Abstract
Previous investigations have increased the knowledge about the pathological processes of inflammatory bowel diseases. Besides the complex organization of immune reactions, the mucosal epithelial lining has been recognized as a crucial regulator in the commencement and persistence of intestinal inflammation. As the intestinal epithelium is exposed to various environmental factors, the intestinal epithelial cells are confronted with diverse cellular stress conditions. In eukaryotic cells, an imbalance in the endoplasmic reticulum (ER) might cause aggregation of unfolded or misfolded proteins in the lumen of ER, a condition known as endoplasmic reticulum stress. This cellular mechanism stimulates the unfolded protein response (UPR), which elevates the potential of the endoplasmic reticulum protein folding, improves protein production and its maturation, and also stimulates ER-associated protein degradation. Current analyses reported that in the epithelium, the ER stress might cause the pathogenesis of inflammatory bowel disease that affects the synthesis of protein, inducing the apoptosis of the epithelial cell and stimulating the proinflammatory reactions in the gut. There have been significant efforts to develop small molecules or molecular chaperones that will be potent in ameliorating ER stress. The restoration of UPR balance in the endoplasmic reticulum via pharmacological intervention might be a novel therapeutic approach for the treatment of inflammatory bowel diseases (IBDs). This review provides novel insights into the role of chemical chaperone UPR modulators to modify ER stress levels. We further discuss the future directions/challenges in the development of therapeutic strategies for IBDs by targeting the ER stress.
Graphical Abstract
Figure depicting the role of endoplasmic reticulum stress-mediated inflammatory bowel disease and the therapeutic role of endoplasmic reticulum stress inhibitors in alleviating the diseased condition.

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Extreme inflammatory reactions trigger several chronic or autoimmune disorders, such as inflammatory bowel disease (IBD). Crohn's disease (CD) and ulcerative colitis (UC) are common IBDs involving the gastrointestinal tract (GI) with similar characteristics, such as fever and loss of weight, and several distinct colonic signs including the ulceration of the colonic mucosa, diarrhea, colon contraction, and motility dysfunction of the gastric tract [1, 2]. Disturbance in the balance of the mucosal immune responses causes overproduction of inflammatory chemokines and cytokines. As a result of this process, it causes protracted inflammatory reactions and irreplaceable tissue impairment. Earlier studies documented the mechanism involved in the development of IBD, but the etiology remains inadequately understood [3, 4]. The IBD therapeutic armamentarium comprises anti-inflammatory agents and immunomodulators, biologics with the specific aim of regulating the inflammatory process and immune responses [4]. Moreover, a subset of individuals with IBD does not respond to the above-mentioned pharmacological approaches although much progress has been achieved. Moreover, the previous data reported that downregulating inflammation of the mucosa leads to mucosal recovery and epithelial layer restoration, which is correlated with reducing the need for surgeries. The genome-wide association analysis (GWAA) showed the association of the epithelial layer of the intestine in maintaining the balance of the mucosa, and several animal studies also determined genes that are rigidly interlinked with the function of the epithelium. Cellular stress signaling comprising autophagy, oxidative stress, endoplasmic reticulum (ER) stress, and mitochondrial balance has been correlated with the differentiation and regulation of the various populations of epithelial cells in the gut [5]. In eukaryotic organisms, signals arising from the ER provoke a transcriptional sequence which helps the cells survive the condition of ER stress. The highly regulated reactions of the unfolded protein response (UPR) aid processing, folding, shipping, and degeneration of proteins emerging from the ER amid the stressed environment [6]. In mammalian cells, three specific UPR signaling cascades prevail that include pancreatic ER kinase (PERK), ER transmembrane inositol-requiring enzyme 1α and β (IRE1α and IRE1β), and activating transcription factor 6 (ATF6) [7]. IRE1 is considered the most maintained transducer of the ER among the reported signaling cascades. Of the two genes of the IRE1 cascade, IRE1α is noted to be a type I transmembrane protein comprising the endoribonuclease domain and a serine/threonine kinase domain in its cytosolic portion. Activated IRE1α splices a 26-basepair intron from an mRNA, which is known to encode a potent transcription factor called X-box-binding protein 1 (XBP1) as depicted in Fig. 1. According to the current reports, ER stress-activated UPR signaling is correlated with the synthesis of several proinflammatory compounds. XBP1 maintains the UPR signaling pathway by elevating the expression of the protein folding-related genes of ER, its secretion, and ER-associated protein degradation (ERAD) [8]. These cascades are usually maintained in an inactivated form by a chaperone known as GRP78 or also known as BiP (binding immunoglobulin protein). However, with the elevated ER stress, GRP78 is confined by the misfolded proteins, hence detaching the GRP78 from the sensing molecules which activates the signaling cascade to overcome the stress environment and to sustain the homeostasis [9]. Moreover, under protracted and acute ER stress, the UPR initiates the cascades, which leads to apoptosis [10]. Additionally, it was found that the cell survival rate during mild stress conditions is obtained via an intrinsic imbalance of proteins and mRNA that induces apoptosis and is correlated with those that promote protein folding and adaptations [9]. ER stress is correlated with various chronic syndromes such as inflammation involving obesity, diabetes, arthritis, and diverse forms of respiratory inflammation and IBD. Despite unclear evidence of the involvement of ER stress as a principle or secondary enforcer of chronic inflammation, alleviating the ER stress condition might have therapeutic potential [11]. Therefore, considering the misfolded or unfolded proteins and ER stress involvement in IBD, it is important to study the vital regulators of misfolded or unfolded proteins and the role of various ER stress inhibitors in alleviating the stress condition.
Endoplasmic Reticulum Stress-Induced Inflammation and Metabolic Disorders
Obesity is a condition characterized by stress and inflammatory reactions in the metabolic tissues, causing lower-grade local inflammation and chronic inflammation, which perform a principle role in blocking the signal from the insulin receptor and damaging intrinsic metabolic balance [12]. Congregating the data from the previous analyses signifies a clear association between metabolic diseases and inflammation. Analyses on obese mice have indicated that macrophages and adipocytes in adipose tissue produce several proinflammatory cytokines that could agitate insulin signaling [13]. Moreover, induction of the NF-κB–Iκ-B signaling cascade performs a significant function in obesity-stimulated inflammation and metabolic anomaly, involving impaired insulin activity. Of concern, the activity of obesity-stimulated proinflammatory cytokines is observed to be reduced in JNK-deficient mice, which as a result are being protected from type-2 diabetes and insulin resistance [14]. The analyzed data suggest that insulin signaling is precisely blocked by enhanced inflammation, which further contributes to the initiation of obesity and type-2 diabetes. The three pathways of the UPR interact with the maintenance of cellular lipogenesis and glucose metabolism and are responsible for the survival and death of β-cells. Reported evidence shows that ER stress can also correlate with inflammation, type-2 diabetes, and obesity. Currently, it was observed that XBP-1 deficient mice in β-cells show moderate glucose intolerance and hyperglycemia leading to a reduction in insulin secretion from β-cells [15]. All the above-discussed studies suggest that there is a strong communication among ER stress, inflammation, and metabolic disorders. Hence, further analysis will highlight this interspersed communication of cellular responses.
