Abstract
Bezafibrate (BF) is a peroxisome proliferator-activated receptor (PPAR) agonist used as a lipid-lowering agent to treat both the familial or acquired combined forms of hyperlipidemia. BF is the only available fibrate drug that acts on all PPAR subtypes of α, β, and δ. Although there are studies that indicate a genotoxic potential associated with the use of fibrates, to our knowledge, the genotoxicity of BF in human peripheral blood lymphocytes has not been studied. In the present study, the genotoxic potential of BF was evaluated using chromosome aberration (CA) and micronucleus (MN) assays in peripheral blood lymphocytes of healthy human subjects. In addition, a high performance liquid chromatography (HPLC) method was used to identify and quantitate the drug passage into the cells. Human peripheral blood lymphocytes were exposed to four different concentrations (100, 175, 250 and 325 μg/mL) of BF for 24- and 48-h treatment periods. As shown by HPLC, in spite of significant passage of BF into human peripheral blood lymphocytes in 24- and 48-h treatment periods, BF was not found to increase the CA and MN frequency. On the other hand, exposing cells to BF for 24- and 48-h treatment periods caused significant concentration-dependent decreases in the mitotic index (r = −0.995, p < 0.01 for 24-h; r = −0.992, p < 0.01 for 48-h) and nuclear division index (r = −0.990, p < 0.01 for 24-h; r = −0.981, p < 0.01 for 48-h). Our results suggest that BF has cytotoxic effect on cultured human peripheral blood lymphocytes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Fibrates are a class of amphipathic carboxylic acids used for a variety of metabolic disorders mainly hypercholesterolemia. Fibrates exert their indirect metabolic modulating effects by activating peroxisome proliferator-activated receptors (PPAR) via a ligand binding mechanism. Upon activation by fibrates, PPARs regulate the expression of several genes functioning in intra- and extracellular lipid metabolism, most importantly those involved in peroxisomal beta-oxidation (Schoonjans et al. 1996; Staels et al. 1998). The hypotriglyceridemic action of fibrates is partly mediated by the decrease of hepatic lipogenesis and by a reduction of the plasma free fatty acids (Schoonjans et al. 1996; Staels et al. 1998; Forcheron et al. 2002).
Fibrates have long been attributed as nongenotoxic carcinogens (Marsman et al. 1988; Rao and Reddy 1996; Gonzalez 1997). Several mechanisms have been proposed for the carcinogenic effect of fibrates including the production of reactive oxygen species (ROS) and subsequent DNA damage, a sustained increase in cell proliferation via growth stimulation or inhibition of apoptosis and the Kupffer cells which are rich in some mitogens and chemotactic factors (Rao and Reddy 1996; Ashby et al. 1994; Cattley et al. 1998; Lake et al. 2000; Rose et al. 2000).
On the other hand, the small number of genotoxicity studies on fibrates also indicate that these compounds exert their genotoxic effects primarily via the production of ROS in short term genotoxicity assays (Tawfeeq et al. 2011; Rocco et al. 2012). Although it was mentioned in those studies that the DNA damage resulting from the generation of ROS has an indirect and repairable character by DNA repair proteins, ROS may also cause persistent DNA damage depending on the period of exposure as shown earlier (Rao and Reddy 1996). In addition, fibrates may act directly via adducts formed on human DNA (Nishimura et al. 2007).
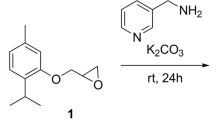
Bezafibrate (BF) (2-(4-{2-[(4-chlorobenzoyl)amino]ethyl}phenoxy)-2-methylpropanoic acid) (Fig. 1), test substance of this study, is a widely used hypolipidemic agent which is known as the only ligand simultaneously for the three PPAR subtypes of α, β, and δ (Honda et al. 2013) with a predominant activity for PPARα (Tanaka 2012). BF is extensively used to treat both the familial or acquired combined forms of hyperlipidemia; however, BF treatment in Sprague–Dawley rats has been shown to induce a slight increase in liver tumor incidence and that incidence was increased at higher doses (Reddy and Lalwai 1983). More recently, BF was shown to modulate the expression of proteins of human hepatocytes which are known as being associated with hepatocarcinogenesis, such as peroxiredoxin-1 and phosphatidylethanolamine-binding protein 1 (Alvergnas et al. 2011). Moreover, BF demonstrated genotoxic potential in the SOS chromotest with E. coli PQ37 and induced a statistically significant reduction in the integrity of human sperm DNA with high fragmentation values (Isidori et al. 2007; Rocco et al. 2012).
