Abstract
The fatty acid-binding proteins play a major role in intracellular transportation of long-chain fatty acids. Nine fatty acid-binding proteins have been identified, with each having individual tissue-specific functions in addition to regulation of fatty acids. This review focuses on the three fatty acid-binding proteins found in the gastrointestinal tract and discusses their role as diagnostic or disease monitoring markers in neonatal necrotizing enterocolitis, acute mesenteric ischemia, celiac disease, and inflammatory bowel disease. Of these three fatty acid-binding proteins, intestinal fatty acid-binding protein is of the most interest due to its exclusive expression in the gastrointestinal tract. The elevation of intestinal fatty acid-binding protein in blood and urine reflects enterocyte damage, regardless of the underlying cause. The short half-life of intestinal fatty acid-binding protein also means it is a relatively sensitive marker. In contrast, there is currently less evidence to support liver fatty acid-binding protein and ileal bile acid-binding protein as sensitive biomarkers in these conditions. More extensive studies with specific endpoints are required to validate the roles of these fatty acid-binding proteins in gastrointestinal diseases.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The term fatty acid-binding protein (FABP) was first coined in 1972 by Ockner et al. [1] following their studies of the absorption of long-chain fatty acids into human enterocytes. Similar FABPs were subsequently found in the cell cytosol of other tissues including brain, myocardium, adipose tissue, kidney, and liver, with each named after the tissue in which they were discovered or predominantly expressed. Nine different tissue-specific FABPs have been identified to date (Table 1), all of which have a similar tertiary structure and a single ligand (fatty acid, cholesterol, or retinoid) bound in an internal water-filled cavity [2].
The primary role of the FABPs is to regulate the uptake and intracellular transport of long-chain fatty acids (≥ 14 carbons). All FABPs bind to a single fatty acid, with the exception of liver FABP (L-FABP) that binds to two fatty acids or other hydrophobic molecules [3]. Recent research suggests that the individual FABPs may also have other tissue-specific functions that are driven by protein–protein and protein–membrane interactions additional to their primary role [4, 5].
This review focuses on the three FABPs found in the gastrointestinal (GI) tract and discusses their role as diagnostic or disease monitoring markers in specific gastrointestinal diseases. Intestinal FABP (I-FABP) and L-FABP are found most abundantly in the mature enterocytes of jejunal villi, with lower amounts present in duodenal enterocytes [6,7,8]. Both I-FABP and L-FAPB are also expressed in colonocytes. While there is evidence that L-FABP expression is increased over that of I-FABP, expression of both proteins is comparatively low in the colon [7, 8]. L-FABP is also expressed in hepatocytes, renal tubular cells, pancreas, and lung [9]. In contrast, the third FABP of interest, ileal FABP, which is also known as ileal bile acid-binding protein (I-BABP), is expressed in the ileum, ovary, and adrenal gland [9].
The gastrointestinal FABPs have unique, tissue-specific roles. This is exemplified by the findings in cell culture and animal models that neither I-FABP nor L-FABP compensates or upregulates each other in the absence of the other proteins [4, 5]. When the L-FABP (Fabp1) gene is knocked out in mice, the remaining I-FABP directs fatty acids toward triacylglycerol synthesis, whereas knockout of I-FABP drives fatty acids and dietary monoacylglycerols toward the oxidative and anabolic pathways, respectively [5]. There is also evidence that L-FABP is required for enterocyte proliferation, suggesting it has a specific role in regulating intestinal homeostasis [4]. I-BABP has an additional specific function of transporting bile acid from the intestinal lumen back to liver via the enterohepatic circulation [10].
I-FABP is the most studied of the three as regards human GI disease because of its specificity to the small intestine. Moreover, I-FABP levels can be detected at low levels in blood consequent to the constant shedding of mature enterocytes from villi as part of normal gut homeostasis. Thus, when enterocytes are damaged, I-FABP levels in the blood are correspondingly elevated. L-FABP can also be detected in the circulation, although evidence suggests that efficient removal of this FABP by the kidneys means it has an estimated plasma half-life of only 11 min [11]. Given their molecular homogeneity, it is likely that I-FABP and I-BABP may also have correspondingly similar circulating half-lives.
Using Gastrointestinal FABPs to Diagnosis and Monitor Gastrointestinal Diseases
The three gastrointestinal FABPs, in particular I-FABP, have been studied in the context of a number of GI and extra-intestinal diseases [12, 13]. Of these, four diseases stand out as regards the reported roles of FABPs in diagnosis and subsequent monitoring of responses to therapy: neonatal necrotizing enterocolitis, acute mesenteric ischemia, celiac disease, and inflammatory bowel disease. These are the focus of this review.
Neonatal Necrotizing Enterocolitis
Neonatal necrotizing enterocolitis (NEC) is a gastrointestinal condition primarily seen in preterm and low-birthweight infants. NEC occurs at a rate of 0.5 to 5 patients per 1000 live births and is associated with a mortality rate of between 15 and 30% [14]. The pathophysiology of this disease is yet to be fully understood, but infants who receive formula milk are three times more likely to develop NEC compared to those who are exclusively breast fed [15]. The initial symptoms of NEC can be non-specific and include feed intolerance, mild abdominal distention, hematochezia, and/or lethargy. The diagnosis of NEC is definitive when evidence of pneumatosis intestinalis is present, with or without other clinical features such as absent bowel sounds and progressive metabolic acidosis. NEC is considered advanced when multiple organs are compromised with worsening of GI features including significant abdominal distension, or pain on palpation.
Bell’s staging system is a commonly used staging system for the various symptoms and signs of NEC [16]. This system includes three stages ranging from suspected (Stage 1), to definite (Stage 2), and advanced (Stage 3). Although advanced stages of NEC can be more obvious clinically, early stages of NEC may present with non-specific features. Consequently, a biomarker that might predict or identify early stage NEC could enable appropriate intervention to be instituted before progression to more advanced disease.
The Role of I-FABP as a Diagnostic and Disease Severity Marker for NEC
Among the three gastrointestinal FABPs, I-FABP (measured in blood or urine) is the most promising diagnostic marker for NEC. Although I-FABP has been evaluated in a number of studies, there is significant heterogeneity (I2 greater than 50%) among these reports, as highlighted in the three published meta-analyses [17,18,19]. The most recent meta-analysis, including 572 infants (262 infants with NEC and 310 healthy controls), found that expression of I-FABP in serum or urine is positively associated with the presence of NEC; standardized mean difference (SMD) = 2.88, 95% confidence intervals (CI) = 2.09–3.67, P < 0.001 [18]. The study also found I-FABP levels increased significantly in those with advanced stage disease (Bell’s stage ≥ 2) compared to those with an early stage of NEC (Bell’s Stage 1), SMD = 0.48, 95% CI = − 0.87 to − 0.09, P = 0.015 [18]. This finding is further supported by additional studies (not included in the meta-analysis) that also describe the sensitivity, specificity, positive predictive value, and negative predictive value of two gastrointestinal FABPs (I-FABP and L-FABP) in the diagnosis of NEC (Table 2). Further to this, there is a wide inconsistency of the best diagnostic cutoff values described by each study. This is likely due to the different test kits used to measure I-FABP and/or different control groups that range from matched controls to patients with other non-NEC conditions.
