Abstract
With stroke being one of the leading causes of disability worldwide, families and social systems may face strain as they adjust to a caregiving role. This strain may be amplified in family systems living in rural areas due to limited access to resources. Thus, it is important for helping professionals such as couple, marriage, and family therapists to understand what facets of this disability are linked with caregiver strain as well as to explore and understand various interventions that may ease caregiver burden. Using existing data from 177 pairs of stroke patients and their family caregivers in rural Mainland China, the present study utilized a moderation analysis to examine (1) the association between stroke patient physical functioning, patient mental health, and their family caregiver burden and (2) how a developed patient rehabilitation intervention program for caregivers moderated the association between patient physical functioning as well as mental health and caregiver burden 6-month post intervention. Results suggested that better patient physical functioning were related to lower levels of caregiver burden (b = − 1.418, p < .001, β = − 0.33). However, the developed rehabilitation intervention program did not significantly moderate the association between stroke patient physical functioning as well as mental health and caregiver burden. These findings provide insight into correlates of stroke patients’ caregiver burden in rural China. Development of more effective rehabilitation programs and interventions for stroke patients and their family caregivers as well how couple, marriage, and family therapists may be uniquely qualified to contribute to such interventions is discussed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
In recent years, stroke has become the leading cause of death in China with notably higher rates of occurrence in rural communities (Wang et al. 2017). In rural China specifically, where more than half of the population lives, 0.92% of the population had a stroke in 2013 compared to 0.36% in 1985 (Wang et al. 2017). Stroke is also the leading cause of adult disability worldwide (Bonita et al. 2004) resulting in approximately 10–11 years of disability-adjusted life (Cadilhac et al. 2010). Within Hong Kong, China more than half of stroke survivors remained dependent on community or family care approximately one year later (Lo et al. 2008). In rural China, especially, formal health care and social service resources for post-stroke could be sparse thus resulting in majority of long term caregiving responsibility being left to family members (Yan et al. 2016). This lack of support and attention offered to caregivers in these rural communities could increase a caregivers’ experiencing strain such as physical and mental health concerns, emotional distress, and financial strain (Berg et al. 2005; Chen et al. 2010). Further, this lack of support may also increase the likelihood of caregivers abusing and having conflict with those they are caring for (Steinmetz 1988). Magnifying this lack of support, many Chinese family caregivers report feeling pressure to avoid seeking assistance or advocating for their own needs (Chen et al. 2010), thus possibly isolating themselves even further.
Despite prevalence rates of stroke and caregiving responsibilities of family members within China and many of the poor consequences of caregivers feeling overly burdened, minimal research has examined how stroke patients’ health are linked with caregiver burden among rural populations. Further, minimal research has examined interventions and efforts to best support these rural caregivers to curb possible burden they may experience. Developing our understanding of these areas could be beneficial for helping professionals such as couple, marriage, and family therapists (CMFT) as they seek for innovative ways to support these family systems and reduce the strain they may be experiencing. Using an existing rural Chinese sample of stroke patients and their caregivers, the present study has a twofold purpose: (1) to understand links of a stroke patient’s mental health and physical functioning with rates of burden their caregiver experiences and (2) how a developed patient rehabilitation intervention program for caregivers moderates the association between patient physical functioning as well as mental health and caregiver burden 6-month post intervention.
Theoretical Foundation
As a guide, the present study utilizes systems theory which views the family and other surrounding contextual factors as a system filled with interacting and moving parts. Rather than seeing individuals within a vacuum, it seeks to understand how each part of a system influence and shape other parts of the system (Bateson 1972). This theory is well developed for Chinese populations because of the culture’s widely accepted beliefs surrounding Confucianism which emphasizes humans as part of interconnected and embedded within a larger network of various positions and roles such as family caregivers (Cheung and Chan 2002). Clinical approaches rooted in systems theory such as structural family therapy (Minuchin 1974) and Satir (1983) has been widely used and successful within Chinese culture (Cheung and Chan 2002; Epstein et al. 2012). Therefore, examining experiences of rural Chinese family caregivers through a systems theory lens may allow for optimal understanding and application in seeking ways to support them. With CMFT’s emphasis on psychological and social well-being by focusing on contextual and systemic factors (Clark and Currie 2009), they may be uniquely equipped to serve this population.
Literature Review
Family Caregivers of Stroke Patients
Family caregivers, such as those supporting stroke patients in China, provide essential support by monitoring patients’ health conditions, overseeing and supporting patients’ rehabilitation activities, assisting in daily physical functioning such as eating, using the toilet, and bathing, as well as providing emotional support for patients (Sit et al. 2004). While engaging in these numerous efforts many family caregivers of stroke patients experience caregiving stress and burden (Caro et al. 2017; Mak et al. 2007). They suffer from physical exhaustion, psychological and emotional distress (Berg et al. 2005; Chen et al. 2010), relationship strain (Forbat et al. 2012), financial burden (Chen et al. 2010), and restrictions on social life (Mackenzie et al. 1998). One study suggested that 40% of family caregivers had somatic symptoms including headaches, stomach discomfort, as well as reduced physical strength and appetite. These same caregivers also reported they received less support from their community networks than they expected (Sit et al. 2004). Despite family caregivers expecting and requiring support from others, many caregivers’ physical and mental health takes lower priority than the patients’ or is often neglected by professionals and community members (Coombs 2007). With these frequently encountered physical and mental health concerns, some have referred to them as the second patient in the family (Sit et al. 2004). Coupling these poor experiences and outcomes with cultural norms that pressure many Chinese caregivers to not express their burden or difficult circumstances (Chen et al. 2010), could leave caregivers feeling even more isolated and unsupported in their roles. Further, this lack of support and attention may also increase the likelihood of abusive and conflict saturated environments with the patient (Steinmetz 1988).
