Abstract
India, the largest populated country in the world with a diversified lifestyle based on regions and economic conditions of the people, provides primary health care for all its citizens which is vital to any government. The accessibility to health infrastructure in rural areas is challenging for the government. The national-level guidelines and policies are in place for developing the infrastructure. Still, there is a need to study the location and its accessibility to health infrastructure. A spatial composite index would help quantify health infrastructure distribution over an area. The health infrastructure inventory like government hospitals, medical stores, blood banks, laboratories and anganwadi centres are primary indicators. The roads and built-up extents support infrastructure indicators that influence access to health infrastructure. The geolocation and its distribution of indicators across the study area in a GIS environment have the uttermost significance. The quantification of geo-located infrastructure is vital to understand its availability and shortfalls. The paper attempts to showcase the methodology of analysing the geospatial outputs representing the infrastructure variability in the Andhra Pradesh state. The Euclidean distance algorithm enabled to quantify the distribution of health infrastructure. Moreover, integrating a multicriteria decision-making approach of different health infrastructure indicators has brought out the spatial accessibility index. The classification of the variability of the spatial accessibility index into five different categories allows policy-maker to concentrate on the areas of poor variability for planning and building developmental goals. The classified accessibility index over the built-up extent provided the goals of immediate concentration when its impact of variability over the population and households was analysed.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Health is a basic need to lead a quality life. The healthcare infrastructure must be within the reach of every citizen. Governments face several challenges in extending health facilities to the entire geographical extent of a state or country (Myers, 2020). The health infrastructure is one of the critical indicators for understanding the healthcare delivery system. It also signifies the investments and priority to create the infrastructure involving the public and private sectors (NHP, 2019). There are adequate health infrastructures like hospitals, medical stores, laboratories and blood banks to determine the major health indicators. There is no denying that India has achieved significant progress in providing health infrastructure to its population (Mann, 2020). However, it is necessary to understand whether it is evenly distributed across the entire geographical extent of the state or country. Health care is a well-articulated goal universally for global, national and state governments.
Under sustainable development goal (SDG) No. 3, good health and well-being are commitments towards the global effort to strengthen treatment and health care. The use of GIS would help in the effective implementation of health infrastructure on the ground. Researchers worldwide have worked on developing and applying various analytical methods to assess health infrastructure. GIS, as a tool, can support decision-makers in the public healthcare system in dealing with planning (Ghorbanzadehet & Blaschke, 2018). Using satellite image-derived data in a GIS environment linked to health information can help obtain the shortfall of infrastructure localities (Ramzi et al., 2017).
Healthcare delivery applications integrated with strategic decision-making processes are essential in planning (Khashoggi & Murad, 2020; Higgs & Gould, 2001). The study on multiple-criteria decision analysis framework using the analytic hierarchy process (Sadler et al., 2019) would help understand neighbourhood relative promoting qualities on a 0–100 scale. There are studies to examine the relationship between health infrastructure and health indicators of Andhra Pradesh for the period of 1980–2010 with tabular data and developed a health infrastructure index focusing on hospitals, nursing homes, beds, doctors and government hospitals using a double log simple regression model. They investigated health sensitivity in response to health infrastructure, estimating its elasticity coefficient (Lakshmi & Sahoo, 2013). With the diversified lifestyle and economic conditions of the people, the government in India faces challenges in providing good quality primary health care for all its citizens. Many guidelines and policies are in place for developing the infrastructure. Still, there is an acute need to study the accessibility of health infrastructure using geospatial techniques. The study must also consider different types of health infrastructures, the spatial distribution and their impact on the population over the settlement areas of the state or country.
The Objective of the Study
The densely populated areas such as cities and big towns have the most health infrastructure facilities. The government health departments try to establish health infrastructure facilities in small towns. There is always a need to study the location and distribution of different health infrastructure facilities, along with associated features which play an essential role in assessing the accessibility to the population and households in the area or locality.
The study must give a holistic assessment that provides a comprehensive measure of accessibility by considering multiple destinations and resources simultaneously. It must consider various factors such as distance from health infrastructure, road transport networks and location of facilities. The assessment must help in capturing the overall accessibility to health infrastructure.
The main objective is to develop a methodology and build a spatial accessibility index that quantifies the distribution of government health infrastructure using geospatial techniques. Further more, develop geospatial data to determine the locations of very good to poor health infrastructure and determine district-level analysis, the impact on the population and households.
