-IV and DSM-5 autism diagnoses, and added SCD criteria eligibility. Mazefsky et al. examined information from prior research participants who had received diagnoses of PDD-NOS, Asperger’s disorder, or high functioning autism. Their research participants had been diagnosed using the ADI-R and either Module 3 or 4 of the ADOS. Mazefsky et al. mapped the ADOS and ADI-R algorithm items on the DSM-5 diagnostic criteria. Their final analysis attempted to find only those who satisfied full DSM-5 criteria, and for this reason they also included several response items that were not algorithm items but aligned with the repetitive behavior criteria stated in the DSM-5.
The current project sought and received permission from Mazefsky et al. (2013) to use their mapping of algorithm items in order to replicate their work with an existing sample of high ability students who had previously received diagnoses of PDD-NOS, Asperger’s Disorder, or Autistic Disorder through the DSM-IV. We compared Mazefsky’s mapping with the DSM-5 and the exact mapping was used for the current study, with some minor changes. Specifically, three additional items on the ADOS Module 3 and two items on Module 4 were included. On Module 3, items A7 (Reporting of Events), B6 (Insight), and C1 (Imagination/Creativity) were included. On Module 4, items B8 (Responsibility) and C1 (Imagination/Creativity) were included. We added these specific items because we believed they assessed for information related to the DSM-5 criteria.
To the researchers’ knowledge, no previous studies have examined the ADOS and ADI-R for a diagnosis of SCD, and therefore no prior mapping was available for this population. One research team member created a mapping of items from the ADOS Modules 3 and 4 and the ADI-R onto the new DSM-5 SCD criteria. This mapping was discussed with the two other team members until consensus was reached. The team discussed each instrument item to make sure we agreed on which SCD diagnostic criterion it was measuring. Consistent with the standard ADOS/ADI-R scoring and the procedure used by Mazefsky et al. (2013), all scores of 3 were converted to 2, such that the range for each item was 0–2.
All members of the team reviewed the ADOS and ADI-R mapping created for the current study, as well as Mazefsky et al.’s mapping. Consensus was that algorithm items could be assigned to no more than one diagnostic criterion to remain consistent with how the ADOS and ADI-R were designed and to prevent artificial elevations, but diverged from Mazefsky et al. (2013) since assessment items loaded onto more than one DSM criterion on their mapping. When there was not consensus about where particular algorithm items best fit with diagnostic criteria for ASD or SCD, the DSM-5 criteria were reviewed and discussed until consensus was reached.
Next, the research team created a table with the mappings of relevant algorithm items from the ADOS and ADI-R (see Tables 1, 2). Each algorithm item was assigned to one DSM-5 diagnostic criterion for both SCD and ASD. Two of the research members reviewed each ADOS and ADI-R scoring protocol, reporting endorsed items on the created map. One team member entered the mapped results into a pre-existing database of the participants. Team members then created a table of the mapped items with column heads corresponding to DSM-5 criteria, cells indicating the items relevant to the criteria, and rows representing individual children. Two team members entered endorsed items into the table for each participant. It was then possible to discern who would receive a DSM-5 diagnosis of ASD and/or SCD based on the ADOS, ADI-R, and the two measures combined.
Team members analyzed the tables to determine those who originally received a DSM-IV diagnosis of autism, Asperger’s, or PDD-NOS, would obtain a DSM-5 diagnosis of ASD, and whether a diagnosis was “lost,” gained, or retained. If DSM-5 criteria for ASD were not met using either instrument, team members determined whether those individuals met criteria for SCD based on their ADOS or ADI-R scores. Again, this method was utilized because SCD was proposed as an alternate diagnosis for people who previously received a diagnosis of PDD-NOS or were less impaired but did not exhibit restricted or repetitive behaviors (APA 2013).
