Abstract
Background
Dapagliflozin, a sodium-glucose cotransporter 2 (SGLT2) inhibitor, is approved for the treatment of type 2 diabetes, heart failure, and chronic kidney disease. DAPA-HF and DELIVER trial results demonstrate that the cardiovascular protective effect of dapagliflozin extends to non-diabetic patients. Hence, the mechanism-of-action may extend beyond glucose-lowering and is not completely elucidated. We have previously shown that dapagliflozin reduces cardiac hypertrophy, inflammation, fibrosis, and apoptosis and increases ejection fraction in BTBR mice with type 2 diabetes.
Methods
We conducted a follow-up RNA-sequencing study on the heart tissue of these animals and performed differential expression and Ingenuity Pathway analysis. Selected markers were confirmed by RT-PCR and Western blot.
Results
SGLT2 had negligible expression in heart tissue. Dapagliflozin improved cardiac metabolism by decreasing glycolysis and pyruvate utilization enzymes, induced antioxidant enzymes, and decreased expression of hypoxia markers. Expression of inflammation, apoptosis, and hypertrophy pathways was decreased. These observations corresponded to the effects of dapagliflozin in the clinical trials.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Dapagliflozin was initially developed as an anti-diabetic drug but has shown additional benefits for reduction of cardiovascular and renal event risk and is currently indicated in type 2 diabetes, heart failure, and chronic kidney disease patients (https://www.accessdata.fda.gov/drugsatfda_docs/label/2023/202293s026lbl.pdf). Dapagliflozin reduces hospitalizations for heart failure, improves quality of life, and reduces the risk of cardiovascular death in heart failure patients [1]. The cardiovascular benefits of dapagliflozin are not solely explained by glucose-lowering action alone because other anti-diabetic drugs do not impact or even deteriorate cardiovascular outcomes [2]. Furthermore, dapagliflozin reduces the risk of cardiovascular death or worsening of heart failure in non-diabetic subjects with heart failure with reduced ejection fraction [3]. Similarly, cardiovascular risk reduction with dapagliflozin was observed in both non-diabetic and diabetic participants with heart failure and preserved or mildly reduced ejection fraction in The Dapagliflozin Evaluation to Improve the Lives of Patients with Preserved Ejection Fraction Heart Failure (DELIVER) trial [4].
Obtaining repeated cardiac biopsies before and after treatment with dapagliflozin for research purposes is not justified due to biopsy-associated health risks. Therefore, animal models provide a reasonable alternative to investigate the mechanism of action. Consistent with the clinical findings, dapagliflozin has shown systemic glucose-lowering and hemodynamic and local cardioprotective effects in heart tissue in both diabetic and non-diabetic rodent models. Dapagliflozin improves echocardiography parameters and decreases total O-GlcNAcylated protein in the hearts of diabetic and lypodystrophic Bscl2-/- knockout mice [5]. Dapagliflozin decreases cardiac inflammation and fibrosis and inhibits the production of reactive oxygen species and calcium entry in isolated cardiomyocytes in db/db mice with angiotensin II-induced cardiomyopathy [6]. Decrease in systolic and diastolic blood pressure, serum TNFα, oxidative stress biomarker malonaldehyde, decreased DNA fragmentation (cell death), and increased cardiac contractility have been observed in dapagliflozin-treated compared to untreated rats with streptozotocin-induced diabetes receiving high-fat diet [7]. Dapagliflozin increases left ventricular developed pressure almost back to healthy control animal level and reduces oxidative stress in Wistar rats with metabolic syndrome [8]. Dapagliflozin inhibits phosphorylation of JNK and p38, reduces apoptosis, heart hypertrophy, interstitial fibrosis, and perivascular fibrosis in transverse aortic constriction-induced pressure overload in a non-diabetic mouse model of cardiac hypertrophy [9].
Our group has previously investigated the effects of dapagliflozin on heart physiology in BTBR mice with diabetic cardiomyopathy [10, 11]. To gain a deeper understanding of the mechanism behind the cardioprotective effects of dapagliflozin, we conducted a follow-up RNA-sequencing study on heart tissue samples from the dapagliflozin-treated and untreated BTBR mice from this animal cohort [11].
Methods
Animals
BTBR mice were housed and treated as previously described [11]. The study was approved by the Institutional Animal Care and Use Committee of the University of Texas Medical Branch. In brief, BTBR mice at 8 weeks of age were allocated to two different treatment groups with 4 mice per group: (1) control (no treatment, as drinking water and regular rodent chow); (2) dapagliflozin; dapagliflozin was mixed in drinking water to provide a daily dose of 1.5 mg/kg body weight for 12 weeks based on an observed daily water intake of about 10 ml/day.
RNA-Sequencing
After final termination at 20 weeks of age, heart tissues from four dapagliflozin-treated and four control BTBR mice were homogenized in 1 ml of Trizol Reagent per 50–100 mg of tissue using a power homogenizer. The sample volume did not exceed 10% of the volume of reagent used for homogenization. Total RNA was isolated and purified using a QIAGEN RNA preparation kit and sent to the UTMB’s Next Generation Sequencing (NGS) Core Laboratory. The core laboratory utilized an Illumina HiSeq 1500 sequencing system to perform RNA-sequencing analysis. Reads were aligned to the mouse mm10 reference genome assembly using STAR version 2.5.4b [12]. Gene expression was quantified using STAR [12]. All samples passed technical quality control.
qRT-PCR
Total RNA from the heart tissue was extracted using TRIzol reagent (Invitrogen, Carlsbad, CA, USA) per the manufacturer’s instruction. A total of 2 μg RNA from each sample was reverse-transcribed into cDNA, and equal amounts of the reverse transcriptional products were subjected to PCR amplification. For the quantification of mRNA expressions, specific primers were used (Table 1). Primer sequences were checked against the mouse GRCm39 genome assembly with UCSC In-Silico PCR service (https://genome.ucsc.edu/cgi-bin/hgPcr). The Ct (threshold cycle) is defined as the number of cycles required for the fluorescence signal to exceed the detection threshold. Expression of the gene relative to GAPDH was calculated as the difference between the threshold values of these two genes (2-Δct). Melting curve analysis was performed during real-time PCR to analyze and verify the specificity of the reaction. Each sample was analyzed in triplicate and normalized by GAPDH. We verified the lack of change in the mRNA expression of GAPDH in the RNA-sequencing experiment. The values were given as the means and individual animal measurements.
Immunoblotting
Samples were homogenized in lysis buffer (in mM): 25 Tris·HCl (pH 7.4), 0.5 EDTA, 0.5 EGTA, 1 phenylmethylsulphonyl fluoride, 1 dithiothreitol, 25 NaF, 1 Na3VO4, 1% Triton X-100, 2% SDS, and 1% protease inhibitor cocktail. The lysate was centrifuged at 10,000×g for 15 min at 4°C, and the supernatants were collected. Protein concentration was determined by the Bradford method. Protein (50 μg) was fractionated by SDS-PAGE (4–20% polyacrylamide gels) and transferred to PVDF membranes (Millipore, Bedford, MA, USA). After blocking, membranes were incubated with the primary antibodies overnight at 4°C. The membranes were then washed and incubated with secondary HRP-conjugated antibodies for 1 h at room temperature. Bound antibodies were detected using the chemiluminescent substrate (NEN Life Science Products, Boston, MA, USA). The protein signals were quantified with an image-scanning densitometer, and the strength of each protein signal was normalized to the corresponding β-actin signal. Data were expressed as percent relative to the expression in the control group (BTBR mice without treatment). Anti-Cd74, anti-Gpx1, anti-Sod3, anti-Vegfa, anti-Hif1α, and anti-Smad3&7 antibodies were purchased from Abcam, MA, USA. Anti-β-actin antibodies were purchased from Sigma-Aldrich.
Statistical Analysis
The study bioinformatician and the NGS core facility were blinded to the results of the functional study [11] at the time of RNA-seq data collection and analysis. Differential expression analysis was performed using DESeq2 version 1.22.2 [13] in R version 3.5.1. Genes with a Benjamini-Hochberg False Discovery rate < 0.05 were considered statistically significant. No minimal fold change cut-off was imposed due to the shrinkage of fold change estimates by DESeq2. Pathway enrichment analysis and prediction of functional consequences of differential expression changes were performed using IPA software (QIAGEN Inc., https://www.qiagenbioinformatics.com/products/ingenuitypathway-analysis). Figures were generated using ggplot2 version 3.3.2 [14].
Data for the RT-PCR and immunoblotting were presented as means and individual animal data measurements. Analysis of variance (ANOVA) with Sidak correction for multiple comparisons was applied to compare the different groups. Values of p < 0.05 were considered statistically significant. In each figure, the p value of the ANOVA is shown together with symbols for the individual comparisons between specific groups.
Results
At the end of the 12-week treatment, fasting serum glucose levels were significantly lower in the dapagliflozin-treated group (177+6 mg/dl versus 380+9 mg/dl; p<0.001) [11].
RNA-Sequencing
Consistent with our previous RT-PCR report [11], the mechanism-of-action target Slc5a2 (SGLT2) had negligible expression below 1 count per million in all RNA-seq samples (not reliably detected). Slc5a1 (SGLT1) levels ranged between 0.7 and 1.5 counts per million, which indicated low expression close to the detection limit and did not change with dapagliflozin (Supplementary Table 1).