Association of ER Stress-Induced Inflammation in Inflammatory Bowel Disease
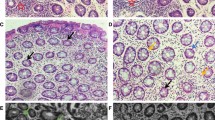
Current analysis from the reported literature suggests that dysregulation of UPR is associated with the pathogenesis of UC and CD, shown in Fig. 2 [9]. Intestinal epithelial cells (IECs) and the secretory cells such as goblet and Paneth cells [16], which are seen in the gut microbiome, are more prone to ER stress. Inflammation in the intestine is documented to be correlated with the UPR via the IRE1 cascades. The ER membrane protein IRE1α plays a significant role in coaxing the conversion of misfolded protein mass in ER into UPRs in the nucleus. IRE1α is a BiP-bound protein [17]. During ER stress, BiP protein binds to accumulated misfolded proteins in ER by detaching with IRE1α because of its higher affinity to the misfolded proteins [17, 18]. BiP-free IRE1α’s luminal domains self-associate, resulting in dimerization and autophosphorylation of the cytoplasmic kinase domain, and activate it [19]. Upon activation, IRE1α generates a new frame shift in the coding sequences to introduce a new termination codon in X-box binding 1 (XBP1) mRNA in a spliceosome-independent pathway [17]. The stable XBP1 transcription factor induces the expression of DnaJ, ERdj4, and ER degradation-enhancing α-mannosidase-like proteins, which are associated with ER-associated degradation as well as protein folding [20]. Removal of the IRE1 gene from the mouse intestinal epithelium led to enhanced protein accumulation correlated with ER stress and resulted in an increased sensitivity to dextran sulfate sodium (DSS)-stimulated colitis [21]. Moreover, the gene IRE1 governs the XBP-1 transcriptional factor, which maintains the expressions of UPR genes. In XBP-1 lacking intestinal tissues, the mediators of ER stress like activating transcription factor 4 (ATF4), GRP78, and CCAAT/enhancer-binding protein homologous protein (CHOP) are upregulated. The expression of CHOP, which was elevated in response to ER stress, was suggested to be accountable for the decrease in the count of Paneth cells in mice, lacking XBP-1 expression [22].
Secretory goblet cells, which are known to synthesize mucus, are responsible for the development of the intestine-microbiome association. The small intestine of XBP-1-lacking mice retain fewer goblet cells, possibly as the cells die because of apoptosis. Currently, studies have reported that single-nucleotide polymorphisms (SNPs) in the Muc2 gene are responsible for the development of spontaneous colitis. This gene encodes for mucin glycoprotein (GP), the crucial constituent in mucin, produced by the goblet cells. Furthermore, the analysis in the engineered mice strains (Eeyore and Winnie) showed that the goblet cells synthesized abnormal Muc2, stored less mucin, and also congregated Muc2 precursor in the ER lumen. The activity of GRP78 and splicing of XBP-1 mRNA was enhanced, signifying the existence of ER stress [23]. However, it is unclear whether the ER stress in the goblet cells is an outcome of accumulating inflammation or is caused by inflammation induced by protein aggregation in ER lumen that contributes to inflammation. So, either the stress in the goblet cells may be the reason for inflammation or it might be an effect of preceding inflammation. There is also evidence of an association between intestinal inflammation and UPR in humans. Deep sequencing analysis indicated new nonsynonymous SNPs (nsSNPs) in the coding region of the XBP-1 promoter. These analyses showed that nsSNPs occur only in individuals with IBD leading to a lack of the transactivation of XBP-1 targeted genes of UPR. This might lead to reduced UPR against ER stress [22]. According to the evidence, the induction of IBD is due to the hypomorphic activity of XBP-1 in the intestinal epithelium (IE). Hence, the appropriate UPR in IE appears to be pivotal for retaining intestinal balance. Insight into the development of inflammation-induced IBD is increasing, and the current analyses in animal models and individuals suffering from IBD signify that the mechanism of ER stress correlates the cellular stress to organ-related inflammation.
UPR: A Cause of Inflammation
A molecular pathway triggered by ER stress involves the activation of transcription factors. Particular enzymes are known to improve the conditions in the ER to restore balance, but if the stress condition is severe, it can activate inflammatory signaling or the apoptosis pathway. Among the numerous chaperones within the ER, GRP78 is known as a central chaperone leading to the initiation of UPR. Activation of UPR signaling results in the activation of various inter-related processes such as the expansion of ER and translational inhibition to alleviate the load of protein synthesis in the lumen to improve the stress condition. The gradual increase of UPR caused by the BiPs is considered a predictable way to quantify the stress condition in ER in human diseases as well as in experimental conditions of ER stress-mediated inflammation.
ER Stress-Induced Inflammatory Responses
There is a developing evidence reporting that a chronic low level of ER stress in some cell types can, in turn, make the cells resistant to the stimulation of inflammatory pathways and activation of NF-κB. The severity of the disease condition in several models such as Heymann nephritis, mesangioproliferative glomerulonephritis, and renal inflammation was decreased when preconditioning with certain ER stressors like thapsigargin or tunicamycin [24, 25].
ER stress is also known to contribute to inflammation by the NF-κB-independent pathway. Though the transcription factor CHOP induces apoptosis during the chronic condition of ER stress, in the absence of danger signals, the immune response may not be activated by apoptosis. However, studies have suggested that the antigen-presenting cells (APCs) can also be activated by signals transmitted by ER stress-induced apoptosis. The expression of cell surface calreticulin, an ER chaperone for glycoproteins (GP), was found to be increased because of retardation in the ER Ca2+ transport in the ER stress condition induced by the inducer thapsigargin. The process of phagocytosis by APCs was increased because of the elevated expression of cell surface calreticulin in cells undergoing ER stress. However, the co-exposure to Toll-like receptor (TLR)-ligand enhanced synthesis of inflammatory cytokines by the APCs [26]. Therefore, the earlier study reports indicate that various mechanisms can be activated by which ER stress can induce inflammation, among which many of them may rely on the ER stressor and the differentiated aspect of the ER stress-affected cells. Another theory is that many secretory proteins are synthesized by immune effector cells, which can undergo the condition of ER stress, for which a proper UPR is crucial for their maintenance.
Role of UPR Regulators in Inflammatory Bowel Disease (IBD) Pathogenesis
IRE1/XBP1 Signaling in Inflammatory Bowel Disease
The relation of IRE1/XBP1 in IBD was identified from the knockout of IRE1-β, which increased the BiP protein level in the mucus of the colon and susceptibility to a known experimental colitis inducer DSS [21, 27]. Corresponding to this study, IRE1-β knockout mice exhibited an impaired barrier function in the intestine and abnormal aggregation of mucin in goblet cells [28]. XBP1 is known as a crucial effector transcription factor of IRE1 signaling for responding to the condition of ER stress and unfolded protein aggregation. XBP1−/−(IEC) mice were experimented upon in further studies, and spontaneous progression of inflammation in the intestine and elevated sensitivity toward DSS was found in them. Furthermore, the intestinal barrier of XBP1−/− (IEC) mice has leakage, and invading pathogens were translocated to tissues such as the liver. This indicates an important function of XBP1 in maintaining the homeostasis of the intestinal and host immune reactions, which might be responsible for the development of IBD [9].
ATF6 Signaling in Inflammatory Bowel Disease
Chemically induced ER stress was found to involve ATF6α function for survival [29]. Transcriptional activation of ER chaperone genes such as BiP, Grp94, and P58IPK mediates the effect of ATF6α [30]. Moreover, Mbtps1 is a gene that encodes ATF6 activator S1P, whose mutation in mice revealed the function of ATF6 in the pathogenesis of IBD [31]. After DSS treatment, P58IPK knockout mice showed fewer goblet cells, higher penetration of inflammatory cells, and high mucosal impairment [32]. This evidence underlines the need for ATF6 signaling involvement in barrier activity of the intestine and further inflammatory reactions. With DSS treatment, these mice showed lower protein concentrations of Grp94 and BiP and impaired ATF6-induced UPR [31]. Understanding of how this pathway regulates the disease is currently lacking. Hence, for further studies, more in vivo analyses are required to find out a potential functional overlap between ATF6 and IBD.
