Abstract
Purpose
A substantial percentage of patients report intolerance or side effects of statin treatment leading to treatment changes or discontinuation. The purpose of this study was to examine statin therapy changes and subsequent effects on low-density lipoprotein cholesterol (LDL-C) among patients with statin intolerance (SI).
Methods
We identified 45,037 adults from Kaiser Permanente Southern California with SI documented between 2006 and 2012. Changes in statin therapy in the year before and after the SI index date were examined. We categorized patients into those who initiated statin therapy, discontinued, up-titrated, down-titrated, or did not switch therapy. We calculated the percentage change in LDL-C from the year before to the year after SI, and the percentage of patients attaining LDL-C < 100 and < 70 mg/dL.
Results
In the year prior to the SI date, 77.8% of patients filled a statin prescription. Following SI, 44.6% had no treatment change, 25.5% discontinued, and 30.0% altered their statin therapy. Of those who altered statin therapy, 52.6% down-titrated and 17.2% up-titrated their dose. Rhabdomyolysis was documented in < 1% of the cohort. The largest changes in LDL-C were experienced by patients who were on a high-intensity statin then discontinued treatment (35.6% increase) and those who initiated a high-intensity statin (25.5% decrease). The proportion of patients achieving LDL-C < 100 mg/dL and LDL-C < 70 mg/dL was the lowest among those who discontinued therapy.
Conclusions
Although adjustments to the statin dosage may be appropriate upon documentation of SI, many of these patients will have high LDL-C. Strategies for LDL-C reduction in patients with SI may be necessary.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Statins are commonly prescribed for adults with elevated low-density lipoprotein cholesterol (LDL-C) and those with high cardiovascular (CV) disease risk to reduce the occurrence of CV events [1]. Although statins are usually well tolerated [2], a substantial percentage of patients report experiencing some degree of intolerance or side effects including muscle aches, dyspepsia, and myopathy, in turn, leading to treatment changes or discontinuation and an unmet treatment need [3,4,5]. Data from patient registries and observational studies indicate that 7 to 29% of statin users report muscle-related symptoms [6]. The prevalence of life-threatening muscular adverse events such as rhabdomyolysis among patients receiving statin therapy, however, is rare (< 1%) [7]. In addition, the relationship between statin therapy and a particular symptom can be difficult to determine in the absence of a thorough clinical examination and documentation of the temporality of symptoms relative to statin initiation [3, 8].
There is no universally agreed upon definition of statin intolerance (SI) [9]. Definitions of SI include statin-associated muscle symptoms (SAMS), statin-induced adverse effects, and the inability to achieve evidence-based doses of statin therapy [10,11,12]. SI may encompass life-threating adverse events like rhabdomyolysis and intolerable SAMS on low statin doses as well as more mild symptoms that may only occur on specific statins or specific doses. The 2013 American College of Cardiology/American Heart Association guidelines recommend that patients with SI be prescribed a lower dose of the same statin or a different statin type [13]. Other approaches to managing patients with SI include changing the dosing interval [14], the addition of non-statin lipid-lowering therapy, or dietary interventions [3]. Given the lack of evidence-based clinical guidelines for managing statin-intolerant patients [8] and an anticipated increase in statin use as a result of broader eligibility criteria [15], understanding statin treatment patterns among patients with SI can inform healthcare providers about the potential unmet need for treatment. The objective of this study was to examine statin treatment patterns, therapy changes, and LDL-C lowering following documentation of SI in a real-world practice setting.
