Abstract
Discordance in estrogen (ER), progesterone (PR), and HER2/neu status between primary breast tumours and metastatic disease is well recognized. In this review, we highlight how receptor discordance between primary tumours and paired metastasis can help elucidate the mechanism of metastasis but can also effect patient management and the design of future trials. Discordance rates and ranges were available from 47 studies (3384 matched primary and metastatic pairs) reporting ER, PR, and HER2/neu expression for both primary and metastatic sites. Median discordance rates for ER, PR, and HER2/neu were 14 % (range 0–67 %, IQR 9–25 %), 21 % (range 0–62 %, IQR 15–41 %), and 10 % (range 0–44 %, IQR 4–17 %), respectively. Loss of receptor expression was more common (9.17 %) than gain (4.51 %). Discordance rates varied amongst site of metastasis with ER discordance being highest in bone metastases suggesting that discordance is a true biological phenomenon. Discordance rates vary for both the biomarker and the metastatic site. Loss of expression is more common than gain. This can affect patient management as it can lead to a reduction in both the efficacy and availability of potential therapeutic agents. Future studies are recommended to explore both the mechanisms of discordance as well as its impact on patient outcome and management.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Systemic treatment choices for metastatic breast cancer are based, in part, on the estrogen (ER), progesterone (PR), and HER2/neu status of the primary cancer. Biopsy of first recurrence is recommended in some but not all guidelines [1–3] and, outside of the clinical trial setting, it is difficult to tell how often biopsies are performed. Biopsies may not routinely offered for a number of reasons: physicians may assume that patients will be inconvenienced by a biopsy, that the receptor profile of the metastasis will be the same as the primary tumour, or that the results of the biopsy will not change patient management [4]. There is, however, an increasing body of literature challenges these assumptions.
1.1 Mechanisms of receptor discordance
Discordance of ER, PR, and Her2/neu status between the primary tumour and subsequent metastases is well recognized [5]; however, these can have both biological and therapeutic implications. Mechanisms of discordance remain unknown and could have both biologic and therapeutic implications. There are several potential explanations for these changes reported in the literature, including variability in assay performance (i.e. technical issues), tumour heterogeneity, and biologic evolution of the tumour (i.e. biological mechanisms)[6]. The accuracy and reliability of immunohistochemical testing is based on multiple factors, such as the method of tissue fixation, method of staining methods, antigen retrieval, and subjective scoring; all of which can have an effect in the final interpretation of the result affect [7–11]. In addition, it is well recognized that even when the same analytic method is used, the reproducibility is sub-optimal, especially for ER [38] and HER2/neu [3], again adding to possibly misleading discordance reporting. A recent publication was able to identify 15 pre-analytical variables that had the ability to affect immunohistochemical accuracy on formalin-fixed paraffin-embedded tissue [11]. There is also heterogeneity with respect to sampling methods. In addition, the differences in sampling methods such as fine-needle aspiration (FNA) or core biopsy versus surgical excision in the primary tumour and the differences in analysis of samples from different tissues are possible technical caveats that could cause a false concordance or discrepancy [12–15].
In addition to the technical issues described above, both inter- and intra-tumoural heterogeneity are emerging to be of greater incidence than previously appreciated. Recent studies based on next generation sequencing have shed new light on tumour heterogeneity, reinforcing the hypothesis that variation in biomarkers may actually reflect clonal genome evolution [5, 16–19]. Tumour heterogeneity may also be due to biological drift, selective pressures of therapy leading to clonal selection with development of a novel cell clone [20]. In addition, it is possible that there are small routinely undetected subclones in the primary that only become evident with metastatic progression [5, 19]. Along this line, as prospectively reported by Hilton and colleagues [21], a significant ER discordance rate between primary tumour and metastatic deposits occurred, and a full concordance amongst metastases arising in multiple bone sites, suggesting the occurrence of a dominant clone diverging in terms of ER immunoreactivity from the primary tumour. The clinical consequences of all these findings are as yet unknown, as well as the optimal timing for retesting a tumour.
In addition to these prospective studies, a meta-analysis has also been published [5]. To date, no studies have been able to elucidate the exact mechanism of observed this discordance. It is thought that these observations are either due to technical issues, such as poor reproducibility of immunohistochemistry, or actually a true biological manifestation. If discordance is a true biologic phenomenon, then we should expect similar discordance rates between metastatic sites as the biologic drivers of discordance (biological drift, selective pressure of therapy leading to clonal selection, or the presence of subclones undetectable in the primary tumour) [5] should be the same in all sites of metastatic disease. In contrast, differing rates of discordance between metastatic sites may reflect a technical issue as biopsies from different tissues require different preparation efforts, leading to significant technical variations.
In the absence of this data, we felt it would be useful to update a systematic review [5] and primarily focus on discordance rate variability between different sites of metastasis. The results of the systematic review have been presented elsewhere [22] and were conducted according to the guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Statement [23] and registered (CRD42013004564) in PROSPERO [24]. Studies that evaluated ER, PR, or HER2/neu receptor status in patient-matched primary breast and metastatic sites were included. Studies with a non-matched specimen between primary and metastatic site, undifferentiated data from different metastatic site, male breast cancer, non-original research, case reports of <5, and analysis conducted with methods other than immunohistochemistry/fluorescent in situ hybridization (IHC/FISH) were excluded. Studies comparing the primary site with concurrent axillary lymph nodes at the time of primary diagnosis were also excluded. We included studies of various analytical IHC or FISH techniques in receptor assessment.