PERK/CHOP Signaling in Inflammatory Bowel Disease
Transcription factor CHOP is involved in apoptosis and inflammatory reactions [33]. Reports on mice and IBD patients indicate increased expression of CHOP in the intestinal epithelium. A study done by Park et al. found that peroxisome proliferator-activated receptor γ, which is a negative regulator of NF-κB, can be suppressed by ER-stress-activated CHOP, therefore resulting in the NF-κB pathway activation. In the development of IBD, interleukin-8 (IL-8) expression enhanced by NF-κB, which is activated and translocated into the nucleus [34]. Besides being complementary to the regulation of cytokines, CHOP also leads to the induction of ROS (reactive oxygen species), penetration of macrophages, and development of IL-1β, which is involved in enhancing the apoptosis of epithelial cells, and leads to the advancement of colitis [35].
Reports suggest that IBD patients have a higher accumulation of IL-23 in the inflamed epithelium, reporting its effective function in the intestinal immune response. Also, anti-IL-23 antibodies have been developed and entered into the therapeutic armamentarium of IBD and rheumatic and dermatologic disorders [36]. CHOP protein was found to increase TLR (Toll-like receptor) stimulated IL-23 biosynthesis by elevating the binding to the IL-23 p19 promoter in ER stressed myeloid cells [37]. Future analyses are recommended to determine the regulation of the transcriptional mechanism associated with intestinal inflammation.
Inflammatory Factors as ER Stress Inducers
Combining the evidence from earlier studies shows that ER stress plays a crucial role in modulating inflammation. However, another concern is delineating how the inflammation and infection-associated factors in the microenvironment influence the processes of protein folding, UPR, and ER stress. Interestingly, very few studies directly relate to how specific inflammatory factors influence the ER stress and protein folding mechanism. One of the common factors known to enhance protein misfolding is oxidative stress, which can be induced by inflammatory cytokines and the oxidative stressors released by macrophages and activated granulocytes. Studies have shown that intracellular reactive oxygen species (ROS) can be triggered by TNF-α in fibrosarcoma cells, which can, in turn, lead to ER stress, but these cells showed protective behavior against the adverse effects of the ROS when preconditioned to ER stress by inducing protein misfolding [38]. The nitric oxide that is synthesized during inflammatory reactions has the potential to activate the UPR by hindering the synthesis of protein disulfide isomerases, resulting in misfolded protein accumulating within the ER [39]. Another mechanism by which the inflammatory cytokines may activate ER stress involves compelling elevated production of secretory protein, like the molecules synthesized during the defense of the mucosa, which are probably prone to misfolding. IL-10, which plays a pivotal role in retaining the intestinal balance, is known to regulate the UPR by hindering ATF6 nuclear translocation in a p38-mediated manner [40]. Though studies report that inflammatory factors can regulate ER stress, further detailed analyses are necessary to delineate how the inflammatory factors during infection affect ER stress.
Association of Environmental Factors and ER Stress Signaling in the Initiation of IBD
Accumulating evidence has shown that unreversed ER stress attributed to a variety of environmental factors might also be a prevailing factor in the induction of intestinal inflammation or a pivotal cause of the permanence of intestinal inflammation (Fig. 3). A number of inflammatory regulators have been observed to either increase or decrease ER stress. For instance, IL-10 has been documented to improve the condition of stress [40], whereas tumor necrosis factor is a crucial provoking factor [38]. Additionally, the conditions commonly encountered during the inflammatory phases are hypoxia and redox homeostasis, which are crucial promoters of ER stress [41]. Thus, imbalance among the anti- or proinflammatory regulators may be a pivotal contributor to stimulation of the UPR beyond levels that are significant for maintaining homeostasis. Considering the consequential environmental contribution to UC and CD, it is remarkable that distinct products of the metabolic pathway of the intestinal microbiome might affect the UPR directly. These analyses highlighted the association of immune reaction with the initiation of IBD [42].
Pictorial representation of how the disrupted cellular homeostasis and proteostasis lead to the activation of unfolded protein responses (UPRs) and their associated signaling proteins. The figure demonstrates how the prolonged activation of the UPR pathway eventually contributes to the development of inflammatory bowel disease
In the past few years, the progress in microbial analysis has altered from infectious to commensal agents. Based on adequately available data, a consequential body of evidence has suggested that the normal enteric flora perform a crucial role in the initiation of IBD [41, 42]. A recent analysis reported that probiotics effectively affect the host by regulating the gut microbial balance, which can alleviate both experimental colitis and human IBD. These reports add a crucial dimension to the function of gut microbiota in IBD [43].
Targeting UPR and ER Stress in IBD Therapeutics
Therapeutic approaches to IBD have been controversial because of the limited knowledge of its pathogenesis. Previous evidence has reported that dysregulated ER stress signaling in the IECs is correlated with the initiation of IBD. In this summary, small molecules or chemical compounds able to reverse the folding of the misfolded proteins or increase the potential of the ER lumen for protein folding might be a promising approach to prevent or cure IBD [42]. Studies have reported that in obese individual, small molecules or chemical chaperones like 4-phenylburyrate (4-PBA) and tauroursodeoxycholic acid (TUDCA) alleviate the condition of ER stress by increasing the protein folding in tissues like liver or muscle [44,45,46]. Additionally, analysis conducted on a mouse model of colitis induced by DSS showed the potential of ursodeoxycholic acid (UDCA) and lithocholic acid (LCA) in alleviating colonic inflammation by inhibiting epithelial apoptosis [47]. Furthermore, it has been reported that amino acids such as glycine and L-glutamine supplementation can restore IECs from the condition of ER stress and apoptosis by elevating the expression of tight junction proteins and improving the barrier activity of intestinal epithelial cells [48, 49]. A recent report suggested that the oral administration of 4-PBA downregulates ER stress signaling in colonic IECs, which positively improves DSS-stimulated colitis [32]. Moreover, the stimulation of CHOP and BiP and the synthesis of TNF-α were observed to be decreased by vaticanol B. This signifies an effective impact of 4-PBA and vaticanol B in alleviating the function of ER and sustaining the membrane integrity of the ER [50]. Various natural products like berberine (BBR), which is a plant-based active ingredient, is known to attenuate the response of ER stress as a substituent chemical agent. Consequently, a current analysis showed the potential of berberine to alleviate the condition of inflammation and reduce apoptosis in a colitis mouse model [51]. The data from the previous studies recommend a possible role of different substances in regulating ER stress, some of which could represent a novel approach; a few of them are discussed below.
Inhibitors of ER Stress
Progression of several chronic syndromes induced by ER stress-driven apoptosis leads to therapeutic intervention. Some of the small molecules, chemical compounds, which act as chaperones might interact with one of the three pathways of UPR to retain the balance of the endoplasmic reticulum by elevating the folding potential of protein or lowering the accumulation of misfolded or unfolded proteins as shown in Fig. 4. To determine the efficiency in repressing ER stress in terms of several diseases such as inflammation, obesity, and diabetes along with their adverse effects in in vivo and in vitro studies, some of the inhibitors were studied and are explained below (Table 1).
KIRA6
Kinase inhibiting RNase attenuator 6 is a promising and specific inhibitor of IRE1 kinase that is an ATP-competitive imidazopyrazinyl-naphthalenyl-phenylurea-based compound. Studies have shown KIRA6 to be a cell-permeable and non-toxic inhibitor which has the potential to inhibit oligomerization of IRE1 and support cell survival under the condition of ER stress. Additionally, in retinal degeneration induced by chronic ER stress in P23H rats, KIRA6 was analyzed, where favorable preservation of photoreceptors was reported [60].
