Abstract
Introduction
The association between early resuscitation volume and clinical outcomes remains controversial in acute pancreatitis. In the present study, we aimed to identify the association between resuscitation volume and the development of acute kidney injury (AKI) and other clinical outcome metrics.
Methods
Patients admitted to our center with moderately severe acute pancreatitis (MSAP) and severe acute pancreatitis (SAP) from January 2009 to December 2013 were reviewed retrospectively. Patients were stratified into two groups on the basis of the volume of fluid infused during the first 24 h. The primary clinical endpoint was incidence of AKI. Moreover, AKI lasting time, utilization of continuous renal replacement therapy and lasting time, creatinine increase, and other clinical metrics were also compared. The potential risk factors of new-onset AKI were also analyzed.
Results
A total of 179 patients were included, and aggressive fluid resuscitation (≥ 4 l) was associated with increased incidence of AKI compared with nonaggressive group (53.12% vs. 25.64%, p = 0.008), longer AKI lasting time (p = 0.038), and increased creatinine increase (p < 0.001) during hospitalization. Moreover, utilization of continuous renal replacement therapy was more frequent in aggressive group (40.63% vs. 24.36%, p = 0.108), and the lasting time of continuous renal replacement therapy was also longer (p = 0.181), though both not statistically different. Moreover, in multivariate analysis, aggressive resuscitation [OR 4.36 (1.52–13.62); p = 0.001] and chloride exposure [OR 2.53 (1.26–5.21); p = 0.012] in the first 24 h were risk factors of new-onset AKI.
Conclusion
In patients with MSAP and SAP, aggressive fluid resuscitation was associated with increased incidence and longer duration of AKI. Moreover, aggressive resuscitation and chloride exposure in the first 24 h were risk factors of new-onset AKI.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The causes of hypovolemia are multifactorial in acute pancreatitis (AP), including vomiting, reduced oral intake, third spacing of fluids, and diaphoresis. Consequently, tissue hypoperfusion could develop, leading to organ dysfunctions, especially for the kidney which is sensitive to insufficient perfusion. It has been reported that 25–59.5% patients developed acute kidney injury (AKI) during the natural course of severe form of AP [1, 2]. Previous guidelines for the management of AP suggested that an aggressive fluid resuscitation (300–500 ml/h for the first 6 h and then 250 ml/h to maintain blood volume) contributed to maintaining stable and adequate intravascular volume in organs such as the kidney [3]. However, aggressive fluid resuscitation is reported to be a double-edge sword as excessive fluid admission would aggravate tissue edema [4] and result in impaired oxygen delivery due to a hemodilution-induced decrease in hematocrit (HCT) [5].Therefore, an appropriate early fluid resuscitation protocol is of important clinical value in treating AP, as adequate resuscitation may help prevent the development of potential organ dysfunction.
Unfortunately, no consensus on the early fluid resuscitation of AP has been reached yet. To date, only 10 humans studies regarding early resuscitation exist and some of them only focused on mild form of acute pancreatitis [6,7,8,9]. Patients with mild form of AP mostly do not suffer severe hypovolemia, so fluid resuscitation may not affect outcome significantly. Other studies focused on more severe form of AP [4, 10,11,12,13,14], and the definitions of aggressive resuscitation or nonaggressive resuscitation varied from center to center. In addition, none of these studies clearly clarified the relationship between resuscitation volume in the first 24 h and clinical outcomes. In the present study, we aimed to identify the association between resuscitation volume and the development of AKI and other clinical outcome metrics.