We detected 1382 differentially expressed genes in dapagliflozin-treated compared to untreated BTBR mouse hearts. Pathway enrichment analysis indicated reduced activity of pro-hypertrophy and pro-inflammation pathways after treatment with dapagliflozin (Table 2). By contrast, anti-hypertrophy p53 signaling [15] was increased. Ingenuity Pathway Analysis (IPA) software Diseases and Functions analysis confirmed that the expression changes were compatible with decreased hypertrophy (2.2-fold reduction, p-value 1.8e-28), decreased cell death (strongest reduction for gene set “Cell death of osteosarcoma cells,” 5.7-fold reduction, p-value 2.4e-12), and reduced tissue injury (gene set “Infarction,” 2.5-fold reduction, p-value 1.5e-14). In addition to the systematic analysis, we investigated the expression of marker genes such as key enzymes, kinases, and transcription factors (Fig. 1).
Marker genes. a Dapagliflozin reduced expression of key enzymes in glycolysis, acetyl-CoA production and tricarboxylic acid cycle, indicating reduced reliance on glucose as energy source by diabetic mouse heart. b Dapagliflozin upregulated endogenous antioxidant enzymes and c reduced expression of hypoxia markers. Dapagliflozin decreased expression of d pro-hypertrophy and e inflammation markers. f Overall effect on heart fibrosis could not be inferred from RNA-seq due to conflicting directionality of expression changes. g Marker expression indicated reduced cell death in dapagliflozin-treated animals. Most markers participate in multiple processes (e.g., Hif1a participates in both hypoxia and inflammation), i.e., classification in this figure is provisional
RT-PCR
We confirmed the mRNA expression changes with dapagliflozin using RT-PCR. Dapagliflozin reduced the mRNA levels of genes related to glucose as an energy source [Hexokinase-1 (Hk1), Hexokinase-2 (Hk2), and Phosphoglycerate kinase 1 (Pgk1)] (Fig. 2). Dapagliflozin increased mRNA levels of genes of antioxidant enzymes [Glutathione Peroxidase-1 (Gpx1), Glutathione Peroxidase-3 (Gpx3), Glutathione Peroxidase-4 (Gpx4), Metallothionein-2 (Mt2), Metallothionein-3 (Mt3), and Superoxide dismutase-3 (Sod3)], while it decreased the levels of Superoxide dismutase-2 (Sod2) (Fig. 3). In addition, dapagliflozin decreased mRNA levels of genes associated with response to hypoxia [hypoxia inducible factor 1 subunit alpha (HIF1α), BTB domain and CNC homolog 1 (Bach1), Egl-9 family hypoxia inducible factor 3 (Egln3), and vascular endothelial growth factor A (Vegfa)] (Fig. 4). Dapagliflozin reduced the mRNA of genes associated with hypertrophy [Fos proto-oncogene, AP-1 transcription factor subunit (Fos), FOS like 2, AP-1 transcription factor subunit (Fosl2), and integrin linked kinase (Ilk)] (Fig. 5). Dapagliflozin reduced the expression of the pro-inflammatory gene Cd74 (Fig. 6) and increased the anti-apoptotic genes [annexin A4 (Anxa4), cyclin dependent kinase inhibitor 1A (Cdkn1a), activating transcription factor 5 (Atf5), AXL receptor tyrosine kinase (Axl), and growth arrest specific 6 (Gas6)] (Fig. 6). In addition, dapagliflozin increased mRNA levels of Col14a1, mothers against decapentaplegic homolog 7 (Smad7), and tissue inhibitor of metalloproteinase 1 (Timp1) and decreased the levels of mothers against decapentaplegic homolog 3 (Smad3), matrix metallopeptidase 15 (Mmp15), and Pdgfa mRNA levels (Fig. 6).
Immunoblotting
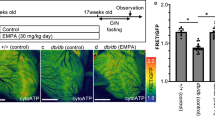
Compared to non-diabetic mice, the heart of the BTBR mice had lower expression of Gpx1, Sod3, and Smad7 and higher expression of Hif1α, Vegfa, Cd74, and Smad3. Dapagliflozin attenuated all these changes, increasing Gpx1, Sod3, and Smad7 and decreasing protein levels of Hif1α, Vegfa, Cd74, and Smad3 compared to the untreated BTBR mice (Fig. 7).
Changes in protein expression of selected markers. a Samples of immunoblotting. b Densitometric analysis of Gpx1. c Densitometric analysis of Sod3. d Densitometric analysis of Hif1α. e Densitometric analysis of Vegfa. f Densitometric analysis of Cd74. g Densitometric analysis of Smad3. h Densitometric analysis of Smad7. There were 4 animals in each group. *p < 0.02 versus BTBR group. τ p < 0.02 versus BTBR+DAPA group
Discussion
In our previous studies, we have shown that dapagliflozin ameliorated the development of diabetic cardiomyopathy in BTBR ob/ob mice with type 2 diabetes [10, 11]. Specifically, dapagliflozin increased ejection fraction, reduced left ventricular end systolic and diastolic volumes, and had no effect on heart rate in BTBR mice [11]. Dapagliflozin attenuated the myocardial activation of the NOD-like receptor 3 (NLRP3) inflammasome and reduced levels of NLRP3, apoptosis-associated speck-like protein (ASC), interleukin-1β (IL-1β), IL-6, caspase-1, and tissue necrotic factor α (TNFα). Dapagliflozin attenuated the increase in collagen-1 and -3 levels and decreased apoptosis. The beneficial effects of dapagliflozin were mediated by adenosine monophosphate kinase (AMPK) activation [10, 11].
The current study confirmed a reduction in inflammation and specifically in type I cytokine signaling (IPA pathway term “IL-18 signalling”) in the hearts of BTBR mice treated with dapagliflozin based on RNA-seq. We observed that Akt1 mRNA expression (decrease in RNA-seq in this study) was dis-concordant with the increase in Akt activity (phosphorylation) in the heart of dapagliflozin-treated BTBR mice [11]. We view increased Akt phosphorylation [11] as a more physiologically relevant readout. We found that dapagliflozin also alters several key pathways associated with the utilization of glucose as an energy source, antioxidant enzymes, response to hypoxia, hypertrophy, fibrosis, and apoptosis in the hearts of BTBR mice with type 2 diabetes with advanced diabetic cardiomyopathy and systolic dysfunction.
Our advanced diabetic cardiomyopathy model study showed similar processes affected by SGLT2 inhibitor treatment to a previous study, which assessed the effects of SGLT2 inhibitor ertugliflozin on cardiac metabolic gene expression in mice with high-fat, high-glucose diet-induced type 2 diabetes [16]. They induced an early stage of diabetic cardiomyopathy, characterized by myocardial hypertrophy and fibrosis and diastolic dysfunction. Ertugliflozin attenuated oxidative stress, increased contractile reserve, and increased expression of genes involved in oxidative phosphorylation and fatty acid metabolism [16]. More granular observations on individual gene level were specific to our advanced diabetic cardiomyopathy study and, in part, novel (summarized in Table 3 and described in detail below).
Local SGLT2 Expression in Heart
Consistent with our previous studies [11], we observed only traces of SGLT2 mRNA expression in bulk mouse hearts that were below the reliable detection limit. Hence, dapagliflozin-mediated effects were likely systemic.
Local Sglt1 Expression in Heart
Previously, we have found that dapagliflozin (1.5 mg/kg/d) does not change myocardial SGLT1 mRNA levels in the animals used in the current study [11]. Currently, RNA-sequencing confirmed this finding. Yet, in a previous experiment using identical condition, dapagliflozin (1.0 mg/kg/d) reduced SGLT1 mRNA levels [10]. It could be that at a lower dose, dapagliflozin reduces SGLT1 expression. This should be verified in additional studies.
Glucose as an Energy Source
Hk1 and Hk2
It is well known that SGLT2 inhibitors decrease the glucose utilization in the heart while increasing ketone body utilization as an energy source [53]. However, the signaling mechanisms of this phenomenon are unclear [53, 54]. As the bulk heart tissue shows only low traces of SGLT2 expression, the effects are probably indirect. Here, we found that dapagliflozin reduces the expression of Hk1 and Hk2 mRNA levels. Hk1 and Hk2 are rate-limiting enzymes of glycolysis. Downregulation of these enzymes should lead to decreased glucose utilization [55]. Uthman et al. reported that canagliflozin, but not dapagliflozin and empagliflozin, significantly reduced the expression of Hk2 protein in human coronary artery endothelial cells in vitro. The decrease in Hk1 protein levels was not statistically significant in their model [18]. We were not able to find other reports on the effects of SGLT2 inhibitors on Hk1 or Hk2 expression in the heart.
Pgk1
Pgk1 catalyzes one of the two ATP-producing reaction steps in the glycolytic pathway via the reversible conversion of 1,3-diphosphoglycerate to 3-phosphoglycerate. Pgk1 may act as a link between glucose metabolism, oxidative stress, and hypoxia because it is a target gene of Hif1α [56]. Pgk1 expression is reduced (normalized) in the kidney of chronic kidney disease patients treated with SGLT2 inhibitors [19]. Here, we found that dapagliflozin reduced Pgk1 mRNA levels in the heart.
