Abstract
The aim of our study was to evaluate the anti-inflammatory, anti-nociceptive, and anti-oxidant action of Riparin B in vivo. We performed experiments in which we induced paw edema by carrageenan and other mediators, carrageenan-induced peritonitis and the level of myeloperoxidase (MPO) activity, pro-inflammatory cytokines (TNF-α and IL-1β), malondialdehyde (MDA) acid, and glutathione (GSH) from the peritoneal fluid. We also performed behavior tests such as acetic acid-induced writhing, formalin-induced linking, and the hot plate test. Among the doses tested of the Riparin B (1, 3, and 10 mg/kg), the dose of 10 mg/kg showed the strongest effect, and this dose was able to reduce the paw edema induced by carrageenan, dextran, histamine serotonin, bradykinin, 48/80, and PGE2. Similarly, the Riparin B in the same dose reduced cell migration and significantly decreased the nociception induced by formalin and acetic acid and reversed the parameters of the oxidative stress. Thus, we can infer that Riparin B exhibits anti-inflammatory, anti-nociceptive, and anti-oxidant actions in vivo.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Natural products, including those derived from plants, have, over the years, contributed greatly to the development of modern therapeutic drugs [1]. However, substances with interesting activities often present in very low amounts, and their availability is dependent on factors such as seasonal variability, day and hour of collection, growth stage, climate, soil composition, and the part of the plant from which the active compounds are extracted [2]. Thus, the supply issues can be resolved by synthesis of the compound, with development of synthetic analogues with more manageable properties and reduced complexity [3].
Synthesis and modification of substances from medicinal plants to try to obtain new structures with pharmacological activity has been a challenge frequently in the field of pharmacological science [4]. An appreciable amount of work has been done to improve isolation of natural substances, increase desirable properties, and minimize adverse effects.
Among the prototypes used for synthetic production are the alkaloids extracted from Aniba riparia [5]. Alkaloids derivatives of plants possess potent anti-oxidative and anti-inflammatory properties [6]. It has been described in the literature that several modified or synthetic compounds of substances extracted from Aniba riparia possess several biological effects, which include an anti-nociceptive effect (Riparin I) [7], an anti-inflammatory effect (Riparin II) [8], and an anxiolytic effect (Riparin III) [9]. Some synthetic Riparin-derived compounds (Riparin A, B, C, D, E, and F) also demonstrate an anti-oxidant action in vitro [5]. However, until now, no data have demonstrated the anti-inflammatory, analgesic, and anti-oxidant activities of Riparin B in an animal model.
Free radicals have long been implicated in connective tissue damage, occurring by inflammation [10]. Vast evidence has recently implicated intracellular ROS production in the modulation of inflammation [11]. Furthermore, during inflammation, the mediators released result in sustained activation and sensitization of both primary nociceptors and higher-order neurons involved in the transmission of the nociceptive input [12]. Thus, substances or drugs capable of inhibiting excessive production of free radicals, chelating iron, or scavenging free radicals could be evaluated as potential anti-inflammatory compounds [13].
Considering the anti-oxidant potential of Riparin B, our work aimed to evaluate the activity of this compound in models of general inflammation and pain, as well as to demonstrate its anti-oxidant action in vivo.

METHODS
Drugs and Reagents
The λ-carrageenan, indomethacin, bradykinin, serotonin, dextran sulfate, histamine, captopril, acetic acid, formaldehyde, and dimethyl sulfoxide (DMSO) were purchased from Sigma Chemical (Saint Louis, MO, USA). Heparin and morphine were provided by Merck (São Paulo, Brazil). All drugs were dissolved in sterile saline (0.9 % w/v). Riparin B was dissolved in 2.0 % DMSO. In all protocols, DMSO (2.0 %) was administered as a control group to Riparin B; all other chemicals were of analytical grade and obtained from standard commercial suppliers.
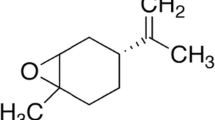
Preparation and Synthesis of Riparin B
The preparation of Riparin B was performed using methodology described previously in literature [5]. Using the Schotten-Baumann reaction, N-[2-(3,4-dimethoxyphenyl)-ethyl]-benzamide (Riparin B) was prepared with 3.5 mmol of benzoyl chloride plus 7.0 mmol of 3,4-dimethoxyphenethylamine. The reaction was stopped after 30 min and resulted in 0.82 g of the compound, Riparin B, with a melting point of 90 °C and a yield of 80.44 % [5].
Animals
Male Swiss mice weighing 25–30 g were used. The animals were housed in temperature-controlled rooms and received food and water ad libitum. All experiments were conducted in accordance with the currently established principles for the care and use of research animals (National Institutes of Health (NIH) guidelines) and were approved by the Ethics Committee on Animal Use in the College Integral Differential EAEC/FACID under protocol number 017/13.
Carrageenan-Induced Paw Edema
The animals were randomly divided into six groups (n = 6), and edema was induced by injection of 50 μL of a suspension of carrageenan (500 μg/paw) in 0.9 % sterile saline into the right hind paw. The mice were pretreated intraperitoneally (i.p.) with either 0.9 % NaCl (group I, untreated control), 2.0 % DMSO (group II untreated control), indomethacin 10 mg/kg (group III, positive control), or 1, 3, or 10 mg/kg of Riparin B (groups IV, V, and VI, respectively) 1 h before carrageenan injection. Paw volume was measured with a plethysmometer (Panlab, Barcelona, Spain) immediately before (Vo) and at 1, 2, 3, and 4 h after carrageenan treatment (Vt) as previously described [14]. The effect of pretreatment was calculated as the percentage of inhibition of edema relative to paw volume of the saline-treated controls as previously described [15] according to the following formula: % inhibition of edema = (Vt − Vo)“Control” − (Vt − Vo)“Treated”)/(Vt − Vo)“Control”) × 100.
Paw Edema Induced by Different Inflammatory Agents
To induce paw edema with different inflammatory agents, in the animals, injections (50 μL each) of dextran (Dxt, 500 g/paw), serotonin (5-HT, 1 %, w/v), histamine (Hist, 1 %, w/v), bradykinin (Bk, 6 nmol), 48/80, (12 μg/paw) or prostaglandin E2 (PGE2) (3 nmol/paw) into the right hind paw were administered. In the experiment with bradykinin, the animals were pretreated with captopril (5 mg/kg, i.p.) 1 h prior to bradykinin induction to prevent bradykinin degradation. One group received 50 μL of 0.9 % sterile saline and served as an untreated control group. Riparin B (10 mg/kg), indomethacin (10 mg/kg, reference control), or DMSO (2 %) were injected i.p. 1 h before intraplantar injection of phlogistic agents. Paw volume was measured immediately before and at selected intervals of time of 30 min per 2 h.