Of the 7359 citations identified from the initial literature search, 47 met the eligibility criteria (Appendix 1). The detailed characteristics of the 47 studies (n = 3384 paired samples from primary tumours and corresponding metastases) are presented in Table 1. Only seven studies used prospectively collected data [21, 23–28]. For all 47 studies, the mean/median age of study subjects ranged from 45 to 64 years. Thirty-four studies reported on ER, 25 on PR, and 41 on HER2/neu. The number of studies including data for different sites of metastases was as follows: lymph nodes (n = 25), bone (n = 9), brain (n = 9), liver (n = 8), lung (n = 6), and GI tract (n = 1). Unfortunately, the quality of the studies was on the whole low (Supplemental Table 1 and 2). Of the 47 included studies, only five studies were judged to be of low risk of bias or applicability [27, 29–32]. It was often unclear from the studies whether the test results were interpreted without knowledge of the results from the primary disease or if the same tests were used to test the primary breast tumour and metastatic site or if all eligible patients were included in the analysis.
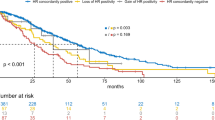
Total receptor discordance rate between primary tumour and metastatic site was assessed in 47 studies (3384 paired samples). Of these, 34 studies (1894 paired samples) assessed ER status, 25 studies (1213 paired samples) assessed PR status, and 41 studies (1828 paired samples) assessed HER2/neu receptor status. Total discordance rates are presented by metastatic site and all sites combined for each of three receptors in Fig. 1. Median discordance rates between primary and paired metastasis for ER, PR, and HER2/neu expressions were 14 % (range 0–67 %, IQR 9–25 %), 21 % (range 0–62 %, IQR 15–41 %), and 10 % (range 0–44 %, IQR 4–17 %), respectively.
Specific information regarding the direction of change in receptor expression (i.e. loss or gain of receptor) was available for a total of 1396 of the 3384 paired samples, respectively. Table 2 summarizes median percent change in the expression of ER, PR, and/or HER2/neu status by metastatic and all sites combined. From the available data, overall, 128/1396 (9.17 %) pairs had a loss of receptor status, while 63/1396 (4.51 %) match pairs had a gain of receptor status in the metastasis compared with primary tumour. For ER, 63/565 matched pairs (11.15 %) had a loss of receptor status while 15/565 matched pairs had a gain of receptor status. For PR, 24/267 (8.99 %) matched pairs had a loss of receptor status while 9/267 (2.62 %) had a gain of receptor status. For HER2/neu protein, 41/564 (7.27 %) matched pairs had a loss of receptor status, while 39/564 (6.91 %) have a gain of receptor status.
Discordance rates were highest for bone metastases [ER: 48 % (range 0–67 %), IQR (32–57 %); PR: 50 % (range 36), IQR (29–43 %); HER2/neu: 16 % (range 9–38), IQR (11–25 %)] when compared to all other sites (lymph node, lung, liver, brain, and gastrointestinal tract). At all sites, HER2/neu was less likely to show discordance than either ER or PR. Given that bone has unique technical issues that do not apply to other sites of metastases and the small number of samples for which data is available, a large amount of change observed from this site of disease may be spurious in nature. Thus given the high reproducibility of Her2/neu testing and the similar discordance rates between different sites of metastasis, where tissue processing is less variable, this data would therefore suggest that the mechanism of discordance is truly biological in nature at all sites, HER2/neu was less likely to show discordance than either ER or PR.
1.2 Impact of discordance on patient clinical and treatment outcomes
Prior to the BRIT and DESTINY studies, the majority of studies investigating biomarker discordance were small and retrospective in nature, with variable discordance ranges (minimum to maximum) for ER (7–32 %), PR (24–54 %), and HER2/neu (9–34 %), respectively [31, 33–40]. For a number of reasons, it is a major challenge to interpret the effects of receptor discordance on actual patient management. These reasons include the following: the recruitment of heterogeneous patient populations (from newly recurrent patients to patients with multiple previous metastasis), variability in the site of metastasis (e.g. bone vs. liver metastasis as outlined above), variations in the treatment the patient is receiving at the time of biopsy, variability in the assay used to measure the receptor, and lack of central pathology review [41].
The British BRIT study and the Canadian DESTINY study attempted to control for many of these limitations [42]. In order to increase the available data, the two studies were reported both individually and as a pooled analysis. For this pooled analysis, receptor discordance was defined as a change in ER, PR, or HER2 status (in any direction) between the primary tumour and the metastasis. This study reported receptor discordance rates for each biomarker as follows: ER 12 %, PR 31 %, and HER2/neu 5 %. In 14.2 % of cases, patients enrolled in the study had their management changed based on these biopsy results. Although the pooled analysis provided significant insights into receptor discordance in breast cancer, there were some important limitations to the work.
First, physicians enrolling patients in the biopsy study may be biased towards making treatment changes and therefore the effect of receptor discordance on treatment selection may be overstated. Second, switching therapies based on discordance may not actually have an effect on patient outcomes and only the DESTINY study explored this question. Seventeen woman (14 %; 95 % CI, 8.4 to 21.5 %) had a change in treatment compared with the pre-biopsy therapeutic plan. Changes in management included the addition of trastuzumab in women with gain of HER2 overexpression (n = 6), the use of chemotherapy in place of endocrine therapy in whose with loss of ER (n = 5), no change to previous treatment in those with benign disease or second primary (n = 4), and provision of endocrine therapy in place of chemotherapy for those gaining ER (n = 2).