Patients’ Physical and Mental Health Conditions Associated with Caregiver Burden
Previous research has suggested that a stroke patient’s physical and mental capacities are linked with caregiver burden. For example, stroke patient’s physical functioning, as assessed by the Barthel-Index (Mahoney and Barthel 1965), is inversely related with caregiver burden (Visser-Meily et al. 2005). Specifically, as stroke patients were more physically dependent on their caregiver to do daily functions such as showering, feeding, using the toilet, and moving around, the more likely the caregiver would report experiencing larger burdens 1 year later. Further, previous research has suggested that stroke patients who are experiencing poor emotional and cognitive stability may increase the risk for their caregivers to encounter burnout (Chen et al. 2010; van den Heuvel et al. 2001). Other research evaluating stroke patients from South Korea suggested that patients’ increased physical disability and higher rates of depressive symptoms were linked with higher reports of caregiver burnout (Choi-Kwon et al. 2005). However, a study conducted in Hong Kong, China suggested that a stroke patient’s physical abilities may not be related to their caregiver’s physical health, mental health, and experiences with burnout (Chen et al. 2010) and other studies conducted in the West found similar results (Thommessen et al. 2001). Lastly, there was no study that tested the relationship between patients’ health and family caregivers’ health. With these mixed results and limited studies in rural China, additional research is necessary to better understand family caregivers in rural China, their experiences with burnout, and what interventions and systemic factors can best support them and their efforts.
Rehabilitation Intervention for Stroke Patient and Caregivers
Some scholars have suggested that rehabilitation programs should not merely focus on stroke patients, but rather needs a systemic approach that is inclusive of both patient and caregiver (McCullagh et al. 2005). Traditionally, stroke rehabilitation is an intervention primarily used to assist victims of stroke to cope with impairments caused by the stroke (Langhorne et al. 2011). Previous studies evaluating these rehabilitation interventions have predominantly focused on the wellbeing of stroke patients. Few rehabilitation studies examined caregiver burden after a rehabilitation intervention program despite previous research indicating that familial and community support factors are important for the improvement of the stroke patient (Kalra et al. 2004; McCullagh et al. 2005). Of the limited studies available, there is seemingly promise to this systemic approach. Rehabilitation interventions that include caregivers or have a component specifically for caregivers that focus on areas such as moving, handling, and simple nursing tasks for the patient has been linked with lower reports of caregiver burden and improved psychological functioning of the caregiver (Kalra et al. 2004). Moreover, these types of programs have illustrated a reduction in caregivers’ levels of anxiety and depression in the months following the intervention (McCullagh et al. 2005). Interventions including teaching nursing skills sought to improve family caregivers’ competency on delivering care which have also been previously illustrated to reduce burden (Ostwald et al. 1999). However, research has not consistently illustrated this as in the case of a home-based intervention for caregivers (Anderson et al. 2000). Due to the sparse and inconsistent research evaluating caregiver burden within rural China and other populations, further consideration is needed to best guide helping professionals to offer interventions and support that will benefit both patient and caregiver.
The Present Study
Driven by the need to address the lack of caregiving research among rural Chinese stroke patients and using systems theory as a guide, the present study used existing data from 177 stroke patients and their family caregivers to fulfill a two-fold purpose. First, to examine the associations between stroke patient physical functioning and mental health condition with caregiver burden among a rural population in China. Second, to examine if a stroke rehabilitation program that included caregivers could alter how a stroke patient’s physical functioning and mental health condition interacts with caregiver burden. Specifically, this is done through a dyadic moderation analysis examining links between physical functioning and mental health of stroke patients, caregiver burden symptoms, and a rehabilitation intervention including caregivers. Further, this analysis examined how this rehabilitation intervention may have moderated or buffered the association between a stroke patient’s health and caregiver burden symptoms 6-months after the intervention (see Fig. 1). Two hypotheses are proposed:
-
1.
Higher reports of stroke patient physical functioning and mental stability will be associated with lower reports of caregiver burden 6-months after patient discharge. The stroke rehabilitation program will significantly moderate or alter the link between the stroke patient’s physical functioning as well as mental stability and caregiver burden 6-months after patient discharge. Specifically, that despite stroke patients’ low physical functioning and mental stability, that caregivers that participated in the rehabilitation intervention will still experience lower caregiver burden.
Method
Procedures
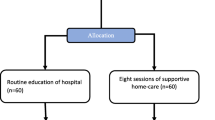
The present study analyzed existing data from RECOVER, a parallel-arm randomized controlled trial conducted in three county hospitals located in Liaoning Province (northeast), NingXia Hui People Autonomous Region (northwest), and Chongqing Municipality, China (southwest) (Yan et al. 2016). Patients and family caregivers were recruited by trained nurses in each hospital with support from physicians. Physicians gave permission to nurses to begin recruitment once they believed that stroke patients were in a state of suitable health to begin baseline assessment and rehabilitation activities. After recruitment, eligible and consenting patients were randomized into the control group and the intervention group by a 1:1 ratio. The design, implementation of the intervention, and the reporting of this experimental study followed the suggestions of CONSORT 2010 statement on parallel group randomized trials (Schulz et al. 2010).
Established randomization procedures and a secure, central, password protected, and internet-based computerized system were used. Randomization was stratified by functional status within two groups: Barthel Index 0–<40 vs. 40–80. Within each Barthel Index stratum, block randomization technique was adopted to reduce the possibility of large imbalance in the number of patients randomized into the two groups within a short time period. The block size varies to avoid nurses’ attempting to guess which group the patient may be randomized into. After nurses completed baseline evaluation on a digital application through secure and password-protected connections, the application automatically informed nurses of patients’ allocation status.
Intervention
We developed a simplified stroke rehabilitation program that included family caregivers based on previous research (McCullagh et al. 2005). Family caregivers were first trained by nurses and then applied the principles of caregiving to disabled stroke patients that they were caring for in rural China. This simplified rehabilitation program provided information about the care process and trained caregivers to respond effectively to stroke related problems, such as feeding, bathing, grooming, dressing, toilet use, and how to manage poor moods of the stroke patient. The aim of this intervention was to improve patient physical functioning but also to reduce caregiver burden (Yan et al. 2016).
We recruited at least two and up to three nurses from each county hospital who were then trained centrally by rehabilitation physicians and physiotherapists from Peking University First Hospital in Beijing, China. A care-based method and the teach-back technique were used to assure nurses’ ability and effectiveness to train caregivers. We also designed a menu-style checklist for nurses to facilitate the training and guide the intervention. Patient and family caregivers were trained by these nurses and were given an aid of an easy-to-understand picture-rich rehabilitation manual, specially designed for this study. The manual is based upon the principles of being evidence-based, practical and feasible with a multi-faceted health education and operation guide. Beyond the manual, prior to discharge, patients and caregivers in the intervention group were also given a videodisk of the operational training process to provide basic principles and tips on conducting rehabilitation services if the caregiver was seeking additional support. Since this video was given as supplemental material and there may have been limitations in caregivers ability to fully utilize or apply it, assessment of its use and helpfulness was not a central focus of this study.
