Abstract
Objective
To investigate the relationship between intra-abdominal hypertension (IAH) and acute renal failure (ARF) in critically ill patients.
Design and setting
Prospective, observational study in a general intensive care unit.
Patients
Patients consecutively admitted for > 24 h during a 6-month period.
Interventions
None.
Measurements and results
Intra-abdominal pressure (IAP) was measured through the urinary bladder pressure measurement method. The IAH was defined as a IAP ≥12 mmHg in at least two consecutive measurements performed at 24-h intervals. The ARF was defined as the failure class of the RIFLE classification. Of 123 patients, 37 (30.1%) developed IAH. Twenty-three patients developed ARF (with an overall incidence of 19%), 16 (43.2%) in IAH and 7 (8.1%) in non-IAH group (p < 0.05). Shock (p < 0.001), IAH (p = 0.002) and low abdominal perfusion pressure (APP; p = 0.046) resulted as the best predictive factors for ARF. The optimum cut-off point of IAP for ARF development was 12 mmHg, with a sensitivity of 91.3% and a specificity of 67%. The best cut-off values of APP and filtration gradient (FG) for ARF development were 52 and 38 mmHg, respectively. Age(p = 0.002), cumulative fluid balance (p = 0.002) and shock (p = 0.006) were independent predictive factors of IAH. Raw hospital mortality rate was significantly higher in patients with IAH; however, risk-adjusted and O/E ratio mortality rates were not different between groups.
Conclusions
In critically ill patients IAH is an independent predictive factor of ARF at IAP levels as low as 12 mmHg, although the contribution of impaired systemic haemodynamics should also be considered.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Although an association between intra-abdominal hypertension (IAH) and oliguria was observed in the late nineteenth century [1], it is only recently that clinicians have begun to fully recognize the detrimental effects of increased intra-abdominal pressure (IAP) on renal function [2–5]. Most of the studies on this topic have been performed in the abdominal surgical setting, where IAP values of 18 mmHg [2], 20 mmHg [3] and 25 mmHg [4] have been identified as critical for renal failure occurrence; however, in experimental settings it has been suggested that renal haemodynamics and function are highly sensitive, even to moderate increases in IAP, with remarkable impairment between 10 and 15 mmHg [6–8].
As stated by the final report of the 2004 International ACS Consensus Definitions Conference [9], IAH is now defined as an IAP ≥12 mmHg. In the same report, the inclusion of pressures at which organ dysfunction becomes apparent in the majority of patients is claimed in defining IAH. To the best of our knowledge, in critically ill patients a critical IAP value for acute renal failure (ARF) development has not yet been identified. The primary aims of the present study were to investigate the relationship between IAH and ARF in a mixed population of critically ill patients, and to evaluate if a critical threshold value of IAP above which this association becomes significantly more frequent can be identified. Secondary aims were to evaluate predictive factors for ARF and IAH, and to assess the relationship between abdominal perfusion pressure (APP) and ARF.
Materials and methods
A prospective, observational study was performed over a 6-month period. The institutional review board approved the protocol. Informed consent was obtained from patients or their next of kin.
All consecutive adult patients admitted for more than 24 h in a mixed ICU were enrolled. Exclusion criteria were: contraindication to intravesical pressure measurement (pelvic fracture with associated bladder injuries, haematuria, neurogenic bladder); chronic renal failure requiring haemodialysis; and refusal of patients or their next of kin. For patients who were admitted more than once only the first admission was evaluated.
Demographic data, pre-existing comorbidities, primary diagnostic category (i.e. medical and surgical), and Acute Physiology and Chronic Health Evaluation (APACHE II) score were collected on admission. Clinical aetiological factors and predisposing conditions for increased IAP, as well as associated conditions, as defined by the International ACS Consensus Definitions Conference [9], were also recorded for each patient.