Despite these findings, in the DESTINY study, discordance in receptors between the primary tumour and metastases was not associated with a difference in OS (median OS 27.6 and 30.2 months for the concordant and discordant groups, respectively; HR 0.94; 95 % CI, 0.49 to 0.85) [15]. Although, the evaluation was limited by the relatively small study numbers. Five other studies reported shorter survival for those with specific discordances [2, 31, 43–45]. Very few of the studies reported on treatments used for metastatic disease in these patients, and there was limited information on available baseline characteristics of the patients and their tumours from the reports. Interestingly, there have been reports that when there was a gain in the receptor status, 12–14.2 % of patients had a change in their treatment plan [36–38].
However, none compared outcomes for patients with receptor discordances whose systemic therapy for metastatic disease was guided by results from the metastases versus results from the primary tumour. Thus, evidence is lacking to determine the optimal basis for selecting a treatment regimen when discordances are found.
1.3 Impact of discordance on clinical trial design
Irrespective of the mechanism behind these changes, the impact on actual patient outcomes requires ongoing and future studies, particularly if we are to continue to individualize and improve treatment modalities in breast cancer. To help oncologists manage the clinical implications of biomarker discordance between the primary and metastatic sites, the American Society of Clinical Oncology (ASCO) Expert Panel recently published guidelines [6] on this specific topic. ASCO recommends that in patients with accessible metastases, biopsy for confirmation of malignancy and retesting of ER, PR, and HER2/neu status should be offered. With discordance of results between primary and metastatic tissues, the Panel consensus is to use preferentially the ER, PR, and HER2 status of the metastasis to direct therapy if supported by the clinical scenario and patient’s goals for care. The strength of these recommendations was noted to be “moderate”, as the evidence quality was “insufficient”. Although the Panel recognizes that there is sufficient evidence for biomarker change from primary to metastasis, there is no evidence to demonstrate that systemic therapy choices affect health outcomes when biomarker change occurs.
Interestingly, the ASCO guidelines specifically mention careful attention to assay performance in the retesting of biomarkers of bone metastases. The decalcification of bone biopsy material for the analysis of ER, PR, and HER2 may alter the outcome of the tumour analysis [46, 47]. Whenever possible, testing of bone metastases should be performed using a validated assay with a sample that has not been decalcified during preanalytic processing. Use of ethylenediaminetetraacetic acid-based decalcification solutions may help, as well as the ability to physically separate viable tumour from skeletal tissue, so that at least some of the tumour can be processed without having to undergo decalcification, although this may not be feasible for small biopsy specimens. A calcified specimen may yield a false negative result, and the Panel recommends that consideration should be given to an additional and more suitable biopsy sample for testing.
What are the downsides for performing an additional biopsy routinely in metastatic patients? A biopsy, even though it is often carried out by a percutaneous image guided technique, cannot always be performed safely for the patients. Complications do occur in the form of bleeding, infection, patient discomfort, perforation, and unintended organ injury [19]. The Society of Interventional Radiology reports a threshold of 2 % for major complications [48]. At the 2013 ASCO annual meeting, Dr. Andre reported that biopsy was complicated by a serious adverse event in 9 out of 423 patients within the SAFIR01 trial [49]. In addition, although it may be technically feasible to conduct biopsies at metastatic sites, approximately 20 % of biopsies cannot be analyse due to poor quality or insufficient cells, especially biopsies done with a fine needle aspirate or core biopsies of the bone or bone marrow [50]. Finally, it has to be acknowledged that routine additional biopsies may be financially costly for the health care system, especially when the clinical implications for treatment are not that clear.
2 Discussion
In this current review, we will summarize the state of the literature plus present data from a previously performed systematic review to highlight how the direction (i.e. gain or loss of receptor expression), extent of discordance in ER, PR, and HER2/neu status between primary breast cancers, and their paired metastasis can effect patient management. In addition, we evaluate how discordance could impact on the design of future clinical trials.
Receptor discordance between primary and metastasis is a recognized phenomenon in a number of tumour types [12] and can present a challenge to patient management. It is important to understand patient attitudes towards having biopsies performed for receptor analysis. A frequently cited reason for not performing biopsies is that patients will not accept them; however, this is not borne out by the literature. One study reported that up to 82 % of patients with suspected metastatic lesion agreed to undergo a biopsy [13]. In general, the morbidity and complication rate associated with the procedure are minimal in experienced centres. In the DESTINY trial, patient satisfaction was assessed, and while 34 % of patients reported pre-biopsy anxiety, and 59 % post-biopsy pain, the vast majority (89 %) would recommended metastatic biopsy to other patients [42]. In theory, there are two main ways in which discordance will affect future trial design. Firstly, is to design trials that will elucidate the mechanism of discordance and the second is how this discordance will itself affect the design of future trials.
3 Future trials to further elucidate mechanisms of receptor discordance
Given that so many studies have now shown that receptor discordance is a true biological phenomenon, prospective trials are needed to evaluate whether or not this discordance has any impact on patient outcomes in terms of either progression free or overall survival.