Methods
Setting and Study Population
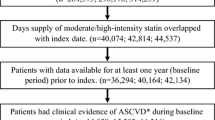
This study was conducted among members of Kaiser Permanente Southern California (KPSC), a large, integrated healthcare delivery system that provides comprehensive care for more than four million members. The KPSC membership is highly representative of the overall Southern California population [16]. Data on medical care are captured through structured administrative and clinical databases and electronic health records (EHR). Most KPSC members (> 95% in recent years) have outpatient prescription drug coverage which gives them the incentive to fill prescriptions at KPSC pharmacies; thus, the majority of statin prescriptions among patients in the current study were captured. Among all KPSC members, we identified 51,347 patients who were aged ≥ 18 years with SI documented in their EHR by a physician between January 1, 2006 and December 31, 2012. Statin intolerance was identified when the name of a statin was listed in the allergy section of the EHR and through a search of the patient problem list for the term “statin.” The first SI date documented within the study period, or January 1, 2006 for patients with SI documented prior to the study period, was used as the index date. Patients without 12 months of continuous membership or a drug benefit before their index date were excluded (n = 6310). After exclusions, a total of 45,037 individuals remained in the cohort (Fig. 1).
Baseline Patient Characteristics
We extracted patient demographics, comorbidities, pharmacy, and laboratory data from administrative and clinical databases and the EHR. Baseline characteristics of the study population were defined based on data closest to the index date in the 12 months prior to and including the index date. These included sociodemographics (age, sex, and race/ethnicity), body mass index, blood pressure, Charlson Comorbidity Index (hypertension, myocardial infarction (MI), congestive heart failure, peripheral vascular disease, cerebrovascular disease, chronic pulmonary disease, renal disease, diabetes), CV-related comorbidities, rhabdomyolysis, myopathy, number of concomitant medications, cholesterol levels, creatine kinase (CK), and alanine aminotransferase (ALT). Use of statins (including combinations) and other lipid-lowering agents was identified by the sold date of the prescription and was assessed during the baseline period and 12 months following the SI index date, or until disenrollment or death.
Statistical Analysis
We examined the distribution of the type and dose of the last statin filled in the year before SI was documented and the first statin filled on the index date or within the year after SI was documented. We calculated the percentage of patients not on a statin and the percentage on high-, moderate-, and low-intensity statin therapy pre- and post-SI index date. We also examined the percent of patients with a change in the intensity of their statin medication in the year before SI. Statin intensity (Supplemental Table 1) was categorized by daily dose according to the 2013 American College of Cardiology/American Heart Association Cholesterol guidelines [17]. We then calculated the percentage of patients who initiated statin therapy (i.e., no statin therapy within 1 year prior to index date), discontinued, down-titrated, up-titrated, or did not change therapy in the year after the documented SI. Patients who disenrolled from the health plan within the year post-SI index date were included in the discontinued group. Baseline patient characteristics across these groups were examined. The distribution of triglycerides, CK, and ALT levels was highly skewed; therefore, we calculated medians and interquartile ranges for these variables. We calculated the mean percentage change of LDL-C from baseline to 1 year after the SI date, and the percentage of patients attaining LDL-C of < 100 and < 70 mg/dL by the post-SI treatment pattern groups. To provide the most proximate LDL-C result for patients who initiated, discontinued (or disenrolled during follow-up), or switched statin therapy, we used the first LDL-C measurement between 30 days and 1 year following the statin initiation, discontinuation, or switch date. For patients who did not switch therapy, we used the last LDL-C measurement between 60 days and 1 year after the index date. A large proportion of patients who did not switch therapy had an LDL-C measurement on the index date; therefore, using the measurement between 60 days and 1 year allowed ample time to observe a change in LDL-C. If a patient did not have an LDL-C value in the post-SI period, they were not included in the LDL-C analyses (n = 9426).
The study protocol was reviewed and approved by the KPSC Institutional Review Board, and a waiver for written informed consent was obtained due to the nature of the study. Compliance with Health Insurance Portability and Accountability Act (HIPAA) regulations was ensured.
Results
Among the 45,037 patients in the cohort, 35,059 (77.8%) filled a statin prescription in the year prior to the index date. Of these patients, 18.9, 59.3, and 21.9% received a high, moderate, and low-intensity statin, respectively (Table 1). In addition, 85.1% of those who filled their statin prescription had no previous changes to the intensity of their statin medication in the year before SI. Among those taking a statin prior to documentation of SI, 40.4% of patients had no change in statin treatment, 32.7% discontinued treatment, 20.3% down-titrated, and 6.6% up-titrated their statin medication following the SI date.
