Abstract
Diabetic retinopathy (DR) is a frequent complication of diabetes mellitus, and a common cause of vision impairment and blindness in these patients, yet many aspects of its pathogenesis remain unresolved. Furthermore, current treatments are not effective in all patients, are only indicated in advanced disease, and are associated with significant adverse effects. This review describes the microvascular features of DR, and how pericyte depletion and low-grade chronic inflammation contribute to the pathogenesis of this common ophthalmic disorder. Existing, novel and investigational pharmacological strategies aimed at modulating the inflammatory component of DR and ameliorating pericyte loss to potentially improve clinical outcomes for patients with diabetic retinopathy, are discussed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
DR is one of the most common complications of diabetes mellitus, and a leading cause of vision loss, yet its pathogenesis remains incompletely understood. DR is characterised by retinal microvascular dysfunction and degeneration, with disruption of the retinal neurovascular unit (rNVU) and subsequent blood-retinal barrier (BRB) dysfunction. Pericyte dysfunction and loss is an early feature of this process. This occurs in a local and systemic diabetic environment characterised by chronic low-grade inflammation with maladaptive sequalae. Understanding the role of retinal inflammation in the pathophysiology of DR, particularly how it relates to microvascular degeneration and pathological neovascularisation, is critical in order for the development of novel therapies to complement, or improve upon, current treatment options. This review describes what is currently known about the role of inflammation in the pathogenesis of DR, with particular emphasis on pericyte dysfunction and dropout, and associated retinal microvascular dysfunction and degeneration. Current therapies for DR are discussed, along with new and potential treatment strategies aimed at controlling or reversing DR though mitigation of DR-associated inflammation or via direct pharmacological protection of pericytes to preserve the rNVU.
Diabetic retinopathy
Approximately one-third of the world’s diabetic population have DR, and a third of this population have vision-threatening retinopathy (Cheung et al. 2010). Vision is primarily affected when two late-stage complications occur, namely diabetic macular oedema and proliferative DR (Cheung et al. 2010; Rubsam et al. 2018; Wang and Lo 2018). These sight threatening complications occur with either type I (juvenile-onset or insulin-dependent) or type II (maturity-onset) diabetes mellitus (Eagle 2011; Lim 2019).
DR may be divided into two stages based upon the proliferation status of the retinal microvasculature: an early, non-proliferative (NPDR) phase and a later proliferative (PDR) phase. An initial, and seemingly invariable, feature of NPDR is degeneration and depletion of capillary pericytes, the mural cells that wrap around capillary endothelial cells (Frank 2004; Wang and Lo 2018). Pericyte loss is followed by endothelial cell (EC) loss, both executed by apoptosis (Frank 2004; Wang and Lo 2018). Although capillary pericyte degeneration occurs in other diseases, it is much more severe in a retina with DR, suggesting that additional local factors in the intraocular microenvironment contribute to this profound pericyte loss. Low-grade, subclinical inflammation is present throughout the development of DR, likely contributing to pericyte depletion (Adamis 2002). The pericyte secretome, the tissue- and stimulus-specific pro- and anti-inflammatory factors, growth factors, and extracellular matrix secreted in response to changes in the retinal microenvironment, also has a role in modulating DR inflammatory events (Frank 2004; Gaceb and Paul 2018; Vujosevic and Toma 2018).
The International Clinical Disease Severity Scale for DR, a 5-stage clinical disease severity classification system, was developed in 2003 (Wilkinson et al. 2003). The first 3 stages (no apparent retinopathy, mild NPDR characterised by a few microaneurysms, and moderate NPDR with more microaneurysms and intraretinal haemorrhages) may progress to a fourth stage of severe NPDR and a fifth stage of PDR. Diabetic macular oedema is independently classified as apparently present or absent, with a further assessment of the distance of the oedema from the central macula. The advent of new technologies for the evaluation of DR may lead to enhancements of current classification systems; however, the basis for DR staging is likely to remain largely unchanged (Wu et al. 2013).
The early stage of DR is characterised by BRB breakdown, which leads to retinal oedema (the major cause of visual loss in type 2 diabetic patients), haemorrhages, exudates, and capillary microaneurysms (Cheung et al. 2010). Weakening of capillary walls due to focal pericyte loss is important in the development of microaneurysms, many of which are cellular, suggesting that endothelial cell (EC) proliferation could be involved in their formation (Stitt et al. 1995). The characteristic ‘soft exudates’, or ‘cotton-wool spots’, observed in DR are not true exudates, but rather represent focal areas of impeded axoplasmic flow, caused by focal retinal ischaemia resulting from pre-capillary arteriolar thrombosis (Garner 1993). Histologically, cotton wool spots are dilated axons in the nerve fibre layer filled with eosinophilic axoplasm. They contain oval-shaped cytoid bodies, which have an eosinophilic, nucleus-like structure composed of aggregated organelles (Garner 1993; Eagle 2011). Retinal neovascularisation occurs in the later, proliferative phase of DR and predisposes to vitreous haemorrhage, the organisation of which contributes to fibroplasia with corresponding retinal and vitreous fibrosis, leading to eventual total blindness from tractional retinal detachment (Lim 2019). Figures 1, 2, 3, and 4 are colour fundus photographs demonstrating typical clinical features of NPDR and PDR. Figures 5 and 6 demonstrate typical features of PDR seen with fundus fluorescein angiography.
Proliferative diabetic retinopathy and macular oedema in the left eye of a patient previously treated with pan-retinal photocoagulation (green arrows) and focal laser (blue arrows) photocoagulation, highlighting previous neovascularisation (purple arrow) and lipid exudates (black arrows) (colour figure online)
Severe proliferative diabetic retinopathy in the left eye. Areas of neovascularisation at the disc (red arrows) are visible, as is previous pan-retinal (green arrows) and focal laser scars (blue arrows), retinal haemorrhages (purple arrows) and exudates near the fovea (yellow arrows) (colour figure online)
Pericytes
Pericytes were first described by Carl Eberth in Germany in 1871, and independently by Charles-Marie Rouget in France in 1873, and named “Rouget cells”. However, in recognition of their perivascular location, they were renamed “pericytes” by the German anatomist, Karl Zimmermann, in 1923 (Trost et al. 2016; Harrell et al. 2018).
Although the pericyte, sequestered in its perivascular niche, has for too long been underappreciated, the important functions of these vascular cells are now increasingly being recognised. Pericytes are specialised mural cells which occupy a perivascular site at the abluminal aspect of microvessels (Trost et al. 2016). They are embedded in the same basement membrane that embraces ECs, and extend processes along, and around, pre-capillary arterioles, capillaries, and post-capillary venules, covering several ECs and their connecting tight junctions (Armulik et al. 2011). Attachment of pericytes to the basement membrane helps regulate their functions, which become altered if detachment occurs (Harrell et al. 2018; Geranmayeh et al. 2019). The basement membrane between pericytes and ECs is thin in the retina, permitting close interaction between these cells. Pericytes have both anti-apoptotic and anti-proliferative effects on ECs and, accordingly, depletion of pericytes compromises the vascular architecture (Harrell et al. 2018; Trost et al. 2016). Contact between pericytes and ECs occurs in two forms. At “peg-and-socket” type junctions, pericyte cytoplasmic projections (pegs) are inserted into EC invaginations (sockets), while, at adherent junctions, microfilaments attached to the pericyte plasma membrane are embedded in the contiguous EC cytoplasm (Harrell et al. 2018). No intercellular junctions have been identified between pericytes.