In conclusion, the present analysis shows broad rates of discordance across both sites and biomarkers. To further explore the clinical implications of biomarker conversion in breast cancer patients, randomized clinical trial in metastatic breast cancer patients are needed. It is based on receptor expression of the primary tumour versus that of the metastasis. Studies are also needed whereby biopsies of multiple sites of metastasis are performed in the same patient at the same time, as this will help elucidate the mechanism of metastasis in different disease sites. In addition, prospective studies are needed to look at biopsies of different sites of metastatic disease at different time intervals to elucidate the effects of treatment on tumour behaviour. In addition, the creation of metastatic tissue bio-repository is of great importance in the area of understanding the biological mechanisms of mixed responses. In this setting, patients may well be responding at multiple metastatic sites while progressing at others. Biopsies in this setting could provide a unique insight into the mechanism of sensitivity and resistance.
While these types of study may not be feasible at all centres, the creation of metastatic tissue bio-repositories could potentially facilitate further translational research on the clinical and treatment implications of biomarker discordance. An essential component of these is ensuring that all patients are appropriately consented to allow their tissues to be subjected to multiple types of analysis in situations where patients are receiving novel treatments [51–55].
4 How receptor discordance could impact design of future clinical trials
In addition to learning why receptor discordance occurs as discussed above, we also want to see how discordance can be used to improve clinical trial design. Given the increased interest in the mechanisms of endocrine resistance, and the very low event rates being observed [56], future trials may well wish to identify patients’ greatest risk of relapse or progression be it through demonstration of discordance and loss of progesterone expression. Currently, trials of patients with early stage ER/PR positive disease have such low event rates that these trials need to be enormous and take many years to complete [57]. While many centres are evaluating the use of sequential biopsies in the neoadjuvant and window of opportunity settings [58–62], these brief studies will be more valuable for assessing the brief effects of novel agents on the tumour rather than long-term effects such as receptor discordance and its mechanisms. A greater understanding of the mechanisms of discordance could also would lead to more rational clinical trial design where, for example, progression of disease may not actually reflect drug failure but rather a change in the receptor profile that the action of the drug was supposed to mediated through. Similar to the challenge facing investigators of trials in ER positive populations, the low event rates in patients with ER positive Her2/neu positive also make trials design challenging, so a better appreciation of receptor discordance upon recurrence could allow for more rationale trial design too.
5 Conclusion
In order to plan future studies, it is important to realize the limitations of the current literature. The main strength of this review is with its systematic and exhaustive nature of included articles for receptor discordance in different metastatic sites. This data would appear to confirm that while there were significant technical issues with respect to tissue processing in the past; it is most likely that receptor discordance is a true biological phenomenon. This being so it is important that we all strive to perform studies to not only explore the mechanism of this discordance but also to use this information to develop more rational clinical trials to ultimately allow the delivery of truly personalized care.
References
Cardoso, F., Harbeck, N., Fallowfield, L., et al. (2012). Locally recurrent or metastatic breast cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Annals of Oncology, 23(Suppl 7), vii11–19.
Van Poznak, C. H., Temin, S., Yee, G. C., et al. (2011). American Society of Clinical Oncology executive summary of the clinical practice guideline update on the role of bone-modifying agents in metastatic breast cancer. Journal of Clinical Oncology, 29, 1221–1227.
Wolff, A. C., Hammond, M. E., Hicks, D. G., et al. (2013). Recommendations for human epidermal growth factor receptor 2 testing in breast cancer: American Society of Clinical Oncology/College of American Pathologists clinical practice guideline update. Journal of Clinical Oncology, 31, 3997–4013.
Amir, E., & Clemons, M. (2009). Should a biopsy be recommended to confirm metastatic disease in women with breast cancer? Lancet Oncology, 10, 933–935.
Aurilio, G., Disalvatore, D., Pruneri, G., et al. (2014). A meta-analysis of oestrogen receptor, progesterone receptor and human epidermal growth factor receptor 2 discordance between primary breast cancer and metastases. European Journal of Cancer, 50, 277–289.
Van Poznak, C., Somerfield, M. R., Bast, R. C., et al. (2015). Use of biomarkers to guide decisions on systemic therapy for women with metastatic breast cancer: American Society of Clinical Oncology Clinical Practice Guideline. Journal of Clinical Oncology, 33, 2695–2704.
Sighoko, D., Liu, J., Hou, N., et al. (2014). Discordance in hormone receptor status among primary, metastatic, and second primary breast cancers: biological difference or misclassification? The Oncologist, 19, 592–601.
Rhodes, A., Jasani, B., Barnes, D. M., et al. (2000). Reliability of immunohistochemical demonstration of oestrogen receptors in routine practice: interlaboratory variance in the sensitivity of detection and evaluation of scoring systems. Journal of Clinical Pathology, 53, 125–130.
Rudiger, T., Hofler, H., Kreipe, H. H., et al. (2002). Quality assurance in immunohistochemistry: results of an interlaboratory trial involving 172 pathologists. The American Journal of Surgical Pathology, 26, 873–882.
Khoury, T., Sait, S., Hwang, H., et al. (2009). Delay to formalin fixation effect on breast biomarkers. Modern Pathology, 22, 1457–1467.
Engel, K. B., & Moore, H. M. (2011). Effects of preanalytical variables on the detection of proteins by immunohistochemistry in formalin-fixed, paraffin-embedded tissue. Archives of Pathology & Laboratory Medicine, 135, 537–543.
Monaco, S. E., Nikiforova, M. N., Cieply, K., et al. (2010). A comparison of EGFR and KRAS status in primary lung carcinoma and matched metastases. Human Pathology, 41, 94–102.