Alterations in blood lymphocyte chromosomes are among the most widely used indicators of genotoxic exposure and a comparison of cancer risk with chromosome aberration (CA) frequency is possible because CAs in peripheral blood lymphocytes have been validated as biomarkers of increased cancer risk (Bonassi et al. 2008; Carrano and Natarajan 1988). Both chromatid and chromosome-type CAs are associated with cancer risk (Hagmar et al. 1998, 2004). Furthermore, micronucleus (MN) can be also formed as a result of chromosome breaks and dysfunction of mitotic apparatus. Like the CA frequency, epidemiological evidence indicate that MN frequency in peripheral blood lymphocytes can be used as a biomarker in the prediction of cancer in a population of healthy individuals (Bonassi et al. 2011; Fenech et al. 2011).
In the present study, to examine whether treatment of human peripheral lymphocytes with BF leads to DNA damage, we performed CA and MN tests as the highly sensitive cytogenetic damage markers to detect DNA damage. Cytotoxicity of BF was evaluated using the mitotic index (MI) and the nuclear division index (NDI). We also performed high performance liquid chromatography (HPLC) to determine and quantitate the drug passage into the cells.
Materials and methods
Cukurova University Institutional review board was informed of the protocol to be used with the human subjects, and approved the protocol for the work described prior to the performance of the experiments. In addition, all healthy blood donors gave informed consent for the participation in this study.
Identification and quantification of the amount of BF passage into human peripheral lymphocytes (HPLC techniques)
In each test (both CA and MN assays) we established a DMSO control group (a control tube without human peripheral lymphocytes) containing the highest concentration of BF (Sigma-Aldrich, St. Louis, MO, USA, CAS registry number: 41859-67-0) (325 µg/mL in DMSO). This test tube was incubated together with the experimental groups (BF-treated human peripheral lymphocytes) for 48 h at 37 °C. In this DMSO control group, we calculated the % (percentage) of diminished BF amount. The diminished BF amount both in DMSO control tube (without human peripheral lymphocytes) and the BF-treated groups (containing human peripheral lymphocytes) was assessed using HPLC technique. The difference of diminished BF amount between the control and the BF-treated groups (containing human peripheral lymphocytes) gave the amount of BF passage into human lymphocytes.
The following methodology has been applied to determine the decrease (passing quantity) of BF in BF-treated groups containing human peripheral lymphocytes: At the end of the culture period (48 h), cells were centrifuged at 1200 rpm for 15 min, the supernatant was taken and stored at −20 °C. The BF amount in supernatants was determined using HPLC technique.
The extraction, identification and quantification of BF from the supernatant
The extraction of BF from the supernatant was performed according to liquid–liquid extraction method proposed by Anchisi et al. (1998). Following extraction, samples were transferred to HPLC vials and loaded to HPLC instrument (Anchisi et al. 1998). Shimadzu (Istanbul, Turkey; Applied Prominence Sil-20A) HPLC instrument was used for separation of BF and separations were performed on an Inertsil ODS-4 column (column size: 2.1 × 50 mm, pore size: 3 µm, C/N: 5020-04012, S/N: 0AF50056, GL Sciences, Tokyo, Japan). The injector temperature was 25 °C and 5 min equilibrium time was allowed between injections. The oven temperature and injection volume was set to 25 °C and 20 µL, respectively. The flow rate was 1 mL/min. In this study, phosphate buffer—methanol (35:65, phosphate buffer 0.01 M, pH 3.5) were used as mobile phase. The UV detection was made at 230 nm and BF was identified at 1.12 th min (retention time). Using this bioanalytical method, the quantity of BF in 1 mL medium was determined. Since the BF amount in the medium (325 µg/mL) was recorded at the start of the cultures (both the control and BF-treated human lymphocyte cultures), the reduction rate (%) of BF in cultures (with human peripheral lymphocytes) versus control was calculated using the amounts that were determined by HPLC technique.