Antioxidant Enzymes
Oxidative stress contributes to the development of diabetic cardiomyopathy [57]. SGLT2 inhibitors have been previously reported to ameliorate oxidative stress in rodent cardiomyopathy models [6, 33], but the specific molecular mechanisms affected by SGLT2i treatment in heart tissue have not been elucidated. We found that dapagliflozin increased the myocardial mRNA levels of several antioxidant enzymes (Gpx1, Gpx3, Gpx4, Mt1, Mt2, Mt3, and Sod3) and decreased the levels of Sod2. Immunoblotting confirmed that dapagliflozin increased the myocardial protein levels of Gpx1 and Sod3 in the diabetic mice.
Glutathione Peroxidases
mRNA levels of Gpx1 were reported to be elevated in the myocardium of diabetic mice [20]. On the other hand, Chao et al. reported reduced myocardial mRNA levels of Gpx1 in diabetic hearts compared to non-diabetic hearts and that natural antioxidant compounds caffeic acid and ellagic acid increased Gpx1 levels [21]. The effects of diabetes on Gpx3 have not been described before. It was suggested that Gpx4 deficiency leads to diabetes via ferroptosis-dependent pancreatic beta cell destruction [58]. High sucrose and high-fat diet induced more cardiac fibrosis and upregulation of pro-inflammatory and pro-fibrotic genes in Gpx4+/- mice than in wild-type mice [59]. Overexpression of mitochondria Gpx4 attenuated hydrogen peroxide production and lipid peroxidation in the myocardium and the deterioration of left ventricular systolic function in mice with type 1 diabetes [60]. To the best of our knowledge, no previous studies reported on the effects of SGLT2 inhibition on Gpx1, Gpx3, and Gpx4.
Metallothioneins
Diabetes decreases the myocardial mRNA expression and increases polymerization of the copper-responsive metallothioneins Mt1 and Mt2, leading to reduced antioxidant capacity of the heart [17]. Overexpression of metallothionein increases the expression of Hif1α (see below) and Hk2 (see above) and ameliorates diabetic cardiomyopathy [28, 61]. Cardiomyocyte-specific overexpression of Mt2 attenuated the development of diabetic cardiomyopathy and restored expression of glucose metabolism-related proteins, baseline total Akt phosphorylation, ERK1/2 phosphorylation in the heart of Akt2-knock out mice with type 2 diabetes [62] or in streptozotocin-induced diabetic mice [63]. Changes in Mt3 expression in the diabetic heart have not been described before. Likewise, the effects of SGLT2 inhibition of the myocardial expression of metallothioneins have not been previously described. However, it was suggested that metallothionein activation is downstream of nuclear transcription factor erythroid 2-related factor 2 (Nrf2) based on an elegant sulforaphane treatment experiment in Mt1 and Nrf2 knockout mice with diabetic cardiomyopathy [64]. Nrf2 is a master regulator of antioxidant response. Nrf2 and the downstream metallothionein system could be indirectly modulated by SGLT2 inhibitors because SGLT2 inhibitors mimic starvation and increase the availability of ketone bodies, which in turn activate Nrf2 [42].
Sod3
Extracellular superoxide dismutase (Sod3) protects against oxidative stress by detoxification of highly reactive superoxide [57]. Serum and myocardial superoxide dismutase activity are lower in rats with alloxan-induced diabetes [22]. Diabetic patients with rs1799895 R213G variation in the Sod3 gene (which has lower antioxidant capacity) have an increased risk for cardiovascular disease and heart failure [65]. Here, we found that dapagliflozin increased myocardial mRNA and protein levels of Sod3.
Sod2
Sod2 [manganese-dependent superoxide dismutase (MnSOD)] also has potent antioxidant activity. Surprisingly, we found that dapagliflozin mildly decreased myocardial Sod2 levels. Kain et al. found lower Sod2 protein levels in the hearts of diabetic rats [23]. Similarly, Ding et al. reported that myocardial protein levels of Sod2 were reduced in mice with type 2 diabetes and exenatide increased the levels [24]. It was found that urinary Sod2 activity is higher among patients with type 2 diabetes treated with than without SGLT2 inhibitors [27]. Cotrin et al. reported that cardiac Sod2 mRNA levels were reduced in mice with diet-induced type 2 diabetes [25]. Levels significantly increase in mice receiving empagliflozin [25]. Oshima et al. also found that empagliflozin increased Sod2 protein levels in the hearts of diabetic rats after myocardial infarction [26]. Thus, the difference among studies could be related to the stage of diabetic cardiomyopathy (advanced with systolic dysfunction in our model) or different effects of empagliflozin versus dapagliflozin. Alternatively, Sod2 might be decreased due to a feedback loop with Hif1α [66].
Response to Hypoxia
Hif1α
There are conflicting reports on the effect of diabetes on the myocardial expression of Hif1α and the effects of Hif1α on the progression of diabetic cardiomyopathy. Xue et al. reported that diabetes did not affect myocardial Hif1α mRNA levels in mice but decreased Hif1α protein levels by affecting protein nuclear translocation [28]. Metallothionein increased myocardial Hif1α mRNA and protein levels in non-diabetic and diabetic mice and lead to attenuation of diabetic cardiomyopathy [28]. Bohuslavova et al. reported that the deterioration of left ventricular function was more severe in heterozygous Hif1α knock-out (Hif1α+/-) than in wild-type diabetic mice, suggesting a protective role for Hif1α [67]. Stabilization of Hif1α by Molidustat improves post-ischemic recovery of function in the diabetic heart [56].
On the other hand, Gao et al. reported that 25 mM glucose increased myocardial Hif1α protein levels in vitro in human cardiomyocytes and that Hif1α increases Sox9 expression, leading to glucose-induced hypertrophy [68]. Huang et al. found that Hif1α induces insulin-like growth factor (IGF1)-binding protein 3 (IGFBP3) overexpression, leading to cardiac cell apoptosis both in vitro and in vivo [69].
Kim et al. reported that empagliflozin increases Hif1α expression in the renal medulla in non-diabetic uni-nephrectomized rats [29]. Luseoglifozin reduced Hif1α protein levels in human renal proximal tubular epithelial cells in vitro [30]. Packer suggested that diabetes increases the expression of Hif1α and decreases the expression of Hif2α, promoting inflammation and fibrosis in the kidneys [70]. On the other hand, Ghanim et al. found that dapagliflozin decreased Hif1α expression in the mononuclear cells of patients with type 2 diabetes [31]. However, the effect of SGLT2 inhibition on Hif1α expression in the diabetic heart has not been reported. Here, we report that dapagliflozin reduced both Hif1α mRNA and protein levels.
Bach1
We found that dapagliflozin reduced the myocardial mRNA levels of BTB and CNC homology 1 (Bach1), a transcriptional repressor of antioxidative enzymes [71]. Myocardial Bach1 protein expression is increased in db/db mice relative to non-diabetic C57BLKS/J mice [32]. Seven days of exposure to exogenously administered antioxidant sodium sulfide reduced nuclear expression of Bach1 in the hearts of db/db diabetic mice with a resultant increase in heme oxygenase-1 (HO-1) expression [32]. The effect of SGLT2 inhibition on Bach1 expression has not been reported, but the downstream gene HO-1 is increased by empagliflozin in the heart of diabetic KK-Ay mice, which is consistent with inhibition of Bach1 [33].
Egln3
Egln3 encodes a Prolyl hydroxylase-3 that mediates hydroxylation of proline residues in target proteins, including HIF1α. It leads to proteasomal destruction of HIF1α [72]. Myocardial levels of prolyl hydroxylase-3 are increased in rats with diabetic cardiomyopathy, and downregulation of prolyl hydroxylase-3 with shRNA decreased high glucose-induced apoptosis in H9c2 cardiomyoblasts exposed to high glucose and improved left ventricular function in diabetic rats [34]. Here, we found that dapagliflozin reduced myocardial Egln3 mRNA levels, which might potentially mediate some of the protective effects of dapagliflozin in the diabetic heart. We were not able to find previous reports on the effects of SGLT2 inhibition on Egln3 or prolyl hydroxylase-3 expression or activity.
Vegfa
In mice with streptozotocin-induced type 1 diabetes, myocardial Vegfa protein levels and microvascular density (Cd31 staining) are reduced [35, 73]. Overexpression of decorin upregulated the expression of Vegfa and attenuated the decrease in capillary density in the hearts of diabetic rats. This was associated with improvement in left ventricular function [74]. Myocardial Vegfa protein levels, capillary density, and left ventricular systolic function were lower in diabetic rats than in non-diabetic rats, and Neuregulin-1 restored these abnormalities [36].
In high-fat diet + streptozotocin-induced type 2 diabetes, SGLT2 inhibition improved cardiac function and reduced myocardial Vegfa protein levels. It was shown that SGLT2 inhibition reduced the levels of microRNA-30d, and the effect of SGLT2 inhibition on Vegfa was microRNA-30d dependent [37]. In human renal proximal tubular epithelial cells, SGLT2 inhibition with luseogliflozin reduced the expression of Vegfa mRNA [30]. So, although earlier reports suggested Vegfa depletion in diabetic models which could lead to microvascular depletion, two more recent reports support our findings that SGLT2 inhibition with dapagliflozin reduces myocardial Vegfa mRNA and protein expression. Also, Vegfa is regulated by Hif1α, and its expression tends to follow Hif1α expression and activity [75]. Thus, reduced Vegfa with dapagliflozin treatment could be a marker of normalization of Hif1α activity and reduction of tissue hypoxia [75].
