Abstract
Dependence of stroke survivors regarding the ability to perform activities of daily living imposes a burden on family caregivers. The study evaluated the effect of the family-centered empowerment program on the ability of Iranian patients with stroke to perform activities of daily living, as well as on family caregiver burden. In this randomized controlled trial study, a total of 90 pairs of patients with stroke and their family caregivers was selected and randomly assigned to the intervention or control groups. Patients and their family caregivers participated in four family-centered empowerment program sessions over four consecutive days while the patient was hospitalized. The difference in the ability of patients with stroke in the intervention and control groups to perform activities of daily living was not significant 2 weeks after the intervention. However, the ability of patients with stroke in the intervention group to perform activities of daily living increased significantly 2 months after the intervention compared with the control group: 66 ± 35.95 and 51.31 ± 36.28, respectively (p = 0.047). Two weeks after the intervention, the family caregiver burden significantly decreased in the intervention group (29.55 ± 15.38) compared with the control group (38.77 ± 18.53 and p = 0.012). The burden in the intervention group also decreased 2 months after the intervention compared with the control group: 22.95 ± 15.68 and 36.11 ± 18.88, respectively (p < 0.001). Nurses can use the family-centered empowerment program to improve the quality of life of patients with stroke, and to reduce the burden of family caregivers.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Stroke is a leading cause of death and the major cause of disability and dependency in activity of daily living worldwide around the world [1]. The incidence of this disease in Iran was much higher in comparison to Western countries and often happened earlier ages. In Iran, this value has been reported 139 per 100,000 people [2].
Despite having disabilities, most patients return home immediately after discharge, and are cared for by family members [3]. A large number of patients with post-stroke depend on their family members to provide care and help with their activities of daily living (ADLs) [4]. The dependence of patients with stroke on family members imposes a burden on the family and is associated with many problems [5]. According to previous studies, 25–54% of caregivers reported the experience of care burden in the first 6 months after stroke [6].
It is necessary to improve the ability of patients with stroke to perform ADLs and to find ways to reduce the family caregiver burden (FCB). Given that in Iran, families play an important role for the provision of care to patients and their family care givers, and family caregivers take the caring role, their empowering is essential. On the other hand, Iranian nurses are in unique opportunity to interact and empower patient and their family [7]. In this regard, the present study aimed to determine the effect of family-centered empowerment program (FCEP) on the ability of Iranian patients with stroke to perform ADLs and on the FCB.
Family-centered empowerment model
Family-centered empowerment provides opportunities for family caregivers to acquire knowledge and skills so that they can manage family life optimally and, consequently, enhance the lifestyles and quality of life of all family members [8]. Alhani [9] developed a family-centered empowerment model (FCEM) for chronic disease at the Tarbiat Modares University in Tehran, Iran (Fig. 1). This model was developed through qualitative research and using a meta-analysis after coding, the formation and development of concepts, identification of the psychosocial process and the emergence of the central concept (family-centered empowerment) as a native practical model. In the second stage, the model test was conducted using a quantitative semi-experimental research for the first time in Iran [9]. The model consists of four stages: (1) determining perceived threat through discussion method; (2) self-efficacy via problem-solving method; (3) improving self-esteem through educational participation method and (4) process and outcome evaluations [10].
Family-centered empowerment and activities of daily living
ADLs are daily activities that individuals do to maintain their own well-being, including eating and drinking, moving, going to the toilet, personal hygiene, dressing, and taking care of the body [11]. Long-term follow-up studies have shown that stroke has a long-term effect on ADLs even after many years of the incidence [12]. Patients with post-stroke often suffer from disabilities that influence their daily life and make them dependent on others [13]. The role of family caregiver as one part of a supportive system for improving the quality of life of patients after stroke is highlighted. Family caregivers are the spouse, child or close friend who provide care to a person in need of help [14].
Family caregivers need to be knowledgeable and empowered about ADLs, mobility, rehabilitation, and problem-solving, as well as understand how to prevent complications associated with severe disability [15]. However, family caregivers often feel that they are weakly informed and not well educated, and are dissatisfied with the type and quality of available emotional and technical support given to them [16]. Therefore, the first hypothesis of this study is as follows:
H1: the FCEP is effective in improving the ability of patients with stroke to perform ADLs.