Across the entire cohort (n = 45,037), 44.6% of patients had no treatment change, and 25.5 and 30.0% discontinued and changed their statin therapy, respectively (Table 2). Of those whose statin therapy changed following SI, 52.6% down-titrated and 17.2% up-titrated their dose, and 30.1% were newly started on a statin although they have may been taking a statin prior to the 1-year look-back period. The majority of patients (59.8%) in the cohort were female, the mean age was 63.4 (11.6) years, 0.9% had a history of rhabdomyolysis, and 4.1% had mild liver disease (Table 2). Those who discontinued statin therapy were more likely to have a diagnosis of rhabdomyolysis and myopathy, and were less likely to have a history of MI than patients with changes to their statin medication. Although most patients did not have a CK measure in the year prior to SI, among those with a measurement, patients who discontinued statin therapy had a higher median CK (116, IQR 72–233 IU/L); however, the value was within the normal reference range. The median ALT values were also within normal range and did not vary across the groups. Additional baseline characteristics are presented in Supplemental Table 2. The use of other lipid-lowering agents in the year prior to the SI index date was 13.8% and was highest among patients who were newly started on a statin with 8.7% receiving a cholesterol absorption inhibitor such as ezetimibe (Table 3). Within the year following the SI index date, 24.9% of all patients filled a prescription for a non-statin lipid-lowering agent. Use of cholesterol absorption inhibitors increased from 5.5 to 11.1% between the pre- and post-SI index date and was highest (15.4%) among patients who discontinued their statin following the SI index date.
Figure 2 shows the percent change in LDL-C from pre- to post-SI index date by statin intensity treatment pattern groups. The largest percentage increases in LDL-C levels were among patients who were on a high-intensity statin then either discontinued (35.6% increase) or switched to a low-intensity statin (18.9% increase). In contrast, patients who newly initiated therapy and those who up-titrated had the largest mean percentage reductions in LDL-C, ranging from a reduction of 12.2% among patients who were up-titrated from a low- to medium-intensity statin to a 25.5% reduction among patients who initiated a high-intensity statin. Figure 3 shows the proportion of patients with LDL-C of < 100 and < 70 mg/dL by statin intensity treatment pattern groups. The proportion of patients with LDL-C < 100 mg/dL was highest (60.4%) among those who remained on a high-intensity statin after the SI date. The proportion of patients with LDL-C < 70 mg/dL was highest (26.7%) in those who were up-titrated from a low- to high-intensity statin. Patients who discontinued statin therapy had the lowest percentage achieving LDL-C < 100 mg/dL and LDL-C < 70 mg/dL. Fewer than half of patients who down-titrated their statin dose achieved LDL-C < 100 mg/dL and < 8% achieved LDL-C < 70 mg/dL.
LDL-C goal attainment among statin-intolerant patients after a change in statin therapy. An asterisk indicates that LDL-C was measured between 30 days and 1 year after the statin switch date. The first LDL-C in this time period was used for individuals with multiple LDL-C measures. Double asterisks indicate that LDL-C was measured between 60 days and 1 year after the statin intolerance date. The last LDL-C in this time period was used for individuals with multiple LDL-C measures. NS-NS, no statin to no statin; High, high-intensity statin; Med, medium-intensity statin; Low, low-intensity statin; Disc, discontinued statin; NS, no switch in statin therapy
Discussion
The majority of patients in this study cohort who filled a statin prescription in the year prior to SI either discontinued or down-titrated the treatment following documented SI. A small percentage of patients in our study were re-challenged with a second statin in the year prior to SI, and few had a diagnosis of rhabdomyolysis or measurement of CK levels. Further, among patients with a CK measurement, the median values were not abnormally elevated. The largest proportion of patients with LDL-C < 100 mg/dL was among those who remained on a high-intensity statin after the SI date while less than half of patients who down-titrated their statin dose achieved LDL-C < 100 mg/dL.