Hypertrophy
ILK Signaling
ILK overactivation promotes cardiac hypertrophy [76]. ILK signaling was the top down-regulated pathway in dapagliflozin-treated BTBR mice RNA-seq in our study. We did not confirm phosphorylated and total ILK due to a lack of specific commercial reagents for mouse at the time when the study was conducted. However, we believe that ILK signaling warrants investigation in future studies as it has been computationally predicted as part of the SGLT2 mechanism of action [77] and proposed as part of the cardioprotective mechanism of empagliflozin [78].
c-Fos
c-Fos encodes a 62 kDa protein, which forms a heterodimer with c-Jun, resulting in the formation of activator protein-1 (AP-1) complex which binds DNA at AP-1-specific sites at the promoter and enhancer regions of target genes and converts extracellular signals into changes of gene expression. c-Fos protein levels were increased in neonatal rat cardiomyocytes exposed to high glucose concentrations. c-Fos levels were lower in cardiomyocytes exposed to NFκB inhibitor or protein kinase C inhibitors in addition to high glucose levels [79] and to β-blockers [38]. These interventions also ameliorated cardiomyocyte hypertrophy. A similar increase in myocardial c-Fos protein levels was described in diabetic rats [80]. An increase in myocardial c-Fos levels was seen in rats with type-1, but not with type-2 (Zucker Diabetic Fatty) diabetes [81]. AP-1 (which is composed of c-Fos and c-Jun) mediates cardiomyocyte apoptosis when cells are exposed to high saturated fatty acid levels [82]. Finally, a recent network pharmacology analysis suggested that c-FOS is involved in the pathogenesis of diabetic cardiomyopathy [83].
The effects of SGLT2 inhibitors on myocardial c-FOS expression have not been previously reported. In non-diabetic mice, a single dose of dapagliflozin increases c-Fos expression in the brain [39]. Here, we found that in mice with type 2 diabetes, dapagliflozin decreased myocardial c-Fos levels. This pathway could (partially) explain the anti-hypertrophic effects of the SGLT2 inhibitors.
Fosl2
FOS Like 2 (Fosl2 or AP-1 transcription factor subunit) is one of the four members of the Fos family. When incorporated into the AP-1 complex, it regulates cell differentiation, proliferation, and transformation. Fosl2 is involved in multiple fibrotic processes, including lung fibrosis [84]. Fosl2 is a significant regulator of the leptin gene and is associated with adiposity [85, 86]. Yet, Li et al. reported lower mRNA and protein levels in the peripheral blood of patients with type 2 diabetes than in controls with normal glucose tolerance test [87]. We found that dapagliflozin decreased myocardial Fosl2 mRNA levels. We did not find previous reports on the effects of diabetes on myocardial Fosl2 levels. Moreover, we were not able to find previous reports on the effects of SGLT2 inhibition on Fosl2 expression.
Proinflammatory Genes
Cd74
Cd74 encoded a protein that is associated with the class II major histocompatibility complex (MHC), serving as a chaperone that regulates antigen presentation for immune response. It also serves as a cell surface receptor for the cytokine macrophage migration inhibitory factor (MIF). We found that Cd74 mRNA and protein levels were lower in the hearts of the dapagliflozin-treated diabetic mice. In neonatal mouse ventricular cells, Cd74 is essential for MIF-induced adenosine monophosphate kinase (AMPK) activation with subsequent increased glucose transporter type 4 (GLUT4) expression [88]. MIF limits myocardial ischemic injury [89]. There have been no previous reports on the effects of SGLT2 inhibition on Cd74 levels.
Apoptosis
Anxa4
Annexin IV (Anxa4) is part of the annexin family of calcium-dependent phospholipid-binding proteins. Anxa4 is known to target several genes associated with diabetes, including diabetes-induced β-cell apoptosis [90]. The effects of diabetes on Anxa4 expression in the heart or the effects of SGLT2 inhibition on Anxa4 expression have not been reported. In our model, dapagliflozin increased Anxa4 mRNA levels.
Cdkn1a
Cyclin-dependent kinase-inhibitor 1 (Cdkn1a, also called P21) encodes a protein that regulates cell cycle progression, terminal differentiation, and apoptosis. It is associated with senescence. Methylation of Cdkn1a leads to inhibition of several cyclin-cyclin-dependent kinase complexes and contributes to diabetes-induced oxidative damage and cardiomyopathy [91]. Myocardial levels of Cdkn1a are higher in mice with streptozotocin-induced diabetic cardiomyopathy than in control non-diabetic mice [41]. Cdkn1a is involved in hyperglycemia-induced cardiomyocyte hypertrophy [40].
Renal levels of Cdkn1a mRNA and protein are increased in streptozotocin-induced diabetic mice [92]. Dapaglilozin, but not glimepiride, reduced Cdkn1a levels in the kidney in db/db mice [42]. Empagliflozin reduced Cdkn1a protein levels in the aortas of obese ZSF1 rats [43]. In human, kidneys express SGLT2, but, in contrast to the rat study [43], there is no SGLT2 expression in the aorta or arteries in human (https://gtexportal.org/home/gene/SLC5A2). Of note, aorta samples profiled by the GTEx consortium include both diabetic and non-diabetic individuals [93]. The effects of SGLT2 inhibition on the expression of Cdkn1a in the heart (that does not express SGLT2) have not been previously reported. In our model, dapagliflozin increased Cdkn1a mRNA levels. Thus, the effects of SGLT2i on Cdkn1a are likely indirect or not mediated by SGLT2 itself [93].
Atf5
Activating transcription factor 5 (Atf5) possesses DNA-binding transcription activator activity, RNA polymerase II-specific activity, RNA polymerase II transcription regulatory region sequence-specific DNA binding activity, and tubulin binding activity. Atf5 levels increase during mitochondrial stress [94]. Atf5 promotes β-cell survival during stress [95]. However, it has not been reported if levels of Atf5 are altered in the diabetic heart. We were not able to find reports on the effects of SGLT2 inhibition on Atf5 expression. In our model, dapagliflozin increased Atf5 mRNA levels.
Axl
Axl encodes a tyrosine-protein kinase receptor. Axl is an inhibitor of the innate immune response. Overexpression of Axl improves endothelial function in cells exposed to high glucose and hypoxia [96]. However, Axl could be involved in diabetic retinopathy [97]. We found no reports on the effects of diabetic on Axl expression in the heart or on the effects of SGLT2 inhibitors on Axl levels. In our model, dapagliflozin increased Axl mRNA levels.
Gas6
Growth arrest-specific 6 (Gas6) is a ligand of Axl. Levels are elevated in the vitreous of patients with proliferative diabetic retinopathy [97]. Gas6 affects the expression of adiponectin and is associated with insulin resistance in adipocytes [98]. It is also involved in mesangial cell proliferation and diabetic nephropathy [99]. The effects of diabetes on myocardial Gas6 levels have not been reported. We have not been able to find previous reports on the effects of SGLT2 inhibition on Gas6 expression. In our model, dapagliflozin increased Gas6 mRNA levels.
Fibrosis
Col14a1
Here, we found that dapagliflozin increased myocardial Col14a1 mRNA levels. Col14a1 encodes the alpha chain of XIV collagen. Changes in collagen XIV in the preretinal membrane were reported in diabetic patients [100]. Increased levels of the alpha chain of XIV collagen were seen in the placenta of women with gestational diabetes [101]. However, there are no reports on the effects of diabetes on myocardial Col14a1 or on the effects of SGLT2 inhibition on Col14a1 expression.
Smad7
Mothers against decapentaplegic homolog 7 (SMAD7) blocks signaling by transforming growth factor-β receptors via preventing the interaction between Smad2 and Smad4. Van Linthout et al. [44] reported that myocardial Smad7 protein levels were higher in rats with streptozotocin-induced diabetes. By contrast, Zhang et al. [102], Wang et al. [45], and Malek and Gaikwad [103] found reduced levels compared to non-diabetic rats, supporting our findings. Malek and Gaikwad found that treatment with a dual angiotensin receptor-neprilysin inhibitor (ARNi) reduced myocardial inflammation and fibrosis and increased Smad7 expression [103]. Hyperglycaemia increased collagen production and decreased Smad7 levels via upregulation of miR-150-5p levels in cardiac fibroblasts. Silencing miR-150-5p increased Smad7 levels and reversed all these changes [104]. Thus, increasing Smad7 levels with dapagliflozin, as found in our study, could be potentially beneficial. We have not found other studies reporting on the effects of SGLT2 inhibitor on Smad7 levels.
Smad3
We found that myocardial Smad3 protein concentrations were higher in the diabetic than in the non-diabetic mice. Dapagliflozin reduced Smad3 mRNA and protein levels. Smad3 is involved in transmitting signals from the cell surface to the nucleus, and it is a component of the transforming growth factor-β signaling pathway. Smad3 is involved in cardiac fibrosis [105]. In rats with streptozotocin-induced diabetes, myocardial levels of phosphorylated Smad3 are increased [46]. Inhibition of Smad3 phosphorylation attenuated the expression of α-smooth muscle actin in cardiac fibroblasts exposed to transforming growth factor [46]. Wang et al. showed that type 2 diabetes increased myocardial levels of phosphorylated SMAD3 without a detectable effect on total SMAD3 levels [45]. Exercise improved left ventricular function and decreased phosphorylated SMAD3 levels in their model [45]. Myocardial concentrations of phosphorylated SMAD3 were higher in db/db mice than in non-diabetic mice. Follistatin ameliorated diabetic cardiomyopathy and reduced phosphorylated SMAD3 levels in these db/db mice [106]. Deletion of Smad3 protected db/db mice against the development of diabetic cardiomyopathy [107].
