Abstract
This research aims to identify the accessibility of the entire population, especially the slum population to existing healthcare facilities (HCF) as well as the slum neighborhoods having low geographic accessibility, and finally, to provide an analytical model for the people living in areas that are outside the coverage range of existing healthcare facilities (HCF) across the study area. Spatial data has been collected and used based on the road network, elevation, location of HCF, municipal boundary, slum point, and satellite images from various sources. Also, non-spatial data such as socioeconomic variables are collected from questionnaires survey within a particular period. The spatial analysis tool like as near, network analysis, and predictive analysis in the ArcGIS platform was used to examine geographic accessibility. The results of the spatial analysis show that the distribution of public healthcare facility centers in the study area has not been uniformly distributed. Across 84% of areas in the study area have sound spatial accessibility with traveling time coverage is about 12 min. However, 16% of areas have a traveling time of 12 to 30 min under low accessibility with existing slum neighborhoods. Therefore, the low spatial accessibility areas are demanding new healthcare facilities in the study area. The Analytical Hierarchy Process (AHP) is employed to find the most optimal and efficient locational suitability for building new healthcare facility centers. The finding of AHP analysis for site suitability of healthcare facilities revealed five major classes as most suitable (2%), suitable (5%), moderate (35%), poor (54%), and very poor (4%) in the study area. Moreover, the realistic framework of this study helps to measure geographic accessibility and suitability in any geographical area.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In the developing countries, geographic access to healthcare facilities is one of the key challenges in ensuring healthy lives and promoting wellbeing for all at all ages in achieving the 3rd sustainable development goal due to distance to facilities, ease of travel cost and travel time (Reshadat et al., 2018; Shah et al., 2016; Subal et al., 2021). Geographical or spatial accessibility refers to the physical access of people to a location e.g., healthcare facility (El Karim & Awawdeh, 2020; Kim et al., 2018; McGrail & Humphreys, 2014). Spatial accessibility is the combination of availability and accessibility dimensions as stated by Penchansky and Thomas in 1981 can be measured by a time–space framework such as vehicular travel time, distance and Euclidean distance is influenced by the topology and structure of the road network for identifying deprived areas and people (Lawal & Anyiam, 2019; Mishra et al., 2021; Shaw & Sahoo, 2020). Geographic access to healthcare facilities is a multidimensional process and can be described by five key dimensions: availability, accessibility, accommodation, affordability, and acceptability, more explicitly describe as the supply of healthcare services with physical proximity (travel distance and time) on a particular geographical location at a reasonable price concerning the population in need (Liu et al., 2022; Shaw & Sahoo, 2020; Tao et al., 2020). The location of healthcare centers near homes can lead to more recurrent visits resulting in better family health outcomes (Dos Anjos Luis & Cabral, 2016; Parry et al., 2018; Vadrevu & Kanjilal, 2016).
‘Health for all’ doctrine indicates that everyone should have access to appropriate healthcare facilities in a time–space framework, acceptable and affordable way (Lawal & Anyiam, 2019; Basu et al., 2018). Affordable and accessible healthcare can reduce potential health risk and the rate of hospitalization. Dependency and a higher rate of admissions to hospitals in an area may provide evidence of the inaccessibility of people to primary healthcare centers (Shah et al., 2016; Shaw & Sahoo, 2020; Shen et al., 2020). The steady expansion of urban areas with population growth requires regular assessment of the accessibility of healthcare facilities across urban areas (Dutta et al., 2021b; Yin et al., 2018) because limited access to facilities (Lawal & Anyiam, 2019) may cause an epidemic outburst such as Covid-19 virus.
In developing countries, locations of primary healthcare are generally decided by local government officers often made on political or pragmatic considerations, and as a result, far from optimal locations (Karim & Awawdeh, 2020; Sedenu et al., 2016). There is a close relationship between infant as well as maternal mortality and distance to healthcare facilities as PHCs act as the distributor of polio and another major vaccine for infants and pregnant women (Rahman and Smith, 2000). Lack of accessibility to healthcare facility as the result of low public investment in health sectors encourage entrepreneur of private healthcare facility forcing people to access these facilities, which often lead to higher healthcare expenditures, health shocks and medical poverty trap (Basu et al., 2018; Shi et al., 2022). Private facilities do not provide affordable healthcare facilities to economically weaker sections and lower-income deprived groups (Basu et al., 2018). Therefore, the allocation of public healthcare facilities should be based on accessibility and affordability gaps as per guidelines of the National Health Policy (NHP)- 2002 (Basu et al., 2018) and the National Urban Health Mission (NUHM)- 2013 as to develop smart and healthy city as well as providing affordable and essential primary health care services to the urban poor so that needs of the healthcare are met (Abdelkarim, 2019; Abdullahi & Pradhan, 2012).
The steady population growth with resulting urbanization is high in an established small town than in metropolitan or million-plus cities (Alabi, 2011; Lawal & Anyiam, 2019). Slums are now developed in small towns than in metropolitan cities due to in-migration from surrounding rural counterparts into the vacant or unprivileged areas in the town. The haphazard development of slums and low-income communities in the study area demanded accessible and affordable healthcare services. But the earlier study (Dutta et al., 2021b) shows that the healthcare facility centers have not been properly distributed. As per the NFHS-5 report (2019–20), antenatal care visits and maternal care are much lower in the Paschim Medinipur district in West Bengal. The study area of Midnapore municipality is the eyes of the Paschim Medinipur district. Only the tertiary categories of healthcare services are available where most of the specialized doctors and facilities attracted huge people from rural and slum areas. The rapid expansion of the small town justifies the rational evaluation of the spatial distribution pattern of the existing healthcare center with the accessibility to people and to find the accessibility gap by establishing a new healthcare center. In this regard, the spatial accessibility model (SAM) is a useful geospatial analytical technique that incorporated geospatial models with GIS, GPS, and remote sensing algorithms to determine the best location for a healthcare facility in the urban area. The hypothesis was whether there is a significant difference between accessibility and location of existing healthcare facility centers or adequate for providing effective healthcare services. Based on the selected hypothesis, a set of objectives were chosen for the present study (1) Identify the deprived slum neighborhoods from the existing healthcare facilities (2) Propose a suitable site for new healthcare facilities that covering deprived slum neighborhoods.
