Abstract
Esculetin, a coumarin derivative from various natural plants, has an anti-inflammatory property. In the present study, we examined if esculetin has any salutary effects against lipopolysaccharide (LPS)-induced acute lung injury (ALI) in mice. Acute lung injury (ALI) was induced via the intratracheal administration of LPS, and esculetin (20 and 40 mg/kg) was given intraperitoneally 30 min before LPS challenge. After 6 h of LPS administration, lung tissues were collected for analysis. Pretreatment with esculetin significantly attenuated histopathological changes, inflammatory cell infiltration, and production of pro-inflammatory cytokines, such as tumor necrosis factor (TNF)-α, interleukin (IL)-1β, and IL-6, in the lung tissue. Furthermore, esculetin inhibited the protein kinase B (AKT), extracellular signal-regulated kinase (ERK), and nuclear factor-kappa B (NF-κB) pathways and downregulated the expression of RORγt and IL-17 in LPS-induced ALI. Our results indicated that esculetin possesses anti-inflammatory and protective effects against LPS-induced ALI via inhibition of the AKT/ERK/NF-κB and RORγt/IL-17 pathways.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Acute lung injury (ALI) and acute respiratory distress syndrome (ARDS), which is its more severe form, are widespread inflammatory processes in the lung, which could result in pulmonary interstitial edema, deteriorated lung compliance, and subsequent severe hypoxemia [1]. Despite extensive advances in supportive care, including ventilatory and non-ventilatory strategies, the mortality rate of ALI remains quite high at approximately 40% [2]. The pathogenesis of ALI is acute inflammatory response characterized by the accumulation and activation of inflammatory cells, secretion of pro-inflammatory cytokines and chemokines, production of reactive oxygen species (ROS), and subsequent death of pulmonary cells [3,4,5,6]. Accordingly, several studies have shown that anti-inflammatory mediators or anti-inflammatory drugs could treat early-stage ALI [7,8,9]. Lipopolysaccharide (LPS), a major component of the outer membrane present in gram-negative bacteria [10], is an extremely strong stimulator of the innate immunity system [11] and has been often used to induce ALI in several animal models [12].
Nuclear factor-kappa B (NF-κB), a key nuclear transcription factor, is an important regulator of inflammatory processes and immune responses [13]. Previous studies have shown that NF-κB plays a vital role in the pathogenesis of ALI/ARDS [14, 15]. The activation of NF-κB induced by LPS is required for the maximal transcription of various inflammatory mediators, including tumor necrosis factor (TNF)-α, interleukin (IL)-1β, and IL-6, in ALI [16]. Excessive production of these pro-inflammatory cytokines is significantly associated with the severity of ALI [17]. Moreover, the mitogen-activated protein kinase (MAPK) signaling pathway, which regulates the intracellular signal transduction to extracellular stimuli, plays an important role in the expression of pro-inflammatory mediators and activation of NF-κB [18]. The MAPK families, including extracellular signal-regulated kinase (ERK), c-Jun N-terminal kinase (JNK), and p38, mediate inflammatory processes and immune responses in LPS-induced ALI [19]. A recent study has shown that the inhibition of MAPK and NF-κB activity could attenuate inflammatory responses during LPS-induced ALI [20]. Furthermore, growing evidence has indicated that the protein kinase B (AKT) pathway, an important cellular signaling that regulates numerous cellular processes, plays a key role in cell survival and inflammatory processes [21]. In addition, another recent study has revealed that AKT could regulate NF-κB activity [22].
IL-17, a signature cytokine of the T help 17 (Th17) cell subset, is a pro-inflammatory cytokine that plays a crucial role in the recruitment and activation of neutrophils [23]. Apart from Th17 cells, IL-17 is also produced by innate immune cells, such as natural killer (NK) cells, NKT cells, and γδ T cells [24]. Moreover, previous study has shown that IL-17 facilitates neutrophil recruitment and accumulation by upregulating the expression of chemokines in pulmonary infection [25]. Moreover, IL-17 has been involved in various inflammatory pulmonary diseases, including autoimmune diseases, asthma, and infection [26,27,28,29]. The overexpression of IL-17 could lead to the upregulation of inflammatory cytokines and chemokines, which recruit and activate inflammatory cells in the lung [30]. A recent study has shown that anti-IL-17 can protect against LPS-induced ALI mediated by the decreased expression of inflammatory cytokines [31].
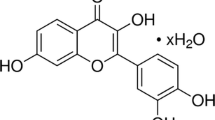
Esculetin (6,7-dihydroxycoumarin) is a coumarin derivative found in the products of various natural plants, such as Artemisia capillaris, Ceratostigma willmottianum, and Euphorbia lathyris [32]. Esculetin possesses diverse biological and pharmacological properties, including anti-asthma, anti-inflammatory, anti-nociceptive, antioxidative, antitumor, and antiviral activities [33,34,35]. Although esculetin has a protective effect against LPS-induced lung injury via partly inhibiting the NF-κB pathway, the detailed mechanism about the protective role of esculetin had not been investigated in a previous study [36]. We hypothesized that esculetin protects against LPS-induced ALI through MAPK/NF-κB and IL-17 pathways. Therefore, the present study aimed to investigate the protective role of esculetin against LPS-induced lung injury via the modulation of the AKT, MAPK, NF-κB, and IL-17 pathways. Importantly, our study may provide future directions for ALI treatment in humans and animals.