Chromosome aberration assay
The method of Evans (1984) was followed for preparation of the CA test with minor modifications. This study was conducted according to the IPCS guidelines (Albertini et al. 2000). Whole blood (0.2 mL) from four healthy donors (two male [24 and 25 year-old] and two female [23 and 25 year-old], nonsmokers) was added to 2.5 mL PB-MAX (supplemented with phytohemagglutinin) (GIBCO—Life Technologies, Carlsbad, CA, USA) chromosome medium. The kidney bean-derived lectin, phytohemagglutinin (PHA), is a powerful mitogen for human T-cells (Benn and Delach 2008). 72 h after the addition of PHA to the culture, about 45% of cells (T-lymphocytes) are in S phase (Howe et al. 2014). Thus, the presence of PHA in the chromosome medium containing whole blood culture, allowed us to specifically induce human peripheral blood lymphocytes for mitotic division and the metaphases we detected are derived from PHA-induced human peripheral blood lymphocytes. Therefore, in spite of the fact that there are many other cell types in the whole blood culture (red blood cells, granulocytes [e.g. neutrophils], monocytes etc.), we only induced T-cells (T-lymphocytes) for further mitotic division in order to be able to arrest them at metaphase.
The healthy blood donors were not using any medication or dietary supplements throughout the study. Cultures were incubated at 37 °C for 72 h. The cells were treated with 100, 175, 250 and 325 µg/mL BF dissolved in DMSO, for 24 h (BF was added 48 h after initiating the culture) and 48 h (BF was added 24 h after initiating the culture), respectively. A negative control and a positive control (Mitomycin-C, 0.2 µg/mL, Sigma M-05030 (Sigma, St. Louis, MO, USA) were also used. The cells were exposed to colchicine (0.06 µg/mL, Sigma C9754) 2 h before harvesting. At the end of the incubation, cells were centrifuged at 1200 rpm for 15 min. Then, the cells were treated with 0.4% KCl (37 °C) as the hypotonic solution and methanol: glacial acetic acid (3:1) as the fixative (at room temperature 22 ± 1 °C, fixative treatments were repeated three times). The cells were centrifuged at 1200 rpm for 15 min after each fixative treatment. The staining of the air-dried slides was performed following the standard methods using 5% Giemsa stain for CA. The percentage of cells showing structural and/or numerical chromosome alterations were obtained by calculating the percentage of the aberrant metaphases from each concentration and treatment period. The CA was classified according to the ISCN (International System for Human Cytogenetic Nomenclature) (Paz-y-Miño et al. 2002). CAs were evaluated in 100 well-spread metaphases per donor (totally 400 metaphases per concentration). Gaps were not evaluated as CA (Mace et al. 1978). CAs were classified as structural and numerical aberrations. Structural CAs consisted of the chromatid type (breaks and exchanges) and the chromosome type (breaks, fragments, sister chromatid unions, chromatid exchanges, ring chromosomes and dicentrics) abnormalities, whereas the numerical CAs consisted of polyploid cells. For the determination of the genotoxicity, only the structural CAs were taken into consideration. The MI was determined by scoring 3.000 cells from each donor.
In vitro cytokinesis-block micronucleus assay
For the analysis of MN in binucleated lymphocytes, 0.2 mL of fresh whole blood (1/10 heparinized) was used to establish the cultures which were incubated for 68 h. The cells were treated with 100, 175, 250 and 325 µg/mL BF for 24- and 48-h treatment periods. To block cytokinesis, cytochalasin B (Sigma, C6762) was added at 44 h of the incubation at a final concentration of 6 µg/mL. After an additional 24-h incubation at 37 °C, cells were initially harvested by centrifugation at 1200 rpm for 15 min and further processed identically as described for the preparation of CA slides, with the exception of a 5 min hypotonic treatment step at 37 °C. Finally, the slides were stained with 5% Giemsa (Kirsch-Volders et al. 2003; Rothfuss et al. 2000). In all subjects, 1.000 binucleated lymphocytes were scored from each donor (4.000 binucleated cells were scored per concentration). A total of 1.000 cells (4.000 cells for each treatment concentration) were scored to calculate the nuclear division index (NDI) for the cytotoxicity of BF using the formula: NDI = (M1) + (2 × M2) + (3 × M3) + (4 × M4)/N, where M1–M4 represent the number of cells with one to four nuclei and N is the total number of the cells scored (Fenech 2000).
