Abstract
Background
Theoretically, use of the stylet during endoscopic ultrasound-guided fine-needle aspiration (EUS-FNA) will prevent the tip of the needle from being blocked and the sample from being contaminated, improving the quality and diagnostic yield of specimens.
Aim
This meta-analysis aimed to evaluate any benefit from the use of a stylet during EUS-FNA.
Methods
MEDLINE, EMBASE, WEB of SCIENCE, and the Cochrane Central Register of Controlled Trials were searched for articles published through October 2015. A fixed-effects model was used to calculate the pooled effects when there is no heterogeneity and a random-effects model was used in situations with significant heterogeneity.
Results
Five prospective randomized controlled studies and two retrospective studies of a total of 5491 specimens (2504 specimens in the S+ group and 2987 specimens in the S− group) were included in this study. The pooled analysis demonstrated no significant differences in the adequate sample rate between the S+ group (2135/2504, 85.26 %) and S− group (2609/2987, 87.35 %) [odds ratio 0.94 (95 % confidence interval 0.79–1.11), p = 0.45]. Furthermore, the rate of cellularity > 50 %, the contamination rate, and the blood contamination rate were not significantly superior in the S+ group when compared with the S− group.
Conclusions
Whether the use of a stylet improves the proportion of adequate specimens or quality of the specimen is questionable. Our results suggest that the use of a stylet dose not guarantee any advantage during EUS-guided tissue sampling.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Endoscopic ultrasound-guided fine-needle aspiration (EUS-FNA) has become widely accepted as an effective standard technique for establishing tissue diagnosis for patients with suspected gastrointestinal tract and adjacent organ (lymph nodes, mediastinal masses, or adrenal tumors), gastrointestinal subepithelial lesions, and pancreatic neoplasms [1–3]. However, especially in regards to pancreatic neoplasm, this technique presents a high diagnostic accuracy but a relatively low negative predictive value (NPV): median figures for sensitivity, specificity, NPV, and diagnostic accuracy are 83 % (range 54 – 95 %), 100 % (range 71– 100 %), 72 % (range 16 – 92 %) and 88 % (range 65 – 96 %), respectively [3–7]. Thus far, many technical trials including manipulation of the stylet have been investigated for their potential to improve the diagnostic yield of EUS-FNA, because many confounding factors have been suggested to affect the diagnostic outcomes. These include the degree of technical difficulty, experience of the echoendoscopist and the cytopathologist, type and diameter of the needle, characteristics of the lesion (anatomical location, size, stiffness of the target lesion), number of passes, application of suction, method of tissue acquisition, and immediate on-site cytopathology assessment [8–10]. Among these trials, several reports [11–14] have focused on the need for a stylet during EUS-FNA. Theoretically, the puncture for the lesion needs to be performed with a stylet in the needle lumen to prevent blockage or contamination by the intestinal mucosal tissue and to allow more adequate aspiration of the target tissue. Furthermore, a stylet is needed to maintain needle stiffness, allowing a puncture of a fibrotic lesion [12]. Contrary to the above, some intriguing studies recently found that the use of a stylet can lead to increased procedure time and the risk of an unintentional needle stick injury, especially when multiple passes are needed [2, 15]. In particular, controversies exist regarding the sample adequacy and diagnostic yield for EUS-FNA. One study [11] reported that the use of the stylet resulted in lower sample quality with significant difference, although other studies [2, 12–15] reported that the stylet did not affect clinical outcomes, such as sample adequacy or diagnostic yield, and thus its clinical benefit in daily practice may be limited.
Several studies consistently reported that there were no advantages to using a stylet during EUS-FNA, but each of those studies had limitations, such as small sample sizes. Moreover, a meta-analysis on this subject has not been previously performed. Therefore, the aim of our meta-analysis is to discover if there is any benefit from the use of a stylet during EUS-FNA.
Materials and Methods
This systematic review was conducted and reported according to the preferred reporting items for systematic review and meta-analyses (PRISMA) statement [16].