A review of evidence from randomized controlled trials regarding the safety and efficacy of statin therapy indicates that tolerance of statins is similar to placebo thus the beneficial effects of treatment outweigh the adverse effects [18]. In addition, a meta-analysis of 18 clinical trials showed the prevalence of serious adverse events among statin users to be rare [19]. Similarly, the prevalence of rhabdomyolysis was low in our study. A study conducted among 63,624 patients at high risk for CV disease morbidity and mortality in an integrated healthcare system found that 0.5% of patients had a history of rhabdomyolysis with statin use [20]. This finding is lower than the prevalence in our study which was conducted among more than 45,000 patients in a similar healthcare delivery system; however, we only selected patients with SI and did not limit our study to patients at high risk of CV disease. The higher prevalence of rhabdomyolysis in our cohort might be attributed to the fact that the majority of patients were current statin users. Few patients in our study had a CK measurement in the year prior to SI being documented. This finding suggests that patients may report symptoms associated with SI which may lead physicians to document this information in the EHR in the absence of biomarkers used to assess statin-associated adverse effects.
The finding that a large number of patients in our study discontinued statin therapy is consistent with a study conducted at the Cleveland Clinic between 1995 and 2010 among patients with documented intolerance to two statins and at least 6 months of lipid-lowering therapy use [21]. Over a nearly 3-year follow-up period, 28% of patients discontinued statin therapy after documentation of SI although there was more use of non-prescription drugs than the daily statin dosing group. These patients experienced an 8% reduction in LDL-C. In comparison, patients in our study who discontinued statin treatment, on average experienced an increase in LDL-C; however, a larger proportion of patients in the Cleveland Clinic study had concomitant use of other lipid-lowering drugs which may have resulted in the reductions seen in that study versus our study. In our study, the proportion of patients receiving a non-statin lipid-lowering agent nearly doubled between the pre- and post-SI date suggesting that clinicians perceive an unmet need for additional LDL-C lowering. Using a non-statin lipid-lowering drug is an alternative to statin use for SI patients [3, 22]. Patients who discontinued statin treatment in our study were less likely to have a history of MI than patients who switched to a different statin after SI. A study of 10,138 adults who completed the Internet-based Understanding Statin Use in America and Gaps in Patient Education (USAGE) Survey found that respondents who discontinued statin therapy were less likely to have CV disease than those who switched statins [4]. Not having a history of MI may provide patients and providers with a sense of lower risk for CV events and thus an increased confidence in discontinuing statin use.
A substantial proportion of patients in our study did not achieve LDL-C < 100 mg/dL across all groups. Although attainment of LDL-C < 100 mg/dL was highest among patients who remained on a high-intensity statin and those who were up-titrated to a high-intensity statin after the SI date, fewer than 60% of patients in any statin treatment group achieved this previously recommended treatment goal. Studying the clinical and economic consequences of SI compared with a matched cohort of statin users without SI in an integrated US health system from 2008 through 2014, Graham and colleagues found 60% of SI patients not achieving LDL-C goal [23]. In addition, SI patients had a higher risk for non-fatal CV events and higher health care costs highlighting the need for alternative lipid management options. Zhang et al. conducted a retrospective cohort study to assess the association between continued statin use following a presumed adverse reaction to a statin and subsequent death, MI, or stroke among 22,266 patients [5]. Similar to our study, 30% of patients discontinued statin therapy after the presumed adverse reaction. Moreover, the incidence of CV events and death was 10–20% lower among patients who continued statin therapy during an average of 4 years of follow-up time. In a cohort study of Medicare recipients who began statin therapy within 30 days of hospital discharge for MI, incidence rates of CV events and death were determined for those with SI compared to patients with high adherence to statins [24]. Between 2007 and 2014, SI was not associated with an increased risk of death; however, the incidence rate for recurrent MI and coronary heart disease events was significantly higher for patients with SI. The findings from these studies strongly suggest that patients have an unmet need for further reductions in LDL-C and CV events.