Methods
Participants
From January 2009 to December 2013, a consecutive series of patients with AP admitted to the surgical intensive care unit of the institute of General Surgery, Jinling Hospital within 72 h from the onset of the disease were reviewed retrospectively. Our center is a national referral center for AP, and we treat more than 200 patients every year. Diagnosis of AP was based on abdominal pain suggesting AP, serum amylase at least three times the upper limit of normal or computed tomography, and patients were defined as different stages of AP on the basis of the development of (peri)pancreatic necrosis and organ failure according to the revised Atlanta classification [15]. Patients were classified as SAP and MSAP. SAP was defined as objective evidence of organ failure lasts longer than 48 h (e.g., circulatory shock, acute renal failure, acute pulmonary failure) as defined in the Atlanta classification and/or local complications of necrosis (e.g., acute peripancreatic fluid collection, acute necrotic collection, walled-off necrosis, abscess of pseudocyst). Moderately severe acute pancreatitis (MSAP) is characterized by the presence of transient organ failure or local or systemic complications in the absence of persistent organ failure. We excluded patients with mild form of AP according to revised Atlanta classification so as to enroll more patients suffered from hypoperfusion. Moreover, patients were excluded if there was a known history of AP, chronic pancreatitis, cardiovascular dysfunction on admission, cancer on admission, pregnancy on admission, or age younger than 18.
Ethics Statement
Each participant provided written informed consent after being provided with an explanation of the study by phone, letter, or email. The study was conducted in accordance with the ethical principles contained within the Declaration of Helsinki. This study was also reviewed by the Institutional Review Board of Jinling hospital.
Management
All patients received standard medical treatment according to the guidelines [3]. Dynamic electrocardiogram monitoring system was used to detect the basic vital sign and artery oxygen saturation for all patients while Pulse index Contour Continuous Cardiac Output was used when patients developed shock. For nutritional support, early enteral nutrition (within 48 h) was applied during the study period. Prophylactic antibiotics were routinely adopted in patients with moderate AP or above. Infected pancreatic necrosis was treated using surgical drainage including percutaneous drainage, negative-pressure irrigation, and endoscopic or surgical necrosectomy. Our criteria for transferring patients from SICU (Severe acute pancreatitis Intensive Care Unit) to general wards are patients without any of the followings: organ dysfunction, uncontrolled bleeding, severe infection complications like sepsis, unstable hemodynamics.
For the fluid administration, no specific early resuscitation protocol was available during the study period in our center. The goals of early fluid resuscitation in our center are to keep the basic vital sign stable, HCT below 45%, and to maintain urine output more than 0.5 ml/(kg h) in patients without AKI according to the physicians who were on duty. Moreover, saline and Ringer lactate are the mostly used for early fluid resuscitation in our center, while 5% albumin and 20% albumin were only seldom used in the early fluid resuscitation. Other types of fluid would also be administrated when necessary. For example, 5% sodium bicarbonate solution was adopted to reverse severe acidosis, while 5% fructopyranose or 5% fructose and sodium chloride solution were adopted when there was a hyperglycemia. In our center, intravenous administration was the only way for fluid administration within 24 h of presentation as oral intake of fluid was unallowed in the first day.
Definitions
Definitions of aggressive resuscitation or nonaggressive resuscitation in previous studies vary from center to center, lacking a unified standard. We used a 4 l resuscitation volume to divide patients into two groups as it was the upper limit of nonaggressive resuscitation as well as an average of aggressive resuscitation volume and nonaggressive resuscitation volume in previous studies.
AKI was defined when serum level increased more than 1.5 times of baseline or increased more than 0.3 mg/dl or urine output decreased below 0.5 ml/(kg h) for more than six hours according to acute kidney injury network (AKIN) classification [16], while new-onset AKI was defined if patients developed AKI after admission. The lasting time of AKI was defined as the time from diagnosis of AKI to the time when the kidney function went back to normal. The definitions of organ dysfunction were based on a score of 2 or more in the sequential organ failure assessment (SOFA) scoring system [17]. MODS was defined as the combined dysfunction of 2 major organ systems [18]. ACS (abdominal compartment syndrome) was defined as sustained intra-abdominal pressure (IAP) of > 20 mm Hg with the presence of an attributable organ failure. Sepsis was defined when patients developed SIRS as well as infection according to Surviving Sepsis Campaign Guidelines Committee [19]. Hypoperfusion was defined if a blood lactate concentration was above 4 mmol/l or oliguria (urine output < 0.5 ml/(kg h) for more than 6 h). Cardiovascular dysfunction was defined if mean arterial pressure (MAP) was lower than 65 mmHg after adequate fluid was loaded or vasoactive agents were needed to maintain MAP ≥ 65 mmHg. Pancreatic necrosis was diagnosed according to the results of contrast-enhanced computed tomography performed at least 48 h after the onset of the disease. Our criteria for the diagnosis of pancreatic infection are as follows: positive findings in bacterial culture of abdominal fluid and repeated temperature increases.