Literature review
Using various methodological options of geographic information systems (GIS), researchers can easily measure geographic accessibility (Shaw & Sahoo, 2020; Zhang et al., 2021). Despite medical facilities as well as economic development, mortality rates are still high due to low geographic accessibility in India (Gao et al., 2021; Huerta Munoz & Källestål, 2012; Lawal & Anyiam, 2019; Mansour, 2016; Shaw & Sahoo, 2020; Shaw & Sahoo, 2020; Waithaka, 2015). Many studies have focused on areas of geographic inaccessibility (Lawal & Anyiam, 2019; Wielebski & Medyńska-gulij, 2018), hospitals and doctor shortages, mortality risk, etc. (Shaw & Sahoo, 2020). Numerous studies have tried to show that healthcare facilities and services are inequitably distributed to meet the needs of the people (Ajala et al., 2017; Lawal & Anyiam, 2019; Kim et al., 2018; Bauer et al., 2020; Gao et al., 2021; Rekha et al., 2020; Shen et al., 2020; Shi et al., 2022; Song et al., 2018; Subal et al., 2021; Zhang et al., 2021). These studies also shows that every person has an equal chance of being able to access healthcare services. Through information about the demand (Polo et al., 2015; Rekha et al., 2017; Sedenu et al., 2016; Shah et al., 2016) for healthcare services and the availability of these services, urban authority can improve their healthcare infrastructure and reduce healthcare inequalities (Kim et al., 2018; Lawal & Anyiam, 2019; Abdelkarim, 2019; Basu et al., 2018; Bauer et al., 2020; Dutta et al., 2021b; El Karim & Awawdeh, 2020; Gao et al., 2021; Maleki Rastaghi et al., 2018; Miç et al., 2019; Mishra et al., 2021; Parry et al., 2018; Rekha et al., 2017; Shah et al., 2016; Shen et al., 2020; Shi et al., 2022; Song et al., 2018; Subal et al., 2021; Vadrevu & Kanjilal, 2016; Zhang et al., 2021; Zhang et al., 2016). By increasing healthcare facilities and services, poor people are more facilitating socially is expected to improve their quality of life (Moisi et al., 2010; Albert & Assad, 2019; Dutta et al., 2021a, b; McGrail & Humphreys, 2014). For achieving sustainable development goals, the government healthcare policies need to be more generalized to promote health status and socioeconomic development because healthcare facilities and services are uneven due to socioeconomic conditions from the grass-root level in developing countries (Mansour, 2016). Developing countries should improve their healthcare services (Asare-akuffo et al., 2019; Hosseini et al., 2021; Miç et al., 2019; Mishra et al., 2021; Shaw & Sahoo, 2020) due to very high population with low GDP, limited and uneven distribution of healthcare facilities (HCF), and infrastructure also, especially in India (Assad, 2019). Due to the rapid growth of urban and suburban areas through continuous migration, demand for healthcare facilities (HCF) is increasing simultaneously (Al-Taiar et al., 2010; Delamater et al., 2012; Lawal & Anyiam, 2019; Maleki Rastaghi et al., 2018; Shah et al., 2016; Waithaka, 2015; W. Zhang et al., 2016) and for that reason raise the building of new healthcare facilities (HCF) is considered as one of the most important steps to easily accessible, proficient, and the affordable healthcare system by poor people to achieving the Millennium Development Goals of every government (Lawal & Anyiam, 2019; Ajala et al., 2017). On 1st May 2013, the Indian government launched the National Urban Health Mission (NUHM) covering all cities and towns with a population of 50,000 and above (according to the 2011 census), which is focused on providing primary healthcare services to the urban poor mainly slum dwellers (Dutta et al., 2021b). India’s healthcare system is composed of primary, secondary, and tertiary public healthcare facilities. Despite healthcare facilities and services, during health shocks i.e., acute abdominal conditions, accidents especially in surgical conditions have not been available in primary and most of the time in secondary healthcare facilities. As a result, they are forced for travelling to tertiary healthcare facilities, and then mortality risk will be increased at a considerable level (Kim et al., 2018; Miç et al., 2019). To ensure public health facilities, the local government should also be involved in the design, rational allocation, and construction of healthcare infrastructures with the compliance of national and state health policies (Moisi et al., 2010). The rapid growth of cities and towns in India has raised concerns in the healthcare system regarding the distribution of healthcare services to the growing population (Lawal & Anyiam, 2019; Danjuma, 2015). Aside from this, the lack of proper education, human resources, and awareness, maintaining healthcare facilities by continuing financial support are also important factors that affect the efficient healthcare system (Danjuma, 2015; Mohammadi et al., 2018; Rekha et al., 2017; Zhang et al., 2016). Moreover, the government needs to plan for the developing infrastructures of existing healthcare facilities and set up new healthcare facilities which have not been planned in the last few years. For instances, the healthcare system was collapsed during the times of the COVID-19 pandemic (Kang et al., 2020; Liu et al., 2022). Therefore, the proper allocation of healthcare facilities within a proper location is an important aspect of the rational distribution of healthcare services. In this regard, geospatial analysis of healthcare facilities and services will be more beneficial to the people as well as urban planners and authorities.
Location of the study area
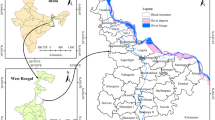
The Midnapore municipality of Paschim Medinipur district continues to fulfill responsibilities as a district headquarters in West Bengal with long historical purposes (http://midnaporemunicipality.com; Dutta et al., 2021b). The study area (Fig. 1) is located on the southwestern part of Paschim Medinipur and the laterite track of the Kasai River bank with slight roughness varies in elevation ranges from 23 to 60 m from mean sea level (Dutta et al., 2021b). The Midnapore municipality contains 25 municipal wards and 156 notified slums with 4 hospitals and 8 primary healthcare facilities (Table 1) (Dutta et al., 2021b; http://midnaporemunicipality.com). The class-I town, as well as Midnapore municipality, is a fast-growing city (Dutta et al., 2021b) having a 1,68,496 population (as per the 2011 census) with very high population density varies 3000–29,000 per km2 (ward wise) (Dutta et al., 2021b). Census of India, 2011, revealed that the male and female population is 84,977 and 84,287 respectively, while the sex ratio and child sex ratio are 992 and 985 correspondingly along with literates persons are 88.99% whereas male literate 92.52% and female literate 85.44%. In addition, the slum population is 50,943 which is nearly 30.09% of the total population of the town. The addition of haphazard land use such as unplanned residential, and commercial areas, and uneven distribution of governmental facilities is a barrier to equal distribution. Also, due to being the district headquarters, huge daily migrant people are gathered for taking facilities, especially health facilities over the district area (Dutta et al., 2021b) which reduces mobility and accessibility of vehicles. We targeted the slum neighborhoods of Midnapore municipality because, in the study area, public health facilities are more needed for the urban poor (Dutta et al., 2021a, b). The drivers for the demand of healthcare facility are due to low monthly income with multidimensional poverty, low health facility ratio with accessibility and mobility, and 52.45% of slum households are sick seasonally as well as 41.85% visiting foregone medical care for chronic illness (Authors survey, 2022).
Materials and methods
Data collection and preparation
The required data for the spatial accessibility analysis were collected from different sources. Data and information on municipal wards, slum neighbourhoods, boundaries, population were collected from Midnapore municipality as a base map (http://midnaporemunicipality.com). Coordinates points of the 12 public healthcare facilities (Table 1) were collected by using the GPS device. The datasets as well as collected municipal data and coordinates points of HCF were digitized and projected to GCS WGS-1984 coordinate system and forwarded to create a GIS database. For computing the multidimensional poverty index (MPI), a structured questionaries survey was conducted from 1st October to 24th December, 2019 over the notified 156 slum areas using simple random sampling. The network datasets of the study area were downloaded from the open street map (OSM). The OSM datasets were extracted by open street map add-in tools in ArcGIS 10.4 (https://www.esri.com). The extracted datasets contain road networks, administrative buildings, points of interest, water features, and natural features as spatial attributes. The natural features, water features, points of interest, and administrative buildings are considered as obstacles that reduces the accessibility and mobility to direct access to healthcare facilities (Lawal & Anyiam, 2019). The SRTM-DEM and Landsat 8 OLI data (row-139, path – 44 and date – 27/02/2021) with both are 30 m resolution is archived from the USGS website (https:// earthexplorer.usgs.gov) for computation of a degree of slope and land use and landcover accordingly. The datasets were projected into the same coordinate system and computed the percent of a slope using the methods of Wang and Liu, 2006. All the datasets are arranged into the framework of the present study and create a GIS database for further analysis and methodological development (Fig. 2).
Methods
The present study is an integration of raster and vector datasets with statistical and model-building operations that perform to analysis of accessibility across the study area. The statistical computations were performed using MS Excel v2016 (https://www.microsoft.com). However, the GIS model building and mapping were done using ArcGIS v10.4 (https://www.esri.com), and raster datasets were processed via Erdas Imagine (https://www.hexagongeospatial.com) software. The adopted methodological framework is presented in Fig. 2 with the methods are as follows:
Near
The near analysis algorithm is a geoprocessing tool of the ArcGIS (https://www.esri.com) platform used to compute distance and proximity attributes within two input feature datasets (point, line, polygon) using Euclidean distance (https://www.esri.com). The proximity distance between slum neighborhoods and healthcare facilities (HCF) is user-specified in a measurable unit (meter) (Dutta et al., 2021b). There is a noticeable disadvantage of the tool is that it cannot determine the distance and proximity attribute in a dataset (Assad, 2019). And another one is that when two or more features are located at the same distance, the tool randomly chooses one of them for the nearest feature (https://www.esri.com).