Eligibility Criteria and Definitions
Both prospective and retrospective cohort studies, case–control studies, and randomized clinical trials (RCTs) of adult patients who underwent EUS-FNA, published as full articles, were considered. Studies were eligible for inclusion in the meta-analysis if they met the following criteria: (1) comparative design for evaluating the sample quality and diagnostic ability of the specimen from EUS-FNA with or without a stylet; (2) data not duplicated in another manuscript; and (3) endpoints including at least one appropriate cyto-pathological outcome among the following: adequate specimen, cellularity, contamination, or blood contamination. Inclusion was not restricted by study size or language. Exclusion criteria were: (1) comments, reviews, or guideline articles; (2) studies reporting non-gastrointestinal endoscopy, such as laparoscopic procedures or bronchoscopy; (3) studies providing no data on cyto-pathological outcomes; and (4) studies repeatedly reported (in which case, only the latest reported article was selected).
Adequate samples were defined as passes providing representative tissue from the sampled organ. The widely accepted definition for cellularity was the percentage area of slides that contained cells of the representative lesion: “0,” no representative cells present; “1,” representative cells present in <25 % area of the slides; “2,” representative cells present in 25–50 % area of the slides; “3,” representative cells present in >50 % area of the slides. Similarly, contamination was defined as the following: “0,” no contamination seen; “1,” contamination present in <25 % area of the slides; “2,” contamination present in 25–50 % area of the slides; “3,” contamination present in >50 % area of the slides. Finally, blood contamination was defined as the following: “1,” minimal; “2,” moderate; “3,” significant.
Information Sources and Search Strategy
A literature search was conducted to identify all relevant studies that compared the clinical outcomes for EUS-guided tissue sampling with and without a stylet. A systematic literature search of MEDLINE, EMBASE, and WEB of SCIENCE databases and the Cochrane Central Register of Controlled Trials updated was conducted. Furthermore, manual searching through other sources was conducted according to PRIMA flow diagram. The following medical subject heading terms were used: “endoscopic ultrasound,” “fine-needle aspiration,” and “stylet.” Internet search engines, Google Scholar, and Yahoo were also searched with the relevant key words. The latest date for updating the search was 1 October 2015.
Study Selection
After removing duplicate studies, the titles and abstracts of studies found by the searches were examined to exclude articles with irrelevant study designs. If available, the full texts of all selected studies were screened according to the inclusion and exclusion criteria. Selected full text articles were critically appraised for relevance and validity. Two investigators (S.W.P. and J.H.K.) independently evaluated the studies for their eligibility and subsequently resolved any disagreements by discussion, together with clinical expert consultation.
Data Extraction and Study Quality Assessment
The data retrieved from each study included the year of publication, country, research design, number of individuals and specimens in the S+ and S− groups, type of needle used, number of needle passages in each group, and the primary and secondary outcomes. To avoid bias in the data extraction process, two investigators (S.W.P. and J.H.K.) independently evaluated each study’s quality and compared their results with one another on blinded state regarding journal titles, author names, and institutional affiliations. In cases of disagreement, the third investigator made a determinative decision. To minimize the risk of bias in the included studies, a formal quality assessment was conducted. The methodological quality of the RCT was assessed by two authors independently (S.W.P. and J.H.K.) using Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011) [17]. Furthermore, the quality of the selected non-randomized retrospective studies was evaluated using the Newcastle–Ottawa Scale (NOS) [18], which evaluated studies with a star-rating system ranging from 0 (the lowest quality) to 9 (the highest quality) stars, based on three study components, including selection, comparability, and outcome assessment. Articles that were awarded five or more stars were considered high-quality studies, whereas the other studies were considered to be of low quality.
Evaluation Criteria for Endpoints
The primary end point was the rate of adequate specimens from EUS-guided tissue sampling with or without a stylet. Secondary end points were: (1) the rate of cellularity > 50 %; (2) the contamination rate; (3) the blood contamination rate; (4) diagnostic ability.