Assessment of Myeloperoxidase Activity in Paw
Following the induction of paw edema by carrageenan, segments of the sub-plantar paw tissue (50 mg) were removed from mice in each group for assessment of myeloperoxidase (MPO). These samples were stored at −80 °C in 1.5-mL Eppendorf tubes for subsequent determination of MPO activity. MPO is an enzyme found predominantly in the azurophilic granules of polymorphonuclear leukocytes and has been used as a quantitative index for evaluating inflammation in various tissues. Samples were suspended in buffer hexadecyltrimethylammonium (pH 6.0, 50 mg of tissue per mL of buffer) and then crushed with a tissue homogenizer. Thereafter, they were centrifuged at 4500 revolutions per minute (rpm) for 12 min at a temperature of 4 °C. The supernatant was then collected. Levels of MPO activity in tissue were determined using 1 % hydrogen peroxide as a substrate for MPO. One unit of MPO is defined as the amount capable of converting 1 μmol of hydrogen peroxide into water in 1 min at 22 °C. The test measures hydrogen peroxide degradation and the production of superoxide anion, which is responsible for the conversion of o-dianisidine to a brown compound. The change in optical density of the samples following the addition of o-dianisidine was measured by spectrophotometer at 450 nm as a function of reaction time. The results were expressed as units of MPO (UMPO)/milligram tissue.
Carrageenan-Induced Peritonitis
Mice were pretreated by oral administration of 250 μL sterile saline or indomethacin 10 mg/kg or Riparin B (10 mg/kg). One hour later, the animals were injected (i.p.) with 250 μL of carrageenan (500 μg/cavity). The mice were euthanized by cervical dislocation under anesthesia 4 h later, and the peritoneal cavity was washed with 1.5 mL heparinized phosphate-buffered saline (PBS) to count peritoneal cells. Total cell counts were performed in a Neubauer chamber, and differential cell (neutrophils) counts (total of 100 cells) were carried out on cytocentrifuge slides stained with hematoxylin and eosin. The results are presented as the number of total leukocyte cells or neutrophils per milliliter of peritoneal exudate.
Cytokine Measurements
After the peritonitis assay, samples of peritoneal fluid were collected, and the levels of interleukin-1 beta (IL-1β) and tumor necrosis factor alpha (TNF-α) were evaluated using sandwich ELISA. Briefly, microliter plates were coated overnight at 4 °C with antibodies against mouse IL-1β or TNF-α (2 μg/mL). Blocking of nonspecific binding sites was accomplished by incubating the plates with PBS containing 2.0 % bovine serum albumin (BSA) for 90 min at 37 °C. After blocking the plates, the test samples and each standard (at various dilutions) were added in duplicate and incubated at 4 °C for 24 h. The plates were washed three times with buffer. After washing the plates, 50 μL of biotinylated sheep polyclonal anti-IL-1β and anti-TNF-α (diluted 1:1000 with 1.0 % BSA assay buffer) was added to the wells. After a further incubation at room temperature for 1 h, the plates were washed, and 50 μL of streptavidin-HRP (diluted 1:5000) was added to all wells. The reagent o-phenylenediamine dihydrochloride (50 μL) was added 15 min later, and the plates were incubated in the dark at 37 °C for 15–20 min. After color development, the reaction was stopped with the addition of sulfuric acid (1 M), and absorbance was measured at 490 nm. The results are expressed as picograms per milligram of protein and reported as mean ± SD.
Acetic Acid-Induced Writhing Test
The acetic acid writhing test was used to evaluate analgesic activity [16]. The mice (n = 6 per group) were injected (i.p.) with 0.6 % acetic acid, and the intensity of nociception was quantified by counting the total number of writhes, which included abdominal muscle contractions and hind paw extension over 20 min. The animals received Riparin B (10 mg/kg, i.p.) or DMSO (control group, 2.0 %, v/v) 1 h before acetic acid injection. Morphine (5 mg/kg, s.c.) was administered 30 min before acetic acid as a reference condition.
Formalin Test
This test, which produces a local tissue injury to the paw, has been used as a model for tonic pain and localized inflammatory pain [17]. Twenty microliters of 2.5 % formalin was administered into the right hind paw of the mice. The licking time was recorded from 0 to 5 min (phase 1, neurogenic) and from 20 to 25 min (phase 2, inflammatory), after formalin injection [17]. The mice (n = 5 per group) were treated with Riparin B (10 mg/kg, i.p.) or DMSO (2.0 %) for 30 min before formalin injection. Morphine (5 mg/kg, s.c.) was also administered 30 min before formalin injection and used as a reference compound.
Hot Plate Test
The hot plate test also measures analgesic activity. Each mouse was placed twice onto a heated plate (50 ± 1 °C) separated by a 30-min interval. The first trial familiarized the animal with the test procedure, and the second trial served as the control for the reaction time (licking the paw or jumping). Animals showing a reaction time greater than 20 s were excluded. After the second trial (control reaction time), groups of animals (n = 5) received sterile saline (0.9 %, i.p.), Riparin B (10 mg/kg, i.p.), or morphine (5 mg/kg, s.c.; reference drug). The reaction times were measured at time zero (0 time) and 30, 60, 90, and 120 min after the compounds were administered with a cutoff time of 4 s to avoid paw lesions.
Measurement of Malondialdehyde
The samples of peritoneal fluid were collected, and malondialdehyde (MDA) concentration was measured using the method described previously with modifications [18].
Measurement of Levels of Glutathione
Glutathione (GSH) levels in the peritoneal fluid were determined according to the method described previously with modifications [19].
Statistical Analysis
Results are expressed as means ± SEM (n = 5–6 animals per group as indicated), and statistical analysis was performed using one-way analysis of variance (ANOVA) followed by the Newman−Keuls post hoc test. Statistical significance was set at p < 0.05.