The other two meta-analyses included studies that measured I-FABP in blood, and both found this to provide a moderately accurate diagnostic marker with medium sensitivity but high specificity [17, 19]. Cheng et al. [19] reported a pooled sensitivity of 0.67 for NEC Bell Stage 1, 0.74 for NEC Bell Stage 2 and 0.83 for NEC Bell Stage 3. In contrast, Yang et al. [17] calculated the pooled sensitivity and specificity of plasma I-FABP for diagnosing NEC (Bell Stage 2 or 3) to be 0.64 (95% CI = 0.53–0.74) and 0.91 (95% CI = 0.84–0.95), respectively. In a sub-analysis, urinary I-FABP was found to be equally sensitive but less specific than plasma I-FABP, with pooled sensitivity and specificity of 0.64 (95% CI = 0.53–0.74) and 0.73 (95% CI = 0.64–0.80), respectively. In addition, standardizing to urine creatinine (urine I-FABP:Cr) to adjust for variable urine concentrations did not appreciably affect the sensitivity or specificity of I-FABP [17].
GI FABPs Compared to Other NEC Diagnostic Markers/Combination Markers
Other biomarkers have also been evaluated as diagnostic markers for NEC and many of them have been considered in concert with the FABP proteins. Fecal calprotectin (S100A8/A9), a protein released mainly from activated neutrophils, is widely used as a biomarker of GI inflammation [20]. While the measurement of fecal calprotectin in infants with NEC has slightly higher sensitivity than urinary I-FABP:Cr (0.81 versus 0.79), specificity is lower (0.79 versus 0.85) [21]. However, when measured in combination (urine I-FABP:Cr and fecal calprotectin), the sensitivity and specificity for the diagnosis of NEC increased to 94% and 79%, respectively [21].
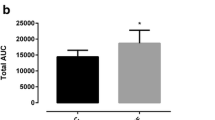
The finding that fecal calprotectin is raised in infants with NEC fits with one of the underlying hypotheses for the development of NEC, which is dysregulation of the immune system and activation of proinflammatory cytokines such as interleukin-8 (IL-8) [22,23,24]. One study has compared serum IL-8 levels to levels of serum I-FABP and L-FABP in infants with and without NEC [25]. All three markers were significantly elevated in the infants with NEC (Bell’s stage ≥ 2) compared to age-matched controls, with IL-8 observed to have the highest area under the curve (AUC) of 0.99, suggesting that serum IL-8 may be a better diagnostic marker than I-FABP or L-FABP.
A recent systematic review, however, involving ten studies with NEC Bell stage ≥ 2 as the target condition, analyzed the utility of a group of serum inflammatory response amplification markers that included IL-8, monocyte chemoattractant protein 1 (MCP-1), interleukin 10 (IL-10), and IL-1 receptor antagonist (IL-1ra) as diagnostic markers for NEC [26]. This study determined that IL-10 and IL-1ra had the highest sensitivity and specificity (100% and 90%, and 100% and 91.7%, respectively) within this group of proteins. I-FABP and ischemia-modified albumin were found to have sensitivity and specificity similar to those of IL-10 and IL-1ra (100% and 91%, and 94.7% and 92%, respectively) in diagnosing NEC [26].
The combination of L-FABP and I-FABP with a marker that reflects alteration in intestinal barrier function has also been evaluated in the diagnosis of NEC. In this study involving 20 infants with NEC stage ≥ 2, 40 infants with septicemia and 40 control infants, the combination of L-FABP, I-FABP and trefoil factor 3 (TFF3), also known as the LIT score [27], was evaluated. The plasma level of each marker was ranked on a scale of 0 to 3 based on defined cutoff values (i.e., low, medium and high), giving a combined range between 0 and 9. The study found that a LIT score > 4.5 had the highest diagnostic accuracy in differentiating NEC from septicemia and controls, providing sensitivity of 50% and specificity of 96%. In addition, a LIT score greater than 6 identified infants who would not survive their episode of NEC, with sensitivity and specificity of 78% and 91%, respectively. To date, no further assessments of the LIT score as a means to diagnose NEC have been reported.
Marker to Predict Timing and Need for Surgery
While most infants with NEC are managed medically, 20–40% will need surgical intervention. Severe NEC needing surgical intervention is associated with mortality up to 50%, especially in the smallest and least mature infants [14]. Having a biomarker that could predict a more complicated NEC course would assist clinicians in deciding which infants to consider for surgical intervention, and timing of the procedure.
Several studies, with the exception of that by Ng et al. [27] using the LIT score, have demonstrated that a single measurement of I-FABP or L-FABP when NEC is suspected or established (by the presence of pneumatosis intestinalis) is not able to distinguish infants needing surgical intervention from those requiring medical treatment only [25, 28, 29]. It appears that sequential measurements of I-FABP (with increasing expression) over a period of time may have a role in differentiating these infants, as exemplified by a small prospective study involving 37 infants (including 22 infants with NEC stage ≥ 2) [29]. This study found that subsequent plasma and urinary I-FABP levels measured between 8 and 16 h following the onset of clinical features associated with NEC were able to differentiate those infants with a subsequent complicated course (surgical intervention and/or death) from those who had a non-complicated course. A cutoff value of 19 ng/mL for plasma I-FABP provided sensitivity and specificity of 88% and 88%, and a cutoff value of 232 ng/ml for urinary I-FABP gave sensitivity of 71% and specificity of 80% [29]. An unrelated study with a similar sample size evaluated serial measurements (every 24 h from onset of symptoms): The mean serum I-FABP level measured at 72 h was significantly higher in infants who underwent surgery compared to those who received medical treatment only (P = 0.001) [28]. In contrast is the single study that has shown that a LIT score greater than 4.5 (based on single blood measurement taken at clinical presentation) is able to distinguish those infants needing surgery from those who only required medical treatment, with sensitivity of 83% and specificity of 100% [27].
Collectively, these studies suggest that serial assessment of I-FABP alone or in combination with other markers in the first days following diagnosis of NEC may be helpful in prediction of the course of condition, especially regarding the need for surgical intervention. However, this concept remains to be validated in a larger trial.
I-FABP Correlates with Disease Extent at Laparotomy
As well as having a biomarker to indicate the need for surgery in infants with NEC, being able to predict the extent of disease prior to surgical intervention would be useful for surgeons when consulting parents on disease prognosis and for surgical planning. Two small studies showed that plasma I-FABP, urine I-FABP, and urine I-FABP:Cr were associated with disease extent at laparotomy [30, 31]. One study of nine infants with NEC also found that the level of I-FABP in urine at the onset of disease correlated significantly better than plasma I-FABP as regards the length of bowel resection needed (spearman 0.92, P = 0.001 versus spearman 0.68, P = 0.04, respectively) [31]. However, measurement of I-FABP in plasma (measured in 19 infants with NEC) was unable to differentiate between those infants needing small intestinal resection and those needing colonic resection [31]. An unrelated study found the urine I-FABP:Cr ratio in infants who had small intestinal involvement appeared higher than those with isolated or mainly colonic involvement [30]. This finding has potential clinical relevance, but larger studies are needed to provide evidence to support the concept of prognosticating outcome with I-FABP.