Simmons, C., Miller, N., Geddie, W., et al. (2009). Does confirmatory tumor biopsy alter the management of breast cancer patients with distant metastases? Annals of Oncology, 20, 1499–1504.
Welter, S., Jacobs, J., Krbek, T., et al. (2008). Pulmonary metastases of breast cancer. When is resection indicated? European Journal of Cardio-Thoracic Surgery, 34, 1228–1234.
Yonemori, K., Tsuta, K., Shimizu, C., et al. (2008). Immunohistochemical profiles of brain metastases from breast cancer. Journal of Neuro-Oncology, 90, 223–228.
Shipitsin, M., Campbell, L. L., Argani, P., et al. (2007). Molecular definition of breast tumor heterogeneity. Cancer Cell, 11, 259–273.
Stoecklein, N. H., & Klein, C. A. (2010). Genetic disparity between primary tumours, disseminated tumour cells, and manifest metastasis. International Journal of Cancer, 126, 589–598.
Navin, N., Kendall, J., Troge, J., et al. (2011). Tumour evolution inferred by single-cell sequencing. Nature, 472, 90–94.
Criscitiello, C., Andre, F., Thompson, A. M., et al. (2014). Biopsy confirmation of metastatic sites in breast cancer patients: clinical impact and future perspectives. Breast Cancer Research, 16, 205.
Karlsson, E., Appelgren, J., Solterbeck, A., et al. (2014). Breast cancer during follow-up and progression—a population based cohort on new cancers and changed biology. European Journal of Cancer, 50, 2916–2924.
Hilton, J. F., Amir, E., Hopkins, S., et al. (2011). Acquisition of metastatic tissue from patients with bone metastases from breast cancer. Breast Cancer Research and Treatment, 129, 761–765.
Yeung, I.C. C.M., Addison, C.L., Hutton, B., Zhu, X., Mazzarello, S.(2013). Arnaout A. Breast cancer biomarker discordance between primary and sites of metastasis—a systematic review. In ASCO Annual Meeting 2013. Journal of Clinical Oncology.
Solomayer, E. F., Becker, S., Pergola-Becker, G., et al. (2006). Comparison of HER2 status between primary tumor and disseminated tumor cells in primary breast cancer patients. Breast Cancer Research and Treatment, 98, 179–184.
Dikicioglu, E., Barutca, S., Meydan, N., & Meteoglu, I. (2005). Biological characteristics of breast cancer at the primary tumour and the involved lymph nodes. International Journal of Clinical Practice, 59, 1039–1044.
Cho, E. Y., Han, J. J., Choi, Y. L., et al. (2008). Comparison of Her-2, EGFR and cyclin D1 in primary breast cancer and paired metastatic lymph nodes: an immunohistochemical and chromogenic in situ hybridization study. Journal of Korean Medical Science, 23, 1053–1061.
Amir, E., Ooi, W. S., Simmons, C., et al. (2008). Discordance between receptor status in primary and metastatic breast cancer: an exploratory study of bone and bone marrow biopsies. Clinical Oncology (Royal College of Radiologists), 20, 763–768.
Santinelli, A., Pisa, E., Stramazzotti, D., & Fabris, G. (2008). HER-2 status discrepancy between primary breast cancer and metastatic sites. Impact on target therapy. International Journal of Cancer, 122, 999–1004.
Kamby, C., Rasmussen, B. B., & Kristensen, B. (1989). Oestrogen receptor status of primary breast carcinomas and their metastases. Relation to pattern of spread and survival after recurrence. British Journal of Cancer, 60, 252–257.
Cardoso, F., Di Leo, A., Larsimont, D., et al. (2001). Evaluation of HER2, p53, bcl-2, topoisomerase II-alpha, heat shock proteins 27 and 70 in primary breast cancer and metastatic ipsilateral axillary lymph nodes. Annals of Oncology, 12, 615–620.
van Agthoven, T., Timmermans, M., Dorssers, L. C., & Henzen-Logmans, S. C. (1995). Expression of estrogen, progesterone and epidermal growth factor receptors in primary and metastatic breast cancer. International Journal of Cancer, 63, 790–793.
Hoefnagel, L. D., van de Vijver, M. J., van Slooten, H. J., et al. (2010). Receptor conversion in distant breast cancer metastases. Breast Cancer Research, 12, R75.
Tapia, C., Savic, S., Wagner, U., et al. (2007). HER2 gene status in primary breast cancers and matched distant metastases. Breast Cancer Research, 9, R31.
Gong, Y., Han, E. Y., Guo, M., et al. (2011). Stability of estrogen receptor status in breast carcinoma: a comparison between primary and metastatic tumors with regard to disease course and intervening systemic therapy. Cancer, 117, 705–713.
Lindstrom, L. S., Karlsson, E., Wilking, U. M., et al. (2012). Clinically used breast cancer markers such as estrogen receptor, progesterone receptor, and human epidermal growth factor receptor 2 are unstable throughout tumor progression. Journal of Clinical Oncology, 30, 2601–2608.
Lower, E. E., Glass, E., Blau, R., & Harman, S. (2009). HER-2/neu expression in primary and metastatic breast cancer. Breast Cancer Research and Treatment, 113, 301–306.
Zidan, J., Dashkovsky, I., Stayerman, C., et al. (2005). Comparison of HER-2 overexpression in primary breast cancer and metastatic sites and its effect on biological targeting therapy of metastatic disease. British Journal of Cancer, 93, 552–556.