Statistical Analysis
The meta-analysis was carried out with Review Manager 5.3 software (provided by the Cochrane Collaboration). Statistical analysis for dichotomous variables including the rate of adequate specimens, the rate of cellularity > 50 %, the contamination rate, and the blood contamination rate was performed using the odds ratio (OR) as the summary statistic [with a corresponding 95 % confidence interval (CI)]. For outcome data regarding diagnostic ability, we calculated mean differences or the standardized mean difference. Heterogeneity among the studies was assessed using the Chi squared test. A p value < 0.05 was considered to suggest significant heterogeneity. At the same time, I 2 was also used to assess heterogeneity. An I 2 > 50 % was considered to indicate statistical significance. Meta-analysis was to be calculated by using a fixed-effects model when no heterogeneity was detected. If any heterogeneity existed, heterogeneity was to be explored by subgroup analysis or a random-effects model.
Results
Study Selection
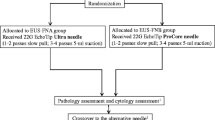
Our search strategy yielded a total of 37 potential studies for the meta-analysis (Fig. 1). After searching the titles and abstracts, we excluded 11 repeated articles. Then, based on the inclusion and exclusion criteria, nine articles were excluded: five studies were unrelated to the present meta-analysis and four studies dealt with only non-gastrointestinal endoscopy, such as percutaneous methods or bronchoscopy. Among the remaining 17 papers, an additional ten articles were excluded due to inappropriate study design (review articles). Finally, seven studies were found to be appropriate for meta-analysis [2, 11–14, 19, 20]. These studies described a total of 5491 specimens: 2504 specimens in the S+ group and 2987 specimens in the S− group. All studies were published in the past 6 years, from 2010 to 2015. Five studies [2, 11, 13, 15, 20] were prospective randomized controlled studies (RCTs) (one [15] of the five RCTs was a prospective single-blind randomized crossover study) and two studies [12, 14] were retrospective studies. Of the seven studies, three [2, 12, 13] were conducted in the USA, two [11, 14] in Canada, and one each in India [20] and Japan [15]. All studies were reported as full-text articles in English. The baseline characteristics of the studies included in the meta-analysis are summarized in Table 1.
Risk of Bias in Included Studies
A summary of the risk of bias across the five RCTs [2, 11, 13, 15, 20] is given in Figs. 2 and 3. Randomization and allocation concealment were adequately described in four [2, 11, 13, 15] of the included studies and were judged as unclear in the remaining one study [20]. The studies were not double blind because the endoscopist must know the technique to be applied. However, the review authors judged that the outcome and the outcome measurement were not likely to be influenced by lack of blinding. Only one study [20] was judged as unclear for incomplete outcome data; all remaining studies were judged as having low risk of bias. A total of four studies [2, 11, 13, 15] were rated as having low risk of bias for selected outcome reporting. The remaining one study was rated as having unclear risk of bias. However, in the absence of initial study protocols, it was not clear whether all studies reported outcomes as pre-specified in the trial protocol. Other potential sources of bias were noted in the design of studies in terms of interventions used and outcomes assessed. Although some studies used different definitions of outcome measurement, almost all studies included in the meta-analysis that reported adequacy of specimens, cellularity, and contamination criteria were very similar, suggesting that the definition of these outcomes was not a source of bias. Furthermore, the result of the NOS assessment is shown in Table 2. According to the protocol, two articles [12, 14] were regarded as high quality reports with seven stars.
Adequate Specimens
All of the included studies [2, 11–15, 20] reported the rate of adequacy of specimens, and the pooled analysis using the fixed-effects model showed a higher adequacy rate in the S− group (2609/2987, 87.35 %) than in the S+ group (2135/2504, 85.26 %), but the difference was not statistically significant [pooled OR 0.94 (95 % CI 0.79–1.11), p = 0.45] (Fig. 4a). The χ 2 and I 2 were 9.02 (p = 0.17) and 33 %, respectively, indicating no significant heterogeneity among the studies with respect to the rate of adequacy of specimens.
