Abstract
Background
Discordance rates of hormone receptor (HR) and human epidermal growth factor-2 (HER2) status between primary and recurrent breast cancer were reported to be in the wide range of 10–40 %, although its prognostic relevance remains to be elucidated.
Methods
Fifty-five breast cancer patients had biopsies or resections of recurrent lesions. Pathological assessments of the HR and HER2 status of primary and recurrent lesions were performed in a single laboratory at Keio University Hospital. Tumors were classified as luminal (HR+ and HER2−), luminal/HER2 (HR+ and HER2+), HER2 (HR− and HER2+), or triple negative (HR− and HER2−).
Results
Discordance rates in estrogen receptor (ER), progesterone receptor (PgR) and HER2 status between primary tumors and recurrent lesions were 16.4, 30.9 and 10.2 %, respectively. Overall, 14 patients (25.5 %) changed subtypes at recurrent lesions. Patients with a gain in ER and PgR status had a significantly longer disease-free interval compared with the corresponding concordant-negative patients (ER: 99.0 vs. 18.5 months, p = 0.037, PgR: 141.0 vs. 24.4 months, p = 0.011). Patients with a loss of HER2 status experienced a trend toward shorter time to progression, compared with patients who maintained HER2 positivity (4.0 vs. 18.4 months, p = 0.051).
Conclusions
Discordance in receptor status between primary and recurrent breast cancers were seen in 10–30 %. A gain in HR status was significantly associated with better prognosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer is the most common cancer in women worldwide with approximately 1,400,000 new diagnoses and more than 450,000 deaths each year [1]. Despite the development of adjuvant therapies for breast cancer, around 30 % of early breast cancer patients will later relapse [2, 3].
Estrogen receptor (ER), progesterone receptor (PgR) and human epidermal growth factor-2 (HER2) status is clinically used to define breast cancer subtypes and treatments are usually selected according to these subtypes. Hormone receptor (HR) and HER2 status in primary tumors usually help in making decisions about systemic therapies for recurrent breast cancer. However, changes in receptor status throughout tumor progression have been described [4, 5]. Previous studies have shown discordance rates of 10–40 % for HR and 5–20 % for HER2 status [6–8]. Although biopsy of recurrent breast cancer has been recently recommended by international clinical guidelines [9], the clinical impact remains unclear and prognostic relevance remains to be elucidated.
The aim of this study is to investigate ER, PgR and HER2 status of primary tumors and recurrent lesions, and to assess the discordance rate and its prognostic impact.
Patients and methods
Case selection
From a prospective database including all patients with recurrent breast cancer from January 2001 to June 2013 at Keio University Hospital, we retrospectively identified consecutive cases of patients who had biopsies or resections of recurrent lesions. Inclusion criteria included primary, unilateral breast cancer with subsequent development of loco-regional or distant recurrence with recorded receptor status of ER, PgR, and HER2 in both primary tumors and recurrent lesions. Exclusion criteria included bilateral breast cancer, male gender, ipsilateral breast tumor recurrence after breast-conserving surgery and stage IV breast cancer. In patients with more than one recurrent lesion, the site of biopsy was chosen by the radiologist according to feasibility and safety criteria.
Pathological assessment
HR status was assessed by immunohistochemistry (IHC). HR staining was performed with the IView DAB Detection Kit and Ventana ES Autostainer (Ventana Medical Systems, Tuscon, AZ, USA) using primary antibodies against ER (Clone SP1; Ventana) and PgR (Clone 1E2; Ventana). HR status was determined using the Allred score and defined as positive when the score was 3 or more. HR status was considered positive in cases of ER and/or PgR positivity.
HER2 status was assessed by IHC or fluorescence in situ hybridization (FISH) analysis. HER2 staining was performed with the IView DAB Detection Kit and Ventana ES Autostainer using HER2 antibody (Clone 4B5; Ventana). FISH analysis was performed with a PathVysion HER2 DNA Probe Kit (Abbott Japan, Japan) according to the manufacturer’s instructions. The average copy number for each probe was determined and the amplification ratio was calculated as the ratio between the average copy number per cell for HER2 and chromosome 17. A positive result was defined as a HER2 gene to chromosome 17 ratio >2.0. Tumors with a score of 3+ by IHC or gene amplification by FISH were considered HER2 positive.