RESULTS
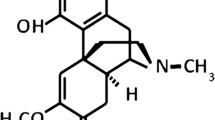
Chemical Structure
The chemical structure was performed according to the method described above. The complete reaction of this synthesis and the results obtained on 1H-NMR and 13C-NMR was completely described by Nunes et al. 2014.
Effect of Riparin B on Carrageenan-Induced Paw Edema in Mice
As shown in Table 1, the administration of carrageenan into the right hind paw (500 μg/paw) induced severe edema within 1 h of injection, which gradually heightened until reaching its peak at 4 h after injection (1 h: 0.047 ± 0.011 mL; 2 h: 0.080 ± 0.012 mL; 3 h: 0.100 ± 0.007 mL; 4 h: 0.122 ± 0.005 mL). Indomethacin (10 mg/kg) administration significantly decreased paw edema after 1 h, and this inhibitory effect was maintained throughout the experimental period (*p < 0.05), with a maximal inhibition of 88.52 %. The pretreatment with Riparin B induced significant inhibition of paw edema throughout the experimental period. At 3 h, compared to the carrageenan group, the animals pretreated with Riparin B at doses of 1, 3, and 10 mg/kg showed reductions in edema of 64.0, 78.0, and 96.0 %, respectively (Table 1). Riparin B, at a dose of 10 mg/kg, showed the maximal effect against carrageenan-induced paw edema. Therefore, this dose was selected for all subsequent protocols.
Effect of Riparin B on Paw Edema Induced by Several Inflammatory Mediators
Our results demonstrate that pretreatment with Riparin B (10 mg/kg) was able to reduce paw edema at 30 min (peak time) after injection with all stimuli. Pretreatment with Riparin B (0.022 ± 0.0040 mL) reduced paw edema induced by dextran (0.0980 ± 0.0080 mL; Fig. 1a). In addition, the same dose of Riparin B showed a significant reduction in paw volume after treatment with inflammatory mediators (Riparin B + Hist = 0.0375 ± 0.0094 mL (Fig. 1b); Riparin B + 5-HT = 0.0650 ± 0.0057 mL (Fig. 1c); Riparin B + Bk = 0.0400 ± 0.0081 mL (Fig. 1d); Riparin B + 48/80 = 0.0350 ± 0.0050 mL (Fig. 1e), and Riparin B + PGE2 = 0.0160 ± 0.0060 mL (Fig. 1f)) when compared with that observed in groups of animals treated with the mediators alone (histamine (0.0575 ± 0.0047 mL) (Fig. 1b), serotonin (5-HT) (0.1100 ± 0.0040 mL) (Fig. 1c), bradykinin (0.0700 ± 0.0100 mL) (Fig. 1d), 48/80 (0.0800 ± 0.0044 mL) (Fig. 1e), and PGE2 (0.0550 ± 0.0050 mL) (Fig. 1f)). As expected, the saline group did not present with any inflammatory effect.
Effect of Riparin B on paw edema induced by several inflammatory mediators. Paw edema was induced by dextran (Dxt, a 500 g/paw; 50 μl), histamine (Hist, b 1 %, w/v; 50 μL), serotonin (5-HT, c 1 %, w/v; 50 μL), bradykinin (Bk, d 6 nmol/paw; 50 μL), 48/80 (e 12 μg/paw; 50 μL), or PGE2 (f 3 nmol/paw; 50 μL) injections into the plantar right paw. Paw volume was measured immediately before and at selected intervals of 30 min for 2 h after inflammatory stimulus. Each point represents the mean ± SEM from five animals. Asterisk (p < 0.05) indicates a significant difference between the dextran and inflammatory mediators groups. Statistical analyses were performed using ANOVA, followed by the Newman–Keuls test.
Effect of Riparin B on Carrageenan-Induced Myeloperoxidase Activity in Paw Tissue
In Fig. 2a, our results demonstrated that carrageenan produced a marked increase in MPO activity (37.15 ± 8.40 UMPO/mg of tissue), while the group treated with Riparin B (10 mg/kg, i.p.) showed a considerable inhibition of MPO activity (13.30 ± 4.87 UMPO/mg of tissue) equivalent to a 64.20 % reduction in the action of this tissue enzyme (Fig. 2a).
Anti-inflammatory effect of Riparin B on carrageenan-induced myeloperoxidase activity in paw tissue and peritonitis in mice. a Saline (Sal; s.c.) or carrageenan (Cg; 500 g/paw) was injected into the plantar surface of mice. One hour before Sal or Cg injection, the animals were treated with 2.0 % DMSO, indomethacin (Ind; 10 mg/kg, i.p.), or Riparin B (10 mg/kg, i.p.). Myeloperoxidase (MPO) activity was detected in the paw tissue after 4 h. b and c represent total leukocyte counts and neutrophil counts per cavity, respectively. Mice were administered 250 μL of 2.0 % DMSO, saline (po), indomethacin (Ind; 10 mg/kg, po), or Riparin B (10 mg/kg, po), followed by the injection of 500 μg of carrageenan diluted in 250 μL of saline solution (i.p.) after 1 h. The mice were killed 4 h later, and the peritoneal cavity was washed with 1.5 mL of heparinized phosphate-buffered saline (PBS) to harvest the peritoneal cells. The values are represented as the means ± SEM. Octothorpe indicates p < 0.05 compared to the Sal group; asterisk indicates p < 0.05 compared to the carrageenan group. Statistical analyses were performed using ANOVA, followed by the Newman–Keuls test.
Anti-Inflammatory Effect of Riparin B on Carrageenan-Induced Peritonitis in Mice
Carrageenan administration into the peritoneal cavity promoted an increase of leukocytes (16.48 × 103 ± 0.58 × 103 cells/mL) and neutrophil cells (15.22 × 103 ± 0.81 × 103 cells/mL) in the peritoneal fluid. However, pretreatment with Riparin B (10 mg/kg) showed significantly reduced peritoneal leukocyte migration (2.52 × 103 ± 0.61 × 103 cells/mL) (Fig. 2b), and the same dose also considerably diminished the neutrophil count (1.80 × 103 ± 0.42 × 103 cells/mL) (Fig. 2c).
