Abstract
In a resource-constrained society in developing nations like India, the importance of health care infrastructure allocation is often undermined and overlooked. This paper aims to quantify the gap in accessing affordable health care facilities faced by the socio-economically weaker sections of society. Majority of the older cities in India have a central core and surrounding peri-urban areas, which were added later on to minimize the stress of urban expansion and to provide adequate infrastructure. This research states that installation of new facilities for catering to the growing needs of citizens in expanding cities is the need of the hour. We propose a novel technique for maximizing the health care coverage of the peri-urban areas by establishing the minimum number of new public health care facilities. Our aim is to suggest strategies for efficient implementation of policies such as the National Urban Health Mission and the National Health Policy. We considered Kolkata Municipal Corporation, India as a case study to assess our proposed methodology. The southern periphery, which was added in 1981 and has currently expanded again in 2015, is completely devoid of public health care facilities. Our optimization model showed that 13 new public facilities are required in the southern periphery, out of which five are extremely critical. The rise in health care coverage from 76.19 to 90.05 % by taking only the southern periphery into consideration shows the impact of the new facilities placed according to the proposed framework.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In resource-constrained societies of low-income countries like India, the importance of health care infrastructure allocation is often undermined and overlooked leading to slow progress towards agreed health goals (Travis et al. 2004). Urbanization and expansion of cities in such nations only leads to increasing pressure on the existing facilities if additional ones are not provided for the needs of the growing population. Public investment in health care infrastructure has been historically low in India (Reddy et al. 2011). For the period 2011–2015, only 4.7 % of the Gross Domestic Product of India has been invested in total health expenditure (out of which 1.4 % is for the public health sector), which contrasts sharply with 10.2 % for Japan (8.6 % in public sector) and 17.1 % for USA (8.3 % in public sector) (WorldBank 2016). Low public investment has led to proliferation of private players in the health care sector over the last 20 years. Accessibility and quality issues concerning public facilities are forcing people to seek out private outlets, which often lead to higher health care expenditures (Selvaraj and Karan 2009). Consequently, millions of households are being pushed below the poverty line and into health shocks. Health shock refers to an inability to seek adequate and appropriate medical care which may be due to economic reasons, unavailability of proper resources, etc. It is generally captured by negative changes in Body Mass Index, and adverse health shocks are associated with reductions in earned income due to increased out-of-pocket (OOP) expenditures (Wagstaff 2007). The development of public health care infrastructure should be planned based on accessibility and affordability gaps, which can be estimated by understanding the socio-economic classifications in Indian society. With a substantial proportion of the population belonging to economically weaker sections and lower income group (Patel et al. 2014), additional private facilities do not provide affordable people-centered opportunities. This has led to (i) increased OOP expenditure in terms of health care services and transportation (Balarajan et al. 2011), (ii) increased dependency in terms of mobility and information, (iii) delayed health care seeking activity, often resulting in social seclusion and disparity, and (iv) overcrowding of public providers in the city core. Like previous national policies, the Urban and Regional Development Plans Formulation and Implementation (URDPFI) Guidelines 2015 recommended allocation of health infrastructure as per population norms. The National Health Policy (NHP) 2002 (MoHFW 2002) and the National Urban Health Mission (NUHM) 2013 (MoHFW 2012) suggested architectural correction of the health system (Husain 2011) i.e. moving away from infrastructure allocation based on population or population density based allocation to a critical accessibility time-based allocation, so that ‘health for all’ is ensured.
Rahman and Smith (2000) have found that only a handful of academic location-allocation studies in developing nations (which are generally purely mathematical in nature) have claimed implementation of their results, since locational decisions are usually taken by local elected leaders or government officers. Therefore, it is essential that we consider national health care policies and guidelines while attempting to bridge the gap in spatial accessibility of health infrastructure. This is especially important since the World Health Organization had decreed that addressing inequalities in health, urban poverty and the needs of vulnerable groups should be the foremost aims of a ‘Healthy City’ (WHO 1986). Majority of the Indian metropolises are similar in nature in terms of economic distribution of the population with the economically disadvantaged sections facing the same obstacles in availing affordable and accessible health care service delivery options (Iyer et al. 2007). Additionally, major cities within India like Kolkata are undergoing rapid urbanization which leads to neighboring hinterlands being incorporated within the city municipal boundaries. The fallout of this phenomenon is the growing disparity in access to infrastructure. Urban city expansion strategies are often based on (a) developing green field satellite towns adjacent to the existing cities (Rumbach 2014) and (b) encompassing the existing peri-urban areas within the city limits (Kontgis et al. 2014). In case of the city of Kolkata, we observe both, but the city suffers considerably in terms of equitable access to affordable facilities. On one hand, the green field developments have its own planning process, gestation period and socio-economic fabric; on the other hand, the peri-urban areas often inherited organic growth and underdevelopment in terms of social and physical infrastructure (Dahiya 2003; Shaw 2005) with inevitable dependency on the older city core.