Summary
In summary, I-FABP is shown to be a moderately sensitive, but highly specific stand-alone biomarker for the diagnosis of NEC. The available evidence also suggests that diagnostic accuracy can be further improved by measuring I-FABP in combination with other biomarkers. Larger well-designed studies, however, are required to validate the potential for this biomarker to predict the need for surgical intervention and/or the extent of disease involvement in infants with NEC.
Acute Mesenteric Ischemia
Acute mesenteric ischemia (AMI) occurs when blood flow is unable to meet the metabolic demands of the intestinal mucosa [32]. Although the initial response is vasodilation, prolonged ischemia leads to vasoconstriction, activation of systemic inflammatory pathways, full-bowel wall thickness injury, infarction and eventually death. AMI can originate from various pathophysiological causes including vascular narrowing or blockage by a thrombus, mechanical volvulus, or any underlying process resulting in low blood pressure (e.g., shock or heart failure). Typically, AMI presents with sudden onset of symptoms such as severe abdominal pain, nausea or vomiting, indicative of an acute abdomen.
At present, diagnosis of AMI relies on the clinician’s clinical expertise, imaging findings, and general blood markers such as leukocyte count, base excess, lactate dehydrogenase, creatine kinase, alanine aminotransferase, and D-dimer level. Most of these clinically used markers are non-specific. For example, D-dimer assessment (a marker of thrombosis) for AMI, exhibits good sensitivity (96%) but poor specificity (40%) [33]. There is a clear need for more specific markers that could differentiate AMI from other causes of an acute abdomen and that might potentially serve as early indicators prompting earlier intervention.
I-FABP as a Marker of Enterocyte Damage in an Ischemic-Reperfusion Event
I-FABP is of particular interest in the context of AMI due to its responsiveness during an ischemic–reperfusion event [34, 35]. A study of 32 adults who underwent a pancreaticoduodenectomy (27 patients who had 6 cm of their jejunum removed underwent ischemia time of 15, 30 or 60 min followed by 30 and 120 min of reperfusion with comparison to five untreated controls) found plasma I-FABP levels progressively increased with ischemia time, and that this increase correlated with epithelial damage (r = − 0.82, P < 0.001) [35]. While I-FABP levels progressively declined following reperfusion, levels only returned to baseline in those patients who had 15 or 30 min ischemia time. This occurred 120 min after reperfusion, and the epithelial lining was restored. In contrast, I-FABP levels did not return to baseline at 120 min in the patients who had 60 min of ischemia time. This correlated with irrepairable epithelial damage, which manifested as markedly shortened villi exposing the subepithelial space [35]. Collectively, these findings suggest that I-FABP is a sensitive marker for enterocyte damage following a significant episode of ischemia.
I-FABP Compared to Other Clinical Markers
The identification of I-FABP as a sensitive marker of an ischemia–reperfusion event has informed other human studies comparing I-FABP to other established clinical blood markers. All but one of these studies found I-FABP to be the best diagnostic marker of AMI, evidenced by I-FABP having the largest AUC in receiver operating characteristic curve analyses [36,37,38,39,40,41]. One study involving 120 patients in a critical care setting, however, found d-lactate and l-lactate to be superior to I-FABP in the diagnosis of AMI [42]. Almost half (39) of the 81 patients in this study with unlikely or no intestinal ischemia were diagnosed with shock; these patients were potentially predisposed to some degree of enterocyte damage secondary to their shock, leading to release of I-FABP and limiting the differentiation from the AMI group. The two lactate markers were found to be more sensitive than I-FABP in this study. This may reflect the critically ill nature of the patient group, where l-lactate is likely to be elevated and d-lactate, which is exclusively produced by the bowel flora, is likely to translocate into the blood stream during a severe bowel ischemic event.
I-FABP as a Diagnostic Marker for AMI
Despite various studies supporting I-FABP as a specific diagnostic marker for AMI, there are a range of recommended I-FABP cutoff levels within the individual studies (with various sensitivities and specificities) (Table 3). The wide variation of optimal diagnostic thresholds could be due to a few reasons, such as having different study endpoints. For example, in the studies by Cronk et al. [36] and Kanda et al. [41], the definition of AMI was based on findings at surgery while other studies [39, 40] defined AMI according to imaging, surgical and histological findings. Other reasons may include the different underlying causes of AMI and whether cases of colonic ischemia were included in the studies. Matsumoto et al. [40] compared patients with small bowel vascular intestinal ischemia to non-vascular ischemia and another non-ischemia group, while Cronk et al. [36] only included mechanically strangulated small bowel in their cohort. Subsequently, Güzel et al. [38] included all patients with gastrointestinal ischemia (small bowel and/or colon) in their study.
A recent meta-analysis combined the results of 1246 patients (that includes most studies in Table 3) and found serum I-FABP could be a useful diagnostic marker of AMI in patients who present with acute abdominal symptoms [43]. The pooled sensitivity, specificity, positive and negative likelihood ratio, and AUC were 80% (95% CI 72–86%), 85% (95% CI 73–93%), 5.5 (95% CI 2.8–10.8), 0.23 (95% CI 0.15–0.35), and 0.86 (95% CI 0.83–0.89), respectively [43]. This study also found substantial heterogeneity in the sensitivity and specificity analysis due to the reasons discussed above.
Urine I-FABP as a Diagnostic Marker for AMI
Urine, as a less-invasive and easily accessible body fluid, has been increasingly utilized for I-FABP measurement as an alternative method of diagnosing AMI. Two small studies, involving 21 and 22 patients with AMI (included in Table 3), found urine I-FABP measurement may be comparable to (if not more sensitive than) blood I-FABP in diagnosing AMI [36, 44]. A larger sample size is needed to validate urinary I-FABP as an alternative way of diagnosing AMI.
GI FABP Markers in Predicting AMI Disease Location and Extent
Despite the diagnostic value of the I-FABP, this marker does not predict the disease location (whether ischemia involves the small intestine, colon or both), or the extent of ischemia. In studies that included small bowel and colon ischemia [38, 39, 44], only one study has addressed this question. Güzel et al. [38] measured serum levels in 30 patients with AMI and reported that I-FABP levels do not correlate with disease location or disease extent. In contrast, an unrelated study that evaluated plasma I-BABP levels in all patients with intestinal ischemia found this marker to have the potential in identifying those with ileal ischemia compared to those without ileal involvement, 18.4 ng/mL vs 2.9 ng/mL, respectively (P = 0.05) [44].
Summary
In summary, I-FABP appears to be a promising diagnostic marker for AMI. Most studies show that blood I-FABP is able to distinguish intestinal ischemia from non-ischemic events in the abdomen. However, it is unclear whether I-FABP can differentiate between small intestinal and colonic ischemia or determine the extent of ischemia, a point that highlights the need for well-defined study endpoints to be included in the design of future studies.