Data Collection and Outcome Measures
Baseline data including age, sex, etiology, the SOFA score, Ranson score, the APACHE II score, lactate, HCT, body weight, and the incidence of hypoperfusion were recorded on admission. SOFA score and APACHE II score were assessed on a daily basis during days 1–3 after admission. Chloride exposure in the first 24 h was also collected. The development of other systemic and local complications, such as systemic inflammatory response syndrome (SIRS) and pancreatic pseudocyst, the utilization of vasoactive agents and mechanical ventilation, the duration of both hospital and ICU (Intensive Care Unit) stay, the need for surgical intervention and hospital mortality were also recorded. In all patients, incidence of AKI on admission, the most serious diagnosis of AKI (final diagnosis), and AKI lasting time during hospitalization were recorded, as well as CRRT (continuous renal replacement therapy) utilization, creatinine increase (creatinine increased from baseline to peak creatinine level during hospitalization) and daily urine output.
Statistical Analysis
Data were analyzed using SPSS 17.0 for Windows (SPSS, Chicago, IL, USA). All statistical tests were two-tailed, and significance level was set at p < 0.05. Student T test was adopted to analyze continuous variables (like fluid volume, SOFA score) assessed by t test between the aggressive resuscitation and nonaggressive resuscitation group and expressed as mean ± SD. Other quantitative data were analyzed by Mann–Whitney test and expressed as mean (the 25% percentile–the 75% percentile), while all classable data were analyzed by Chi-square test and were expressed as number (percentage). The potential risk factors of new-onset AKI were analyzed (including sex, age, etiology, APACHE II score, SOFA score, aggressive resuscitation, SIRS, Hypoperfusion, Lactate, HCT, Body weight, Creatinine). Continuous variables were assessed using t test or nonparametric Mann–Whitney U test as indicated in the univariate analysis. Continuous variables were also transformed to categorical variates (ordinal variates when needed) based on prior studies and clinical experience. Chi-squared analysis or Fisher’s exact test was used for categorical variables. A logistic regression model was used for multivariate analysis to identify the independent risk factors for new-onset AKI, odds ratios (ORs) and 95% confidence intervals (CIs) calculated. Statistical analyses were conducted at a significance level of 0.10 for univariate analysis and 0.05 for multivariate analysis.
Results
Patient Characteristics
A total of 1055 patients admitted to our center from January 2009 to December 2013 were screened for inclusion. Five of them were with cancer; 18 patients were pregnant; 69 patients were without organ dysfunction and pancreatic necrosis; 7 patients developed cardiovascular dysfunction when admitted to our hospital; and 846 patients were not within 72 h from the onset of AP. As a result, a total of 179 patients with AP were enrolled in this retrospective study including 55 patients in the aggressive fluid resuscitation group and 124 patients in the nonaggressive fluid resuscitation group.
Table 1 shows the demographic and clinical data of these patients. There was no significant difference between two groups in terms of age, sex, etiology, and comorbidities. Moreover, no significant differences were observed in terms of HCT level, lactate level, development of hypoperfusion, development of SIRS (80.65% vs. 83.64%, p = 0.682), and body weight between the two groups on admission. Regarding severity on admission, there were also no significant differences in several scoring systems such as APACHE II score, Ranson score, and SOFA Score, and in laboratory parameters associated with severity including the first 3 days creatinine levels (p > 0.05), as well as in diagnosis of AKI (Table 2) on admission (p > 0.05).