Network analysis
The network analysis in the GIS platform (https://www.esri.com) is performed to determine the most valuable and efficient routes that people can easily and comfortably travel to the nearest facility (Abdelkarim, 2019; El Karim & Awawdeh, 2020; Lawal & Anyiam, 2019; Maleki Rastaghi et al., 2018; Mansour, 2016; Miç et al., 2019; Polo et al., 2015; U et al., 2018; Waithaka, 2015). The two input datasets, for example, one as a facility and another one as a demand point are required to create a network dataset (El Karim & Awawdeh, 2020; Polo et al., 2015) for solving the different aspects of routing problems of distinct categories such as service area, closest facility, shortest path analysis, location-allocation, etc. (https://www.esri.com). In this study, we used service area and location-allocation tools (Openshaw, 1983; Zhang et al., 2016; Zhao et al., 2019) as to enhance the accessibility to healthcare facilities (HCF).
Service area
A service area analysis is a GIS operation (Network analysis tool) (https://www.esri.com) that analyzes how much area facilitating by a facility center in a required time through the accessible ways in a region (Dutta et al., 2021b). Also, a service area is a combining datasets of existing road network, facility centers, and road type (one-way, two-way, etc.), allowing speed, and barriers (traffic jams, natural and cultural barriers) in compliance with the setting of the study area (El Karim & Awawdeh, 2020; Miç et al., 2019). The required traveling time depends on vehicle speed that is controlled by road conditions (quality and efficiency) (Gao et al., 2021; Kim et al., 2018; Målqvist et al., 2010; Moïsi et al., 2010; Shen et al., 2020), local topographical factors, traffic jams, availability of footpaths, etc. and these are considered as the attributes of network layers (El Karim & Awawdeh, 2020). The traveling time calculate through the mathematical equation expressed as:
In Midnapore municipality, most of the roads are one-way, and as a result, in the way, the vehicle's speed is considered as 40 km/hr (Mansour, 2016). The network datasets were configured with the service area tool at different times such as 3, 6, 9, and 12 min respectively. The resulting output of the service area analyzed the efficiency of healthcare facilities across the study area (El Karim & Awawdeh, 2020; Miç et al., 2019).
Location-allocation
A location-allocation algorithm is used to identify the optimum demand location (Mishra et al., 2021; Møller-Jensen, 1998; Vora et al., 2015; Zhao et al., 2019; Zhang et al., 2016; Shaw & Sahoo, 2020; Abdelkarim, 2019; Basu et al., 2018; El Karim & Awawdeh, 2020; Maleki Rastaghi et al., 2018; Miç et al., 2019; Polo et al., 2015; Waithaka, 2015; Zhang et al., 2016). Also, it is employed to reduce or minimize the travel distance, time, and costs, a deficit of facilities, suggest new demand locations, and maximize the coverage capacity of a facility center (Mishra et al., 2021; Zhao et al., 2019). Accessibility between demand site and facilities center, distance has a crucial role in quantification e.g., Euclidean distance, Manhattan distance, network distance, and time distance (Mishra et al., 2021; Polo et al., 2015). Most of the researchers used network distance from those distances, however, the Location allocation model is available in the network analysis extension of the ArcGIS environment (https://www.esri.com). There are four types of locational problem-solving assumptions such as minimize impedance, minimize facilities, maximum coverage, and maximum attendance (El Karim & Awawdeh, 2020; Miç et al., 2019; Mishra et al., 2021; Polo et al., 2015). The uses of the location-allocation model are different aspects but the three main components of this model are supporting road network is the existing road network, the demand side, and the facilities center (Mishra et al., 2021; Vora et al., 2015; Zhao et al., 2019; Polo et al., 2015). Also, in different aspects of locational problem-solving assumptions, the researchers mostly use impedance distances due to improving the quality and easy access of a facility (Polo et al., 2015). A user is willing to travel a maximum acceptable distance to access a particular facility which is the impedance distance of accessibility (Mishra et al., 2021; Zhao et al., 2019). In this study, we employed the location-allocation model to find out the accessible and inaccessible slum neighborhoods to healthcare facilities (HCF) with a set of 3 km impedance distance during health shocks (Shah et al., 2016). Therefore, a location-allocation model is reemployed to validate that whether proposed healthcare facilities (HCF) are in the best appropriate location or not.
Predictive analysis
Predictive analysis is an add-in tool available in the ArcGIS environment which predicts multiple sets of raster data (ESRI, 2014). This tool is also performed to developed complex queries on multiple or single raster bands (Lawal & Anyiam, 2019). The capabilities of this tool are to extract information from raster bands using different queries that take into different obstacles such as building, waterbody, etc. This tool also contains the Speed model, distance from, and time from, these are described are as follows:
Distance from
The distance from tool can finds how far an unknown location is as per area of interest from a known location (e.g., point, line, or polygons) (ESRI, 2014). This finding distance is based on the shortest linear distance as per the set of locations. We used this tool to identify the measuring distance from the road across the study area.
Time from
The time from tool of predictive analysis is used to find the least accumulated travel time from the closest source location or facilities center to each cell of the raster dataset (ESRI, 2014). This tool also finds distance in terms of travel time in a constant velocity using an algorithm of raster calculator. Also, this tool allows a speed model as an input, where multiple effects that can control travel time and speed (ESRI, 2014; Lawal & Anyiam, 2019). We use this tool to identify the accessibility in terms of traveling time from slum neighborhoods to healthcare facilities (HCF) across the study area.
Speed model builder
The speed model is a complex query-based building model available in predictive analysis tools within ArcGIS (ESRI, 2014). This tool supports analyst specified conditions building model which predicts moving or stationary object/events location (Lawal & Anyiam, 2019). The speed model works like proximity analysis over a raster band but objects or events can be specified as constraints to movement and computed travel time in addition to distance to a destination (ESRI, 2014). The specified speed depends on different surfaces and terrain as a conditioning surface created by the speed model (ESRI, 2014). For example, high slopes of terrain affected vehicle speed as well as traffic jams, and road environments affected vehicle speed (Lawal & Anyiam, 2019). Also, the speed model depends on local knowledge and understanding across the area. However, the achievable speed of constraint moving objects to access healthcare facilities ranges from 10 km/hr to 40 km/hr depending on terrain characteristics, road environments, and distance from a road, which is summarized in Table 2. The accommodated scenarios as a condition of speed model using in time from tool to computed traveling time to nearest healthcare facilities.
Results
Evaluation of accessibility efficiency of existing healthcare facilities (HCF)
Catchment area of HCFs and accessibility
Most of the slum neighborhoods are confused to choose the nearest healthcare facilities during an emergency. Naturally, during health shocks, they traveled too much distance which increased the mortality risk of a patient (Lawal & Anyiam, 2019). The application of a vector-based near tool identifies the nearest healthcare facilities to doing the right choice in an emergency (Fig. 3) (Dutta et al., 2021b). The spatial accessibility index was created using the Near_dist attribute field after the GIS operation by the near tool between healthcare facilities (HCF) and slum neighborhoods. However, from Fig. 3, the output map represents the accessibility of each slum neighborhood to healthcare facilities. Most of the slum neighborhoods such as Raja Bazar, sepoy Bazar, Keranitola, and Barabazar (70%) have much better accessibility and about 23% of slum neighborhoods such as station road, bhuniapara, ashoke nagar have moderate accessibility to healthcare facility across the study area. only 8% of total slum neighborhoods are in low accessibility zones such as Gandhi ghat, Kabar danda, tantigeria, and baro astana. They must travel to a single facility or during emergencies to the existing healthcare facilities (Dutta et al., 2021b). Due to the uneven distribution of healthcare facilities (Dutta et al., 2021b), these slums are not facilitated by the existing healthcare facilities.
