Abstract
In continuation with our previous studies on osthole, bergapten, a closely related furanocoumarin was investigated for its ameliorative effect on chemically induced neurogenic and inflammatory hyperalgesia and inflammation in mice. Chemical hyperalgesia and inflammation was induced by administration of formalin (intraplantar), acetic acid (intraperitoneal) and carrageenan (intraplantar) to different groups of animals. Pain responses were quantified and median effective dose (ED50) of bergapten was calculated. Lipopolysaccharide challenge was administered to study inflammatory cytokines which were analyzed in plasma using ELISA. The expression of poly ADP-ribose polymerase (PARP), cyclooxygenase (COX-2) and inducible nitric oxide synthase (iNOS) was quantified by immnofluorescence staining. Bergapten was found to ameliorate both neurogenic and inflammatory hyperalgesia precipitated by formalin, acetic acid induced writhing and carrageenan induced paw inflammation with ED50 dose of 2.96 mg/kg. Bergapten also significantly decreased the levels of TNF-α and IL-6 and the expression of PARP, COX-2 and iNOS in the spine. It is concluded that bergapten is an interesting molecule with significant analgesic and anti-inflammatory activity emanating through the modulation of multiple pain mediating pathways.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Coumarins are important secondary metabolites abundantly found in numerous plants of medicinal significance that protect the plants from environmental stresses and insults (Venugopala et al. 2013; Asif 2015). Furanocoumarins are known for pharmacological effects including analgesic/antipyretic, anti-inflammatory, antimicrobial, antiproliferative, antioxidative and antiviral actions (Tian et al. 2017). Bergapten (5-methoxypsoralen) present in the plants of rutaceae and umbelliferae family such as Cnidium monnieri is widely used for its medicinal values (Navarra et al. 2015; Liao et al. 2018) such as anticoagulant (Mira et al. 2017), anti-inflammatory (Bose et al. 2011), antiproliferative (Hung et al. 2017) and anticancer activity (Yang et al. 2018). It has also been reported to have anticonvulsant effects (Luszczki et al. 2010). 8-Methoxypsoralen and 5-methoxypsoralen formulations are used in the clinical management of skin ailments like psoriasis, vitiligo and mycosis fungoides (Al-Asmari et al. 2017).
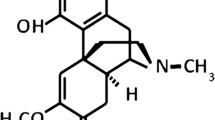
Pain is a physical and mental suffering, and often associated with co-morbidities including depression, anxiety and stress affecting the patient’s daily activities (Stubbs et al. 2016; Pitcher 2018). Clinically available options for pain mitigation comprise of NSAIDS and opioids, while neuropathic pain is treated with anticonvulsants (Slater et al. 2010). However, all these drugs suffer from certain limitations necessitating the need to explore new chemical moieties for the treatment of pain. Since plant medicines are known to have relatively fewer adverse effects than synthetic analogs probably because they are naturally synthesized in plants and hence the living cells have better tolerability towards these molecules, the phytochemicals offer interesting leads in new drug development. After the successful investigations for analgesic activity of osthole (Singh et al. 2018), the current study was undertaken to explore the medicinal potential of another natural product bergapten, for which to the best of our knowledge, comprehensive studies on antihyperalgesic effect and its modulation of PARP, COX-2 iNOS and inflammatory cytokines are not reported. Therefore, the current investigation was focused to explore the analgesic and anti-inflammatory activity of bergapten and its role in modulation of PARP, COX-2, iNOS and inflammatory cytokines.
Materials and methods
Chemicals
Indomethacin, substance-P, l-arginine, L-NAME were purchased from Sigma-Aldrich while all other analytical grade chemicals and reagents were procured from authorized local suppliers. Bergapten was a gift sample from Sugam Herbal Creation, Nanital, Uttrakhand and the structure of the procured sample was established by NMR and LC–MS spectrometry. TNF-α and IL-6 (mouse cytokine) kits were purchased from Krishgen Biotech, Mumbai, India. Mouse monoclonal anti-iNOS antibody was procured from Sigma Aldrich, USA and rabbit polyclonal COX-2, PARP antibodies were obtained from Santa Cruz Biotech, USA. Goat anti-mouse IgG1 secondary antibody, Alexa Fluor 546 and goat anti-rabbit IgG (H+L) secondary antibody, Alexa Fluor 546 were supplied by Invitrogen, USA.