Statistics
Values of the control, solvent control, positive control and the exposed groups were expressed as the mean (±SE) from four separate experiments. The comparisons between the control, solvent control, positive control and the exposed groups were performed using t test at p ≤ 0.05. Concentration–response relationships were determined from the correlation and regression coefficients for the percentage of cells with CA, micronucleated binuclear lymphocytes (BNMN) as well as for the MI and NDI. Also, the remaining BF amounts in the supernatants of BF-treated cultures and DMSO control (Table 4—control tube without human peripheral blood lymphocytes) were assessed using HPLC technique. By comparing the final BF amount between the DMSO control and BF-treated cultures, the percentage (%) of BF that was passed to cells has been calculated. Then, the statistical significance between the % BF in DMSO control and BF-treated cultures was determined using the t test at p ≤ 0.05.
Results
The genotoxicity-inducing effect of BF in human peripheral lymphocytes has been studied at 4 different concentrations (100, 175, 250 and 325 µg/mL) and 2 different periods (24 and 48 h). These concentrations were selected from range-finding studies which showed that the viability in the highest concentration group reduced the mitotic index (MI) approximately 50% of control. The range-finding methodology was adapted from OECD Guideline 487 in which at least three analysable test concentrations should be evaluated. However, in order to study the concentration–response relation in detail, we selected 4 closely spaced concentrations of BF to be able to obtain better concentration–response data.
Table 1 shows the results of various treatments on the formation of chromosome aberration (CA) in human lymphocytes. BF induces CA when tested at 100 and 175 µg/mL in 24-h treatment, and at 100, 175 and 250 µg/mL in 48-h treatment period when compared with the negative control. However, when compared with the solvent control (DMSO), the abnormal cell percentage and the number of CA/cell did not show significant statistical difference in human lymphocytes treated with BF. Thus, BF does not induce CA (Fig. 2).
Chromosome aberrations and micronucleated binuclear human peripheral blood lymphocytes treated with BF for 24 and 48 h. a chromatid (B′) break (325 µg/ml BF, 48-h treatment, ♀) b chromosome (B″) break (250 µg/ml BF, 48-h treatment, ♀) c sister chromatid union (325 µg/ml BF, 24-h treatment, ♀) d binuclear cell with 1 micronucleus (100 µg/ml BF, 24-h treatment, ♂) e binuclear cell with 2 micronuclei (175 µg/ml BF, 48-h treatment, ♀)
Also, increasing BF concentrations did not cause a significant increase in the percentage of the binuclear cells with micronuclei for 24- and 48-h treatment periods. %MN was also not significantly increased when compared with both the negative and the solvent controls in cells treated with BF for 24- and 48-h treatment periods (Table 2).
The effects of various treatments of BF on cell-cycling kinetics in human peripheral lymphocytes have been assessed by using the MI and nuclear division index (NDI). While the MI is used to quantify the effect of BF on mitotic division, the NDI shows the effect of BF on nuclear division. In the present study, BF significantly reduced the MI at the two lowest concentrations when compared to the negative control in 24-h treatment, however, 24-h treatment with BF did not lead to a marked decrease in the MI when compared with the solvent control. In 48-h treated cultures, BF significantly reduced the MI at all concentrations up to 325 µg/mL when compared to the negative control; however, this decrease is statistically significant only at the two highest concentrations (250 and 325 µg/mL) when compared to the solvent control (Table 3). Moreover, BF, in both 24- and 48-h treatments, caused a concentration-dependent decrease in the MI (r = −0.995, p < 0.01 for 24-h; r = −0.992, p < 0.01 for 48-h). In accordance, NDI was significantly reduced at the three highest concentrations in the 24-h treatment and at all concentrations in the 48-h treatment when compared with the negative control (Table 3). Also, compared with the solvent control, various concentrations of BF treatment in cultured lymphocytes caused a significant reduction of NDI at the two highest concentrations (250 and 325 µg/mL) in 24-h treatment and at all concentrations in 48-h treatment. The reducing effect of BF on nuclear division of lymphocytes, as revealed by NDI, was clearly concentration-dependent in both 24- and 48-h treatment periods (r = −0.990, p < 0.01 for 24-h; r = −0.981, p < 0.01 for 48-h). Taking the MI and NDI into account together, BF particularly showed cytotoxic effect in 48-h treatment.