The IAP was measured via a Foley bladder catheter, according to a standardized technique [9, 10]. The IAP was always measured at end-expiration in the complete supine position and in stable conditions. The transducer was zeroed at the level of the mid-axillary line, and 25 ml of saline were employed as bladder instillation volume. Measurements were performed on admission and at least every 24 h (more frequently if it was clinically required), until death or discharge. Risk, injury, failure, loss, and end-stage kidney failure (RIFLE) classification [11] and Sequential Organ Failure Assessment (SOFA) score were computed daily.
The IAH was defined as a pathological elevation of IAP at or above 12 mmHg [9, 11, 12], in at least two consecutive measurements performed at 24-h intervals. The IAH was defined as “primary” if associated with injury or disease in the abdominopelvic region (abdominal trauma, ruptured abdominal aortic aneurysm, haemoperitoneum, acute pancreatitis, secondary peritonitis, retroperitoneal haemorrhage or liver transplantation), and “secondary” when result of an extra-abdominal cause (sepsis, capillary leak, major burns, or other conditions requiring massive fluid resuscitation) [9]. Abdominal compartment syndrome (ACS) was defined as a sustained IAP > 20 mmHg (with or without an APP < 60 mmHg), associated with new organ dysfunction/failure [9, 10].
The ARF was defined, according to the failure class definition of the RIFLE criteria [11], as a threefold increase of serum creatinine with respect to basal value, or a GFR decrease of 75%, or a serum creatinine > 4 mg/dl or a urine output < 0.3 ml/kg h–1 for 24 h, or as anuria for 12 h. When the basal serum creatinine was elevated, an abrupt rise of at least 0.5 mg/dl to more than 4 mg/dl defined ARF, and when basal value was not known, in absence of a known history of chronic renal disease, it was estimated using a modification of diet in renal disease (MDRD) equation for assessment of kidney function, assuming a GFR of 75 ml/min per 1.73 m2 [11].
The IAH and ARF were considered potentially related when the time interval between their onsets was less than 48 h [4]. The APP, defined as mean arterial pressure (MAP) minus IAP, and filtration gradient (FG), which equals the difference between the glomerular filtration pressure (GFP) and the proximal tubular pressure (PTP) (FG = GFP–PTP = MAP-2 × IAP) [9, 10], were calculated whenever IAP was measured. Cumulative fluid balance (calculated by subtracting the output from the intake of the 72 h preceding the worst IAP value), diuretics administration and continuous renal replacement therapy (CRRT) requirement were recorded for each patient. Shock was defined as a cardiovascular SOFA subscore > 3, i.e. hypotension requiring dopamine > 5 μg/kg min–1, or norephinephrine and/or epinephrine < 0.1 μg/kg min–1.
Patients were followed up until hospital death or discharge, whichever came first.
Continuous normally distributed data are expressed as mean ± standard deviation (SD) and compared using unpaired Student's t-test. Non-normally distributed data are expressed as median and interquartile ranges and compared using the Mann–Whitney U-test. Categorical data are expressed as number and percentage and compared using chi-square or the Fisher's exact tests. Logistic regression analysis was then performed, with ARF as the dependent outcome variable. Potential promoting factors with a p level < 0.10 in univariate analysis and those judged clinically important were included in the model. The power of the model was tested by the Hosmer–Lemeshow goodness-of-fit test. The effect of potential confounding factors was determined by introducing each factor independently in the final model and considering the variation in the model fit [13]. To evaluate the role of each variable as independent risk factor, all variables associated with ARF at the < 0.05 level of risk in logistic analysis were introduced in a backward stepwise logistic regression model with an α to remove of 0.05. The same analysis was also performed with IAH and mortality, as the dependent outcome variables.
Receiver operator characteristic (ROC) curves were plotted to identify the threshold values of IAP, APP and FG that optimized each variable sensitivity (the ability to identify true positives) and specificity (the ability to identify true negatives) for predicting ARF development.
Observed/expected (O/E) mortality ratios were reported for each group using the observed-to-APACHE II expected rates per group. Ninety-five percent confidence intervals (CI) were calculated according to Hosmer and Lemeshow [14].
In all comparisons, a p-value of < 0.05 was considered statistically significant.