Effect of Riparin B on Carrageenan-Induced Cytokine Production in Peritonitis
As shown in Fig. 3, intraperitoneal administration of carrageenan induced a marked increase in IL-1β (564.9 ± 52.32 pg/mL) (Fig. 3a) and TNF-α (506.6 ± 49.86 pg/mL) (Fig. 3b). Pretreatment with Riparin B (10 mg/kg, i.p.) reduced IL-1β (78.91 ± 17.25 pg/mL) and TNF-α (13.77 ± 5.39 pg/mL) concentrations significantly.
Effect of Riparin B on carrageenan-induced cytokine production in peritonitis. Mice were pretreated with Riparin B (10 mg/kg, i.p.). One hour later, 250 μL of carrageenan (500 μg/cavity, i.p.) was injected into the peritoneal cavity, and the levels of interleukin IL-1β (a) and of TNF-α (b) were measured 4 h later. Each point represents the mean ± SEM of six animals for each group. Asterisk indicates p < 0.05 compared to DMSO (2.0 %) + carrageenan group; octothorpe indicates p < 0.05 compared to the saline group. Statistical analysis was performed using ANOVA, followed by the Newman–Keuls test.
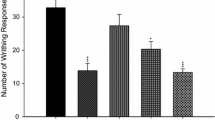
Effect of Riparin B on Nociceptive Tests
In the writhing test, the pretreatment with Riparin B (10 mg/kg, i.p.), 1 h prior to acetic acid injection, produced a significantly decreased (p < 0.05) abdominal writhing response (68.54 %) compared to the group treated with acetic acid alone (Fig. 4a). Morphine (5 mg/kg, subcutaneously) administration also reduces the writhing movements (97.65 %). In formalin test, our results demonstrated that administration of Riparin B reduces licking time in the first or neurogenic phase 52.64 % (Fig. 4b), as well as in the second or inflammatory phase 94.18 % (Fig. 4b) as compared with the formalin-only group. As expected, morphine significantly reduced the formalin response in both phases. The morphine inhibitory effect varied from a 69.15 % reduction in licking time in the first phase to a 100 % reduction in the second phase (Fig. 4b). In the hot plate, we can observe that the animals pretreated with Riparin B did not show an increase in latency for this test at any time points analyzed (Fig. 4c), when compared to the control group (DMSO). Administration of the reference drug, morphine, induced a significant increase in latency time in the hot plate test, as expected, which persisted for at least 90 min (Fig. 4c).
Effect of Riparin B on nociceptive tests. In all protocols of nociception, DMSO 2.0 %, saline (Sal), Riparin B (10 mg/kg), or morphine (5 mg/kg) were administered 30 min before introduction of the nociceptive stimulus. In a, we observe the effect of Riparin B in the acetic acid-induced writhing response in mice. b shows the effect of Riparin B on both phases of the formalin stimulus in mice. c shows the effect of Riparin B in the hot plate test in mice. The values are expressed as the mean ± SEM of six mice. Asterisk (p < 0.05) indicates a statistically significant difference from the acetic acid or formalin + DMSO (2.0 %) groups; octothorpe (p < 0.05) indicates a statistically significant difference with saline or Riparin B group. Statistical analyses were performed using ANOVA followed by the Newman–Keuls test.
Effect of Riparin B on MDA and GSH Levels in the Peritoneal Exudate of Mice
In the Fig. 5, we observe that the injection of carrageenan into the peritoneal cavity showed significantly increased MDA levels (41.83 ± 1.78 nmol/g of tissue) (Fig. 5a) compared to the saline-treated group (20.38 ± 2.30 nmol/g of tissue). By contrast, the group pretreated with Riparin B (10 mg/kg) had significantly reduced MDA levels (25.74 ± 2.06 nmol/g of tissue), as compared to the carrageenan group (Fig. 5a). Furthermore, Fig. 5b shows that treatment with carrageenan (93.67 ± 44.68 mg/g of tissue) increases the consumption of glutathione as compared to the saline group (410.7 ± 47.78 mg/g of tissue). It was also observed that pretreatment with Riparin B caused a significant increase (313.0 ± 38.71 mg/g of tissue) in glutathione levels compared to the carrageenan-only group.
Effect of Riparin B on MDA and GSH levels in the peritoneal exudate of mice. One hour before the experiment, animals were treated with 2.0 % DMSO or Riparin B (10 mg/kg). MDA (a) or GSH (b) levels in the peritoneal exudate were evaluated 4 h after carrageenan administration. Values are expressed as means ± SEM of MDA in nanomoles per milliliter of saline or milligrams per gram of tissue for GSH. Asterisk indicates p < 0.05 compared to carrageenan + DMSO group; octothorpe indicates p < 0.05 compared to saline group. Statistical analysis was performed using analysis of variance followed by the Newman–Keuls test.
DISCUSSION
Riparin B is a synthetic, riparin-derived compound that has a demonstrated anti-oxidant potential in vitro [5]. Knowing that oxidative stress plays an important role in the pathogenesis of inflammatory processes [20–22] and pain maintenance, we evaluated several models in vivo to establish the anti-inflammatory, anti-nociceptive, and anti-oxidant effects of Riparin B. Our data showed that Riparin B exhibited anti-inflammatory, anti-nociceptive, and anti-oxidant activities in vivo experimental models.
Inflammation is a complex program of intracellular signal transduction and transcription events, driven by the release of multiple pro-inflammatory mediators such as cytokines, chemokines, and growth factors [23, 24]. This event occurs as a primary protective response of the body. The inflammatory response is accompanied by intense leukocytes migration to the site of damage and increased vascular permeability, causing an accumulation of plasma proteins and release of the reactive oxygen species [25] and pain that together contribute to further exacerbation of the inflammatory reaction and the loss of function [26] on inflamed tissues [27].
To verify the action of Riparin B in an inflammatory model, we performed carrageenan-induced paw edema. Carrageenan administration induces edema in the mouse paw and is characterized by two phases. The first, or early phase, is characterized as a low-intensity edema with diffuse cellular infiltrate [23], release of histamine and serotonin, and the subsequent release of bradykinin and prostaglandins (vascular phase) [28, 29]. The late, or second phase, is characterized by cytokine production, release of macrophages and mast cells, and intense neutrophil infiltration into the inflammatory site [30, 31]. Our data demonstrated that the pretreatment with Riparin B reduced the carrageenan-induced paw edema in both the early (vascular phase) and late phases of inflammation, suggesting that its anti-edematogenic effect is mediated by the inhibition of several chemical mediators as well as by a reduction of neutrophil migration.