To determine the passing amount of BF into human lymphocytes the supernatant taken from centrifuged tubes at the end of both treatment periods (24- and 48-h) was further analyzed using HPLC. The quantified amount of BF that has passed into the cells is presented in Table 4. The results clearly show that the percentage BF passage into cells has statistical significance in cultures that were prepared for both the CA and MN tests when compared to DMSO control (Table 4).
Discussion
In this study, we evaluated the genotoxic potential of BF using CA and MN tests. To the best of our knowledge, this is the first study to evaluate the in vitro genotoxic effects of BF in cultured human peripheral lymphocytes. We used the MI and NDI as indicators of cytotoxicity to determine the effects of BF on lymphocyte cell division. Moreover, a quantitative approach using HPLC was undertaken to quantify the amount of BF passage to human peripheral lymphocytes.
Our results showed that BF was unable to induce CA and MN in human peripheral lymphocytes. However, Isidori et al. (2007) reported that BF and its photoproduct 2B induced a significant SOS response in E. coli PQ37 at concentrations between 0.625–5 mg/L. In the same study, structurally dissimilar fibrates, fenofibrate and gemfibrozil, have been also reported to induce a significant SOS response and to exert a high mutagenic effect in TA98 and TA100 strains of S. typhimurium. However, although BF does not induce CA and MN formation in our study, BF should not be considered a nongenotoxic drug. The mechanism leading to both frameshift mutations and SOS response in bacteria requires DNA strand breaks, which is the common mutation that may also cause CA.
Moreover, BF (57 ng/L), gemfibrozil (380 ng/L) and the structurally dissimiliar atorvastatin (statin group, 13 ng/L) have been reported to induce damage to sperm DNA isolated from human samples in the comet, diffusion and tunnel assays and in the RAPD–PCR, respectively (Rocco et al. 2012). The reason for the apparent discordance that BF could not induce CA and MN in our study, but apparently induces DNA damage in the comet assay (Rocco et al. 2012) is not clear but negative CA and MN versus positive comet assay results should be interpreted carefully. If the comet assay is carried out quickly after the treatment of cells with the test material, the comet data could be positive while the primary damage may have been sufficiently repaired, giving negative results with respect to CA and MN (Wiedemann and Schutz 2008). Thus, because the comet assay and the in vitro CA and MN assays evaluate relatively different aspects of DNA damage (dependent on the sampling time), it should not be surprising that such discrepancies exist.
The present study clearly demonstrates a BF-induced concentration-dependent cytotoxicity in human peripheral lymphocytes as revealed by significant decreases in both the MI and NDI. Our results on the cytotoxicity of BF are in apparent concordance with the study of Rocco et al. (2012). BF, in the diffusion assay, clearly induces DNA fragmentation and apoptosis in human sperm cells even at a very low concentration (57 ng/L). It was also shown that clofibrate, a structural analogue of BF, increased the production of superoxide anion four-fold over the controls and increased the cytotoxicity of BCNU (N,N′-bis(2-chloroethyl)-N-nitrosourea) in L1210 cells (Lawson and Gwilt 1993). Clofibrate have also been reported to increase cellular sensitivity to adriamycin-treated human (CML) and murine leukemia (P388) cells in vitro (Parekh et al. 1990; Chitnis et al. 1989). It has been previously proposed that one of the mechanisms of carcinogenic action of peroxisome proliferators occurs due to perturbation of lipid metabolism and subsequent ROS formation leading to indirect DNA damage (Rao and Reddy 1996). Interestingly, BF and clofibrate both share a toxicophore with a chlorine atom at the 4-position of the phenyl ring which is suspected to be a possible rodent carcinogen (Benigni and Giuliani 1996). Thus, our data may suggest that BF induces oxidative stress and subsequent DNA damage.