Pericyte coverage in the retina, and their topographical density, is higher than in any other tissue, ensuring optimal integrity of the retinal microvasculature. The pericyte:EC ratio in the retina is 1:1, compared to 1:2.5 in the kidney, 1:5 in the cerebral cortex, 1:10 in the lung, and 1:100 in skeletal muscle (Armulik et al. 2011; Smith et al. 2012; Schallek et al. 2013; Rudziak et al. 2019). Their abundance in the retina emphasises the important structural and functional roles entrusted to these cells. Retinal coverage by pericytes is widely regarded to be essential for EC survival, especially with stressors such as the hyperglycaemia of diabetes mellitus (Hammes et al. 2002; Trost et al. 2016; Park et al 2017; Harrell et al. 2018). Pericytes are not considered to be capable of replication in the adult retina (Alikhani et al. 2010).
Pericytes are a heterogeneous population of cells, with a dual origin from neuroectodermal and mesodermal germ layers, the former neural crest cells predominating (Trost et al. 2016). There are also different subtypes of pericytes, subserving different functions (Santos et al. 2018). In the brain, and probably also the retina, pericytes in certain microvascular regions appear to have different functions (Attwell et al. 2016). Those in pre-capillary arterioles have more circumferential processes and express more smooth muscle α-actin, equipping them for a role in the regulation of cerebral blood flow. Pericytes in capillaries, by contrast, appear to be more responsible for blood–brain barrier (BBB) maintenance, while those in post-capillary venules control the entry of immune cells into the brain (Attwell et al. 2016).
Depending on the prevailing pathological state, signalling pathways can encourage pericytes to assume a variety of morphologies and functions, and express different marker profiles (Santos et al. 2018). However, one of the major impediments to defining the different roles of pericytes has been the difficulty in precisely identifying these cells as there is no single molecular marker for pericytes, in part due to the varied lineage and pluripotent capability (Trost et al. 2016). The expression of histological markers may also alter in response to different retinal pathologies, these conditions engendering diverse and often complex signalling mechanisms. The failure to precisely identify pericytes has produced conflicting experimental results and, as a result, some of the putative functions of this cell type remain controversial (Santos et al. 2018). Moreover, in vitro culture conditions create a different microenvironment to that of the in vivo retina, and may influence the behaviour of pericytes, rendering extrapolation of in vitro results to the living eye problematic (Armulik et al. 2011). Histological pericyte identification requires a combination of perivascular location, morphology, and at least two pericyte molecular markers (Armulik et al. 2011). For identification of retinal pericytes, a combination of nerve fibre/glial antigen 2 (NG2) and platelet-derived growth factor receptor beta (PDGFRβ) is recommended; however, in vitro and in vivo antigen expression may differ (Trost et al. 2016; Harrell et al. 2018). Moreover, expression of pericyte markers is dynamic and varies between different tissues, developmental stages, and the state of activation (Armulik et al. 2011; Trost et al. 2016; Santos et al. 2018; Geranmayeh et al. 2019).
Pericytes in the brain, and possibly also in the retina, have many similarities to mesenchymal stem cells (MSC) (Lange et al. 2013). They possess a pluripotent differentiation potential, enabling them to generate a variety of cell types. Multipotent pericytes can transdifferentiate into neural cells (neurons, astrocytes, microglia, and oligodendrocytes), mesenchymal cells (adipocytes, chondrocytes, osteoblasts, fibroblasts, myofibroblasts), and vascular smooth muscle cells (vSMC) (Trost et al. 2016). In a manner similar to MSC, pericytes become activated by inflammatory mediators then function to attenuate inflammation and promote tissue repair (Lange et al. 2013; Mendel et al. 2013; Trost et al. 2016).
The neurovascular unit and blood-retinal barrier
Pericytes are part of the rNVU. The rNVU is comprised of neurons, glia (astrocytes, Müller cells, and microglia), vascular ECs, and pericytes (Sweeney et al. 2016). The rNVU regulates blood flow to meet changing retinal metabolic demands and, therefore, is critical for maintenance of homeostasis (Sweeney et al. 2016). It is an essential component of retinal inflammatory responses (Hill et al. 2014; Sweeney et al. 2016; Duh et al. 2017).
The BRB, which resembles the BBB in most respects, forms the vascular component of the rNVU, and plays an important role in homeostatic regulation of the retinal microenvironment (Kaur et al. 2008). It is divided into inner and outer parts. The inner BRB (iBRB) is formed by tight junctions (zonulae occludentes) between contiguous retinal capillary ECs, which rest on a basement membrane covered by the foot processes of astrocytes and Müller cells (Cunha-Vaz et al. 2011). The latter cells, together with pericytes, contribute to the proper functioning of the iBRB but, since pericytes do not form a continuous perivascular layer, their contribution to a diffusion barrier is limited (Cunha-Vaz et al. 2011). The outer BRB (oBRB) is formed by tight junctions between retinal pigment epithelial (RPE) cells (Cunha-Vaz et al. 2011). The iBRB maintains the integrity of the inner two-thirds of the retina, while the oBRB maintains the outer one-third. The eye is an immune-privileged site largely due to the BRB and the immunosuppressive intraocular environment, with entry of leucocytes restricted and the RPE serving an immunomodulatory role. (Kaur et al. 2008; Cunha-Vaz et al. 2011).
There is an intimate relationship between EC and pericytes, involving paracrine (cell-to-cell) and juxtacrine (close contact-dependent) signalling, this communication being required for normal pericyte function and BRB maintenance. Factors involved in this intercellular signalling include PDGF-B, transforming growth factor β (TGFβ), sphingosine-1-phosphate, and Notch (Armulik et al. 2011).
Pericyte apoptosis
Pericyte apoptosis has been suggested to occur by a number of mechanisms: (1) diabetic hyperglycaemia-induced reduction in PDGF-B/PDGFRβ signalling; (2) disruption of protective EC-pericyte signalling by EC-secreted angiopoietin-2 (Ang2); (3) microglial pro-inflammatory-mediated activation of pro-apoptotic, and inhibition of pro-survival molecules; (4) reactive oxygen species (ROS) damage to pericyte mitochondria, releasing cytochrome C, and activating the caspase-dependent apoptotic cascade; (5) generation of tumour necrosis factor-alpha (TNF-α) and advanced glycation end-products (AGES) which are formed when reducing sugars such as glucose react in a non-enzymatic manner with nucleic acids, proteins, and lipids, both of which bind to receptors on pericytes, inducing apoptosis through activation of the transcription factor, Forkhead box 01 (FOX01); and (6) glutamate excitotoxicity (Barber et al. 2011; Beltramo and Porta 2013; Eshaq et al. 2017; Ferland-McCollough et al. 2017; Kusuhara et al. 2018).
Loss of pericytes, attended by EC degeneration and basement membrane thickening, results in the eventual formation of acellular capillaries, which are basement membrane-lined tubes, devoid of ECs and pericytes (Garner 1993). These abnormal capillaries are prone to microaneurysm formation and haemorrhage, and are associated with vascular occlusion, sometimes abetted by thrombosis secondary to residual EC injury, leading to a failure of perfusion and ischaemic-hypoxic retinal injury (Ferland-McCollough et al. 2017). Ischaemia-hypoxia causes increased expression of vascular endothelial growth factor (VEGF) by ECs and glial cells, produced, in part, by upregulation of hypoxia-inducing factor 1 (Ferland-McCollough et al. 2017). Loss of structural support for retinal capillaries by pericyte depletion, and EC degeneration, can produce a localised weakness of the vessel wall, exacerbated by increased capillary blood flow and intraluminal pressure and dysfunction of attached glia, leading to a mural outpouching or microaneurysm (Ferland-McCollough et al. 2017). When a microaneurysm ruptures, haemorrhage occurs.
Pericyte loss also contributes to BRB disruption, increased vascular permeability, and vasogenic macular oedema (Ferland-McCollough et al. 2017). The latter is an important cause of vision loss as the macula is the central portion of the retina, responsible for the greatest visual acuity. While high levels of Ang2 expression from ECs in the diabetic retina might exacerbate pericyte apoptosis, pericyte loss itself leads to reduced expression of Ang1 (from pericytes), which in turn may result in further BRB dysfunction through a reduction in the EC-pericyte stabilising effect of Ang1/Tie2 interaction (Armulik, Abramsson and Betsholtz 2005). BRB destabilisation by Ang2/Tie2 stimulation is associated with the progression to PDR which is heralded by the formation of new blood vessels (angiogenesis), the angiogenic response of ECs being regulated by inflammatory cytokines and growth factors (Armulik, Abramsson and Betsholtz 2005; Cheung et al. 2010). These leaky, fragile, immature blood vessels also contribute to retinal oedema and haemorrhage.