Results
Autism Spectrum Disorder
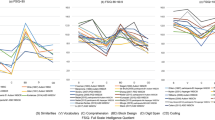
The ADOS provided fewer opportunities to assess all B criteria (restricted, repetitive patterns or behavior), as well as criterion A3 (deficits in developing, maintaining, and understanding relationships) for Module 4, as evidenced by the restricted possible score ranges (see Table 3). The means for all A criteria were above the threshold for diagnosis, with the exception of A3 of ADOS Module 4. Approximately 56% of individuals who completed Module 4 had evidence of A3 criterion based on the ADOS, but 100% of these same individuals evidenced this criterion based on the ADI-R. Repetitive behavior symptoms, as assessed by the B criteria, were less likely to be observed on either ADOS Modules 3 or 4, as all criteria except B1 were assessed by only one item (thus a score of 2 on a single item would have been required to meet the threshold for that criterion). The rates of repetitive behavior symptoms were most variable across the ADI-R. Means for ADI-R were at or above the cut-off for all B criteria, except B4 (hyper- or hyporeactivity to sensory input or unusual interest in sensory aspects of the environment). Table 3 provides means, ranges, and number of participants for the ADOS Modules 3 and 4 and the ADI-R. The ADI-R appeared to capture higher rates of repetitive behaviors, and offered a wider range of behaviors to observe or endorse when compared to the ADOS.
Table 4 depicts the percentages of individuals who demonstrated impairment on the ADOS and ADI-R alone and combined. The vast majority of individuals (91%) showed evidence of impairment on all three A criteria. Approximately 69% of individuals had evidence of at least two different types of repetitive behaviors (B criterion) based on the ADI-R. In contrast, based on the ADOS, only one individual (2.8%, Module 3) demonstrated clear evidence of at least two repetitive behaviors (B criterion). These findings are markedly different from the Mazefsky et al. (2013) observations with a sample not identified as gifted, in which 41% (Module 3) and 29% (Module 4) demonstrated evidence of at least two B criteria.
Our difference between participants who met DSM-5 ASD criteria on the ADOS alone as opposed to the ADI-R alone was more drastic than the difference reported by Mazefsky et al. (2013). Using the ADOS algorithm items alone, 37.8% of participants met full DSM-5 ASD criteria, while the ADI-R algorithm items resulted in 100% of the sample meeting full diagnostic criteria. As a result, all participants also met diagnostic criteria when the two instruments were used together. Looking at ADOS Module 3 alone, 52.7% of participants met ASD diagnostic criteria, while adding the information from ADI-R algorithm items increased this rate to 100% of individuals. Using ADOS Module 4 items alone, none of the nine participants met diagnostic criteria for ASD, but all participants met criteria when the ADI-R was also included.
Social Communication Disorder
The diagnosis of SCD is relevant for individuals who may demonstrate social difficulty without repetitive behaviors (Gibson et al. 2013). Twenty-eight participants would not have received an ASD diagnosis based on the ADOS alone (all participants met criteria when data from the ADOS and ADI-R were used). It is possible these individuals would then be considered for a SCD diagnosis if an ADI-R were not a part of the child’s comprehensive evaluation. We therefore continued to investigate the second research question that asked what percentage of those who did not meet diagnostic criteria for ASD would meet criteria for SCD. However, answering this question was problematic because no ADOS algorithm items contributed to the A4 criteria for SCD (difficulty understanding what is not explicitly stated, and nonliteral or ambiguous meanings of language). Therefore, the team members assessed all other criteria in determining an SCD diagnosis.
While criterion A3 (difficulties following rules for conversation and storytelling) had the largest possible range of scores, with seven items contributing from Module 3 and six items contributing from Module 4, the remaining criteria (A1 and A2, deficits in communication for social purposes and impairment of ability to change communication to match the context or needs of the listener) could only be assessed using one or two items for either module (see Table 5). The limited number of contributing items also impacted the ability to determine whether deficits resulted in functional limitations in effective communication, social participation, social relationships, academic achievement, or occupational performances (the B criterion). Yet, the means were at or above the threshold for diagnosis for all Module 3 criteria, with the exception of A4 (difficulty understanding what is not explicitly stated, and nonliteral or ambiguous meanings of language; as noted above, there were no algorithm items that contributed to this) and B (deficits result in functional limitations in effective communication, social participation, social relationships, academic achievement, or occupational performances, individually or in combination). Means for Module 4 criteria were at or above the threshold for diagnosis for criteria A3 and B (see Table 6).