The training was focused on the ten domains in the Barthel Index (Mahoney and Barthel 1965) classified into three groups: mobility (transfer, mobility, and stairs), self-care (grooming, feeding, dressing, and bathing), and toileting (bowel, bladder, and toilet use). The intervention package also included: (1) brief information on stroke recovery trajectory, risk identification, management of low mood for patients and caregivers, and importance of repeated practice of specific activities; (2) patient-centered joint goal setting with patient, caregiver, and nurse; and (3) discharge planning focusing on rehabilitation, summarizing the training provided to each caregiver, goals set for the patient, and steps to be taken to achieve the goals. The in-hospital component emphasizing task-oriented operational training was delivered in 3–6 short (15–30 min) sessions to patients and caregivers. Nurses also provided follow-up care via three phone calls to the patients and/or family caregivers after the patients were discharged at Weeks 2, 4, and 8. Nurses discussed progress and problems patients or caregivers encountered since discharge or the last phone call with the patient or the caregiver and proposed feasible solutions, when possible. Patients in the control group received conventional care as usual. Normally they receive symptom-targeted medical treatment and regular nursing care without rehabilitation services. The outcome evaluation included baseline assessment, pre-discharge evaluation via face-to-face interview, 3-month, and 6-month post-intervention telephone interview.
Sample
The total sample was composed of 246 stroke patients and 246 family caregivers. Those caregivers that transitioned into the role after the initial rehabilitation intervention (a total of 67) were excluded from the present study as they did not receive the intervention. We also removed two caregivers when two stroke patients passed away between the intervention and the follow-up. This resulted in a total of 177 pairs of stroke patients and their family caregivers used in this study, with 94 in the control group and 83 in the intervention group. The control group was coded as “0” and the intervention group was coded as “1”. The mean age of family caregivers was 52.10 years (SD = 12.57, ranging from 20 to 80). Of the family caregivers, 45.20% reported being female, 59.15% reporting being male, and 5.65% did not report their gender. Further, 50.28% of family caregivers were a spouse of the patient, 42.94% were a child of the patient, 0.56% were a sibling of the patient, 0.56% were a parent of the patient, and 5.65% did not report their relation to the patient. The caregivers used in this analysis were quite diverse in terms of income, educational background, and caregiver burden as exhibited in Table 1.
Measures
Family Caregiver Burden
At 6-month post-intervention, family caregivers were asked about the amount of burden they experienced in taking care of their stroke patient. The indicators of family caregivers burden were assessed using the five subscales of the Chinese version of the Caregiver Burden Inventory: time dependency, development, physical health, emotional health, and social relationships (Chou et al. 2002). Previous research has indicated that the Chinese version of the Caregiver Burden Inventory is a valid and reliable research instrument in measuring caregiver burden in Chinese populations (Chou et al. 2002). Sample items include “He/she is dependent on me,” “I feel that I am missing out on life,” “My health has suffered,” “I feel angry about my interactions with him/her,” and “I feel resentful of other relatives who could but do not help.” Responses range from 0 = Rarely to 4 = Nearly Always, with higher scores evidence of greater level of care burden. The sum was calculated for each subscale. Cronbach’s alpha indicated acceptable reliability for each of the five subscales (time dependency: α = 0.93; development: α = 0.88; physical health: α = 0.96; emotional health: α = 0.79; and social relationship: α = 0.87). The sum of each subscale functioned as an indicator for constructing a latent variable of family caregiver burden.
Physical Functioning
At the baseline assessment, stroke patients were asked about their performance in daily activities using the Barthel Index. This 10-item scale has three domains: mobility, self-care, and continence/toileting (Mahoney and Barthel 1965). It has a maximum score of 100. It has been used with Chinese populations with acceptable reliability (Dai et al. 2000). Sample activities include feeding, bathing, grooming, dressing, toilet use, and mobility. Although each activity was scored differently, lower scores (e.g. 0) indicated greater dependence or inability to do a specific activity and higher scores (e.g. ranges 5–15) indicated more independence or ability to complete activity with no assistance (see Mahoney and Barthel 1965). For example, the activity of being mobile has responses of 0 = immobile or < 50 yards; 5 = wheelchair independent, including corners, > 50 yards; 10 = walks with help of one person (verbal or physical) > 50 yards; or 15 = independent (but may use any aid; for example, stick) > 50 yards. The 10 items were summed with higher scores indicating better functioning with daily activities. Cronbach’s alpha indicated acceptable reliability with α = 0.85.
Mental Health
At the baseline assessment, the 2-item scale of the Patient Health Questionnaire (PHQ-2) assessed stroke patients’ mental health. PHQ-2 is a valid and reliable tool for Chinese populations (Zhang et al. 2013). The two items used were “Little interest or pleasure in doing things”, and “Feeling down, depressed, or hopeless.” Participants rated their responses over the last two weeks using 0 = not at all, 1 = several days, 2 = more than half the days, to 3 = nearly every day. These items were reverse coded and summed with higher scores indicating better mental health functioning. The two items Cronbach’s alpha was acceptable with α = 0.92.
Control Variables
Due to previous research indicating that gender and family income being linked with caregiver well-being and burden, they were utilized as controls (Tang and Chen 2002; van Den Heuvel et al. 2001). Family caregivers’ gender was measured at the 6-month follow-up. Gender was indicated by 1 = male and 2 = female. Family income was measured at the baseline assessment before the intervention. Family income was coded as following: 1 = less than 5000 RMB, 2 = 5000–99,99 RMB, 3 = 10,000–19,999 RMB, 4 = 20,000–29,999 RMB, 5 = 30,000–39,999 RMB, 6 = 40,000–49,999 RMB, 7 = 50,000–99,999 RMB, 8 = more than 100,000 RMB.
Analytic Plan
The purpose of this study was to test the associations of patients’ physical functioning and mental health with their family caregiver’s burden. Further, to test whether a simplified stroke rehabilitation program can moderate the relationship of patients’ physical functioning and mental health with their family caregiver’s burden. These was examined through a dyadic moderating analysis, a form of structural equation modeling, using Mplus 7.0 using individual raw data (Muthén and Muthén 2012).