Results
Two hundred fifteen patients were admitted during the study period. Patients who were < 18 years of age (n = 6), those who were admitted for less than 24 h (n = 67), those who were readmitted (n = 7), those with missing data (n = 11) and those with chronic renal failure requiring haemodialysis (n = 1) were excluded from analysis.
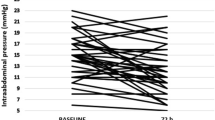
In the remaining 123 patients, 1008 IAP measurements were performed. Thirty-seven (30.1%) patients developed IAH (IAH group). Prevalence on admission of IAH was 19% (Fig. 1a). The mean onset time of IAH was 2.4 ± 3.3 days from admission. Primary IAH occurred in 10 patients (27.1%), secondary IAH in 25 patients (67.5%) and ACS in 2 patients (5.4%).
a Prevalence on admission and daily incidence of intra-abdominal hypertension (IAH) and acute renal failure (ARF) during the first week of ICU stay. b Mean extra-renal and renal sepsis-related organ failure assessment (SOFA) score during the first week of ICU stay in patients with and without IAH. For each day, extrarenal SOFA on the left and renal SOFA on the right. ∗ p < 0.05 vs. non-IAH group
Patients with IAH were significantly older, had more pre-existing comorbidities, a higher severity of illness on admission (as indicated by the APACHE II score; Table 1) and more severe organ dysfunctions (as indicated by the SOFA score associated to the worst IAP value; Table 1) when compared with non-IAH patients. The SOFA scores during the first week of ICU stay in IAH and non-IAH patients are shown in Fig. 1b. Furthermore, IAH patients presented significantly lower values of APP and FG, a greater positive fluid balance and more frequently received diuretics, and required CRRT than non-IAH patients (Table 2).
Sixteen patients developed ARF in IAH group and 7 in non-IAH group (p < 0.05; Table 2). The mean onset time of ARF was 3.4 ± 4.4 days from admission in IAH group as compared with 5.6 ± 9 days in non IAH-group. The mean lag period between IAH and ARF onset was 1 ± 1.8 day. Evolution of ARF during the first week of ICU stay, as well as evolution of IAH, is represented in Fig. 1a.
In the logistic model shock, IAH, APP, APACHE-II score, FG, surgical admission and sepsis were significantly associated with ARF (Table 3). According to the level of significance, the stepwise analysis rated shock as most critical in the model for ARF development, followed by IAH and APP (Table 3).
The ROC curve analysis obtained by plotting ARF vs. the corresponding worst IAP values showed a significant area under the curve (AUC) with a cut-off point for ARF of 12 mmHg (Fig. 2). The ROC curve analysis obtained by plotting ARF vs the worst corresponding APP and FG values showed an AUC of 0.825 (SE 0.058; 99% CI 0.68–0.97; p < 0.0001) and 0.85 (SE 0.053; 99% CI 0.71–0.99; p < 0.0001), with best cut-off values at 52 and 38 mmHg, respectively.
The IAH was significantly associated with age, cumulative fluid balance, shock, sepsis and abdominal surgery (Table 3). When these factors were fitted in the stepwise regression model, age, cumulative fluid balance and shock reached a statistical significance, being the only independent risk factors of IAH (Table 3).
Raw hospital mortality rate was significantly higher in patients with IAH (Table 1); however, risk-adjusted and O/E ratio mortality rates were not different between groups (Table 1). Mortality rate did not differ between patients with primary and secondary IAH (80 vs. 64%, respectively). All patients with ACS (n = 2) died. Binomial analysis revealed that ARF (OR 4.37, 95% CI 1.26–7.09; p = 0.02), IAH (OR 4.11, 95% CI 1.39–8.15; p = 0.01), neurological failure (OR 3.88, 95% CI 1.38–10.9; p = 0.01), surgical admission (OR 2.47, 95% CI 1.01–5.81; p = 0.04) and APACHE-II score (OR 2.11, 95% CI 2.03–3.2; p = 0.04) were significantly correlated with hospital death. Neurological failure (p = 0.001), IAH (p = 0.002) and ARF (p = 0.01) were independently associated with increased mortality in the stepwise analysis (χ 2 = 10.95, p = 0.115).