Data from the 71st Round of National Sample Survey titled ‘India – Social Consumption: Health’ (MoSPI 2015) reveals that India still experiences a considerable gap in providing equitable access to health care facilities. Longer waiting times were cited as a reason for not opting for government sources, which is an indication of the existing public facilities being overburdened (Duggal 2001). The quality gap in service delivery and gaps in spatial accessibility were also given as major reasons for going to private facilities. However, it is noteworthy that private health care facilities are associated with high OOP expenditures, which ultimately lead to a conscious constraint on the urban poor’s health seeking behavior.
In order to balance the supply and demand for health care needs, new public facilities need to be provisioned with an aim to alleviate the service quality and accessibility concerns about the existing ones. Rahman and Smith (2000) comprehensively review the existing location-allocation models for health care and conclude that most of them are based on either or both of these two assumptions: (i) each health facility has an infinite capacity to serve consumer demand, and (ii) the study has used a single criterion objective function such as minimizing the travel time or the health cost. This paper aims to overcome both these assumptions by performing multi-criterion optimization taking the policy guidelines as constraints, thereby limiting the capacity of each facility. Review studies by Scott (1970) and Tomintz and Garcia-Barrios (2014) highlight the improvement in modeling approaches to location-allocation planning for health care over the years, but their application to developing nations still remains a concern. Several researchers have emphasized upon the use of geographical mapping software such as GIS in network and public health intervention planning (Birkin et al. 2002; Gesler et al. 2004; Cromley and McLafferty 2011). In light of these studies, our research uses GIS as a tool in order to map the study area, identify locations which require intervention and the locations of the proposed facilities. Several models can be found in the literature which aim to reduce the gap in service quality. The most popular one seems to be the SERVQUAL model, which has been used in the health care sector extensively (Babakus and Mangold 1992; Kilbourne et al. 2004; Butt and de Run 2010). However, this paper does not focus on the quality aspect. We aim to address the spatial accessibility gap so that the burden on existing facilities can be mitigated to some extent.
A novel framework is proposed that can be used to allocate new infrastructure to ameliorate the ever-increasing pressure faced by existing health care facilities. The methodology is demonstrated through a case study of the city of Kolkata, India due to availability of data for this city. The latest urban and health care policy guidelines issued by the Government of India are incorporated in our framework. The rest of the paper is structured as follows. Section 2 provides an in-depth analysis of urban and health care policies issued by the Government of India until 2015, followed by a description of the health care seeking behavior for residents of peri-urban areas in Section 3. The framework for allocation of new health care facilities based on minimizing the gap in spatial accessibility is outlined in Section 4. The results of applying this framework to Kolkata are examined in Section 5, followed by discussions and conclusions in Section 6.
Indian Health Care Policy Context
Development of health care infrastructure in India has been based majorly on the population density criterion, as demonstrated by previous national health care policies. Such an approach often overlooked the needs of the population, thereby neglecting measures of system evaluation such as utilization rate and stress on available resources. To counter the growing stress of unavailability, private investment in health care delivery was encouraged to provide an alternative for the people. However, the issue of inequality and disparity emerged and has persisted since. The NHP 1983 aimed towards majorly reducing inequalities affecting access and quality through the following measures: (i) providing a well-dispersed network of primary health care services, and (ii) ensuring that the approach to health care consists of an integrated package of services instead of a collection of disparate health interventions. However, conflict of priority between the central and the state government has often led to the negligence of the development of public health and related issues since health care is a state responsibility (Peters et al. 2003).
In response, the NHP 2002 emphasized the need to increase the overall utilization of the public health care facilities (PHCFs). To speed up the process of economic development, social elevation and improving the quality of life, the National Rural Health Mission in 2005 and the NUHM in 2013 were launched with the objective to carry out necessary architectural correction in the basic health care delivery system and improve accessibility to health care facilities for the deprived groups. Rashtriya Swasthya Bima Yojna (RSBY) was launched in 2008 to provide health insurance to all economically weaker sections, especially those below the poverty line. Studies seeking to determine the effectiveness of this scheme by focusing on a particular state of India (Rajasekhar et al. 2011; Nandi et al. 2012; Devadasan et al. 2013) have found varying results. However, it was concretely concluded by Narayana (2010) that the RSBY is far from achieving full penetration on a national scale, thereby making it essential for future policies and interventions to target the economically weaker sections.