To specifically evaluate the action of Riparin B on the vascular phase of carrageenan-induced acute inflammation, we elicited paw edema, induced by dextran, histamine, serotonin, bradykinin, PGE2, and/or 48/80 compound. The increase in vascular permeability observed during the acute phase of the inflammatory process can be induced by administration of dextran sulfate [32, 33]. During dextran-induced paw edema, the increased vascular permeability is dependent on mast cell degranulation as well as on the action of histamine, serotonin, bradykinin, and PGE2 on the vascular endothelium, which causes leakage of fluid and proteins into the interstitium. The same process is induced by the synthetic 48/80 compound [33–38]. In the present study, the Riparin B promoted the significant reduction of paw edema induced for histamine, serotonin, bradykinin, PGE2, and 48/80 compound. Accordingly to our data, we can infer that Riparin B can modulate the events involved in the vascular phase of the inflammatory response by inhibiting the release or activity of inflammatory mediators.
The carrageenan-induced inflammatory response in paw tissue is known to be accompanied by intense leukocyte migration, primarily of neutrophils [39]. This response can be measured using the neutrophil-specific enzyme myeloperoxidase (MPO), which is an indicator of neutrophil migration into the inflammatory site [40] as this enzyme has been found in neutrophil azurophilic granules [41, 42]. Our results demonstrated that carrageenan administration induced a marked increase in MPO activity and the pretreatment with Riparin B (10 mg/kg, i.p.) showed a considerable reduction of MPO concentration in paw tissue. This result suggests that the anti-inflammatory action of Riparin B may involve the inhibition of leukocyte migration and neutrophil infiltration.
To confirm our hypothesis, we induced peritonitis by the intraperitoneal administration of carrageenan. This important pharmacological experimental tool is used to examine acute peritoneal inflammation, which allows quantification of cell migration, resident cell activation, and levels of several pro-inflammatory cytokines [42]. Our results showed that the treatment with Riparin B also reduced the total (leukocytes) and differential (neutrophils) count in the peritoneal fluid during the peritonitis assay.
Previous studies have demonstrated that carrageenan administration into the peritoneal cavity promotes the overproduction and release of TNF-α and IL-1β by activating the resident cells [43]. These inflammatory cytokines represent a powerful chemotactic factor, which activates inflammatory cells (such as mature neutrophils) and induces diapedesis at the inflammatory site [44]. Our results showed that the intraperitoneal administration of carrageenan increases the levels of IL-1β and TNF-α and the pretreatment with Riparin B reduced the concentrations of these inflammatory cytokines significantly. Thus, based on the literature and our own data, we can infer that the anti-inflammatory effect of Riparin B involves, in part, the inhibition of neutrophil infiltration and the release of the pro-inflammatory cytokines, TNF-α and IL-1β, into the site of inflammation.
There is a strong link between inflammation and pain sensation. During inflammation, the sensitization of primary nociceptive neurons occurs, producing hyperalgesia. This sensitization is caused by the direct action of inflammatory mediators such as prostaglandins (e.g., PGI2, PGE2) and sympathetic amines (epinephrine, dopamine) on nociceptor receptors [45–47]. Considering the relationship between inflammation and the development of pain, we decided to investigate the anti-nociceptive action of Riparin B, using three pain models: acetic acid-induced writhing, formalin-induced nociception test, and the hot plate test.
The acetic acid-induced writhing reaction in mice has been largely used as a screening tool for the assessment of analgesic or anti-inflammatory compounds. It is a typical model for inflammatory pain, which has long been widely used as a tool to screen for analgesic or anti-inflammatory properties of new agents [48]. Administration of acetic acid into the peritoneal cavity irritates the serous membranes and provokes a stereotypical behavior in experimental animals, characterized by abdominal contractions and twisting of the dorsal abdominal muscles [39]. This model involves various nociceptive mechanisms, such as the release of biogenic amines (e.g., histamine and serotonin), cyclooxygenases, and their metabolites [49]. These mediators activate chemosensitive, nociceptor-dependent pain by inducing capillary permeability [50, 51] and effectively reducing the nociception threshold [49].
Our data demonstrated that the pretreatment with Riparin B (10 mg/kg, i.p.) reduced significantly (p < 0.05) the number of abdominal constrictions. Morphine administration also reduces the writhing movements. From these data, we can infer that Riparin B was able to reduce acetic acid-induced writhing, by modulating the reduction of synthesis or liberation of inflammatory mediators involved.
Formalin-induced nociception was another model utilized in this study. Formalin injected into the mice paw causes an overt, pain-like behavior characterized by two phases. The first phase (0–5 min) is dependent of the release of neurotransmitters (such as serotonin), molecules from resident cells (such as histamine), and activation of TRPA1 receptors expressed by neurons. The second phase (25–30 min) depends on inflammatory mediators induced in response to the formalin stimulus and includes cytokines [46, 52]. Our results demonstrated that the pretreatment with Riparin B was able to reduce the licking time on both phases of the assay. According to these data, we can infer that Riparin B produces anti-nociceptive effects by inhibiting the action and release of inflammatory mediators such as serotonin and histamine and that it blocks the effect of pro-inflammatory cytokines (IL-1β and TNF-α) on nociceptive neurons.
In order to evaluate the involvement of central mechanisms on the anti-nociceptive effect of Riparin B, the hot plate test was performed. This test is a well-known model for evaluating acute thermal nociception and, specifically, central nociception [53]. It also measures responses to inflammation and hyperalgesia [54].
In our manuscript, the treatment with Riparin B did increase the latency time in any time points analyzed. On the other hand, the morphine induced a significant increase in latency time. These results suggest that the anti-nociceptive effect of Riparin B depends on peripheral inflammatory events, rather than on a central-acting mechanism.
Oxidative stress has been proposed to play an important role in the pathogenesis of inflammation by promoting the production of several cytokines, including the pro-inflammatory cytokines IL-1β, IL-6, and TNF-α [21], which are responsible for activating neutrophils and inducing migration to the inflammatory site. TNF-α and IL-1β activate NADPH oxidase (nicotinamide adenine dinucleotide phosphate oxidase), resulting in the production of superoxide anion, activation of NFκB, and, consequently, the production of cytokines [21, 46, 49–58]. Therefore, this relationship between cytokines and oxidative stress explain the importance of oxidative stress in inflammation and hyperalgesia [55, 58, 59]. Thus, the present study also investigated the effect of Riparin B on oxidative stress models in animals with two measurements: glutathione (GSH) and malondialdehyde (MDA).