Discussion
In critically ill patients IAH is associated with ARF, and the critical threshold of IAP for predicting ARF development was found to be 12 mmHg.
In the present study, IAH was an independent promoting factor of ARF, confirming the findings of previous studies performed in other settings [2, 4]. In abdominal surgical patients IAH, defined as an IAP > 18 mmHg, has been rated as the fourth most important risk factor for ARF [2]. In liver recipients, renal impairment has been found to be independently correlated with IAH and the most sensitive and specific IAP value for ARF was found to be 25 mmHg [4]; however, in a mainly medical population of critically ill patients values of IAP > 12 mmHg on admission were associated with a greater degree of renal dysfunction, as compared with controls [15]. In our sample of critically ill patients, the ROC analysis indicates that an IAP cut-off value of 12 mmHg has the best sensitivity/specificity ratio for ARF. This analysis allows a comprehensive representation of discrimining ability over the entire range of IAP and does not require the selection of a particular decision threshold [15], i.e. a priori IAH definition is not required. The results of the ROC analysis imply that a random critically ill patient with renal failure has a higher value of IAP than a random patient without renal failure in 85% of cases [16]. The lower threshold value of IAP for ARF founded in our sample, as compared with surgical patients [2, 4], may well reflect a lower tolerance to even moderate increase of IAP in critically ill patients affected by various concomitant insults.
In clinical setting, the links between ARF and IAH are not yet fully understood. Renal impairment in IAH is considered a multifactorial process, related to haemodynamic, endocrine and local effects [5]. Direct hydrostatic effects by mechanical compression increasing renal vascular resistance coupled with a decrease in cardiac output are the most likely causes [17]. In the present study, shock and IAH were the strongest independent predictors of ARF, confirming previous results by Sugrue et al. [2], who were the first to prospectively identify hypotension and IAH as the main independent promoting factors of renal impairement in a large sample of abdominal surgery patients. Abdominal perfusion pressure, depending on both systemic arterial pressure and IAH and considered an accurate predictor of visceral perfusion [18], and filtration gradient have been hypothesized to be key factors in the development of the IAH-induced renal failure [18, 19]. In our sample, patients with IAH presented significantly lower values of APP and FG than patients without IAH, and APP was an independent promoter of ARF; thus, a pivotal role of haemodynamic impairment in mediating the IAH-induced renal injury in the critically ill must be underscored.
Although intravascular fluid replacement was proposed to prevent the deleterious effects of IAH on renal function [20], this approach does not seem to prevent ARF [21] and may favour IAH occurrence. Recently, several authors have found a strong correlation between positive fluid balance and increased IAP in surgical and trauma patients [4, 22]. Furthermore, in surgical critically ill patients, net fluid balance has been recognized as the only causative factor of ACS [23]. On the other side, a negative fluid balance, obtained by means of aggressive ultrafiltration, has been recently proposed among the conservative strategies to decrease IAP in patients with IAH [24]. In the present study, shock and cumulative fluid balance were the main independent predictors of IAH. Moreover, nearly 70% of IAH patients in our sample exhibited extra-abdominal causes of increased IAP, i.e. clinical conditions requiring vigorous fluid resuscitation and characterized by impaired capillary permeability, such as SIRS, shock and sepsis. In patients with severe acute pancreatitis, the removal of causative cytokines of hyperpermeability may reduce IAP [25]. It can be supposed that “third space” losses from compromised bowel capillary endothelium by reperfusion (such as after haemorrhagic shock) or by inflammatory mediators injury (such as during SIRS or sepsis) associated with a positive fluid balance may lead to gut oedema and increase in IAP. The IAH, by impairing systemic haemodynamics and renal function, may foster a fluid overload condition, leading to a vicious cycle that perpetuates IAH itself and renal failure.