The data were first explored with descriptive statistics to examine the data distribution and missing data in STATA 14 (Stata Corporation 2015). Data normality values were within acceptable ranges of skewness (< |3.0|) and kurtosis (< |10.0|) (Kline 2011). Across the 10 variables used in the study, missing data ranged from 0.00% (family income) to 5.65% (family caregiver gender). As a result, we used maximum likelihood (FIML) to handle missing data for our primary analysis (Acock 2005). Further, we included caregiver age and family members number as auxiliary variables to improve the performance of the FIML data estimator and to improve statistical power (Collins et al. 2001). Correlations were computed to examine the bivariate associations among the constructs. It revealed that observations were independent (See Table 2).
After testing the correlations between the variables, a confirmatory factor analysis (CFA) on family caregiver burden was first conducted to ensure that the measurement model fit the data well before testing the full, primary analysis. The CFA demonstrated a good fit to the data by using the model index guidelines (Hu and Bentler 1999): χ2 (2) = 1.25, p = .53, root mean square error of approximation (RMSEA) = 0.00, 95% CI (0.000–0.134), comparative fit index (CFI) = 1.000, Tucker–Lewis Index (TLI) = 1.006, and standardized root mean square residual (SRMR) = 0.007. After ensuring an appropriate measurement model, we proceeded to run our full, primary analysis of a dyadic moderation analysis through Mplus 7.0 (Muthén and Muthén 2012). To examine the specific moderation capabilities of the rehabilitation program on the association between patients’ health (physical functioning and mental health) and caregivers’ burden, this path analysis was constructed with standardized variables of physical functioning, mental health, and interaction terms of standardized variables. This consisted of Caregiver Burden being regressed on Pt. Physical Functioning, Pt. Mental Health, Intervention, Physical Functioning × Intervention (interaction term), and Mental Health × Intervention (interaction term). Caregivers’ burden was also regressed on two control variables: gender and family income. We did not include caregivers’ education as control variable in our final model because when running the model, we discovered education in this population did not affect burden outcomes. Based on the parsimony principle, we did not include it.
Results
Descriptives and Correlations
The total scores of family caregivers burden near or above 36 indicates a risk of burnout and a greater need for respite and other services (Novak and Guest 1989). Based on 36-point cutoff, 27.7% of caregivers in this sample were equal to or above 36 points indicating numerous caregivers at risk for burnout. The results of the correlation analysis can be viewed in Table 2. Patients’ mental health were significantly associated with family caregivers’ burden including physical health (r = − .34, p < .001), time dependency (r = − .18, p < .05), development (r = − .26, p < .001), and social relationships (r = − .36, p < .001), except emotional health. Moreover, stroke patients’ physical health were significantly associated with family caregivers’ burden including physical health (r = − .319, p < .001), emotional health (r = − .23, p < .01), time dependency (r = − .39, p < .001), development (r = − .42, p < .001), and social relationships (r = − .33, p < .001). However, the rehabilitation intervention was not significantly associated with caregiver outcomes. Further, patients’ physical functioning were not associated with their own mental health.
Structural Equation Modeling Results
After testing correlations and the measurement model through a confirmatory factor analysis, the full dyadic moderation model was conducted including control variables to evaluate our two hypotheses (see Fig. 2). The model indicated appropriate fit to the data: χ2 (30) = 54.59, p = .004, root mean square error of approximation (RMSEA) = 0.07, 95% CI (0.039–0.099), comparative fit index (CFI) = 0.962, Tucker-Lewis Index (TLI) = 0.943, standardized root mean square residual (SRMR) = 0.038 (Hu and Bentler 1999). The standardized factor loadings for caregiver burden ranged from 0.78 to 0.91.
Model and standardized results of the rehabilitation intervention program moderating the link of physical functioning and mental health with caregiver burden 6 months later while controlling for caregiver gender and family income (n =177 stroke patients and their caregivers). Model fit indices χ2(30) = 54.59; RMSEA = 0.007, 95% CI (0.04–0.10); CFI = 0.96; TLI = 0.94; SRMR = 0.04. ap < 0.10, *p < 0.05, **p < 0.001 (two-tailed)
Our first hypothesis that a patient’s physical functioning and mental health would be inversely linked with their caregiver’s burden was partially supported. Specifically, when stroke patients reported higher rates of physical functioning their caregivers reported significantly less amounts of caregiver burden (b = − 1.418, p < .001, β = − 0.33). In other words, for one standard deviation improvement in patients’ physical functioning, there were a 0.33 standard deviation reduction in caregivers’ burden. Although not statistically significant at the 0.05 level, the association between stroke patients’ mental health and their caregivers’ burden were approaching significance within this sample (b = − 0.758, p = .072, β = − 0.178). Our second hypothesis that our rehabilitation intervention program would moderate the link of patients’ physical functioning and mental health with their caregivers’ burden was not supported within this sample. Overall, this model accounted for 27.5% of the variance in family caregivers’ burden.
Discussion
The purpose of this study was to examine the associations of stroke patient physical functioning and mental health with their family caregivers’ burden 6-months after discharge from a medical setting presently living in a rural Chinese area. Further, we examined if a simplified stroke rehabilitation program moderated or buffered the above association of physical functioning and mental health with caregiver burden. A dyadic moderating analysis was employed to analyze 177 pairs of stroke patients and family caregivers. Although results indicated that the rehabilitation program did not significantly moderate or reduce caregivers’ burden, other results indicated that stroke patients’ physical functioning was associated with caregiver burden 6-month after the rehabilitation program was offered. That is as stroke patients reported better physical functioning their caregiver experienced less burden. Additionally worth noting, the association between stroke patients’ mental health and their caregiver burden was approaching significance. Specifically, better mental health rates of the stroke patient were linked with lower rates of caregiver burden.
This study evaluating links between patients’ health, caregiver burden, and a rehabilitation program may be important for several reasons. First, minimal research has been completed evaluating caregivers’ experience with stroke patients in rural China. This study adds to this gap within the present literature and expands our understanding of experiences within this population. Second, descriptive statistics of the sample shine a light on the prevalence of concerning reports of caregiver burden. Third, this study reinforces the need for systemic helping professionals including CMFTs to understand that the decreased physical functioning of the patient is significantly linked with increased caregiver burden.