Relationship Between Aggressive Resuscitation and the Development of Acute Kidney Injury in AP
However, more patients developed AKI (52.73%) in the aggressive fluid resuscitation group (Table 2) during hospitalization compared to 28.23% in the nonaggressive fluid resuscitation group (p = 0.002). Moreover, significantly more new-onset AKI cases were detected in patients receiving aggressive fluid resuscitation when compared with the nonaggressive group (16.36% vs. 4.84%, p = 0.017). In addition, significant differences could be observed in stage 2 of final diagnosis of AKI (p = 0.003), while no differences were observed in stage 1 or stage 3 between the two groups (Table 2). Further data also revealed that patients in aggressive fluid resuscitation group suffered a longer AKI lasting time (Fig. 1, p = 0.038). Besides that, utilization of CRRT was more frequent in the aggressive group (47.27% vs. 30.65%, p = 0.042. Increase from baseline to peak creatinine level (Table 3) was also higher (0.85 (0.23–1.09) versus 0.35 (0.00–0.30) mg/dl, p < 0.001). There were no differences in terms of the development of oliguria on admission (Fig. 2). However, more patients in the following seven days developed oliguria in aggressive group, though there were not statistical differences. Subgroup analysis demonstrated that patients with new-onset AKI received significantly more resuscitation fluid than others (4501 (3237–5916) versus 3316 (2655–3909) ml, p = 0.002). And there were no differences in resuscitation volume between APACHE II score on admission ≥ 8 group and APACHE II score on admission < 8 group (3550 ± 1380 vs. 3526 ± 1058 ml, p = 0.928).
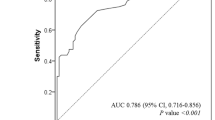
To further investigate the relationship between aggressive resuscitation and the development of AKI in AP, we analyzed the potential risk factors of new-onset AKI, and 49 patients with pre-exiting AKI were excluded. Factors including sex, age, etiology, APACHE II score, SOFA score, aggressive resuscitation, SIRS, hypoperfusion, lactate, HCT, body weight, creatinine were analyzed by univariate analysis. Among the included potential risk factors, 5 were significantly different between patients with and without new-onset AKI patients. Logistic regression analysis results showed that aggressive resuscitation and chloride exposure in the first 24 h were independently associated with new-onset AKI (Table 4).
Clinical Outcomes Between Aggressive Fluid Resuscitation Group and Nonaggressive Fluid Resuscitation Group in AP
For other clinical outcome measures, there were no significant differences in terms of pancreatic necrosis, pancreatic pseudocyst, pancreatic infection, operation intervention, utilization of vasoactive agents, utilization of mechanical ventilation, mechanical ventilation day, hospital day, ICU day, and hospital mortality between the two groups (Table 5). Nonetheless, a tendency of worse outcome in aggressive group was observed, such as the incidence of MODS (47.27% vs. 24.19%, p = 0.003), ACS (7.27% vs. 0.81, p = 0.037).
Discussion
Early fluid resuscitation is crucial to the management of AP and hitherto existing guidelines for the management of AP mostly recommended an aggressive resuscitation therapy strategy to improve long-term outcome [3]. However, the association between fluid resuscitation and renal function has not been well studied and studies in hemorrhagic shock had clearly demonstrated that limited fluid resuscitation could improve clinical outcomes and prevent potential organ dysfunctions [20, 21]. In this study, our results suggest that patients receiving aggressive fluid resuscitation suffered significant higher rate of AKI and longer AKI lasting time (p < 0.05). Worse but no statistically different outcomes of patients in the aggressive group were also observed illustrated by higher incidence rate of MODS, longer hospital duration, etc., although no difference in fluid loss and disease severity could be seen at admission, as evidenced by similar levels of HCT, APACHEII score, Ranson score, and SOFA score.
The following mechanisms may explain this phenomenon. First, it is without doubt that the ultimate goal of fluid resuscitation is to reduce tissue hypoxia. However, it has been reported that in some patients, fluid resuscitation increased cardiac output remarkably while oxygen delivery and oxygen consumption remain unchanged or even decreased [5]. This was due to a hemodilution-induced decrease in HCT. A significant increase in HCT has been noted as a danger signal requiring urgent fluid resuscitation in the early stage of AP [22], and it has been used as a resuscitation goal for decades in the early fluid resuscitation of AP. However, studies by Mao et al. [4, 11] demonstrated that rapid hemodilution (HCT decreased below 35% within the first 24 h) was associated with worst clinical outcomes. In our study, both of the two groups showed high HCT levels [44.77 (41.20–49.30)% vs. 43.69 (38.03–50.53)%, p = 0.608] at admission and after first 24-h resuscitation, HCT of patients in both groups decreased significantly. Moreover, aggressive resuscitation is mostly accompanied by edema, which may also contribute to the development of AKI in three different ways [23]: First, visceral edema secondary to aggressive resuscitation has been considered as a risk factor for intra-abdominal hypertension, which can consequently cause compromised renal blood flow and ultimately resulting in AKI [24, 25]. Second, excessive chloride accompanied with aggressive resuscitation has been shown to impair renal function as well [26]. Third, diuretics frequently used to treat edema may further contribute to worsening of renal dysfunction [27].