MATERIALS AND METHODS
Animals
Adult male C57BL/6C (B6) mice (20–25 g, 8–10 weeks old) were purchased from BioLASCO Taiwan Co., Ltd. (Taipei, Taiwan). All mice were housed in an environmentally controlled facility with a 12-h light and dark cycle and were allowed ad libitum access to sterile food and clean water. All animal experimental procedures were performed in accordance with the guidelines of the Animal Welfare Act and e Guide for Care and Use of Laboratory Animals from the National Institute of Health. The protocols were approved by the Institutional Animal Care and Use Committee of Chang Gung Memorial Hospital.
Experimental Model and Treatments
The mice were randomly separated into six groups, each with 5–6 mice: control group (phosphate-buffered saline [PBS]), esculetin alone group, LPS group, dexamethasone (Dex) + LPS group, esculetin 20 mg/kg + LPS group, and esculetin 40 mg/kg + LPS group. Dex (5 mg/kg), esculetin (20 and 40 mg/kg) [36], and equal volume of saline were administered intraperitoneally 30 min before LPS challenge. Moreover, 2.5 μg/g of LPS in 50 μl PBS was injected to the trachea to induce lung injury [37]. After 6 h of LPS treatment, the mice were anesthetized and sacrificed, and the lung tissues were harvested for further analyses.
Histology and Immunohistochemistry
The lungs were excised and fixed in 4% paraformaldehyde and embedded in paraffin. For histological examination, sections of 4-μm thickness were stained using hematoxylin and eosin (H&E). For immunohistochemical staining, the sections were incubated in primary antibody against Ly-6G (neutrophil; 1:500; BD Biosciences Pharmingen, San Diego, CA, USA), Mac-2 (macrophage; 1:500; eBioscience, Inc., San Diego, CA, USA), RORγt (1:500; Thermo Fisher Scientific, Inc. Waltham, MA, USA), or IL-17 (1:500; Abcam, Cambridge, MA, USA). After rinsing with PBS, the sections were incubated in biotin and streptavidin horseradish peroxidase (HRP)-conjugated secondary antibody (IHC Select; Millipore). Finally, after washing with PBS, the immune complex was visualized using 3,3′-diamino-benzidine chromogen reagent (IHC Select; Millipore).
Measurement of TNF-α, IL-1β, IL-6, and IL-23 Levels in the Lung
For evaluating immune response at the site of inflammation, we measured the levels of TNF-α, IL-1β, IL-6, and IL-23. The lung tissues were homogenized in lysis buffer (20 mM HEPES, 1 mM 2-mercaptoethanol [2-ME], 3 mM MgCl2, 150 mM NaCl, 1 M dithiothreitol [DTT], 0.1 mM phenylmethylsulfonyl fluoride [PMSF], 0.25 μg leupeptin, 0.05 μg pepstatin A, and 0.01 μg aprotinin) on ice. Next, to obtain the supernatants, tissue homogenates were centrifuged at 12000 g for 10 min at 4 °C. Finally, the levels of TNF-α, IL-1β, IL-6, and IL-23 were measured in accordance with the manufacturer’s instructions with absorbance at 450 nm.
Western Blotting
The lung tissues were homogenized in lysis buffer (20 mM HEPES, 1 mM 2-ME, 3 mM MgCl2, 150 mM NaCl, 1 M DTT, 0.1 mM PMSF, 0.25 μg leupeptin, 0.05 μg pepstatin A, and 0.01 μg aprotinin). Then, the homogenized tissues were sonicated for 15 s and centrifuged at 12000 g for 10 min at 4 °C. Moreover, 10% sodium dodecyl sulfate polyacrylamide gel electrophoresis was used to separate the protein, followed by electroblotting onto polyvinylidene fluoride membrane. After blocking in 5% fat-free milk solution for 1 h and rinsing thrice with Tris-buffer (1% Tween-20), the membrane was incubated with specific primary antibody against ERK, JNK, p38, AKT, NF-κB, RORγt, phospho-ERK, phospho-JNK, phosphon-p38, phospho-AKT, and phospho-NF-κB (1:1000; Cell Signaling Technology, MA, USA) overnight at 4 °C. After washing and incubation with HRP-conjugated secondary antibody (Cell Signaling Technology, MA, USA) for 1 h at room temperature, the final immune complexes were visualized using the enhanced chemiluminescence system. The antibody specific to β-actin (Proteintech Group, Inc., Chicago, IL, USA) was used to confirm the loading accuracy.
Statistical Analysis
All data were presented as mean ± standard error of mean (each group with 5–6 mice). One-way analysis of variance and Tukey’s multiple comparison tests were used to analyze the results. The Prism 6.0 Software (GraphPad Software Inc., San Diego, CA, USA) was used to perform the statistical analyses. A p value < 0.05 was considered statistically significant.
RESULTS
Effects of Esculetin on Histological Changes in the Lung
To evaluate the effect of esculetin on ALI, the lungs of mice were harvested 6 h after the administration of LPS. Then, the lung tissues were fixed and stained with H&E. The LPS group showed extensive histopathological changes, such as alveolar wall thickening, interstitial edema, and pulmonary congestion, compared to the control group (Fig. 1). These histopathological findings were ameliorated by pretreatment with Dex (5 mg/kg) or esculetin (20 and 40 mg/kg) 30 min before LPS challenge (Fig. 1). These results indicated that esculetin could ameliorate LPS-induced lung injury.
Effects of esculetin on histological changes in the lung induced by LPS. Dex (5 mg/kg), esculetin (ES, 20 and 40 mg/kg), or equal volume of saline was administered intraperitoneally 30 min before intratracheal LPS challenge. Mice were sacrificed after 6 h of LPS challenge, and lungs were harvested for H&E staining. Representative histological changes of the lung tissues obtained from six groups. (100 × magnifications are shown).