In an attempt to more fully understand stroke patients’ caregivers’ experiences in rural China, results of this study suggest that high percentage of family caregivers struggled with care burden. The average reported burden was 24.5 and over a quarter (27.7%) of caregivers in this sample reached 36 points or above on the CBI. Previous literature suggests that scores over 36 points indicate clinically concerning caregiver burden and that one should seek professional assistance (Novak and Guest 1989). Although some Western research indicates similar mean scores of reported caregivers’ burden (approximately 26) as the present study’s (Settineri et al. 2014), with the present sample being rural Chinese it is important to more fully understand the cultural context of these reports. Many among this population accept that it is a family’s sole responsibility to care for the elderly and sick and once in this role, many caregivers are then discouraged to fully express their personal feelings and experiences (Chen et al. 2010). With the present study’s caregiver burden evaluation being self-report these Chinese caregivers may not be fully transparent about their experiences or underreporting the severity of them due to these culture norms. If underreporting, this may indicate that this population may be experiencing elevated or above average caregiver burden.
Previous literature indicates that there may be several reasons why this population is encountering high rates of caregiver burden. First, the suppression of feelings may not only affect a caregivers’ mental health, but also physical health as well (Chen et al. 2010). Moreover, this group of caregivers may be less likely to express their own concerns and needs (Lui et al. 2000). This suggests that there may be cultural norms that create barriers for family caregivers to express needs and seek necessary support. Further, rooted in Chinese culture, the obligation or not feeling like one has a choice to take care of a family member might be a risk factor for burden. Lastly, many individuals and families living in rural China have low formal education levels with some estimating that only 10.06% have a high school or higher degree (Liu et al. 2014). This is echoed in the present study, with less than 15% of caregivers in the sample report having a high school or higher degree. This is worth noting because previous research has suggested that lower educational levels of a family caregiver is linked with a lack of understanding and applying information on best practices of care taking of a stroke patient (Sit et al. 2004). This link may be in part because much of the information and education that is given to caretakers is in written format. Thus, if a caretaker is experiencing difficulty with comprehending and understanding the written material, they may be less likely to implement the suggested guidance which therefore result in higher amounts of strain and burden.
Despite different cultural backgrounds, our results are consistent with previous studies, that have demonstrated family caregiver burden being associated with stroke patients’ physical functioning and mental health conditions, even after several months of the stroke event (Choi-Kwon et al. 2005; van den Heuvel et al. 2001). Knowing this mechanism is important for developing interventions to support and alleviate burden for caregivers as previous literature has indicated the need for unique and comprehensive emotional and support methods for stroke patients and their caregivers (Greveson and James 1991). For example, when using rehabilitation programs for reducing caregiver burden, developers of the program should also consider the toll that deterioration of mental and physical functioning of patients may have on the caregivers and provide methods for coping, resilience, and social support within their unique systems. Further, as understood through a systems theory lens, these findings indicate that helping professionals may also find it advantageous in reducing caregiver burden by troubleshooting ways to improve autonomy of the stroke patient to relieve stress on the caregiver.
Results of the present study did not support our hypothesis that the rehabilitation intervention would be significantly linked with lower rates of caregiver burden. Surprisingly, the family caregivers from our intervention group had higher levels of burden (see Table 1). With this intervention not successfully reducing caregiver burden it is important to reflect upon different strategies, contextual issues, and support methods that may result in lower caregiver burden rates. There are at least four plausible explanations why our intervention was not linked with lower rates of burden. First, previous literature has suggested that the duration and intensity of a rehabilitation program may impact its effectiveness (Toseland et al. 1990). The present intervention was only 30 min for each session with a maximum of five sessions of the program, totaling 150 min of training for caregivers. This amount of time might not be adequate for caregivers to learn and master all necessary skills to best care for stroke patients when they are back at home without nurses’ help. Another plausible reason why it did not reduce burden is because the program primarily focused on teaching how to care for patients’ physical and emotional needs rather than the caregivers’. This is not only illustrated in previous research that found similar results with a comparable structured rehabilitation program focused on patient needs (Anderson et al. 2000), but it also reinforces cultural norms that caregivers’ needs and difficulties are not as important as the patients’. Thirdly, with our intervention focusing on best care for the patient it may put more pressure, responsibility, and extra work on the caregiver which could result in increased burden. Caregivers may have viewed the intervention and practice of the intervention as additional stress, instead of a resource or tool to improve their experience of caregiving. This may possibly explain the intervention group reporting higher rates of burden compared to the control group. Lastly, our intervention is a practical support which may have reduced caregivers’ burden at the early stage, however, early stage relief was not measured but rather measured 6-months after the intervention was offered. Dowsell et al. (2000) demonstrated that caregivers need more practical support at the early stage of stroke patients’ rehabilitation with psychological support increasing over time. For future interventions, measuring caregiver burden at multiple timepoints could offer a more detailed illustration caregivers’ experiences directly after the intervention as well as months and years later.
Implication for Intervention and Treatment
Our study suggests that interventions are needed for family caregivers in rural China due to the prevalence and high level of reported care burden. Further, results indicates that stroke patient physical functioning and mental health conditions are possible risks for burn-out among family caregivers 6 months later after hospital discharge. This suggests that a potentially critical facet of intervention for reducing family caregiver burden is to help stroke patients physical functioning and mental wellbeing. This could be in the form of rehabilitation programs not just focusing on caregivers helping stroke patients with specific activities, but helping caregivers understand practices that promote physical autonomy of the patient. As assessed in the Barthel Index (Mahoney and Barthel 1965) representing physical functioning this could be done in ways such as helping the home become more wheelchair accessible and the patient being more wheelchair independent. The helping professional could also discuss with the caregiver and patient ways that the patient can participate in dressing and grooming as to not put the entire responsibility upon the caregiver. Based upon our results, this improved physically functioning, even in small or incremental ways, would be linked with lower rates of caregiver burden. Further, with the link of poorer patient mental health and increased caregiver burden it is recommended that mental health professionals such as CMFTs be included in treatment of stroke patients. This could be in form of the initial rehabilitation intervention or through ongoing treatment post release from a medical setting. This echoes the growing literature and research supporting CMFTs actively engaged within the medical community (Aamar et al. 2015).