Celiac Disease
Celiac disease (CeD) is a common chronic immune-mediated enteropathy that affects up to 1.4% of the global population [45]. The condition is induced by persistent gluten exposure in genetically susceptible individuals, producing a range of classic gastrointestinal malabsorption symptoms and/or non-specific symptoms that include weight loss, failure to thrive, iron deficiency, headache, or osteoporosis [46].
I-FABP as an Adjunct Diagnostic Marker for Celiac Disease
Diagnosis of CeD typically relies on duodenal morphology using the Marsh–Oberhuber classification [47] after recognition of possible symptoms and measurement of various serological markers. This diagnosis is referred to as biopsy-proven. In 2012, the European Society of Paediatric Gastroenterology Hepatology and Nutrition (ESPGHAN) introduced a non-biopsy CeD-based protocol [48], but this has yet to be considered universally for children or for adults [49, 50]. There are many reasons why a simpler and less-invasive diagnostic process would be advantageous, and additional biomarkers may be able to guide and support this non-biopsy pathway.
Among the gastrointestinal FABPs, I-FABP is shown to be a better CeD marker than L-FABP, which likely reflects the specific expression of this FABP in the small intestine [7]. Blood and urine I-FABP levels positively correlate with the severity of villous atrophy (assessed as Marsh-Oberhuber grading histologically) and anti-tissue transglutaminase IgA (TTG-IgA) levels at diagnosis [7, 51, 52]. In addition, elevated I-FABP levels appear to be able to distinguish patients with CeD from patients with inflammatory bowel disease (IBD) [6], although this finding remains to be validated in a larger study. Collectively, these studies indicate a role for I-FABP as an alternative or adjunctive diagnostic marker for CeD.
In addition, measurement of I-FABP appears to be advantageous in children who do not fulfill the non-biopsy CeD criteria [53]. A sub-analysis of one study identified 30 children with anti-TTG-IgA levels < 10x upper limit of normal (ULN), and of these children, 14 (46.7%) children had plasma I-FABP > 450 pg/mL (defined to be abnormal by authors). All 14 patients were confirmed to have CeD by biopsy, which suggests that I-FABP may also have an adjunctive diagnostic role in pediatric CeD. The significance of this is the potential to reduce the need for intestinal biopsies, given that children having an endoscopy are usually given a general anesthetic.
I-FABP as a Monitoring Marker for Celiac Disease
Assessment of adherence to a gluten-free diet (GFD) following a diagnosis of CeD can be challenging. Systematic interviews by experienced dietitians or clinicians provide a subjective tool, but the only objective assessments routinely available are the normalization of celiac antibodies over time (reflecting mucosal recovery after starting a GFD), or repeat intestinal biopsies. Reports and meta-analysis have indicated that normalization of serological markers does not consistently reflect mucosal healing due to its low sensitivity in detecting persistent villous atrophy [54,55,56,57]. Furthermore, normalization of elevated serum TTG-IgA has been reported to take > 1 year in 75% of GFD adherent children with CeD [58]. Hence, there is a need for other markers to objectively monitor disease progression.
I-FABP has been identified as a useful marker in monitoring progress due to its rapid normalization following commencement of a GFD. In a follow-up study of 79 children with newly diagnosed CeD, both plasma I-FABP and TTG-IgA levels reduced significantly following three weeks of GFD. However, of these two markers, only I-FABP levels were found to have normalized (normal range < 450 pg/mL defined by study) at 26 weeks [53]. Similarly, in another study involving 20 children with CeD commencing a GFD, within three months after gluten withdrawal 80% of these children had I-FABP levels below the study threshold level of 224 pg/mL that best discriminates CeD (Marsh ≥ 3) from non-CeD [52].
Interestingly, in a study of 69 adults with CeD, I-FABP levels significantly reduced after six months of a GFD [51]. Subsequently, levels plateaued for another one to two years rather than normalizing to the levels seen in an individual without CeD, and despite repeatedly normal duodenal histology. In contrast, TTG-IgA levels normalized in 77% of these patients within two years of follow-up. Together, these findings suggest that further studies are needed to validate the I-FABP normalization threshold following the commencement of a GFD. There is a possibility that there may be no additional benefit in measuring I-FABP levels beyond 6 months.
I-FABP as a Marker for Refractory Celiac Disease (rCeD)
Most patients with CeD can be treated successfully with a GFD. However, a small group will develop refractory celiac disease (rCeD) despite strict adherence to a GFD. This can be defined as having persistent or recurrent symptoms of malabsorption and villous atrophy despite strict GFD [46]. The additional finding of aberrant intraepithelial T-cells characterizes type 2 rCeD, which is recognized to have a higher risk of developing enteropathy-associated T cell lymphoma.
Persistent elevation of I-FABP levels following commencement of GFD may suggest rCeD [51, 59], as evidenced in a subgroup of six patients in the I-FABP follow-up study (mean GFD of 19 months). These patients with persistently elevated I-FABP levels also scored at least Marsh ≥ 2 on repeat duodenal histology, despite some having normalized TTG-IgA (n = 3) or EMA (n = 3) [51]. A second study also identified 16 patients with rCeD had significantly elevated I-FABP levels compared to patients who showed mucosal recovery on a GFD [59]. In this study, a cutoff of 660 pg/mL gave the highest specificity and sensitivity (94% and 69%, respectively), in identifying rCeD. However, when I-FABP levels were assessed in conjunction with antibodies against luminal protein pancreatic GP2 protein (GP21), specificity was comparable (89%) and sensitivity increased to 80% [59]. These findings suggest that I-FABP alone or in combination with other markers may play a role in screening for rCeD, thereby facilitating prompt investigation and management.
I-FABP Role in Gluten Re-Challenge
Currently, a gluten re-challenge is required to confirm a diagnosis of CeD in situations where a GFD is commenced without adequate diagnostic assessment or when an individual wants to challenge their diagnosis. In general, adults are recommended to consume at least 3 g per day of gluten for 6 weeks [60] prior to endoscopy, whereas children need at least 10–15 g gluten per day for 4 to 6 weeks [61]. However, measurement of I-FABP may have a role in shortening the gluten challenge period prior to repeat endoscopy.
I-FABP during a gluten challenge has proven to be a more responsive marker than any of the conventional celiac serologies such as TTG-IgA, deamidated gliadin peptides (DGP IgA/IgG) or anti-actin (AAA-IgA) [62]. This study involved a 2-week gluten challenge in 20 adults with biopsy-proven CeD in remission (asymptomatic with normalized TTG-IgA levels) on a GFD for at least 12 months. I-FABP was the only marker significantly elevated by day 14 of the gluten challenge [62]. While the other serological markers did increase, maximum levels were seen at day 28, two weeks after commencement of a GFD. I-FABP levels in this study also positively correlated with the intraepithelial lymphocyte (IEL) count at baseline and at day 14 (r = 0.458, P = 0.042 and r = 0.654, P = 0.002, respectively). These outcomes suggest that using I-FABP as an early marker of gluten-induced enteropathy has the potential to greatly shorten the duration of a gluten challenge prior to histologic confirmation.