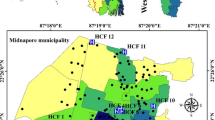
Study Area and Data
The study was carried out for Andhra Pradesh, India, covering an area of approximately 163,000 sq km, as shown in Fig. 1. The state of Andhra Pradesh stands seventh biggest in the area and the tenth most populous state in the country. The state consists of 13 districts. Further, each district consists of multiple mandals or blocks, and each mandal has multiple villages. The spatial analyses were carried out at the pixel level.
The selection of indicators is vital in data preparation in a geographical information system (GIS) environment. The best method to build the GIS-based indicators data is through field data collection. Seven indicators influence the spatial accessibility index for government health infrastructure. The type of government hospital is the first and most crucial indicator influencing the population's health. There are different types of hospitals which are considered sub-indicators, like super-speciality hospitals, multi-speciality hospitals, general hospitals, area hospitals, community hospitals, primary health centres, urban health centres and other hospitals. The medical store is the second indicator consisting of wholesale medical stores, retail medical stores, wholesale cum retail medical stores and medical stores in hospitals as sub-indicators under the medical store as indicators. The sub-indicators under the blood bank consist of independent blood banks, blood storage centres and blood banks or storage centres in the hospitals. These are considered the third important indicator. The other four indicators are laboratory, anganwadi centres, built-up areas and road information. The information like hospitals, medical stores, blood banks, laboratories and anganwadi centres are captured using the mobile app. The built-up extent information is derived using satellite-based remote sensing technique using Indian Remote Sensing Satellite (IRS) Linear Imaging Self-Scanning Sensor III (LISS-III) data sets of 2016–17, which are mapped on a 1:50,000 scale as part of the third cycle of the Natural Resources—Census (NR—Census) Land Use and Land Cover (LULC) project.
The land use and land cover classes were interpreted based on image parameters, viz. tone, texture, pattern, size, shape and association, for delineating the levels I and II classes by heads-on (onscreen) digitisation methods (Saxena et al., 2019). The road data set with six different types of roads was collected from the Open street map portal. The LULC is visually interpreted on a 1:50,000 scale using LISS-3 data @ 23.5 m, and 3 × 3 pixels are considered to identify the features. The GPS accuracy in the mobile app is restricted to 20 m. Considering the above statements on pixel size and the number of pixels to identify the feature and GPS accuracy of the mobile app data, the output pixel size is fixed at 100 m.
Methodology
The indicators like the hospitals, medical stores, blood banks and roads have a set of sub-indicators representing their types influencing the study. The geospatial representation gives a different perspective to identify the location variability of different types of hospitals and their impact on an area. Five of seven indicators were considered to capture information using mobile field data collection methods. With the advent of information and communication technologies, the gadgets such as smartphones capture data. The mobile apps were designed and developed to capture three primary data from the field: location information, photographs and valued-added information about the infrastructure. The location information is captured using the location-based service of smartphones GPS. The health infrastructure parameters are captured in the form of attribute information, and a pictorial representation of health infrastructure is captured using the smartphone camera (Annamalai et al., 2015). The captured data are pushed to a centralised database server through web services using an internet facility utilising mobile data or USB or WiFi connectivity. The data are retrieved using a geo-portal to validate its correctness w.r.t. the attributes and photographs of the health infrastructure (Annamalai et al., 2022; Nowak et al., 2020). The process of capturing attributes with geolocation parameters and photographs together is recorded as part of field data collection and is also called evidence-based geo-tagging.
Spatial Accessibility Index (SAI) for Health Infrastructure
The mobile app data in the central repository are retrieved to prepare the GIS layers representing point features. Similarly, the road and built-up extent data sets are represented in polylines and polygons, respectively. These feature data sets are used to compute the spatial accessibility index for health infrastructure. They are computed using the distance-to-source approach, and it is derived using proximity analysis through the spatial Euclidean distance algorithm with output in raster data format.
The Euclidean distance formula is represented as:
where as(q, p) are two points in Euclidean n-space.
(qi, pi) are Euclidean vectors, starting from the origin of the space.n is n-space
The spatial Euclidean distance data represent a 0-pixel value over the health infrastructure, and the distance radially increases to the farthest pixel. The analytical hierarchal process (AHP)-based multicriteria decision-making technique is used to derive the spatial index of 0 to 100 to address all 7 indicators through proximity analysis that brings out infrastructure factors in the study (Jeganathan et al., 2011; Kumar & Shaikh, 2013). The distance raster layers of each sub-indicator and indicators need to rescale their values to a common baseline for AHP analysis. The process of rescaling the distance raster is carried out using a simple map algebra equation.