Based upon the results indicating that the intervention was not linked with lower caregiver burden, we wonder if future rehabilitation programs should consider even more systemic factors beyond the physical and psychological functioning of the patient. Previous literature has suggested that attending to family caregivers’ psychological needs could be beneficial in reducing burdens they may experience (Anderson et al. 2000). For example, some scholars suggested that an intervention should include educating caregivers about self-efficacy, teaching them how to use social support for their own self-care, and use coping strategies for reducing stress (van den Heuvel et al. 2001). Further, by offering other acceptable and helpful options for practical support and assistance may encourage caregivers to seek outside help such as nurses or other family members when in need rather than solely carrying the responsibility of the patient, a common cultural norm within Chinese culture. Second, duration and intensity of the intervention could also be considered to ensure that appropriate and exhaustive training is offered to the participants. Additionally, previous research has indicated that caregivers have different needs at different moments in the caregiving process with more practical support at the beginning and psychological support later on (Dowswell et al. 2000). It may be helpful for future interventions to address this by offering initial practical and hands on support at the beginning of the caretaking process and then offer follow up services that predominantly focus on psychological and social support later on. This psychological support could be in the form of support groups or psychotherapy which have both been illustrated as effective in reducing caregiver burden (Sörensen et al. 2002). This approach may better fit the time sensitive needs of caretakers and therefore possibly curb increased reports of caregiver burden.
Couple, marriage, and family therapists (CMFT) may be uniquely prepared to assist in development of and contribution to future interventions due to their training and experience in systemic treatment. With CMFTs emphasis on psychological and social well-being by focusing on contextual and systemic factors, they could first offer psychoeducation and basic tools to stroke patients to reduce the possibility of mental health conditions such as depression that are typically linked with poor physical health experiences (Clark and Currie 2009). As suggested in the present study, mental health of the patient may be an important factor to focus on as it is linked with caregiver burden. Further, with previous literature indicating the importance of psychological and social support needed for caregivers initially and especially as time passes (Dowswell et al. 2000), these clinicians could also assist in leading support groups that were comprised of caregivers, individual therapy, or psychoeducational workshops in how to best avoid burnout (Lee et al. 2007). Providing these services may help caregivers feel less isolated, more supported, and learn how to manage their own physical and mental health in such a way that may reduce the burden they feel and improve overall satisfaction with their responsibility. Also, with much of what caregivers experience in rural China being shaped by cultural norms such as the responsibility of care solely falling on the family (Yan et al. 2016), the patient is the priority (Coombs 2007), self-sacrifice (Sit et al. 2004), and not expressing one’s needs (Lui et al. 2000), CMFTs need to be aware of and discuss these contextual factors that may be worsening the burden they are experiencing. For both stroke patient and caregivers, CMFTs could focus on connecting them with practical resources and avenues for support to help break the stigma of carrying the burden alone and not expressing needs they may have (Chen et al. 2010). Lastly, CMFTs can work with other professionals as a medical team to develop interventions to help reduce family caregiver burden.
Limitations and Future Directions
Notwithstanding it’s strengths, the present study carries numerous limitations. First, although the study sample size was sufficient, but a larger sample from other rural communities would have provided greater analytical power and generalizability to more rural Chinese caregivers. Second, examining family caregiver burden was not the main aim of the utilized rehabilitation intervention, but rather an exploratory goal. Future clinical interventions and research could ensure that this is an overt focus of projects in both the development of interventions and the assessment of them. This then could possibly provide interventions better tailored to caregivers’ and their specific needs as well as more rich and nuanced data on its effectiveness. Third, we did not measure the CBI at baseline but only at the 6-month follow up. Therefore, our data did not follow the change process of family caregiver burden over time. Randomized control trials specifically focused on family caregiver burden are needed to test whether this intervention can help reduce burden initially and over time.
Further, other aspects of data tracking related to the intervention were limited such as to what extent the video offered to caregivers was used, the initial mental and physical health of caregivers prior to the intervention, and access as well as use of other relationships and support systems for the caregiver. Finally, self-reported measures were used to create constructs of stroke patient physical functions, mental health conditions, and family caregiver burden, which may not most accurately portray experiences within the system. Future research could incorporate self-report data, professionally assessed medical data, and possibly observational data to most accurately capture experiences within these caregiver and patient settings.
Conclusion
This study found that stroke patient physical functioning and mental health conditions following a stroke were linked with family caregiver burden 6-months later. These findings provide initial insights into risk factors of patient characteristics leading to family caregiver burden and potential mechanisms of intervention for reducing family caregiver burden. Even though our simplified rehabilitation program did not reduce family caregivers burden, it did provide implications for future interventions to consider caregiver burden, mental health of the patient, sensitivity to education levels of caregivers, and intensity as well as duration of the intervention. Based on the risk factors of caregiver burden and the implications of this intervention, future intervention should not only focus on training family caregivers to take care of stroke patients, but a rehabilitation program should also focus on the needs of patients and family caregivers concurrently by providing different dimensional care. Couple, marriage, and family therapists are well suited to offer this additional dimension as their systemic training and experience focus on mental and social well-being of patients and caregivers.
References
Aamar, R., Lamson, A., & Smith, D. (2015). Qualitative trends in psychosocial treatment for underserved patients with type 2 diabetes. Contemporary Family Therapy, 37(1), 33–44. https://doi.org/10.1007/s10591-015-9326-x.
Acock, A. (2005). Working with missing values. Journal of Marriage and Family, 67(4), 1012–1028. https://doi.org/10.1111/j.1741-3737.2005.00191.x.
Anderson, C., Rubenach, S., Mhurchu, C. N., Clark, M., Spencer, C., & Winsor, A. (2000). Home or hospital for stroke rehabilitation? Results of a randomized controlled trial. Stroke, 31(5), 1024–1031. https://doi.org/10.1161/01.STR.31.5.1024.
Aprile, I., Di Stasio, E., Romitelli, F., Lancellotti, S., Caliandro, P., Tonali, P., … Padua, L. (2008). Effects of rehabilitation on quality of life in patients with chronic stroke. Brain Injury, 22, 451–456. https://doi.org/10.1080/02699050802060639.
Bateson, G. (1972). Steps to an ecology of mind. New York: Ballantine.