Family-centered empowerment and caregiver burden
Providing continuous care for a patient with stroke has psychological and emotional consequences to family members [17]. Caregivers under high burden were easy to get health physical and mental problems and a decrease of quality of life. Caregiver burden is defined as the emotional and physical response of caregivers to changes and demands of the provision of care to patients with physical and mental problems [6]. In the literature, even though evidence is available regarding care strain and reduction of care burden, little attention has been paid to the reduction of the outcome of care burden among the survivors of stroke [1].
Caregivers might experience many problems if they undertake the caregiving role without any plan after a stroke and lack caregiving information and skills [5]. Therefore, there is a need to change the focus of rehabilitation of stroke from patient-centered to caregiver-centered [1]. Studies in Iran have not focused on care burden in family caregivers of patients with stroke [18]. Since FCEM aims at enhancing family health and patient health [19], the second hypothesis of the study is as follows:
H2: the FCEP is effective in reducing the FCB.
Literature review
A few studies have been conducted on the effect of empowerment of family caregivers on their burden and the daily living activities of patients with stroke. Hekmatpou et al. studied the effect of patient care education on care and the quality of life of family caregivers in patients with stroke [2]. However, various studies about the impact of FCEM on different groups have been performed in Iran. Hakime et al. investigated the effect of FCEM on the level of parents’ knowledge of children with ostomy [20]. Vahedian-Azimi et al. assessed the effect of FCEM on the quality of life in patients with myocardial infarction [21]. Teymouri et al. examined the effect of FCEM on the quality of life of parents with asthmatic children [22]. The other study investigated the effect of FCEM on the self-efficacy and self-esteem of patients undergoing coronary artery bypass grafting surgery [23]. However, despite the high prevalence of stroke in Iran, no study has been conducted similar to the aim of the present study.
Methods
Participants
This randomized controlled trial was conducted from February 2017 to April 2018. Participants was selected in the neurology wards of three referral educational hospitals affiliated with XXX (university name) in XXX (city name), Iran. The sample size was calculated as follows:
the value of the variance (σ) of the FCB was determined to be 15 on the basis of a study by Azimi et al. [24].
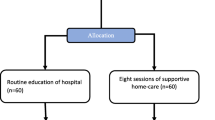
Each participant was randomly assigned to either the intervention group or the control group using a coin tossed by the first researcher. Because there were sample dropouts, sampling continued until the desired number for each group was achieved. For example, if the coin toss indicated that a participant should enter a group that had met the required sample size, the person would not be enrolled in the study. The coin toss would continue until a person was assigned to the group that required more participants. This process continued until the required number of participants was reached in each group.
A total of 118 pairs, or dyads, of patients and their family caregivers were enrolled in the study. Initially, there were 58 dyads in the intervention group; however, during the study, 13 dyads left the group (dropout rate of 22%). There were 60 dyads initially in the control group, although 15 dyads left the group (dropout rate of 25%). A total of 24 dyads from both groups were excluded because of death, stroke, and rehospitalization, while 4 dyads were excluded because of a lack of adequate participation. Finally, the study was conducted with 45 dyads in each of the two groups. To prevent contamination of the participants in the intervention group, after each participant was assigned to the appropriate group, the next participant was not selected until the previous patient had been discharged. The inclusion and exclusion criteria are presented in Table 1. Details of the study stages and changes in the number of participants are shown in Fig. 2.
The mean age of the family caregivers in the intervention and control groups was 41.1 years ± 11 years and 40.6 years ± 11.7 years, respectively; the mean age of the patients in the intervention and control groups was 67.2 years ± 12.0 years and 66.8 years ± 11.1 years, respectively. According to the independent t test, there was no significant difference between the groups: p = 0.841 and p = 0.863, respectively (Table 2). The mean number of hospitalization days was 8.67 days ± 2.95 days and 9.67 days ± 5.01 days in the intervention and control groups, respectively, which was not significant between the groups (p = 0.639). Other demographic and clinical characteristics of patients with stroke and their family caregivers are shown in Tables 3 and 4, respectively.