Retinal inflammation
Inflammation is a “double-edged sword”, being a host defence response to tissue injury and promoting homeostasis in the short-term but, when triggered inappropriately, and especially when chronically activated, inflammation can be detrimental and drive the progression of diseases such as DR. DR has many of the characteristics of a low-grade, subclinical, chronic inflammatory disease, and localised inflammatory processes play a role in many of the microvascular changes which form part of the DR morphological expression (Tang and Kern 2011). Pericyte depletion, for example, is one of the earliest pathological changes in DR, which is produced, in part, by retinal inflammation (Kowluru et al. 2010; Tang and Kern 2011; Whitcup et al. 2013; Ogura et al. 2017).
The diabetic environment provokes increased local and systemic expression of inflammatory cytokines, chemokines, and growth factors, all of which are involved in the development of DR by creating a pro-inflammatory milieu (Tang and Kern 2011; Shabab et al. 2017; Rubsam et al. 2018). Several pro-inflammatory mediators have been detected at increased levels in the aqueous fluid, vitreous and serum of patients with DR, with higher levels being associated with more advanced stages of DR (Vujosevic and Simo 2017; Wu et al. 2017; Rubsam, Parikh and Fort 2018). The inflammatory mediators that have been found to be involved in DR include vascular adhesion molecules, pro- and anti-inflammatory cytokines, pro-inflammatory/angiogenic chemokines, anti-inflammatory/anti-angiogenic chemokines, transcription factors, pro-inflammatory/angiogenic and anti-inflammatory/anti-angiogenic growth factors, anti-inflammatory/pro-angiogenic growth factors, and innate immune response cells (retinal EC with toll-like receptors) (Vujosevic and Toma 2018).
Leucostasis, caused by leucocyte-EC adhesion occurs early in DR, contributing to microvascular occlusion (Joussen et al. 2004; Tang and Kern 2011). It also leads to EC damage and loss by apoptosis, enacted by the Fas/Fas ligand pathway, contributing to BRB disruption (Joussen et al. 2003; Duh et al. 2017). Leucostasis is amplified due to hyperglycaemia-induced increased expression of leucocyte integrins (CD11a, CD11b, and CD18), which bind to EC leucocyte chemo-attractant adhesion molecules (intercellular adhesion molecule-1 (ICAM-1), vascular cell adhesion molecule-1 (VCAM-1), platelet endothelial cell adhesion molecule 1 (PECAM 1), and E- and P-selectins) (Joussen et al. 2004; Wang et al. 2012; Kastelan et al. 2013). Chemokines, such as monocyte chemotactic protein-1 (MCP-1), macrophage inflammatory protein-1α (MIP-α), and MIP-β, which attract and activate leucocytes, and inflammatory cytokines (tumour necrosis factor alpha (TNF-α), interleukin-6 (IL-6), IL-8, and IL-1β), are increased in DR and contribute to this process (Kastelan et al. 2013).
Glial activation and neurodegeneration accompany the microvascular changes in DR. Müller cells, the principal retinal macroglial cells, react to hyperglycaemia by reactive gliosis and production of pro-inflammatory cytokines (Rubsam et al 2018). Microglia, the major resident immunocompetent cells in the central nervous system, become activated in DR, migrate from the inner-to-outer retinal layers, and increase secretion of TNF-α, IL-6, MCP-1, and VEGF (Duh et al. 2017; Madiera et al. 2015). Astrocytes also amplify the inflammatory process by producing pro-inflammatory cytokines (Duh et al. 2017; Madiera et al. 2015). Retinal neurodegeneration occurs early in DR with neuronal apoptosis, retinal ganglion cells being damaged initially, followed by outer nuclear layer neurons and associated photoreceptors (Barber et al. 2011; Rubsam et al. 2018).
Activated pericytes also contribute to retinal inflammation in DR. In the presence of inflammatory cytokines such as interferon gamma (IFN-Y), IL-17, TNF-α, and IL-1β, pericytes secrete a plethora of chemokines and cytokines to attract immune cells to the site of retinal inflammation (Harrell et al. 2018). These pro-inflammatory mediators include IL-1β, IL-6, TNF-α, reactive oxygen species (ROS), nitric oxide, low density lipoprotein receptor-related protein-1, and matrix metalloproteinases (MMP2 and MMP9) for activation of microglia, astrocytes and ECs (Hill et al. 2014). They also secrete anti-inflammatory factors such as IL-10 (Harrell et al. 2018). Pericytes may also directly regulate blood flow, enhancing the delivery of leucocytes to injured areas of the retina (Armulik et al. 2011). They release chemokine ligand 10 (CXCL10), which attracts helper CD4 + and CD8 + cytotoxic T lymphocytes and natural killer (NK) cells to sites of inflammation, while pericyte-derived CXCL8 and CXCL1 recruit neutrophils (Jansson et al. 2014). Moreover, pericytes produce MCP-1, MIP-α, and chemokine ligand 5 (CCL5), which bind to CCR2, CCR3, and CCR5, respectively, to modulate monocyte, macrophage, and CD4, CD8 and NK cell trafficking (Harrell et al. 2018). Pericytes constitutively express major histocompatibility complex (MHC) class 1 and, in vitro, can be stimulated by IFN-Y to express MHC class II, indicating their potential to act as professional antigen presenting cells (APCs) (Hill et al. 2014; Harrell et al. 2018).
Leucocytic passage across microvessels is a critical event in retinal inflammation, permitting their recruitment to sites of tissue damage. In response to stimulation by cytokines and chemokines, the role of the pericyte changes from one of stabilisation of ECs to one where it modifies the BRB in ways that assist the transendothelial passage of inflammatory cells into the retina (Hill et al. 2014). In this migration across the vascular wall, neutrophils (and monocytes) must traverse the vascular endothelium, the pericyte sheath, and their associated basement membrane, with the result that they often tend to accumulate between the endothelium and the vascular basal lamina. In inflammation, pericytes downregulate tight junction proteins and remodel the basement membrane to foster leucocytic transmigration, a process aided by BRB breakdown from pericyte-derived MMPs (Hill et al. 2014). Low levels of adhesion molecules (ICAM-1 and VCAM-1) are constitutively expressed by pericytes but, when these cells are activated by inflammatory mediators, their expression is increased, and active binding of leucocytes ensues (Hill et al. 2014). Pericyte guidance is required for infiltrating neutrophils to move along their processes and, induced by neutrophil-pericyte contact, permissive gaps open up between adjacent pericytes, thus facilitating neutrophil extravasation (Wang et al. 2012). These inflammatory cells then breach the astrocytic and Müller cell barriers to enter the retina. Pericytes are also implicated in modulating the trafficking of T cells across vascular endothelium in extraretinal tissues (Harrell et al. 2018). Under these conditions, pericytes develop a detached, migratory phenotype. Pericytes have been shown to function as perivascular macrophages, engulfing material requiring disposal by receptor-mediated endocytosis, pinocytosis, and phagocytic pathways, and are known to possess numerous lysosomes to degrade phagocytosed material (Rustenhoven et al. 2017).
Human retinal pericyte-reactive antibodies have been detected in plasma of patients with DR. These antibodies were shown to induce complement-mediated pericyte injury in vitro (Zhang et al. 2016). Breakdown of the BRB in DR allows immunoglobulins and complement factors access to retinal pericytes, potentially inducing a cytotoxic effect leading to pericyte drop-out. Whether these antibodies play a role in the onset of DR, or represent a contributory mechanism of inflammation that develops in the later stages of BRB breakdown, remains to be elucidated.