Animals
Swiss albino mice (either sex) with body weight ranging from 30 to 40 g were taken from Central Research Institute, Kasauli. The animals were housed in central animal house of Guru Nanak Dev University and maintained as per the standard guidelines with free access to feed (Aashirwad Industries, Chandigarh) and water. The protocols for the animal studies were approved by the institutional animal ethics committee (226/CPCSEA 2015/11). All procedures were conducted between 09:00 and 17:00 h in accordance with the Committee for the Purpose of Control and Supervision of Experiments on Animals (CPCSEA), Minsitry of Environment, Forests and Climate Change, Govt. of India guidelines.
Acetic acid-induced writhing
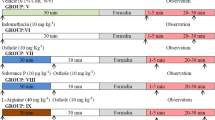
Acetic acid-induced writhing is a well-documented model of visceral pain (Pitcher et al. 2017). Acetic acid (0.6%) was administered intraperitoneally and the number of writhes, i.e., abdominal contractions was quantified for a period of 30 min post-acetic acid injection (Nogueira et al. 2003). The schematic presentation of treatment groups is summarized in Fig. 1a.
ED50 of bergapten
Median effective dose (ED50) of bergapten was calculated in the acetic acid model by varying the dose in a randomized manner with each dose group comprising of five animals and maximum dose of 20 mg Kg−1. Results were calculated in terms of percent anti-nociceptive activity. The response data obtained were fitted using analysis of variance (ANOVA). Best-fitted model having p value < 0.001 (highly significant) and non-significant lack of fit (p > 0.05) indicated strong signal as compared to model noise. The best-fitted regression equation is used for plotting one factor graph and the corresponding dose at which 50% anti-nociceptive activity is seen was determined.
Formalin-induced nociception
Freshly prepared 2% formalin solution was administered to the animals via subcutaneous route under the plantar surface of the right hind paw. The animals were placed individually in the observation chamber and flinching response was monitored for a period of 30 min (Pinho-Ribeiro et al. 2003). The schematic presentation of treatment groups is summarized in Fig. 1b.
Involvement of COX and NO pathways in the observed effect of bergapten
The involvement of cyclooxygenase (COX) pathway was studied by pre-treatment of the animals with substance-P which is a known modulator of COX and the involvement of nitric oxide (NO) pathway was studied using pre-treatment with l-arginine (NO precursor) and l-NAME (NO synthase inhibitor). The findings were further corroborated from immunofluorescence staining using antibodies for PARP, COX-2 and iNOS. The schematic presentation of treatment groups is summarized in Fig. 1c.
Immunohistological expression studies
Mice were anaesthetized with ketamine (40 mg/kg, i.p) after 2 h of formalin injection and pre-perfusion with 4% paraformaldehyde phosphate buffer solution for 4 h was given. Post-perfusion, L4–L5 section of spinal cord was removed and immersed overnight in 30% v/v sucrose solution maintained at 4 °C. Ten random sections of 10-µm sections of the spinal tissue were obtained using cryomicrotome (Leica Biosystems) and incubated separately with each of the primary antibodies including rabbit polyclonal PARP (1:200), mouse monoclonal anti-iNOS (1:100) and rabbit polyclonal COX-2 (1:150) for 48 h, followed by alternate washing with the PBS and PBST buffers. In the next step, the sections were incubated for 2 h with either goat anti-mouse IgG (1:2000) or goat anti-rabbit (1:2000). Repeated washings were given with the PBS as required. The imaging of the slides was done using confocal microscope (Nikon Eclipse Xi).