Effects of Esculetin on the Infiltration of Neutrophil in the Lung
To investigate the infiltration and accumulation of neutrophils in LPS-induced ALI, lung sections were immunohistochemically stained with Ly6G antibody, a specific marker for granulocyte. The LPS group presented with dominant neutrophil infiltration in the lung tissue compared with the control group. The Dex (5 mg/kg) and esculetin (20 and 40 mg/kg) pretreated groups had significantly reduced neutrophil accumulation in the lung tissue compared to the LPS group (Fig. 2).
Effects of esculetin on neutrophil infiltration in the lung induced by LPS. Dex (5 mg/kg), esculetin (ES, 20 and 40 mg/kg), or equal volume of saline was administered intraperitoneally 30 min before intratracheal LPS challenge. Mice were sacrificed after 6 h of LPS challenge and lungs were harvested. The lung sections were immunostained with Ly6G antibody (brown). Representative immunohistochemical staining of the lung tissues obtained from six groups. (200 × magnifications are shown).
Effects of Esculetin on the Infiltration of Macrophages in the Lung
To investigate the infiltration and accumulation of macrophages in LPS-induced ALI, lung sections were immunohistochemically stained with Mac-2 antibody, a specific marker for macrophage. The LPS group presented with obvious macrophage infiltration in the lung tissue compared with the control group. The Dex (5 mg/kg) and esculetin (20 and 40 mg/kg) pretreated groups had significantly reduced macrophage accumulation in the lung tissue compared with the LPS group (Fig. 3).
Effects of esculetin on macrophage infiltration in the lung induced by LPS. Dex (5 mg/kg), esculetin (ES, 20 and 40 mg/kg), or equal volume of saline was administered intraperitoneally 30 min before intratracheal LPS challenge. Mice were sacrificed after 6 h of LPS challenge and lungs were harvested. The lung sections were immunostained with Mac-2 antibody (brown). Representative immunohistochemical staining of the lung tissues obtained from six groups. (200 × magnifications are shown).
Effects of Esculetin on Pneumonic TNF-α, IL-1β, IL-6, and IL-23 Levels
To evaluate the effects of esculetin on the expression of pro-inflammatory cytokine in LPS-induced lung injury, we measured the levels of TNF-α, IL-1β, IL-6, and IL-23 in the lung tissues using ELISA. The pulmonary levels of TNF-α, IL-1β, IL-6, and IL-23 were significantly elevated in the LPS group than in the control group. No differences were observed in the levels of these pro-inflammatory cytokines between the control and esculetin alone groups. About 30 min prior to the administration of LPS, pretreatment with Dex (5 mg/kg) significantly decreased the pulmonary TNF-α, IL-1β, IL-6, and IL-23 levels (p < 0.005, 0.005, 0.005, and 0.05, respectively) than LPS group. Moreover, pretreatment with esculetin (20 mg/kg) attenuated pulmonary TNF-α, IL-1β, and IL-6 levels (p < 0.01, p < 0.01, p < 0.005, respectively) than LPS group. Furthermore, pretreatment with a higher dose of esculetin (40 mg/kg) significantly attenuated pulmonary TNF-α, IL-1β, IL-6, and IL-23 levels (p < 0.01, 0.005, 0.005, and 0.05, respectively) than LPS group (Fig. 4). These results indicated that pretreatment with esculetin could reduce the production and expression of pro-inflammatory cytokines in LPS-induced lung injury.
Effects of esculetin on TNF-α (a), IL-1β (b), IL-6 (c), and IL-23 (d) levels in the lung induced by LPS. Dex (5 mg/kg), esculetin (ES, 20 and 40 mg/kg), or equal volume of saline was administered intraperitoneally 30 min before intratracheal LPS challenge. Mice were sacrificed after 6 h of LPS challenge and lungs were harvested for ELISA assay. All values are represented as mean ± SEM (n = 6 per group). #p < 0.05, ##p < 0.01, ###p < 0.005 vs. the control group; *p < 0.05, **p < 0.01, ***p < 0.005 vs. the LPS group.
Effects of Esculetin on ERK, JNK, p38, AKT, and NF-κB Expression and Phosphorylation in the Lung
We further investigated the AKT, MAPK family protein, and NF-κB expression and phosphorylation in the lung tissues induced by LPS. No significant differences were observed in pulmonary AKT, ERK, JNK, p38, and NF-κB protein expressions between the control and esculetin alone groups. The AKT, ERK, and NF-κB activity, as determined by its phosphorylation, increased in the LPS group compared with the control group. Moreover, pretreatment with Dex (5 mg/kg) or esculetin (20 and 40 mg/kg) 30 min before the administration of LPS significantly decreased the phosphorylated AKT, ERK, and NF-κB expressions compared with the LPS group (Fig. 5). However, no significant differences were observed in the pulmonary JNK and p38 protein expressions and phosphorylation among the six groups. Taken together, our data indicated that pretreatment with esculetin could attenuate the AKT, ERK, and NF-κB phosphorylation and activation in the lung in LPS-induced ALI.
Effects of esculetin on ERK (a), JNK (b), p38 (c), AKT (d), and NF-κB (e) expression and phosphorylation in the lung induced by LPS. Dex (5 mg/kg), esculetin (ES, 20 and 40 mg/kg), or equal volume of saline was administered intraperitoneally 30 min before intratracheal LPS challenge. Mice were sacrificed after 6 h of LPS challenge, and lungs were harvested for western blotting analysis. The bands were analyzed using densitometry. All values are represented as mean ± SEM (n = 5–6 per group). ##p < 0.01, ###p < 0.005 vs. the control group; **p < 0.01, ***p < 0.005 vs. the LPS group.