Among the included studies, one study [15] dealt with only histopathological adequacy of specimens instead of cytological adequacy of specimens. Therefore, cytological adequacy of specimens was examined in six studies [2, 11–14, 20]; five studies [2, 11, 12, 14, 20] used a standard end-hole 22 gauge needle and the other one study [13] used a standard end-hole 22 or 25 gauge needle. The subgroup analysis of the six studies that dealt with only cytological adequacy of specimens showed similar results with no statistically significant difference in the rate of adequacy of specimens [pooled OR 0.92 (95 % CI 0.76–1.12), p = 0.42]. The χ 2 and I 2 were 8.93 (p = 0.11) and 44 %, respectively, indicating no significant heterogeneity among the studies with respect to cytological adequacy of specimens (Fig. 4b).
Cellularity
Four studies [2, 12, 13, 17] reported cellularity from EUS-FNA with or without the stylet. The pooled analysis using the fixed-effects model demonstrated no significant differences between the S+ (305/837, 36.44 %) and S− groups (311/853, 36.46 %) regarding the rate of cellularity > 50 % [pooled OR 1.01 (95 % CI 0.80–1.27), p = 0.92) (Fig. 5a). No heterogeneity was identified among the studies (p = 0.89, I 2 = 0 %).
Among four included studies [2, 12, 13, 15], one study [15] used a different definition for cellularity. Thus, cellularity using the same definition was examined in three studies [2, 12, 13]. The subgroup analysis of three studies for the rate of cellularity > 50 % using the same definition showed similar results, with no statistically significant difference between the S+ (143/617, 23.18 %) and S− groups (151/633, 23.85 %) [pooled OR 1.00 (95 % CI 0.76–1.31), p = 0.98]. No heterogeneity was identified among the studies (p = 0.75, I 2 = 0 %) (Fig. 5b).
Contamination
The contamination rate was reported in four studies [2, 12, 13, 15]. Pooled analysis using a fixed-effects model demonstrated no significant differences between the groups regarding the contamination rate [S+ group (20/837, 2.39 %) vs. S− group (26/853, 3.04 %): OR 0.79 (95 % CI 0.44–1.44), p = 0.45] (Fig. 6). There was no heterogeneity among the studies (p = 0.63, I 2 = 0 %).
Blood Contamination
Five studies [2, 11–13, 20] reported the blood contamination rate (“3,” significant), including 801 specimens in the S+ group and 886 specimens in the S− group. In a pooled analysis with a random-effects model, the blood contamination risk was slightly higher in the S+ group (249/801, 31.09 %) than in the S− group (270/886, 30.47 %), but this difference was not statistically significant [OR 1.19 (95 % CI 0.75–1.90), p = 0.46] (Fig. 7). The χ 2 and I 2 were 15.35 (p = 0.004) and 74 %, respectively, which indicated significant heterogeneity among the studies with respect to the blood contamination rate.
Discussion
We investigated seven studies to determine whether the use of the stylet during EUS-FNA was associated with clinical outcomes, such as sample adequacy or diagnostic yield. Although the use of a stylet has been found to improve the quality of specimens obtained by preventing blockage by the intestinal mucosa, thereby reducing contamination and allowing for an improved overall diagnostic yield of EUS-FNA [4, 11, 21], there is no consensus regarding the role of the stylet, and few studies with large numbers of patients have compared the endoscopic and cytopathological outcomes with or without a stylet. To date, most endosonographers tend to use a stylet during EUS-FNA based on the unsubstantiated premise that the use of a stylet improves the quality of the specimen [22]. Contrary to this premise, recent data suggests that the use of a stylet does not guarantee any advantage with regard to the diagnostic yield of malignancy or to the quality of specimens obtained [2, 11, 12]. Thus, this meta-analysis is meaningful because we were the first to compare important cytopathological parameters such as adequacy, amount of blood, and cellularity among specimens obtained with and without a stylet during EUS-FNA.