Spatial accessibility by predictive analysis
The complex query and raster-based proximity analysis tool as the predictive analysis used to find traveling distance and time from healthcare facilities (HCF) to slum neighborhoods across the study area (Lawal & Anyiam, 2019). Distance from tool of predictive analysis deployed for finding the distance from the road to slum neighborhoods as well as every pixel across the study area (Fig. 4). The finding key points from this analysis that the periphery regions of the study area are around ± 400 m and mostly in the northeastern side (ward 1) about 850 m distance from the road network respectively. Most of the slum neighborhoods on the road network are indicated from the output map (Fig. 4) (Dutta et al., 2021b) and the analysis also shows that these are the area which is off the road in speed model building.
However, the speed model builder has created a combination of the road environment, distance from the road network, terrain attributes, and healthcare facilities (HCF)(Lawal & Anyiam, 2019). These using conditions are combined to find travel time from each healthcare facility (HCF) across the study area as well as slum neighborhoods. The obtained results are the accommodation of conditions of the speed model shown in Table 2 (Lawal & Anyiam, 2019). The analysis shows that accessibility to HCF in terms of a travel time maximum of ± 31 min, while the average travel time is around ± 8 min over the study area. Most of the slum neighborhoods and areas under study area have high spatial accessibility except periphery regions such as golapi chak, baishakhi palli, naram pur, bara astana, and rajar purkur, etc. (Fig. 5).
Most of the slum neighborhoods are within a well position to access emergency care. From Fig. 5, average traveling time from the slum neighborhoods to healthcare facility centers ranges between 5 to 11 min. Mainly, the periphery regions of the study area are facing problems during health shocks to access medical care within half an hour. Following Lawal and Anyiam (2019) works, the degree of accessibility as term as traveling time are over 20 min which may increase mortality risk during health shocks (vehicle accident, trauma, gynaecology, etc.). Perhaps it is worse in the real world than the results of the analysis because of huge traffic jams in barabazar, keranitola, panchur chawk, raja bazar, sipoi bazar, LIC more, Midnapore central bus stand, ashokenagar, Midnapore railway station road areas and lacking transport availability (Ambulance) which is not included in this analysis.
The results also identify the characteristics of road environments, cultural and environmental obstacles such as off-roads, administrative buildings, waterways, parks, etc. are the reasons for the worst access to healthcare facilities that produce difficulty in navigation during health shocks. For foregone care, the results find about have too high spatial accessibility in the central part and low pocket accessibility areas are north-eastern (ward 1), southern (Wards 17 and 18), and western part (Wards 24 and 25) of the study area. After computation in the study area, about 84% area has high spatial accessibility, and sixteen percent in very poor to poor accessibility. Moreover, the analysis indicates that most of the HCFs are clustered pattern in the center and distributed northeast to southwest directionally (Dutta et al., 2021b) which hinders their facilities.
Despite this, there are two phenomena firstly, slum neighborhoods are not facilitated easily by healthcare facilities (HCF) because most of the time primary healthcare are not able to treatment during health shocks. Secondly, the questionnaire survey on the study area find that health shock is more responsible for poverty rather than the distance to healthcare facilities. As a result, they are forced and pressurized to get health services from the district medical college & hospital (MMC&H). The rapid increase in demanding population and high population/HCF ratio demand establish new healthcare facility across the study area.
Spatial accessibility through network analysis
Firstly, the service area analysis evaluates geographic accessibility in terms of coverage areas through traveling time from existing healthcare facilities to study areas by road network during health shocks (Fig. 6) (Dutta et al., 2021b). The results of service area analysis show that there are approximately thirty-one slum neighborhoods such as kabar danga, golapi chawk, tantigeria, nibeditapalli, bara astana are not under the coverage area of existing healthcare facilities, these are representing about 19.8% of total slums and sixteen thousand population of total slum population approximately (Fig. 6). And, the other one hundred twenty-five slum neighborhoods (80.2%), as well as thirty-four thousand population of the total slum population, are under the coverage area of existing healthcare facilities accordingly. Also, the results indicate that the uncovered area (around 8 km2 area) traveled over 20 min during an emergency for a health facility. Approximately, twenty-seven slums (around 2.8 km2) such as momin mahalla, pakija baste, surja nagar, berballavpur, narampur under coverage area with 0–3 min travelling time, and, forty slums (around 4.7 km2) jelepara, daspara, dewan nagar are under coverage area of 3- 6 min traveling time, as well as, twenty-eight slums (around 5.2 km2) halugali baste, sekhpura, bhunia para are under coverage area of 6–9 min traveling time and, at last, thirty slums (around 7.3 km2) rajarpukur, station road, jelepara bastee are under coverage areas of 9–12 min traveling time simultaneously (Fig. 6). Most of the slum neighborhoods of the northwestern part and a few of the north-eastern, southwestern, and southern are considering as low accessibility in terms of traveling time during emergencies. The analysis is recommended to add provisional healthcare facilities in deprived healthcare service areas with the help of geospatial analysis.
Secondly, the location-allocation model is used to measure and authenticate the level of accessibility from HCF to slum neighborhoods of Midnapore municipality. The location-allocation model for this study has been set an impedance distance or threshold distance of 3 km during health shocks (Shah et al., 2016). The result (Fig. 7) indicates that catchment areas or slum neighborhoods of existing facilities and distant access from HCFs represent pockets of inaccessibility or deprived health facilities in slum neighborhoods. Most of the slum neighborhood in the central part such as barabazar, nimtala chawk, choto bazar, berballavpur, raja bazar, burdge town, keranitola, narampur of the study area have sound spatial accessibility through the road network but slum neighborhoods in the north-western part such as golapi chawk, nepali para and in the southern part such as Gandhi ghat, mahatabpur are the areas of inaccessibility. Also, the result identified about 15% and 85% of slums neighborhoods have inaccessibility and high spatial accessibility accordingly. But there are some slum neighborhoods that are under the catchment area of HCF in this model shows too much travel distance during emergencies.
Thus, after identifying poor to very poor accessible or deprived areas of healthcare facilities demand for new healthcare facility centers (HCF). Because a facility with a suitable location plays a vital role in socioeconomic aspects across a region (Mishra et al., 2021; Dutta et al., 2021b; Kim et al., 2018; Pyrialakou et al., 2016; Yin et al., 2018). In an appropriate location like existing HCFs of the study area which affects the service quality and others costs. However, the addition of healthcare facilities does not a solution whenever healthcare facilities are not in a proper optimal location. The result (Fig. 7) also validates by surveying, people from deprived areas are reported that they are demanding health facilities for a long time (Dutta et al., 2021b).
Assessing suitability for new healthcare facilities (HCF)
The inequality of healthcare services demands new healthcare facilities for upgrading the level of healthcare facilities as well as social well-being and standard of living (Asare-akuffo et al., 2019; Bauer et al., 2020; Chen et al., 2020; El Karim & Awawdeh, 2020; Guida et al., 2022; Lawal & Anyiam, 2019; Liu et al., 2022; Orr et al., 2022; Rekha et al., 2017; Shah et al., 2016; Shi et al., 2022; Vadrevu & Kanjilal, 2016; Wang & Wang, 2020; Zhang et al., 2016; Zheng et al., 2021). The above spatial analysis of the GIS algorithm identifies the lack of geospatial accessibility that helps to enhance the healthcare facilities. The appropriate location of healthcare facilities plays a very effective role in a medical emergency in the developing countries (Basu et al., 2018; Dutta et al., 2021b; Kuldeep et al., 2017; Rekha et al., 2017; Vora, Yasobant, Patel, et al., 2015). The low spatial accessibility areas are faced mortality risk, travel costs and time, and harassment day by day (Bauer et al., 2020; W. Chen et al., 2020; Chen et al., 2019; El Karim & Awawdeh, 2020; Shen et al., 2020). As there is no possibility of reallocating the existing healthcare facilities, therefore the only option is to established a new healthcare facility. Establishing new healthcare facilities, so called, as healthcare site suitability (HSS) is very important for reducing the inequality of healthcare facilities between urban core to urban periphery, urban to rural, and capital to the village (Abdelkarim, 2019; Asare-akuffo et al., 2019; Leone et al., 2019; Vadrevu & Kanjilal, 2016; W. Zhang et al., 2016; Zheng et al., 2021). Healthcare site selection is accomplished through significant analysis which finds suitable to unsuitable areas for established a new healthcare facilities (Dutta et al., 2021b). To assess the suitability, we have developed the Multi-Criteria Decision Making (MCDM) algorithm in GIS environment considering the multiple evaluation criteria (B. Das et al., 2019; Das, 2019; Nithya et al., 2019; Patra et al., 2018). In this phenomenon, GIS is an integrating platform of Remote Sensing, GPS, primary and secondary data, and statistical modeling that enhance the planning and management of healthcare site selection in an area (Dutta et al., 2021b). Based on the above spatial accessibility analysis, we used multiple significant criteria to analyze through Analytical Hierarchy Process (AHP) in the GIS environment (Das et al., 2019; Das, 2019; Nithya et al., 2019; Patra et al., 2018).