Summary
In short, I-FABP is shown to have a potential diagnostic and monitoring role in CeD. It appears that I-FABP in combination with TTG-IgA may be advantageous in the development of non-biopsy-based diagnostic protocols. Moreover, I-FABP appears to have potential as an indicator of mucosal recovery following commencement of a GFD, a biomarker of adherence to GFD and in the identification of those who are at risk of rCeD.
Inflammatory Bowel Disease
Inflammatory bowel disease (IBD) is a chronic relapsing inflammatory disorder of the GI tract, mainly divided into two subtypes known as Crohn’s disease (CD) and ulcerative colitis (UC) [63]. CD can manifest in any segment of the GI, most commonly involving the terminal ileum in adults [64] and the ileocolonic region in children [65]. On the other hand, UC is isolated to the colon, with more extensive disease typically seen in children than in adults [66].
I-FABP as a Marker of Monitoring Disease Progression and Disease Extent in IBD
The diagnosis of IBD involves a combination of clinical features, along with biochemical, endoscopic, histological, and radiological assessments. None of the three gastrointestinal FABP markers have been assessed as IBD diagnostic markers. However, I-FABP has been investigated regarding a role for monitoring remission and predicting disease extent.
Sarikaya et al. [67] measured serum I-FABP in 41 individuals with active CD, 33 with CD in remission, and 37 healthy controls. I-FABP was the highest in those with active disease and positively correlated with Crohn’s Disease Activity Index (CDAI) scores and C-reactive protein (CRP) levels (r = 0.319, P = 0.006 and r = 0.253, P = 0.008, respectively). Interestingly, another smaller study that involved ten adults with mostly active Crohn’s colitis found serum I-FABP levels to be reflective of tumor necrosis factor (TNF)-α levels [68]. Both markers were elevated prior to and reduced after anti-TNF-α antibody therapy. These data suggest that I-FABP could be a useful monitoring and prognostic marker in patients receiving anti-TNF-α treatment. However, neither of these two studies provided detailed descriptions of disease phenotype or follow-up endoscopic re-assessment for mucosal healing.
Measurement of I-FABP levels was less helpful in a Dutch study [69]. This report evaluated plasma I-FABP in adults with CD and UC. Endoscopically active disease was defined by a Simple Endoscopic Score ≥ 4 for CD or Mayo endoscopy sub-score ≥ 1 for UC, and clinically active disease was defined by using a combination of fecal calprotectin > 250ug/g, positive clinical activity index (Harvey-Bradshaw index > 4 for CD and Simple Clinical Colitis Activity Index > 3 for UC) and CRP > 5 mg/L. I-FABP was unable to differentiate between patients with active disease and those in remission, whether defined by endoscopic or clinical scores. The study also found that plasma I-FABP was not able to identify the active disease site in CD or UC.
Another study evaluated I-FABP levels in a group of 42 patients with UC [70]. Twenty-two patients had left-side colitis, and the other 20 patients were shown to have pancolitis. The mean serum I-FABP level was significantly higher in the patients with pancolitis compared to those with left-sided colitis (249.9 ± 58.4 pg/mL and 61.8 ± 8.5 pg/mL, respectively). Similarly, mean I-FABP level was significantly higher in those with severe disease (having an endoscopic score > 10 based on Meyers’ scoring system [71]) than those with mild disease (260.5 ± 60.6 pg/mL versus 61.5 ± 7.9 pg/mL, respectively). The authors concluded that elevation of I-FABP levels in the subjects with severe or pancolonic disease is secondary to potential backwash ileitis. This, however, remains to be validated.
Summary
To summarize, I-FABP does not appear to have sufficient sensitivity for use as a disease monitoring biomarker in IBD. However, some of the available data are based upon small cohorts, indicating a need for further evaluations.
Evaluation of FABPs in Other Gastrointestinal Conditions
Preliminary reports have evaluated these three FABPs in conditions such as cystic fibrosis-related enteropathy [72], chemotherapy-related intestinal enteropathy [73], intestinal transplantation [74], primary bile acid malabsorption [75], and intestinal related trauma [76, 77]. In addition, L-FABP has also been studied in extra-intestinal diseases such as nonalcoholic fatty liver disease [13] and insulin resistance [78].
Conclusions
Of the three gastrointestinal FABPs, I-FABP is of most interest due to its exclusive expression in the GI tract and its short half-life, allowing it to be a relatively sensitive disease marker. I-FABP elevation is mainly reflective of enterocyte damage, regardless of etiology. Overall, I-FABP has shown to be a promising diagnostic marker for NEC, AMI and CeD but not for IBD. Disease diagnostic accuracy may further improve when I-FABP is used in combination with other biomarkers. Sequential I-FABP measurements after diagnosis of NEC may prognosticate disease extent, allowing timely surgical intervention; however, this approach has not been explored for AMI. On the other hand, I-FABP seems to have a role in monitoring CeD where the expression falls significantly more quickly than anti-TTG-IgA following commencement of a GFD, providing the advantage of reassuring patients that mucosal recovery is progressing well. Unfortunately, there are currently insufficient data to use I-FABP as a disease monitoring biomarker in IBD. However, limited data based upon small studies do indicate a need for further evaluations.
L-FABP and I-BABP have also been studied in the setting of various diseases of the GI tract with limited evidence to date. The lower value of these two proteins in the setting of these conditions may reflect their lack of specificity to the intestinal tract compared to other complementary biomarkers.
References
Ockner RK, Manning JA, Poppenhausen RB, Ho WK. A binding protein for fatty acids in cytosol of intestinal mucosa, liver, myocardium, and other tissues. Science.. 1972;177:56–58.
Chmurzynska A. The multigene family of fatty acid-binding proteins (FABPs): function, structure and polymorphism. J Appl Genet.. 2006;47:39–48. https://doi.org/10.1007/BF03194597.
Storch J, Thumser AE. Tissue-specific functions in the fatty acid-binding protein family. The Journal of biological Chem.. 2010;285:32679–32683. https://doi.org/10.1074/jbc.R110.135210.
Rodriguez Sawicki L, Bottasso Arias NM, Scaglia N, et al. FABP1 knockdown in human enterocytes impairs proliferation and alters lipid metabolism. Biochim Biophys Acta Mol Cell Biol Lipids.. 2017;1862:1587–1594. https://doi.org/10.1016/j.bbalip.2017.09.006.
Lagakos WS, Gajda AM, Agellon L, et al. Different functions of intestinal and liver-type fatty acid-binding proteins in intestine and in whole body energy homeostasis. Am J Physiol Gastrointest Liver Physiol.. 2011;300:G803–G814. https://doi.org/10.1152/ajpgi.00229.2010.
Bottasso Arias NM, Garcia M, Bondar C, et al. Expression Pattern of Fatty Acid Binding Proteins in Celiac Disease Enteropathy. Mediators Inflamm.. 2015;2015:738563. https://doi.org/10.1155/2015/738563.
Derikx JP, Vreugdenhil AC, Van den Neucker AM, et al. A pilot study on the noninvasive evaluation of intestinal damage in celiac disease using I-FABP and L-FABP. J Clin Gastroenterol.. 2009;43:727–733. https://doi.org/10.1097/MCG.0b013e31819194b0.