Carrageenan-induced paw oedema
Anti-inflammatory activity was assessed using carrageenan induced paw oedema model (Hajhashemi et al. 2012). This method involves measuring acute inflammatory response on administration of 100 µL of carrageenan (1%) w/v into the plantar surface of hind paw in each mouse. The extent of inflammation was expressed as paw oedema measured at a varied time interval between 15 and 360 min. The difference in the volume of both hind paws (including paw exhibiting oedema) was measured by plethysmometer (Medicaid Systems, India). The maximum possible effect (MPE) of bergapten in carrageenan-induced paw oedema test was calculated using Eq. 1. The schematic presentation of treatment groups is summarized in Fig. 1d.
where [PV]c is the Paw volume of control group; [PV]T is the Paw volume of test group.
Measurement of TNF-α and IL-6
Animals were divided into five groups. Group-1 is normal control and was administered vehicle, i.e., 0.1% carboxymethyl cellulose (CMC) intraperitoneally. Group-2 was lipopolysaccharide (LPS) treated control group, where LPS was administered i.p. at a dose of 1 mg/kg. The remaining three groups were pre-treated with bergapten at doses 5, 10, 20 mg/kg, respectively. LPS was administered 30 min following the bergapten treatment. Blood samples for TNF-α estimation were collected by cardiac puncture under anesthesia 2 h after LPS administration. The sampling for IL-6 was done 6 h post-LPS administration. Centrifugation of the samples was carried out at 5000 rpm for 10 min at 10 °C. Blood plasma was collected and stored at 20 ºC until further estimations. Estimation of TNF-α and IL-6 was carried out using commercially available ELISA kits and the results were expressed as picogram per milliliter (pg/mL).
Statistical analysis
All the results are expressed as mean ± standard error mean (SEM). One-way and two-way ANOVA followed by Tukey’s test was used to calculate statistical significance.
Results
Effect of bergapten on acetic acid-induced writhing
Treatments with indomethacin (10 mg kg−1) and bergapten (10 mg kg−1) markedly attenuated acetic acid-induced writhing (Fig. 2a).
ED50 of bergapten
% Anti-nociceptive activity was found to be ranging from 23.3% at 1.5 mg/kg to 92.4% at 20 mg/kg. There was an increase in % anti-nociceptive activity up to the dose of 10 mg kg−1. However, further increase in the dose did not affect the response. Regression equation was numerically optimized to yield a 50% increase in antinociceptive activity and ED50 was found to be 2.96 mg kg−1 (Fig. 2b).
Effect of bergapten treatment on formalin-induced hyperalgesia
Formalin-induced pain test was found to produce distinct biphasic response. First peak in nociceptive activity was evident in the first 5 min; whereas second peak was found at 20–30 min after the formalin injection (Fig. 3a). Treatment with indomethacin did not attenuate the first phase but markedly attenuated the second phase; whereas, bergapten treatment was found to attenuate both the phases significantly with 43.8% reduction in the first phase and 60.5% reduction in flinching in the second phase (Fig. 3b).
a Effect of bergapten on formalin-induced flinchings in mice. b Effect of bergapten on formalin-induced flinchings in neurogenic and inflammatory phases in mice. c Modulation of the analgesic effect of bergapten by substance-P pre-treatment. d Modulation of the analgesic effect of bergapten by l-arginine, L-NAME pre-treatment. All values are expressed as mean ± SEM. Statistical differences were determined by two-way ANOVA followed by Tukey’s test. ap < 0.05 vs. control, bp < .005 vs. indomethacin, cp < 0.05 vs. bergapten
Mechanistic studies for COX and NO pathway
Substance-P pre-treatment completely prevented the anti-nociceptive effect of bergapten in both phases (Fig. 3c). l-arginine pre-treatment was found to reverse the antinociceptive effect of bergapten in both phases; whereas l-NAME pre-treatment did not alter the effect of bergapten (Fig. 3d).
Immunohistological findings of PARP, COX-2 and iNOS expression
Immunofluoresent staining with antibodies revealed a marked increase in the expression of PARP, COX-2 and iNOS in L-5 (lumbar) region of the spinal cord in formalin-treated control animals as compared to normal animals. Bergapten treatment showed a marked reduction in the expression of PARP (Fig. 4), COX-2 (Fig. 5) and iNOS (Fig. 6) in L-5 region of the spine as compared to formalin control group.