Although public health initiatives over the years have contributed significantly to the improvement of health indicators such as demographic changes (life expectancy, crude birth rate etc.) and infrastructure (beds, Primary Healthcare Centers etc.), the limited success of the public health system in meeting the preventive and curative requirements of the general population (De Costa and Diwan 2007) cannot be overlooked. The NUHM, which was passed in 2013, focused on delivering affordable and essential primary health care services to the urban poor. This can be achieved through development of a need-based city-specific urban health care system, which ensures availability of resources for providing essential primary health care to the urban poor. Public facilities provide essential health care services at nominal prices to society and hence are referred to as affordable facilities. This is why it is essential to provide additional public facilities so that the health care needs of the urban poor are met. From the urban point of view, it is also necessary to reduce the travel time to the destination hospital, which is highly inconvenient when one is ill. Therefore, there is an imminent need to also address the increasing travel times due to the destination facility lying in a neighborhood far away from the source neighborhood.
Behavior in Peri-Urban Areas
In metropolitan cities, there is a tendency of polarization of services. In the case of any Indian metropolitan city, the same is observed even for health care facilities. Urban areas, housing 27 % of the population, witness a concentration of about 75 % of health infrastructure, medical man power and other health resources (Patil et al. 2002). Based on the argument that choice might be a function of infrastructure parameters and individual characteristics (Luo and Whippo 2012), health care seeking behavior was assumed to be an outcome of supply and quality of the health care services and demand subjected to affordability and perceived seriousness of illness. In general, the following phenomena were observed: (1) longer travel distance to destination, affecting travel time and cost, although public transportation is subsidized, (2) inter and intra household interactions (Jana et al. 2014), and (3) higher OOP expenditure (van Doorslaer et al. 2006).
This research makes use of the following dataset for analysis ‘Social Consumption: Health, NSS, 71st Round (January - June 2014)’. The National Sample Survey Office carries out National Samples Surveys quite regularly based on specific domains, such as health, consumer expenditure, etc. The entire geographical area of the country is divided into rural and urban sectors considering each district and state. Accordingly, households are randomly sampled from each sector and interviewed based on a specific questionnaire pertaining to consumption of health care facilities.
We extracted a dataset of 405 samples from the national level database, all of whom are residents of the Kolkata Municipal Corporation (KMC). It was found that 94 % (379/405) took medical advice and went to health care facilities. The remaining 6 % can be classified as the ‘do-nothing’ segment. It is not surprising to find extremely low proportions of patients going to ‘ANM/ASHA/AWWFootnote 1’ (0 %) and ‘PHC/Dispensary/CHC/Mobile medical unitFootnote 2’ (1 %), since such facilities are majorly found in rural areas. The aforementioned facilities are henceforth referred to as PUB01 and PUB02 respectively. These health care options are much more popular among rural residents in India, given that urban residents have access to much better and larger facilities. Figure 1 shows that 14 % of the sample went to ‘Public hospital’ (PUB03), while 77 and 8 % went to ‘Private doctor/clinic’ (PVT01) and ‘Private hospital’ (PVT02) respectively. The skewed use for private health care service delivery options is characteristic of urban residents (Selvaraj and Karan 2009), which is independent of the status of ailment as seen from Table 1. The reasons for not preferring public facilities as revealed by the survey respondents are enumerated in Fig. 2.
Another interesting observation from Fig. 2 is that a combined 89 % of the surveyed residents felt that the quality of services provided by public facilities was not satisfactory; even if satisfactory, the facilities were located too far or they had to wait for a very long duration. These insights lead us to the conclusion that the public health care facilities have to be majorly revamped in terms of breadth of services and spatial accessibility (De Costa and Diwan 2007). Long waiting times indicate the substantial gap between supply and demand for such existing facilities. Moreover, private facilities induce higher OOP expenditures, which might not be affordable for the urban poor and marginalized sections. Therefore, it is imperative that enhancement of the public health care sector be given adequate importance.
To that effect, this research proposes a methodology to remove spatial accessibility gaps in availing health care infrastructure. Using the case study of Kolkata, we identify locations where new facilities must be provided in order to mitigate the burden on existing facilities. Moreover, extremely crucial locations (among those obtained in the previous step) are also identified for provisioning of health care infrastructure by the government.
Conceptual Framework
The majority of the older cities in India have a central core and surrounding peri-urban areas that are added later in order to minimize the stress of urban expansion and to provide adequate infrastructure (Shaw 2005). In general, the older central core has an adequate number of health care facilities whereas the newly added peri-urban areas experience gaps in terms of public (affordable) health care facilities. Keeping the argument proposed by Allen (2003) that planning and management of the peri-urban interface cannot simply be based on the extrapolation of planning approaches and tools applied in rural and urban areas, we propose to divide the urban area into two parts: Part A, which consists of the older city core area and Part B, which consists of the newly added areas.