3-Hydroxy-2-Naphthoic Acid
3-Hydroxy-2-naphthoic acid (3-HNA) is a chemical chaperone that has a structure combined between salicylate and 4-PBA. It has a higher degree of solubility and potentiality than other available hydroxynaphthoic acids. In the ob/ob diabetic mice model, the chemical chaperone 3-HNA was analyzed for its anti-diabetic impact; the compound was reported to protect pancreatic cells from apoptosis induced by palmitic acid by decreasing the ER stress conditions [61, 62].
Tauroursodeoxycholic Acid (TUDCA)
Tauroursodeoxycholic acid (TUDCA) is a combination of taurine and ursodeoxycholic acid (UDCA). TUDCA is derived from bile acid. The potency of TUDCA or UDCA is ascribed to its cytoprotective effects on hepatocytes. TUDCA has been reported to be more efficient than UDCA. The chaperone property of TUDCA is due to the amino acid taurine, which is an organic osmolyte. Reports have indicated that TUDCA is a promising chemical chaperone having the potential to improve the condition of ER stress by increasing protein folding in ER. Moreover, in leptin-deficient (ob/ob) mice, TUDCA was observed to reverse the ER stress condition, which causes an enhanced level of tolerance for glucose, insulin signaling, and regulation of hyperglycemia [57]. Interestingly, distinctions were made by the studies related to the capacity of 4-PBA and TUDCA in preserving a mutant protein, which fails to achieve the proper arrangement in the ER lumen and triggers the UPR activation, and they are further targeted for degradation. However, a systematic analysis pointed to TUDCA as a promising chemical chaperone with greater potential as a pharmaceutical target for the treatment of ER stress-related disorders like IBD [52].
4-Phenylbutyric Acid
4-Phenylbutyrate (PBA) is primarily utilized for the treatment of urea cycle diseases [63]. It has also been evidenced to be a potent therapeutic approach for the treatment of several diseases, including spinal muscular atrophy, homozygous β-thalassemia, and a range of tumors [64, 65]. Studies have documented that 4-PBA may function as an inhibitor of histone deacetylase, as a chemical chaperone, or as a scavenger of ammonia [53]. Moreover, 4-PBA has been observed to repress ER stress and anti-inflammatory effects [66]. Previous analyses showed that the ER stress is repressed considerably by 4-PBA in the kidneys of streptozotocin (STZ)-instigated diabetic nephropathy (DN) in male Sprague-Dawley rats by decreasing the hydroxyproline activity of NADPH oxidase, the activity of NF-κB, and the level of malondialdehyde. The study done by Kazuhiko Ono et al. (2017) reported that orally administered PBA delayed the development of experimental colitis. Treatment with PBA has not been reported to show any particular adverse effects in the available IBD therapeutics and has added benefits through the oral route of administration. Therefore, PBA might be among the promising therapeutic agents [53].
Quercetin
Quercetin is a polyphenolic bioflavonoid usually found in plant food sources. Quercetin possesses antioxidant anti-inflammatory, anti-diabetic, anti-ulcer, anti-carcinogenic, and anti-viral properties. Natsume et al. showed for the first time that quercetin has the potential to downregulate the expression of GRP78 along with the capacity to hinder the activation of IRE1 and PERK. Treatment with quercetin revoked thapsigargin-instigated ER stress because of the calcium deregulation by inhibiting PI3K (phosphoinositide-3-kinase) in LS180 cells [56]. However, a clear evaluation of the effect of quercetin against ER stress-mediated various diseases including IBD has to be explored to determine its role in alleviating the diseased condition.
N-Acetylcysteine (NAC)
A derivative of L-cysteine known as N-acetyl cysteine (NAC) is also a glutathione precursor in mammals. Analysis has established that NAC has an anti-hyperglycemic effect that has the potential to protect β-cells against alloxan-induced diabetic CD1 mice, diabetic db/db mice, and Zucker diabetic fatty rats. Recently we have seen that NAC plays a crucial role in diabetic nephropathy, which is mediated by ER stress [59, 67]. The expression of ER stress markers was significantly reduced by NAC in Otsuka Long-Evans Tokushima fatty rats. However, the principle molecular mechanisms in the decrease of ER stress have not been evaluated to date. Moreover, the available literature shows that NAC can effectively decrease oxidative stress by substituting ER stress-mediated complications and the accumulation of ROS [57].
Ursolic Acid
Ursolic acid (UA) is a pentacyclic triterpenoid compound reported to possess several beneficial properties, such as anti-inflammatory, anti-oxidant, and anti-glycative. UA is found in fruits, various edible plants, spices, and herbs. A report established that UA can inhibit the development of nonalcoholic fatty liver disease mediated by ER stress [68]. This study is among the few analyses that targeted inhibition of ER stress-mediated lipid disorders. Furthermore, UA remarkably reduced hyperlipidemia-mediated CHOP accumulation, phosphorylation of c-Jun N-terminal kinase (JNK), and IRE1α activation in the livers of the db/db mice with hepatic steatosis [57].
Isoflavones
Isoflavones are important phytoestrogens. They are found in several legumes such as soy. Isoflavones play a major role in stunting ER stress. They reduce the expression of the immunoglobulin binding protein (BiP) mRNA, which leads to the activation of IRE1α to generate UPR response and enhance protein folding to deteriorate the accumulated misfolded proteins in ER. It also plays a crucial role in splicing X-box binding protein-1 (Xbp-1) mRNAs and C/EBP homologous protein, which is an important step in IRE1α-induced ER stress alleviation [69, 70].
Paeonol
Paeonol is a plant-derived drug that can inhibit ER stress. Choy et al. (2009) experimented on tunicamycin-induced ER-stressed mice and showed that paeonol is a potent ER stress inhibitor. Paeonol, when co-treated with Tempol and TUDCA, showed good ER stress inhibition effects. The expressions of ER stress markers like GRP78 and ATF6 and phosphorylation of eukaryotic translation initiation factor 2 alpha (eIF2α) were alleviated [71]. Decrease in ROS levels also reduced ER stress-induced oxidative stress in mice undergoing the treatment. Through the AMPK/PPARδ signaling pathway, paeonol protects the aorta from ER stress [72]. Paeonol increases the expression of 5′adenosine monophosphate-activated protein kinase (AMPK), thus elevating the expression of peroxisome proliferator-activated receptor δ (PPARδ) protein. An increase in the levels of these two proteins prevents high levels of ER stress and ROS production.
Telmisartan
Telmisartan, which is a drug to treat hypertension, is an angiotensin II receptor blocker. It exhibits anti-ER stress effects via the anti-oxidative, AMPK/PPARδ signaling, and apoptotic pathways [73]. Studies have shown that GRP78, CHOP, and caspase 12, which are significant ER stress markers, were decreased in telmisartan treatment. The levels of anti-apoptotic proteins such as Bcl-2 protein increased with the administration of telmisartan. It helps in the reduction of apoptosis and ROS levels in the cells. Telmisartan can reduce inositol-requiring enzyme/endonuclease 1α (IRE1α) expression [58]. This enzyme plays a vital role in the apoptotic signaling pathway, which is mainly triggered by ER stress. Jing Wang et al. in their studies observed that treatment of kidney epithelial cells with telmisartan diminished the expression levels of ER stress markers such as GRP78 and phospho-eIF2α and also reduced inflammasome markers such as NLRP3 and ASC [74]. Thus, telmisartan has the potential to be incorporated in therapies related to cardiovascular ailments [75], hypertension, type 2 diabetes, and renal disease [76], involving ER stress inhibition and alleviation of the disease symptoms.