Immunofluorescence staining of Group-1, Group-2 and Group-3 with PARP antibody showing DAPI-, TRITC-positive cells and average intensity in the transverse section of spinal cord (200× magnification). All values are expressed as mean ± SEM. Statistical differences were determined by one-way ANOVA followed by Tukey’s test ap < 0.05 vs. control group and bp < 0.05 formalin-treated group
Immunofluorescence staining of Group-1, Group-2 and Group-3 with COX-2 antibody showing DAPI-, TRITC-positive cells and average intensity in the transverse section of spinal cord (200× magnification). All values are expressed as mean ± SEM. Statistical differences were determined by one-way ANOVA followed by Tukey’s test ap < 0.05 vs. control group and bp < 0.05 formalin-treated group
Immunofluorescence staining of Group-1, Group 2 and Group 3 with iNOS antibody showing DAPI-, TRITC-positive cells and average intensity in the transverse section of spinal cord (200× magnification). All values are expressed as mean ± SEM. Statistical differences were determined by one-way ANOVA followed by Tukey’s test ap < 0.05 vs. control group and bp < 0.05 formalin-treated group
Effect of bergapten on paw oedema induced by carrageenan
Carrageenan injection was found to increase the paw volume steadily and peak oedema was evident after 45 min of carrageenan injection into the intraplantar region. Treatment with indomethacin (10 mg kg−1) and bergapten (10 mg kg−1) (Li et al. 2016) was found to reduce the paw oedema significantly and maximum anti-inflammatory effect was observed at 240 min of carrageenan injection (Fig. 7a, b).
Effect of bergapten treatment on plasma cytokines
LPS treatment enhanced the production of TNF-α and IL-6. However, bergapten produced a significant reduction in the level of both TNF-α and IL-6 in a dose-dependent manner. The doses of 5, 10, 20 mg kg−1 diminished the level of TNF-α by 33.0, 66.3 and 86.0% (Fig. 8a) and IL-6 by 40.6, 63.3 and 82.6%, respectively (Fig. 8b). For determining IC50 of bergapten, analyses were run by varying dose of bergapten from 5 mg/kg to 20 mg/kg in triplicates, and % inhibition of TNF-α and IL-6 was recorded as response. ANOVA modeling suggested second-order regression equation and explained 94.5% variance in the data (Coeff. of determination = 0.945). Fitted ANOVA model shows a highly significant model fitting at p value < 0.0001 along with the model statistics and regression equations which is given in Table 1. The one factor plot of bergapten vs. percentage inhibition of TNF-α indicated IC50 of bergapten 7.27 mg/kg (Fig. 8c) and IL-6 was found 6.9 mg kg−1 (Fig. 8d).
Effect of bergapten on plasma levels of a TNF-α and b IL-6 in mice. All values are expressed as mean ± SEM. Statistical differences were determined by one-way ANOVA followed by Tukey’s test ap < 0.05 vs. control group, bp < 0.05 vs. LPS treated group, cp < 0.05 vs. 5 mg kg−1 and dp < 0.05 vs. 10 mg kg−1. c Median inhibitory concentration (IC50) of bergapten on TNF-α, d on IL-6
Discussion
The current investigation was undertaken to explore the analgesic, anti-inflammatory effect and mechanism of action of naturally occurring furanocoumarin, bergapten. Further, the effect of bergapten treatment on the expression of PARP, COX-2 and iNOS pathways and inflammatory cytokines (TNF-α and IL-6) was also studied. The anti-hyperalgesic effect was studied by a well-established model of acetic acid-induced writhing that mimics visceral pain (Pitcher 2018; Pinho-Ribeiro et al. 2003) and formalin-induced hyperalgesia. Intraperitoneal injection of acetic acid induces pain response quantified as number of abdominal constrictions or writhes for a period of 30 min. Similar response was observed in our study. Acetic acid treatment is documented to exhibit nociception by inducing the release of inflammatory cytokines such as TNF-α, IL-6, IL-1β and IL-8 (Satyanarayana et al. 2004).