Our study has a number of limitations. First, this study was limited to EHR data from a single health plan where the majority of patients have a drug benefit. As such, its findings may not be generalizable to other populations, such as uninsured populations. Second, no direct contact was made with patients or providers to determine the reason for SI being documented or the reason for discontinuation of statin therapy; therefore, we are unable to determine specific barriers to managing patient with adverse effects to statins. Third, a patient could have had SI prior to the study period or enrollment in the health plan which could be a reason patients may have not been taking a statin within the year prior to cohort entry although they may have been re-challenged with a statin post-index date. The primary advantage of our study is that it was conducted in a large, diverse population in a real-world clinical setting. Use of an EHR also allows complete capture of laboratory results, comorbidities, and prescription patterns. To our knowledge, only one other study examining SI using an EHR has reported laboratory measures relevant to SI, changes in LDL-C, patients’ medical history, and statin treatment patterns. Lastly, our study included all patients with documented SI; thus, our results provide a broader view of statin treatment patterns, therapy changes, and LDL-C lowering than studies limited to patients with CV disease.
Conclusions
In this patient population, a small proportion of those with documented SI also had a diagnosis of rhabdomyolysis. A large proportion of patients, however, discontinued or down-titrated their statin medication. These same patients also experienced an increase in LDL-C levels. Adjustments to the statin dosage may be appropriate upon documentation of SI; however, limited guideline recommendations for statin-intolerant patients may result in non-evidence-based practices. Additional interventions to help overcome SI, such as prescribing an alternative appropriate statin and rechallenging a patient with the same statin, and reduce LDL-C have the potential to facilitate further reduction in CV risk.
References
Stone NJ, Robinson JG, Lichtenstein AH, Bairey Merz CN, Blum CB, Eckel RH, et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63(25 Pt B):2889–934.
Baigent C, Keech A, Kearney PM, Blackwell L, Buck G, Pollicino C, et al. Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90,056 participants in 14 randomised trials of statins. Lancet. 2005;366(9493):1267–78.
Rosenson RS, Baker SK, Jacobson TA, Kopecky SL, Parker BA. An assessment by the Statin Muscle Safety Task Force: 2014 update. J Clin Lipidol. 2014;8(3 Suppl):S58–71.
Wei MY, Ito MK, Cohen JD, Brinton EA, Jacobson TA. Predictors of statin adherence, switching, and discontinuation in the USAGE survey: understanding the use of statins in America and gaps in patient education. J Clin Lipidol. 2013;7(5):472–83.
Zhang H, Plutzky J, Shubina M, Turchin A. Continued statin prescriptions after adverse reactions and patient outcomes: a cohort study. Ann Intern Med. 2017;167(4):221–7.
Stroes ES, Thompson PD, Corsini A, Vladutiu GD, Raal FJ, Ray KK, et al. Statin-associated muscle symptoms: impact on statin therapy—European Atherosclerosis Society Consensus Panel Statement on Assessment, Aetiology and Management. Eur Heart J. 2015;36(17):1012–22.
Rosenson RS. Current overview of statin-induced myopathy. Am J Med. 2004;116(6):408–16.
Rosenson RS, Baker S, Banach M, Borow KM, Braun LT, Bruckert E, et al. Optimizing cholesterol treatment in patients with muscle complaints. J Am Coll Cardiol. 2017;70(10):1290–301.
Banach M, Rizzo M, Toth PP, Farnier M, Davidson MH, Al-Rashidi K, et al. Statin intolerance—an attempt at a unified definition. Position paper from an International Lipid Expert Panel. Arch Med Sci. 2015;11(1):1–23.
Hovingh GK, Gandra SR, McKendrick J, Dent R, Wieffer H, Catapano A, et al. Identification and management of patients with statin-associated symptoms in clinical practice: a clinician survey. Atherosclerosis. 2016;245:111–7.
Kopecky S, Baum S, Foody JM, et al. Insights into statin intolerance. Clin Cardiol. 2015;38(9):520–6.
Tompkins R, Schwartzbard A, Gianos E, Fisher E, Weintraub H. A current approach to statin intolerance. Clin Pharmacol Ther. 2014;96(1):74–80.