It was shown that transforming growth factor-β increases SGLT2 expression in the kidney via SMAD3 phosphorylation [108]. High glucose increased SMAD3 phosphorylation in human proximal tubule epithelial cells, and dapagliflozin reduced SMAD3 phosphorylation in vitro [47]. However, the effects of SGLT2 inhibition on the myocardial levels of Smad3 have not been reported before. Smad3 inhibition might be a potential target mediating the cardiac anti-fibrotic effects of SGLT2 inhibition.
Timp1
Dapagliflozin increased myocardial mRNA levels of tissue inhibitor of metalloproteinase 1 (Timp1). Myocardial mRNA levels of Timp1 were reported to be reduced in streptozotocin-induced diabetic mice, along with an increase in TGFβ1 [48, 49]. On the other hand, Wang et al. [45] and Dawood et al. [50] found an increase in myocardial Timp1 mRNA expression in streptozotocin-induced type 2 diabetic rats. Wang et al. reported that exercise ameliorated cardiac fibrosis and reduced the expression of Timp1 in their model [45], while Dede et al. reported that exercise increased Timp1 levels [49]. Meng et al. found that in human cardiac fibroblasts incubated with high glucose, Timp1 mRNA increased. Phlorizin (100 μM) decreased the expression, while dapagloflozin (100 μM) had no effect, suggesting SGLT1-mediated effect [51]. Dawood et al. reported that metformin decreased myocardial Timp1 mRNA levels in rats with type 2 diabetes [50]. More recently, Cotrin et al. found that empagliflozin decreased myocardial Timp1 levels in mice with diet-induced type 2 diabetes [25]. Thus, so far, we have conflicting data as to the effect of diabetes on myocardial Timp1 expression. Moreover, while Meng et al. reported that dapagliflozin had no effect on Timp1 expression in cardiac fibroblasts in vitro, we found that in vivo, dapagliflozin increased the levels.
Mmp15
Matrix metallopeptidase 15 (Mmp15) is involved in the breakdown of extracellular matrix. We found that dapagliflozin decreased myocardial Mmp15 mRNA levels in the diabetic mice. mRNA levels of Mmp15 were significantly higher in the atria of high-salt-sensitive rats than in normotensive rats [109]. We found no reports on the effects of diabetes or SGLT2 inhibition on Mmp15 expression.
Pdgfa
Platelet-derived growth factor subunit A (Pdgfa) can form a homodimer or heterodimer with the subunit B (Pdgfb), activate Pdgfra and Pdgfrb receptors, and trigger myocardial fibrosis [110]. Pdgf signaling is increased in the heart of high-fat diet + streptozotocin and db/db diabetic cardiomyopathy models [52]. In this study, we found that dapagliflozin reduced Pdgfa gene and protein expression in BTBR mouse heart.
Conclusions
In the current study, we investigated whole heart transcriptome using RNA-sequencing and identified several genes whose myocardial expression was altered by dapagliflozin in mice with advanced diabetic cardiomyopathy. These genes might be involved in mediating the favorable protective effects of SGLT2 inhibition against the progression of diabetic cardiomyopathy and even the progression of cardiomyopathy and heart failure in non-diabetic models. We have not established a cause and effect. It could be that the observed changes of some of the genes are simply secondary to the decrease in serum glucose levels induced by dapagliflozin [11]. Based on the findings of the current study, further studies are needed using control groups in which similar magnitudes of glucose-lowering effects are obtained with other glucose-lowering agents that lack reported favorable cardiovascular protecting effects (for example, glimepiride or glyburide) to verify if these changes are specific to SGLT2 inhibition. As the heart does not express SGLT2 [10, 11, 111], indirect effects mediated by mediators secreted by the kidneys that express SGLT2 are plausible.
We provide the RNA-sequencing data set as a resource (Supplementary Table 1) that can be used together with other studies for meta-analysis and deriving further insights into the molecular mechanisms of SGLT2 inhibitors. Ultimately, such studies might help to develop additional agents that could augment the protective effects of SGLT2 inhibitors or be used in patients with contraindications for SGLT2 therapy in the future.
Data Availability
RNA-sequencing read counts and differential expression results (Supplementary Table 1), IPA pathway analysis results without p-value cut-off (Supplementary Table 2), and z-score transformed expression values for Fig. 2 (Supplementary Table 3) are enclosed with this article. Raw FASTQ files could not be recovered.
References
Wiviott SD, Raz I, Bonaca MP, et al. Dapagliflozin and cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2019;380(4):347–57. https://doi.org/10.1056/NEJMoa1812389.
Cefalu WT, Kaul S, Gerstein HC, et al. Cardiovascular outcomes trials in type 2 diabetes: where do we go from here? Reflections from a diabetes care editors' expert forum. Diabetes Care. 2018;41(1):14–31. https://doi.org/10.2337/dci17-0057.
McMurray JJV, Solomon SD, Inzucchi SE, et al. Dapagliflozin in patients with heart failure and reduced ejection fraction. N Engl J Med. 2019;381(21):1995–2008. https://doi.org/10.1056/NEJMoa1911303.
Inzucchi SE, Claggett BL, Vaduganathan M, et al. Efficacy and safety of dapagliflozin in patients with heart failure with mildly reduced or preserved ejection fraction by baseline glycaemic status (DELIVER): a subgroup analysis from an international, multicentre, double-blind, randomised, placebo-controlled trial. Lancet Diabetes Endocrinol. 2022;10(12):869–81. https://doi.org/10.1016/S2213-8587(22)00308-4.
Joubert M, Jagu B, Montaigne D, et al. The sodium-glucose cotransporter 2 inhibitor dapagliflozin prevents cardiomyopathy in a diabetic lipodystrophic mouse model. Diabetes. 2017;66(4):1030–40. https://doi.org/10.2337/db16-0733.
Arow M, Waldman M, Yadin D, et al. Sodium-glucose cotransporter 2 inhibitor dapagliflozin attenuates diabetic cardiomyopathy. Cardiovasc Diabetol. 2020;19(1):7. https://doi.org/10.1186/s12933-019-0980-4.
Saleh S, Hanna G, El-Nabi SH, et al. Dapagliflozin, a sodium glucose cotransporter 2 inhibitors, protects cardiovascular function in type-2 diabetic murine model. J Genet. 2020;99:1–8. https://doi.org/10.1007/s12041-020-01196-9.
Olgar Y, Turan B. A sodium-glucose cotransporter 2 (SGLT2) inhibitor dapagliflozin comparison with insulin shows important effects on Zn(2+)-transporters in cardiomyocytes from insulin-resistant metabolic syndrome rats through inhibition of oxidative stress. Can J Physiol Pharmacol. 2019;97(6):528–35. https://doi.org/10.1139/cjpp-2018-0466.
Shi L, Zhu D, Wang S, Jiang A, Li F. Dapagliflozin attenuates cardiac remodeling in mice model of cardiac pressure overload. Am J Hypertens. 2019;32(5):452–9. https://doi.org/10.1093/ajh/hpz016.
Ye Y, Bajaj M, Yang HC, Perez-Polo JR, Birnbaum Y. SGLT-2 Inhibition with dapagliflozin reduces the activation of the Nlrp3/ASC inflammasome and attenuates the development of diabetic cardiomyopathy in mice with type 2 diabetes. Further Augmentation of the Effects with Saxagliptin, a DPP4 Inhibitor. Cardiovasc Drugs Ther. 2017;31(2):119–32. https://doi.org/10.1007/s10557-017-6725-2.
Chen H, Tran D, Yang HC, et al. Dapagliflozin and ticagrelor have additive effects on the attenuation of the activation of the NLRP3 inflammasome and the progression of diabetic cardiomyopathy: an AMPK-mTOR interplay. Cardiovasc Drugs Ther. 2020;34(4):443–61. https://doi.org/10.1007/s10557-020-06978-y.
Dobin A, Davis CA, Schlesinger F, et al. STAR: ultrafast universal RNA-seq aligner. Bioinformatics. 2013;29(1):15–21. https://doi.org/10.1093/bioinformatics/bts635.
Love MI, Huber W, Anders S. Moderated estimation of fold change and dispersion for RNA-seq data with DESeq2. Genome Biol. 2014;15(12):550. https://doi.org/10.1186/s13059-014-0550-8.
Wickham H. ggplot2: elegant graphics for data analysis. New York: Springer; 2016.
Mak TW, Hauck L, Grothe D, Billia F. p53 regulates the cardiac transcriptome. Proc Natl Acad Sci USA. 2017;114(9):2331–6. https://doi.org/10.1073/pnas.1621436114.
Croteau D, Luptak I, Chambers JM, et al. Effects of sodium-glucose linked transporter 2 inhibition with ertugliflozin on mitochondrial function, energetics, and metabolic gene expression in the presence and absence of diabetes mellitus in mice. J Am Heart Assoc. 2021;10(13):e019995. https://doi.org/10.1161/JAHA.120.019995.