In addition to hyperglycaemia, dyslipidaemia is a major risk factor for diabetes, and there is a strong association between dyslipidaemia and the development of DR. Lipids and their metabolites, especially those derived from polyunsaturated fatty acids, can act as signalling molecules (termed bioactive lipids) and are involved in regulation of inflammation, angiogenesis, and homeostatic maintenance (Elmasry et al. 2019).
The cyclooxygenase/prostaglandin and lipoxygenase/leukotriene pathways, in particular, are important players in the inflammation associated with the development of DR (Ricciotti and FitzGerald, 2011; Zhang et al. 2011). In DR, diabetes provokes specific alterations in retinal lipid metabolism, and intensive dyslipidaemia therapy can significantly retard the progression of DR. These alterations are characterised by a shift in the fatty acid profile, especially for arachidonic acid (AA) (Ibrahim et al. 2015; Elmasry et al. 2019). Metabolites of AA, termed eicosanoids and including prostaglandins and leukotrienes, are biologically active lipid mediators that regulate (amplify or reduce) inflammation. AA can be metabolised by 3 enzymes: cyclooxygenase (COX), lipoxygenase (LOX) and cytochrome P450 (Tessaro et al. 2015).
Prostaglandins are lipids derived from AA by the action of COX-1 and -2 isoenzymes, with COX-2 expression being more robustly induced by inflammatory stimuli. Their biosynthesis is blocked by NSAID’s. In DR, the retina has a distinctive lipid profile, its high levels of COX-2 (released by activated inflammatory cells and glia) resulting in abnormal production of pro-inflammatory prostaglandins (Semeraro et al. 2015; Tessaro et al. 2015).
Leukotrienes are lipid mediators associated with acute and chronic inflammation. The first substrate in the leukotriene cascade is AA, which is converted by 5-lipoxygenase (5-LOX) (also known as arachidonate 5-lipoxygenase or ALOX5) into the unstable leukotriene A4 (LTA4), and subsequently metabolised to LTB4. The final products of the leukotriene cascade are potent pro-inflammatory mediators (Rinaldo-Matthis and Haeggstrom, 2010; Tersey et al. 2015). Hyperglycaemia increases leukotriene production by retinal glial cells, and LTA4 and LTB4 are markedly higher in DR patients. LTB4 is a leucocyte attractant and linked to ROS generation, cytokine production, and apoptosis, leading to increased retinal capillary permeability, thus contributing to the pro-inflammatory milieu and capillary degeneration in DR (Gubitosi-Klug et al. 2008). 5-LOX-derived 5-hydroxyeicosatetraenoic acid (5-HETE), a major pro-inflammatory eicosanoid, is markedly increased in the vitreous of diabetic versus non-diabetic patients, resulting in increased leucocytic adhesion, capillary hyperpermeability, and neovascularisation. Another lipoxygenase, 15-LOX (also termed arachidonate 15-lipoxygenase or ALOX15) may also contribute to the development of DR, especially by increasing retinal vascular permeability (Elmasry et al. 2019).
The interplay between the sustained hyperglycaemia of diabetes mellitus, pericyte loss and its secretome, chronic low-grade inflammation, and clinicopathological changes in DR are shown in Fig. 7.
Pharmacological intervention strategies
Tight glycaemic control has proven benefits in delaying the onset, and reducing the progression of, vascular complications including DR. This has been demonstrated in the Diabetes Control and Complications Trial (The DCCT Research Group 1993), and the U.K. Prospective Diabetes Study (UKPDS Group 1998) in type 1 and type 2 diabetes respectively. Both studies demonstrated that achieving a glycated haemoglobin (HbA1c) assay target of ≤ 7% reduced the development and progression of DR, with benefits persisting for up to 20 years. Despite this knowledge, maintaining tight glycaemic control in many diabetic patients may be very challenging. Furthermore, progression of DR continues despite attainment of euglycaemia in previously poorly controlled diabetic patients. This ‘metabolic memory’ may be due to epigenetic modifications and persistent oxidative stress, and necessitates effective management of DR beyond rectification of hyperglycaemia (Kowluru 2017).
Over the past few decades, laser photocoagulation has proven to be a relatively safe and effective means of treating PDR and diabetic macular oedema. The Diabetic Retinopathy Study (DRS) (The DRS Research Group 1981) and Early Treatment Diabetic Retinopathy Study (ETDRS) (ETDRS Research Group 1995) demonstrated the efficacy of panretinal laser photocoagulation (PRP), with timely treatment reducing the risk of severe visual loss by 50–60% in patients with disease more advanced than moderate NPDR, while focal/grid laser in diabetic macular oedema threatening the centre of the macular reduced the risk of moderate visual loss by > 50%. However, PRP is inherently destructive, producing side-effects including deficits in peripheral vision, dark adaptation and night vision, in addition to possible complications from misdirected burns or excessively intense burns (Deschler et al. 2014). Macular laser can be complicated by burn spread, misdirected (foveal) burns, paracentral scotomas and development of choroidal neovascularisation (Deschler et al. 2014).
Vitrectomy is used in cases of non-clearing vitreous haemorrhage from PDR, or to relieve vitreomacular traction if present with macular oedema (Duh et al. 2017). However, this later strategy has been found to have inconsistent results with regard to visual acuity despite transient improvements in retinal thickness, and has been associated with complications including cataract (68%), retinal break (7.1%), increased intraocular pressure (5.2%), epiretinal membrane (3.3%) and vitreous haemorrhage (2.4%) (Kim et al. 2019). Hence the role of vitrectomy in the management of diabetic macular oedema requires further investigation.
While laser photocoagulation still plays a significant role in the treatment of DR and diabetic macular oedema, anti-VEGF pharmacotherapy is now a frontline treatment (Kim et al. 2019; Krick and Bressler 2018). Intravitreal injections of anti-VEGF antibody fragments have beneficial effects in reducing retinal oedema and neovascularisation (Kusuhara et al. 2018). Numerous anti-VEGF drugs including bevacizumab, ranibizumab, pegaptanib and aflibercept, are now used in the management of DR and macular oedema (Duh, Sun and Stitt 2017; Kusuhara et al. 2018). However, these drugs are only administered at more advanced stages of the disease, can cause adverse side-effects and have a relatively short half-life, often requiring monthly injections (Wang and Lo 2018). Repeated intravitreal injection is associated with a risk of infectious endophthalmitis, with an incidence per patient of 0.019–1.6%, and ocular haemorrhage is always a small but serious risk associated with intravitreal injection (Falavarjani and Nguyen 2013). There may also be a low risk (0–0.67%) of rhegmatogenous retinal detachment after intravitreal anti-VEGF injection, possibly due to the mechanical forces associated with the injection (Falavarjani and Nguyen 2013). Furthermore, tractional retinal detachment develops or progresses following anti-VEGF therapy in about 5.2% of cases (Falavarjani and Nguyen 2013). While a transient rise in intraocular pressure is inevitable with intravitreal injection, anti-VEGF therapy may result in sustained pressure elevations via a number of proposed mechanisms (Falavarjani and Nguyen 2013). There is also concern over the effect of repeated anti-VEGF treatment on choroidal vessels which require VEGFA stimulation from the RPE for survival (Kusuhara et al. 2018). Moreover, anti-VEGF treatment fails in a significant proportion of cases for numerous reasons including pharmacokinetic and patient factors, but may also be partly explained by the fact that about one-third of patients with PDR have undetectable levels of VEGF in their vitreous fluid, suggesting VEGF-independent pathways are driving the pathogenesis in this subset of patients (Vujosevic and Simo 2017).