Formalin is known to induce a biphasic pain response comprising of an initial neurogenic phase mediated at the spinal level and a delayed phase of inflammatory pain which occurs due to combined inputs from the afferent and peripheral nociceptive pathways (Yi et al. 2011; Fischer et al. 2014). While opioid analgesics are known to block both the neurogenic and inflammatory phases of formalin hyperalgesia, NSAIDS, on the contrary, do not attenuate the neurogenic hyperalgesia but effectively blocks the inflammatory phase (McNamara et al. 2007). Bergapten was found to inhibit both acetic acid-induced writhing and the phases of formalin-induced hyperalgesia. Furthermore, bergapten exhibited significant decrease in the carrageenan-induced paw oedema. Pretreatment with substance-P and l-arginine reversed the analgesic effect of bergapten; whereas l-NAME pretreatment produced no effect. As reported previously, increased expression of COX-2 and iNOS is involved in hyperalgesia in formalin-treated mice (Singh et al. 2018; Hwang et al. 2013). Substance-P, a neurokinin, is also reported to increase the expression of COX-2 (Gallicchio et al. 2006). The findings of the current study indicate a reversal of analgesic effect of bergapten on pretreatment with substance-P thereby suggesting a role of inhibition of COX-2 in the analgesic effect of bergapten. This contention is further supported by the decreased expression of spinal COX-2 in the spinal sections of formalin-treated mice.
Nitric oxide is a gaseous transmitter that has been postulated to be generated at the sites of inflammation and mediates pain and inflammation (Fan et al. 2012). Increased expression of iNOS is known to play pivotal role in several inflammatory conditions such as neuropathic pain (Freire et al. 2009) and carrageenan-induced inflammatory pain in animals (Cury et al. 2011). l-arginine is a precursor of NO and is documented to accentuate formalin-induced hyperalgesia (Schmidtko et al. 2009). Tissue nitric oxide synthesis is catalyzed by the enzyme nitric oxide synthase (NOS) which has three isoforms. While neuronal NOS (nNOS) and endothelial NOS (eNOS) are constitutively expressed, inducible or iNOS is a non-constitutive enzyme expressed at the time of inflammation (Cury et al. 2011; Forstermann and Sessa 2012). Increased expression of iNOS is linked with several chronic inflammatory conditions such as rheumatoid arthritis, multiple sclerosis, dilated cardiomyopathy, asthma and ulcerative colitis and neuropathic pain (Choudhari et al. 2013; Khan et al. 2016). Inhibitors of NOS including l-NAME, which non-selectively inhibits NOS (Meena et al. 2011) and selective iNOS inhibitor GW274150 and GW273629, have been documented to confer analgesic effect in chemically induced pain in several studies (Koch et al. 2007; Wang et al. 2015; Wang et al. 2005). In the current investigation, pretreatment with l-NAME did not alter the effect of bergapten. Studies have revealed that the expression of iNOS is induced by oxidative insults, inflammatory cytokines and other types of tissue stresses such as hypoxia (Ohtsu et al. 2010). COX-2 and iNOS have been documented to be produced in large amounts under inflammatory conditions (Jean et al. 2008).
Ploy(ADP-ribose) polymerase (PARP), an enzyme responsible for nicking DNA and transferring ADP to nuclear proteins, has been documented to play a role in inflammatory conditions (Ahmad et al. 2014). Studies have revealed PARP inhibitors to have ameliorative effects in animal models of acute and chronic inflammation (Patcher and Szabo 2007; Bai and Virag 2012). PARP has been reported to play a role in ischemia reperfusion injury produced by peroxynitrile (Szabo et al. 2002). Furthermore, PARP has been shown to control the expression of nitric oxide synthase (Le Page et al. 1998). Studies have revealed that treatment with 3-aminobenzamide, a PARP inhibitor, ameliorates the expression of iNOS, COX-2 and inflammatory cytokines in adjuvant-induced arthritis in mice (Ahmad et al. 2014). Bergapten treatment was found to decrease the PARP expression in the spinal sections of formalin treated mice. Bergapten treatment also decreased the level of inflammatory cytokines TNF-α and IL-6 in mice. These findings corroborate the hypothesis that anti-hyperalgesic and anti-inflammatory effects of bergapten might be mediated by the inhibition of iNOS COX-2 expression and the inflammatory cytokines.