Zhang S, Liu H, Amarsingh GV, et al. Diabetic cardiomyopathy is associated with defective myocellular copper regulation and both defects are rectified by divalent copper chelation. Cardiovasc Diabetol. 2014;13:100. https://doi.org/10.1186/1475-2840-13-100.
Uthman L, Kuschma M, Romer G, et al. Novel anti-inflammatory effects of canagliflozin involving hexokinase II in lipopolysaccharide-stimulated human coronary artery endothelial cells. Cardiovasc Drugs Ther. 2021;35(6):1083–94. https://doi.org/10.1007/s10557-020-07083-w.
Nair V, Schaub J, Alakwaa F, et al. WCN23-0761 SGLT2 inhibitor treatment may enhance kidney oxygenation and attenuate HIF1a expression in young persons with type 2 diabetes. Kindney Int Rep. 2023;8(3):S197–S8. https://doi.org/10.1016/j.ekir.2023.02.439.
Nagatomo Y, Meguro T, Ito H, et al. Significance of AT1 receptor independent activation of mineralocorticoid receptor in murine diabetic cardiomyopathy. PLoS One. 2014;9(3):e93145. https://doi.org/10.1371/journal.pone.0093145.
Chao PC, Hsu CC, Yin MC. Anti-inflammatory and anti-coagulatory activities of caffeic acid and ellagic acid in cardiac tissue of diabetic mice. Nutr Metab (Lond). 2009;6:33. https://doi.org/10.1186/1743-7075-6-33.
Mushtaq I, Bashir Z, Sarwar M, et al. N-acetyl cysteine, selenium, and ascorbic acid rescue diabetic cardiac hypertrophy via mitochondrial-associated redox regulators. Molecules. 2021;26(23) https://doi.org/10.3390/molecules26237285.
Kain V, Kumar S, Sitasawad SL. Azelnidipine prevents cardiac dysfunction in streptozotocin-diabetic rats by reducing intracellular calcium accumulation, oxidative stress and apoptosis. Cardiovasc Diabetol. 2011;10:97. https://doi.org/10.1186/1475-2840-10-97.
Ding W, Chang WG, Guo XC, et al. Exenatide protects against cardiac dysfunction by attenuating oxidative stress in the diabetic mouse heart. Front Endocrinol (Lausanne). 2019;10:202. https://doi.org/10.3389/fendo.2019.00202.
Cotrin JC, de Souza GSM, Petito-da-Silva TI, et al. Empagliflozin alleviates left ventricle hypertrophy in high-fat-fed mice by modulating renin angiotensin pathway. J Renin Angiotensin Aldosterone Syst. 2022;2022:8861911. https://doi.org/10.1155/2022/8861911.
Oshima H, Miki T, Kuno A, et al. Empagliflozin, an SGLT2 inhibitor, reduced the mortality rate after acute myocardial infarction with modification of cardiac metabolomes and antioxidants in diabetic rats. J Pharmacol Exp Ther. 2019;368(3):524–34. https://doi.org/10.1124/jpet.118.253666.
Nabrdalik-Lesniak D, Nabrdalik K, Sedlaczek K, et al. Influence of SGLT2 inhibitor treatment on urine antioxidant status in type 2 diabetic patients: a pilot study. Oxid Med Cell Longev. 2021;2021:5593589. https://doi.org/10.1155/2021/5593589.
Xue W, Liu Y, Zhao J, et al. Activation of HIF-1 by metallothionein contributes to cardiac protection in the diabetic heart. Am J Physiol Heart Circ Physiol. 2012;302(12):H2528–35. https://doi.org/10.1152/ajpheart.00850.2011.
Kim S, Jo CH, Kim GH. Effects of empagliflozin on nondiabetic salt-sensitive hypertension in uninephrectomized rats. Hypertens Res. 2019;42(12):1905–15. https://doi.org/10.1038/s41440-019-0326-3.
Bessho R, Takiyama Y, Takiyama T, et al. Hypoxia-inducible factor-1alpha is the therapeutic target of the SGLT2 inhibitor for diabetic nephropathy. Sci Rep. 2019;9(1):14754. https://doi.org/10.1038/s41598-019-51343-1.
Ghanim H, Abuaysheh S, Hejna J, et al. Dapagliflozin suppresses hepcidin and increases erythropoiesis. J Clin Endocrinol Metab. 2020;105(4) https://doi.org/10.1210/clinem/dgaa057.
Peake BF, Nicholson CK, Lambert JP, et al. Hydrogen sulfide preconditions the db/db diabetic mouse heart against ischemia-reperfusion injury by activating Nrf2 signaling in an Erk-dependent manner. Am J Physiol Heart Circ Physiol. 2013;304(9):H1215–24. https://doi.org/10.1152/ajpheart.00796.2012.
Li C, Zhang J, Xue M, et al. SGLT2 inhibition with empagliflozin attenuates myocardial oxidative stress and fibrosis in diabetic mice heart. Cardiovasc Diabetol. 2019;18(1):15. https://doi.org/10.1186/s12933-019-0816-2.
Xia Y, Gong L, Liu H, et al. Inhibition of prolyl hydroxylase 3 ameliorates cardiac dysfunction in diabetic cardiomyopathy. Mol Cell Endocrinol. 2015;403:21–9. https://doi.org/10.1016/j.mce.2015.01.014.
Han B, Baliga R, Huang H, Giannone PJ, Bauer JA. Decreased cardiac expression of vascular endothelial growth factor and redox imbalance in murine diabetic cardiomyopathy. Am J Physiol Heart Circ Physiol. 2009;297(2):H829–35. https://doi.org/10.1152/ajpheart.00222.2009.
Gui C, Zeng ZY, Chen Q, et al. Neuregulin-1 promotes myocardial angiogenesis in the rat model of diabetic cardiomyopathy. Cell Physiol Biochem. 2018;46(6):2325–34. https://doi.org/10.1159/000489622.
Zhang WY, Wang J, Li AZ. A study of the effects of SGLT-2 inhibitors on diabetic cardiomyopathy through miR-30d/KLF9/VEGFA pathway. Eur Rev Med Pharmacol Sci. 2020;24(11):6346–59. https://doi.org/10.26355/eurrev_202006_21533.
Wang M, Lv Q, Zhao L, et al. Metoprolol and bisoprolol ameliorate hypertrophy of neonatal rat cardiomyocytes induced by high glucose via the PKC/NF-kappaB/c-fos signaling pathway. Exp Ther Med. 2020;19(2):871–82. https://doi.org/10.3892/etm.2019.8312.
Nguyen T, Wen S, Gong M, et al. Dapagliflozin activates neurons in the central nervous system and regulates cardiovascular activity by inhibiting SGLT-2 in mice. Diabetes Metab Syndr Obes. 2020;13:2781–99. https://doi.org/10.2147/DMSO.S258593.
Raut SK, Singh GB, Rastogi B, et al. miR-30c and miR-181a synergistically modulate p53-p21 pathway in diabetes induced cardiac hypertrophy. Mol Cell Biochem. 2016;417(1-2):191–203. https://doi.org/10.1007/s11010-016-2729-7.
Cheng Y, Li J, Wang C, et al. Inhibition of long non-coding RNA metastasis-associated lung adenocarcinoma transcript 1 attenuates high glucose-induced cardiomyocyte apoptosis via regulation of miR-181a-5p. Exp Anim. 2020;69(1):34–44. https://doi.org/10.1538/expanim.19-0058.
Kim MN, Moon JH, Cho YM. Sodium-glucose cotransporter-2 inhibition reduces cellular senescence in the diabetic kidney by promoting ketone body-induced NRF2 activation. Diabetes Obes Metab. 2021;23(11):2561–71. https://doi.org/10.1111/dom.14503.
Park SH, Farooq MA, Gaertner S, et al. Empagliflozin improved systolic blood pressure, endothelial dysfunction and heart remodeling in the metabolic syndrome ZSF1 rat. Cardiovasc Diabetol. 2020;19(1):19. https://doi.org/10.1186/s12933-020-00997-7.
Van Linthout S, Seeland U, Riad A, et al. Reduced MMP-2 activity contributes to cardiac fibrosis in experimental diabetic cardiomyopathy. Basic Res Cardiol. 2008;103(4):319–27. https://doi.org/10.1007/s00395-008-0715-2.
Wang SQ, Li D, Yuan Y. Long-term moderate intensity exercise alleviates myocardial fibrosis in type 2 diabetic rats via inhibitions of oxidative stress and TGF-beta1/Smad pathway. J Physiol Sci. 2019;69(6):861–73. https://doi.org/10.1007/s12576-019-00696-3.
Talior-Volodarsky I, Connelly KA, Arora PD, Gullberg D, McCulloch CA. alpha11 integrin stimulates myofibroblast differentiation in diabetic cardiomyopathy. Cardiovasc Res. 2012;96(2):265–75. https://doi.org/10.1093/cvr/cvs259.
Pan X, Phanish MK, Baines DL, Dockrell MEC. High glucose-induced Smad3 linker phosphorylation and CCN2 expression are inhibited by dapagliflozin in a diabetic tubule epithelial cell model. Biosci Rep. 2021;41(6) https://doi.org/10.1042/BSR20203947.
Xiao T, Zeng O, Luo J, et al. Effects of hydrogen sulfide on myocardial fibrosis in diabetic rats: changes in matrix metalloproteinases parameters. Biomed Mater Eng. 2015;26(Suppl 1):S2033–9. https://doi.org/10.3233/BME-151508.