Berg, A., Palomäki, H., Lönnqvist, J., Lehtihalmes, M., & Kaste, M. (2005). Depression among caregivers of stroke survivors. Stroke, 36, 639–643. https://doi.org/10.1161/01.STR.0000155690.04697.c0.
Bonita, R., Mendis, S., Truelsen, T., Bogousslavsky, J., Toole, J., & Yatsu, F. (2004). The global stroke initiative. The Lancet Neurology, 3, 391–393. https://doi.org/10.1016/S1474-4422(04)00800-2.
Cadilhac, D. A., Dewey, H. M., Vos, T., Carter, R., & Thrift, A. G. (2010). The health loss from ischemic stroke and intracerebral hemorrhage: Evidence from the North East Melbourne stroke incidence study (NEMESIS). Health and Quality of Life Outcomes, 8, 49–56. https://doi.org/10.1186/1477-7525-8-49.
Caro, C. C., Mendes, P. V. B., Costa, J. D., Nock, L. J., & Cruz, D. M. C. D. (2017). Independence and cognition post-stroke and its relationship to burden and quality of life of family caregivers. Topics in Stroke Rehabilitation, 24, 194–199. https://doi.org/10.1080/10749357.2016.1234224.
Chen, Y., Lu, J., Wong, K. S., Mok, V. C., Ungvari, G. S., & Tang, W. K. (2010). Health-related quality of life in the family caregivers of stroke survivors. International Journal of Rehabilitation Research, 33(3), 232–237. https://doi.org/10.1097/MRR.0b013e328338b04b.
Cheung, G., & Chan, C. (2002). The Satir model and cultural sensitivity: A Hong Kong reflection. Contemporary Family Therapy, 24(1), 199–215. https://doi.org/10.1023/A:101433802.
Choi-Kwon, S., Kim, H. S., Kwon, S. U., & Kim, J. S. (2005). Factors affecting the burden on caregivers of stroke survivors in South Korea. Archives of Physical Medicine and Rehabilitation, 86(5), 1043–1048. https://doi.org/10.1016/j.apmr.2004.09.013.
Chou, K. R., Jiann-Chyun, L., & Chu, H. (2002). The reliability and validity of the Chinese version of the caregiver burden inventory. Nursing research, 51(5), 324–331.
Clark, D. M., & Currie, K. C. (2009). Depression, anxiety, and their relationship with chronic diseases: A review of the epidemiology, risk, and treatment evidence. Medical Journal of Australia, 194, s54–s90.
Collins, L. M., Schafer, J. L., & Kam, C. M. (2001). A comparison of inclusive and restrictive strategies in modern missing data procedures. Psychological Methods, 6(4), 330–351. https://doi.org/10.1037/1082-989X.6.4.330.
Coombs, U. E. (2007). Spousal caregiving for stroke survivors. Journal of Neuroscience Nursing, 39(2), 112–119.
Dai, Y. T., Lou, M. F., Yip, P. K., & Huang, G. S. (2000). Risk factors and incidence of postoperative delirium in elderly Chinese patients. Gerontology, 46(1), 28–35. https://doi.org/10.1159/000022130.
Dowswell, G., Lawler, J., & Young, J. (2000). Unpacking the ‘black box’ of a nurse-led stroke support service. Clinical Rehabilitation, 14(2), 160–171. https://doi.org/10.1191/026921500672130349.
Epstein, N. B., Berger, A. T., Fang, J. J., Messina, L. A., Smith, J. R., Lloyd, T. D., … Liu, Q. X. (2012). Applying western-developed family therapy models in China. Journal of Family Psychotherapy, 23(3), 217–237. https://doi.org/10.1080/08975353.2012.705661.
Forbat, L., McManus, E., & Haraldsdottir, E. (2012). Clinical implications for supporting caregivers at the end-of-life: Findings from a qualitative study. Contemporary Family Therapy, 34, 282–292. https://doi.org/10.1007/s10591-012-9194-6.
Greveson, G., & James, O. (1991). Improving long-term outcome after stroke—The views of patients and carers. Health Trends, 23(4), 161–162.
Hu, L., & Bentler, P. M. (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal, 6, 1–55. https://doi.org/10.1080/10705519909540118.
Kalra, L., Evans, A., Perez, I., Melbourn, A., Patel, A., Knapp, M., & Donaldson, N. (2004). Training carers of stroke patients: Randomised controlled trial. BMJ, 328(7448), 1099–1101.
Kline, R. B. (2011). Principles and practice of structural equation modeling (3rd edn.). New York: Guilford.
Langhorne, P., Bernhardt, J., & Kwakkel, G. (2011). Stroke rehabilitation. The Lancet, 377(9778), 1693–1702. https://doi.org/10.1016/S0140-6736(11)60325-5.
Lee, J., Soeken, K., & Picot, S. J. (2007). A meta-analysis of interventions for informal stroke caregivers. Western Journal of Nursing Research, 29(3), 344–356. https://doi.org/10.1177/0193945906296564.
Liu, H., Li, S., Xiao, Q., & Feldman, M. (2014). Social support and psychological well-being under social change in urban and rural China. Social Indicators Research, 119(2), 979–996. https://doi.org/10.1007/s11205-013-0534-1.
Lo, R. S., Cheng, J. O., Wong, E. M., Tang, W. K., Wong, L. K., Woo, J., & Kwok, T. (2008). Handicap and its determinants of change in stroke survivors. Stroke, 39(1), 148–153. https://doi.org/10.1161/STROKEAHA.107.491399.
Lui, M. H., Lee, D. T., & Mackenzie, A. E. (2000). Community care of older Chinese people in Hong Kong: A selective review. Australasian Journal on Ageing, 19(4), 180–184. https://doi.org/10.1111/j.1741-6612.2000.tb00232.x.
Mackenzie, A. E., Holroyd, E. E., & Lui, M. H. (1998). Community nurses’ assessment of the needs of Hong Kong family carers who are looking after stroke patients. International Journal of Nursing Studies, 35(3), 132–140. https://doi.org/10.1016/S0020-7489(98)00008-X.
Mahoney, F. L., & Barthel, D. W. (1965). Functional evaluation: The Barthel index. Maryland State Medical Journal, 14, 61–65.