Measures
The modified Rankin Scale, which was originally developed by Dr. Rankin in 1957, was used to measure the severity of disability in patients with stroke in the intervention and control groups [25]. Using the Rankin scale, the degree of the severity of disability was categorized as follows: 0 for no abnormal neurological symptoms; Grade 1 for no significant disability, able to carry out all usual duties; Grade 2 for a slight disability in which the patient is not able to perform all previous activities, but is able to take care of themselves without assistance; Grade 3 for a moderate disability in which the patient needs some help from others, but can walk without help; Grade 4 for a moderate-to-severe disability in which the patient is not able to walk without the help of others and the patient requires assistance with ADLs; and Grade 5 for a severe disability in which the patient is bedridden and requires constant care [26]. Patients with Grades 3, 4, or 5 degree of disability, as determined by the researcher, were included in the study. A literature review conducted on studies that used the modified Rankin scale confirmed the construct and convergent validities, as well as the test–retest reliability (0.81–0.95) [25]. In the present study, the reliability of the modified Rankin scale was assessed in a pilot study that involved 20 patients with stroke; Cronbach’s alpha was calculated to be 0.92.
The data collection tools were a demographic and clinical information questionnaire for patients and family caregivers, the caregiver burden inventory (CBI), and the Barthel index (BI). The demographic and clinical information questionnaire for patients and family caregivers included 15 questions: seven items for the family caregivers and eight items for the patients. The CBI contained 24 items with five subscales: time dependence burden (items 1–5), developmental burden (items 6–10), physical burden (items 11–14), emotional burden (items 15–19), and social burden (items 20–24). The responses of the caregivers were scored using a five-point Likert scale that ranged from never (0) to almost always (5) [27]. Novak and Guest evaluated the construct validity of the CBI for patients with cerebrovascular abnormalities [28]. One study determined the psychometric properties of the tool for an Iranian dialysis patient and obtained a Cronbach’s alpha of 0.9 [29]. For the present study, the reliability of the CBI was determined in a pilot study that involved 20 family caregivers; Cronbach’s alpha was 0.91, which verified the reliability of the instrument.
The BI is the most commonly used tool to assess the ability of a patient to perform ADLs. In this study, the BI was used to examine 10 activities and the total score ranged from 0 to 100 indicating the self-sufficiency in performing ADLs and determining the level of need and dependency of the patient. The scores for different items are as follows: the personal hygiene and bathing 0, 1, 3, 4, and 5; the feeding, toileting, stair climbing, dressing, bowel control and bladder control 0, 2, 5, 8, and 10; and the bed to chair transfer and ambulation 0, 3, 8, 12, 15. The score of each item is maximum if the activity is normal and minimum if there is no activity [30]. The original BI was developed by Mahoney and Barthel (1965). The psychometric properties of the original BI were assessed in patients with stroke [31]. The validity of the Iranian version was confirmed in a study on a group of patients with stroke that determined that the test–retest reliability was 0.989 [32]. For the present study, the Cronbach’s alpha for the BI was 0.91 according to the pilot study, which involved 20 patients with stroke.
Intervention
The FCEP was implemented for family caregivers and patients in the intervention group in 1-h sessions for four consecutive days during hospitalization of the patient. The intervention was led by the first researcher and held in the ward classroom on the ward. The first three steps were implemented as shown in Table 2. The fourth step was implemented during the data collection stage and involved evaluating the effect of the FCEP on the ability of patients with stroke to perform ADLs and on the FCB.
Procedure
Data collection involved the family caregivers completing questionnaires at three stages: before the intervention, after 2 weeks in the neurology wards of hospitals, and 2 months after the intervention in their homes and returned it by mail. To ensure the continuity of the subjects’ participation in the study and completion of the questionnaires up to the last stage, the intervention and control groups were conducted phone counseling weekly via their family caregivers and their questions would be answered.
Data analysis
The descriptive statistics were the mean and standard deviation for the description of demographic data in the intervention and control groups. The Chi-squared test, the Mann–Whitney U test, and Fisher’s exact test were used to assess differences between the participants including patients and family caregivers in terms demographic characteristics between the intervention and control groups. The normality of data was evaluated using The Kolmogorov–Smirnov test. The intergroup differences in terms of the ability of patients with stroke to perform ADLs and the FCB in the intervention and control groups at three stages were assessed using the repeated measures ANOVA test. The t test helped to intragroup comparisons in terms of the ability of patients with stroke to perform ADLs and FCB on different stages of the study as a post hoc analysis. The findings were considered significant at p < 0.05.