Effects of Esculetin on RORγt and IL-17 Expression in the Lung
To investigate the possible anti-inflammatory mechanism of esculetin in LPS-induced ALI, lung sections were immunohistochemically stained with RORγt and IL-17 antibody. The LPS group showed significant RORγt and IL-17 expressions in the lung tissues compared with the control group. Moreover, the Dex (5 mg/kg) and esculetin (20 and 40 mg/kg) pretreated groups showed significantly decreased RORγt and IL-17 expressions in the lung tissues compared to the LPS group (Figs. 6A, 7). We further examined the RORγt expression in the lung tissues using the western blotting assay. The expression of ROR significantly increased in the LPS group compared with the control group. Furthermore, pretreatment with Dex (5 mg/kg) or esculetin (20 and 40 mg/kg) 30 min before the administration of LPS decreased the RORγt expression compared to the LPS group (Fig. 6B) Taken together, our result indicated that pretreatment with esculetin could reduce the expression of RORγt and IL-17 in the lung in LPS-induced ALI.
Effects of esculetin on RORγt expression in the lung induced by LPS. Dex (5 mg/kg), esculetin (ES, 20 and 40 mg/kg), or equal volume of saline was administered intraperitoneally 30 min before intratracheal LPS challenge. Mice were sacrificed after 6 h of LPS challenge and lungs were harvested. (A) The lung sections were immunostained with RORγt antibody (brown). Representative immunohistochemical staining of the lung tissues obtained from six groups. (200 × magnifications are shown). (B) Protein extracted from the lung tissues analyzed by western blotting. The bands were analyzed using densitometry. All values are represented as mean ± SEM (n = 5–6 per group). #p < 0.05, ###p < 0.005 vs. the control group; *p < 0.05, ***p < 0.005 vs. the LPS group.
Effects of esculetin on IL-17 expression in the lung induced by LPS. Dex (5 mg/kg), esculetin (ES, 20 and 40 mg/kg), or equal volume of saline was administered intraperitoneally 30 min before intratracheal LPS challenge. Mice were sacrificed after 6 h of LPS challenge and lungs were harvested. The lung sections were immunostained with IL-17 antibody (brown). Representative immunohistochemical staining of the lung tissues obtained from six groups. (200 × magnifications are shown).
DISCUSSION
In the current study, we investigated the protective effect of esculetin on LPS-induced ALI in mice. Our data showed that pretreatment with esculetin significantly attenuated LPS-induced histopathological changes, decreased the infiltration of inflammatory cells, and reduced the production of pro-inflammatory cytokines (i.e., TNF-α, IL-1β, and IL-6) in the lung tissue. Moreover, pretreatment with esculetin suppressed the phosphorylation of AKT, ERK, and NF-κB proteins and inhibited the expression of RORγt and IL-17 in the LPS-induced lung tissue. Taken together, our results indicated that esculetin has protective effects against LPS-induced ALI in mice, and the anti-inflammatory mechanism might involve the inhibition of AKT/ERK/NF-κB and RORγt/IL-17 pathways.
ALI is characterized by acute inflammatory reaction, infiltration of inflammatory cells, release of exudative secretions, pulmonary cell death, and subsequent parenchyma injury [5, 6, 38]. Growing evidence has shown that neutrophils are essential in initiating and aggravating inflammatory responses and pathological processes [39]. The inhibition of neutrophil recruitment could attenuate LPS-induced ALI by reducing the production of ROS and the secretion of pro-inflammatory cytokines [40]. Moreover, macrophages are also crucial in immune reactions and inflammatory processes in the acute phase of ALI mediated by attenuating neutrophil recruitment and reducing pro-inflammatory mediators in the lungs [41]. Based on the histopathological findings of the current study, pretreatment with esculetin significantly attenuated pulmonary parenchyma injury and inhibited neutrophil and macrophage infiltration and accumulation in the lungs. In addition, pro-inflammatory cytokines (TNF-α, IL-1β, and IL-6) are secreted from active pulmonary and immune cells and are important in eliciting the inflammatory cascade in ALI, including inflammatory cell infiltration, histopathological changes, and severity of injury [17, 42]. Consistent with the previous literature, our results showed that esculetin has anti-inflammatory properties and pretreatment with esculetin significantly reduces the release and production of pro-inflammatory cytokines in LPS-induced ALI.
Accumulating evidence has shown that NF-κB, a crucial transcription factor of inflammation, plays a key role in the development and pathogenesis of ALI [15, 43]. The phosphorylation and activation of NF-κB contributes to the production of pro-inflammatory cytokines, such as TNF-α, IL-1β, and IL-6 [16, 22]. In this study, we found that pretreatment with esculetin obviously reduced the phosphorylation of NF-κB induced by LPS. Moreover, the MAPK protein family plays a key role in inducing the activation of NF-κB and the secretion of pro-inflammatory mediators, leading to inflammation and lung damage in ALI [18, 44]. The ERK, one of the MAPKs, is involved in various cellular processes, including oxidative stress, survival, apoptosis, and inflammatory process [45]. A previous study has shown that ERK signaling contributes to TNF-α production and plays an important role in ALI, whereas the inhibition of ERK provides protective effects against pulmonary inflammatory diseases [46]. Furthermore, a recent study has shown that the activation of the NF-κB pathway that is dependent on ERK can contribute in upregulating the gene of the pro-inflammatory cytokine [20]. In our study, pretreatment with esculetin 30 min prior to the administration of LPS can effectively attenuate the phosphorylation of ERK and NF-κB in the lung tissues, which indicates that esculetin suppresses the ERK and NF-κB activity, leading to the downregulation of pro-inflammatory cytokines. Taken together, our results indicated that pretreatment with esculetin reduces the secretion and production of pro-inflammatory cytokines via the inhibition of the ERK/NF-κB pathway.