For anti-inflammatory therapy, intravitreal corticosteroids effectively suppress a wide range of mediators causing diabetic macular oedema, including VEGF, TNF-α, IL-1β, and chemokines (Wang and Lo 2018). They also inhibit molecules that promote leucostasis and downregulation of EC tight junctions, which otherwise would lead to BRB disruption and increased vascular permeability. Intravitreal corticosteroids, such as triamcinolone, fluocinolone, and dexamethasone, rapidly decrease macular oedema with associated improvement in visual acuity (Kim et al. 2019). However, due to their short-term and transitory efficacy, and high incidence of adverse effects such as cataract formation and glaucoma, corticosteroids are generally used as a second-line option for patients who prove to be refractory to anti-VEGF therapy (Kusuhara et al. 2018; Wang and Lo 2018).
Looking forward, while new anti-VEGF drugs are being developed, with increased duration of action being a particularly desirable characteristic, other options which may offer complementary effects are being investigated. Reducing EC sensitivity to pro-angiogenic and pro-inflammatory stimuli including VEGF and TNF-α by modulating the Ang2/Tie2 pathway is a promising therapeutic strategy with numerous agents already developed and some encouraging results arising from phase 2 clinical trials (Rubsam et al. 2018). AKB-9778, a small-molecule antagonist of vascular endothelial-protein tyrosine phosphatase (VE-PTP) which blocks inactivation of Tie2, has been shown to significantly reduce central subfield thickness in patients with diabetic macular oedema when combined with ranibizumab therapy compared with ranibizumab monotherapy (Campochiaro and Peters 2016). Another phase 2 trial demonstrated the safety and efficacy of faricimab, a dual inhibitor of Ang2 and VEGF-A, achieving superior visual acuity gains (and improved secondary outcome measures) versus ranibizumab in treatment-naïve patients with diabetic macular oedema (Sahni et al. 2019). The RUBY study (ClinicalTrials.gov ID NCT02712008), however, failed to show superiority of REGN910-3, a combination of antibodies blocking VEGF and Ang2, over aflibercept monotherapy. Given aflibercept is now considered the gold standard for treatment of diabetic macular oedema, a trial comparing faricimab versus aflibercept would be useful. Furthermore, trials investigating the effects of increasing, or potentiating the effects of, Tie2 agonists, with the goal of counterbalancing the increase in Ang2 and decrease in pericyte-derived Ang1, appears indicated (Whitehead et al. 2019).
Semaphorin 3A and 3E may offer therapeutic potential in mitigating endothelial dysfunction in DR. Neuron-derived semaphorin 3E causes retraction of endothelial filopodia, and low levels of this protein have been identified in the aqueous fluid of human eyes with PDR (Kwon et al. 2015). Augmenting chemorepulsive signals such as this may prevent aberrant angiogenesis. This hypothesis is yet to be tested. Conversely, Semaphorin 3A, which is induced in early diabetes, has been shown to cause iBRB breakdown in a diabetic mouse model (Cerani et al. 2013). The potential therapeutic effects of blocking Semaphorin 3A in DR have yet to be investigated in human trials. Semaphorin 3A is of particular interest given is potential to protect the BRB in the early stages of diabetes.
Looking beyond corticosteroids, alternative anti-inflammatory strategies are being investigated in the context of DR. Inhibition of COX-2 reduces ICAM-1 expression and leucostasis, the injurious effects of TNF-α and VEGF, vascular leakage, and capillary endothelial apoptosis (Nasrallah et al. 2016; Zhang et al. 2011). The selective COX-2 inhibitor, rofecoxib, also causes an anti-angiogenic response in the DR retina (Wilkinson-Berka et al. 2003). Unfortunately, their off-target adverse effects such as heart attack and stroke, have precluded their systemic use in human clinical trials (Zhang et al. 2011). Mice deficient in 5-LOX have decreased retinal capillary degeneration and reduced neovascularisation in DR models, therefore, suggesting 5-LOX inhibition as a potential pathway for therapeutic intervention (Talaballi et al. 2010). Antibodies against the pro-inflammatory cytokine IL-6 (EBI-031) and its receptor (tocilizumab), have been developed, with phase 1 clinical trials planned. Antibody neutralisation of ICAM-1, or its leucocyte receptor CD18, has been shown to inhibit retinal leukocyte-endothelial cell adhesion and acellular capillary formation in an animal model (Joussen et al. 2001).
Neutralising antibodies to TNF-α (infliximab) and IL-1β (canakinumab) have also been investigated. Infliximab was evaluated in a small phase 3 study including patients with laser photocoagulation-resistant diabetic macular oedema (Sfikakis et al. 2010). Infliximab treatment was well tolerated, and visual acuity was 24.3% greater in infliximab-treated eyes compared to placebo-treated eyes. Larger trials of longer duration are indicated. The effect of canakinumab on retinal neovascularisations in PDR was invested in a phase 1 study (Stahel et al. 2016). Systemic treatment showed stabilisation but no regression of neovascularisation, but did result in reduced retinal oedema, falling short of statistical significance with only six participants enrolled in the study. Treatment was also associated with a significant decrease in HbA1c which is likely to have multiple benefits if maintained long-term in diabetic patients. Further study of canakinumab is warranted.
Tetracycline antibiotics, via their immunomodulatory and neuroprotective effects through inhibition of nitric oxide, cyclooxygenases, prostaglandins, IL-1β, TNF-α and caspases, have been investigated in small phase I/II trials with mixed results. In a phase 2 study, Scott et al. (2014a, b) investigated whether oral doxycycline could improve or slow the development of retinal dysfunction, or induce regression or slow progression of DR in patients with mild to moderate NPDR over a 24 month period. No significant treatment effect was determined. This was in contrast to a proof-of-concept trial of oral doxycycline in patients with severe NPDR or non-high risk PDR, which demonstrated significantly improved foveal sensitivity in the treatment group relative to placebo (Scott et al. 2014b). The authors suggested the discrepancy in findings might relate to doxycycline having differing effects at different stages of DR, with more efficacy in the later stages which are associated with more inflammation. Small sample size may also account for the negative outcome. Oral minocycline has also been evaluated in a phase 1/2 trial for efficacy in diabetic macular oedema (Cukras et al. 2012). This small trial demonstrated a positive treatment effect in terms of visual function, central macular oedema, and vascular leakage within the six month follow-up period. Larger studies are indicated to evaluate the efficacy of tetracyclines in the treatment of DR.
MCP-1 knockout diabetic mice demonstrate significantly reduced levels of retinal vascular leakage and BRB dysfunction compared to mice expressing MCP-1, suggesting MCP-1 blockade as an important therapeutic target in diabetic macular oedema (Rangasamy et al. 2014). MCP-1 receptor antagonism has been evaluated for efficacy in management of diabetic nephropathy with positive results (Yap, Frankel and Tam 2017); however, no studies have evaluated selective MCP-1 blockade in the context of DR. Research into this potential therapeutic target in DR is warranted. Since activated pericytes express numerous pro-inflammatory mediators shared with leukocytes and ECs, some of the aforementioned therapeutic effects of anti-inflammatory therapy are likely also occurring at the pericyte level of the rNVU.
Retinal pericyte depletion in DR is associated with BRB disruption, increased vascular permeability, perivascular leucocyte infiltration, and inflammation (Kusuhara et al. 2018). Therefore, preservation of retinal pericytes could help to restore BRB homeostasis and ameliorate these effects (Kusuhara et al. 2018). A number of drugs have been investigated for this purpose. The drug fenofibrate, a peroxisome proliferator-activated receptor α agonist (PPARα), for example, has been shown to decrease pericyte depletion and ameliorate retinal acellular capillary formation in DR (Ding et al. 2014). Furthermore, fenofibrate treatment in the Fenofibrate Intervention and Event Lowering in Diabetes (FIELD) clinical trial was associated with less retinopathy needing laser treatment, albeit in post-hoc and secondary analysis (Keech et al. 2007). Somatostatin has been demonstrated to favourably modulate apoptotic/survival pathways in human retinal pericytes during microglia-mediated inflammation (Mazzeo et al 2017). Furthermore, β-agonists, via protein kinase B activation in pericytes, appear to have a pro-survival effect on pericytes and reduce EC permeability in the diabetic murine retina (Yun et al. 2018). The development of neutralising antibodies to pericyte-reactive autoantibodies may also represent a promising therapeutic strategy.