Pelsers MMAL, Namiot Z, Kisielewski W, et al. Intestinal-type and liver-type fatty acid-binding protein in the intestine. Tissue distribution and clinical utility. Clin Biochem.. 2003;36:529–535. https://doi.org/10.1016/S0009-9120%2803%2900096-1.
Furuhashi M, Hotamisligil GS. Fatty acid-binding proteins: role in metabolic diseases and potential as drug targets. Nat Rev Drug Discov.. 2008;7:489–503. https://doi.org/10.1038/nrd2589.
Praslickova D, Torchia EC, Sugiyama MG, et al. The ileal lipid binding protein is required for efficient absorption and transport of bile acids in the distal portion of the murine small intestine. PLoS One.. 2012;7:e50810. https://doi.org/10.1371/journal.pone.0050810.
van de Poll MC, Derikx JP, Buurman WA, et al. Liver manipulation causes hepatocyte injury and precedes systemic inflammation in patients undergoing liver resection. World J Surg.. 2007;31:2033–2038. https://doi.org/10.1007/s00268-007-9182-4.
Thumser AE, Moore JB, Plant NJ. Fatty acid binding proteins: tissue-specific functions in health and disease. Curr Opin Clin Nutr Metab Care.. 2014;17:124–129. https://doi.org/10.1097/MCO.0000000000000031.
Wang G, Bonkovsky HL, de Lemos A, Burczynski FJ. Recent insights into the biological functions of liver fatty acid binding protein 1. J Lipid Res.. 2015;56:2238–2247. https://doi.org/10.1194/jlr.R056705.
Lin PW, Stoll BJ. Necrotising enterocolitis. Lancet.. 2006;368:1271–1283. https://doi.org/10.1016/S0140-6736(06)69525-1.
McGuire W, Anthony MY. Donor human milk versus formula for preventing necrotising enterocolitis in preterm infants: systematic review. Arch Dis Child Fetal Neonatal Ed.. 2003;88:F11–F14.
Lee JS, Polin RA. Treatment and prevention of necrotizing enterocolitis. Semin Neonatol.. 2003;8:449–459. https://doi.org/10.1016/S1084-2756(03)00123-4.
Yang G, Wang Y, Jiang X. Diagnostic value of intestinal fatty-acid-binding protein in necrotizing enterocolitis: a systematic review and meta-analysis. Indian J Pediatr.. 2016;83:1410–1419. https://doi.org/10.1007/s12098-016-2144-9.
Liu Y, Jiang L-F, Zhang R-P, Zhang W-T. Clinical significance of FABP2 expression in newborns with necrotizing enterocolitis. World J Pediatr WJP.. 2016;12:159–165. https://doi.org/10.1007/s12519-015-0035-1.
Cheng S, Yu J, Zhou M, Tu Y, Lu Q. Serologic intestinal-fatty acid binding protein in necrotizing enterocolitis diagnosis: a meta-analysis. BioMed Res Int.. 2015;2015:156704. https://doi.org/10.1155/2015/156704.
Lin JF, Chen JM, Zuo JH, et al. Meta-analysis: fecal calprotectin for assessment of inflammatory bowel disease activity. Inflamm Bowel Dis.. 2014;20:1407–1415. https://doi.org/10.1097/MIB.0000000000000057.
Reisinger KW, Van der Zee DC, Brouwers HAA, et al. Noninvasive measurement of fecal calprotectin and serum amyloid A combined with intestinal fatty acid-binding protein in necrotizing enterocolitis. J Pediatr Surg.. 2012;47:1640–1645. https://doi.org/10.1016/j.jpedsurg.2012.02.027.
Benkoe T, Baumann S, Weninger M, et al. Comprehensive evaluation of 11 cytokines in premature infants with surgical necrotizing enterocolitis. PLoS One.. 2013;8:e58720. https://doi.org/10.1371/journal.pone.0058720.
Cho SX, Berger PJ, Nold-Petry CA, Nold MF. The immunological landscape in necrotising enterocolitis. Expert Rev Mol Med.. 2016;18:e12. https://doi.org/10.1017/erm.2016.13.
Terrin G, Stronati L, Cucchiara S, De Curtis M. Serum markers of necrotizing enterocolitis: a systematic review. J Pediatr Gastroenterol Nutr.. 2017;65:e120–e132. https://doi.org/10.1097/MPG.0000000000001588.
Benkoe TM, Mechtler TP, Weninger M, Pones M, Rebhandl W, Kasper DC. Serum levels of interleukin-8 and gut-associated biomarkers in diagnosing necrotizing enterocolitis in preterm infants. J Pediatr Surg.. 2014;49:1446–1451. https://doi.org/10.1016/j.jpedsurg.2014.03.012.
Terrin G, Stronati L, Cucchiara S, De Curtis M. Serum markers of necrotizing enterocolitis: a systematic review. J Pediatr Gastroenterol Nutr.. 2017;65:e120–e132. https://doi.org/10.1097/MPG.0000000000001588.
Ng EW, Poon TC, Lam HS, et al. Gut-associated biomarkers L-FABP, I-FABP, and TFF3 and LIT score for diagnosis of surgical necrotizing enterocolitis in preterm infants. Ann Surg.. 2013;258:1111–1118. https://doi.org/10.1097/SLA.0b013e318288ea96.
Aydemir C, Dilli D, Oguz SS, et al. Serum intestinal fatty acid binding protein level for early diagnosis and prediction of severity of necrotizing enterocolitis. Early Hum Dev.. 2011;87:659–661. https://doi.org/10.1016/j.earlhumdev.2011.05.004.
Schurink M, Kooi EMW, Hulzebos CV, et al. Intestinal fatty acid-binding protein as a diagnostic marker for complicated and uncomplicated necrotizing enterocolitis: a prospective cohort study. PLoS One.. 2015;10:e0121336. https://doi.org/10.1371/journal.pone.0121336.
Evennett NJ, Hall NJ, Pierro A, Eaton S. Urinary intestinal fatty acid-binding protein concentration predicts extent of disease in necrotizing enterocolitis. J Pediatr Surg.. 2010;45:735–740. https://doi.org/10.1016/j.jpedsurg.2009.09.024.
Heida FH, Hulscher JBF, Schurink M, et al. Intestinal fatty acid-binding protein levels in Necrotizing Enterocolitis correlate with extent of necrotic bowel: results from a multicenter study. J Pediatr Surg.. 2015;50:1115–1118. https://doi.org/10.1016/j.jpedsurg.2014.11.037.
Clair DG, Beach JM. Mesenteric Ischemia. N Engl J Med.. 2016;374:959–968. https://doi.org/10.1056/NEJMra1503884.
Cudnik MT, Darbha S, Jones J, Macedo J, Stockton SW, Hiestand BC. The diagnosis of acute mesenteric ischemia: a systematic review and meta-analysis. Acad Emerg Med.. 2013;20:1087–1100. https://doi.org/10.1111/acem.12254.