Dede E, Liapis D, Davos C, et al. The effects of exercise training on cardiac matrix metalloproteinases activity and cardiac function in mice with diabetic cardiomyopathy. Biochem Biophys Res Commun. 2022;586:8–13. https://doi.org/10.1016/j.bbrc.2021.11.013.
Dawood AF, Alzamil NM, Hewett PW, et al. Metformin protects against diabetic cardiomyopathy: an association between Desmin-Sarcomere injury and the iNOS/mTOR/TIMP-1 fibrosis axis. Biomedicines. 2022;10(5) https://doi.org/10.3390/biomedicines10050984.
Meng L, Uzui H, Guo H, Tada H. Role of SGLT1 in high glucose level-induced MMP-2 expression in human cardiac fibroblasts. Mol Med Rep. 2018;17(5):6887–92. https://doi.org/10.3892/mmr.2018.8688.
Li W, Lou X, Zha Y, et al. Single-cell RNA-seq of heart reveals intercellular communication drivers of myocardial fibrosis in diabetic cardiomyopathy. Elife. 2023:12. https://doi.org/10.7554/eLife.80479.
Saucedo-Orozco H, Voorrips SN, Yurista SR, de Boer RA, Westenbrink BD. SGLT2 Inhibitors and ketone metabolism in heart failure. J Lipid Atheroscler. 2022;11(1):1–19. https://doi.org/10.12997/jla.2022.11.1.1.
Chen S, Coronel R, Hollmann MW, Weber NC, Zuurbier CJ. Direct cardiac effects of SGLT2 inhibitors. Cardiovasc Diabetol. 2022;21(1):45. https://doi.org/10.1186/s12933-022-01480-1.
Da Silva D, Ausina P, Alencar EM, et al. Metformin reverses hexokinase and phosphofructokinase downregulation and intracellular distribution in the heart of diabetic mice. IUBMB Life. 2012;64(9):766–74. https://doi.org/10.1002/iub.1063.
Sousa Fialho MDL, Purnama U, Dennis K, et al. Activation of HIF1alpha rescues the hypoxic response and reverses metabolic dysfunction in the diabetic heart. Diabetes. 2021;70(11):2518–31. https://doi.org/10.2337/db21-0398.
Byrne NJ, Rajasekaran NS, Abel ED, Bugger H. Therapeutic potential of targeting oxidative stress in diabetic cardiomyopathy. Free Radic Biol Med. 2021;169:317–42. https://doi.org/10.1016/j.freeradbiomed.2021.03.046.
Sha W, Hu F, Xi Y, Chu Y, Bu S. Mechanism of ferroptosis and its role in type 2 diabetes mellitus. J Diabetes Res. 2021;2021:9999612. https://doi.org/10.1155/2021/9999612.
Katunga LA, Gudimella P, Efird JT, et al. Obesity in a model of gpx4 haploinsufficiency uncovers a causal role for lipid-derived aldehydes in human metabolic disease and cardiomyopathy. Mol Metab. 2015;4(6):493–506. https://doi.org/10.1016/j.molmet.2015.04.001.
Baseler WA, Dabkowski ER, Jagannathan R, et al. Reversal of mitochondrial proteomic loss in type 1 diabetic heart with overexpression of phospholipid hydroperoxide glutathione peroxidase. Am J Physiol Regul Integr Comp Physiol. 2013;304(7):R553–65. https://doi.org/10.1152/ajpregu.00249.2012.
Feng W, Wang Y, Cai L, Kang YJ. Metallothionein rescues hypoxia-inducible factor-1 transcriptional activity in cardiomyocytes under diabetic conditions. Biochem Biophys Res Commun. 2007;360(1):286–9. https://doi.org/10.1016/j.bbrc.2007.06.057.
Huang S, Wang J, Men H, et al. Cardiac metallothionein overexpression rescues diabetic cardiomyopathy in Akt2-knockout mice. J Cell Mol Med. 2021;25(14):6828–40. https://doi.org/10.1111/jcmm.16687.
Gu J, Yan X, Dai X, et al. Metallothionein preserves Akt2 activity and cardiac function via inhibiting TRB3 in diabetic hearts. Diabetes. 2018;67(3):507–17. https://doi.org/10.2337/db17-0219.
Gu J, Cheng Y, Wu H, et al. Metallothionein is downstream of Nrf2 and partially mediates sulforaphane prevention of diabetic cardiomyopathy. Diabetes. 2017;66(2):529–42. https://doi.org/10.2337/db15-1274.
Kobylecki CJ, Afzal S, Nordestgaard BG. Genetically low antioxidant protection and risk of cardiovascular disease and heart failure in diabetic subjects. EBioMedicine. 2015;2(12):2010–5. https://doi.org/10.1016/j.ebiom.2015.11.026.
Gao YH, Li CX, Shen SM, et al. Hypoxia-inducible factor 1alpha mediates the down-regulation of superoxide dismutase 2 in von Hippel-Lindau deficient renal clear cell carcinoma. Biochem Biophys Res Commun. 2013;435(1):46–51. https://doi.org/10.1016/j.bbrc.2013.04.034.
Bohuslavova R, Kolar F, Sedmera D, et al. Partial deficiency of HIF-1alpha stimulates pathological cardiac changes in streptozotocin-induced diabetic mice. BMC Endocr Disord. 2014;14:11. https://doi.org/10.1186/1472-6823-14-11.
Gao Q, Guan L, Hu S, et al. Study on the mechanism of HIF1a-SOX9 in glucose-induced cardiomyocyte hypertrophy. Biomed Pharmacother. 2015;74:57–62. https://doi.org/10.1016/j.biopha.2015.07.009.
Huang YT, Liu CH, Yang YC, et al. ROS- and HIF1alpha-dependent IGFBP3 upregulation blocks IGF1 survival signaling and thereby mediates high-glucose-induced cardiomyocyte apoptosis. J Cell Physiol. 2019;234(8):13557–70. https://doi.org/10.1002/jcp.28034.
Packer M. Mechanisms leading to differential hypoxia-inducible factor signaling in the diabetic kidney: modulation by SGLT2 inhibitors and hypoxia mimetics. Am J Kidney Dis. 2021;77(2):280–6. https://doi.org/10.1053/j.ajkd.2020.04.016.
Kondo K, Ishigaki Y, Gao J, et al. Bach1 deficiency protects pancreatic beta-cells from oxidative stress injury. Am J Physiol Endocrinol Metab. 2013;305(5):E641–8. https://doi.org/10.1152/ajpendo.00120.2013.
Yan B, Jiao S, Zhang HS, et al. Prolyl hydroxylase domain protein 3 targets Pax2 for destruction. Biochem Biophys Res Commun. 2011;409(2):315–20. https://doi.org/10.1016/j.bbrc.2011.05.012.
Li CL, Liu B, Wang ZY, et al. Salvianolic acid B improves myocardial function in diabetic cardiomyopathy by suppressing IGFBP3. J Mol Cell Cardiol. 2020;139:98–112. https://doi.org/10.1016/j.yjmcc.2020.01.009.
Lai J, Chen F, Chen J, et al. Overexpression of decorin promoted angiogenesis in diabetic cardiomyopathy via IGF1R-AKT-VEGF signaling. Sci Rep. 2017;7:44473. https://doi.org/10.1038/srep44473.
Ramakrishnan S, Anand V, Roy S. Vascular endothelial growth factor signaling in hypoxia and inflammation. J Neuroimmune Pharmacol. 2014;9(2):142–60. https://doi.org/10.1007/s11481-014-9531-7.
Lu H, Fedak PW, Dai X, et al. Integrin-linked kinase expression is elevated in human cardiac hypertrophy and induces hypertrophy in transgenic mice. Circulation. 2006;114(21):2271–9. https://doi.org/10.1161/CIRCULATIONAHA.106.642330.
Wicik Z, Nowak A, Jarosz-Popek J, et al. Characterization of the SGLT2 interaction network and its regulation by SGLT2 inhibitors: a bioinformatic analysis. Front Pharmacol. 2022;13:901340. https://doi.org/10.3389/fphar.2022.901340.
Gupte M, Umbarkar P, Lal H. Mechanistic insights of empagliflozin-mediated cardiac benefits: nearing the starting line : editorial to: "Empagliflozin improves left ventricular diastolic dysfunction in a genetic model of type 2 diabetes" by N. Hammoudi et al. Cardiovasc Drugs Ther. 2017;31(3):229–32. https://doi.org/10.1007/s10557-017-6741-2.
Min W, Bin ZW, Quan ZB, Hui ZJ, Sheng FG. The signal transduction pathway of PKC/NF-kappa B/c-fos may be involved in the influence of high glucose on the cardiomyocytes of neonatal rats. Cardiovasc Diabetol. 2009;8:8. https://doi.org/10.1186/1475-2840-8-8.
Wang M, Zhang WB, Zhu JH, Fu GS, Zhou BQ. Breviscapine ameliorates hypertrophy of cardiomyocytes induced by high glucose in diabetic rats via the PKC signaling pathway. Acta Pharmacol Sin. 2009;30(8):1081–91. https://doi.org/10.1038/aps.2009.95.