The following novel formulation is used to model the problem. Figure 3 outlines the proposed methodology in brief, while the following paragraphs elucidate each step of the framework. Although Shariff et al. (2012) has presented a location allocation model for health care facility planning (adapted from Pirkul and Schilling (1991)) in Malaysia using genetic algorithm, data constraints in developing nations often inhibit implementation of such models. To ensure implementation, our proposed framework has been modeled as a less data-intensive and computationally easier approach which includes policy guidelines as well.
The study area has to be divided into G grids, each having dimensions of 500 × 500 m. The grids, however, will not have uniform population density because the density will be assigned to the grids based on the wards to which they belong. For greater predictive accuracy, a finer resolution of grid size (such as 100 m) may be taken. However, we have considered the dimension in this study as 500 m for computational ease. The population of the study area can be taken as \( {P}_0 \) (in millions), while the area is equal to \( {A}_{0\;}\left(=G*500*500/{10}^6=0.25G\right) \) km2. The objective is to minimize \( \sum_i{n}_i^{\prime } \), where \( {n}_i^{\prime } \) represents the number of new PHCFs that have to be placed in the i th grid. This has to be subjected to the following constraints.
Maximizing the coverage of health care in the study area requires minimization of the void space when the areas of influence for new facilities are placed in that area. Such an approach calls for a hexagonal area of influence rather than considering the traditional square or triangular tiling. Hexagonal tiling, or hextille (Conway et al. 2008), is the densest way to arrange circles in two dimensions (Coxeter 1973), as has also been proved by the Honeycomb Conjecture (Hales 2001). The area of a hexagon \( (A) \) is given by \( 3{r}^2. sin\left({60}^o\right) \), where \( r \) is the radius of the hexagon (taken as two kilometers in this study). The accessibility radius of two kilometers has been considered based on ease of walkability and mode available to people in form of rickshaws (both manual and motor driven). Moreover, the Government of India has decreed that the “time-to-care” should be within 30 min, i.e. health care delivery facilities should be within 30 min of walking distance (MoHFW 2014). There are several medical studies in the literature which have found average walking speeds to be between 4 and 5 kmph (Knoblauch et al. 1996; Bohannon 1997). Since inclusion of patients in the travelling group will decrease the speed, we consider the lower value of 4 kmph in order to be conservative. Thus, our considered limit of two kilometers \( \left(=30\; mins*4\; kmph\right) \) stands validated. Therefore, the minimum number of new PHCFs that must be installed is equal to \( \left({A}_0/A=0.25G/10.39\right) \), where the area of a hexagon \( (A) \) with radius equal to two kilometers is 10.39 km2. If \( {n}_i^{\prime } \) is the number of new facilities that have to be provided in the i th grid, then:
The first constraint given by Equation (1) aims to maximize the coverage of the study area such that the areas of influence of the new facilities cover the entire study area. From Table 2 given by URDPFI, it is clearly understood that 0.10 million population has to be taken as the critical population while determining the number of new facilities.
Thus, the minimum number of new facilities according to policy guidelines is equal to \( \left({P}_0/0.10=\right)\;10{P}_0 \). This ensures that the proposed model caters to the population to be served by each facility, thereby placing a constraint on the capacity of the facility.
where \( N\left(=D.n^{\prime}\right) \) is a column matrix denoting accessibility to all (both existing and to-be-installed) facilities and \( D \) is the accessibility (to existing facilities) matrix. If a destination grid l is more than the accessibility radius of two kilometers (according to the road network) away from origin grid k or is otherwise inaccessible due to uninhabitable or arable land, then \( {D}_{kl} \) will be equal to 0; otherwise \( {D}_{kl} \) is equal to 1. This constraint ensures that each grid has access to at least one health care facility within a radius of two kilometers.
This constraint ensures that the facility matrix obtained after optimization is an improvement upon the current facility matrix \( (n) \) which has been constructed using the existing system. A metric for improvement is to compare the health care coverage in the study area before and after placing the new facilities. This will serve as a performance measure for the proposed framework.
where \( {PoP}_i^a \) represents the population of the grids which have access to a public health care facility within two kilometers and \( {PoP}_i \) represents the total population of the study area.