Selection of suitable criterion for new healthcare facilities
Healthcare facilities are most efficient when they are in the optimal location with emerging demands (Dutta et al., 2021b). The multicriteria decision-making (MCDM) helps to find the optimal and suitable location for any kind of geospatial planning in the GIS platform (Ahmed et al., 2016; Chandra et al., 2020; Das et al., 2019; Dutta et al., 2021b). For this study of healthcare accessibility, we used the most efficient criteria to identify the optimal location a healthcare facility centers. For finding the suitable location of healthcare facilities, we considered a set of most efficient criteria (Shown in Fig. 8) as:
Land use and land cover
Land use and land cover (LULC) is a dominant factor in any kind of planning to do in the present or future (S. Das, 2019). Land use and land cover (LULC) were classified for the study area using the sentinel-2A image. The operation of unsupervised classification algorithm on sentinel-2A image in Erdas imagine 2014 platform shows the major types of land use and landcover (Figs. 8 and 9a) are settlement (42.68%), vegetation (24.28%), waterbody (3.90%), grassland (4.91%), and fallow land (24.21%). We preferred mainly fallow land and grassland as the site for a new healthcare facility.
Distance to poverty-affected areas
We considered poverty as an evaluation criterion for the construction of new sites for healthcare facilities (Dutta et al., 2021b). Poverty indicates a low level of socioeconomic status under threshold value (as per rules of the government of India, minimum Rs. 900/- per head in a monthly expenditure) (Dutta et al., 2021b). We have estimated the multidimensional poverty index (MPI) using household survey data such as per head income, per head monthly expenditure, assets, level of education, etc. The process of MPI estimation was adopted from Dutta et al., 2021b and as:
The summation of deprivation matrix (gij) multiplied by the weighted value (wj) of each indicator calculate the deprivation score (CI) (Dutta et al., 2021b). After estimating the deprivation score, the households which are under the threshold value considered as ‘multiple 2021’ households. The total count of multiple deprived households divided by the total count of households in a ward of the study area represents the headcount ratio (HCR) (Dutta et al., 2021b). The average (A) number of multiple deprived households in each ward multiplied by headcount ratio revealed the final MPI value in percentage (%) for each ward of the study area (shown in Fig. 9b) (Dutta et al., 2021b). Mostly ward 7, ward 5 and ward 3 are in multiple deprived in the study area.
Distance to slum areas
In Midnapore municipality, 156 notified slums neighborhoods are identified till now. This realistic framework focuses on providing sustainable public healthcare facilities to urban poor as well as slum neighborhoods. The multiple-ring buffer in the ArcGIS platform was performed to classify multiple distances from slum neighborhoods (Fig. 9c).
Distance to population density areas
Population density is an important factor for planning and establishing of a new site for healthcare facilities (Das, et al., 2021). Using the population data of Midnapore municipality to calculate the population density. Figure 9d shows that most of the population is clustered in the center of the town and slum neighborhoods also (Das, et al., 2021). We predominantly focus on the high population density wards for planning the new sites of healthcare facilities.
Distance to existing healthcare facilities
At the starting point of this study, we discussed the twelve healthcare facility centers that are distributed haphazardly in the study area. Dutta reported that the healthcare facilities are distributed from the northeast to the southwest. Thus, we considered the new site away of existing healthcare facilities (Fig. 9e). The north-eastern site, western and southern site is the most demanded site for new healthcare facilities in the study area (Fig. 9e).
Distance to the major road network
From Fig. 9f the deep green colour shows the major road network influencing zone of the study area. The major road is the only road in the study area on which vehicles runs in two ways. As a result, vehicle speeds are interrupted as well as mortality rates, travel costs, etc. are increased due to low spatial accessibility (Das, et al., 2021; Lawal & Anyiam, 2019; Rekha et al., 2017). The distance away from a major road, we considered, these sites are highly recommended for new healthcare facilities.
Elimination of constraint land
After setting the evaluating criteria for the site of new healthcare facilities, there is an arising problem of constraints land. Constraint land is preoccupied by administrative buildings, universities, colleges, government buildings, playgrounds, parks, etc., where no development activities with construction can be performed in the present or future (Abdullahi & Pradhan, 2012). In this study, these kinds of lands (Fig. 10) approximately 2.39 km2 are not permissible and available for construction of new healthcare facilities by the government authority (Abdullahi & Pradhan, 2012). Therefore, we used the erase tool of ArcGIS environment (vs.10.4) for removing these sites before analysis (Dutta et al., 2021b).
Criterion weight and results through AHP
The Analytical Hierarchy Process (AHP) is an expert opinion-based methodology that helps to judge multicriteria for any kind of geospatial study (Chandra et al., 2020; Das et al., 2019; Das, 2019; Nithya et al., 2019; Patra et al., 2018). The AHP method is widely used for exploring different natural phenomena (such as landslide susceptibility zonation mapping, flood hazard zonation mapping, natural resource exploration, etc.,), site suitability identification, resource management, etc. (Chandra et al., 2020; Das et al., 2019; Das, 2019; Nithya et al., 2019; Patra et al., 2018). In this study, we have used suitability analysis for finding a new site of healthcare facilities. For new site selection, we considered the pairwise comparison matrix of the AHP which is based on multicriteria decision-making (MCDM) for giving hierarchal order to selecting multicriteria with their priority and rank (Patra et al., 2018). Satty (1980) was developed pairwise comparison matrix as well as the AHP methodology (Chandra et al., 2020; Das et al., 2019; Nithya et al., 2019; Patra et al., 2018). Pairwise comparison matrix has been used for assigning weights (1–9 scale) of different criteria based on their influences (Nithya et al., 2019). The assigning weights scale recommended by Thomas Satty in 1980 as (Tables 3 and 4):
For justification and evaluation of the assigning weights in pairwise comparison matrix, consistency ratio (CR) value should be equal or under 0.1, otherwise, the matrix will not be accepted (Nithya et al., 2019; Patra et al., 2018). The CR value is calculated using the following equation as:
Here, CI = Consistency index and RI = Random index.
Also, CI represents the consistency of every criterion’s judgment. CI is calculated using the following equation:
where, λmax is the largest eigenvalue and n represents number of criteria.
Random index (RI) value was provided by Satty (1980) based on several criteria selected for the study (Chandra et al., 2020; Das et al., 2019; Das, 2019; Nithya et al., 2019; Patra et al., 2018). Thereafter, the valuable assigning weights were used in the ArcGIS environment for the final site suitability analysis using overlay techniques (Das et al., 2019). After overlay, the resultant map (shown in Fig. 11) is classified into five categories such as most suitable, suitable, moderate, poor, and very poor. The most suitable areas for new healthcare facilities are only for 2% shown in ward 1 and ward 25. Suitable areas are shown in nearly Gandhi ghat, Vidyasagar university, tantigeria, and ward no. 1 as 5%. Most of the places of core area in study area are shown as moderate and poor as 35% and 54% respectively, and very poor only 4% (Fig. 12 and Table. 5).