The possibility that, like brain pericytes, retinal pericytes have pluripotential, MSC-like characteristics, suggests that they could be used to promote repair of retinal tissue (Trost et al. 2016). Transplantation of human adipose tissue-derived pericytes, for example, may protect against DR by adopting a pericyte morphology and providing vascular support (Mendel et al. 2013). Controlling pro-apoptotic pericyte factors, in concert with transplantation, could provide a robust management strategy for mitigating the microvasculopathy of DR.
Other therapeutic agents have been developed for the management of DR. MTP-131, a peptide targeting the mitochondrial phospholipid, cardiolipin, has been shown to attenuate mitochondrial oxidative stress and seemingly reduce apoptosis of retinal neurons in vitro, and has been shown to reverse visual decline in a diabetic mouse model (Alam et al. 2015; Chen et al. 2017). Alpha-lipoic acid (ALA), a mitochondrial antioxidant, has been shown to reduce retinal endothelial cell loss and preserve pericyte coverage of retinal capillaries in rat diabetic models, but was ineffective in preventing the occurrence of clinically significant macular oedema in a phase 3 trial (Kowluru and Odenbach 2004; Lin et al. 2006; Haritoglou et al. 2011). ARA290, an erythropoietin-derived peptide, was demonstrated to limit neuroglial and vascular degeneration in a diabetic rat model without exacerbating neovascularisation (McVicar et al. 2011). Lipoprotein-associated phospholipase A2 (Lp-PLA2) inhibitor, darapladib, taken orally, has been demonstrated to afford modest gains in vision and improvements in macular oedema in a phase 2a trial, possibly through suppression of BRB breakdown (Staurenghi et al. 2015).
In conclusion, DR is both a microvascular disease, in which marked pericyte depletion is an early and distinctive pathological feature, and a chronic, low-grade inflammatory disorder. The diabetic hyperglycaemic environment provokes an increased local and systemic expression of inflammatory mediators (cytokines, chemokines, and growth factors), all of which help to create a pro-inflammatory milieu that fosters the development and progression of DR. The pathogenesis of DR is complex and multifactorial, providing strong rationale for the use of multiple therapeutic strategies. Current strategies are largely limited to the late stages of DR when significant and likely irreversible damage has occurred. Accordingly, pharmacological strategies that address the early pathological events by controlling inflammation and preventing or reducing microvascular degeneration are highly desirable.
References
Adamis AP (2002) Is diabetic retinopathy an inflammatory disease. Br J Ophthalmol 86:363–365
Alam NM, Mills WC, Wong AA, Douglas RM, Szeto HH, Prusky GT (2015) A mitochondrial therapeutic reverses visual decline in mouse models of diabetes. Dis Model Mech 8(7):701–710
Alikhani M, Roy S, Graves DT (2010) FOXO1 plays an essential role in apoptosis in retinal pericytes. Mol Vis 16:408–415
Armulik A, Abramsson A, Betsholtz C (2005) Endothelial/pericyte interactions. Circ Res 6:512–523
Armulik A, Genove G, Betsholtz C (2011) Pericytes: developmental, physiological, and pathological perspectives, problems, and promises. Dev Cell 21:193–215
Attwell D, Mishra A, Hall CN, O’Farrell FM, Dalkara T (2016) What is a pericyte? J Cereb Blood Flow Metab 36:451–455
Barber A, Gardner TW, Abcouwer SF (2011) The significance of vascular and neural apoptosis to the pathology of diabetic retinopathy. Invest Ophthalmol Vis Sci 52:1156–1163
Beltramo E, Porta M (2013) Pericyte loss in diabetic retinopathy: mechanisms and consequences. Curr Med Chem 20(26):3218–3225
Campochiaro PA, Peters KG (2016) Targeting Tie2 for treatment of diabetic retinopathy and diabetic macular edema. Curr Diab Rep 16(12):1–11
Cerani A, Tetreault N, Menard C, Lapalme E, Patel C, Sitaras N, Beaudoin F, Leboeuf D, De Guire V, Binet F, Dejda A, Rezende FLA, Miloudi K, Sapieha P (2013) Neuron-derived semaphorin 3A is an early inducer of vascular permeability in diabetic retinopathy via neuropilin-1. Cell Metab 4:505–518
Chen M, Liu B, Ma J, Ge J, Wang K (2017) Protective effect of mitochondria-targeted peptide MTP-131 against oxidative stress-induced apoptosis in RGC-5 cells. Mol Med Rep 15(4):2179–2185
Cheung N, Mitchell P, Wong TY (2010) Diabetic retinopathy. Lancet 376:124–136
Cukras CA, Petrou Ph, Chew EY, Meyerle CB, Wong WT (2012) Oral minocycline for the treatment of diabetic macular edema (DME): results of a phase I/II clinical study. Invest Ophthalmol Vis Sci 53(7):3865–38774
Cunha-Vaz J, Bernades R, Lobo C (2011) Blood-retinal barrier. Eur J Ophthalmol 21(Suppl 6):S3–S9
Deschler EK, Sun JK, Silva PS (2014) Side-effects and complications of laser treatment in diabetic retinal disease. Semin Ophthalmol 5–6:290–300
Early Treatment Diabetic Retinopathy Study Research Group (1995) Focal photocoagulation treatment of diabetic macular edema. Relationship of treatment effect to fluorescein angiographic and other retinal characteristics at baseline ETDRS report no 19. Arch Ophthalmol 113:1144–1155
Ding L, Cheng R, Hu Y, Takahashi Y, Jenkins A, Keech A, Humphries K, Gu X, Elliott M, Xia X, Ma J (2014) Peroxisome proliferator-activated receptor alpha protects capillary pericytes in the retina. Am J Pathol 184:2709–2720
Duh EJ, Sun JK, Stitt AW (2017) Diabetic retinopathy: current understanding, mechanisms, and treatment strategies. JCI Insight 2:e93751
Eagle RC (2011) Eye pathology. An atlas and text, 2nd edn. Lippincott Williams & Wilkins, Philadelphia, pp 139–140
Elmasry K, Ibrahim AS, Abdulmoneim S, Al-Shabrawey M (2019) Bioactive lipids and pathological retinal angiogenesis. Br J Pharmacol 176:93–109
Eshaq RS, Aldalati AM, Alexander JS, Harris NR (2017) Diabetic retinopathy: breaking the barrier. Pathophysiology 24(4):229–241
Falavarjani KG, Nguyen QD (2013) Adverse events and complications associated with intravitreal injection of anti-VEGF agents: a review of literature. Eye 7:787–794
Ferland-McCollough D, Slater S, Richard J, Reni C, Mangialardi G (2017) Pericytes, an overlooked player in vascular pathobiology. Pharm Ther 171:30–42
Frank RN (2004) Diabetic retinopathy. N Eng J Med 350:48–58
Gaceb A, Paul G (2018) Pericyte secretome. Adv Exp Med Biol 1109:139–163
Garner A (1993) Histopathology of diabetic retinopathy in man. Eye 7:250–253
Geranmayeh MH, Rahbarghazi R, Farhoudi M (2019) Targeting pericytes for neurovascular regeneration. Cell Commun Signal 17:26