Ki67 antibody (Clone SP6; Thermo Scientific, Japan) was used at a 1:200 dilution with heat-induced antigen retrieval using Target Retrieval Solution, (pH 6; Dako) heated to 121 °C for 10 min. For the Ki67 labeling index, a total of 400 cells were counted from 3 consecutive high-power magnifications.
Tumors were classified as luminal (ER+ and/or PgR+, and HER2−), luminal/HER2 (ER+ and/or PgR+, and HER2+), HER2 (ER−, PgR−, and HER2+), or triple negative (TN) (ER−, PgR−, and HER2−).
Statistical analysis
Statistical differences between groups were determined using a chi-squared test. The disease-free interval (DFI) and time to progression (TTP) were calculated using the Kaplan–Meier curves and compared using the log-rank test. Events for the calculation of DFI included the first occurrence of loco-regional and distant breast cancer recurrence or death as a result of any cause. TTP was calculated as the duration between biopsy and first documented evidence of progressive disease or death as a result of any cause. p values <0.05 were considered statistically significant. Data were analyzed using IBM SPSS Statistics Version 19 (SPSS Inc., Chicago, IL, USA).
Results
Patient characteristics
Fifty-five breast cancer patients who had biopsies or resections of recurrent lesions were identified. The median age at primary diagnosis was 50.0 years and ranged from 27 to 78 years (Table 1). Twenty-six patients (47.3 %) had breast-conserving surgery and 29 patients (52.7 %) had a mastectomy. Adjuvant therapies included chemotherapy for 35 (63.6 %), endocrine therapy for 41 (74.5 %) and trastuzumab for 3 patients (5.5 %). Breast irradiation was performed in 27 patients (49.1 %). The mean tumor size was 2.4 cm (standard deviation 1.5 cm) and the clinical nodal status was positive in 32.7 % of patients. Primary tumors stained positive for ER in 41 (74.5 %), PgR in 38 (69.1 %) and HER2 in 13 patients (23.7 %). The median age at the time of recurrence was 58.0 years and ranged from 31 to 82 years (Table 2). The median interval between surgery for primary breast cancer and biopsy or resection of recurrence was 66.7 months (range 8.4–281.2 months). Sites of biopsy or resection were loco-regional recurrences (LRR) in 20 patients (36.4 %) and distant metastases (DM) in 35 patients (63.6 %). Needle biopsies using radiological guidance were performed for 30 patients and excisional biopsies or resections were carried out for 25 patients. ER, PgR and HER2 status of recurrent lesion was positive in 72.7, 49.1 and 27.3 %, respectively.
Discordance in single receptor status
Discordance in ER status was observed in 9 patients (16.4 %), with gain in 4 patients and loss in 5 patients (Table 3). A change in PgR status was identified in 17 patients (30.9 %) with loss of PgR as the main change (14/17). HR discordance was observed in 9 patients (16.4 %), with gain in 3 patients and loss in 6 patients. The HR discordance rate was fairly similar to the ER discordance rate. HER2 status was changed in 5 patients (10.2 %). Among 36 patients with HER2-negative primary tumors, 2 patients (5.6 %) gained HER2 positivity, whereas 3 out of 13 patients (23.1 %) with HER2-positive primary tumors changed to HER2 negative. Quantitative changes of ER and PgR status from primary tumors to recurrent lesions were calculated using the Allred score and are shown as a waterfall plot (Fig. 1a, b). Quantitative changes in HER2 status using the IHC score are also shown in Fig. 1c. Receptor discordance was mainly caused by loss of receptor status.
The median ki67 values of primary tumors (8 samples) and recurrent lesions (30 samples) were 64.5 and 30 %, respectively. Among 8 patients with paired ki67 at primary and recurrent lesions, increased, unchanged and decreased ki67 values were observed in 3, 1 and 4 patients, respectively.
Discordance in subtypes
Overall, 14 patients (25.5 %) had changed subtypes at recurrent lesions (Table 4). The highest rate (75.0 %) of discordance was observed in HER2 type primary tumors: 2 patients (50.0 %) changed to luminal/HER2 type and 1 patient (25.0 %) changed to TN type. Conversely, TN type was the most stable subtype: a change from TN type to luminal type was observed in 1 patient (12.5 %). Patients with luminal and luminal/HER2 type showed similar discordance rates of 22.6 and 25.0 %, respectively.