Discussion
The purpose of this study was to determine what percentage of high ability youth diagnosed with an autism spectrum disorder under DSM-IV-TR would still meet criteria under DSM-5, based on the results from the ADI-R and ADOS, and to assess whether those who no longer met ASD criteria would meet SCD criteria. Results indicated diagnostic determination was highly dependent on what tools were used in the assessment process. Specifically, all 45 participants would receive a DSM-5 ASD diagnosis if the ADOS and ADI-R were administered in combination. However, if the ADOS was administered alone, the results changed dramatically. If solely examining the ADOS Module 3 data, 19 (52.7%) would not meet DSM-5 criteria, and if solely examining the ADOS Module 4 data, 9 (100%) would not meet DSM-5 criteria. It is therefore recommended both the ADI-R and ADOS be administered in diagnostic evaluations to avoid a large false negative rate and potential misdiagnosis among high ability populations. While administration in conjunction is recommended, it is not always practiced in clinical settings. Because the ADI-R takes 2–3 h to complete, there may be a tendency to substitute its administration with a thorough clinical interview that may miss some data the ADI-R would capture in a standardized way. With the advent of DSM-5, these tools continue to be extremely useful, but the ADOS was not as effective administered alone; the specificity went down significantly, particularly in those who were assessed using Module 4. These results are consistent with previous findings necessitating the use of clinical assessment tools and parent interviews in the diagnostic process (Huerta et al. 2012; Kulage et al. 2014).
A second important conclusion concerns criterion B (restricted patterns of behaviors). Based on our mapping of the criteria, a maximum of two ADOS items assessed each B criterion, and these behaviors must occur within the context of the assessment administration (Lord et al. 2002), even though DSM-5 emphasizes symptoms are either current or by history. In a single testing appointment, restricted patterns of behavior may not be detected, particularly among a high ability sample that may have learned to manage these symptoms in public. Therefore simply adding more criterion B items to the ADOS may not address the issue. Additionally, it is possible that high ability youth with ASD may have a distinct behavioral phenotype with respect to restricted and repetitive patterns of behavior. Among our sample, the most common criteria B symptoms observed on the ADOS were B1 (Stereotyped or repetitive motor movements, use of objects or speech) and B3 (highly restricted, fixated interests that are abnormal in intensity or focus). Examining individual items loading onto these criteria reveals interesting additional phenotypic information. Specifically, our participants demonstrated on the ADOS most frequent and significant elevations on item D4 (excessive interest in unusual or highly specific topics or objects) with observations of this symptom among 40% of participants, followed by and A4 (stereotyped/idiosyncratic language or phrases) at 29% and D2 (hand and finger and other complex mannerisms) at 18%. On the ADI-R, 87% scored a 1 or higher on item 68 (circumscribed interests); frequencies and severities were relatively similar on the other individual questions within the B1 and B3 criteria: item 33 (40%; stereotyped utterances and delayed echolalia), 77 (40%; hand and finger mannerisms), 76 (31%; unusual attachment to objects), 67 (29%; unusual preoccupations), 69 (29%; repetitive use of objects or interests in parts of objects), 78 (24%; other complex mannerisms or stereotyped body movements), and 38 (16%; neologisms/idiosyncratic language). It may be that criteria B manifest differently in high ability youth, but this requires further investigation since this is the first study to report item-level responses on the ADOS within this population. It is recommended practitioners be cognizant criterion B symptoms may not detected by an ADOS but that circumscribed interests are very commonly reported on the ADI-R by parents of high ability children with ASD.
SCD has been proposed to be an accurate diagnosis for those who no longer meet criteria for ASD in the DSM-5 (Greaves-Lord et al. 2013). Others have questioned the ability of SCD to “catch” individuals who fall below the ASD diagnostic threshold (Kulage et al. 2014), which is inconsistent with what was proposed following the DSM-5 Field Trial (Regier et al. 2013). Instead, it is possible students may be misdiagnosed as having SCD if the gold standard in autism diagnostics is not used in clinical settings. Because not all clinicians administer both the ADOS and ADI-R, an SCD diagnosis could be considered if a child does not meet the threshold for ASD following ADOS administration.