Recently, accumulative evidence had shown the correlation between hyperchloremia and AKI in critically ill and other clinical situations [28,29,30,31]. Increased plasma chloride is a common consequence of short-time rapid fluid resuscitation with crystalloids (saline mostly), which is a repeatedly recommended therapeutic measure for patients in shock or with dehydration in the early phases of acute pancreatitis [32,33,34]. The frequent use of saline in patients with SAP could probably lead to a considerable chloride load which can be clinically relevant [35]. So we collected the data of chloride exposure in the first 24 h (mEq) after admission in these patients and made a comparison between the aggressive and nonaggressive groups, but find no difference (425.38 ± 35.12 vs. 407.63 ± 12.56, p = 0.553) (Table 1). We also did additional univariate and multivariate analyses to further clarify its role in AKI development. We found that chloride exposure in the first 24 h was higher in patients with new-onset AKI (506.0 ± 43.0) than patients without AKI (335.3 ± 17.5) and was a risk factor of new-onset AKI in SAP patients even adjusted for fluid volume in the multivariate analysis (p = 0.012).
Some previous studies demonstrated that severity of AP on admission is associated with resuscitation volume evidenced by patients in ICU who received more fluid than other patients [12]. But in our study, there were no differences in the resuscitation volume between patients with APACHE II score on admission ≥ 8 and patients with APACHE II score on admission < 8. This may be due to the factor that patients with cardiovascular dysfunction on admission were excluded in our study but not in previous ones. Moreover, there was no difference in volume depletion between the aggressive and nonaggressive groups evidenced by comparable HCT level, lactate level, and the presence of hypoperfusion and SIRS before resuscitation. Body weight at admission, which may bring bias to the resuscitation volume, also showed no difference between the two study groups.
As fluid strategy is much less important in patients with mild AP, we classified patients according to Atlanta classification of AP and excluded patients with mild form of AP to ensure that most patients enrolled presented hypoperfusion at admission. When it comes to the other studies focusing on severe form of AP, studies by Gardner et al. [13] and Brown et al. [14] demonstrated that aggressive resuscitation could improve mortality and inadequate resuscitation was associated with pancreatic necrosis, which were in contrast to our results. However, in both of the two studies, HCT level, a poor indicator for severity [36], was the only variable used to compare severity, making their results less clinically reliable. Moreover, they did not examine the rate of AKI which was the primary end point of this study.
Some other studies which were consistent with our study demonstrated that rapid hemodilution was associated with mortality [4, 10, 11]. However, in these studies, patients with cardiovascular dysfunction at admission were included and subgroup analysis was not available. As there is no doubt that these patients needed much more fluid to maintain MAP and showed higher mortality rate, inclusion of them would certainly impact the results. During our study period, a total of 7 patients developed cardiovascular dysfunction at admission and they showed remarkably high mortality (71.43%) and received a median of 7881 ml resuscitation volume within the first 24 h. Obviously, these patients developed a significantly different course of the disease from the others, and thus, addition of them to the analysis might bring a considerable bias to the study.
In general, patients in our study presented with more severe form of AP, making it more clinically valuable, as early resuscitation strategy is thought to be more decisive in these patients. Moreover, our study got a longer observational period and included more metrics mainly focusing on the severity, duration, and treatment of AKI.
Nonetheless, our study is with its limitations. First of all, it was a retrospective study, so we could not study the relationship between resuscitation volume and cardiac output, oxygen delivery, or oxygen consumption, if any; it might offer more clinical information. Second, the sample size was relatively small in the aggressive group. It is possible that the lack of difference in mortality and other clinical outcome measures is partly related to the small number of patients studied. Finally, for the fluid administration, no rigorous early resuscitation protocol was available during the study period in our center. The final decision regarding administration of fluid was decided according to the physician’s judgment rather than a previously implemented resuscitation protocol.