Gancberg, D., Di Leo, A., Cardoso, F., et al. (2002). Comparison of HER-2 status between primary breast cancer and corresponding distant metastatic sites. Annals of Oncology, 13, 1036–1043.
St Romain, P., Madan, R., Tawfik, O. W., et al. (2012). Organotropism and prognostic marker discordance in distant metastases of breast carcinoma: fact or fiction? A clinicopathologic analysis. Human Pathology, 43, 398–404.
Aitken, S. J., Thomas, J. S., Langdon, S. P., et al. (2010). Quantitative analysis of changes in ER, PR and HER2 expression in primary breast cancer and paired nodal metastases. Annals of Oncology, 21, 1254–1261.
Liu, J., Deng, H., Jia, W. et al. (2012) Comparison of ER/PR and HER2 statuses in primary and paired liver metastatic sites of breast carcinoma in patients with or without treatment. Journal of Cancer Research and Clinical Oncology.
Khasraw, M., Brogi, E., & Seidman, A. D. (2011). The need to examine metastatic tissue at the time of progression of breast cancer: is re-biopsy a necessity or a luxury? Current Oncology Reports, 13, 17–25.
Amir, E., Clemons, M., Purdie, C. A., et al. (2012). Tissue confirmation of disease recurrence in breast cancer patients: pooled analysis of multi-centre, multi-disciplinary prospective studies. Cancer Treatment Reviews, 38, 708–714.
Dieci, M. V., Barbieri, E., Piacentini, F., et al. (2013). Discordance in receptor status between primary and recurrent breast cancer has a prognostic impact: a single-institution analysis. Annals of Oncology, 24, 101–108.
Hoefnagel, L. D., Moelans, C. B., Meijer, S. L., et al. (2012). Prognostic value of estrogen receptor alpha and progesterone receptor conversion in distant breast cancer metastases. Cancer, 118, 4929–4935.
Niikura, N., Liu, J., Hayashi, N., et al. (2012). Loss of human epidermal growth factor receptor 2 (HER2) expression in metastatic sites of HER2-overexpressing primary breast tumors. Journal of Clinical Oncology, 30, 593–599.
Darvishian, F., Singh, B., Krauter, S., et al. (2011). Impact of decalcification on receptor status in breast cancer. The Breast Journal, 17, 689–691.
Alers, J. C., Krijtenburg, P. J., Vissers, K. J., & van Dekken, H. (1999). Effect of bone decalcification procedures on DNA in situ hybridization and comparative genomic hybridization. EDTA is highly preferable to a routinely used acid decalcifier. The Journal of Histochemistry and Cytochemistry, 47, 703–710.
Gupta, S., Wallace, M. J., Cardella, J. F., et al. (2010). Quality improvement guidelines for percutaneous needle biopsy. Journal of Vascular and Interventional Radiology, 21, 969–975.
Andre, F., Bachelot, T., Commo, F., et al. (2014). Comparative genomic hybridisation array and DNA sequencing to direct treatment of metastatic breast cancer: a multicentre, prospective trial (SAFIR01/UNICANCER). Lancet Oncology, 15, 267–274.
Amir, E., Freedman, O., Carlsson, L., et al. (2013). Randomized feasibility study of de-escalated (every 12 wk) versus standard (every 3 to 4 wk) intravenous pamidronate in women with low-risk bone metastases from breast cancer. American Journal of Clinical Oncology, 36, 436–442.
Jacobs, C., Simos, D., Addison, C., et al. (2014). Pharmacotherapy of bone metastases in breast cancer patients—an update. Expert Opinion on Pharmacotherapy, 15, 1109–1118.
Jacobs, C., Amir, E., Paterson, A., et al. (2015). Are adjuvant bisphosphonates now standard of care of women with early stage breast cancer? A debate from the Canadian Bone and the Oncologist New Updates meeting. Journal of Bone Oncology, 4, 54–58.
Hutton, B., Mazzarello, S., & Clemons, M. (2015). Dosing strategies of bone-targeting agents. JAMA Internal Medicine, 175, 1864–1865.
Bedard, P. L., Freedman, O. C., Howell, A., & Clemons, M. (2008). Overcoming endocrine resistance in breast cancer: are signal transduction inhibitors the answer? Breast Cancer Research and Treatment, 108, 307–317.
Hong, B. Y., Ibrahim, M. F., Fernandes, R., et al. (2016). De-escalation of bone-targeted agents for metastatic prostate cancer. Current Oncology, 23, e77–78.
Goss, P.E., Ingle, J.N., Pritchard, K.I. et al. (2016). Extending aromatase-inhibitor adjuvant therapy to 10 years. The New England Journal of Medicine.
Freedman, O. C., Verma, S., & Clemons, M. J. (2005). Using aromatase inhibitors in the neoadjuvant setting: evolution or revolution? Cancer Treatment Reviews, 31, 1–17.
Jacobs, C., Clemons, M., Addison, C., et al. (2016). Issues affecting the loco-regional and systemic management of patients with invasive lobular carcinoma of the breast. The Breast Journal, 22, 45–53.
Levasseur, N., Clemons, M., Hilton, J., et al. (2015). Neoadjuvant endocrine therapy and window of opportunity trials: new standards in the treatment of breast cancer? Minerva Chirurgica, 70, 181–193.
Arnaout, A., Robertson, S., Kuchuk, I., et al. (2015). Evaluating the feasibility of performing window of opportunity trials in breast cancer. International Journal of Surgical Oncology, 2015, 785793.