This study has several features that may limit the generalizability of the findings. Firstly, the patient sample was not large enough to compare the predictive value of all the known potential promoting factors of ARF considered, and we cannot exclude the potential role of uncontrolled confounding variables; however, it is encouraging that our findings are in accordance with previous studies on the same subject [2, 4]. Secondly, IAP was measured only at daily intervals during the study period, or more frequently if clinically required. A more standardized approach to IAP measurement, as recently recommended [10], might have improved IAH definition and its causal relationship with ARF. Thirdly, we considered a temporal relation between IAH and ARF of 48 h. The effects of IAH on renal function require a mean lag period of 2.7 days, but this period may extend from 0 to 35 days [2]; therefore, it may be possible that the effects of IAH on renal function would appear more gradually. Finally, therapeutic interventions to reduce IAP were not investigated.
Conclusion
In conclusion, in critically ill patients IAH is a key promoting factor of acute renal failure. This association is observed at IAP values lower than previously reported in other settings. An intra-abdominal pressure of 12 mmHg is critical for renal failure development, although the contribution of impaired systemic haemodynamics, as evidenced by the decrease in abdominal perfusion pressure and filtration gradient, should also be considered.
References
Wendt E (1876) Über den Einfluss des intraabdominalen Druckes auf die Absonderungsgeschwindigkeit des Harnes. Arch Physiologische Heilkunde 57:527–534
Sugrue M, Jones F, Deane SA, Bishop G, Bauman A, Hillman K (1999) Intra-abdominal hypertension is an independent cause of postoperative renal impairment. Arch Surg 134:1082–1085
Sugrue M, Buist MD, Hourihan F, Deane S, Bauman A, Hillman K (1995) Prospective study of intra-abdominal hypertension and renal function after laparotomy. Br J Surg 82:235–238
Biancofiore G, Bindi ML, Romanelli AM, Boldrini A, Consani G, Bisa M, Filipponi F, Vagelli A, Mosca F (2003) Intra-abdominal pressure monitoring in liver transplant recipients: a prospective study. Intensive Care Med 29:30–36
De Laet I, Malbrain ML, Jadoul JL, Rogiers P, Sugrue M (2007) Renal implications of increased intra-abdominal pressure: Are the kidneys the canary for abdominal hypertension? Acta Clin Belg Suppl 62:119–130
Lacey SR, Bruce J, Brooks SP, Griswald J, Ferguson W, Allen JE, Jewett TC Jr, Karp MP, Cooney DR (1987) The relative merits of various methods of indirect measurement of intraabdominal pressure as a guide to closure of abdominal wall defects. J Pediatr Surg 22:1207–1211
Chiu AW, Azadzoi KM, Hatzichristou DG, Siroky MB, Krane RJ, Babayan RK (1994) Effects of intra-abdominal pressure on renal tissue perfusion during laparoscopy. J Endourol 8:99–103
McDougall EM, Monk TG, Wolf JS Jr, Hicks M, Clayman RV, Gardner S, Humphrey PA, Sharp T, Martin K (1996) The effect of prolonged pneumoperitoneum on renal function in an animal model. J Am Coll Surg 182:317–328
Malbrain ML, Cheatham ML, Kirkpatrick A, Sugrue M, Parr M, De Waele J, Balogh Z, Leppäniemi A, Oliera C, Ivatury R, D'Amours S, Wendon J, Hillman K, Johansson K, Kolkman K, Wilmer A (2006) Results from the International Conference of Experts on Intra-abdominal Hypertension and Abdominal Compartment Syndrome. I. Definitions. Intensive Care Med 32:1722–1732
Cheatham ML, Malbrain MLNG, Kirkpatrick A, Sugrue M, Parr M, DeWaele J, Balogh Z, Leppäniemi A, Olvera C, Ivatury R, D'Amours S, Wendon J, Hillman K, Wilmer A (2007) Results from the International Conference of Experts on intra-abdominal hypertension and abdominal compartment syndrome. II. Recommendations. Intensive Care Med 33:951–962