Conclusion
In patients with MSAP and SAP according to the Atlanta classification, aggressive fluid resuscitation was associated with increased incidence of AKI and longer duration of AKI. Moreover, aggressive resuscitation and chloride exposure in the first 24 h were risk factors of new-onset AKI.
References
Wig JD, Bharathy KG, Kochhar R, et al. Correlates of organ failure in severe acute pancreatitis. JOP. 2009;10:271–275.
Vege SS, Gardner TB, Chari ST, et al. Low mortality and high morbidity in severe acute pancreatitis without organ failure: a case for revising the Atlanta classification to include “moderately severe acute pancreatitis”. Am J Gastroenterol. 2009;104:710–715.
Tenner S, Baillie J, DeWitt J, et al. American College of Gastroenterology guideline: management of acute pancreatitis. Am J Gastroenterol. 2013;108(9):1400–1415; 1416.
Mao EQ, Fei J, Peng YB, et al. Rapid hemodilution is associated with increased sepsis and mortality among patients with severe acute pancreatitis. Chin Med J (Engl). 2010;123:1639–1644.
Monnet X, Julien F, Ait-Hamou N, et al. Lactate and venoarterial carbon dioxide difference/arterial-venous oxygen difference ratio, but not central venous oxygen saturation, predict increase in oxygen consumption in fluid responders. Crit Care Med. 2013;41:1412–1420.
Warndorf MG, Kurtzman JT, Bartel MJ, et al. Early fluid resuscitation reduces morbidity among patients with acute pancreatitis. Clin Gastroenterol Hepatol. 2011;9:705–709.
Wall I, Badalov N, Baradarian R, et al. Decreased mortality in acute pancreatitis related to early aggressive hydration. Pancreas. 2011;40:547–550.
Kuwabara K, Matsuda S, Fushimi K, et al. Early crystalloid fluid volume management in acute pancreatitis: association with mortality and organ failure. Pancreatology. 2011;11:351–361.
de-Madaria E, Soler-Sala G, Sanchez-Paya J, et al. Influence of fluid therapy on the prognosis of acute pancreatitis: a prospective cohort study. Am J Gastroenterol. 2011;106(10):1843–1850.
Mao EQ, Tang YQ, Fei J, et al. Fluid therapy for severe acute pancreatitis in acute response stage. Chin Med J (Engl). 2009;122:169–173.
Mao EQ, Tang YQ, Li L, et al. Strategy of controlling fluid resuscitation for severe acute pancreatitis in acute phase. Zhonghua Wai Ke Za Zhi. 2007;45:1331–1334.
Eckerwall G, Olin H, Andersson B, et al. Fluid resuscitation and nutritional support during severe acute pancreatitis in the past: what have we learned and how can we do better? Clin Nutr. 2006;25:497–504.
Gardner TB, Vege SS, Chari ST, et al. Faster rate of initial fluid resuscitation in severe acute pancreatitis diminishes in-hospital mortality. Pancreatology. 2009;9:770–776.
Brown A, Baillargeon JD, Hughes MD, et al. Can fluid resuscitation prevent pancreatic necrosis in severe acute pancreatitis? Pancreatology. 2002;2:104–107.
Dellinger EP, Forsmark CE, Layer P, et al. Determinant-based classification of acute pancreatitis severity: an international multidisciplinary consultation. Ann Surg. 2012;256:875–880.
Mehta RL, Kellum JA, Shah SV, et al. Acute Kidney Injury Network: report of an initiative to improve outcomes in acute kidney injury. Crit Care. 2007;11:R31.
Vincent JL, Moreno R, Takala J, et al. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the working group on sepsis-related problems of the European Society of Intensive Care Medicine. Intensive Care Med. 1996;22(7):707–710.
Marshall JC, Cook DJ, Christou NV, et al. Multiple organ dysfunction score: a reliable descriptor of a complex clinical outcome. Crit Care Med. 1995;23:1638–1652.
Dellinger RP, Levy MM, Rhodes A, et al. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2012. Crit Care Med. 2013;41:580–637.