Stone NJ, Robinson JG, Lichtenstein AH, Goff DC Jr, Lloyd-Jones DM, Smith SC Jr, et al. Treatment of blood cholesterol to reduce atherosclerotic cardiovascular disease risk in adults: synopsis of the 2013 American College of Cardiology/American Heart Association cholesterol guideline. Ann Intern Med. 2014;160(5):339–43.
Awad K, Mikhailidis DP, Toth PP, Jones SR, Moriarty P, Lip GYH, et al. Efficacy and safety of alternate-day versus daily dosing of statins: a systematic review and meta-analysis. Cardiovasc Drugs Ther. 2017;31(4):419–31.
Pencina MJ, Navar-Boggan AM, D’Agostino RB Sr, Williams K, Neely B, Sniderman AD, et al. Application of new cholesterol guidelines to a population-based sample. N Engl J Med. 2014;370(15):1422–31.
Koebnick C, Langer-Gould AM, Gould MK, Chao CR, Iyer RL, Smith N, et al. Sociodemographic characteristics of members of a large, integrated health care system: comparison with US Census Bureau data. Perm J. 2012;16(3):37–41.
Goff DC Jr, Lloyd-Jones DM, Bennett G, Coady S, D’Agostino RB Sr, Gibbons R, et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63(25 Pt B):2935–59.
Collins R, Reith C, Emberson J, Armitage J, Baigent C, Blackwell L, et al. Interpretation of the evidence for the efficacy and safety of statin therapy. Lancet. 2016;388(10059):2532–61.
Silva MA, Swanson AC, Gandhi PJ, Tataronis GR. Statin-related adverse events: a meta-analysis. Clin Ther. 2006;28(1):26–35.
Saeed B, Wright E, Evans M, Lewis M, Steinbuhl S. Prevalence of statin intolerance in a high risk cohort and management strategies in contemporary cardiology. Clin Med Res. 2013;11(3):136.
Mampuya WM, Frid D, Rocco M, Huang J, Brennan DM, Hazen SL, et al. Treatment strategies in patients with statin intolerance: the Cleveland Clinic experience. Am Heart J. 2013;166(3):597–603.
Kones R, Rumana U. Current treatment of dyslipidemia: evolving roles of non-statin and newer drugs. Drugs. 2015;75(11):1201–28.
Graham JH, Sanchez RJ, Saseen JJ, Mallya UG, Panaccio MP, Evans MA. Clinical and economic consequences of statin intolerance in the United States: results from an integrated health system. J Clin Lipidol. 2017;11(1):70–79 e71.
Serban MC, Colantonio LD, Manthripragada AD, Monda KL, Bittner VA, Banach M, et al. Statin intolerance and risk of coronary heart events and all-cause mortality following myocardial infarction. J Am Coll Cardiol. 2017;69(11):1386–95.
Funding
This study was funded by a contractual agreement between the Southern California Permanente Medical Group and Amgen Corporation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Teresa N. Harrison, Jin-Wen Y. Hsu, Rong Wei, and Ronald D. Scott declare that they have no conflict of interest. Robert S. Rosenson has received research grants from Akcea, Amgen, Astra Zeneca, Medicines Company, and Regeneron, speaker honorarium from Kowa and Pfizer, royalties from UpToDate, and is a member of advisory boards for Amgen, C5, CVS Caremark, Easy Vitals, Regneron, and Sanofi. Emily B. Levitan has received research funding from Amgen Inc., served on advisory boards for Amgen, and consulted for research projects funded by Novartis. T. Craig Cheetham has received research support from Bristol Myers-Squibb and Pfizer. Kristi Reynolds and Paul Muntner have received research support from Amgen.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of study, formal consent was not required.
Rights and permissions
About this article
Cite this article
Harrison, T.N., Hsu, JW.Y., Rosenson, R.S. et al. Unmet Patient Need in Statin Intolerance: the Clinical Characteristics and Management. Cardiovasc Drugs Ther 32, 29–36 (2018). https://doi.org/10.1007/s10557-018-6775-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10557-018-6775-0