In conclusion, the results of present studies provide useful insights into the analgesic, and anti-inflammatory potential of bergapten that is possibly emerging through the modulation of PARP, COX-2, iNOS expression and inflammatory cytokines.
References
Ahmad SF, Attia SM, Zoheir KMA, Ashour AE, Bakheet SA (2014) Attenuation of the progression of adjuvant-induced arthritis by 3-aminobenzamide treatment. Int Immunopharmacol 19:52–59
Al-Asmari AK, Athar MT, Kadasah SG (2017) An updated phytopharmacological review on medicinal plant of Arab region: apium graveolens linn. Pharmacogn Rev 11(21):13–18
Asif M (2015) Pharmacological activities and phytochemistry of various plant containing coumarin derivatives. Curr Sci Perspect 1(3):77–90
Bai P, Virag L (2012) Role of poly(ADP-ribose) polymerases in the regulation of inflammatory processes. FEBS Lett 64:327–337
Bose SK, Dewanjee S, Sahu R, Dey SP (2011) Effect of bergapten from Heracleum nepalense root on production of proinflammatory cytokines. Nat Prod Res 25(15):1444–1449
Choudhari SK, Chaudhary M, Bagde S, Gadbail AR, Joshi V (2013) Nitric oxide and cancer: a review. World J Surg Oncol 11(1):1–11
Cury Y, Picolo G, Gutierrez VP, Ferreira SH (2011) Pain and analgesia: the dual effect of nitric oxide in the nociceptive system. Nitric Oxide 25(3):243–254
Fan W, Huang F, Wu Z, Zhu X, Li D, He H (2012) The role of nitric oxide in orofacial pain. Nitric Oxide 26(1):32–37
Fischer M, Carli G, Raboisson P, Reeh P (2014) The interphase of the formalin test. Pain 155(3):511–521
Forstermann U, Sessa WC (2012) Nitric oxide synthases: regulation and function. Eur Heart J 33(7):829–837
Freire MAM, Guimaraes JS, Gomes-Leal W, Pereira A (2009) Pain modulation by nitric oxide in the spinal cord. Front Neurosci 3(2):175–181
Gallicchio M, Rosa AC, Benetti E, Collino M, Dianzani C, Fantozzi R (2006) Substance-P-induced cyclooxygenase-2 expression in human umbilical vein endothelial cells. Br J Pharmacol 147(6):681–689
Hajhashemi V, Zolfaghari B, Yousefi A (2012) Antinociceptive and anti-inflammatory activities of Satureja hortensis seed essential oil, hydroalcoholic and polyphenolic extracts in animal models. Med Princ Pract 21(2):178–182
Hung WL, Suh JH, Wang Y (2017) Chemistry and health effects of furanocoumarins in grapefruit. J Food Drug Anal 25(1):71–83
Hwang HT, Wecksler A, Wagner KD, Hammock B (2013) Rationally designed multitarget agents against inflammation and pain. Curr Med Chem 20(13):1783–1799
Jean YH, Chen WF, Duh CY, Huang SY, Hsu CH, Lin CS, Sung CS, Chen IM, Wen ZH (2008) Inducible nitric oxide synthase and cyclooxygenase-2 participate in anti-inflammatory and analgesic effects of the natural marine compound lemnalol from Formosan soft coral Lemnalia cervicorni. Eur J Pharmacol 578(2–3):323–331
Khan S, Choi RJ, Lee J, Kim YS (2016) Attenuation of neuropathic pain and neuroinflammatory responses by a pyranocoumarin derivative, anomalin in animal and cellular models. Euro J Pharmcol 774:95–104
Koch A, Zacharowski K, Boehm O, Stevens M, Lipfert P, Von Giesen HJ, Wolf A, Freynhagen R (2007) Nitric oxide and pro-inflammatory cytokines correlate with pain intensity in chronic pain patients. Inflamm Res 56(1):32–37