In accordance with our findings, BF was shown to cause obvious concentration-dependent reduction in cell proliferation and induction of cytotoxicity in human rhabdomyosarcoma cells by an apoptotic-like injury through a pathway dependent on PPARα and repression of phosphorylation of AKT upon DNA damage (Maiguma et al. 2003; Zhao et al. 2010). It has been recognized that DNA lesions initiate pathways responsible for the cell-cycle arrest to repair DNA damage or, alternatively, DNA lesions can mediate clearance of affected cells through apoptosis or senescence (Heijink et al. 2013). Thus, we are of the opinion that BF-induced unrepaired DNA damage may have either caused cell-cycle delay or rapidly directed human lymphocytes to cytotoxic pathways as detected by significant concentration-dependent reduction of both the MI and NDI.
Conclusion
BF does not induce chromosome aberrations or micronuclei, but exerts potent cytotoxic effect in human peripheral lymphocytes; however, it should also be mentioned that other genotoxicity test systems have proven that BF is also capable to induce DNA damage in bacteria as well as in human sperm (Isidori et al. 2007; Rocco et al. 2012). Moreover, the use of hypolipidemic agents in long-term has been associated with myopathy, myalgia, decline in brain functions, amnesia (Abd and Jacobson 2011) and anemia (Ariad and Hechtlinger 1993; Kacirova and Grundmann 2015). Therefore, it is essential that hypolipidemic drugs should be tested not only for their genotoxic potential but also for their ability to disturb distinct cellular processes which lead to cytotoxicity, in order to provide a deeper understanding of the potential risks related to exposure.
References
Abd TT, Jacobson TA (2011) Statin-induced myopathy: a review and update. Expert Opin Drug Saf 10:373–387
Albertini RJ, Anderson D, Douglas GR, Hagmar L, Hemminki K, Merlo F, Natarajan AT, Norppa H, Shuker DEG, Tice R, Waters MD, Aitio A (2000) IPCS guidelines for the monitoring of genotoxic effects of carcinogens in humans. Mutat Res 463:111–172
Alvergnas M, Rouleau A, Lucchi G, Heyd B, Ducoroy P, Richert L, Martin H (2011) Proteomic mapping of bezafibrate-treated human hepatocytes in primary culture using two-dimensional liquid chromatography. Toxicol Lett 201:123–129
Anchisi C, Fadda AM, Maccioni AM, Dessì S (1998) Determination of bezafibrate concentration by high performance liquid-chromatography in serum of rats treated with lead nitrate. Farmaco 53:690–692
Ariad S, Hechtlinger V (1993) Bezafibrate-induced neutropenia. Eur J Haematol 50:179
Ashby J, Brady A, Elcombe CR, Elliott BM, Ishmael J, Odum J, Tugwood JD, Kettle S, Purchase IF (1994) Mechanistically based human hazard assessment of peroxisome proliferator-induced hepatocarcinogenesis. Hum Exp Toxicol 13:S1–S117
Benigni R, Giuliani A (1996) Quantitative structure-activity relationship (QSAR) studies of mutagens and carcinogens. Med Res Rev 16:267–284
Benn P, Delach J (2008) Human lymphocyte culture and chromosome analysis. Cold Spring Harb Protoc 3:1–7
Bonassi S, Norppa H, Ceppi M, Strömberg U, Vermeulen R, Znaor A, Cebulska-Wasilewska A, Fabianova E, Fucic A, Gundy S, Hansteen IL, Knudsen LE, Lazutka J, Rossner P, Sram RJ, Boffetta P (2008) Chromosomal aberration frequency in lymphocytes predicts the risk of cancer: results from a pooled cohort study of 22 358 subjects in 11 countries. Carcinogenesis 29:1178–1183
Bonassi S, El-Zein R, Bolognesi C, Fenech M (2011) Micronuclei frequency in peripheral blood lymphocytes and cancer risk: evidence from human studies. Mutagenesis 26:93–100