Saleh, R. R., Bouganim, N., Hilton, J., et al. (2014). Neoadjuvant endocrine treatment for breast cancer: from bedside to bench and back again? Current Oncology, 21, e122–128.
Hilton, J., Arnaout, A., & Clemons, M. (2014). Primary endocrine therapy as an approach for patients with localized breast cancer deemed not to be surgical candidates. Current Opinion in Supportive and Palliative Care, 8, 53–58.
Gaedcke, J., Traub, F., Milde, S., et al. (2007). Predominance of the basal type and HER-2/neu type in brain metastasis from breast cancer. Modern Pathology, 20, 864–870.
Vincent-Salomon, A., Jouve, M., Genin, P., et al. (2002). HER2 status in patients with breast carcinoma is not modified selectively by preoperative chemotherapy and is stable during the metastatic process. Cancer, 94, 2169–2173.
Martinez, S. R., Young, S. E., Giuliano, A. E., & Bilchik, A. J. (2006). The utility of estrogen receptor, progesterone receptor, and Her-2/neu status to predict survival in patients undergoing hepatic resection for breast cancer metastases. The American Journal of Surgery, 191, 281–283.
D'Andrea, M. R., Limiti, M. R., Bari, M., et al. (2007). Correlation between genetic and biological aspects in primary non-metastatic breast cancers and corresponding synchronous axillary lymph node metastasis. Breast Cancer Research and Treatment, 101, 279–284.
Lorincz, T., Toth, J., Badalian, G., et al. (2006). HER-2/neu genotype of breast cancer may change in bone metastasis. Pathology and Oncology Research, 12, 149–152.
Gong, Y., Booser, D. J., & Sneige, N. (2005). Comparison of HER-2 status determined by fluorescence in situ hybridization in primary and metastatic breast carcinoma. Cancer, 103, 1763–1769.
Davidson, B., Konstantinovsky, S., Nielsen, S., et al. (2004). Altered expression of metastasis-associated and regulatory molecules in effusions from breast cancer patients: a novel model for tumor progression. Clinical Cancer Research, 10, 7335–7346.
Schwarz, C., Lubbert, H., Rahn, W., et al. (2004). Medical thoracoscopy: hormone receptor content in pleural metastases due to breast cancer. The European Respiratory Journal, 24, 728–730.
Bozzetti, C., Personeni, N., Nizzoli, R., et al. (2003). HER-2/neu amplification by fluorescence in situ hybridization in cytologic samples from distant metastatic sites of breast carcinoma. Cancer, 99, 310–315.
Tsutsui, S., Ohno, S., Murakami, S., et al. (2002). EGFR, c-erbB2 and p53 protein in the primary lesions and paired metastatic regional lymph nodes in breast cancer. European Journal of Surgical Oncology, 28, 383–387.
Zheng, W. Q., Lu, J., Zheng, J. M., et al. (2001). Variation of ER status between primary and metastatic breast cancer and relationship to p53 expression*. Steroids, 66, 905–910.
Omoto, Y., Kurosumi, M., Hozumi, Y., et al. (2010). Immunohistochemical assessment of primary breast tumors and metachronous brain metastases, with particular regard to differences in the expression of biological markers and prognosis. Experimental and Therapeutic Medicine, 1, 561–567.
Nedergaard, L., Haerslev, T., & Jacobsen, G. K. (1995). Immunohistochemical study of estrogen receptors in primary breast carcinomas and their lymph node metastases including comparison of two monoclonal antibodies. APMIS, 103, 20–24.
Shao, M. M., Liu, J., Vong, J. S., et al. (2011). A subset of breast cancer predisposes to brain metastasis. Medical Molecular Morphology, 44, 15–20.
Sari, E., Guler, G., Hayran, M., et al. (2011). Comparative study of the immunohistochemical detection of hormone receptor status and HER-2 expression in primary and paired recurrent/metastatic lesions of patients with breast cancer. Medical Oncology, 28, 57–63.
Falck, A. K., Ferno, M., Bendahl, P. O., & Ryden, L. (2010). Does analysis of biomarkers in tumor cells in lymph node metastases give additional prognostic information in primary breast cancer? World Journal of Surgery, 34, 1434–1441.
Ditsch, N., Mayer, B., Rolle, M., et al. (2003). Estrogen receptor expression profile of disseminated epithelial tumor cells in bone marrow of breast cancer patients. Recent Results in Cancer Research, 162, 141–147.
De la Haba-Rodriguez, J. R., Ruiz Borrego, M., Gomez Espana, A., et al. (2004). Comparative study of the immunohistochemical phenotype in breast cancer and its lymph node metastatic location. Cancer Investigation, 22, 219–224.
McCann, A. H., Dervan, P. A., O'Regan, M., et al. (1991). Prognostic significance of c-erbB-2 and estrogen receptor status in human breast cancer. Cancer Research, 51, 3296–3303.
Botteri, E., Disalvatore, D., Curigliano, G., et al. (2012). Biopsy of liver metastasis for women with breast cancer: impact on survival. Breast, 21, 284–288.
Jensen, J. D., Knoop, A., Ewertz, M., & Laenkholm, A. V. (2012). ER, HER2, and TOP2A expression in primary tumor, synchronous axillary nodes, and asynchronous metastases in breast cancer. Breast Cancer Research and Treatment, 132, 511–521.
Brogi, E., Murphy, C. G., Johnson, M. L., et al. (2011). Breast carcinoma with brain metastases: clinical analysis and immunoprofile on tissue microarrays. Annals of Oncology, 22, 2597–2603.