The values in the rescaled raster layer represent a pixel value of 100 over the health infrastructure and 0 to its farthest pixel. The relative importance of criteria and alternatives assesses pairwise comparisons. For the n criteria, compare each criterion with every other criterion and assign a preference score based on their relative importance. The preferences are typically expressed on a numerical scale, 1–9, where 1 represents equal importance, and 9 represents extreme importance. It is necessary to derive a score for each sub-indicator as per their importance concerning the health infrastructure's role in the system. Saaty's nine-point scoring scale is used to develop the pairwise comparison matrix, as shown in Table 1.
The matrix is constructed based on pairwise comparisons, with rows representing the criteria and columns representing alternatives. The matrix contains the preference scores assigned to each set of indicators or sub-indicators. The weights are derived by calculating the geometric mean of the preference scores in each column of the pairwise comparison matrix. This step helps quantify the relative importance of each criterion. The consistent matrix must be a significant cause by a standard scale; each element has weight, which does not change when compared to another element, as shown in Eq. 3.
1, \(a12\)- the intensity of importance. \(w1\) to \(wn\) weights of each indicator or sub-indicator
The eigenvector (λmax) essentially multiplies the weights of each criterion by the performance scores or evaluations of the alternatives to obtain weighted scores. Sum up the weighted scores to obtain a final score for each alternative. Every criterion gets its weight to represent its importance. The higher value represents the more important criteria in the overall decision. The quality of the pairwise comparison matrix and its weights are evaluated using the consistency index and the consistency ratio.
The consistency index (CI) is calculated from the given equation as
The consistency ratio (CR) is calculated by dividing the consistency index (CI) by the random index (RI), which must be less than 1/10th, and then the comparison is consistent and acceptable. The RI is considered based on Table 2 (Do & Kim, 2012).
The weighted sum tool in GIS software is used to compute SAI through overlay analysis for various GIS layers representing sub-indicators and indicators. The SAI output is a continuous raster data set. An unsupervised machine learning algorithm generates discrete data to demarcate the boundaries of very good infrastructure class to the poor class. The improved sequential ordering (ISO) cluster classifier algorithm is used to classify the spatial accessibility index information. The ISO cluster is an unsupervised density-based clustering algorithm that partitions data pixels into clusters based on their density. The output converts a continuous index into a discrete group of classes. The discrete group of classes are categorised from very good to poor classes. The spatial analysis techniques are used to derive the approximate percentage of area under each discrete class. The census information, such as population and households, is integrated with the administrative boundary layers featuring state, district, block and village for analysing the impact of population and households using zonal statistics analysis of health infrastructure classes, as shown in Fig. 2.
Results and Discussion
Data Collection and Generation of Spatial Data
The data collection and preparation to develop a composite spatial accessibility index addressing health infrastructure were carried out using different data sources. Towards this, three mobile applications were developed to collect field data that capture locations of hospitals, medical stores, laboratories, blood banks and anganwadi centres. The screenshot of the Bhuvan Vidya mobile app to capture hospital data is shown in Fig. 3 and separate solutions to capture anganwadi and medical stores-related information. The built-up area information is extracted from a land use/land cover map of 1:50,000 scale in vector format, which is interpreted using remotely sensed multi-temporal satellite data sets of 2016–17. The OSM road layer represents roads in six levels.
Government hospitals are categorised into eight types. Each type has its importance and role to play in the well-being of its population. The developed mobile app facilitates to geo-tag the buildings of health infrastructure with photographs. The app has a provision to capture attribute details like hospitals with its type like super-speciality, multi-speciality, general, area, community, primary health centre, urban health centre, and others. Information on the timings of the service and the availability of in-house—blood banks/blood storage centres/medical stores are also collected.
A total of 1644 hospital infrastructures were geo-tagged using the mobile app. The moderation activity was carried out to validate the values in attribute fields correlated with photographs and other sources of information. The number of hospitals under different types is shown in Table 3.
The information on medical stores, laboratories and blood banks was captured using Bhuvan Drugs mobile app by field district-level nodal officers and geo-tags were validated by moderators, as mentioned in Table 4. Apart from dedicated laboratories in the state, the minimum basic types of tests are carried out in the PHC. The anganwadi centres provide elementary healthcare facilities. They are part of the public healthcare system, educating the population on healthcare, well-being and preschool activities. There are 53,151 anganwadi centres distributed well across Andhra Pradesh.