Ethical considerations
Data collection was carried out after an introduction letter was presented to the authorities of the selected hospitals and explanations about the study objectives and method were given to the head nurses and nurses on the neurology wards. The study objectives and method were also explained to the participants. Participants were ensured of the confidentiality of their names and information. The participants were also informed that their participation in the study was voluntary and that they could leave the study at any time. Written informed consent was obtained from all participants. In addition, at the end of the data collection, the control group received information about how to care for patients with stroke.
Results
The result of the statistical tests confirmed that there were no differences between the participants of the two groups in terms of the following demographic characteristics: sex, education, marital status, occupation, relationship to the patient, chronic disease, and degree of disability.
The Kolmogorov–Smirnov test indicated that the data were normal. Table 5 shows the changes in the ability of patients with stroke to perform ADLs in both the intervention and control groups at different stages. The results of the repeated measures ANOVA showed that there was a significant change in the ability to perform ADLs in both groups at different stages of the study (p < 0.001). This difference could be attributed to the treatment and recovery process of the patients, rather than to the FCEP. However, the results of the t test showed a significant difference between the groups 2 months after the intervention (p < 0.047). In general, the FCEP increased the ability of patients with stroke to perform ADLs 2 months after the intervention.
Table 6 shows the changes in the level of FCB in both groups at different stages. The repeated measures ANOVA showed that there was a significant change in the FCB in the intervention and control groups at different stages: p < 0.001 and p = 0.008, respectively. The results of the t test also showed that there was a significant difference between the groups 2 weeks and 2 months after the intervention: p = 0.012 and p = 0.001, respectively. Based on the results of the statistical analyses, the FCEP reduced the level of FCB 2 weeks and 2 months after the intervention.
Discussion
The findings of this study confirmed the first hypothesis of the research and showed that the FCEP was effective in improving the ability of patients with stroke to perform ADLs. These findings were consistent with the results of other studies. For example, one study showed that the FCEP is effective in the adherence of patients with stroke to their treatment regimens [33]. Teo and Chen found that home-based motor rehabilitation exercises had a positive impact in improving functional outcome of stroke patients in the ability to perform ADLs and patients and caregivers were empowered to continue rehabilitation at home [34]. Wang et al. also revealed that a caregiver-mediated home-based intervention can improve the physical performance and ability to perform ADLs of patients with chronic stroke [35]. Although the results of the present study were consistent with many studies, Bertilsson et al. demonstrated that patient-centered educational interventions did not significantly increase the ability of patients with stroke to perform ADLs [36]. The difference in the results may be attributed to the inadequate impact that patient-centered interventions have in patients with stroke; the patients may not respond properly to educational interventions because of their characteristics and condition. In that study, the mean age of the patients with stroke was 74 years and one-quarter of them suffered from moderate to severe stroke. Also, 44% of them were dependent on their family caregivers for ADLs. Perhaps the same effect on the ineffectiveness of patient-centered educational interventions can influence the ability of patients with stroke to perform ADLs. However, the intervention in the present study was focused on family caregivers who had a good physical and mental status and were thus able to transfer the knowledge they learned during the FCEP to the patients.
The second hypothesis was also confirmed by the research findings of this study: the FCEP was shown to be effective in reducing the FCB. These findings were consistent with the results of other studies. For example, one study found that the FCEP improved the satisfaction and quality of life in caregivers of patients with multiple sclerosis [37]. Another study showed that providing telephone support and training to caregivers of patients with stroke reduced their burden [38]. Vloothuis et al. demonstrated that early discharge with e-health support and caregiver-mediated exercises for patients with stroke reduced stress and burden [39]. Graf et al. showed that providing training, education, and support over the phone and internet was effective in reducing the burden and symptoms of depression in family caregivers of patients with stroke [40].
In contrast to the results of the present study, Forster et al. assessed the effectiveness of a training program provided to caregivers of patients with stroke and concluded that there was no significant difference between the intervention and control groups regarding the reduction of FCB [41]. The contradicting results may be attributed to the lack of post-discharge follow-up programs and the ineffectiveness of purely educational interventions for patients with stroke. In the present study, after the FCEP was completed and the patient was discharged from hospital, phone counseling and follow-ups were provided to the family caregiver, which is a strong point and should not be ignored since they may play a role in the success of the intervention. The support of patients and their caregivers should begin with hospitalization and continue to the patient’s home or a nursing home [42].