In terms of the adequacy of specimens, our pooled data indicates that there were no significant differences between the S+ and S− groups, although only one study [11] among the seven reported that the rate of adequate specimens without the stylet was higher than with the stylet during EUS–FNA. In this prospective analysis, contrary to our results, Sahai et al. found that sample adequacy was lower and bloodiness higher in the S+ group, suggesting that the quality of samples obtained with a stylet may actually be inferior. Our lack of significant results between the S+ and S− groups can be attributed to several factors: not all studies provided an explicit definition of adequacy of specimen; therefore, the results may be influenced to a greater or lesser extent. Also, there may be a discrepancy between the method of tissue sampling (the aim of one study [15] was histological adequacy and that of the other six studies [2, 11–14, 20] was cytological adequacy). Hence, it can be difficult to provide a precise assessment of the adequacy of specimens, although we conducted subgroup analysis for studies with only cytological outcomes after excluding one study [15] regarding histological adequacy and the results of the subgroup analysis was similar to that of all seven studies.
Another concern when using a stylet to prevent blockage or contamination by the intestinal mucosa and allow more adequate aspiration is the qualitative improvement of cellularity. Among the RCTs analyzed in our review, cellularity was defined differently (one study [15] used the definition of cellularity as a scoring system from 0 to 5, while the other three studies used percentage area of slides that contained cells of the representative lesion from 0 to 3); we did not find any differences in the cellularity in either the S+ or S− groups.
Although there is limited data comparing the use of EUS-FNA with or without a stylet, none of the included studies in our review has shown any differences between the groups. In one retrospective analysis of four studies that reported cellularity, Wani et al. [12] compared EUS-FNA with and without a stylet for 228 lesions. The authors did not find a significant difference in cellularity [15]. Similarly, the same group also performed a similar prospective RCT [13] with 550 lesions to compare the performance of EUS-FNA with or without a stylet and concluded that there was no significant difference between the S+ and S− groups for cellularity. This lack of a significant difference may be attributed to a certain amount of subjectivity in their assessment by cytopathologists, although predefined criteria were used to compare the cytologic characteristics of the specimens and the cytopathologists were blinded to the technique used to obtain the specimens in order to obviate any bias. Also, most studies conducted by two or more cytopathologists did not assess the interobserver agreement among cytopathologists in the assessment of EUS-FNA specimens. Variability in the diagnosis of malignancy among pathologists and its impact on the results cannot be excluded.
Additionally, our review revealed that contamination, including blood contamination, in the S+ group tended to be higher than in the S− group, though not at a level reaching significance, similar to the differences between both groups for other outcomes. Theoretically, the use of a stylet will prevent the tip of the needle from being blocked by a plug of digestive wall tissue and/or contamination of the sample before entering the FNA target lesion, thereby producing improved overall outcomes. In clinical practice, Sahai et al. [11] initially reported the effect of the stylet on EUS-FNA in a prospective study in which a single endosonographer performed EUS-FNA of 135 lesions in 111 patients with a 22-gauge needle. However, in that study, the proportion of bloody samples was higher in the S+ group than in the S− group (75 vs. 52 %, p < 0.0001), suggesting that the use of the stylet during EUS-FNA could hinder cytological diagnosis. Similarly, our results suggest that this theory is invalid. Use of the stylet did not change the contamination rate or the frequency of bloody and/or inadequate samples; however, this observation may be attributed to type II error, as none of these studies are powered sufficiently to detect a true benefit or the interobserver disagreement among cytopathologists in the assessment of EUS-FNA specimens.
Furthermore, the lack of differences between all the endpoints assessed (quality of specimen and cytological characteristics) may be related to different lesion sites because the hardness of each lesion was different. In other words, the included studies did not use the same lesion to compare the two groups. For example, the tissue of the lymph node is softer and has less fibrotic tissue than pancreatic malignancies (especially pancreatic ductal adenocarcinoma). Finally, although suction for negative pressure, which may have increased the amount of blood, was applied equally in all patients of both groups, suction effects can in no way be negligible.