Le Page C, Sanceau J, Drapier JC, Wietzerbin J (1998) Inhibitors of ADP ribosylation impair in-ducible nitric oxide synthase gene transcription through inhibition of NFκB activation. Bio-chem Biophys Res Commun 243:451–457
Li XJ, Zhu Z, Han SL, Zhang ZL (2016) Bergapten exerts inhibitory effects on diabetes-related osteoporosis via the regulation of the PI3K/AKT, JNK/MAPK and NF-κB signaling pathways in osteoprotegerin knockout mice. Int J Mol Med 38(6):1661–1672
Liao M, Song G, Cheng X, Diao X, Sun Y, Zhang L (2018) Simultaneous determination of six coumarins in rat plasma and metabolites identification of bergapten in vitro and in vivo. J Agri Food Chem 66(18):4602–4613
Luszczki JJ, Andres-Mach M, Glensk M, Skalicka-Wozniak K (2010) Anticonvulsant effects of four linear furanocoumarins, bergapten, imperatorin, oxypeucedanin, and xanthotoxin, in the mouse maximal electroshock-induced seizure model: a comparative study. Pharmacol Rep 62(6):1231–1236
McNamara CR, Mandel-Brehm J, Bautista DM, Siemens J, Deranian KL, Zhao M, Hayward NJ, Chong JA, Julius D, Moran MM, Fanger CM (2007) TRPA1 mediates formalin-induced pain. Proc Natl Acad Sci 104(33):13525–13530
Meena S, Kumar A, Chauhan S (2011) Possible involvement of nitric oxide mechanism in the protective effect of Melatonin against sciatic nerve ligation induced behavioral and biochemical alterations in rats. Int J Drug Dev Res 3:224–233
Mira A, Alkhiary W, Shimizu K (2017) Antiplatelet and anticoagulant activities of angelica shikokiana extract and its isolated compounds. Clin Appl Thromb Hemost 23(1):91–99
Navarra M, Ferlazzo N, Cirmi S, Trapasso E, Bramanti P, Lombardo GE, Gangemi S (2015) Effects of bergamot essential oil and its extractive fractions on SH-SY5Y human neuroblastoma cell growth. J Pharm Pharmacol 67(8):1042–1053
Nogueira CW, Quinhones EB, Jung EA, Zeni G, Rocha JB (2003) Anti-inflammatory and antinociceptive activity of d iphenyl diselenide. Inflamm Res 52(2):56–63
Ohtsu N, Takaoka K, Segawa E, Hashitani S, Noguchi K, Kishimoto H, Urade M (2010) Antitumor effects of inhibitors of nitric oxide synthase or cyclooxygenase-2 on human KB carcinoma cells overexpressing COX-2. Oncol Rep 24(1):31–36
Patcher P, Szabo C (2007) Role of poly(ADP-ribose) polymerase 1 (PARP-1) in cardiovascular diseases: the therapeutic potential of PARP inhibitors. Cardiovasc Drug Rev 25:235–260
Pinho-Ribeiro FA, Hohmann MS, Borghi SM, Zarpelon AC, Guazelli CF, Manchope MF, Casagrande R, Verri WA Jr (2003) Protective effects of the flavonoid hesperidin methyl chalcone in inflammation and pain in mice: role of TRPV1, oxidative stress, cytokines and NF-κB. Chem Biol Interact 228:88–99
Pitcher MH (2018) The impact of exercise in rodent models of chronic pain. Curr Osteoporos Rep 16(4):1–16
Pitcher MH, Gonzalez-Cano R, Vincent K, Lehmann M, Cobos EJ, Coderre TJ, Baeyens JM, Cervero F (2017) Mild social stress in mice produces opioid-mediated analgesia in visceral but not somatic pain states. J Pain 18(6):716–725
Satyanarayana PS, Jain NK, Singh A, Kulkarni SK (2004) Isobolographic analysis of interaction between cyclooxygenase inhibitors and tramadol in acetic acid-induced writhing in mice. Prog Neuropsychopharmacol Biol Psychiatry 28(4):641–649
Schmidtko A, Tegeder I, Geisslinger G (2009) No NO, no pain? The role of nitric oxide and cGMP in spinal pain processing. Trends Neurosci 32(6):339–346