GSH is an endogenous anti-oxidant enzymatic complex that protects the cells against reactive oxygen species generated during pathological injuries. GSH exerts this protective effect primarily by keeping the sulfhydryl groups of proteins reduced and preventing them from reacting with free radicals [60]. MDA is generated by the lipoperoxidative processes that take place as a consequence of oxidative injury in tissue [61]. Our results clearly demonstrated that the administration of Riparin B increased the levels of GSH and decreased the concentration of MDA in peritoneal fluid. According to our findings and based on the literature, we can infer that Riparin B decreases inflammation-induced tissue damage by stimulating the production and action of endogenous antioxidants (GSH) and decreasing lipid peroxidation in the organism.
CONCLUSION
In summary, our manuscript demonstrates that Riparin B can inhibit inflammatory pathways by modulating the formation of pathological signs of inflammation including paw edema induced by several mediators, neutrophil migration, cytokine release, and hyperalgesia. Further, these effects seem to be dependent on the inhibition of free radicals in inflammatory events. These findings suggest that Riparin B represents an important pharmacological tool to promote tissue resistance against damage that occurs during an inflammatory condition.
REFERENCES
Calixto, J.B., M.F. Otuki, and A.R. Santos. 2003. Anti-inflammatory compounds of plant origin. Part I. Action on arachidonic acid pathway, nitric oxide and nuclear factor kappa B (NF-kappaB). Planta Medica 69(11): 973–983.
Soares, A.M., F.K. Ticli, S. Marcussi, M.V. Lourenço, A.H. Januário, S.V. Sampaio, J.R. Giglio, B. Lomonte, and P.S. Pereira. 2005. Medicinal plants with inhibitory properties against snake venoms. Current Medicinal Chemistry 12: 2625–2641.
Molinski, T.F., D.S. Dalisay, S.L. Lievens, and J.P. Saludes. 2009. Drug development from marine natural products. Nature Reviews Drug Discovery 8(1): 69–85.
Radjasa, O.K., Y.M. Vaske, G. Navarro, H.C. Vervoort, K. Tenney, R.G. Linington, and P. Crews. 2011. Highlights of marine invertebrate-derived biosynthetic products: Their biomedical potential and possible production by microbial associants. Bioorganic and Medicinal Chemistry 19(22): 6658–6674.
Nunes, G.B.L., P.R. Policarpo, L.M. Costa, T.G. Da Silva, C.G.G. Militão, C.A. Câmara, J.M. Barbosa Filho, S.J.C. Gutierrez, M.T. Islam, and R.M. De Freitas. 2014. In vitro antioxidant and cytotoxic activity of some synthetic riparin-derived compounds. Molecules 19(4): 4595–4607.
Essa, M.M., N. Braidy, W. Bridge, S. Subash, T. Manivasagam, R.K. Vijayan, S. Al-Adawi, and G.J. Guillemin. 2012. Review of natural products on Parkinson’s disease pathology. Journal of Aging Research & Clinical Practice 3(3): 127–136.
Araújo, F.L., C.T. Melo, N.F. Rocha, B.A. Moura, C.P. Leite, J.F. Amaral, J.M. Barbosa-Filho, S.J. Gutierrez, S.M. Vasconcelos, G.S. Viana, and F.C. de Sousa. 2009. Antinociceptive effects of (O-methyl)-N-benzoyl tyramine (riparin I) from Aniba riparia (Nees) Mez (Lauraceae) in mice. Naunyn-Schmiedeberg’s Archives of Pharmacology 380: 337–344.
Carvalho, A.M.R., N.F.M. Rocha, L.F. Vasconcelos, E.R.V. Rios, M.L. Dias, M.I.G. Silva, M.M.F. Fonteles, J.M. Barbosa Filho, S.J.C. Gutierrez, and F.C.F. De Sousa. 2013. Evaluation of the anti-inflammatory activity of riparin II (O-methil-N-2-hidroxi-benzoyl tyramine) in animal models. Chemico-Biological Interactions 205: 165–172.
De Melo, C.T.V., A.P. Monteiro, C.P. Leite, F.L.O. De Araújo, V.T.M. Lima, J.M. Barbosa-Filho, M.M.F. Fonteles, S.M.M. Vasconcelos, G.S.B. Viana, and F.C.F. Sousa. 2006. Anxiolytic-like effects of (O-methyl)-N-2,6-dihydroxybenzoyl-tyramine (riparin III) from Aniba riparia (NEES) MEZ (Lauraceae) in mice. Biological and Pharmaceutical Bulletin 29: 451–454.
Geetha, T., P. Varalakshmi, and L.R. Mary. 1998. Effect of triterpenes from Crataeva nurvata stem bark on lipid peroxidation in adjuvant induced arthritis in rats. Pharmacological Research 37: 191–195.
Quignard, E.L.J., S.M. Nunomura, A.M. Pohlit, A.M. Alecrim, A.C.S. Pinto, C.N. Portela, L.C.P. Oliveira, L.C. Don, L.F. Rocha e Silva, and M.C. Henrique. 2004. Median lethal concentrations of amazonian plant extracts in the brine shrimp assay. Pharmaceutical Biology 42: 253–257.
Marchand, F., M. Perretti, and S.B. McMahon. 2005. Role of the immune system in chronic pain. Nature Reviews Neuroscience 6: 521–532.
Nguemfo, E.L., T. Dimo, A.B.. Dongmo, A.G.B. Azebaze, K. Alaoui, A.E. Asongalem, Y. Cherrah, and P. Kamtchouing. 2009. Anti-oxidative and anti-inflammatory activities of some isolated constituents from the stem bark of Allanblackia monticola Staner L.C (Guttiferae). Inflammopharmacology 17: 37–41.
Winter, C.A., E.A. Risley, and G.W. Nuss. 1962. Carrageenin-induced edema in hindpaw of the rat as an assay for anti-inflammatory drugs. Proceedings of the Society for Experimental Biology and Medicine 111: 544–547.
Lanhers, M.C., J. Fleurentin, P. Dorfman, F. Mortier, and J.M. Pelt. 1991. Analgesic, antipyretic and anti-inflammatory properties of Euphorbia hirta. Planta Medica 57: 225–231.