AKT, an important signaling pathway involved in various cellular processes, is crucial in cell survival, proliferation, and inflammatory responses against extracellular stimuli [21, 47]. Moreover, recent studies have revealed that the inhibition of the AKT signaling ameliorated LPS-induced ALI by downregulating the NF-κB activity and reducing the production of ROS and pro-inflammatory cytokines [22, 48]. In this study, pretreatment with esculetin significantly reduced the phosphorylation of AKT in the lung tissues. Our results indicated that the protective activity of esculetin might involve the suppression of the phosphorylation of AKT and the subsequent NF-κB pathway.
IL-17, a pro-inflammatory cytokine produced mainly by Th17, plays an essential role in the recruitment of neutrophils and immune responses against extracellular infection [23, 49]. Previous studies have also shown that IL-17 facilitates neutrophil recruitment and accumulation by upregulating the expression of chemokines in LPS-induced ALI [23, 50]. In the current study, we found that IL-17 was significantly expressed in the lungs of the LPS group via immunohistological staining; meanwhile, pretreatment with esculetin substantially reduced the expression of IL-17 in the lung tissues. Recent studies have also shown that neutralizing IL-17 with antibody could attenuate the severity of LPS-induced ALI by the downregulation of pro-inflammatory cytokines [30, 31]. To understand the detailed mechanism of the protective effects of esculetin, we further examined the expression of RORγt, one of the most important nuclear transcription factors in the differentiation of Th17 cells [51]. Growing evidence has demonstrated that RORγt-dependent IL-17A pathway is crucial for pathogenesis of intestinal and pulmonary inflammation [52, 53]. A previous study had shown that the level of IL-17 was significantly elevated and the degree of neutrophilic pulmonary inflammation was also enhanced following mycobacteria infection in RORγt-overexpressing mice [54]. Moreover, a recent study found that RORγt inverse agonist could reduce the expression of IL-17 and diminish the neutrophil infiltration in the lung in asthmatic mice model [55]. In the current study, the expression of RORγt in the LPS group was increased; meanwhile, pretreatment with esculetin significantly reduced the expression of RORγt in the lung tissues. Taken together, our data indicated that pretreatment with esculetin protects against LPS-induced ALI partly via the RORγt/IL-17 pathway.
In addition, a previous study has indicated that the AKT signaling pathway could enhance the nuclear translocation of RORγt and facilitate the differentiation of Th17 cells [56]. Recent studies have also shown that IL-23 facilitates the differentiation of Th17 cells and the IL-23/IL-17 axis plays a critical role in the pathogenesis of acute lung injury [57, 58]. Furthermore, another study has demonstrated that treatment with anti-IL-23 antibody could markedly attenuate airway hyperresponsiveness and pulmonary inflammatory cell infiltration via IL-17 pathway [59]. In our study, pretreatment with esculetin significantly reduced the level of IL-23, which indicated that esculetin might inhibit IL-23/IL-17 axis in LPS-induced ALI model. However, there are potential limitations for our study. Administration of esculetin 30 min before LPS challenge was chosen for the present study. It is unknown whether esculetin posttreatment has beneficial effects in LPS-induced ALI. To make clear this concern, we would add posttreatment experimental design and evaluate the application of esculetin for the treatment of ALI in our future studies.
In conclusion, esculetin has protective effects against LPS-induced ALI in mice by attenuating inflammatory immune cell infiltration and reducing the production of pro-inflammatory cytokines. The anti-inflammatory mechanism of esculetin might involve the inhibition of the AKT/ERK/NF-κB and RORγt/IL-17 pathways (Fig. 8). Therefore, esculetin may be a therapeutic agent for ALI. In the future, comprehensive studies must be conducted to validate the clinical applications of esculetin.
Schematic summary for the protective and anti-inflammatory effects of esculetin on LPS-induced acute lung injury in mice. Esculetin pretreatment effectively protects against LPS-induced acute lung injury by reducing inflammatory responses via the inhibition of the AKT/ERK/NF-κB and RORγt/IL-17 pathways.
References
Mokra, D., and P. Kosutova. 2015. Biomarkers in acute lung injury. Respiratory Physiology & Neurobiology 209: 52–58.
Bellani, G., J.G. Laffey, T. Pham, E. Fan, L. Brochard, A. Esteban, L. Gattinoni, et al. 2016. Epidemiology, patterns of care, and mortality for patients with acute respiratory distress syndrome in intensive care units in 50 countries. JAMA 315 (8): 788–800.
Chignard, M., and V. Balloy. 2000. Neutrophil recruitment and increased permeability during acute lung injury induced by lipopolysaccharide. American Journal of Physiology: Lung Cellular and Molecular Physiology 279 (6): L1083–L1090.
Goodman, R.B., J. Pugin, J.S. Lee, and M.A. Matthay. 2003. Cytokine-mediated inflammation in acute lung injury. Cytokine and Growth Factor Reviews 14 (6): 523–535.
Chopra, M., J. S. Reuben, and A. C. Sharma. 2009. Acute lung injury: Apoptosis and signaling mechanisms. Experimental Biology and Medicine (Maywood, N.J.) 234 (4):361-371.