Computation of Spatial Infrastructure Index
The SAI computation is carried out using an AHP-based pairwise comparison technique. The weights of each indicator are derived. The Euclidean distance algorithm calculates spatial distance maps from point, line, or polygon information. The distance maps are generated as a raster image for each sub-indicator and indicator. Each pixel is considered for distance computation and depicted in pixel value. The pixel value represents the distance from the nearest source of the health infrastructure facility. The generation of spatial infrastructure index for medical store or pharmacy is discussed in detail. The pixel values over the medical store locations represent 0-pixel values on the distance raster image. The pixels far from the medical store location would represent the radial distance of the nearest medical store.
The medical store or pharmacy GIS layer is prepared from a geo-tagged data set categorised into five types such as retail sale (Retail), wholesale (Wholesale), retail and wholesale (BothRW), pharmacy in hospital (Inhouse) and other pharmacy stores (Other). The distance rasters are generated based on the type of medical store, and the raster layers are shown in Fig. 4. The maximum pixel values are extracted from each distance raster image and rounded to the next higher value called maximum threshold distance. As stated in the Methodology section, the rescaling or ranking process is carried out to bring all the layers to a common baseline.
The pairwise comparison matrix is derived using Saaty's nine-point weighing scale for all indicators or sub-indicators. In connection to the medical store, the “Inhouse—Inhouse” class cannot be differentiated between them. So its relative weight is stated as 1, whereas the “Inhouse-BothRW” do have differences between them. So it is rated in between equals and moderate importance over one another when compared with the rest of the sub-indicators. Hence it is stated as 2. When it comes to BothRW-Inhouse, it is the inverse of Inhouse-BothRW. Hence it is stated as ½.
The corresponding criteria weights are computed as stated in the methodology. Likewise, all the relative comparison values and criteria weights are derived and shown in Table 5.
The consistency measurements are computed by multiplying the matrix to get the resultant matrix. The average value of the resultant matrix is 5.108, called the eigenvector (λmax). The consistency ratio (CR) is calculated by dividing the consistency index (CI) by the random index (RI), which must be less than 1/10th. The comparison is consistent and acceptable (Do & Kim, 2012). The consistency index (CI) is calculated as = (λ max—n) / (n− 1) = 0.027, consistency ratio (CR) = 0.027/1.12 = 0.024. Likewise, pairwise comparison matrixes are developed for hospitals, blood banks and roads. The criteria weights, the consistency index and the consistency ratio, are computed for all indicators, with sub-indicators addressing hospitals, medical stores, blood banks and roads, as shown in Table 6.
The pairwise comparison matrix is computed for indicators such as hospitals, medical stores, blood banks, roads, laboratories, built-up and anganwadi centres. The rescaled layers like laboratories, built-up and anganwadi are directly used in the composite index computation, whereas they do not have sub-indicators. The weighted sum function of overlay analysis is used to compute the composite index with criteria weights mentioned in Table 7. The minimum and maximum representation index values of the spatial accessibility index are 36.6 and 95.04, respectively, in Fig. 5.
The spatial accessibility index data for health infrastructure is classified using an unsupervised classification technique. The ISO clustering algorithm is used to classify SAI data into five classes, with the 20 iterations considered to define the classes. These five classes are categorised as very good (with a higher value), good, average, below-average and poor class (with a lower value). Every 100 m x 100 m pixel is defined with one of the five classes, as shown in Fig. 6. The percentage of area is computed considering the entire geographical extent of the Andhra Pradesh state. Further, district-wise statistics were generated for the five classes to assess the status of district-level health infrastructure. The zonal statistics operation is used to bring out the values based on the sum of pixels falling in a particular class under each zone.
The analysis is carried out for the built-up area class separately. The total area of the Andhra Pradesh state is 162,975 sq km, out of which 5156.41 sq km is the built-up area which amounts to 3.16%. Based on the classification of the spatial accessibility index, the health infrastructure over the built-up area in the state is 53.0%, 24.2%, 15.2%, 6.5% and 1.1%, respectively. The built-up area of 53% and 24.2% is under the very good and good categories, whereas 1.1% and 6.5% fall under poor and below-average categories, where health infrastructure development must improve, as shown in Fig. 7.