Bellomo R, Ronco C, Kellum JA, Mehta RL, Palevsky P, and the ADQI Workgroup (2004) Acute renal failure: definition, outcome measures, animal models, fluid therapy and information technology needs: the Second International Consensus Conference of the Acute Dialysis Quality Initiative (ADQI) Group. Crit Care 8:R204–R210
Malbrain ML, Chiumello D, Pelosi P, Wilmer A, Brienza N, Malcangi V, Bihari D, Innes R, Cohen J, Singer P, Japiassu A, Kurtop E, De Keulenaer BL, Daelemans R, del Turco M, Cosimini P, Ranieri M, Jacquet L, Laterre PF, Gattinoni L (2004) Prevalence of intra-abdominal hypertension in critically ill patients: a multicentre epidemiological study. Intensive Care Med 30:822–829
Katz MH (2003) Multivariable analysis: a primer for readers of medical research. Ann Intern Med 138:644–650
Hosmer DW, Lemeshow S (1995) Confidence interval estimates of an index of quality performance based on logistic regression models. Stat Med 14:2161–2172
Malbrain MLNG, Chiumello D, Pelosi P, Bihari D, Innes R, Ranieri VM, del Turco M, Wilmer A, Brienza N, Malcangi V, Cohen J, Japiassu A, De Keulenaer BL, Daelemans R, Jacquet L, Laterre P-F, Frank G, de Souza P, Cesana B, Gattinoni L (2005) Incidence and prognosis of intraabdominal hypertension in a mixed population of critically ill patients: a multiple-center epidemiological study. Crit Care Med 33:315–322
Zweig MH, Campbell G (1993) Receiver-operating characteristic (ROC) plots: a fundamental evaluation tool in clinical medicine. Clin Chem 39:561–577
Sugrue M (2005) Abdominal compartment syndrome. Curr Opin Crit Care 11:333–338
Malbrain M (2002) Abdominal perfusion pressure as a prognostic marker in intra-abdominal hypertension. In: Vincent JL (ed) Yearbook of intensive care and emergency medicine. Springer, Berlin Heidelberg New York, pp 792–814
Ulyatt DB (1992) Elevated intra-abdominal pressure. Australas Anesth 10(3):108–114
Meldrum DR, Moore FA, Moore EE, Franciose RJ, Sauaia A, Burch JM (1997) Prospective characterization and selective management of the abdominal compartment syndrome. Am J Surg 174:667–673
Biancofiore G, Bindi ML, Romanelli AM, Bisà M, Boldrini A, Consani G, Filipponi F, Mosca F (2003) Postoperative intra-abdominal pressure and renal function after liver transplantation. Arch Surg 138:703–706
Balogh Z, McKinley BA, Cocanour CS, Kozar RA, Valdivia A, Sailors RM, Moore FA (2003) Supranormal trauma resuscitation causes more cases of abdominal compartment syndrome. Arch Surg 138:637–642
McNelis J, Marini CP, Jurkiewicz A, Fields S, Caplin D, Stein D, Ritter G, Nathan I, Simms H (2002) Predictive factors associated with the development of abdominal comparment syndrome in the surgical intensive care unit. Arch Surg 137:133–136
Malbrain ML, Deeren D, De Potter TJR (2005) Intra-abdominal hypertension in the critically ill: it is time to pay attention. Curr Opin Crit Care 11:156–171
Oda S, Hirasawa H, Shiga H, Matsuda K, Nakamura M, Watanabe E, Moriguchi T (2005) Management of intra-abdominal hypertension in patients with severe acute pancreatitis with continuous hemodiafiltration using a polymethyl methacrylate membrane hemofilter. Ther Apher Dial 9:355–361
Acknowledgements
The authors express their sincere gratitude to P. Trerotoli, Assistant Professor, Department of Biomedical Sciences and Human Oncology, University of Bari, Italy, for his precious contribution to statistical analysis.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dalfino, L., Tullo, L., Donadio, I. et al. Intra-abdominal hypertensionand acute renal failurein critically ill patients. Intensive Care Med 34, 707–713 (2008). https://doi.org/10.1007/s00134-007-0969-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-007-0969-4