Wen, Z., L. Fan, Y. Li, Z. Zou, M.J. Scott, G. Xiao, S. Li, et al. 2014. Neutrophils counteract autophagy-mediated anti-inflammatory mechanisms in alveolar macrophage: Role in posthemorrhagic shock acute lung inflammation. Journal of Immunology 193 (9): 4623–4633.
Su, X., L. Wang, Y. Song, and C. Bai. 2004. Inhibition of inflammatory responses by ambroxol, a mucolytic agent, in a murine model of acute lung injury induced by lipopolysaccharide. Intensive Care Medicine 30 (1): 133–140.
Deal, E.N., J.M. Hollands, G.E. Schramm, and S.T. Micek. 2008. Role of corticosteroids in the management of acute respiratory distress syndrome. Clinical Therapeutics 30 (5): 787–799.
Zhang, Y., J. Wu, S. Ying, G. Chen, B. Wu, T. Xu, Z. Liu, et al. 2016. Discovery of new MD2 inhibitor from chalcone derivatives with anti-inflammatory effects in LPS-induced acute lung injury. Scientific Reports 6: 25130.
Rossol, M., H. Heine, U. Meusch, D. Quandt, C. Klein, M.J. Sweet, and S. Hauschildt. 2011. LPS-induced cytokine production in human monocytes and macrophages. CRC Critical Reviews in Immunology 31 (5): 379–446.
Bhattacharyya, J., S. Biswas, and A.G. Datta. 2004. Mode of action of endotoxin: Role of free radicals and antioxidants. Current Medicinal Chemistry 11 (3): 359–368.
Rubenfeld, G.D., E. Caldwell, E. Peabody, J. Weaver, D.P. Martin, M. Neff, E.J. Stern, and L.D. Hudson. 2005. Incidence and outcomes of acute lung injury. New England Journal of Medicine 353 (16): 1685–1693.
Hayden, M.S., and S. Ghosh. 2008. Shared principles in NF-kappaB signaling. Cell 132 (3): 344–362.
Everhart, M.B., W. Han, T.P. Sherrill, M. Arutiunov, V.V. Polosukhin, J.R. Burke, R.T. Sadikot, J.W. Christman, F.E. Yull, and T.S. Blackwell. 2006. Duration and intensity of NF-kappaB activity determine the severity of endotoxin-induced acute lung injury. Journal of Immunology 176 (8): 4995–5005.
Chen, Z., X. Zhang, X. Chu, X. Zhang, K. Song, Y. Jiang, L. Yu, and X. Deng. 2010. Preventive effects of valnemulin on lipopolysaccharide-induced acute lung injury in mice. Inflammation 33 (5): 306–314.
Lv, H., Z. Yu, Y. Zheng, L. Wang, X. Qin, G. Cheng, and X. Ci. 2016. Isovitexin exerts anti-inflammatory and anti-oxidant activities on lipopolysaccharide-induced acute lung injury by inhibiting MAPK and NF-kappaB and activating HO-1/Nrf2 pathways. International Journal of Biological Sciences 12 (1): 72–86.
Wu, H., Y. Yang, S. Guo, J. Yang, K. Jiang, G. Zhao, C. Qiu, and G. Deng. 2017. Nuciferine ameliorates inflammatory responses by inhibiting the TLR4-mediated pathway in lipopolysaccharide-induced acute lung injury. Frontiers in Pharmacology 8: 939.
Hommes, D.W., M.P. Peppelenbosch, and S.J. van Deventer. 2003. Mitogen activated protein (MAP) kinase signal transduction pathways and novel anti-inflammatory targets. Gut 52 (1): 144–151.
Huang, W.C., C.L. Lai, Y.T. Liang, H.C. Hung, H.C. Liu, and C.J. Liou. 2016. Phloretin attenuates LPS-induced acute lung injury in mice via modulation of the NF-kappaB and MAPK pathways. International Immunopharmacology 40: 98–105.
Santos, Lamd, G.B. Rodrigues, F.V.B. Mota, M.E.R. Franca, K.P. de Souza Barbosa, W.H. Oliveira, S.W.S. Rocha, et al. 2018. New thiazolidinedione LPSF/GQ-2 inhibits NFkappaB and MAPK activation in LPS-induced acute lung inflammation. International Immunopharmacology 57: 91–101.
Hyam, S.R., I.A. Lee, W. Gu, K.A. Kim, J.J. Jeong, S.E. Jang, M.J. Han, and D.H. Kim. 2013. Arctigenin ameliorates inflammation in vitro and in vivo by inhibiting the PI3K/AKT pathway and polarizing M1 macrophages to M2-like macrophages. European Journal of Pharmacology 708 (1–3): 21–29.
Jiang, K., S. Guo, C. Yang, J. Yang, Y. Chen, A. Shaukat, G. Zhao, H. Wu, and G. Deng. 2018. Barbaloin protects against lipopolysaccharide (LPS)-induced acute lung injury by inhibiting the ROS-mediated PI3K/AKT/NF-kappaB pathway. International Immunopharmacology 64: 140–150.
Rudner, X.L., K.I. Happel, E.A. Young, and J.E. Shellito. 2007. Interleukin-23 (IL-23)-IL-17 cytokine axis in murine Pneumocystis carinii infection. Infection and Immunity 75 (6): 3055–3061.
Cua, D.J., and C.M. Tato. 2010. Innate IL-17-producing cells: The sentinels of the immune system. Nature Reviews: Immunology 10 (7): 479–489.