Location Allocation Problem: a Case Study
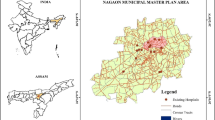
Kolkata, a 300 year old city, has been dynamically growing over time, with components such as planned city core and satellite townships, defunct industrial estate, scattered squatter settlements and splinters of modern living (U. Sengupta 2006). In 1981, KMC expanded from 100 wards to 141 wards when the southern and southwestern peripheries were amalgamated within the city limits. Figure 4 depicts the wards according to their phase of addition to the KMC as well as their populations. Arguably, these peri-urban areas had noticeable traffic congestion and poor accessibility to basic infrastructure as they became part of KMC. Although the need for infrastructure development, upgrade and expansions was assessed, yet developmental and financial constraints often curbed the initiatives (Mehta and Pathak 1998). After three decades of such expansion, this paper argues that there is still a formidable difference in access to opportunity, which has its root cause in fragmented policy formulations affecting the growth dynamics and vibrancy of cities (Gnaneshwar 1995).
Figure 5a shows the accessibility of all health care facilities, while Fig. 5b shows only public (affordable) facilities in the KMC area. Areas with deeper colors in Fig. 5 have access to health facilities within a smaller radius. As the accessibility radius increases, the intensity of the color on the map decreases. The critical accessibility distance for effective coverage has been taken as two kilometers, as discussed earlier. A close look at Fig. 5b reveals that there are several areas in the periphery of the KMC which do not have access to PHCFs, i.e. the white or uncolored areas. We take up the southern area (as marked in Fig. 5b) for our case study because it is the largest and most populated one among the aforementioned areas. It is also noteworthy that this is the new direction of urban expansion as per Government of West Bengal notifications and therefore, it is important to plan for facilities to support this urban sprawl. Moreover, the western periphery consists of wetland area majorly (see Fig. 4), which houses a very small proportion of the total population of the KMC area.
The southern area has 214 grids, out of which 37 grids have to be excluded as they are majorly arable or uninhabitable land. Another reason for exclusion is that the geographical centroid of these grids is more than 100 m (critical walking distance) away from the nearest road network point, which means that the grid does not have basic access to the transport network. Thus, the number of grids in the study area \( (G) \) is equal to 177, which corresponds to an area of 44.25 km2. The population of the study area \( \left({P}_0\right) \) is equal to 0.86 million. Equation (1) gives the critical number of new public facilities as 5, while Equation (2) gives the same as 9. Thus, combining the two equations will give the following constraint:
Therefore, our aim is to:
subject to the constraints given by Equations (3), (4) and (6). Since our study area (just the southern area of the KMC) does not have any existing public health care facilities, the n matrix in Equation (4) is a zero matrix. The optimization yields the total number of new PHCFs required in the study area to be equal to 13, the locations of which have been depicted in Fig. 6. The health care coverage of the KMC, which has been calculated from Equation (5), rises from 76.19 to 90.05 % due to the newly allocated facilities.
Discussions
Lack of provisioning of affordable basic services in the peripheral regions of rapidly growing megacities in developing countries is a cause of concern for increasing disparity and lower quality of life. Even after decades of urban expansion, the gap in access to basic infrastructure persists. Health care service being one of the primary needs, it is not surprising that cities in developing nations still do not meet the norms of ‘Healthy Cities’ as set by WHO. This paper highlights the current disparity of service provisioning and proposes a framework for allocation of new health care facilities to meet the gap in the basic needs of citizens, especially in the newly added regions. Although there are constraints based on both economic and spatial accessibility to affordable health care facilities for the urban poor, this paper focuses only on the gap in spatial accessibility faced by those living in peri-urban areas (majorly low income groups and economically weaker sections).
The proposed optimization technique is based on maximizing the health care coverage of the study area by establishing the minimum number of new PHCFs (public and therefore, affordable). Although there are several private health care facilities in the study area, the issue of differential health expenditure while using public vs private facilities remains a pressing concern (A. Sengupta and Nundy 2005). Based on Figs. 5a and 6, we can identify three zones in our study area (as marked in Fig. 6) which do not have access to even a single health care facility (public or private). Thus, it is imperative that the new PHCFs obtained from the optimization results be allocated first in those three zones before other zones are taken into consideration. Based on the gravity of the living situation of the people in those three zones, we have identified five critical PHCFs (out of 13) which have to be constructed at the earliest. Recently, in 2014, the National Health Mission (MoHFW 2015) had decreed in its State Program Implementation Plans that five PHCs need to be set up in the KMC region in 2015–16 based on the growing population and health care needs. We propose that the five new PHCFs outlined in Fig. 6 be established imminently as per implementation of the latest NRHM policy. Recently, addition of three new wards in the southwestern periphery led to the total number of wards in the KMC rising from 141 to 144. This southern expansion of the KMC highlights the immediate importance of the proposed locations of three of the five critical PHCFs, i.e. the ones placed in the southern periphery.