Considering the even distribution of population and households across built-up areas at the village level, the raster-based overlay analysis is carried out to derive the total population percentage under each class. The impact of the population considering 4,68,64,156 as per the 2011 census for different classes is computed. The percentage of the population from very good to poor is represented as 54.82%, 24.3%, 13.67%, 6.06% and 1.16%, respectively. Further, the impact on the households considering 1,20,40,405 as per the 2011 census for different classes is computed. The percentage of households from very good to poor is 55.73%, 24.45%, 13.16%, 5.61% and 1.04%, respectively. The study has revealed that 5.61% and 1.04% of households and 6.06% and 1.16% of the population fall under below-average and poor categories of accessibility to health infrastructure. The study suggests that the government look into these areas and develop a plan.
The district-wise statistics are derived from identifying the focus built-up area considering the districts concerned are Anantapur, Chittoor and Kurnool, with poor and below-average classes falling below the average state level. Whereas districts like Srikakulam need to improve in small pockets, other districts have good and very good health infrastructure classes, as shown in Fig. 8.
Conclusions
The spatial distribution of health infrastructure is vital for any government while dealing with different healthcare challenges and situations. The good spatially distributed infrastructure enables access within the shortest possible distance and effort, which would be vital for people with critical health conditions. The distribution of health infrastructure indicates the healthcare delivery system. It describes the essential support of public health activities and welfare mechanisms in a state or country. The study of the spatial accessibility index for health infrastructure quantifies its distribution over the study area. The identification of indicators and their sub-indicators is a crucial part.
Further generating data sets, the quality of data sets to build a spatial accessibility index over large geographical extents is challenging. The use of integrated solutions that utilise the Geo-ICT framework to capture data from the field and the use of information-derived outputs from remote sensing and other sources are some of the methods used in data creation that have proven very effective. The information collected using Geo-ICT methods requires complete representation of the field in the form of geo-tagging, failing which would act as one of the study's limitations. The enhancements in data collection can lead to capturing missing geo-tags to enrich the quality of the result. The research uses the Euclidean distance algorithm to quantify the distribution. The analytical hierarchical process method has helped make complex decisions by breaking them down into a hierarchical structure. The pairwise comparison matrix helped compare the relative importance of different indicators and sub-indicators. The consistency ratio check calculation helped ensure the validity of the decision-making process in pairwise comparison. The generation of the spatial accessibility index using indicators and sub-indicators in a GIS environment helped in giving a perspective view of the areas of interest where more concentration is required to develop the health infrastructure.
The spatial accessibility index identified areas with poor and below-average health infrastructure facilities. The SAI enabled health planners to understand geographic imbalances in accessing them. The information can guide the establishment of new facilities or the redistribution of existing resources to underserved areas. The integration of population and households to classified SAI data can help policymakers identify areas and populations experiencing unequal access to government services. The valuable derived information can be interventions that aim to reduce health disparities and improve social justice. The analysed data helped equitable access to quality health care for vulnerable communities, low-income groups and the remotest rural areas. The analysis is helpful during the public health emergencies like the COVID-19 situation.
The study is a way forward for the government department to effectively manage and improve government health infrastructure in the state or the country as a whole.
It is a reliable tool for the decision support system to prioritise healthcare infrastructure planning and investments and regional healthcare recruitment policies. It also helps in reducing the household out-of-pocket expenditure on accessing health care. It creates and locates the need-based right to healthcare assets and human resources for the right geographical area for a restorative, rehabilitative and preventive healthcare system. The mapping of the hospitals, medical stores, laboratories and blood banks/storage centres is dimensions related to health infrastructure. The fifth dimension is the distance in the GIS interface that would give a paradigm shift in access to the healthcare system and epidemiological studies.
References
Annamalai, L., Arulraj, M., Nagamani, P.V. & Jai, Sankar. G. (2022). Geo-information communication technology (Geo-ICT) framework to prevent spread of corona virus disease (COVID-19). Journal of the Indian Society of Remote Sensing, 50(6), 1163–1175. https://doi.org/10.1007/s12524-022-01498-8
Annamalai, L., Sarathkumar, V.V., Raikumar, M.V. (2015). Bhuvan Mobile Applications, Bhuvan Documents, NRSC-RSAA-ASDCIG-Aug-2015-TR-731. https://bhuvanapp1.nrsc.gov.in/2dresources/documents/5_Bhuvan_Mobile_Applications.pdf. Accessed: 13th Oct 2021.