Discussion
Despite the development of healthcare facilities in India, peoples are in trouble going through taking a single facility (Rekha et al., 2017; Das, et al., 2021). The realistic framework of this article planned for healthcare facilities to the urban poor as well as urban peripheral communities (Das, et al., 2021). In most developing southeast-Asian countries, especially India, planning of healthcare facilities confronted lots of barriers such as efficient and proper planning, huge population, construction site, etc. (Al-Taiar et al., 2010; Basu et al., 2018; Leone et al., 2019; Rekha et al., 2017; Sedenu et al., 2016; Vora et al., 2015). The optimal location or site of healthcare facilities is very much effective to reduce mortality rates as well as facilitate the pupils (Das, et al., 2021; Huerta Munoz & Källestål, 2012; Reshadat et al., 2018; Yin et al., 2018; Mishra et al., 2021). The connection between the location of healthcare facilities and spatial accessibility is required to be regularly analyzed for providing better facilities (Lawal & Anyiam, 2019). In this article, we employed different GIS techniques to analyze spatial accessibility. The near tool of the ArcGIS platform was employed to analyze the spatial accessibility index (SAI). The resultant map as SAI represents the nearest healthcare facilities from the slum neighborhoods. Also, the service area and location-allocation model in the network analysis extension tool of the ArcGIS platform was used to analyze the coverage of existing healthcare facilities based on road networks. Predictive analysis is an add-in tool of the ArcGIS platform also employed for calculating the traveling time to healthcare facilities using road networks and terrain slopes. The inequality in healthcare facilities ensuring after different spatial analyses. The result of healthcare inequality meets the low spatial accessibility, for instances, mortality rates are very high in rural to urban poor and peripheral communities in India due to the low spatial accessibility and inequality of healthcare distribution. Thus, the demand for healthcare facilities is increasing simultaneously with the increasing population. This study mainly focuses on sustaining health facilities in the slum neighborhoods as well as the total community. Therefore, we have set different evaluation criteria based on spatial analysis which is mostly facilitated to the urban poor. By employing the AHP method, the site suitability for new healthcare facilities is generated. The results of this site suitability analysis show the difference in suitability for the sites of new healthcare facility (Table. 5).
Conclusion
The framework of this study reflects healthcare planning for the Midnapore municipality of West Bengal, India. The adopted methodology evaluates the existing healthcare facilities and improves equitable healthcare facilities for future demand using the GIS-based approach entrenched in ArcGIS 10.4 (ESRI; Lawal & Anyiam, 2019; Mansour, 2016; Owen et al., 2010). This study found largely increased public health demand in developing countries especially slums and rural areas due to poverty as well as sustainable development (Shaw & Sahoo, 2020; Vora et al., 2015). Although poverty is responsible for inadequate health facilities in slums and rural areas during health shocks in different accessibility dimensions (Hossain & Laditka, 2009; Kuldeep et al., 2017; Owen et al., 2010; Shaw & Sahoo, 2020; Vora et al., 2015). The robust analysis of accessibility level to healthcare facilities will be effective for the improvement of healthcare services and planning implementation. Geographic access during health shocks tackles remote access with population/HCF ratio, road environments, terrain characteristics, climatic conditions, and other cultural factors which create a barrier between facilities and patients as well as healthcare utilization (Dutta et al., 2021b; Lawal & Anyiam, 2019; Mansour, 2016). Geographic barriers should be reduced to discover new innovative technology such as telehealth, information, and communication technology (ICT). This study supports measuring geographic accessibility, infrastructure development, road network, and environment development and recommended potential optimal locations for new HCF in deprived health service areas (Mishra et al., 2021). This article suggests to stakeholders such as researchers, urban planners, planning commissions, and local planning authorities to take actionable policies to improve geographic accessibility and healthcare utilization. The measuring accessibility will be more reliable when poverty, population/HCF ratio, the structure of the population, and healthcare capacity are included in this framework. There is an opportunity for the researchers to do more research on geographic accessibility and healthcare facilities to the communities in every time–space framework.
References
Abdelkarim, A. (2019). Integration of Location-Allocation and Accessibility Models in GIS to Improve Urban Planning for Health Services in Al-Madinah Al-Munawwarah, Saudi Arabia. Journal of Geographic Information System, 11(06), 633–662. https://doi.org/10.4236/jgis.2019.116039
Abdullahi, S, & Pradhan, B. (2012). Spatial modelling of site suitability assessment for hospitals using geographical information system-based multicriteria approach at Qazvin city , Iran. https://doi.org/10.1080/10106049.2012.752531
Ahmed, A. H, Mahmoud, H, & Aly, A. M. M. (2016). Site Suitability Evaluation for Sustainable Distribution of Hospital Using Spatial Information Technologies and AHP : A Case Study of Upper Egypt, Aswan City, pp 578–594.
Albert, C, & Assad, R. (2019). Building GIS framework based on multi criteria analysis for hospital site selection in developing countries. Abstract, 6(4), 1–6.
Al-Taiar, A., Clark, A., Longenecker, J. C., & Whitty, C. J. M. (2010). Physical accessibility and utilization of health services in Yemen. International Journal of Health Geographics, 9, 1–8. https://doi.org/10.1186/1476-072X-9-38
Asare-akuffo, F, Twumasi-boakye, R, Appiah-opoku, S, & Sobanjo, O. (2019). Spatial accessibility to hospital facilities : The case of Kumasi. Ghana. African Geographical Review, 00(00), 1–14. https://doi.org/10.1080/19376812.2019.1636667
Basu, R., Jana, A., & Bardhan, R. (2018). A health care facility allocation model for expanding cities in developing nations: Strategizing urban health policy implementation. Applied Spatial Analysis and Policy, 11(1), 21–36. https://doi.org/10.1007/s12061-016-9208-0
Bauer, J, Klingelhöfer, D, Maier, W., Schwettmann, L, & Groneberg, D. A. (2020a). Prediction of hospital visits for the general inpatient care using floating catchment area methods : a reconceptualization of spatial accessibility. International Journal of Health Geographics, 1–11. https://doi.org/10.1186/s12942-020-00223-3
Bauer, J, Klingelhöfer, D, Maier, W, Schwettmann, L, & Groneberg, D. A. (2020b). Spatial accessibility of general inpatient care in Germany : An analysis of surgery, internal medicine and neurology. Scientific Reports, 0123456789, 1–10. https://doi.org/10.1038/s41598-020-76212-0
Bryant, J, Jr, & Delamater, P. L. (2019). Annals of GIS Examination of spatial accessibility at micro- and macro-levels using the enhanced two-step floating catchment area ( E2SFCA ) method. Annals of GIS, 25(3), 219–229. https://doi.org/10.1080/19475683.2019
Chandra, S., Chiranjit, P., & Indrajit, G. (2020). Assessment of groundwater potentiality using geospatial techniques in Purba Bardhaman district. West Bengal. Applied Water Science, 10(10), 1–13. https://doi.org/10.1007/s13201-020-01302-3
Chen, X., Jia, P., & Chen, X. (2019). A comparative analysis of accessibility measures by the two-step floating catchment area ( 2SFCA ) method. International Journal of Geographical Information Science, 0(0), 1–20. https://doi.org/10.1080/13658816.2019.1591415
Chen, W., Liu, W., & Liu, Z. (2020). Integrating Land Surface Conditions and Transport Networks to Quantify the Spatial Accessibility of Cities in China. https://doi.org/10.1080/17445647.2019.1692081
Das, B., Pal, S. C., Malik, S., & Chakrabortty, R. (2019). Modeling groundwater potential zones of Puruliya district, West Bengal, India using remote sensing and GIS techniques. Geology, Ecology, and Landscapes, 3(3), 223–237. https://doi.org/10.1080/24749508.2018.1555740
Das, S. (2019). Groundwater for Sustainable Development Comparison among influencing factor, frequency ratio, and analytical hierarchy process techniques for groundwater potential zonation in Vaitarna basin, Maharashtra, India. Groundwater for Sustainable Development, 8, 617–629. https://doi.org/10.1016/j.gsd.2019.03.003
Delamater, P. L., Messina, J. P., Shortridge, A. M., & Grady, S. C. (2012). Measuring geographic access to health care: Raster and network-based methods. International Journal of Health Geographics, 11, 1–18. https://doi.org/10.1186/1476-072X-11-15
Dos Anjos Luis, A., & Cabral, P. (2016). Geographic accessibility to primary healthcare centers in Mozambique. International Journal for Equity in Health, 15(1), 1–13. https://doi.org/10.1186/s12939-016-0455-0
Dutta, B., Roy, U., Das, M., & Das, S. (2021a). QUALITY OF LIFE AND HEALTH SECURITY AMONG THE SLUM. August.