Singh G, Bhatti R, Mannan R, Singh D, Kesavan A, Singh P (2018) Osthole ameliorates neurogenic and inflammatory hyperalgesia by modulation of iNOS, COX-2, and inflammatory cytokines in mice. Inflammopharmacology. https://doi.org/10.1007/s10787-018-0486-9
Slater D, Kunnathil S, McBride J, Koppala R (2010) Pharmacology of non-steroidal anti-inflammatory drugs and opioids. Inflammopharmacology 27(4):400–411
Stubbs B, Koyanagi A, Thompson T, Veronese N, Carvalho AF, Solomi M, Mugisha J, Schofield P, Cosco T, Wilson N, Vancampfort D (2016) The epidemiology of back pain and its relationship with depression, psychosis, anxiety, sleep disturbances, and stress sensitivity: data from 43 low-and middle-income countries. Gen Hosp Psychiatry 43:63–70
Szabo G, Baahrle S, Stumpf N, Sonnenberg K, Szabo E, Pacher P, Csont T, Schulz R, Dengler TJ, Liaudet L, Jagtap PG (2002) Poly(ADP-ribose) polymerase inhibition reduces reperfusion injury after heart transplantation. Circ Res 90(1):100–116
Tian Y, Shi R, Gao M, Wang H, Du Y, Zhang L, Zhang M (2017) Differentiation of furanocoumarin isomers with ratio of relative abundance of characteristic fragment ions and application in Angelicae dahuricae radix. Chromatographia 80(9):1401–1410
Venugopala KN, Rashmi V, Odhav B (2013) Review on natural coumarin lead compounds for their pharmacological activity. Biomed Res Int 2013:1–14
Wang WK, Angell AD, Craig C, Dawson J, Garvey E, Moncada S, Monkhouse J, Rees D, Russell LJ, Russell RJ, Schwartz S (2005) GW274150 and GW273629 are potent and highly selective inhibitors of inducible nitric oxide synthase in vitro and in vivo. Br J Pharmacol 145(3):301–312
Wang C, Chen H, Luo H, Zhu L, Zhao Y, Tian H, Wang R, Shang P, Zhao Y (2015) Microgravity activates p38 MAPK-C/EBPβ pathway to regulate the expression of arginase and inflammatory cytokines in macrophages. Inflamm Res 64(5):303–311
Yang Y, Zheng K, Mei W, Wang Y, Yu C, Yu B, Deng S, Hu J (2018) Anti-inflammatory and proresolution activities of bergapten isolated from the roots of Ficus hirta in an in vivo zebrafish model. Biochem Biophys Res Commun 496(2):763–769
Yi M, Zhang H, Lao L, Xing GG, Wan Y (2011) Anterior cingulate cortex is crucial for contra-but not ipsi-lateral electro-acupuncture in the formalin-induced inflammatory pain model of rats. Mol Pain 7(1):61–68
Acknowledgements
RB is thankful to Department of Science & Technology, Govt. of India for financial support (Grant No. EMR/2016/005878) under Extra Mural Research Project. GS and AK are thankful to the University Grants Commission (UGC) (Grant No. F1-17.1/2017-18/RGNF-2017-18-SC-PUN-35330), New Delhi for scholarship under NFSC and MANF scheme respectively. The authors also gratefully acknowledge the facilities provided by the UGC (Grant No. F1-17.1/2017-18/MANF-2017-18-PUN-84339) under university with potential for excellence (UPE) scheme.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Authors do not have any conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Singh, G., Kaur, A., Kaur, J. et al. Bergapten inhibits chemically induced nociceptive behavior and inflammation in mice by decreasing the expression of spinal PARP, iNOS, COX-2 and inflammatory cytokines. Inflammopharmacol 27, 749–760 (2019). https://doi.org/10.1007/s10787-019-00585-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10787-019-00585-6