Gubitosi-Klug RA, Talahalli R, Du Y, Nadler JL, Kern TS (2008) 5-lipoxygenase, but not 12/15-lipoxygenase, contributes to degeneration of retinal capillaries in a mouse model of diabetic retinopathy. Diabetes 57:1387–1393
Hammes HP, Lin J, Renner O, Shani M, Lundqvist A, Betsholtz C, Brownlee M, Deutsch U (2002) Pericytes and the pathogenesis of diabetic retinopathy. Diabetes 51:3107–3112
Haritoglou C, Gerss J, Hammes HP, Kampik A, Ulbig MW (2011) Alpha-lipoic acid for the prevention of diabetic macular oedema. Ophthalmologica 226:127–137
Harrell CR, Markovic BS, Fellabaum C, Arsenijevic A, Djonev V, Volarevic V (2018) Molecular mechanisms underlying therapeutic potential of pericytes. J Biomed Sci 25:21
Hill J, Rom S, Ramirez SH, Persidsky Y (2014) Emerging roles of pericytes in the regulation of the neurovascular unit in health and disease. J Neuroimmun Pharmacol 9:591–605
Ibrahim AS, Elshafey S, Sellak H, Hussein KA, El-Sherbiny M, Abdelsaid M, Rizk N, Beasley S, Tawfik AM, Smith SB, Al-Shabrawey M (2015) A lipidomic screen of hyperglycaemia-treated HRECs links 12/15-lipoxyhenase to microvascular dysfunction during diabetic retinopathy via NADPH oxidase. J Lipid Res 56:599–611
Jansson D, Rustenhoven J, Feng S, Hurley D, Oldfield RL, Bergin PS, Mee EW, Faull RLM, Dragunow M (2014) A role for human brain pericytes in neuroinflammation. J Neuroinflamm 11:104
Joussen AM, Murata T, Tsujikawa A, Kirchhof B, Brusell S, Adamis A (2001) Leucocyte-mediated endothelial cell injury and death in the diabetic retina. Am J Pathol 158:147–152
Joussen AM, Povlaki V, Mitsiades N (2003) Suppression of Fas-FasL-induced endothelial cell apoptosis prevents diabetic blood-retinal barrier breakdown in a model of streptozotocin-induced diabetes. FASEB J 17:76–78
Joussen AM, Povlaki V, Le MY, Koizumi K, Esser C, Janicki H, Schraermeyer U, Kociok N, Fauser S, Kirchhof B, Kern TS, Adamis AP (2004) A central role for inflammation in the pathogenesis of diabetic retinopathy. FASEB J 18:1450–1452
Kastelan S, Tomic M, Antunica AG et al (2013) Inflammation and pharmacological treatment in diabetic retinopathy. Mediators Inflamm 2013:213130
Kaur C, Foulds WS, Ling EA (2008) Blood-retinal barrier in hypoxic ischaemic conditions: basic concepts, clinical features and management. Prog Retin Eye Res 27:622–647
Keech AC, Mitchell P, Summanen PA, O’Day J, Davis TME, Moffitt MS, Taskinen M-R, Simes RJ, Tse D, Williamson E, Merrifield A, Laatikainen LT, Emden MC, Crimet DC, O’Connell RL, Coleman PG (2007) Effect of fenofibrate on the need for laser treatment for diabetic retinopathy (FIELD) study: a randomised controlled trial. Lancet 370:17–23
Kim EJ, Lin WV, Rodriguez SM, Chen A, Loya A, Weng CY (2019) Treatment of diabetic macular oedema. Curr Diabetes Rep 19(9):68
Kowluru RA (2017) Diabetic retinopathy, metabolic memory and epigenetic modifications. Vision Res 139:30–38
Kowluru RA, Odenbach S (2004) Effect of long-term administration of α-lipoic acid on retinal capillary cell death and the development of retinopathy in diabetic rats. Diabetes 53(12):3233–3238
Kowluru RA, Zhong G, Kanwar M (2010) Metabolic memory and diabetic retinopathy: role of inflammatory mediators in retinal pericytes. Exp Eye Res 90:617–623
Krick TW, Bressler NM (2018) Recent clinically relevant highlights from the Diabetic Retinopathy Clinical Research Network. Curr Opin Ophthalmol 29(3):199–205
Kwon SH, Shin JP, Kim IT, Park DH (2015) Aqueous levels of angiopoietin-like 4 and semaphorin 3E correlate with nonperfusion area and macular volume in diabetic retinopathy. Ophthalmology 122(5):968–975
Kusuhara S, Fukushima Y, Ogura S, Inoue N, Uemura A (2018) Pathophysiology of diabetic retinopathy: the old and the new. Diabetes Metab J 42:364–376
Lange S, Trost A, Tempfer H, Bauer HC, Bauer H, Rohde E, Reitsamer HA, Franklin RJ, Aigner L, Rivera FJ (2013) Brain pericyte plasticity as a potential drug target in CNS repair. Drug Discov Today 18:456–463
Lim JI (2019) Diabetic retinopathy. In: Yanoff M, Duker JS (eds) Ophthalmology, 5th edn. Elsevier, Edinburgh, pp 543–552
Lin J, Bierhaus A, Bugert P, Dietrich N, Feng Y, Vom Hagen F, Nawroth P, Brownlee M, Hammes HP (2006) Effect of R-(+)-alpha-lipoic acid on experimental diabetic retinopathy. Diabetologia 49(5):1089–1096
Madiera MH, Boia R, Santos PF, Ambrosio AF, Santiago AR (2015) Contribution of microglia-mediated neuroinflammation to retinal degenerative disease. Mediators Inflamm 2015:67390
Mazzeo A, Arroba AI, Beltramo E, Valverde AM, Porta M (2017) Somatostatin protects human retinal pericytes from inflammation mediated by microglia. Exp Eye Res 164:46–54
McVicar CM, Hamilton R, Colhoun LM, Gardiner TA, Brines M, Cerami A, Stitt AW (2011) Intervention with an erythropoietin-derived peptide protects against neuroglial and vascular degeneration during diabetic retinopathy. Diabetes 60(11):2995–3005
Mendel TA, Clabough EBD, Kao DS, Demidova-Rice TN, Durham JT, Zotter BC, Seaman SA, Rakoczy EP, Katz AJ, Herman IM, Peirce SM, Yates PA (2013) Pericytes derived from adipose-derived stem cells protect against retinal vasculopathy. PLoS ONE 8:e65691
Nasrallah R, Hassouneh R, Hebert RL (2016) PGE2, kidney disease, and cardiovascular risk: beyond hypertension and diabetes. J Am Soc Nephrol 27:666–676
Ogura S, Ogura Y, Uemura A (2017) Sustained inflammation after pericyte depletion induces irreversible blood-retinal barrier breakdown. JCI Insight 2:e90905
Park DY, Lee J, Kim J, Kim K, Hong S, Han S, Kubota Y, Augustin HG, Ding L, Kim JW, Kim H, He Y, Adams RH, Koh GY (2017) Plastic role of pericytes in the blood-retinal barrier. Nat Commun 8:15296
Rangasamy S, McGuire P, Nitta C, Monickaraj F, Oruganti S, Das A (2014) Chemokine mediated monocyte trafficking into the retina: role of inflammation in alteration of the blood-retinal barrier in diabetic retinopathy. PLoS ONE 9:e108508
Ricciotti E, FitzGerald GA (2011) Prostaglandins and inflammation. Arterioscler Thromb Vas Biol 31:986–1000
Rinaldo-Matthis A, Haeggstrom JZ (2010) Structures and mechanisms of enzymes in the leukotriene cascade. Biochimie 92:676–681
Rubsam A, Parikh S, Fort PE (2018) Role of inflammation in diabetic retinopathy. Int J Med Sci 19:942
Rudziak P, Ellis C, Kowalewska P (2019) Role and molecular mechanisms of pericytes in regulation of leukocyte diapedesis in inflamed tissues. Mediators Inflamm 2019:4123605
Rustenhoven J, Jansson D, Smyth LC, Dragunow M (2017) Brain pericytes as mediators of neuroinflammation. Trends Pharmacol Sci 38:291–304