The 28 participants who would not receive a DSM-5 ASD diagnosis based on the ADOS data alone were evaluated in comparison to DSM-5 SCD criteria. Examination of the SCD matrix (see Table 2) reveals there are no ADOS algorithm items that assess for SCD criterion A4 (understanding and use of sarcasm, idioms, and humor). Additionally, A1 (social communication appropriate for the social context), A2 (altering language for context), and B have a limited number of ADOS Modules 3 and 4 algorithm items assessing deficits in these areas. If an ADI-R was also administered, it would allow for verification of symptoms in all domains that may not be displayed during the 40–60 min ADOS. Available measures of pragmatic language to supplement the comprehensive evaluation include the Children’s Communication Checklist-2 (CCC-2; Bishop 2006), which is considered a screening instrument, and modules within the Test of Pragmatic Language (TOPL; 2nd Ed.; Phelps-Teraski and Phelps-Gunn 2007) and the Social Learning Developmental Test (Bowers et al. 2008). Best practice recommendations for diagnosing pragmatic language impairments include standardized assessments of pragmatics in conjunction with informal observations and receptive and expressive language measures (Young et al. 2005), yet psychologists and psychiatrists rarely administer these tests (Brukner-Wertman et al. 2016). There continues to exist a shortage of tools that accurately reflect the dynamic nature of pragmatic language itself (Adams 2015) and assess for SCD in a standardized, valid, and reliable way (Brukner-Wertman et al. 2016; Norbury 2014). Therefore, at present, there does not appear to be best-practice assessments for comprehensive evaluation of SCD among high ability populations.
Limitations
This study has several limitations. First, the sample size was small, which limits the generalizability of the findings. However, this is a low incidence population (i.e., having both high ability and ASD), which makes finding large sample sizes challenging. There is enough evidence, however, to suggest ASD manifests differently among high ability populations (Doobay et al. 2014; Foley-Nicpon et al. 2010), and current findings support this conclusion. Second, there was no existing matrix for mapping ADOS and ADI-R algorithm items to SCD. While the authors worked together to create this matrix, there was no foundation from which to draw and, thus, bias could have impacted our ability to objectively categorize items. Third, we did not have a comparison group, which would have allowed deciphering whether sensitivity and specificity differences existed depending on one’s ability. Finally, this was not a true replication of the Mazefsky et al. (2013) study, which limits generalizability across studies. However, the procedural similarities far outweighed the differences and were grounded in slightly different interpretations of the ADOS and ADI-R items and how they mapped onto the DSM-5 diagnoses.
Conclusions and Recommendations
Based on our results, the ADOS and ADI-R administered in conjunction have excellent specificity for identifying ASD among high ability populations. It is insufficient to administer the ADOS alone, which is not recommended for best practice (Lord et al. 2012), but may occur in clinical settings. Among high ability populations, criterion B symptoms are not always displayed during ADOS administration, but a large portion of parents report on the ADI-R observing circumscribed interests. Furthermore, the ADOS will not suffice in making a diagnosis of SCD because there is an insufficient number of items per diagnostic criteria, especially since all criteria A must be met. There is a pressing need to develop additional empirically validated instruments to accurately diagnose SCD in populations of individuals, including those who are high ability, who have social communication difficulties without restricted, repetitive patterns of behavior.
References
Adams, C. (2015). Assessment and intervention for children with pragmatic language impairment. In D. A. Hwa-Froelich (Ed.), Social communication development and disorders (pp. 141–170). New York: Psychology Press.
American Psychiatric Association (2013). Diagnostic and statistical manual of mental disorders (5th Ed.). Washington, DC: Author.
Assouline, S. G., Foley Nicpon, M., & Dockery, L. (2011). Predicting the academic achievement of gifted students with autism spectrum disorder. Journal of Autism and Developmental Disabilities. doi:10.1007/s10803-011-1403-x.
Assouline, S. G., Foley Nicpon, M., & Doobay, A. (2009). Profoundly gifted girls and autism spectrum disorder: A psychometric case study comparison. Gifted Child Quarterly, 53(2), 89–106. doi:10.1177/0016986208330565.
Bishop, D. (2006). Children’s Communication Checklist-2 (U.S. ed.). San Antonio, TX: Harcourt Assessment.