Collier, H.O.J., J.C. Dinneen, C.A. Johnson, and C. Schneider. 1968. The abdominal constriction response and its suppression by analgesic drugs in the mouse. British Journal of Pharmacology and Chemotherapy 32: 295–310.
Hunskaar, S., and K. Hole. 1987. The formalin test in mice: dissociation between inflammatory and non-inflammatory pain. Pain 30: 103–104.
Mihara, M., and M. Uchiyama. 1978. Determination of malonaldehyde precursor in tissues by thiobarbituric acid test. Analytical Biochemistry 86: 271–278.
Nagy, L., M. Nagata, and S. Szabo. 2007. Protein and non-protein sulfhydryls and disulfides in gastric mucosa and liver after gastrotoxic chemicals and sucralfate: possible new targets of pharmacologic agents. World Journal of Gastroenterology 13(14): 2053–2060.
Josse, C., J.R. Boelaert, M. Best-Belpomme, and J. Piette. 2001. Importance of post-transcriptional regulation of chemokine genes by oxidative stress. Biochemical Journal 360: 321–333.
Cuzzocrea, S., D.P. Riley, A.P. Caputi, and D. Salvemini. 2001. Antioxidant therapy: a new pharmacological approach in shock, inflammation, and ischemia/reperfusion injury. Pharmacological Reviews 53: 135–159.
Borghi, S.M., T.T. Carvalho, L. Staurengo-Ferrari, M.S.N. Hohmann, P. Pinge-Filho, R. Casagrande, and W.A. Verri Jr. 2013. Vitexin inhibits inflammatory pain in mice by targeting TRPV1, oxidative stress, and cytokines. Journal of Natural Products 76: 1141–1149.
Gutierrez, S.J.C. 2007. Síntese do bowdenol um dihidrobenzofuranoide isolado de bowdichia virgilioides e preparação de derivados da riparina isolada de aniba riparia com potencial atividade biológica. Doctorate Thesis, UFPB/CCS: João Pessoa, Brazil.
Sherwood, E.R., and T. Toliver-Kinsky. 2004. Mechanisms of the inflammatory response. Best Practice & Research. Clinical Anaesthesiology 18: 385–405.
Siddiqui, M.R., K. Tran, S.P. Reddy, and A.B... Malik. 2014. Reactive oxygen species in inflammation and tissue injury. Antioxidants & Redox Signaling 20(7): 1126–1167.
Nathan, C. 2002. Points of control in inflammation. Nature 420: 846–852.
Xavier, S.M., C.O. Barbosa, D.O. Barros, R.F. Silva, A.A. Oliveira, and R.M. Freitas. 2007. Vitamin C antioxidant effects in hippocampus of adult Wistar rats after seizures and status epilepticus induced by pilocarpine. Neuroscience Letters 420: 76–79.
De Brito, T.V., R.S. Prudêncio, A.B... Sales, F. Vieira Jr., S.J. Candeira, Á.X. Franco, K.S. Aragão, R.A. Ribeiro, M.H.P. De Souza, L.S. Chaves, A.L. Freitas, J.V. Medeiros, and A.L.R. Barbosa. 2013. Anti-inflammatory effect of a sulphated polysaccharide fraction extracted from the red algae Hypnea musciformis via the suppression of neutrophil migration by the nitric oxide signalling pathway. Journal of Pharmacy and Pharmacology 65: 724–733.
Dawson, J., A.D. Sedgwick, J.C. Edwards, and P. Lees. 1991. A comparative study of the cellular, exudative and histological responses to carrageenan, dextran and zymosan in the mouse. International Journal of Tissue Reactions 13(4): 171–185.
Cragg, G.M., D.J. Newman, and K.M. Snader. 1997. Natural products in drug discovery and development. Journal of Natural Products 60: 52–60.
De Smet, P.A. 2007. The role of plant-derived drugs and herbal medicines in healthcare. Drugs 54: 801–840.
Rowley, D.A., and E.P. Benditt. 1956. Serotonin and histamine as mediators of vascular injury produced by agents which damage mast cells in rats. Journal of Experimental Medicine 103: 399–415.
Kulkarni, S.K., A.K. Mehta, and J. Kunchandy. 1986. Anti-inflammatory actions of clonidine, guanfacine and B-HT 920 against various inflammagen-induced acute paw oedema in rats. Archives Internationales de Pharmacodynamie et de Thérapie 279(2): 324–334.
Seibert, K., Y. Zhang, K. Leahy, S. Hauser, J. Masferrer, W. Perkins, L. Lee, and P. Isakson. 1994. Pharmacological and biochemical demonstration of the role of cyclooxygenase 2 in inflammation and pain. Proceedings of the National Academy of Sciences 91: 12013–12017.
Lago, J., A. Alfonso, M.R. Vieytes, and L.M. Botana. 2001. Ouabain-induced enhancement of rat mast cells response. Modulation by protein phosphorylation and intracellular pH. Cellular Signalling 13: 515–524.
Okazaki, T., V.S. Ilea, A. Okazaki, K. Wicher, R.E. Reisman, and C.E. Arbesman. 1976. Inhibition of antigen-induced histamine release by ouabain. Journal of Allergy and Clinical Immunology 57: 454–462.
Ennis, M., F.L. Pearce, and P.M. Weston. 1980. Some studies on the release of histamine from mast cells stimulated with polylysine. British Journal of Pharmacology 70: 329–334.
Senol, M., I.H. Ozerol, A.V. Patel, and D.P. Skoner. 2007. The effect of Na+-K+ ATPase inhibition by ouabain on histamine release from human cutaneous mast cells. Molecular and Cellular Biochemistry 294: 25–29.
Carvalho, J.C., J.R. Teixeira, P.J. Souza, J.K. Bastos, D. Dos Santos Filho, and S.J. Sarti. 1996. Preliminary studies of analgesic and anti-inflammatory properties of Caesalpinia ferrea crude extract. Journal of Ethnopharmacology 53: 175–178.
Ajuebor, M.N., A. Singh, and J.L. Wallace. 2000. Cyclooxygenase-2-derived prostaglandin D(2) is an early anti-inflammatory signal in experimental colitis. American Journal of Physiology. Gastrointestinal and Liver Physiology 279(1): 238–244.