Salubrinal
Salubrinal has the potential to ameliorate ER stress in the brain cortex. Rodent studies have shown the downregulation of the GRP78 level, an ER stress marker with salubrinal treatment. Salubrinal also inactivated ER stress-induced autophagy via upregulation of LC3-II and downregulation of p62 levels [77]. Salubrinal enhances the phosphorylation of eukaryotic translation initiation factor 2 alpha (eIF2α) [78]. Phosphorylation of eIF2α is important in cellular defenses against xenotoxicant-induced ER stress. Dephosphorylation of eIF2α is prevented by increasing CHOP expression in the cells [79]. Activating transcription factor 4 (ATF4) is elevated in the presence of salubrinal [80]. ATF4 triggers unfolded protein response (UPR) target genes, which are involved in progression of numerous metabolic and neurodegenerative diseases. Salubrinal impairs the activity of kainic acid, which is responsible for ER deterioration and malfunction [81].
Other Inhibitors
MKC-3946 has been documented to have the potential to inhibit IRE1α endonuclease activity. The molecule has a solubilizing group and an expanded hydrophobic core. In multiple myeloma cells it has been reported that this agent can hinder the splicing of XBP1 by blocking the IRE1 α cascade [54]. Another agent, olmesartan, is also reported to show attenuation of CHOP, GRP78, and caspase 12 in autoimmune myocarditis rat model immunized with pocrine cardiac myosin [55]. A study reported by Shaojie et al. reported that administration of artesuante (ARS) to DSS-induced colitis mice significantly suppressed the expression of GRP78 along with IRE1α-XBP1s and PERK-eIF2α-ATF4-CHOP signaling cascade activation. Furthermore, ARS also suppressed DSS-induced apoptosis [82]. Another study reported the beneficial property of trierixin, which inhibited the XBP1-luciferase activation in HeLa/XBP1-luc cells and endogenous XBP1 splicing in HeLa cells [83]. Data obtained from the study done by Crespo et al. signified that glutamine, which is abundantly found in the tissues, has the potential to alleviate the condition of 2,4,6-trinitrobenzenesulfonic acid (TNBS)-induced colitis due to its anti-apoptotic effect and by regulating the ER stress signaling cascade [84]. Besides the existing synthetic inhibitors, a few of the natural inhibitors are also documented to have potential in repressing ER stress, like the polyphenolic component of green tea epigallocatechin-3-gallate and soy component genistein [85]. Several analyses focused specifically on the significance of advanced glycation end product (AGE) inhibitors in sustaining ER lumen balance comprising of tempol, TM2002, and curcumin [86]. Curcumin used in a concentration-dependent approach was documented to downregulate the expression of BiP and GRP94 in bovine aortic endothelial cells by hindering the AP-1 transcription factor [57]. Moreover, in high-fat diet rodents, the administration of tempol was found to reduce damaged endothelium-dependent vasorelaxation and the condition of ER stress [87]. Another natural agent known as lachnum polysaccharide (LEP) was reported to show promising effects on alleviating the condition of IBD by restoring intestinal barrier integrity by modulating the expression of tight junction proteins and mucus layer protecting proteins in DSS-induced colitis [88]. Furthermore, M10, a myricetin-derived compound, was also reported to inhibit ER stress-induced autophagy in inflamed colonic mucosal cells and might be a promising agent for the treatment of IBD [89].
Intestinal Epithelial Cells as Future Therapeutic Targets for IBD
Intestinal epithelium cells (IECs), including Paneth cells, goblet cells, absorptive enterocytes, and enteroendocrine cells, form a barrier in the gut against intruding microbes and also maintain the integrity of the mucosal barrier and its homeostasis. Goblet cells are known to produce and release mucins against invading proinflammatory microbes to defend the mucosa. Besides mucin synthesis, these cells are also involved in secreting cytokines like IL-7 to regulate the immune response in the intestinal mucosa [5]. Unlike goblet cells, Paneth cells are vesicles containing microbicidal peptides and proteins to protect against intruding microbes. Once the Paneth cells recognize the invasion of the microbes into the lumen, they start releasing their contents against the microbicidal contents. The membrane rigidity of the GI tract is important in defending the host from a harsh environment, and impairment in the mucosal barrier leads to the development of various gastrointestinal diseases, including IBD. Various analyses have reported that IECs are associated with the induction of several immune response mechanisms to regulate intestinal balance [4, 5]. Misfolding of protein in the ER of IECs has been observed to contribute directly to the development of IBD. Patients with active IBD generally have elevated ER stress markers in the colonic epithelium. Also, even non-affected mucosal tissues of IBD patients have symptoms of damaged integrated stress response to conditions such as ER stress, oxidative stress, and inflammation. Therefore, accumulating the data, further evaluation for the principle mechanisms correlated with pathophysiological modifications of UPR due to ER stress in the intestines might permit us to understand the complex pathogenesis in the development of IBD, which could represent a potent therapeutic target for its treatment.
Discussion
Current analyses have challenged the belief that the epithelium functions as a mere barrier between the niche and the body; instead, the intestinal epithelium performs an active and imperative function in regulating the mucosal balance by interacting with pathogenic and commensal microorganisms, the immune system, and metabolites. An altered population of IECs and their activity may directly influence the homeostasis of the mucosa and contribute to the development of intestinal inflammation. ER stress is a functionally significant cellular mechanism in IECs comprising the secretory cells. Genetically, these secretory cells have higher efficiency in ER protein folding and its maturation, intracellular synthesis, and trafficking. The synthesis of mucin and anti-microbial peptides is regulated by enteric signals comprising cholinergic stimuli, microbial molecules, bile salts, and regulation of the immune system in an NF-κB–dependent pathway [8, 90].
Under a pathogenic environment the ROS, inflammatory stimuli, microorganisms, and their metabolites may cause ER activity. The accumulation of these might cause the aggregation of unfolded or misfolded proteins in the ER lumen [91]. Therefore, to confront the altered environment, the secretory IECs may need intact and potent UPR signaling, ERAD, and ER chaperones to accomplish the requirement of protein folding, maturation, and secretion. The chronic condition of ER stress can be induced by environmental or genetic factors. The altered cellular processes might damage the activity and balance of the IECs, causing the epithelial cell to undergo apoptosis, damaging the barrier function, and causing inflammation of the intestine. Previous studies endorsed therapeutic approaches to IBD that depended on the regulation of the host’s immune system [8, 92]. Current advancement in knowledge on the activity of the intestinal epithelium and the function of cellular stress cascades in the homeostasis of the mucosa leads to a novel therapeutic approach that was not accepted earlier. Though monotherapy utilizing ER stress-regulating components like the chemical chaperones may not be sufficient to stop the inflammatory response, their supplementation might be beneficial in conjunction with conventional IBD drugs. Accumulating evidence from previous studies shows that tauroursodeoxycholic acid and 4-phenylbutyrate can significantly alleviate dextran sulfate sodium-induced colitis via regulation of ER stress markers and regulating the barrier function in intestinal epithelial cells [52]. On the other hand, glutamine, which is abundantly found in the tissues, is also reported to improve TNBS-induced colitis by restoring ER function and alleviating the intestinal balance [42]. Furthermore, several natural inhibitors like curcumin, tempol, and very recently LEP and myrecitin derived-M10 compound had shown significant potential in alleviating IBD by repressing ER stress. These novel ER stress inhibitors thus should be promising agents for the treatment of IBD. However, for the small molecules and ER stress inhibitors studied, it has been reported that they display biphasic effects which are concentration-dependent. Therefore, further research has to focus on delineating the principle molecular mechanisms associated with ER stress inhibitors in IBD to provide novel targets for therapeutic intervention.