Sahni J, Patel SS, Dugel PU, Khanani AM, Jhaveri CD, Wykoff CC, Hershberger VS, Pauly-Evers M, Sadikhov S, Szczesny P, Schwab D, Nogoceke E, Osbourne A, Weikert R, Fauser S (2019) Simulataneous inhibition of angiopoietin-2 and vascular endothelial growth factor-A with Faricimab in diabetic macular edema: BOULEVARD phase 2 randomized trial. Ophthalmology 126(8):1155–1170
Santos GSP, Prazeres PHDM, Mintz A, Birbrair A (2018) Role of pericytes in the retina. Eye 32:483–486
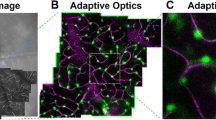
Schallek J, Geng Y, Nguyen HV, Williams DR (2013) Morphology and topography of retinal pericytes in the living mouse retina using in vivo adaptive optics imaging and ex vivo characterisation. Invest Ophthalmol Vis Sci 54:8237–8250
Scott IU, Jackson GR, Quillen DA, Klein R, Liao J, Gardner TW (2014a) Effect of doxycycline vs placebo on retinal function and diabetic retinopathy progression in mild to moderate non-proliferative diabetic retinopathy A randomised proof-of-concept clinical trial. JAMA Ophthalmol 132(9):1137–1142
Scott IU, Jackson GR, Quillen DA, Larsen ML, Klein R, Liao J, Holfort S, Munch IC, Gardner TW (2014b) Effect of doxycycline vs placebo on retinal function and diabetic retinopathy progression in patients with severe nonproliferative or non-high-risk proliferative diabetic retinopathy. A randomised clinical trial. JAMA Ophthalmol 132(5):535–543
Semeraro F, Cancarini A, dell’Omo R, Rezzola S, Romano MR, Costagliola C (2015) Diabetic retinopathy: vascular and inflammatory disease. J Diabetes Res 2015:582060
Sfikakis PP, Grigoropoulos V, Emfietzoglou I, Theodossiadis G, Tentolouris N, Delicha E, Katsiari C, Alexiadou K, Hatziagelaki E, Theodossiadis PG (2010) Infliximab for diabetic macular edema refractory to laser photocoagulation. Diabetes Care 7:1523–1528
Shabab T, Khanabdali R, Moghadamtousi SZ, Kadir HA, Mohan G (2017) Neuroinflammation pathways: a general review. J Neurosci 127:624–633
Smith S, Chand S, Savage C (2012) Biology of the renal pericyte. Nephrol Dial Transpl 27(6):2149–2155
Stahel M, Becker M, Graf N, Michels S (2016) Systemic interleukin 1β inhibition in proliferative diabetic retinopathy: a prospective open-label study using canakinumab. Retina 2:385–391
Staurenghi G, Ye L, Magee MH, Danis RP, Wurzelmann J, Adamson P, McLaughlin MM (2015) Darapladib, a lipoprotein-associated phospholipase A2 inhibitor, in diabetic macular edema: a 3-month placebo-controlled study. Ophthalmology 122(5):990–996
Stitt AW, Gardiner TA, Archer DB (1995) Histological and ultrastructural investigation of retinal microaneurysm development in diabetic patients. Br J Ophthalmol 79(4):362–367
Sweeney MD, Ayyadurai S, Zlokovic BV (2016) Pericytes of the neurovascular unit: key functions and signalling pathways. Nat Neurosci 19:771–783
Talaballi R, Zarini S, Sheibani N, Murphy RC, Gubitosi-Klug RA (2010) Increased synthesis of leukotrienes in the mouse model of diabetic retinopathy. Invest Ophthalmol Vis Sci 3:1699–1708
Tang J, Kern TS (2011) Inflammation in diabetic retinopathy. Prog Retin Eye Res 30:343–358
Tersey SA, Bolanis E, Holman TR, Maloney DJ, Nadler JL, Mirmira RG (2015) Minireview: 12-lipoxygenase and islet β-cell dysfunction in diabetes. Mol Endocrinol 29:791–800
Tessaro FHG, Ayala TS, Martins JO (2015) Lipid mediators are critical in resolving inflammation: a review of the emerging roles of eicosanoids in diabetes mellitus. BioMed Res Int 2015:568408
The Diabetes Control and Complications Trial Research Group (1993) The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med 329:977–986
The Diabetic Retinopathy Study Research Group (1981) Photocoagulation treatment of proliferative diabetic retinopathy. Clinical application of the Diabetic Retinopathy Study (DRS) findings. DRS Report Number 8. Ophthalmology 88:583–600
Trost A, Lange S, Schroedi F, Bruckner D, Motloch KA, Bogner B, Kaser-Eichberger A, Strohmaier C, Runge C, Algner L, Rimera FJ, Reitsamer HA (2016) Brain and retinal pericytes: origin, function and role. Frontiers Cell Neurosci 10:1–13
UK Prospective Diabetes Study (UKPDS) Group (1998) Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet 352:837–853
Vujosevic S, Simo R (2017) Local and systemic inflammatory biomarkers of diabetic retinopathy: an integrative approach. Invest Ophthalmol Vis Sci 58:68–75
Vujosevic S, Toma C (2018) Diabetic retinopathy: an inflammatory disease. Ann Eye Sci 3:52
Wang W, Lo ACY (2018) Diabetic retinopathy: pathophysiology and treatments. Int J Med Sci 19:1816
Wang S, Cao C, Chen Z, Bankaitis V, Tzima E, Sheibani N, Burridge K (2012) Pericytes regulate vascular basement membrane remodelling and govern neutrophil extravasation during inflammation. PLoS ONE 7:e45499
Whitcup SM, Nussenblatt RB, Lightman SL, Hollander DA (2013) Inflammation in retinal disease. Int J Inflamm 2013:348092
Whitehead M, Osbourne A, Widdowson PS, Yu-Wai-Man P, Martin KR (2019) Angiopoietins in diabetic retinopathy: current understanding and therapeutic potential. J Diabetes Res 2019:5140521
Wilkinson CP, Ferris FL, Klein RE, Lee PP, Agardh CD, Davis M, Dills D, Kampik A, Pararajasegaram R, Verdaguer JT (2003) Global Diabetic Retinopathy Project Group. Proposed international clinical diabetic retinopathy and diabetic macular oedema disease severity scales. Ophthalmology 110:1677–1682
Wilkinson-Berka JL, Alousis NS, Kelly DJ, Gilbert RE (2003) COX-2 inhibition and retinal angiogenesis in a mouse model of retinopathy of prematurity. Invest Ophthalmol Vis Sci 44:974–979
Wu L, Fernandez-Loaiza Sauma J, Hernandez-Bogantes E, Masis M (2013) Classification of diabetic retinopathy and diabetic macular oedema. World J Diabetes 4:290–294
Wu H, Hwang D, Song X, Tao Y (2017) Association between aqueous cytokines and diabetic retinopathy stage. J Ophthalmol 2017:9402198
Yap HL, Frankel AH, Tam FWK (2017) Review article – MCP-1: a potential target for diabetic microvascular complications? Urol Nephrol Open Access J 5(3):00171
Yun J, Jeong H, Kim K, Han MH, Lee EH, Lee K, Cho C (2018) β-adrenergic receptor agonists attenuate pericyte loss in diabetic retinas through Akt activation. FASEB J 32(5):2323–2338
Zhang W, Liu H, Rojas M, Caldwell RW, Caldwell RB (2011) Anti-inflammatory therapy for diabetic retinopathy. Immunotherapy 3:609–628
Zhang L, Li Y, Payne J, Srivastava S, Fan X, Fung J, Li X, Kern TS, Lin F (2016) Presence of retinal pericyte-reactive autoantibodies in diabetic retinopathy patients. Sci Rep 6:20341
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Spencer, B.G., Estevez, J.J., Liu, E. et al. Pericytes, inflammation, and diabetic retinopathy. Inflammopharmacol 28, 697–709 (2020). https://doi.org/10.1007/s10787-019-00647-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10787-019-00647-9