Another question that must be addressed is the exact spatial location of the facility within the grid. Erkut and Neuman (1989) highlighted the difficulty in determining the exact location by solely using location-allocation modeling. Such an approach might be used to identify a few candidate sites, but the final site selection is a complex problem and should be tackled using a multi-objective decision making process. Our research does not provide any insight on this issue and has placed the facility at the geographical centroid of the grid. Such allocations cannot be done without obtaining data from field surveys and establishing the distribution of government-owned land in those zones. The grid size of 500 m taken in the case study is, thus, a safer approximation than the finer resolution of 100 m. Taking this grid size for our optimization calculations provides room for surveying and then accurately allocating government-owned land for establishment of new PHCFs.
The increased health care coverage of 90.05 % by taking only the southern periphery shows the impact of the new facilities placed according to the proposed optimization model. Increasing the accessibility of the facilities by establishing a comprehensive road network can enhance this coverage further. Some grids, although within the area of influence of the new facilities, do not have access due to gaps in the transport network. There is also room for further improvement by placing similar facilities in the other peripheral regions not taken into consideration in this research, i.e. the white or uncolored regions in Fig. 5b apart from the southern region.
Travis et al. (2004) stressed upon the importance of focusing on health-systems strengthening instead of disease priority for achievement of the Millennium Development Goals. There is a need for integration of urban planning and development interventions together with allied policies governing basic services such as health care and education, to promote simultaneous strategies to fulfill the need of the people and reduce inconsistencies. Disparity owing to locational aspects was found to have grave consequences, clearly illustrating locational disadvantages of the residents in peripheral wards with pockets of underdevelopment. The effects of fragmented policies and inconsistent focus of initiatives in developing nations often lead to over-stressing on existing infrastructure, social seclusion and lower quality of life. Although core areas of cities might have adequate number of health care facilities, the urban poor have to face affordability issues due to service delivery at private facilities causing patients to incur huge OOP expenditures. Peri-urban areas suffer further due to limited number of public (affordable) health care facilities in those regions. Moreover, there are gaps in spatial accessibility that need to be addressed, one of which is the lack of a comprehensive transport network. With respect to developing nations like India, it is evident that people are forced to travel beyond their neighborhood for health activity that suits and fulfill their needs. However, constraints remain critical aspects in health care planning and interventions. Failure to consider or overcome constraints in modeling approaches might lead to the ‘do-nothing’ scenario. Therefore, to achieve equity in meeting varied health care service needs, new and affordable facilities have to be provisioned at the earliest. Such issues have to be addressed by governing bodies through upcoming urban and health care policies.
Notes
ASHA (Accredited Social Health Activist) is a community link volunteer provisioned by NUHM as one ASHA for 1000–2500 urban poor population covering about 200 to 500 households. Similarly, outreach sessions should be organized in the area of every ANM (Auxiliary Nurse Midwife) on a weekly basis in coordination with AWW (Anganwadi Worker). These community volunteers are in direct contact with the people (rural and urban poor) in delivering health care.
The basic health care delivery system in India is implemented through the Primary Health Care Centers (PHCs). NUHM provisions one PHC for every 50,000 population and one CHC (Community Health Center) for every 0.25 million population (0.5 million for metros).
References
Allen, A. (2003). Environmental planning and management of the peri-urban interface: perspectives on an emerging field. Environment and Urbanization, 15(1), 135–148. doi:10.1177/095624780301500103.
Babakus, E., & Mangold, W. G. (1992). Adapting the SERVQUAL scale to hospital services: an empirical investigation. Health Services Research, 26(6), 767–786.
Balarajan, Y., Selvaraj, S., & Subramanian, S. V. (2011). Health care and equity in India. The Lancet, 377(9764), 505–515. doi:10.1016/S0140-6736(10)61894-6.
Birkin, M., Clarke, G., & Clarke, M. P. (2002). Retail geography and intelligent network planning: Wiley.
Bohannon, R. W. (1997). Comfortable and maximum walking speed of adults aged 20—79 years: reference values and determinants. Age and Ageing, 26(1), 15–19. doi:10.1093/ageing/26.1.15.
Butt, M. M., & de Run, E. C. (2010). Private healthcare quality: applying a SERVQUAL model. International Journal of Health Care Quality Assurance, 23(7), 658–673. doi:10.1108/09526861011071580.
Conway, J. H., Burgiel, H., & Goodman-Strauss, C. (2008). The symmetries of things. AMC, 10, 12.
Coxeter, H. S. M. (1973). Regular polytopes: Courier Corporation.
Cromley, E. K., & McLafferty, S. L. (2011). GIS and public health: Guilford Press.