Mak, A. K., Mackenzie, A., & Lui, M. H. (2007). Changing needs of Chinese family caregivers of stroke survivors. Journal of Clinical Nursing, 16(5), 971–979. https://doi.org/10.1111/j.1365-2702.2006.01754.x.
McCullagh, E., Brigstocke, G., Donaldson, N., & Kalra, L. (2005). Determinants of caregiving burden and quality of life in caregivers of stroke patients. Stroke, 36(10), 2181–2186. https://doi.org/10.1161/01.STR.0000181755.23914.53.
Minuchin, S. (1974). Families and family therapy. Cambridge: Harvard University Press.
Muthén, L. K., & Muthén, B. O. (2012). Mplus 7.0 [Computer software]. Los Angeles: Author.
Novak, M., & Guest, C. (1989). Application of a multidimensional caregiver burden inventory. The Gerontologist, 29(6), 798–803.
Ostwald, S. K., Hepburn, K. W., Caron, W., Burns, T., & Mantell, R. (1999). Reducing caregiver burden: A randomized psychoeducational intervention for caregivers of persons with dementia. The Gerontologist, 39(3), 299–309. https://doi.org/10.1093/geront/39.3.299.
Satir, V. (1983). Conjoint family therapy (3rd edn.). Palo Alto: Science and Behavior Books.
Schulz, K. F., Altman, D. G., & Moher, D. (2010). CONSORT 2010 statement: Updated guidelines for reporting parallel group randomised trials. Journal of Clinical Epidemiology, 63(8), 834–840. https://doi.org/10.1016/j.jclinepi.2010.02.005.
Settineri, S., Rizzo, A., Liotta, M., & Mento, C. (2014). Caregiver’s burden and quality of life: Caring for physical and mental illness. International Journal of Psychological Research, 7(1), 30–39.
Shadish, W. R., Cook, T. D., & Campbell, D. T. (2002). Experimental and quasi-experimental designs for generalized causal inference. Belmont: Wadsworth.
Sit, J. W., Wong, T. K., Clinton, M., Li, L. S., & Fong, Y. M. (2004). Stroke care in the home: The impact of social support on the general health of family caregivers. Journal of Clinical Nursing, 13(7), 816–824. https://doi.org/10.1111/j.1365-2702.2004.00943.x.
Sörensen, S., Pinquart, M., & Duberstein, P. (2002). How effective are interventions with caregivers? An updated meta-analysis. The gerontologist, 42(3), 356–372. https://doi.org/10.1093/geront/42.3.356.
Stata Corporation. (2015). Stata 14 [Computer software]. College Station: Stata Corporation.
Steinmetz, S. K. (1988). Elder abuse by family caregivers: Processes and intervention strategies. Contemporary Family Therapy, 10, 256–271. https://doi.org/10.1007/BF00891617.
Tang, Y. Y., & Chen, S. P. (2002). Health promotion behaviors in Chinese family caregivers of patients with stroke. Health Promotion International, 17(4), 329–339. https://doi.org/10.1093/heapro/17.4.329.
Thommessen, B., Wyller, T. B., Bautz-Holter, E., & Laake, K. (2001). Acute phase predictors of subsequent psychosocial burden in carers of elderly stroke patients. Cerebrovascular Diseases, 11(3), 201–206. https://doi.org/10.1159/000047639.
Toseland, R. W., Rossiter, C. M., Peak, T., & Smith, G. C. (1990). Comparative effectiveness of individual and group interventions to support family caregivers. Social Work, 35(3), 209–217. https://doi.org/10.1093/sw/35.3.209.
van den Heuvel, E. T., Witte, L. P. D., Schure, L. M., Sanderman, R., & Jong, B. M. D. (2001). Risk factors for burn-out in caregivers of stroke patients, and possibilities for intervention. Clinical Rehabilitation, 15(6), 669–677. https://doi.org/10.1191/0269215501cr446oa.
Visser-Meily, A., Post, M., Schepers, V., & Lindeman, E. (2005). Spouses’ quality of life 1 year after stroke: Prediction at the start of clinical rehabilitation. Cerebrovascular Diseases, 20(6), 443–448. https://doi.org/10.1159/000088983.
Wang, W., Jiang, B., Sun, H., Ru, X., Sun, D., Wang, L., … Chen, Z. (2017). Prevalence, incidence, and mortality of stroke in China. Circulation, 135(8), 759–771. https://doi.org/10.1161/CIRCULATIONAHA.116.025250.
World Health Organization. (2017). Global Health Estimates 2015: Deaths by cause, age, sex, by country and by region, 2000–2015. Geneva, Swaziland. Retrieved from http://www.who.int/healthinfo/global_burden_disease/GlobalCOD_method_2000_2015.pdf?ua=1.
Yan, L. L., Chen, S., Zhou, B., Zhang, J., Xie, B., Luo, R.,.. . Shi, J. (2016). A randomized controlled trial on rehabilitation through caregiver-delivered nurse-organized service programs for disabled stroke patients in rural China (the RECOVER trial): Design and rationale. International Journal of Stroke: Official Journal of the International Stroke Society, 11(7), 823–830. https://doi.org/10.1177/1747493016654290.
Zhang, Y. L., Liang, W., Chen, Z. M., Zhang, H. M., Zhang, J. H., Weng, X. Q., … Zhang, Y. L. (2013). Validity and reliability of Patient Health Questionnaire-9 and Patient Health Questionnaire-2 to screen for depression among college students in China. Asia-Pacific Psychiatry, 5(4), 268–275. https://doi.org/10.1111/appy.12103.
Funding
Funding was provided by China Medical Board (Grant No. 13-161), The Amsterdam Health and Technology Institute, The China International Center on Chronic Disease Prevention and Duke University.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical Approval
The study was approved by China Medical University, Ningxia Medical University, and Chongqing Medical University’s ethics committees and was registered at Clinicaltrials.gov (NCT02247921).
Informed Consent
Informed consent was obtained from all participants for being included in the study.
Rights and permissions
About this article
Cite this article
Peng, Y., Brown, C.C., Zhang, J. et al. An Examination of a Simplified Stroke Rehabilitation Program for Reducing Family Caregiver’s Burden for Stroke Patients in Rural China. Contemp Fam Ther 41, 168–179 (2019). https://doi.org/10.1007/s10591-018-9482-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10591-018-9482-x