Carrano AV, Natarajan AT (1988) International commission for protection against environmental mutagens and carcinogens. ICPEMC publication no. 14. Considerations for population monitoring using cytogenetic techniques. Mutat Res 204:379–406
Cattley RC, DeLuca J, Elcombe C, Fenner-Crisp P, Lake BG, Marsman DS, Pastoor TA, Popp JA, Robinson DE, Schwetz B, Tugwood J, Wahli W (1998) Do peroxisome proliferating compounds pose a hepatocarcinogenic hazard to humans? Regul Toxicol Pharmacol 27:47–60
Chitnis M, Parekh H, Satyamoorthy K (1989) Differential effect of clofibrate on adriamycin cytotoxicity in P388 murine leukemia cells sensitive and resistant to adriamycin. Tumori 75:100–105
Evans HJ (1984) Human Peripheral Blood Lymphocytes for the Analysis of Chromosome Aberrations in Mutagen Tests. In: Kilbey BJ, Legator M, Nichols W, Ramel C (eds) Handbook of mutagenicity test procedures, 2nd edn. Elsevier Science Publishers BV, Amsterdam, pp 405–427
Fenech M (2000) The in vitro micronucleus technique. Mutat Res 455:81–95
Fenech M, Holland N, Zeiger E, Chang WP, Burgaz S, Thomas P, Bolognesi C, Knasmueller S, Kirsch-Volders M, Bonassi S (2011) The HUMN and HUMNxL international collaboration projects on human micronucleus assays in lymphocytes and buccal cells–past, present and future. Mutagenesis 26:239–245
Forcheron F, Cachefo A, Thevenon S, Pinteur C, Beylot M (2002) Mechanisms of the triglyceride- and cholesterol-lowering effect of fenofibrate in hyperlipidemic type 2 diabetic patients. Diabetes 51:3486–3491
Gonzalez FJ (1997) The role of peroxisome proliferator activated receptor a in peroxisome proliferation, physiological homeostasis, and chemical carcinogenesis. Adv Exp Med Biol 422:109–125
Hagmar L, Bonassi S, Stromberg U, Brogger A, Knudsen LE, Norppa H, Reuterwall C (1998) Chromosomal aberrations in lymphocytes predict human cancer: a report from the European Study Group on Cytogenetic Biomarkers and Health (ESCH). Cancer Res 58:4117–4121
Hagmar L, Stromberg U, Bonassi S, Hansteen IL, Knudsen LE, Lindholm C, Norppa H (2004) Impact of types of lymphocyte chromosomal aberrations on human cancer risk: results from Nordic and Italian cohorts. Cancer Res 64:2258–2263
Heijink AM, Krajewska M, van Vugt MATM (2013) The DNA damage response during mitosis. Mutat Res 750:45–55
Honda A, Ikegami T, Nakamuta M, Miyazaki T, Iwamoto J, Hirayama T, Saito Y, Takikawa H, Imawari M, Matsuzaki Y (2013) Anticholestatic effects of bezafibrate in patients with primary biliary cirrhosis treated with ursodeoxycholic acid. Hepatology 57:1931–1941
Howe B, Umrigar A, Tsien F (2014) Chromosome preparation from cultured cells. J Vis Exp 83:e50203. doi:10.3791/50203
Isidori M, Nardelli A, Pascarella L, Rubino M, Parrella A (2007) Toxic and genotoxic impact of fibrates and their photoproducts on non-target organisms. Environ Int 33:635–641
Kacirova I, Grundmann M (2015) Fenofibrate-induced anemia and neutropenia—a case report. Clin Ther 37:103
Kirsch-Volders M, Sofuni T, Aardema M, Albertini S, Eastmond D, Fenech M, Ishidate M Jr, Kirchner S, Lorge E, Morita T, Norppa H, Surralles J, Vanhauwaert A, Wakata A (2003) Report from the in vitro micronucleus assay working group. Mutat Res 540:153–163
Lake BG, Rumsby PC, Price RJ, Cunninghame ME (2000) Species differences in hepatic peroxisome proliferation, cell replication and transforming growth factor-beta1 gene expression in the rat, Syrian hamster and guinea pig. Mutat Res 448:213–225
Lawson T, Gwilt PR (1993) Clofibrate enhances the DNA damaging action and cytotoxicity of nitrosoureas. Cancer Lett 70:119–122
Mace ML Jr, Daskal Y, Wray W (1978) Scanning electron microscopy of chromosome aberrations. Mutat Res 52:199–206