Derikx JPM, Matthijsen RA, de Bruine AP, et al. Rapid reversal of human intestinal ischemia-reperfusion induced damage by shedding of injured enterocytes and reepithelialisation. PLoS One.. 2008;3:e3428. https://doi.org/10.1371/journal.pone.0003428.
Schellekens DHSM, Grootjans J, Dello SAWG, et al. Plasma intestinal fatty acid-binding protein levels correlate with morphologic epithelial intestinal damage in a human translational ischemia-reperfusion model. J Clin Gastroenterol.. 2014;48:253–260. https://doi.org/10.1097/MCG.0b013e3182a87e3e.
Cronk DR, Houseworth TP, Cuadrado DG, Herbert GS, McNutt PM, Azarow KS. Intestinal fatty acid binding protein (I-FABP) for the detection of strangulated mechanical small bowel obstruction. Curr Surg.. 2006;63:322–325. https://doi.org/10.1016/j.cursur.2006.05.006.
Kittaka H, Akimoto H, Takeshita H, et al. Usefulness of intestinal fatty acid-binding protein in predicting strangulated small bowel obstruction. PLoS One.. 2014;9:e99915. https://doi.org/10.1371/journal.pone.0099915.
Guzel M, Sozuer EM, Salt O, Ikizceli I, Akdur O, Yazici C. Value of the serum I-FABP level for diagnosing acute mesenteric ischemia. Surg Today.. 2014;44:2072–2076. https://doi.org/10.1007/s00595-013-0810-3.
Shi H, Wu B, Wan J, Liu W, Su B. The role of serum intestinal fatty acid binding protein levels and d-lactate levels in the diagnosis of acute intestinal ischemia. Clin Res Hepatol Gastroenterol.. 2015;39:373–378. https://doi.org/10.1016/j.clinre.2014.12.005.
Matsumoto S, Sekine K, Funaoka H, et al. Diagnostic performance of plasma biomarkers in patients with acute intestinal ischaemia. Br J Surg. 2014;101:232–238. https://doi.org/10.1002/bjs.9331.
Kanda T, Tsukahara A, Ueki K, et al. Diagnosis of ischemic small bowel disease by measurement of serum intestinal fatty acid-binding protein in patients with acute abdomen: a multicenter, observer-blinded validation study. J Gastroenterol.. 2011;46:492–500. https://doi.org/10.1007/s00535-011-0373-2.
van der Voort PHJ, Westra B, Wester JPJ, et al. Can serum l-lactate, d-lactate, creatine kinase and I-FABP be used as diagnostic markers in critically ill patients suspected for bowel ischemia. BMC Anesthesiol.. 2014;14:111. https://doi.org/10.1186/1471-2253-14-111.
Sun DL, Cen YY, Li SM, Li WM, Lu QP, Xu PY. Accuracy of the serum intestinal fatty-acid-binding protein for diagnosis of acute intestinal ischemia: a meta-analysis. Sci Rep.. 2016;6:34371. https://doi.org/10.1038/srep34371.
Thuijls G, van Wijck K, Grootjans J, et al. Early diagnosis of intestinal ischemia using urinary and plasma fatty acid binding proteins. Ann Surg.. 2011;253:303–308. https://doi.org/10.1097/SLA.0b013e318207a767.
Singh P, Arora A, Strand TA, et al. Global prevalence of celiac disease: systematic review and meta-analysis. Clin Gastroenterol Hepatol.. 2018;16:823–836. https://doi.org/10.1016/j.cgh.2017.06.037.
Lebwohl B, Sanders DS, Green PHR. Coeliac disease. Lancet.. 2018;391:70–81. https://doi.org/10.1016/S0140-6736(17)31796-8.
Oberhuber G, Granditsch G, Vogelsang H. The histopathology of coeliac disease: time for a standardized report scheme for pathologists. Eur J Gastroenterol Hepatol.. 1999;11:1185–1194.
Husby S, Koletzko S, Korponay-Szabo IR, et al. European society for pediatric gastroenterology, hepatology, and nutrition guidelines for the diagnosis of coeliac disease. J Pediatr Gastroenterol Nutr.. 2012;54:136–160. https://doi.org/10.1097/MPG.0b013e31821a23d0.
Tortora R, Imperatore N, Capone P, et al. The presence of anti-endomysial antibodies and the level of anti-tissue transglutaminases can be used to diagnose adult coeliac disease without duodenal biopsy. Aliment Pharmacol Ther.. 2014;40:1223–1229. https://doi.org/10.1111/apt.12970.
Efthymakis K, Serio M, Milano A, et al. Application of the biopsy-sparing ESPGHAN guidelines for celiac disease diagnosis in adults: a real-life study. Dig Dis Sci.. 2017;62:2433–2439. https://doi.org/10.1007/s10620-017-4672-1.
Adriaanse MPM, Tack GJ, Passos VL, et al. Serum I-FABP as marker for enterocyte damage in coeliac disease and its relation to villous atrophy and circulating autoantibodies. Aliment Pharmacol Ther.. 2013;37:482–490. https://doi.org/10.1111/apt.12194.
Vreugdenhil AC, Wolters VM, Adriaanse MP, et al. Additional value of serum I-FABP levels for evaluating celiac disease activity in children. Scand J Gastroenterol.. 2011;46:1435–1441. https://doi.org/10.3109/00365521.2011.627447.
Adriaanse MPM, Mubarak A, Riedl RG, et al. Progress towards non-invasive diagnosis and follow-up of celiac disease in children; a prospective multicentre study to the usefulness of plasma I-FABP. Sci Rep.. 2017;7:8671. https://doi.org/10.1038/s41598-017-07242-4.
Leonard MM, Weir DC, DeGroote M, et al. Value of IgA tTG in predicting mucosal recovery in children with celiac disease on a gluten-free diet. J Pediatr Gastroenterol Nutr.. 2017;64:286–291. https://doi.org/10.1097/MPG.0000000000001460.
Sharkey LM, Corbett G, Currie E, Lee J, Sweeney N, Woodward JM. Optimising delivery of care in coeliac disease—comparison of the benefits of repeat biopsy and serological follow-up. Aliment Pharmacol Ther.. 2013;38:1278–1291. https://doi.org/10.1111/apt.12510.
Vecsei E, Steinwendner S, Kogler H, et al. Follow-up of pediatric celiac disease: value of antibodies in predicting mucosal healing, a prospective cohort study. BMC Gastroenterol.. 2014;14:28. https://doi.org/10.1186/1471-230X-14-28.
Silvester JA, Kurada S, Szwajcer A, Kelly CP, Leffler DA, Duerksen DR. Tests for serum transglutaminase and endomysial antibodies do not detect most patients with celiac disease and persistent villous atrophy on gluten-free diets: a meta-analysis. Gastroenterology.. 2017;153:689–701. https://doi.org/10.1053/j.gastro.2017.05.015.
Gidrewicz D, Trevenen CL, Lyon M, Butzner JD. Normalization time of celiac serology in children on a gluten-free diet. J Pediatr Gastroenterol Nutr.. 2017;64:362–367. https://doi.org/10.1097/MPG.0000000000001270.