This study is worthwhile for several reasons. First, this research was conducted as a randomized controlled trial and had a high level of evidence [43]. In addition, the results verified the role that family caregivers play in the quality of life of patients and showed that the FCB should be considered a major community health issue [44]. During the course of this study, family caregivers and patients with stroke were followed up concurrently from admission to discharge to home. The study also showed that various interventional strategies, such as face-to-face training, problem-solving, and collaborative learning, can be used to empower both the patient and family caregivers.
Practical implications
Based on the results of this study, the FCEP seems to be an appropriate model in helping patients with stroke and their family caregivers improve their quality of life, self-efficiency, and self-esteem. Because the model has a simple, understandable, and inexpensive design, it can be implemented by nurses and nursing managers, nursing education planners, and other healthcare providers to empower family caregivers, reduce the FCB, and improve the ADLs and quality of life of patients with stroke.
Limitations and future research directions
One of the limitations of the study was the high level of anxiety of the family caregivers. This anxiety was related to the fear of possible death of the patient or level of disability while in hospital, which somewhat reduced their focus on learning the educational topics. Another limitation of the study was the need for follow-up and phone counseling with family caregivers in order to verify and ensure their continued presence until the last stage of data collection, which could affect the data collection at the final stage of data collection. Further studies are necessary to investigate the impact of the FCEP on other healthcare groups, as well as on other aspects of care to determine its strengths, weaknesses, and scope of application. Although the present study was conducted in Iran on the family caregivers of patients with stroke, the authors believe that the results can be generalized to other healthcare areas and other countries.
References
Gbiri CA, Olawale OA, Isaac SO (2015) Stroke management: informal caregivers’ burdens and strains of caring for stroke survivors. Ann Phys Rehabil Med 58:98–103. https://doi.org/10.1016/j.rehab.2014.09.017
Hekmatpou D, Baghban EM, Dehkordi LM (2019) The effect of patient care education on burden of care and the quality of life of caregivers of stroke patients. J Multidiscip Healthc 12:211. https://doi.org/10.2147/JMDH.S196903
Jaracz K, Grabowska-Fudala B, Górna K et al (2014) Caregiving burden and its determinants in Polish caregivers of stroke survivors. Arch Med Sci 10:941. https://doi.org/10.5114/aoms.2014.46214
Caro CC, Mendes PVB, Costa JD et al (2017) Independence and cognition post-stroke and its relationship to burden and quality of life of family caregivers. Top Stroke Rehabil 24:194–199. https://doi.org/10.1080/10749357.2016.1234224
Yilmaz CK, Aşiret GD, Çetinkaya F et al (2019) Effect of progressive muscle relaxation on the caregiver burden and level of depression among caregivers of older patients with a stroke: a randomized controlled trial. Jpn J Nurs Sci 16:202–211. https://doi.org/10.1111/jjns.12234
Zhu W, Jiang YA (2018) Meta-analytic study of predictors for informal caregiver burden in patients with stroke. J Stroke Cerebrovasc Dis 27:3636–3646. https://doi.org/10.1016/j.jstrokecerebrovasdis.2018.08.037
Etemadifar S, Heidari M, Jivad N et al (2018) Effects of family-centered empowerment intervention on stress, anxiety, and depression among family caregivers of patients with epilepsy. Epilepsy Behav 88:106–112. https://doi.org/10.1016/j.yebeh.2018.08.030
Minooei MS, Ghazavi Z, Abdeyazdan Z et al (2016) The effect of the family empowerment model on quality of life in children with chronic renal failure: children’s and parents’ views. Nephrourol Mon. https://doi.org/10.5812/numonthly.36854
Alhani F (2003) Evaluating of family-centered empowerment model on preventing Iron deficiency anemia. Tehran, Iran. (Persian): PhD Dissertation, Tarbiat Modares University