Conclusion and Future Perspectives
IBD is a chronic condition in which environmental and genetic factors, as well as an interaction between the intestinal microbiome and host immune reaction, contribute to the pathogenesis and etiology of the disease. Due to the incomplete knowledge of the disease pathogenesis, the development of IBD therapies has been confronted with unexpected challenges. A promising approach to IBD that is tailored to the individual’s specific situation relies on in-depth insights into the phenotype and the mechanism behind the development of this disease condition. However, the progression of IBD is known to be regulated by ER stress and the UPR signaling cascade. Deregulation in ER stress stimulated by several factors is correlated with susceptibility to intestinal impairment and development of IBD. Therefore, restoring the intestinal balance by reversing the condition of ER stress through the regulation of the signaling pathway is emerging as a promising therapeutic target for treating IBD. The principle mechanisms such as post-translational alteration, protein folding, and degradation are involved in several pathological and physiological mechanisms. Therefore, regulating ER stress signaling without inducing adverse effects is a challenging task that must be precisely mediated before its use for treating IBD patients. Many investigations have reported that UPR homeostasis restoration in both ER and mitochondria via pharmacological intervention could be a new avenue to research when considering novel IBD therapeutics. Another therapeutic strategy can be to target highly secretory intestinal cells such as goblet cells and Paneth cells, which have the greatest possibility of having misfolded proteins in the ER. However, to date very few studies have tested ER stress pathway blockers in in vivo models. Hence, future evaluation of ER stress inhibitors in intestinal cells may lead to a potential therapeutic approach for IBD.
Availability of data and materials
All data generated or analyzed during this study are included in this article.
References
De Souza HS, Fiocchi C. Immunopathogenesis of IBD: current state of the art. Nat Rev Gastroenterol Hepatol. 2016;13:13.
Guariso G, Gasparetto M, Visonà Dalla Pozza L, D’Incà R et al. Inflammatory bowel disease developing in paediatric and adult age. J Pediatr Gastroenterol Nutr. 2010;51:698–707.
Coelho T, Andreoletti G, Ashton JJ, Pengelly RJ et al. Immuno-genomic profiling of patients with inflammatory bowel disease: a systematic review of genetic and functional in vivo studies of implicated genes. Inflamm Bowel Dis. 2014;20:1813–1819.
Dupaul-Chicoine J, Dagenais M, Saleh M. Crosstalk between the intestinal microbiota and the innate immune system in intestinal homeostasis and inflammatory bowel disease. Inflamm Bowel Dis. 2013;19:2227–2237.
Cao SS. Epithelial ER stress in Crohn’s disease and ulcerative colitis. Inflamm Bowel Dis. 2016;22:984–993.
Ron D, Walter P. Signal integration in the endoplasmic reticulum unfolded protein response. Nat Rev Mol Cell Biol. 2007;8:519–529.
Wu J, Kaufman RJ. From acute ER stress to physiological roles of the unfolded protein response. Cell Death Differ. 2006;13:374–384.
Luo K, Cao SS. Endoplasmic reticulum stress in intestinal epithelial cell function and inflammatory bowel disease. Gastroenterol Res Pract. 2015;2015:328791.
Kaser A, Lee AH, Franke A, Glickman JN et al. XBP1 links ER stress to intestinal inflammation and confers genetic risk for human inflammatory bowel disease. Cell. 2008;134:743–746.
Wang M, Wey S, Zhang Y, Ye R, Lee AS. Role of the unfolded protein response regulator GRP78/BiP in development, cancer, and neurological disorders. Antiox Redox Signal. 2009;11:2307–2316.
Hasnain SZ, Lourie R, Das I, Chen AC, McGuckin MA. The interplay between endoplasmic reticulum stress and inflammation. Immunol Cell Biol. 2012;90:260.
Hotamisligil GS. Endoplasmic reticulum stress and the inflammatory basis of metabolic disease. Cell. 2010;140:900–907.
Olefsky JM, Glass CK. Macrophages, inflammation, and insulin resistance. Ann Rev Physiol. 2010;72:219–226.
Hotamisligil GS, Shargill NS, Spiegelman BM. Adipose expression of tumor necrosis factor-alpha: direct role in obesity-linked insulin resistance. Science. 1993;259:87–91.
Özcan U, Cao Q, Yilmaz E, Lee AH et al. Endoplasmic reticulum stress links obesity, insulin action, and type 2 diabetes. Science. 2004;306:457–461.
Linden SK, Sutton P, Karlsson NG, Korolik V, McGuckin MA. Mucins in the mucosal barrier to infection. Mucosal Immunol. 2008;1:183–187.
Junjappa RP, Patil P, Bhattarai KR, Kim HR, Chae HJ. IRE1α implications in endoplasmic reticulum stress-mediated development and pathogenesis of autoimmune diseases. Front Immunol. 2018;6:1289.
Kimata Y, Oikawa D, Shimizu Y, Ishiwata-Kimata Y, Kohno K. A role for BiP as an adjustor for the endoplasmic reticulum stress-sensing protein Ire1. J Cell Biol. 2004;167:445–456.
Okuda N, Fujii T, Inoue H, Ishikawa K, Hoshino T. Enhancing cellulase production by overexpression of xylanase regulator protein gene, xlnR, in Talaromyces cellulolyticus cellulase hyperproducing mutant strain. Biosci Biotechnol Biochem. 2016;80:2065–2068.
Wong MY, DiChiara AS, Suen PH, Chen K, Doan ND, Shoulders MD. Adapting secretory proteostasis and function through the unfolded protein response. Coordinating Organismal Physiology Through the Unfolded Protein Response. 2017; 1–25.
Bertolotti A, Wang X, Novoa I, Jungreis R et al. Increased sensitivity to dextran sodium sulfate colitis in IRE1β-deficient mice. J Clin Investig. 2001;107:585–593.
Lin JH, Li H, Yasumura D, Cohen HR et al. IRE1 signaling affects cell fate during the unfolded protein response. Science. 2007;318:944–949.
Hetz C, Chevet E, Harding HP. Targeting the unfolded protein response in disease. Nat Rev Drug Discov. 2013;12:703–709.
Cybulsky AV, Takano T, Papillon J, Bijian K. Role of the endoplasmic reticulum unfolded protein response in glomerular epithelial cell injury. J Biol Chem. 2005;280:24396–24403.
Inagi R, Kumagai T, Nishi H, Kawakami T et al. Preconditioning with endoplasmic reticulum stress ameliorates mesangioproliferative glomerulonephritis. J Am Soc Nephrol. 2008;19:915–922.
Peters LR, Raghavan M. Endoplasmic reticulum calcium depletion impacts chaperone secretion, innate immunity, and phagocytic uptake of cells. J Immunol. 2011;187:919–921.
Banerjee A, Burra P, Di Liddo R, Arcidiacono D et al. Ameliorative potentials of human umbilical cord derived mesenchymal stem cells in dextran sulphate sodium induced acute colitis in NOD. Cb17/Prkdcscid/J Mice. Gastroenterology. 2012;142:S719.
Kreft H, Jetz W. Global patterns and determinants of vascular plant diversity. Proc Natl Acad Sci. 2007;104:5925.
Wu J, Rutkowski DT, Dubois M, Swathirajan J et al. ATF6α optimizes long-term endoplasmic reticulum function to protect cells from chronic stress. Dev Cell. 2007;13:351–354.
Kroemer G, Mariño G, Levine B. Autophagy and the integrated stress response. Mol Cell. 2010;40:280–283.