Gross S, Adriaanse MP, Nijeboer P, et al. Serum intestinal-fatty acid binding protein as a biomarker for refractory celiac disease. J Gastrointest Liver Dis JGLD.. 2015;24:258–259.
Oxentenko AS, Murray JA. Celiac disease: ten things that every gastroenterologist should know. Clin Gastroenterol Hepatol.. 2015;13:1396–1404. https://doi.org/10.1016/j.cgh.2014.07.024. quiz e127-9.
Murch S, Jenkins H, Auth M, et al. Joint BSPGHAN and Coeliac UK guidelines for the diagnosis and management of coeliac disease in children. Arch Dis Child.. 2013;98:806–811. https://doi.org/10.1136/archdischild-2013-303996.
Adriaanse MPM, Leffler DA, Kelly CP, et al. Serum I-FABP detects gluten responsiveness in adult celiac disease patients on a short-term gluten challenge. Am J Gastroenterol.. 2016;111:1014–1022. https://doi.org/10.1038/ajg.2016.162.
Abraham C, Cho JH. Inflammatory bowel disease. N Engl J Med.. 2009;361:2066–2078. https://doi.org/10.1056/NEJMra0804647.
Baumgart DC, Sandborn WJ. Crohn’s disease. Lancet.. 2012;380:1590–1605. https://doi.org/10.1016/S0140-6736(12)60026-9.
Goodhand J, Dawson R, Hefferon M, et al. Inflammatory bowel disease in young people: the case for transitional clinics. Inflamm Bowel Dis.. 2010;16:947–952. https://doi.org/10.1002/ibd.21145.
Levine A, de Bie CI, Turner D, et al. Atypical disease phenotypes in pediatric ulcerative colitis: 5-year analyses of the EUROKIDS Registry. Inflamm Bowel Dis.. 2013;19:370–377. https://doi.org/10.1002/ibd.23013.
Sarikaya M, Ergul B, Dogan Z, Filik L, Can M, Arslan L. Intestinal fatty acid binding protein (I-FABP) as a promising test for Crohn’s disease: a preliminary study. Clin Lab.. 2015;61:87–91.
Al-Saffar AK, Meijer CH, Gannavarapu VR, et al. Parallel changes in harvey-bradshaw index, TNFalpha, and intestinal fatty acid binding protein in response to infliximab in crohn’s disease. Gastroenterol Res Pract.. 2017;2017:1745918. https://doi.org/10.1155/2017/1745918.
Bodelier AGL, Pierik MJ, Lenaerts K, et al. Plasma intestinal fatty acid-binding protein fails to predict endoscopic disease activity in inflammatory bowel disease patients. Eur J Gastroenterol Hepatol.. 2016;28:807–813. https://doi.org/10.1097/MEG.0000000000000616.
Wiercinska-Drapalo A, Jaroszewicz J, Siwak E, Pogorzelska J, Prokopowicz D. Intestinal fatty acid binding protein (I-FABP) as a possible biomarker of ileitis in patients with ulcerative colitis. Regul Pept.. 2008;147:25–28. https://doi.org/10.1016/j.regpep.2007.12.002.
Meyers S, Sachar DB, Present DH, Janowitz HD. Olsalazine in the treatment of ulcerative colitis among patients intolerant of sulphasalazine: a prospective, randomized, placebo-controlled, double-blind, dose-ranging clinical trial. Scand J Gastroenterol Suppl.. 1988;148:29–37.
Adriaanse MPM, van der Sande LJTM, van den Neucker AM, et al. Evidence for a cystic fibrosis enteropathy. PLoS One.. 2015;10:e0138062. https://doi.org/10.1371/journal.pone.0138062.
Derikx JPM, Blijlevens NMA, Donnelly JP, et al. Loss of enterocyte mass is accompanied by diminished turnover of enterocytes after myeloablative therapy in haematopoietic stem-cell transplant recipients. Ann Oncol Off J Eur Soc Med Oncol.. 2009;20:337–342. https://doi.org/10.1093/annonc/mdn579.
Kaufman SS, Lyden ER, Marks WH, et al. Lack of utility of intestinal fatty acid binding protein levels in predicting intestinal allograft rejection. Transplantation.. 2001;71:1058–1060.
Balesaria S, Pell RJ, Abbott LJ, et al. Exploring possible mechanisms for primary bile acid malabsorption: evidence for different regulation of ileal bile acid transporter transcripts in chronic diarrhoea. Eur J Gastroenterol Hepatol.. 2008;20:413–422. https://doi.org/10.1097/MEG.0b013e3282f41b82.
Relja B, Szermutzky M, Henrich D, et al. Intestinal-FABP and liver-FABP: Novel markers for severe abdominal injury. Acad Emerg Med Off J Soc Acad Emerg Med.. 2010;17:729–735. https://doi.org/10.1111/j.1553-2712.2010.00792.x.
Timmermans K, Sir O, Kox M, et al. Circulating iFABP Levels as a marker of intestinal damage in trauma patients. Shock (Augusta, Ga).. 2015;43:117–120. https://doi.org/10.1097/SHK.0000000000000284.
Shi J, Zhang Y, Gu W, et al. Serum liver fatty acid binding protein levels correlate positively with obesity and insulin resistance in Chinese young adults. PLoS One.. 2012;7:e48777. https://doi.org/10.1371/journal.pone.0048777.
Gollin G, Stadie D, Mayhew J, et al. Early detection of impending necrotizing enterocolitis with urinary intestinal fatty acid-binding protein. Neonatology.. 2014;106:195–200. https://doi.org/10.1159/000362497.
Coufal S, Kokesova A, Tlaskalova-Hogenova H, Snajdauf J, Rygl M, Kverka M. Urinary intestinal fatty acid-binding protein can distinguish necrotizing enterocolitis from sepsis in early stage of the disease. J Immunol Res.. 2016;2016:5727312. https://doi.org/10.1155/2016/5727312.
Thuijls G, Derikx JPM, van Wijck K, et al. Non-invasive markers for early diagnosis and determination of the severity of necrotizing enterocolitis. Ann Surg.. 2010;251:1174–1180. https://doi.org/10.1097/SLA.0b013e3181d778c4.
Gregory KE, Winston AB, Yamamoto HS, et al. Urinary intestinal fatty acid binding protein predicts necrotizing enterocolitis. J Pediatr.. 2014;164:1486–1488. https://doi.org/10.1016/j.jpeds.2014.01.057.
Mannoia K, Boskovic DS, Slater L, Plank MS, Angeles DM, Gollin G. Necrotizing enterocolitis is associated with neonatal intestinal injury. J Pediatr Surg.. 2011;46:81–85. https://doi.org/10.1016/j.jpedsurg.2010.09.069.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Disclosure
SSCH is supported by a Freemasons Paediatric Postgraduate Scholarship.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ho, S.S.C., Keenan, J.I. & Day, A.S. The Role of Gastrointestinal-Related Fatty Acid-Binding Proteins as Biomarkers in Gastrointestinal Diseases. Dig Dis Sci 65, 376–390 (2020). https://doi.org/10.1007/s10620-019-05841-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-019-05841-x