Vahedian-Azimi A, Miller AC, Hajiesmaieli M et al (2016) Cardiac rehabilitation using the family-centered empowerment model versus home-based cardiac rehabilitation in patients with myocardial infarction: a randomised controlled trial. Open Heart 3:e000349. https://doi.org/10.1136/openhrt-2015-000349
Legg LA, Lewis SR, Schofield-Robinson OJ et al (2019) Occupational therapy for adults with problems in activities of daily living after stroke. Cochrane Database Syst Rev 7:CD003585. https://doi.org/10.1002/14651858.CD003585.pub3
Blomgren C, Samuelsson H, Blomstrand C et al (2019) Long-term performance of instrumental activities of daily living in young and middle-aged stroke survivors—impact of cognitive dysfunction, emotional problems and fatigue. PLoS One 14:e0216822. https://doi.org/10.1371/journal.pone.0216822
Rejnö Å, Nasic S, Bjälkefur K et al (2019) Changes in functional outcome over 5 years after stroke. Brain Behav 9:e01300. https://doi.org/10.1002/brb3.1300
Ogunlana MO, Dada OO, Oyewo OS et al (2014) Quality of life and burden of informal caregivers of stroke survivors. Hong Kong Physiother J 32:6–12. https://doi.org/10.1016/j.hkpj.2013.11.003
Pitthayapong S, Thiangtam W, Powwattana A et al (2017) A community based program for family caregivers for post stroke survivors in Thailand. Asian Nurs Res 11:150–157. https://doi.org/10.1016/j.anr.2017.05.009
Araújo O, Lage I, Cabrita J et al (2015) Intervention in informal caregivers who take care of older people after a stroke (InCARE): study protocol for a randomised trial. J Adv Nurs 71:2435–2443. https://doi.org/10.1111/jan.12697
Ganapathy V, Graham GD, DiBonaventura MD et al (2015) Caregiver burden, productivity loss, and indirect costs associated with caring for patients with poststroke spasticity. Clin Interv Aging 10:1793. https://doi.org/10.2147/CIA.S91123
Masoudian N, Sarmadi M, Najafi R et al (2019) Burden of care and quality of life in home caregivers of patients with stroke in Iran. Home Health Care Manag Pract 12:211–217. https://doi.org/10.1177/1084822319843137
Vahedian-Azimi A, Miller AC, Hajiesmaieli M et al (2016) Cardiac rehabilitation using the family-centered empowerment model versus home-based cardiac rehabilitation in patients with myocardial infarction: a randomized controlled trial. Open Heart 3:e000349. https://doi.org/10.1136/openhrt-2015-000349
Hakim A, Palizban E, Ahmadi Angali K (2015) The effect of family-centered empowerment model on the level of parents’ knowledge of children with ostomy. J Pediatr Nurs 1:22–31 (in Persian)
Vahedian-Azimi A, Alhani F, Goharimogaddam K et al (2015) Effect of family-centered empowerment model on the quality of life in patients with myocardial infarction: a clinical trial study. J Nurs Educ 4:8–22 (in Persian)
Teymouri F, Alhani F, Kazemnejad A (2014) The effect of the family-centered empowerment model on the quality of life in parents of children with asthma. Vicenna J Nurs Midwifery Care 22:5–14 (in Persian)
Sanaie N, Nejati S, Zolfaghari M et al (2013) The effect of family-centered empowerment in self efficacy and self-esteem in patients undergoing coronary bypass graft surgery. J Res Dev Nurs Midwifery 10:44–53 (in Persian)
Azimi R, Mohammadi F, Hosseini M et al (2013) The effect of home-based stroke rehabilitation on quality of life of stroke survivors and their family caregiver’s strain. Evid Based Care 3:77–85. https://doi.org/10.22038/EBCJ.2013.729
Banks JL, Marotta CA (2007) Outcomes validity and reliability of the modified Rankin scale: implications for stroke clinical trials: a literature review and synthesis. Stroke 38:1091–1096. https://doi.org/10.1161/01.STR.0000258355.23810.c6
Quinn T, Dawson J, Walters M (2008) Dr John Rankin; his life, legacy and the 50th anniversary of the Rankin stroke scale. Scott Med J 53:44–47. https://doi.org/10.1258/RSMSMJ.53.1.44
Greco A, Pancani L, Sala M et al (2017) Psychometric characteristics of the caregiver burden inventory in caregivers of adults with heart failure. Eur J Cardiovasc Nurs 16:502–510. https://doi.org/10.1177/1474515117693890
Novak M, Guest C (1989) Application of a multidimensional caregiver burden inventory. Gerontologist 29:798–803