Curigliano, G., Bagnardi, V., Viale, G., et al. (2011). Should liver metastases of breast cancer be biopsied to improve treatment choice? Annals of Oncology, 22, 2227–2233.
Park, I. H., Kwon, Y., Ro, J. Y., et al. (2010). Concordant HER2 status between metastatic breast cancer cells in CSF and primary breast cancer tissue. Breast Cancer Research and Treatment, 123, 125–128.
Aoyama, K., Kamio, T., Nishikawa, T., & Kameoka, S. (2010). A comparison of HER2/neu gene amplification and its protein overexpression between primary breast cancer and metastatic lymph nodes. Japanese Journal of Clinical Oncology, 40, 613–619.
Strien, L., Leidenius, M., von Smitten, K., & Heikkila, P. (2010). Concordance between HER-2 and steroid hormone receptor expression between primary breast cancer, sentinel node metastases, and isolated tumor cells. Pathology, Research and Practice, 206, 253–258.
Azam, M., Qureshi, A., & Mansoor, S. (2009). Comparison of estrogen receptors, progesterone receptors and HER-2/neu expression between primary and metastatic breast carcinoma. The Journal of the Pakistan Medical Association, 59, 736–740.
Duchnowska, R., Dziadziuszko, R., Trojanowski, T., et al. (2012). Conversion of epidermal growth factor receptor 2 and hormone receptor expression in breast cancer metastases to the brain. Breast Cancer Research, 14, R119.
Lear-Kaul, K. C., Yoon, H. R., Kleinschmidt-DeMasters, B. K., et al. (2003). Her-2/neu status in breast cancer metastases to the central nervous system. Archives of Pathology & Laboratory Medicine, 127, 1451–1457.
Xu, R., Perle, M. A., Inghirami, G., et al. (2002). Amplification of Her-2/neu gene in Her-2/neu-overexpressing and -nonexpressing breast carcinomas and their synchronous benign, premalignant, and metastatic lesions detected by FISH in archival material. Modern Pathology, 15, 116–124.
Umekita, Y., Sagara, Y., & Yoshida, H. (1998). Estrogen receptor mutations and changes in estrogen receptor and progesterone receptor protein expression in metastatic or recurrent breast cancer. Japanese Journal of Cancer Research, 89, 27–32.
Andersen, J., & Poulsen, H. S. (1988). Relationship between estrogen receptor status in the primary tumor and its regional and distant metastases. An immunohistochemical study in human breast cancer. Acta Oncologica, 27, 761–765.
Bristol Uo. (2013). QUADAS Quality assessment tool for diagnostic accuracy studies. In.
Acknowledgments
Early data from this study were presented at the 2013 ASCO meeting (Journal of Clinical Oncology ASCO Annual Meeting Proceedings, 2013. E11574) SABCS 2013; ASBS (2013); EBCC-9 (2014)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
There was no external funding for this project.
Appendix 2: Quality assessment and statistical analysis of included studies
Quality assessment
Once the final group of articles was agreed upon, two of three authors (CY, FH, IK) independently examined the quality of each article using the Quality Assessment of Diagnostic Accuracy Studies (QUADAS-2) tool [95]. QUADAS-2 is the current version of the QUADAS, the tool used to evaluate the risk of bias and applicability of diagnostic accuracy studies in systematic reviews. It consists of four key domains: patient selection, index test, reference standard, and flow and timing. Each is assessed in terms of risk of bias and the first three in terms of concerns regarding applicability. Signalling questions are included to assist in judgments about the risk of bias (Supplemental Table 2). Risk of bias was judged as “low” if the answers to all signal questions for a domain were “yes”; it was judged as “high” if any signal question in a domain was answered “no”, or as “unclear” if insufficient information was provided. Concern for applicability is assessed in three key areas: patient selection, index test, and reference standard. Concern for applicability was assigned as “low”, “high”, or “unclear” with criteria analogous to those used for risk of bias. If a study is judged as “low” on all domains relating to bias or applicability, then it is considered appropriate to have an overall judgement of “low risk of bias” or “low concern regarding applicability” for that study [95]. If a study is judged “high” or “unclear” on one or more domains, then it may be judged “at risk of bias” or as having “concerns regarding applicability.”
Statistical analysis
To generate summary estimates of the rates of loss of receptor status, gain of receptor status, and total discordance rate, we had planned to pursue random effects meta-analyses of each of these proportions of interest, summarizing findings with pooled proportions and corresponding 95 % confidence intervals if studies were considered clinically homogeneous and if summary estimates were not associated with significant statistical heterogeneity (i.e. an I 2 value of >50 %). Following collection of study level data, we noted that a majority of included studies failed to report the raw data required for meta-analysis (i.e. numbers of events and sample size) and were instead reporting only percentages of each outcome observed. Given this limitation, we decided to provide summary medians and ranges of the proportions of each outcome instead. We explored these quantities both overall and within individual sites of metastasis. For each summary estimate reported, we conservatively report the median and range to be based on the total number of samples that are clear from the individual studies contributing to these estimates.
Rights and permissions
About this article
Cite this article
Yeung, C., Hilton, J., Clemons, M. et al. Estrogen, progesterone, and HER2/neu receptor discordance between primary and metastatic breast tumours—a review. Cancer Metastasis Rev 35, 427–437 (2016). https://doi.org/10.1007/s10555-016-9631-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10555-016-9631-3