Bowers, L., Huisingh, R., & LoGiudice, C. (2008). Social learning developmental test: elementry. East Moline: Linguisystems.
Brennan, L., Barton, M., Chen, C.-M., Green, J., & Fein, D. (2014). Detecting subgroups in children with pervasive developmental disorders—not otherwise specified. Journal of Autism Developmental Disorders, 45(5), 1329–1344.
Brukner-Wertman, Y., Laor, N., & Golan, O. (2016). Social (pragmatic) communication disorder and its relation to the autism spectrum: Dilemmas arising from the DSM-5 classification. Journal of Autism and Developmental Disorders, 46(8), 2821–2829. doi:10.1007/s10803-061-2814-5.
Calhoun, S. L., & Mayes, S. D. (2005). Processing speed in children with clinical disorders. Psychology in the Schools, 42, 333–342.
Cholemkery, H., Medda, J., Lempp, T., & Freitag, C. M. (2016). Classifying autism spectrum disorders by ADI-R: Subtypes or severity gradient? Journal of Autism and Developmental Disorders, 46(7), 2327–2339. doi:10.1007/s10803-016-2760-2.
Cicchetti, D. V., Lord, C., Koenig, K., Ami, K., & Volkmar, F. R. (2008). Reliability of the ADI-R: Multiple examiners evaluate a single case. Journal of Autism and Developmental Disorders, 38, 764–770. doi:10.1007/s10803-007-0448-3.
de Bildt, A., Oosterling, I. J., van Lang, N. D. J., Kuijper, S., Dekker, V., Sytema, S., et al. (2013). How to use the ADI-R for classifying autism spectrum disorders? Psychometric properties of criteria from the literature in 1204 Dutch children. Journal of Autism and Developmental Disorders. doi:10.1007/s10803-013-1783-1.
Doobay, A. F., Foley-Nicpon, M., Ali, S., & Assouline, S. G. (2014). Cognitive, adaptive and psychosocial differences between high ability youth with and without autism spectrum disorders. Journal of Autism and Developmental Disorders, 44, 2026–2040. doi:10.1007/s10803-014-2082-1.
Foley Nicpon, M., Assouline, S., & Stinson, R. (2012). Cognitive and academic distinctions between gifted students with autism and Asperger Syndrome. Gifted Child Quarterly, 56, 77–89.
Foley Nicpon, M., Doobay, A., & Assouline, S. G. (2010). Parent, teacher, and self perceptions of psychosocial functioning in intellectually gifted children and adolescents with autism spectrum disorder. Journal of Autism and Developmental Disabilities, 40(8), 1028–1038. doi:10.1007/s10803-010-0952-8.
Frazier, T. W., Youngstrom, E. A., Speer, L., Embacher, R., Law, P., et al. (2012). Validation of proposed DSM-5 criteria for autism spectrum disorder. Journal of the American Academy of Child and Adolescent Psychiatry, 51(1), 28).
Gibbs, V., Aldridge, F., Chandler, F., Witzlsperger, E., & Smith, K. (2012). Brief report. An exploratory study comparing diagnostic outcomes for autism spectrum disorders under DSM-IV-TR with the proposed DSM-5 revision. Journal of Autism and Developmental Disabilities, 42, 1750–1756. doi:10.1007/s10803-012-1560-6.
Gibson, J., Adams, C., Lockton, E., & Green, J. (2013) Social communication disorder outside autism? A diagnostic classification approach to delineating pragmatic language impairment, high functioning autism, and specific language impairment. Journal of Child Psychology and Psychiatry, 54(11), 1186–1197.
Gotham, K., Risi, S., Pickles, A., & Lord, C. (2007). The autism diagnostic observation schedule: Revised algorithms for improved diagnostic validity. Journal of Autism Developmental Disorders, 37, 613–627.
Greaves-Lord, K., Eussen, M. L., Verhulst, F. C., Minderaa, R. B., Mandy, W., Hudziak, J. J., et al. (2013). Empirically based phenotypic profiles of children with pervasive developmental disorders: Interpretation in the light of the DSM-5. Journal of Autism and Developmental Disorders, 43(8), 1784–1797.