Maiguma T, Fujisaki K, Itoh Y, Makino K, Teshima D, Takahashi-Yanaga F, Sasaguri T, Oishi R (2003) Cell-specific toxicity of fibrates in human embryonal rhabdomyosarcoma cells. Naunyn-Schmiedeberg’s Arch Pharmacol 367:289–296
Marsman DS, Cattley RC, Conway JG, Popp JA (1988) Relationship of hepatic peroxisome proliferation and replicative DNA synthesis to the hepatocarcinogenicity of the peroxisome proliferators di(2-ethylhexyl)phthalate and [4-chloro-6-(2,3-xylidino)-2-pyrimidinylthio]acetic acid (Wy-14,643) in rats. Cancer Res 48:6739–6744
Nishimura J, Dewa Y, Muguruma M, Kuroiwa Y, Yasuno H, Shima T, Jin M, Takahashi M, Umemura T, Mitsumori K (2007) Effect of fenofibrate on oxidative DNA damage and on gene expression related to cell proliferation and apoptosis in rats. Toxicol Sci 97:44–54
Parekh H, Satyamoorthy K, Advani S, Chitnis M (1990) Sensitization of chronic myeloid leukemia cells to Adriamycin cytotoxicity by clofibrate. Tumori 76:18–21
Paz-y-Miño C, Bustamante G, Sanchez ME, Leone PE (2002) Cytogenetic monitoring in a population occupationally exposed to pesticide in Ecuador. Environ Health Perspect 110:1077–1080
Rao MS, Reddy JK (1996) Hepatocarcinogenesis of peroxisome proliferators. Ann N Y Acad Sci 804:573–587
Reddy JK, Lalwai ND (1983) Carcinogenesis by hepatic peroxisome proliferators: evaluation of the risk of hypolipidemic drugs and industrial plasticizers to humans. Crit Rev Toxicol 12:1–58
Rocco L, Peluso C, Cesaroni F, Morra N, Cesaroni D, Stingo V (2012) Genomic damage in human sperm cells exposed ın vitro to environmental pollutants. J Environ Anal Toxicol 2:117
Rose ML, Rusyn I, Bojes HK, Belyea J, Cattley RC, Thurman RG (2000) Role of Kupffer cells and oxidants in signaling peroxisome proliferator- induced hepatocyte proliferation. Mutat Res 448:179–192
Rothfuss A, Schutz P, Bochum S, Volm T, Eberhardt E, Kreirenberg R, Vogel W, Speit G (2000) Induced micronucleus frequencies in peripheral lymphocytes as a screening test for carriers of a BRCA1 mutation in breast cancer families. Cancer Res 60:390–394
Schoonjans K, Staels B, Auwerx J (1996) Role of the peroxisome proliferator-activated receptor (PPAR) in mediating the effects of fibrates and fatty acids on gene expression. J Lipid Res 37:907–925
Staels B, Dallongeville J, Auwerx J, Schoonjans K, Leitersdorf E, Fruchart JC (1998) Mechanism of action of fibrates on lipid and lipoprotein metabolism. Circulation 98:2088–2093
Tanaka T (2012) Preclinical cancer chemoprevention studies using animal model of ınflammation-associated colorectal carcinogenesis. Cancers 4:673–700
Tawfeeq MM, Suzuki T, Shimamoto K, Hayashi H, Shibutani M, Mitsumori K (2011) Evaluation of in vivo genotoxic potential of fenofibrate in rats subjected to two-week repeated oral administration. Arch Toxicol 85:1003–1011
Wiedemann PM, Schutz H (2008) The role of evidence in risk characterization: making sense of conflicting data. Weinheim: Wiley-VCH
Zhao Y, Okuyama M, Hashimoto H, Tagawa Y, Jomori T, Yang B (2010) Bezafibrate induces myotoxicity in human rhabdomyosarcoma cells via peroxisome proliferator-activated receptor a signaling. Toxicol In Vitro 24:154–159
Acknowledgements
This study was sponsored by Cukurova University Research Fund; Grant Number FEF2013YL11.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Topaktas, M., Kafkas, N.E., Sadighazadi, S. et al. In vitro cytogenetic toxicity of bezafibrate in human peripheral blood lymphocytes. Cytotechnology 69, 579–589 (2017). https://doi.org/10.1007/s10616-017-0069-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10616-017-0069-4