Dahiya, B. (2003). Peri-urban environments and community driven development: Chennai, India. Cities, 20(5), 341–352. doi:10.1016/S0264-2751(03)00051-9.
De Costa, A., & Diwan, V. (2007). ‘Where is the public health sector?’: Public and private sector healthcare provision in Madhya Pradesh, India. Health Policy, 84(2–3), 269–276. doi:10.1016/j.healthpol.2007.04.004.
Devadasan, N., Seshadri, T., Trivedi, M., & Criel, B. (2013). Promoting universal financial protection: evidence from the Rashtriya Swasthya Bima Yojana (RSBY) in Gujarat, India. Health Research Policy and Systems, 11(1), 29.
Duggal, R. (2001). Evolution of health policy in India. Centre for Enquiry into Health and Allied Themes.
Erkut, E., & Neuman, S. (1989). Analytical models for locating undesirable facilities. European Journal of Operational Research, 40(3), 275–291. doi:10.1016/0377-2217(89)90420-7.
Gesler, W. M., Hayes, M., Arcury, T. A., Skelly, A. H., Nash, S., & Soward, A. C. M. (2004). Use of mapping technology in health intervention research. Nursing Outlook, 52(3), 142–146. doi:10.1016/j.outlook.2004.01.009.
Gnaneshwar, V. (1995). Urban policies in India — Paradoxes and predicaments. Habitat International, 19(3), 293–316. doi:10.1016/0197-3975(94)00076-E.
Hales, C. T. (2001). The Honeycomb Conjecture. [journal article]. Discrete & Computational Geometry, 25(1), 1–22. doi:10.1007/s004540010071.
Husain, Z. (2011). Health of the national rural health mission. Economic and Political Weekly, 46(4), 53–60.
Iyer, A., Sen, G., & George, A. (2007). The Dynamics of Gender and Class in Access to Health Care: Evidence from Rural Karnataka, India. International Journal of Health Services, 37(3), 537–554. doi:10.2190/1146-7828-5l5h-7757.
Jana, A., Harata, N., Kiyoshi, T., & Ohmori, N. (2014). Exploring the role of social interactions and supports in overcoming accessibility barriers while undertaking health tours in India. Social Work in Public Health, 29(4), 350–367. doi:10.1080/19371918.2013.825895.
Kilbourne, W. E., Duffy, J. A., Duffy, M., & Giarchi, G. (2004). The applicability of SERVQUAL in cross‐national measurements of health‐care quality. Journal of Services Marketing, 18(7), 524–533. doi:10.1108/08876040410561857.
Knoblauch, R., Pietrucha, M., & Nitzburg, M. (1996). Field Studies of Pedestrian Walking Speed and Start-Up Time. Transportation Research Record: Journal of the Transportation Research Board, 1538, 27–38. doi:10.3141/1538-04.
Kontgis, C., Schneider, A., Fox, J., Saksena, S., Spencer, J. H., & Castrence, M. (2014). Monitoring peri-urbanization in the greater Ho Chi Minh City metropolitan area. Applied Geography, 53, 377–388. doi:10.1016/j.apgeog.2014.06.029.
Luo, W., & Whippo, T. (2012). Variable catchment sizes for the two-step floating catchment area (2SFCA) method. Health & Place, 18(4), 789–795. doi:10.1016/j.healthplace.2012.04.002.
Mehta, D., & Pathak, P. (1998). Financing of Urban Services in India: A Case for Appropriate Pricing and Cost Recovery. Habitat International, 22(4), 487–502. doi:10.1016/S0197-3975(98)00028-9.
MoHFW (2002). National Health Policy - 2002. New Delhi, India.
MoHFW. (2012). National Urban Health Mission. New Delhi: Ministry of Health & Family Welfare, Government of India.
MoHFW (2014). Rural Health Statistics 2014–15. In S. Division (Ed.). New Delhi: Ministry of Health and Family Welfare.
MoHFW (2015). National Health Mission: State Program Implementation Plans. (Vol. 2015).
MoSPI (2015). Key Indicators of Social Consumption in India Health. New Delhi, India.
Nandi, S., Kanungo, K., Khan, M. H., Soibam, H., Mishra, T., & Garg, S. (2012). A study of Rashtriya Swasthya Bima Yojana in Chhattisgarh, India. [journal article]. BMC Proceedings, 6(1), 1–2. doi:10.1186/1753-6561-6-s1-o5.
Narayana, D. (2010). Review of the Rashtriya Swasthya Bima Yojana. Economic and Political Weekly, 45(29), 13–18.
Patel, A., Koizumi, N., & Crooks, A. (2014). Measuring slum severity in Mumbai and Kolkata: A household-based approach. Habitat International, 41, 300–306. doi:10.1016/j.habitatint.2013.09.002.