Although we included relevant studies in our review, several limitations of our study need to be considered, as in any meta-analysis. Firstly, we did not conduct publication bias, which may distort the outcome of the overall analysis. Obviously, it did not guarantee that there was no publication bias in our meta-analysis, although Cochrane library may not recommend publication bias when the number of included studies is < 10. The use of different needle types (in three studies [2, 12, 20], a standard 22-gauge needle by Cook Medical was used; in one study [13], a standard 22- or 25-gauge needle by Cook Medical was used; in one study [15], a standard 22-gauge needle by Boston Scientific was used; in the other two studies [11, 14], a standard 22-gauge needle from an unknown company was used) may contribute to heterogeneity that could affect the results. Therefore, these results should be interpreted with caution, as the aim and performance of each needle were not uniform. In addition, not all of the studies provided an explicit definition or criteria for outcomes, especially for the definition of specimen adequacy, cellularity, contamination, or bloodiness. This might have influenced our results to a certain extent. Finally, one of the main goals of our study was to improve the quality of specimens, but the available studies had limited information regarding histological adequacy (in only one study) beyond cytological adequacy.
In conclusion, this meta-analysis exploring the role of the stylet during EUS-FNA procedures shows that the practice of using a stylet during EUS-FNA is questionable as to whether it improves the quality of the specimen obtained. Also, the results of our review challenge the current belief that the use of a stylet during EUS-FNA helps prevent clogging of the lumen of the needle by gut wall tissue. In other words, the use of a stylet during EUS-FNA does not appear to confer any advantage with regards to the adequacy of specimen or diagnostic yield. Echoendoscopists should be aware that it would be reasonable to not use a stylet during EUS-FNA, potentially making the procedure easier and less labor intensive, as well as more time- and cost-efficient.
References
Yamao K, Sawaki A, Mizuno N, Shimizu Y, Yatabe Y, Koshikawa T. Endoscopic ultrasound-guided fine-needle aspiration biopsy (EUS-FNAB): past, present, and future. J Gastroenterol. 2005;40:1013–1023.
Rastogi A, Wani S, Gupta N, et al. A prospective, single-blind, randomized, controlled trial of EUS-guided FNA with and without a stylet. Gastrointest Endosc. 2011;74:58–64.
Dumonceau JM, Polkowski M, Larghi A, et al. Indications, results, and clinical impact of endoscopic ultrasound (EUS)-guided sampling in gastroenterology: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy. 2011;43:897–912.
Eloubeidi MA, Jhala D, Chhieng DC, et al. Yield of endoscopic ultrasound-guided fine-needle aspiration biopsy in patients with suspected pancreatic carcinoma. Cancer. 2003;99:285–292.
Savides TJ, Donohue M, Hunt G, et al. EUS-guided FNA diagnostic yield of malignancy in solid pancreatic masses: a benchmark for quality performance measurement. Gastrointest Endosc. 2007;66:277–282.
Fisher L, Segarajasingam DS, Stewart C, Deboer WB, Yusoff IF. Endoscopic ultrasound guided fine needle aspiration of solid pancreatic lesions: performance and outcomes. J Gastroenterol Hepatol. 2009;24:90–96.
Turner BG, Cizginer S, Agarwal D, Yang J, Pitman MB, Brugge WR. Diagnosis of pancreatic neoplasia with EUS and FNA: a report of accuracy. Gastrointest Endosc. 2010;71:91–98.
Ramesh J, Varadarajulu S. How can we get the best results with endoscopic ultrasound-guided fine needle aspiration? Clin Endosc. 2012;45:132–137.
Lee JH, Stewart J, Ross WA, Anandasabapathy S, Xiao L, Staerkel G. Blinded prospective comparison of the performance of 22-gauge and 25-gauge needles in endoscopic ultrasound-guided fine needle aspiration of the pancreas and peri-pancreatic lesions. Dig Dis Sci. 2009;54:2274–2281.