Huerta, M., Bishop, S. L., Duncan, A., Hus, V., & Lord, C. (2012). Application of DSM-5 criteria for autism spectrum disorder to three samples of children with DSM-IV diagnoses of pervasive developmental disorders. American Journal of Psychiatry, 169(10), 1056–1064. doi:10.1176/appi.ajp.2012.12020276.
Kamp-Becker, I., Ghahreman, M., Heinzel-Gutenbrunner, M., Peters, M., Remschmidt, H., & Becker, K. (2013). Evaluation of the revised algorithm of autism diagnostic observation schedule (ADOS) in the diagnostic investigation of high-functioning children and adolescents with autism spectrum disorders. Autism: The International Journal of Research and Practice, 17(1), 87–102. doi:10.1177/1362361311408932.
Kulage, K. M., Smaldone, A. M., & Cohn, E. G. (2014). How will DSM-5 affect autism diagnosis? A systematic literature review and meta-analysis. Journal of Autism and Developmental Disorders, 44, 1918–1932. doi:10.1007/s10803-0114-2065-2.
Lecavalier, L., Aman, M. G., Scahill, L., Mcdougle, C. J., Mccracken, J. T., Vitiello, B., et al. (2006). Validity of the autism diagnostic interview-revised. American Journal on Mental Retardation, 111, 199–215. doi:10.1352/0895-8017(2006)111[199:VOTADI]2.0.CO;2.
Lord, C., & Bishop, S. L. (2015). Recent advances in autism research as reflected in DSM-5 criteria for autism spectrum disorder. Annual Review of Clinical Psychology, 11, 53–70. doi:10.1146/annurev-clinpsy-032814-112745.
Lord, C., Petkova, E., Hus, V., Gan, W., Lu, F., et al. (2012). A multisite study of the clinical diagnosis of different autism spectrum disorders. Archives of General Psychiatry, 69, 306–313.
Lord, C., Risi, S., Lambrecht, L., Cook, E. H. Jr., Leventhal, B. L., DiLavore, P. C., et al. (2000). The autism diagnostic observation schedule-generic: A standard measure of social and communication deficits associated with the spectrum of autism. Journal of Autism and Developmental Disorders, 30(3), 205–223.
Lord, C., Rutter, M., DiLavore, P. C., & Risi, S. (2002). Autism diagnostic observation schedule. Los Angeles: Western Psychological Services.
Lord, C., Rutter, M., DiLavore, P. C., Risi, S., Gotham, K., & Bishop, S. L. (2012). Autism diagnostic observation schedule, 2nd ed. (ADOS-2). Torrance, CA: Western Psychological Services.
Lord, C., Rutter, M., & Le Couteur, A. (1994). Autism Diagnostic Interview-Revised: A revised version of a diagnostic interview for caretakers of individuals with possible pervasive developmental disorders. Journal of Autism and Developmental Disorders, 24, 659–685. doi:10.1007/BF02172145.
Mayes, S. D., & Calhoun, S. L. (2007). Learning, attention, writing, and processing speed in typical children and children with ADHD, autism, anxiety, depression, and oppositional-defiant disorder. Child Neuropsychology, 13, 469–493.
Mayes, S. D., & Calhoun, S. L. (2008). WISC-IV and WIAT-II profiles in children with high functioning autism. Journal of Autism and Developmental Disorders, 38, 428–493.
Mazefsky, C. A., McPartland, J. C., Gastgeb, H. Z., & Minshew, N. J. (2013). Brief report: Comparability of DSM-IV and DSM-5 ASD research samples. Journal of Autism and Developmental Disabilities, 43, 1236–1242. doi:10.1007/s10803-012-0665y.
McPartland, J. C., Reichow, B., & Volkmar, F. R. (2012). Sensitivity and specificity of proposed DSM-5 diagnostic criteria for autism spectrum disorder. Journal of the American Academy of Child and Adolescent Psychiatry, 51(4), 368–383. doi:10.1016/j.jaac.2012.01.007.
Norbury, C. F. (2014). Practitioner review: Social (pragmatic) communication disorder conceptualization, evidence and clinical implications. Journal of Child Psychology and Psychiatry, 55(3), 204–216. doi:10.1111/jcpp.12154.