Patil, A. V., Somasundaram, K. V., & Goyal, R. C. (2002). Current health scenario in rural India. Australian Journal of Rural Health, 10(2), 129–135. doi:10.1046/j.1440-1584.2002.00458.x.
Peters, D. H., Rao, K. S., & Fryatt, R. (2003). Lumping and splitting: the health policy agenda in India. Health Policy and Planning, 18(3), 249–260. doi:10.1093/heapol/czg031.
Pirkul, H., & Schilling, D. A. (1991). The maximal covering location problem with capacities on total workload. Management Science, 37(2), 233–248.
Rahman, S.-U., & Smith, D. K. (2000). Use of location-allocation models in health service development planning in developing nations. European Journal of Operational Research, 123(3), 437–452. doi:10.1016/S0377-2217(99)00289-1.
Rajasekhar, D., Berg, E., Ghatak, M., Manjula, R., & Roy, S. (2011). Implementing health insurance: the rollout of Rashtriya Swasthya Bima Yojana in Karnataka. Economic and Political Weekly, 46(20), 56–63.
Reddy, K. S., Patel, V., Jha, P., Paul, V. K., Kumar, A. K. S., & Dandona, L. (2011). Towards achievement of universal health care in India by 2020: a call to action. The Lancet, 377(9767), 760–768. doi:10.1016/S0140-6736(10)61960-5.
Rumbach, A. (2014). Do new towns increase disaster risk? Evidence from Kolkata, India. Habitat International, 43, 117–124. doi:10.1016/j.habitatint.2014.03.005.
Scott, A. J. (1970). Location-Allocation Systems: A Review. Geographical Analysis, 2(2), 95–119. doi:10.1111/j.1538-4632.1970.tb00149.x.
Selvaraj, S., & Karan, A. K. (2009). Deepening Health Insecurity in India: Evidence from National Sample Surveys since 1980s. Economic and Political Weekly, 44(40), 55–60.
Sengupta, U. (2006). Government intervention and public–private partnerships in housing delivery in Kolkata. Habitat International, 30(3), 448–461. doi:10.1016/j.habitatint.2004.12.002.
Sengupta, A., & Nundy, S. (2005). The private health sector in India: Is burgeoning, but at the cost of public health care. BMJ: British Medical Journal, 331(7526), 1157–1158.
Shariff, S. S. R., Moin, N. H., & Omar, M. (2012). Location allocation modeling for healthcare facility planning in Malaysia. Computers & Industrial Engineering, 62(4), 1000–1010. doi:10.1016/j.cie.2011.12.026.
Shaw, A. (2005). Peri-Urban Interface of Indian Cities: Growth, Governance and Local Initiatives. Economic and Political Weekly, 40(2), 129–136.
Tomintz, M. N., & Garcia-Barrios, V. M. (2014). Location–Allocation Planning. In The Wiley Blackwell Encyclopedia of Health, Illness, Behavior, and Society: Wiley.
Travis, P., Bennett, S., Haines, A., Pang, T., Bhutta, Z., Hyder, A. A., et al. (2004). Overcoming health-systems constraints to achieve the Millennium Development Goals. The Lancet, 364(9437), 900–906. doi:10.1016/S0140-6736(04)16987-0.
van Doorslaer, E., O’Donnell, O., Rannan-Eliya, R. P., Somanathan, A., Adhikari, S. R., Garg, C. C., et al. (2006). Effect of payments for health care on poverty estimates in 11 countries in Asia: an analysis of household survey data. The Lancet, 368(9544), 1357–1364. doi:10.1016/S0140-6736(06)69560-3.
Wagstaff, A. (2007). The economic consequences of health shocks: Evidence from Vietnam. Journal of Health Economics, 26(1), 82–100. doi:10.1016/j.jhealeco.2006.07.001.
WHO (1986). Healthy Cities. http://www.euro.who.int/en/health-topics/environment-and-health/urban-health/activities/healthy-cities. Accessed 18th May 2016.
WorldBank (2016). World Development Indicators: Health expenditure (% of GDP). http://data.worldbank.org/indicator/SH.XPD.TOTL.ZS. Accessed 18th May 2016.
Acknowledgments
The authors would like to thank the Editor and the two anonymous reviewers for their valuable and constructive comments, which have led to a significant improvement in the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Basu, R., Jana, A. & Bardhan, R. A Health Care Facility Allocation Model for Expanding Cities in Developing Nations: Strategizing Urban Health Policy Implementation. Appl. Spatial Analysis 11, 21–36 (2018). https://doi.org/10.1007/s12061-016-9208-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12061-016-9208-0