Affolter KE, Schmidt RL, Matynia AP, Adler DG, Factor RE. Needle size has only a limited effect on outcomes in EUS-guided fine needle aspiration: a systematic review and meta-analysis. Dig Dis Sci. 2013;58:1026–1034.
Sahai AV, Paquin SC, Gariepy G. A prospective comparison of endoscopic ultrasound-guided fine needle aspiration results obtained in the same lesion, with and without the needle stylet. Endoscopy. 2010;42:900–903.
Wani S, Gupta N, Gaddam S, et al. A comparative study of endoscopic ultrasound guided fine needle aspiration with and without a stylet. Dig Dis Sci. 2011;56:2409–2414.
Wani S, Early D, Kunkel J, et al. Diagnostic yield of malignancy during EUS-guided FNA of solid lesions with and without a stylet: a prospective, single blind, randomized, controlled trial. Gastrointest Endosc. 2012;76:328–335.
Gimeno-Garcia AZ, Paquin SC, Gariepy G, Sosa AJ, Sahai AV. Comparison of endoscopic ultrasonography-guided fine-needle aspiration cytology results with and without the stylet in 3364 cases. Dig Endosc. 2013;25:303–307.
Abe Y, Kawakami H, Oba K, et al. Effect of a stylet on a histological specimen in EUS-guided fine-needle tissue acquisition by using 22-gauge needles: a multicenter, prospective, randomized, controlled trial. Gastrointest Endosc. 2015;82:837–844.
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol. 2009;62:1006–1012.
Higgins J, Green S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. City: The Cochrane Collaboration; 2011.
The Newcastle–Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in metaanalyses. 2004. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp.
Abe Y, Kawakami H, Oba K, et al. Effect of a stylet on a histological specimen in EUS-guided fine-needle tissue acquisition by using 22-gauge needles: a multicenter, prospective, randomized, controlled trial. Gastrointest Endosc. 2015;82:837.e831–844.e831.
Nijhawan S, Singh B, Kumar A, Ramrakhiani D, Mathur A, Gupta G. Randomized controlled trial of comparison of the adequacy, and diagnostic yield of endoscopic ultrasound guided fine needle aspiration with and without a stylet in Indian patients: a prospective single blind study. J Dig Endosc. 2014;5:149–153.
Mertz H, Gautam S. The learning curve for EUS-guided FNA of pancreatic cancer. Gastrointest Endosc. 2004;59:33–37.
Kudo T, Kawakami H, Hayashi T, et al. High and low negative pressure suction techniques in EUS-guided fine-needle tissue acquisition by using 25-gauge needles: a multicenter, prospective, randomized, controlled trial. Gastrointest Endoscopy. 2014;80:1030.e1031–1037.e1031.
Authorship
Conception and design: Jae Hyun Kim, Se Woo Park. Analysis and interpretation of the data: Jae Hyun Kim, Se Woo Park. Drafting of the article: Jae Hyun Kim, Se Woo Park, Mi Kang Kim, Jin Lee, Sea Hyub Kae, Hyun Joo Jang, Dong Hee Koh, Min Ho Choi. Critical revision of the article for important intellectual content: Jae Hyun Kim, Se Woo Park. Final approval of the article: Se Woo Park.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors have no conflicts of interest or financial ties to disclose. Furthermore, this report is a meta-analysis. The author states that the report includes every item in the PRISMA checklist for meta-analysis clinical studies. Also, this manuscript was screened for plagiarism using Turnitin (www.turnitin.com).
Rights and permissions
About this article
Cite this article
Kim, J.H., Park, S.W., Kim, M.K. et al. Meta-Analysis for Cyto-Pathological Outcomes in Endoscopic Ultrasonography-Guided Fine-Needle Aspiration With and Without the Stylet. Dig Dis Sci 61, 2175–2184 (2016). https://doi.org/10.1007/s10620-016-4130-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-016-4130-5