Dutta, B., Das, M., Roy, U., Das, S., & Rath, S. (2021b). Spatial analysis and modelling for primary healthcare site selection in Midnapore town West Bengal. GeoJournal, 1–30, 0123456789. https://doi.org/10.1007/s10708-021-10528-w
El Karim, A. A., & Awawdeh, M. M. (2020). Integrating GIS accessibility and location-allocation models with multicriteria decision analysis for evaluating quality of life in Buraidah city KSA. Sustainability (switzerland), 12(4), 1412. https://doi.org/10.3390/su12041412
ESRI. (2014). Getting Started with the ArcGIS Predictive Analysis. 45.
Gao, F., Jaffrelot, M., & Deguen, S. (2021). Measuring hospital spatial accessibility using the enhanced two-step floating catchment area method to assess the impact of spatial accessibility to hospital and non-hospital care on the length of hospital stay. BMC Health Services Research, 21(1), 1–12.
Guida, C., Carpentieri, G., & Masoumi, H. (2022). Measuring spatial accessibility to urban services for older adults : An application to healthcare facilities in Milan. European Transport Research Review. https://doi.org/10.1186/s12544-022-00544-3
Hossain, M. M., & Laditka, J. N. (2009). Using hospitalization for ambulatory care sensitive conditions to measure access to primary health care: An application of spatial structural equation modeling. International Journal of Health Geographics, 8(1), 51. https://doi.org/10.1186/1476-072X-8-51
Hosseini, A., Farhadi, E., Hussaini, F., & Pourahmad, A. (2021). Analysis of spatial ( in ) equality of urban facilities in Tehran : an integration of spatial accessibility. Environment Development and Sustainability, 24(5), 6527–6555. https://doi.org/10.1007/s10668-021-01715-3
Huerta Munoz, U., & Källestål, C. (2012). Geographical accessibility and spatial coverage modeling of the primary health care network in the Western Province of Rwanda. International Journal of Health Geographics, 11, 1–11. https://doi.org/10.1186/1476-072X-11-40
Kang, J. Y., Michels, A., Lyu, F., Wang, S., Agbodo, N., Freeman, V. L., & Wang, S. (2020). Rapidly measuring spatial accessibility of COVID - 19 healthcare resources : a case study of Illinois USA. International Journal of Health Geographics, 19, 1–17. https://doi.org/10.1186/s12942-020-00229-x
Kim, Y., Byon, Y., & Yeo, H. (2018). Enhancing healthcare accessibility measurements using GIS : A case study in Seoul Korea. PLoS ONE, 13(2), e0193013.
Kuldeep, B., & V., Uniyal, S., & Nagaraja, R. (2017). Space based inputs for health service development planning in rural areas using GIS. Geodesy and Cartography, 43(1), 28–34. https://doi.org/10.3846/20296991.2017.1302049
Lawal, O., & Anyiam, F. E. (2019). Modelling geographic accessibility to primary health care facilities: combining open data and geospatial analysis. Geo-Spatial Information Science, 22(3), 174–184. https://doi.org/10.1080/10095020.2019.1645508
Leone, F., Komorowski, J., Gherardi-leone, M., & Lalubie, G. (2019). Integrating spatial accessibility in the design of volcano evacuation plans in the French West Indies. Journal of Applied Volcanology, 8(1), 1–22. https://doi.org/10.1186/s13617-019-0089-1
Liu, D., Kwan, M. P., Kan, Z., Song, Y., & Li, X. (2022). Racial / ethnic inequity in transit - based spatial accessibility to COVID - 19 vaccination sites. Journal of Racial and Ethnic Health Disparities, 1–9, 0123456789. https://doi.org/10.1007/s40615-022-01339-x
Maleki Rastaghi, M., Barzinpour, F., & Pishvaee, M. S. (2018). A multi-objective hierarchical location-allocation model for the healthcare network design considering a referral system. International Journal of Engineering, Transactions B: Applications, 31(2), 365–373. https://doi.org/10.5829/ije.2018.31.02b.22
Målqvist, M., Sohel, N., Do, T. T., Eriksson, L., & Persson, L. Å. (2010). Distance decay in delivery care utilisation associated with neonatal mortality A case referent study in northern Vietnam. BMC Public Health, 10(1), 762. https://doi.org/10.1186/1471-2458-10-762
Mansour, S. (2016). Geo-spatial information science spatial analysis of public health facilities in Riyadh Governorate, Saudi Arabia : A GIS-based study to assess geographic variations of service provision and accessibility. Geo-Spatial Information Science, 5020, 1–13. https://doi.org/10.1080/10095020.2016.1151205
McGrail, M. R., & Humphreys, J. S. (2014). Measuring spatial accessibility to primary health care services: Utilising dynamic catchment sizes. Applied Geography, 54, 182–188. https://doi.org/10.1016/j.apgeog.2014.08.005
Miç, P., Koyuncu, M., & Hallak, J. (2019). Primary health care center (PHCC) location-allocation with multi-objective modelling: A case study in Idleb Syria. International Journal of Environmental Research and Public Health, 16(5), 811. https://doi.org/10.3390/ijerph16050811
Mishra, S., Sahu, P. K., Pani, A., & Mehran, B. (2021). Spatial planning framework for development of rural activity centers: Method of location allocation, effect on trip length, and policy implications. Papers in Applied Geography, 7(4), 372–391. https://doi.org/10.1080/23754931.2021.1901237
Mohammadi, A., Valinejadi, A., Sakipour, S., Hemmat, M., Zarei, J., & Majdabadi, H. A. (2018). Original Article improving the distribution of rural health houses using elicitation and GIS in Khuzestan Province (the Southwest of Iran). Kerman University of Medical Sciences, 7(4), 336–344. https://doi.org/10.15171/ijhpm.2017.101
Moïsi, J. C., Gatakaa, H., Noor, A. M., Williams, T. N., Bauni, E., Tsofa, B., Levine, O. S., & Scott, J. A. G. (2010). Geographic access to care is not a determinant of child mortality in a rural Kenyan setting with high health facility density. BMC Public Health, 10(1), 1–9.