Predictive factors of receptor discordance
The PgR discordance rate was significantly higher in patients who received adjuvant endocrine therapy than in those who did not (39.0 vs. 7.1 %, p = 0.023), while ER and HER2 discordance were not associated with adjuvant endocrine therapy (ER: 17.1 vs. 14.3 %, p = 0.587, HER2: 10.5 vs. 9.1 %, p = 0.689). In contrast to adjuvant endocrine therapy, adjuvant chemotherapy was not significantly correlated with HR or HER2 discordance. There was no significant difference in HR and HER2 discordance rates between LRR and DM (HR: 15.0 vs. 17.1 %, p = 0.58, HER2: 5.9 vs. 12.5 %, p = 0.426).
Clinical impact
Among 9 patients (16.4 %) with HR discordance and 5 patients (10.2 %) with HER2 discordance, treatments based on recurrent receptor status were performed in 9 patients (64.3 %). One out of 3 patients with HR gain had started endocrine therapy and 5 out of 6 patients with loss of HR were given chemotherapy after biopsy. Two patients with HER2 gain had received trastuzumab, whereas 1 out of 3 patients with HER2 loss had discontinued trastuzumab after biopsy. Among these 9 patients with altered treatment according to receptor status of recurrent lesions, there were 3 patients who remained recurrence-free after resections of recurrent lesions, 1 patient with partial response, 2 patients with stable disease and 3 patients with progression of disease.
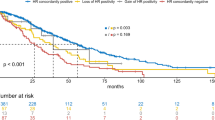
There was no significant association between HER2 discordance and DFI. Conversely, patients with a gain in ER and PgR status had significantly longer DFI compared with the corresponding concordant-negative ER and PgR group (ER: 99.0 vs. 18.5 months, p = 0.037; PgR: 141.0 vs. 24.4 months, p = 0.011), as shown in Fig. 2a, b. No significant impact on survival was observed in the case of ER or PgR loss, when compared with the respective concordant-positive groups (Fig. 2c, d).
Patients with a loss in HER2 status tended towards a worse TTP (4.0 vs. 18.4 months, p = 0.051) when compared with patients who maintained their HER2 positivity. However, HER2 gain did not correlate with TTP (9.1 vs. 8.9 months, p = 0.540). HR loss and gain also were not associated with TTP (loss: 12.9 vs. 11.5 months, p = 0.654, gain: 8.2 vs. 8.5 months, p = 0.949). Time to progression curves for HER2 and HR discordance are shown in Fig. 3.
Safety
There was one serious adverse event related to biopsy: pneumothorax from a punch biopsy of the lung lesion resulted in prolonged hospitalization and was resolved with thorax drainage within 12 days.
Discussion
The systemic therapy for recurrent breast cancer is usually determined using the HR and HER2 status of the primary tumor, and biopsy of recurrent lesions is not widespread in clinical practice, in spite of evidence indicating the existence of discordance in receptor status between primary and recurrent breast cancer [10, 11]. In our study, we found that ER, PgR and HER2 status of recurrent lesions was changed in 16.4, 30.9 and 10.2 % of patients, respectively. Receptor discordance was more common in HR than HER2 status and loss of PgR was most frequently observed. These findings are consistent with a recent pooled analysis of two large prospective studies [4]. In this pooled analysis, the discordance rate of ER, PgR and HER2 were reported as 12.6, 31.2 and 5.5 %, respectively.
We also evaluated the discordance rate of subtypes, with a result of 25.5 % (Table 4). The frequency of changing subtypes in TN primary tumors was lower than that in either luminal or HER2 primary tumors. Similar results were seen in a recent retrospective large single-institution analysis. Assessment of 385 patients with invasive primary breast tumors and matched lymph nodes found that alteration of subtype in TN-type tumors (23.1 %) was less frequent than that in luminal (39.5 %) and HER2 types (25.0 %) [12].