Devlin JJ, DeVito SS, Littlejohn LF, et al. Terlipressin with limited fluid resuscitation in a swine model of hemorrhage. J Emerg Med. 2013;45:78–85.
Li Y, Guo M, Shen J, et al. Limited fluid resuscitation attenuates lung and intestine injury caused by hemorrhagic shock in rats. J Invest Surg. 2014;27:81–87.
Yashiro M, Hamada Y, Matsushima H, et al. Estimation of filtration coefficients and circulating plasma volume by continuously monitoring hematocrit during hemodialysis. Blood Purif. 2002;20:569–576.
Tsai YC, Tsai JC, Chen SC, et al. Association of fluid overload with kidney disease progression in advanced CKD: a prospective cohort study. Am J Kidney Dis. 2014;63(1):68–75.
Cheatham ML, Malbrain ML, Kirkpatrick A, et al. Results from the international conference of experts on intra-abdominal hypertension and abdominal compartment syndrome. II. Recommendations. Intensive Care Med. 2007;33:951–962.
Dalfino L, Tullo L, Donadio I, et al. Intra-abdominal hypertension and acute renal failure in critically ill patients. Intensive Care Med. 2008;34:707–713.
Yunos NM, Bellomo R, Hegarty C, et al. Association between a chloride-liberal vs chloride-restrictive intravenous fluid administration strategy and kidney injury in critically ill adults. JAMA. 2012;308:1566–1572.
Mehta RL, Pascual MT, Soroko S, et al. Diuretics, mortality, and nonrecovery of renal function in acute renal failure. JAMA. 2002;288:2547–2553.
Suetrong B, Pisitsak C, Boyd JH, et al. Hyperchloremia and moderate increase in serum chloride are associated with acute kidney injury in severe sepsis and septic shock patients. Crit Care (Lond, Engl). 2016;20:315.
Sadan O, Singbartl K, Kandiah PA, et al. Hyperchloremia Is associated with acute kidney injury in patients with subarachnoid hemorrhage. Crit Care Med. 2017;45:1382–1388.
Riha HM, Erdman MJ, Vandigo JE, et al. Impact of moderate hyperchloremia on clinical outcomes in intracerebral hemorrhage patients treated with continuous infusion hypertonic saline: a pilot study. Crit Care Med. 2017;45:e947–e953.
Patel N, Baker SM, Walters RW, et al. Serum hyperchloremia as a risk factor for acute kidney injury in patients with ST-segment elevation myocardial infarction undergoing percutaneous coronary intervention. In Proceedings of Baylor University Medical Center 2016;29(1):7–11.
Pezzilli R, Zerbi A, Campra D, et al. Consensus guidelines on severe acute pancreatitis. Dig Liver Dis. 2015;47:532–543.
IAP/APA evidence-based guidelines for the management of acute pancreatitis. Pancreatology. 2013;13:e1–15.
Yokoe M, Takada T, Mayumi T, et al. Japanese guidelines for the management of acute pancreatitis: Japanese guidelines 2015. J Hepato Biliary Pancreat Sci. 2015;22:405–432.
Shaw AD, Raghunathan K, Peyerl FW, et al. Association between intravenous chloride load during resuscitation and in-hospital mortality among patients with SIRS. Intensive Care Med. 2014;40:1897–1905.
Khan Z, Vlodov J, Horovitz J, et al. Urinary trypsinogen activation peptide is more accurate than hematocrit in determining severity in patients with acute pancreatitis: a prospective study. Am J Gastroenterol. 2002;97:1973–1977.
Funding
This study was supported by the National Science Foundation of China (81770641).
Author information
Authors and Affiliations
Contributions
Dr. WL and LK designed the work, Dr. ZT, GL, and JZ collected the data, Dr. BY wrote the paper, and Dr. WM and Dr. YC analyzed the data. All authors have read and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Ye, B., Mao, W., Chen, Y. et al. Aggressive Resuscitation Is Associated with the Development of Acute Kidney Injury in Acute Pancreatitis. Dig Dis Sci 64, 544–552 (2019). https://doi.org/10.1007/s10620-018-5328-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-018-5328-5