Ye, P., P.B. Garvey, P. Zhang, S. Nelson, G. Bagby, W.R. Summer, P. Schwarzenberger, J.E. Shellito, and J.K. Kolls. 2001. Interleukin-17 and lung host defense against Klebsiella pneumoniae infection. American Journal of Respiratory Cell and Molecular Biology 25 (3): 335–340.
Pichavant, M., S. Goya, E.H. Meyer, R.A. Johnston, H.Y. Kim, P. Matangkasombut, M. Zhu, Y. Iwakura, P.B. Savage, R. DeKruyff, S.A. Shore, and D.T. Umetsu. 2008. Ozone exposure in a mouse model induces airway hyperreactivity that requires the presence of natural killer T cells and IL-17. Journal of Experimental Medicine 205 (2): 385–393.
Holloway, T.L., and M.G. Schwacha. 2012. The Th-17 response and its potential role in post-injury pulmonary complications. International Journal of Burns and Trauma 2 (1): 11–17.
Kaur, M., S. Reynolds, L.J. Smyth, K. Simpson, S. Hall, and D. Singh. 2014. The effects of corticosteroids on cytokine production from asthma lung lymphocytes. International Immunopharmacology 23 (2): 581–584.
Sakaguchi, R., S. Chikuma, T. Shichita, R. Morita, T. Sekiya, W. Ouyang, T. Ueda, H. Seki, H. Morisaki, and A. Yoshimura. 2016. Innate-like function of memory Th17 cells for enhancing endotoxin-induced acute lung inflammation through IL-22. International Immunology 28 (5): 233–243.
Ding, Q., G.Q. Liu, Y.Y. Zeng, J.J. Zhu, Z.Y. Liu, X. Zhang, and J.A. Huang. 2017. Role of IL-17 in LPS-induced acute lung injury: An in vivo study. Oncotarget 8 (55): 93704–93711.
Righetti, R.F., T.M. Dos Santos, L.D.N. Camargo, Aristoteles Lrcrb, S. Fukuzaki, F.C.R. de Souza, F.P.R. Santana, et al. 2018. Protective effects of anti-IL17 on acute lung injury induced by LPS in mice. Frontiers in Pharmacology 9: 1021.
Masamoto, Y., H. Ando, Y. Murata, Y. Shimoishi, M. Tada, and K. Takahata. 2003. Mushroom tyrosinase inhibitory activity of esculetin isolated from seeds of Euphorbia lathyris L. Bioscience, Biotechnology, and Biochemistry 67 (3): 631–634.
Wang, C., A. Pei, J. Chen, H. Yu, M.L. Sun, C.F. Liu, and X. Xu. 2012. A natural coumarin derivative esculetin offers neuroprotection on cerebral ischemia/reperfusion injury in mice. Journal of Neurochemistry 121 (6): 1007–1013.
Hongyan, L. 2016. Esculetin attenuates Th2 and Th17 responses in an ovalbumin-induced asthmatic mouse model. Inflammation 39 (2): 735–743.
Han, M.H., C. Park, D.S. Lee, S.H. Hong, I.W. Choi, G.Y. Kim, S.H. Choi, J.H. Shim, J.I. Chae, Y.H. Yoo, and Y.H. Choi. 2017. Cytoprotective effects of esculetin against oxidative stress are associated with the upregulation of Nrf2-mediated NQO1 expression via the activation of the ERK pathway. International Journal of Molecular Medicine 39 (2): 380–386.
Chen, T., Q. Guo, H. Wang, H. Zhang, C. Wang, P. Zhang, S. Meng, Y. Li, H. Ji, and T. Yan. 2015. Effects of esculetin on lipopolysaccharide (LPS)-induced acute lung injury via regulation of RhoA/rho kinase/NF-small ka, CyrillicB pathways in vivo and in vitro. Free Radical Research 49 (12): 1459–1468.
Liu, F.C., H.P. Yu, C.Y. Lin, A.O. Elzoghby, T.L. Hwang, and J.Y. Fang. 2018. Use of cilomilast-loaded phosphatiosomes to suppress neutrophilic inflammation for attenuating acute lung injury: The effect of nanovesicular surface charge. Journal of Nanobiotechnology 16 (1): 35.
Driver, C. 2012. Pneumonia part 1: Pathology, presentation and prevention. British Journal of Nursing 21 (2): 103–106.
Grommes, J., and O. Soehnlein. 2011. Contribution of neutrophils to acute lung injury. Molecular Medicine 17 (3–4): 293–307.
Lee, J.M., C.D. Yeo, H.Y. Lee, C.K. Rhee, I.K. Kim, D.G. Lee, S.H. Lee, and J.W. Kim. 2017. Inhibition of neutrophil elastase contributes to attenuation of lipopolysaccharide-induced acute lung injury during neutropenia recovery in mice. Journal of Anesthesia 31 (3): 397–404.
Huang, X., H. Xiu, S. Zhang, and G. Zhang. 2018. The role of macrophages in the pathogenesis of ALI/ARDS. Mediators of Inflammation 2018: 1264913.
Li, Y.C., C.H. Yeh, M.L. Yang, and Y.H. Kuan. 2012. Luteolin suppresses inflammatory mediator expression by blocking the Akt/NFkappaB pathway in acute lung injury induced by lipopolysaccharide in mice. Evidence-based Complementary and Alternative Medicine 2012: 383608.
Feng, G., Z.Y. Jiang, B. Sun, J. Fu, and T.Z. Li. 2016. Fisetin alleviates lipopolysaccharide-induced acute lung injury via TLR4-mediated NF-kappaB signaling pathway in rats. Inflammation 39 (1): 148–157.