Abbasi A, Asayesh H, Rahmani H et al (2011) The burden on caregivers from hemodialysis patients and related factors. J Res Dev Nurs Midwifery 8:26–33 (in Persian)
Quinn TJ, Langhorne P, Stott DJ (2011) Barthel index for stroke trials: development, properties, and application. Stroke 42:1146–1151. https://doi.org/10.1161/STROKEAHA.110.598540
Duffy L, Gajree S, Langhorne P et al (2013) Reliability (inter-rater agreement) of the Barthel index for assessment of stroke survivors: systematic review and meta-analysis. Stroke 44:462–468. https://doi.org/10.1161/STROKEAHA.112.678615
Oveisgharan S, Shirani S, Ghorbani A et al (2006) Barthel index in a Middle-East country: translation, validity and reliability. Cerebrovasc Dis 22:350–354. https://doi.org/10.1159/000094850
Dehghan nayeri N, Mohammadi S, Pedram razi S et al (2015) Effectiveness of family empowerment program on level of adherence to treatment regimens in stroke patients; a randomized controlled trial. Evid Based Care 5:57–66. https://doi.org/10.22038/EBCJ.2015.4072
Teo SH, Chen Z (2016) Effectiveness of an activity-based home therapy program for stroke patients in Singapore. Arch Phys Med Rehabil 97:e15. https://doi.org/10.1016/j.apmr.2016.09.039
Wang T-C, Tsai AC, Wang J-Y et al (2015) Caregiver-mediated intervention can improve physical functional recovery of patients with chronic stroke: a randomized controlled trial. Neurorehabilitation Neural Repair 29:3–12. https://doi.org/10.1177/1545968314532030
Bertilsson A-S, Eriksson G, Ekstam L et al (2016) A cluster randomized controlled trial of a client-cantered, activities of daily living intervention for people with stroke: 1 year follow-up of caregivers. Clin Rehabil 30:765–775. https://doi.org/10.1177/0269215515603780
Masoodi R, Soleimani MA, Alhani F et al (2013) Effects of family-centered empowerment model on perceived satisfaction and self-concept of multiple sclerosis patients care givers. Koomesh 14:240–248 (in Persian)
Araújo O, Lage I, Cabrita J et al (2016) Telephone assistance to decrease burden in informal caregivers of stroke older people: monitoring and diagnostic evaluation. BMC Health Serv Res 16:92
Vloothuis J, Mulder M, Nijland RH et al (2015) Caregiver-mediated exercises with e-health support for early supported discharge after stroke (CARE4STROKE): study protocol for a randomized controlled trial. BMC Neurol 15:193. https://doi.org/10.1186/s12883-015-0440-z
Graf R, LeLaurin J, Schmitzberger M et al (2017) The stroke caregiving trajectory in relation to caregiver depressive symptoms, burden, and intervention outcomes. Top Stroke Rehabil 24:488–495. https://doi.org/10.1080/10749357.2017.1338371
Forster A, Dickerson J, Young J et al (2013) A cluster randomized controlled trial and economic evaluation of a structured training programme for caregivers of inpatients after stroke: the TRACS trial. Health Technol Assess 17:1. https://doi.org/10.3310/hta17460
Cameron JI, O’Connell C, Foley N et al (2016) Canadian stroke best practice recommendations: managing transitions of care following stroke, guidelines update 2016. Int J Stroke 11:807–822. https://doi.org/10.1177/1747493016660102
Grove SK, Burns N, Gray J (2014) Understanding nursing research: building an evidence-based practice. Elsevier, Amsterdam
Ashghali Farahani M, Ghane G, Sydfatemi N et al (2016) Effect of educational program on the burden of family caregivers of hemodialysis patients. Evid Based Care 6:7–18. https://doi.org/10.22038/EBCJ.2016.6703
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Statement of human and animal rights
All procedures performed within this study were in accordance with the ethical standards of the institutional research ethics committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Deyhoul, N., Vasli, P., Rohani, C. et al. The effect of family-centered empowerment program on the family caregiver burden and the activities of daily living of Iranian patients with stroke: a randomized controlled trial study. Aging Clin Exp Res 32, 1343–1352 (2020). https://doi.org/10.1007/s40520-019-01321-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-019-01321-4