Brandl K, Rutschmann S, Li X, Du X et al. Enhanced sensitivity to DSS colitis caused by a hypomorphic Mbtps1 mutation disrupting the ATF6-driven unfolded protein response. Proc Natl Acad Sci. 2009;106:3300–3305.
Cao SS, Zimmermann EM, Chuang BM, Song B, Nwokoye A, Wilkinson JE et al. The unfolded protein response and chemical chaperones reduce protein misfolding and colitis in mice. Gastroenterology. 2013;144:989.
Strasser A, Puthalakath H. Fold up or perish: unfolded protein response and chemotherapy. Cell Death Differ. 2008;15:3.
Park SH, Choi HJ, Yang H, Do KH et al. Endoplasmic reticulum stress-activated C/EBP homologous protein enhances nuclear factor-κB signals via repression of peroxisome proliferator-activated receptor γ. J Biol Chem. 2010;285:35330–35339.
Namba T, Tanaka KI, Ito Y, Ishihara T et al. Positive role of CCAAT/enhancer-binding protein homologous protein, a transcription factor involved in the endoplasmic reticulum stress response in the development of colitis. Am J Pathol. 2009;174:1786–1798.
Hölttä V, Klemetti P, Sipponen T, Westerholm-Ormio M et al. IL-23/IL-17 immunity as a hallmark of Crohn’s disease. Inflamm Bowel Dis. 2008;14:1175–1184.
Goodall JC, Wu C, Zhang Y, McNeill L, Ellis L, Saudek V et al. Endoplasmic reticulum stress-induced transcription factor, CHOP, is crucial for dendritic cell IL-23 expression. Proc Natl Acad Sci. 2010;107:17698–17703.
Xue X, Piao JH, Nakajima A, Sakon-Komazawa S et al. Tumor necrosis factor α (TNFα) induces the unfolded protein response (UPR) in a reactive oxygen species (ROS)-dependent fashion, and the UPR counteracts ROS accumulation by TNFα. J Biol Chem. 2005;280:33917–33925.
Uehara T, Nakamura T, Yao D, Shi ZQ et al. S-nitrosylated protein-disulphide isomerase links protein misfolding to neurodegeneration. Nature. 2006;441:513–517.
Shkoda A, Ruiz PA, Daniel H, Kim SC et al. Interleukin-10 blocked endoplasmic reticulum stress in intestinal epithelial cells: impact on chronic inflammation. Gastroenterology. 2007;132:190–197.
Todd DJ, Lee AH, Glimcher LH. The endoplasmic reticulum stress response in immunity and autoimmunity. Nat Rev Immunol. 2008;8:663–664.
Ma X, Dai Z, Sun K, Zhang Y et al. Intestinal epithelial cell endoplasmic reticulum stress and inflammatory bowel disease pathogenesis: an update review. Front Immunol. 2017;25:1271.
Danese S, Sans M, Fiocchi C. Inflammatory bowel disease: the role of environmental factors. Autoimmun Rev. 2004;3:394.
Powers ET, Morimoto RI, Dillin A, Kelly JW, Balch WE. Biological and chemical approaches to diseases of proteostasis deficiency. Ann Rev Biochem. 2009;78:959–961.
Delong T, Baker RL, Reisdorph N, Reisdorph R et al. Islet amyloid polypeptide is a target antigen for diabetogenic CD4+ T cells. Diabetes. 2011;60:2325.
Kars M, Yang L, Gregor MF, Mohammed BS et al. Tauroursodeoxycholic acid may improve liver and muscle but not adipose tissue insulin sensitivity in obese men and women. Diabetes. 2010;59:1899–1905.
Lajczak-McGinley NK, Porru E, Fallon CM, Smyth J et al. The secondary bile acids, ursodeoxycholic acid and lithocholic acid, protect against intestinal inflammation by inhibition of epithelial apoptosis. Physiol Rep. 2020;8:e14456.
He Y, Fan X, Liu N, Song Q et al. L-Glutamine represses the unfolded protein response in the small intestine of weanling piglets. J Nutr. 2019;149:1904–1910.
Fan X, Li S, Wu Z, Dai Z et al. Glycine supplementation to breast-fed piglets attenuates post-weaning jejunal epithelial apoptosis: a functional role of CHOP signaling. Amino acids. 2019;51:463–473.
Tabata Y, Takano K, Ito T, Iinuma M et al. Vaticanol B, a resveratrol tetramer, regulates endoplasmic reticulum stress and inflammation. Am J Physiol-Cell Physiol. 2007;293:C411–C418.
Eugene SP, Reddy VS, Trinath J. Endoplasmic reticulum stress and intestinal inflammation: a perilous union. Front Immunol. 2020;11.
Berger E, Haller D. Structure–function analysis of the tertiary bile acid TUDCA for the resolution of endoplasmic reticulum stress in intestinal epithelial cells. Biochem Biophys Res Commun. 2011;409:610–615.
Ono K, Nimura S, Hideshima Y, Nabeshima K, Nakashima M. Orally administered sodium 4-phenylbutyrate suppresses the development of dextran sulfate sodium-induced colitis in mice. Exp Ther Med. 2017;14:5485.
Mimura N, Fulciniti M, Gorgun G, Tai YT et al. Blockade of XBP1 splicing by inhibition of IRE1α is a promising therapeutic option in multiple myeloma. Blood, J Am Soc Hematol. 2012;119:5772–5781.
Sukumaran V, Watanabe K, Veeraveedu PT, Gurusamy N et al. Olmesartan, an AT1 antagonist, attenuates oxidative stress, endoplasmic reticulum stress and cardiac inflammatory mediators in rats with heart failure induced by experimental autoimmune myocarditis. Int J Biol Sci. 2011;7:154.
Natsume Y, Ito S, Satsu H, Shimizu M. Protective effect of quercetin on ER stress caused by calcium dynamics dysregulation in intestinal epithelial cells. Toxicology. 2009;258:164–165.
Sarvani C, Sireesh D, Ramkumar KM. Unraveling the role of ER stress inhibitors in the context of metabolic diseases. Pharmacol Res. 2017;119:412–421.
Tong Q, Wu L, Jiang T, Ou Z, Zhang Y, Zhu D. Inhibition of endoplasmic reticulum stress-activated IRE1α-TRAF2-caspase-12 apoptotic pathway is involved in the neuroprotective effects of telmisartan in the rotenone rat model of Parkinson’s disease. Eur J Pharmacol. 2016;5:106–115.
Tanaka Y, Gleason CE, Tran PO, Harmon JS, Robertson RP. Prevention of glucose toxicity in HIT-T15 cells and Zucker diabetic fatty rats by antioxidants. Proc Natl Acad Sci. 1999;96:10857–10862.
Ghosh R, Wang L, Wang ES, Perera BG et al. Allosteric inhibition of the IRE1α RNase preserves cell viability and function during endoplasmic reticulum stress. Cell. 2014;158:534–538.
Jeong KW, Ku JM, Park MW, Park SM, Yang JE, Nam TG. Hydroxynaphthoic acids identified in a high throughput screening potently ameliorate endoplasmic reticulum stress as novel chemical chaperones. Chem Pharm Bull. 2013;61:740–746.
Park SM, Choi J, Nam TG, Ku JM, Jeong K. Anti-diabetic effect of 3-hydroxy-2-naphthoic acid, an endoplasmic reticulum stress-reducing chemical chaperone. Eur J Pharmacol. 2016;779:157–167.
Diaz GA, Krivitzky LS, Mokhtarani M, Rhead W et al. Ammonia control and neurocognitive outcome among urea cycle disorder patients treated with glycerol phenylbutyrate. Hepatology. 2013;57:2171–2179.