Souza, G.E., F.Q. Cunha, R. Mello, and S.H. Ferreira. 1988. Neutrophil migration induced by inflammatory stimuli is reduced by macrophage depletion. Agents and Actions 24: 377–380.
Montanher, A.B..., S.M. Zucolotto, E.P. Schenkel, and T.S. Fröde. 2007. Evidence of anti-inflammatory effects of Passiflora edulis in an inflammation model. Journal of Ethnopharmacology 109: 281–288.
Chaves, L.S., L.A.D. Nicolau, R.O. Silva, F.C. Barros, A.L. Freitas, K.S. Aragão, R.A. Ribeiro, M.H.L.P. Souza, A.L.R. Barbosa, and J.V.R. Medeiros. 2013. Antiinflammatory and antinociceptive effects in mice of a sulfated polysaccharide fraction extracted from the marine red algae Gracilaria caudata. Immunopharmacology and Immunotoxicology 35: 93–100.
Sutbeyaz, Y., B. Yakan, H. Ozdemir, M. Karasen, F. Doner, and I. Kufrevioglu. 1996. Effect of SC-41930, a potent selective leukotriene B4 receptor antagonist, in the guinea pig model of middle ear inflammation. Annals of Otology, Rhinology and Laryngology 105: 476–480.
Cunha, T.M., W.A. Verri Jr., J.S. Silva, S. Poole, F.Q. Cunha, and S.H. Ferreira. 2005. A cascade of cytokines mediates mechanical inflammatory hypernociception in mice. Proceedings of the National academy of Sciences of the United States of America 102: 1755–1760.
Verri Jr., W.A., T.M. Cunha, C.A. Parada, S. Poole, F.Q. Cunha, and S.H. Ferreira. 2006. Hypernociceptive role of cytokines and chemokines: targets for analgesic drug development? Pharmacology and Therapeutics 112: 116–138.
Zarpelon, A.C., T.M. Cunha, J.C. Alves-Filho, L.G. Pinto, S.H. Ferreira, I.B. McInnes, D. Xu, F.Y. Liew, F.Q. Cunha, and W.A. Verri Jr. 2013. IL-33/ST2 signalling contributes to carrageenin-induced innate inflammation and inflammatory pain: role of cytokines, endothelin-1 and prostaglandin E2. British Journal of Pharmacology 169: 90–101.
Collier, H.O., L.C. Dinneen, C.A. Johnson, and C. Schneider. 1968. The abdominal constriction response and its suppression by analgesic drugs in the mouse. British Journal of Pharmacology 32(2): 295–310.
Duarte, I.D.G., M. Nakamura, and S.H. Ferreira. 1988. Participation of the sympathetic system in acetic acid-induced writhing in mice. Brazilian Journal of Medical and Biological Research 21: 341–343.
Medzhitov, R. 2008. Origin and physiological roles of inflammation. Nature 454: 428–435.
Ikeda, Y., A. Ueno, H. Naraba, and S. Oh-ishi. 2001. Involvement of vanilloid receptor VR1 and prostanoids in the acid-induced writhing responses of mice. Life Science 69: 2911–2919.
Dubuisson, D., and S.G. Dennis. 1977. The formalin test: a quantitative study of the analgesic effects of morphine, meperidine, and brain stem stimulation in rats and cats. Pain 4: 161–174.
Eddy, N.B., and D. Leimbach. 1953. Synthetic analgesics. II. Dithienylbutenyl- and dithienylbutylamines. Journal of Pharmacology and Experimental Therapeutics 107: 385–393.
Bhandare, A.M., A.D. Kshirsagar, N.S. Vyawahare, A.A. Hadambar, and V.S. Thorve. 2010. Potential analgesic, anti-inflammatory and antioxidant activities of hydroalcoholic extract of Areca catechu L. nut. Food and Chemical Toxicology 48: 3412–3417.
Zeashan, H., G. Amresh, C.V. Rao, and S. Singh. 2009. Antinociceptive activity of Amaranthus spinosus in experimental animals. Journal of Ethnopharmacology 122: 492–496.
Verri Jr., W.A., F.T.M.C. Vicentini, M.M. Baracat, S.R. Georgetti, R.D.R. Cardoso, T.M. Cunha, S.H. Ferreira, F.Q. Cunha, M.J.V. Fonseca, and R. Casagrande. 2012. Flavonoids as anti-inflammatory and analgesic drugs: mechanisms of action and perspectives in the development of pharmaceutical forms. Studies in Natural Products Chemistry 36: 297–322.
Wang, Z.Q., F. Porreca, S. Cuzzocrea, K. Galen, R. Lightfoot, E. Masini, C. Muscol, V. Mollace, M. Ndengele, H. Ischiropoulos, and D. Salvemini. 2004. A newly identified role for superoxide in inflammatory pain. Journal of Pharmacology and Experimental Therapeutics 309: 869–878.
Kilpatrick, L.E., S. Sun, H. Li, T.C. Vary, and H.M. Korchak. 2010. Regulation of TNF-induced oxygen radical production in human neutrophils: role of delta-PKC. Journal of Leukocyte Biology 87: 153–164.
Feng, L., Y. Xia, G.E. Garcia, D. Hwang, and C.B. Wilson. 1995. Involvement of reactive oxygen intermediates in cyclooxygenase-2 expression induced by interleukin-1, tumor necrosis factor-alpha, and lipopolysaccharide. Journal of Clinical Investigation 95: 1669–1675.
Amirshahrokhi, K., S. Bohlooli, and M.M. Chinifroush. 2011. The effect of methylsulfonylmethane on the experimental colitis in the rat. Toxicology and Applied Pharmacology 253: 197–202.
Pacher, P., J.S. Beckman, and L. Liaudet. 2007. Nitric oxide and peroxynitrite in health and disease. Physiological Reviews 87: 315–424.
ACKNOWLEDGMENTS
The authors gratefully acknowledge UFPI/CNPq and Research foundation for the state of Piauí—FAPEPI for fellowship support.
Conflict of interest
The authors declare that they have no competing interests.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Santiago, R.F., de Brito, T.V., Dias, J.M. et al. Riparin B, a Synthetic Compound Analogue of Riparin, Inhibits the Systemic Inflammatory Response and Oxidative Stress in Mice. Inflammation 38, 2203–2215 (2015). https://doi.org/10.1007/s10753-015-0203-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10753-015-0203-4