Do, J. Y., & Kim, D. K. (2012). AHP-Based evaluation model for optimal selection process of patching materials for concrete repair: focused on quantitative requirements. International Journal of Concrete Structures and Materials, 6, 87–100. https://doi.org/10.1007/s40069-012-0009-9
Ghorbanzadeh, F. B., & Blaschke, T. (2018). An interval matrix method used to optimize the decision matrix in AHP technique for land subsidence susceptibility mapping. Environmental Earth Sciences, Worldcat, 77, 584. https://doi.org/10.1007/s12665-018-7758-y
Higgs, G., & Gould, M. (2001). Is there a role for GIS in the “new NHS”? Health & Place, 7, 247–259. https://doi.org/10.1016/S1353-8292(01)00014-4
Jeganathan, C., Roy, P. S., & Jha, M. N. (2011). Multi-objective spatial decision model for land use planning in a tourism district of India. Journal of Environmental Informatics, 1, 15–24. https://doi.org/10.3808/jei.201100182
Khashoggi, B. F., & Murad, A. (2020). Issues of healthcare planning and GIS: A review. ISPRS International Journal of Geo-Information, 9(6), 352. https://doi.org/10.3390/ijgi9060352
Kumar, M., & Shaikh, V. (2013). Site suitability analysis for urban development using GIS based multicriteria evaluation technique: A case study of Mussoorie municipal area, Dehradun district, Uttarakhand, India. Journal of the Indian Society of Remote Sensing, 41, 417–424. https://doi.org/10.1007/s12524-012-0221-8
Lakshmi, S. T., & Sahoo, D. (2013). Health infrastructure and health indicators: The case of Andhra Pradesh, India. IOSR Journal of Humanities and Social Science, 6(6), 22–29. https://doi.org/10.9790/0837-0662229
Mann, K. (2020). An analysis of healthcare infrastructure in India. Indian Journal of Applied Research, 10(2). https://doi.org/10.36106/ijar
Myers, J. (2020). India is now the world’s 5th largest economy, World Economic Forum. Accessed from https://www.weforum.org/agenda/2020/02/india-gdp-economy-growthuk-france/. Accessed 24 Sept 2020.
NHP, National Health Profile (2019). Central Bureau of Health Intelligence, Directorate General of Health Service, Govt. of India, 14th Issue. http://www.cbhidghs.nic.in/WriteReadData/l892s/8603321691572511495.pdf. Accessed 13 Oct 2021.
Nowak, M. M., Dziób, K., Ludwisiak, Ł, & Chmiel, J. (2020). Mobile GIS applications for environmental field surveys: A state of the art. Global Ecology and Conservation, 23, e01089. https://doi.org/10.1016/j.gecco.2020.e01089
Ramzi, A. I., & El-Bedawi, M. A. (2019). Towards integration of remote sensing and GIS to manage primary health care centers. Applied Computing and Informatics, 15(2), 109–113. https://doi.org/10.1016/j.aci.2017.12.001
Sadler, R. C., Hippensteel, C., Nelson, V., Greene-Moton, E., & Furr-Holden, C. D. (2019). Community-engaged development of a GIS-based healthfulness index to shape health equity solutions. Social Science Medicine, 227, 63–75. https://doi.org/10.1016/j.socscimed.2018.07.030
Saxena, M.R., Kumar, R., Chandra Mohan, J., Vijayan, D., Modi, M., Behera, D.K., Ganguly, K., Bhardwaj, R., Sahithi, V.S., Harshitha, P., & Begum. I. (2019). Natural Resource Census—Land Use / Land Cover Database for Dissemination through Bhuvan. https://bhuvanapp1.nrsc.gov.in/2dresources/thematic/LULC503/lulc.pdf
Acknowledgements
We sincerely thank Dr MV Ravikumar, Deputy Director, NRSC, for permitting us to conduct the research. We appreciate Dr Ravi Shankar A and his team facilitating the field survey data. Our appreciations are due to the field team of the Department of Anganwadi, Govt. of AP, for their contribution to field data collection. We sincerely thank Mr M Arulraj, Group Head, Bhuvan and Team Bhuvan for their support in developing the web services.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Conflict of interest: No potential conflict of interest among the authors of the research paper.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Lesslie, A., Vazeer, M. & Nagamani, P.V. Development of a Spatial Accessibility Index for Assessing Health Infrastructure Using AHP Approach: A Case Study of Andhra Pradesh State. J Indian Soc Remote Sens 51, 2007–2018 (2023). https://doi.org/10.1007/s12524-023-01739-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12524-023-01739-4