Radovits T, Korkmaz S, Matyas C, et al. An altered pattern of myocardial histopathological and molecular changes underlies the different characteristics of type-1 and type-2 diabetic cardiac dysfunction. J Diabetes Res. 2015;2015:728741. https://doi.org/10.1155/2015/728741.
Oh CC, Lee J, D'Souza K, et al. Activator protein-1 and caspase 8 mediate p38alpha MAPK-dependent cardiomyocyte apoptosis induced by palmitic acid. Apoptosis. 2019;24(5-6):395–403. https://doi.org/10.1007/s10495-018-01510-y.
Zhu N, Huang B, Zhu L, Wang Y. Potential mechanisms of triptolide against diabetic cardiomyopathy based on network pharmacology analysis and molecular docking. J Diabetes Res. 2021;2021:9944589. https://doi.org/10.1155/2021/9944589.
Wernig G, Chen SY, Cui L, et al. Unifying mechanism for different fibrotic diseases. Proc Natl Acad Sci USA. 2017;114(18):4757–62. https://doi.org/10.1073/pnas.1621375114.
Wrann CD, Rosen ED. New insights into adipocyte-specific leptin gene expression. Adipocyte. 2012;1(3):168–72. https://doi.org/10.4161/adip.20574.
Wrann CD, Eguchi J, Bozec A, et al. FOSL2 promotes leptin gene expression in human and mouse adipocytes. J Clin Invest. 2012;122(3):1010–21. https://doi.org/10.1172/JCI58431.
Li J, Li S, Hu Y, et al. The expression level of mRNA, protein, and DNA methylation status of FOSL2 of Uyghur in XinJiang in type 2 diabetes. J Diabetes Res. 2016;2016:5957404. https://doi.org/10.1155/2016/5957404.
Liang Y, Yuan W, Zhu W, et al. Macrophage migration inhibitory factor promotes expression of GLUT4 glucose transporter through MEF2 and Zac1 in cardiomyocytes. Metabolism. 2015;64(12):1682–93. https://doi.org/10.1016/j.metabol.2015.09.007.
Wang J, Tong C, Yan X, et al. Limiting cardiac ischemic injury by pharmacological augmentation of macrophage migration inhibitory factor-AMP-activated protein kinase signal transduction. Circulation. 2013;128(3):225–36. https://doi.org/10.1161/CIRCULATIONAHA.112.000862.
Zhang D, Golubkov VS, Han W, et al. Identification of Annexin A4 as a hepatopancreas factor involved in liver cell survival. Dev Biol. 2014;395(1):96–110. https://doi.org/10.1016/j.ydbio.2014.08.025.
Monkemann H, De Vriese AS, Blom HJ, et al. Early molecular events in the development of the diabetic cardiomyopathy. Amino Acids. 2002;23(1-3):331–6. https://doi.org/10.1007/s00726-001-0146-y.
Kitada K, Nakano D, Ohsaki H, et al. Hyperglycemia causes cellular senescence via a SGLT2- and p21-dependent pathway in proximal tubules in the early stage of diabetic nephropathy. J Diabetes Complications. 2014;28(5):604–11. https://doi.org/10.1016/j.jdiacomp.2014.05.010.
Almeida De Oliveira A, Faustino J, Pedrosa Nunes KJH. Abstract P190: transcriptomic data analysis reveals sex-related differences in the interplay between toll-like receptor 4 and heat-shock protein 70 in the aorta of type 2 diabetic donors. Hypertension. 2019;74(Suppl_1):AP190-AP. https://doi.org/10.1161/hyp.74.suppl_1.P190.
Fiorese CJ, Schulz AM, Lin YF, et al. The transcription factor ATF5 mediates a mammalian mitochondrial UPR. Curr Biol. 2016;26(15):2037–43. https://doi.org/10.1016/j.cub.2016.06.002.
Juliana CA, Yang J, Rozo AV, et al. ATF5 regulates beta-cell survival during stress. Proc Natl Acad Sci USA. 2017;114(6):1341–6. https://doi.org/10.1073/pnas.1620705114.
Pei-Yuan Z, Yu-Wei L, Xiang-Nan Z, et al. Overexpression of Axl reverses endothelial cells dysfunction in high glucose and hypoxia. J Cell Biochem. 2019;120(7):11831–41. https://doi.org/10.1002/jcb.28462.
Wu W, Xu H, Meng Z, et al. Axl is essential for in-vitro angiogenesis induced by vitreous from patients with proliferative diabetic retinopathy. Front Med (Lausanne). 2021;8:787150. https://doi.org/10.3389/fmed.2021.787150.
Su SC, Chiang CF, Hsieh CH, et al. Growth arrest-specific 6 modulates adiponectin expression and insulin resistance in adipose tissue. J Diabetes Investig. 2021;12(4):485–92. https://doi.org/10.1111/jdi.13412.
Arai H, Nagai K, Doi T. Role of growth arrest-specific gene 6 in diabetic nephropathy. Vitam Horm. 2008;78:375–92. https://doi.org/10.1016/S0083-6729(07)00015-5.
Ljubimov AV, Burgeson RE, Butkowski RJ, et al. Basement membrane abnormalities in human eyes with diabetic retinopathy. J Histochem Cytochem. 1996;44(12):1469–79. https://doi.org/10.1177/44.12.8985139.
Burlina S, Banfi C, Brioschi M, et al. Is the placental proteome impaired in well-controlled gestational diabetes? J Mass Spectrom. 2019;54(4):359–65. https://doi.org/10.1002/jms.4336.
Zhang Y, Cui L, Guan G, et al. Matrine suppresses cardiac fibrosis by inhibiting the TGF-beta/Smad pathway in experimental diabetic cardiomyopathy. Mol Med Rep. 2018;17(1):1775–81. https://doi.org/10.3892/mmr.2017.8054.
Malek V, Gaikwad AB. Telmisartan and thiorphan combination treatment attenuates fibrosis and apoptosis in preventing diabetic cardiomyopathy. Cardiovasc Res. 2019;115(2):373–84. https://doi.org/10.1093/cvr/cvy226.
Che H, Wang Y, Li Y, et al. Inhibition of microRNA-150-5p alleviates cardiac inflammation and fibrosis via targeting Smad7 in high glucose-treated cardiac fibroblasts. J Cell Physiol. 2020;235(11):7769–79. https://doi.org/10.1002/jcp.29386.
Frangogiannis NG. Cardiac fibrosis. Cardiovasc Res. 2021;117(6):1450–88. https://doi.org/10.1093/cvr/cvaa324
Wang Y, Yu K, Zhao C, et al. Follistatin attenuates myocardial fibrosis in diabetic cardiomyopathy via the TGF-beta-Smad3 pathway. Front Pharmacol. 2021;12:683335. https://doi.org/10.3389/fphar.2021.683335.
Dong L, Li JC, Hu ZJ, et al. Deletion of Smad3 protects against diabetic myocardiopathy in db/db mice. J Cell Mol Med. 2021;25(10):4860–9. https://doi.org/10.1111/jcmm.16464.
Panchapakesan U, Pegg K, Gross S, et al. Effects of SGLT2 inhibition in human kidney proximal tubular cells--renoprotection in diabetic nephropathy? PLoS One. 2013;8(2):e54442. https://doi.org/10.1371/journal.pone.0054442.
Xu H, Qing T, Shen Y, et al. RNA-seq analyses the effect of high-salt diet in hypertension. Gene. 2018;677:245–50. https://doi.org/10.1016/j.gene.2018.07.069.
Gallini R, Lindblom P, Bondjers C, Betsholtz C, Andrae J. PDGF-A and PDGF-B induces cardiac fibrosis in transgenic mice. Exp Cell Res. 2016;349(2):282–90. https://doi.org/10.1016/j.yexcr.2016.10.022.
Ye Y, Jia X, Bajaj M, Birnbaum Y. Dapagliflozin attenuates Na(+)/H(+) exchanger-1 in cardiofibroblasts via AMPK activation. Cardiovasc Drugs Ther. 2018;32(6):553–8. https://doi.org/10.1007/s10557-018-6837-3.
Acknowledgements
We would like to thank Hsiu-Chiung Yang and Stefano Bartesaghi for the administrative management of the collaboration. We would like to thank the NGS Core facility of the University of Texas for the generation and pre-processing of the RNA-sequencing experiment.
Funding
This research has been funded by AstraZeneca. The first author is an AstraZeneca employee and had direct involvement in the data analysis, interpretation, and planning of the follow-up experiments.
Author information
Authors and Affiliations
Contributions
M.R.—computational analysis of RNA-seq data, hypotheses for follow-up experiments, and first manuscript draft. Y.Y. and Y.B.—study design, in vivo experiments, RT-PCR, and protein quantification. R.Y—literature search, data analysis, and editing the manuscript. All authors contributed to data interpretation, revised the manuscript, and approved the final version.
Corresponding author
Ethics declarations
Conflict of Interest
M.R. is an employee of AstraZeneca and may hold company shares/stocks. Y.Y. and Y. B. received the research grant from AstraZeneca.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(XLSX 6130 kb)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ryaboshapkina, M., Ye, R., Ye, Y. et al. Effects of Dapagliflozin on Myocardial Gene Expression in BTBR Mice with Type 2 Diabetes. Cardiovasc Drugs Ther (2023). https://doi.org/10.1007/s10557-023-07517-1
Accepted:
Published:
DOI: https://doi.org/10.1007/s10557-023-07517-1