Oliveras-Rentas, R. E., Kenworthy, L., Roberson, R. B., Martin, A., & Wallace, G. (2012). WISC-IV profile in high-functioning autism spectrum disorders: Impaired processing speed is associated with increased autism communication symptoms and decreased adaptive communication abilities. Journal of Autism and Developmental Disorders, 42, 655–664.
Phelps-Teraski, D., & Phelps-Gunn, T. (2007). Test of Pragmatic Language (2nd edn.). Austin, TX: Pro-Ed.
Regier, D. A., Narrow, W. E., Clarke, D. E., Kraemer, H. C., Kuramoto, S. J., Kuhl, E. A., et al. (2013). DSM-5 field trials in the United States and Canada, Part II: Test–retest reliability of selected categorical diagnoses. American Journal of Psychiatry, 170(1), 59–70. doi:10.1176/appi.ajp.2012.12070999.
Reis, S. M., Baum, S. M., & Burke, E. (2014). An operational definition of twice-exceptional learners: Implications and applications. Gifted Child Quarterly, 58, 217–230.
Risi, S., Lord, C., Gotham, K., Corsello, C., Chrysler, C., Szatmari, P., et al. (2006). Combining information from multiple sources in the diagnosis of autism spectrum disorders. Journal of the American Academy of Child and Adolescent Psychiatry, 45(9), 1094–1103.
Rutter, M., Le Couteur, A., & Lord, C. (2003). Autism diagnostic interview-revised. Los Angeles, CA: Western Psychological Services.
Swineford, L. B., Thurm, A., Baird, G., Wetherby, A. M., Swedo, S. (2014). Social (pragmatic) communication disorder: A research review of this new DSM-5 diagnostic category. Journal of Neurodevelopmental Disorders, 6, 1.
Van Steensel, F. J. A., Bogels, S. M., & de Bruin, E. I. (2015). DSM-IV versus DSM-5 autism spectrum disorder and social anxiety disorder in childhood: Similarities and differences. Journal of Child and Family Studies, 24(9), 2752–2756. doi:10.1007/s10826-014-0087-2.
Wilson, C. E., Gillan, N., Spain, D., Robertson, D., Roberts, G., Murphy, C. M., et al. (2013). Comparison of ICD-10R, DSM-IVTR and DSM-5 in an adult autism spectrum disorder diagnostic clinic. Journal of Autism and Developmental Disorders, 43, 2515–2525. doi:10.1007/s10803-013-1799-6.
Worley, J. A., & Matson, J. L. (2012). Comparing symptoms of autism spectrum disorders using the current DSM-IV-TR diagnostic criteria and the proposed DSM-V diagnostic criteria. Research in Autism Spectrum Disorders, 6(2), 965–970.
Young, E. C., Diehl, J. J., Morris, D., Hyman, S. L., & Bennetto, L. (2005). The use of two language tests to identify pragmatic language problems in children with autism spectrum disorders. Language, Speech, and Hearing Services in Schools, 36, 62–72.
Acknowledgments
This research was supported in part by a grant from the U.S. Department of Education Jacob K. Javits Program obtained by the Iowa Department of Education and the Belin-Blank International Center for Gifted Education and Talent Development. The authors gratefully acknowledge the students and parents who participated in the research through the Assessment and Counseling Clinic of The University of Iowa Belin-Blank Center.
Author Contributions
Conceptualization, MFN, SLF and KGW; Methodology, MFN, SLF, and KGW; Formal Analysis, MFN, SLF, and KGW; Resources, SGA; Writing - Original Draft, MFN, SLF, and KGW; Writing - Reviewing and Editing, MFN; Visualization, SLF and KGW, Supervision, MFN; Funding Acquisition, SGA.
Funding
This study was funded by the U.S. Department of Education Jacob K. Javits Gifted and Talented Education Act.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There are no known conflicts of interest to report.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the University of Iowa’s research committee (IRB) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Foley-Nicpon, M., L. Fosenburg, S., G. Wurster, K. et al. Identifying High Ability Children with DSM-5 Autism Spectrum or Social Communication Disorder: Performance on Autism Diagnostic Instruments. J Autism Dev Disord 47, 460–471 (2017). https://doi.org/10.1007/s10803-016-2973-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10803-016-2973-4