Nithya, C. N., Srinivas, Y., Magesh, N. S., & Kaliraj, S. (2019). Remote Sensing Applications : Society and Environment Assessment of groundwater potential zones in Chittar basin, Southern India using GIS based AHP technique. Remote Sensing Applications: Society and Environment, 15, 100248. https://doi.org/10.1016/j.rsase.2019.100248
Openshaw, S. (1983). Location-allocation techniques: Practical methods for spatial planning. Planning Outlook, 26(1), 7–14. https://doi.org/10.1080/00320718308711687
Orr, A. M., Stewart, J. L., Orr, A. M., & Stewart, J. L. (2022). Property use diversity and spatial accessibility within urban retailing centres : Drivers of retail rents retailing centres : Drivers of retail rents ABSTRACT. Journal of Property Research, 00(00), 1–28. https://doi.org/10.1080/09599916.2022.2046138
Owen, K. K., Obregón, E. J., & Jacobsen, K. H. (2010). A geographic analysis of access to health services in rural Guatemala. International Health, 2(2), 143–149. https://doi.org/10.1016/j.inhe.2010.03.002
Parry, J. A., Ganaie, S. A., & Bhat, M. S. (2018). GIS based land suitability analysis using AHP model for urban services planning in Srinagar and Jammu urban centers of Jampamp;K. India. Journal of Urban Management, 7(2), 46–56. https://doi.org/10.1016/j.jum.2018.05.002
Patra, S., Mishra, P., & Chandra, S. (2018). Delineation of groundwater potential zone for sustainable development : A case study from Ganga Alluvial Plain covering Hooghly district of India using remote sensing, geographic information system and analytic hierarchy process. Journal of Cleaner Production, 172, 2485–2502. https://doi.org/10.1016/j.jclepro.2017.11.161
Polo, G., Acosta, C. M., Ferreira, F., & Dias, R. A. (2015). Location-allocation and accessibility models for improving the spatial planning of public health services. PLoS ONE, 10(3), 1–14. https://doi.org/10.1371/journal.pone.0119190
Pyrialakou, V. D., Gkritza, K., & Fricker, J. D. (2016). Accessibility, mobility, and realized travel behavior: Assessing transport disadvantage from a policy perspective. Journal of Transport Geography, 51, 252–269. https://doi.org/10.1016/j.jtrangeo.2016.02.001
Rekha, R. S., Radhakrishnan, N., & Mathew, S. (2020). Spatial accessibility analysis of schools using geospatial techniques. Spatial Information Research, 28, 699–708. https://doi.org/10.1007/s41324-020-00326-w
Rekha, R. S., Wajid, S., Radhakrishnan, N., & Mathew, S. (2017). Accessibility Analysis of Health care facility using Geospatial Techniques. Transportation Research Procedia, 27, 1163–1170. https://doi.org/10.1016/j.trpro.2017.12.078
Reshadat, S., Zangeneh, A., Saeidi, S., Teimouri, R., & Yigitcanlar, T. (2018). Measures of spatial accessibility to health centers : Investigating urban and rural disparities in Kermanshah.
Sedenu, A., Muibi, K., Alaga, A., Ajileye, O., Ogbole, J., Kappo, A., Popoola, O., & Mustapha, O.-O. (2016). Spatial analysis of the distribution pattern of primary healthcare facilities in ile – ife metropolis using geographic information system. Journal of Scientific Research and Reports, 10(1), 1–15. https://doi.org/10.9734/jsrr/2016/22339
Shah, T. I., Bell, S., & Wilson, K. (2016). Spatial accessibility to health care services: Identifying under-serviced neighbourhoods in Canadian urban areas. PLoS ONE, 11(12), 1–22. https://doi.org/10.1371/journal.pone.0168208
Shaw, S., & Sahoo, H. (2020). Accessibility to primary health centre in a Tribal District of Gujarat, India: Application of two step floating catchment area model. GeoJournal, 85(2), 505–514. https://doi.org/10.1007/s10708-019-09977-1
Shen, C., Zhou, Z., Lai, S., Lu, L., Dong, W., Su, M., Zhang, J., Wang, X., Deng, Q., Chen, Y., & Chen, X. (2020). Measuring spatial accessibility and within- province disparities in accessibility to county hospitals in Shaanxi Province of Western China based on web mapping navigation data. International Journal for Equity in Health, 19(1), 1–13.
Shi, Y., Yang, J., Keith, M., Song, K., Li, Y., & Guan, C. (2022). Spatial accessibility patterns to public hospitals in shanghai : an improved gravity model. The Professional Geographer, 74(2), 265–289. https://doi.org/10.1080/00330124.2021.2000445
Song, Y., Tan, Y., Song, Y., Wu, P., Cheng, J. C. P., Kim, M. J., Song, Y., Tan, Y., Song, Y., Wu, P., Cheng, J. C. P., & Kim, M. J. (2018). Spatial and temporal variations of spatial population accessibility to public hospitals : A case study of rural – urban comparison. Giscience & Remote Sensing, 55(5), 718–744. https://doi.org/10.1080/15481603.2018.1446713
Subal, J., Paal, P., & Krisp, J. M. (2021). Quantifying spatial accessibility of general practitioners by applying a modified huff three - step floating catchment area ( MH3SFCA ) method. International Journal of Health Geographics, 20, 1–14. https://doi.org/10.1186/s12942-021-00263-3
Tao, R., Downs, J., Beckie, T. M., Chen, Y., Mcnelley, W., Tao, R., Downs, J., Beckie, T. M., Chen, Y., & Mcnelley, W. (2020). Annals of GIS Examining spatial accessibility to COVID-19 testing sites in Florida ABSTRACT. Annals of GIS, 00(00), 1–9. https://doi.org/10.1080/19475683.2020.1833365
Vadrevu, L., & Kanjilal, B. (2016). Measuring spatial equity and access to maternal health services using enhanced two step floating catchment area method (E2SFCA) - A case study of the Indian Sundarbans. International Journal for Equity in Health, 15(1), 1–12. https://doi.org/10.1186/s12939-016-0376-y
Vora, K. S., Yasobant, S., Sengupta, R., De Costa, A., Upadhyay, A., & Mavalankar, D. V. (2015). Options for optimal coverage of free C section services for poor mothers in indian state of Gujarat: Location allocation analysis using GIS. PLoS ONE, 10(9), 1–16. https://doi.org/10.1371/journal.pone.0137122
Waithaka, T. K. K. E. H. (2015). GIS location-allocation model in improving accessibility to health care facilities: A case study of Mt. Elgon Sub-County. International Journal of Science and Research (IJSR), 4(4), 3306–3310.
Wang, F., & Wang, F. (2020). Annals of GIS Why public health needs GIS : A methodological overview Why public health needs GIS : A methodological overview. Annals of GIS, 26(1), 1–12. https://doi.org/10.1080/19475683.2019.1702099
Wielebski, Ł, & Medyńska-gulij, B. (2018). Graphically supported evaluation of mapping techniques used in presenting spatial accessibility. Cartography and Geographic Information Science, 00(00), 1–23. https://doi.org/10.1080/15230406.2018.1479311
Yin, C., He, Q., Liu, Y., Chen, W., & Gao, Y. (2018). Inequality of public health and its role in spatial accessibility to medical facilities in China. Applied Geography, 92, 50–62. https://doi.org/10.1016/j.apgeog.2018.01.011
Zhang, S., Song, X., & Zhou, J. (2021). An equity and efficiency integrated grid- to-level 2SFCA approach : Spatial accessibility of multilevel healthcare. International Journal for Equity in Health, 20(1), 1–14. https://doi.org/10.1186/s12939-021-01553-9
Zhang, W., Cao, K., Liu, S., & Huang, B. (2016). A multi-objective optimization approach for health-care facility location-allocation problems in highly developed cities such as Hong Kong. Computers, Environment and Urban Systems, 59, 220–230. https://doi.org/10.1016/j.compenvurbsys.2016.07.001
Zhao, X., Coates, G., & Xu, W. (2019). A hierarchical mathematical model of the earthquake shelter location-allocation problem solved using an interleaved MPSO–GA. Geomatics, Natural Hazards and Risk, 10(1), 1712–1737. https://doi.org/10.1080/19475705.2019.1609605
Zheng, L., Li, J., Hu, W., & Duan, P. (2021). Analysis of the spatial range of service and accessibility of hospitals designated for coronavirus disease 2019 in Yunnan Province. Geocarto International. https://doi.org/10.1080/10106049.2021.1943008
Acknowledgements
The authors are grateful to Midnapore Municipality for providing the base map of the study area. The authors also would like to thank to all researcher for their competent research, encouragement, and valuable suggestion for undertaking this study.
Funding
This research did not receive any specific grant or financial support from funding agencies.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There is no potential conflict of interest was reported by the authors.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants involved in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Das, M., Dutta, B., Roy, U. et al. Spatial accessibility modeling to healthcare facilities in the case of health shocks of Midnapore municipality, India. GeoJournal 88, 3749–3772 (2023). https://doi.org/10.1007/s10708-023-10838-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10708-023-10838-1