Iannitti T, Palmieri B. Clinical and experimental applications of sodium phenylbutyrate. Drugs in R & D. 2011;11:227–229.
Kusaczuk M, Bartoszewicz M, Cechowska-Pasko M. Phenylbutyric Acid: simple structure-multiple effects. Curr Pharm Design. 2015;21:2147–2156.
Luo ZF, Feng B, Mu J, Qi W et al. Effects of 4-phenylbutyric acid on the process and development of diabetic nephropathy induced in rats by streptozotocin: regulation of endoplasmic reticulum stress-oxidative activation. Toxicol Appl Pharmacol. 2010;246:49–57.
Ho E, Chen G, Bray TM. Supplementation of N-acetylcysteine inhibits NFκB activation and protects against alloxan-induced diabetes in CD-1 mice. FASEB J. 1999;13:1845–1854.
Li JS, Wang WJ, Sun Y, Zhang YH, Zheng L. Ursolic acid inhibits the development of nonalcoholic fatty liver disease by attenuating endoplasmic reticulum stress. Food Funct. 2015;6:1643–1651.
Park YJ, Jang YM, Kwon YH. Isoflavones prevent endoplasmic reticulum stress-mediated neuronal degeneration by inhibiting tau hyperphosphorylation in SH-SY5Y cells. J Med Food. 2009;12:528–535.
Abdelrazek H, Mahmoud M, Tag HM, Greish SM, Eltamany DA, Soliman MT. Soy isoflavones ameliorate metabolic and immunological alterations of ovariectomy in female Wistar rats: antioxidant and estrogen sparing potential. Oxidative Med Cell Longevity. 2019;10:2019.
Choy KW, Lau YS, Murugan D, Mustafa MR. Chronic treatment with paeonol improves endothelial function in mice through inhibition of endoplasmic reticulum stress-mediated oxidative stress. PLoS One. 2017;12:e0178365.
Choy KW, Mustafa MR, Lau YS, Liu J et al. Paeonol protects against endoplasmic reticulum stress-induced endothelial dysfunction via AMPK/PPARδ signaling pathway. Biochem Pharmacol. 2016;15:51–62.
Wang Y, Xue J, Li Y, Zhou X, Qiao S, Han D. Telmisartan protects against high glucose/high lipid-induced apoptosis and insulin secretion by reducing the oxidative and ER stress. Cell Biochem Funct. 2019;37:161–168.
Wang J, Wen Y, Lv LL, Liu H et al. Involvement of endoplasmic reticulum stress in angiotensin II-induced NLRP3 inflammasome activation in human renal proximal tubular cells in vitro. Acta Pharmacologica Sinica. 2015;36:821–830.
Naiel S, Tat V, Padwal M, Vierhout M et al. Protein misfolding and endoplasmic reticulum stress in chronic lung disease: will cell-specific targeting be the key to the cure? Chest. 2020;157:1207–1220.
Unger T. Preclinical and clinical effects of RAS inhibition with a focus on telmisartan. Int Schol Res Not. 2012;2012.
Gao B, Zhang XY, Han R, Zhang TT et al. The endoplasmic reticulum stress inhibitor salubrinal inhibits the activation of autophagy and neuroprotection induced by brain ischemic preconditioning. Acta Pharmacologica Sinica. 2013;34:657–666.
Li RJ, He KL, Li X, Wang LL, Liu CL, He YY. Salubrinal protects cardiomyocytes against apoptosis in a rat myocardial infarction model via suppressing the dephosphorylation of eukaryotic translation initiation factor 2α. Mol Med Rep. 2015;12:1043–1049.
Bastola P, Neums L, Schoenen FJ, Chien J. VCP inhibitors induce endoplasmic reticulum stress, cause cell cycle arrest, trigger caspase-mediated cell death and synergistically kill ovarian cancer cells in combination with Salubrinal. Mol Oncol. 2016;10:1559–1574.
Matsuoka M, Komoike Y. Experimental evidence shows salubrinal, an eIF2α dephosphorylation inhibitor, reduces xenotoxicant-induced cellular damage. Int J Mol Sci. 2015;16:16275–16287.
Kim JS, Heo RW, Kim H, Yi CO et al. Salubrinal, ER stress inhibitor, attenuates kainic acid-induced hippocampal cell death. J Neural Transm. 2014;121:1233–1243.
Yin S, Li L, Tao Y, Yu J, et al. The inhibitory effect of artesunate on excessive endoplasmic reticulum stress alleviates experimental colitis in mice. Front Pharmacol. 2021;12.
Tashiro E, Hironiwa N, Kitagawa M, Futamura Y et al. Trierixin, a Novel Inhibitor of ER Stress-induced XBP1 Activation from Streptomyces sp. J Antibiotics. 2007;60:547–553.
Crespo I, San-Miguel B, Prause C, Marroni N et al. Glutamine treatment attenuates endoplasmic reticulum stress and apoptosis in TNBS-induced colitis. PloS one. 2012;7:e50407.
Schönthal AH. Endoplasmic reticulum stress: its role in disease and novel prospects for therapy. Scientifica. 2012.
Inagi R. Inhibitors of advanced glycation and endoplasmic reticulum stress. Methods Enzymol. 2011;491:361.
Dong Y, Zhang M, Wang S, Liang B et al. Activation of AMP-activated protein kinase inhibits oxidized LDL-triggered endoplasmic reticulum stress in vivo. Diabetes. 2010;59:1386–1396.
Zong S, Ye Z, Zhang X, Chen H, Ye M. Protective effect of Lachnum polysaccharide on dextran sulfate sodium-induced colitis in mice. Food Funct. 2020;11:846–859.
Wang F, Song ZY, Qu XJ, Li F et al. M10, a novel derivative of Myricetin, prevents ulcerative colitis and colorectal tumor through attenuating robust endoplasmic reticulum stress. Carcinogenesis. 2018;39:889–899.
Hooper LV. Epithelial cell contributions to intestinal immunity. Adv Immunol. 2015;126:129–132.
Pathak S, Grillo AR, Scarpa M, Brun P et al. MiR-155 modulates the inflammatory phenotype of intestinal myofibroblasts by targeting SOCS1 in ulcerative colitis. Exp Mol Med. 2015;47:e164.
Kaser A, Martínez-Naves E, Blumberg RS. Endoplasmic reticulum stress: implications for inflammatory bowel disease pathogenesis. Curr Opin Gastroenterol. 2010;26:318.
Acknowledgments
The authors thank Chettinad Academy of Research and Education (CARE) for providing the financial support and SERB, DST, Government of India, and CARE for providing infrastructural support to complete this work.
Funding
This work was supported by grants to Dr. Antara Banerjee (PI) from the SERB-DST, Government of India, file no ECR/2017/001066, and DST Inspire research student grant with award number 190963.
Author information
Authors and Affiliations
Contributions
AB designed the study and conceptualized the work. AB, DD, AD conducted data analysis and wide-ranging aspects of the manuscript preparation and pictorial representations. RD, GCS, SP critically reviewed the draft manuscript and provided feedback on data analyses. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
None. All authors declare that there are no conflicts of/or competing interests.
Ethics approval and consent to participate
Non-applicable. This research does not involve human/animal participants, human/ animal material, or human data.
Consent for publication
All authors have approved the final version of the manuscript and gave consent for publication.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Deka, D., D’Incà, R., Sturniolo, G.C. et al. Role of ER Stress Mediated Unfolded Protein Responses and ER Stress Inhibitors in the Pathogenesis of Inflammatory Bowel Disease. Dig Dis Sci 67, 5392–5406 (2022). https://doi.org/10.1007/s10620-022-07467-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-022-07467-y