Guo, S., K. Jiang, H. Wu, C. Yang, Y. Yang, J. Yang, G. Zhao, and G. Deng. 2018. Magnoflorine ameliorates lipopolysaccharide-induced acute lung injury via suppressing NF-kappaB and MAPK activation. Frontiers in Pharmacology 9: 982.
Yu, S.M., and S.J. Kim. 2015. The thymoquinone-induced production of reactive oxygen species promotes dedifferentiation through the ERK pathway and inflammation through the p38 and PI3K pathways in rabbit articular chondrocytes. International Journal of Molecular Medicine 35 (2): 325–332.
Schuh, K., and A. Pahl. 2009. Inhibition of the MAP kinase ERK protects from lipopolysaccharide-induced lung injury. Biochemical Pharmacology 77 (12): 1827–1834.
Cianciulli, A., R. Calvello, C. Porro, T. Trotta, R. Salvatore, and M.A. Panaro. 2016. PI3k/Akt signalling pathway plays a crucial role in the anti-inflammatory effects of curcumin in LPS-activated microglia. International Immunopharmacology 36: 282–290.
Zhao, M., C. Li, F. Shen, M. Wang, N. Jia, and C. Wang. 2017. Naringenin ameliorates LPS-induced acute lung injury through its anti-oxidative and anti-inflammatory activity and by inhibition of the PI3K/AKT pathway. Experimental and Therapeutic Medicine 14 (3): 2228–2234.
Schwarzenberger, P., W. Huang, P. Ye, P. Oliver, M. Manuel, Z. Zhang, G. Bagby, S. Nelson, and J.K. Kolls. 2000. Requirement of endogenous stem cell factor and granulocyte-colony-stimulating factor for IL-17-mediated granulopoiesis. Journal of Immunology 164 (9): 4783–4789.
Gouda, M.M., and Y.P. Bhandary. 2019. Acute lung injury: IL-17A-mediated inflammatory pathway and its regulation by curcumin. Inflammation 42 (4): 1160–1169.
Ivanov, II, B. S. McKenzie, L. Zhou, C. E. Tadokoro, A. Lepelley, J. J. Lafaille, D. J. Cua, and D. R. Littman. 2006. The orphan nuclear receptor RORgammat directs the differentiation program of proinflammatory IL-17+ T helper cells. Cell 126 (6):1121–1133.
Kanai, T., Y. Mikami, T. Sujino, T. Hisamatsu, and T. Hibi. 2012. RORgammat-dependent IL-17A-producing cells in the pathogenesis of intestinal inflammation. Mucosal Immunology 5 (3): 240–247.
Tsai, H.C., S. Velichko, L.Y. Hung, and R. Wu. 2013. IL-17A and Th17 cells in lung inflammation: An update on the role of Th17 cell differentiation and IL-17R signaling in host defense against infection. Clinical & Developmental Immunology 2013: 267971.
Matsuyama, M., Y. Ishii, H. Sakurai, S. Ano, Y. Morishima, K. Yoh, S. Takahashi, K. Ogawa, and N. Hizawa. 2016. Overexpression of RORgammat enhances pulmonary inflammation after infection with mycobacterium avium. PLoS One 11 (1): e0147064.
Whitehead, G.S., H.S. Kang, S.Y. Thomas, A. Medvedev, T.P. Karcz, G. Izumi, K. Nakano, et al. 2019. Therapeutic suppression of pulmonary neutrophilia and allergic airway hyperresponsiveness by a RORgammat inverse agonist. JCI Insight 4 (14): e125528.
Nagai, S., Y. Kurebayashi, and S. Koyasu. 2013. Role of PI3K/Akt and mTOR complexes in Th17 cell differentiation. Annals of the New York Academy of Sciences 1280: 30–34.
Cauvi, D.M., M.R. Williams, J.A. Bermudez, G. Armijo, and A. De Maio. 2014. Elevated expression of IL-23/IL-17 pathway-related mediators correlates with exacerbation of pulmonary inflammation during polymicrobial sepsis. Shock 42 (3): 246–255.
Yan, B., F. Chen, L. Xu, J. Xing, and X. Wang. 2017. HMGB1-TLR4-IL23-IL17A axis promotes paraquat-induced acute lung injury by mediating neutrophil infiltration in mice. Scientific Reports 7 (1): 597.
Cheng, S., H. Chen, A. Wang, H. Bunjhoo, Y. Cao, J. Xie, Y. Xu, and W. Xiong. 2016. Blockade of IL-23 ameliorates allergic lung inflammation via decreasing the infiltration of Tc17 cells. Archives of Medical Science 12 (6): 1362–1369.
Funding
This work was supported by grants from the Ministry of Science and Technology (MOST108-2314-B-182A-059-MY2) and Chang Gung Memorial Hospital (CMRPG3G1601-2) to Fu-Chao Liu and the Ministry of Science and Technology (MOST105-2314-B-182A-012-MY3) and Chang Gung Memorial Hospital (CMRPG3H0811-3, CMRPG3H1191-3) to Huang-Ping Yu.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that there is no conflict of interests regarding the publication of this paper.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lee, HC., Liu, FC., Tsai, CN. et al. Esculetin Ameliorates Lipopolysaccharide-Induced Acute Lung Injury in Mice Via Modulation of the AKT/ERK/NF-κB and RORγt/IL-17 Pathways. Inflammation 43, 962–974 (2020). https://doi.org/10.1007/s10753-020-01182-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10753-020-01182-4