Several mechanisms can lead to changes in receptor status between primary and recurrent breast cancer. Analytical errors such as variation in receptor determination with different protocols may cause inaccurate results [13]. However, our study used consistent assays for primary tumors and recurrent lesions in a single laboratory at our institute. Breast cancer has also been known to exhibit intratumoral heterogeneity and it can generate sampling errors from both primary tumors and recurrent lesions [14, 15]. In spite of these causes, tumor biological factors cannot be excluded from consideration. Discordance may occur with changes in tumor characteristics throughout progression or by the effect of previous treatments [16, 17].
The clinical impact of biopsy of recurrent lesions on treatment decisions was also analyzed. Our results show that 64.3 % of patients with subtype discordance were provided with new treatments based on recurrent receptor status. The majority of those patients received chemotherapy because of HR loss and all patients with HER2 gain started receiving trastuzumab. Amir et al. [4] reported that changes in treatment were more common in patients with receptor gain than loss. This reason for this may be that physicians tend to consider that discontinuing a target therapy would increase the risk of losing a benefit from a potentially effective therapy. Thus the response to previous lines of therapy could be important when deciding treatment if there is a biopsy result with receptor loss.
We underline the prognostic significance of HR and HER2 discordance between primary and recurrent breast cancer. Patients with a gain in HR status experienced significantly longer DFI compared with the HR concordant-negative patients. The better prognosis in patients with HR gain might be attributable to the slow-growing nature of HR-positive breast cancer. In contrast to post-relapse survival (PRS) which is the outcome common to the majority of studies [6, 18, 19], there has been no report confirming an association between receptor discordance and DFI. Furthermore, a correlation between HR gain and better survival has rarely been assessed, although there are many studies which have demonstrated an association between HR loss and poor prognosis [6, 20]. In a recent retrospective study of 100 patients with liver metastasis from Botteri et al. [21], patients with ER or HER2 gain showed significantly better OS compared with patients with concordant-negative receptor status. In our study, a loss of HER2 status was also associated with worse TTP. HER2 loss has previously been reported as an indicator of poor prognosis. However, this report utilized PRS which does not discount the influence of inappropriate target therapy for discordant cases [6]. However, our definition of TTP was the period between biopsy and first progressive disease or death; therefore, it was not influenced by the duration of inappropriate therapy before biopsy. Consistent with this report, since patients with HER2 loss did not always stop receiving trastuzumab, a poor prognosis associated with HER2 loss cannot be attributed to withdrawal of anti-HER2 therapy.
Our study has its limitations. This is a retrospective study with a small number of patients, so we should consider the various biases in recurrent cases selected for biopsy. Furthermore, biopsies for recurrent lesions were not always performed at the time of first recurrence. Therefore, treatments for a recurrent setting would potentially affect receptor discordance in some cases. Due to these limitations in our data, we cannot robustly deduce the prognostic value of discordance in recurrent breast cancer. However, it is important to highlight that our results show that biopsy for recurrent lesions is feasible and that receptor status was changed in 10–30 % of our patients.
In conclusion, discordance in receptor status between primary and recurrent breast cancer was confirmed in our study. Therefore, tissue confirmation should be considered in order to make effective treatment decisions against recurrent breast cancer. Further research is needed to confirm the relationship between receptor discordance and prognosis.
References
Siegel R, Naishadham D, Jemal A (2012) Cancer statistics, 2012. CA Cancer J Clin 62:10–29
Perez EA, Romond EH, Suman VJ et al (2011) Four-year follow-up of trastuzumab plus adjuvant chemotherapy for operable human epidermal growth factor receptor 2-positive breast cancer: joint analysis of data from NCCTG N9831 and NSABP B-31. J Clin Oncol 29:3366–3373
Early Breast Cancer Trialists’ Collaborative Group (EBCTCG). (2005) Effects of chemotherapy and hormonal therapy for early breast cancer on recurrence and 15-year survival: an overview of the randomised trials. Lancet 365:1687–1717
Amir E, Clemons M, Purdie CA et al (2012) Tissue confirmation of disease recurrence in breast cancer patients: pooled analysis of multi-centre, multi-disciplinary prospective studies. Cancer Treat Rev 38:708–714
Turner NH, Di Leo A (2013) HER2 discordance between primary and metastatic breast cancer: assessing the clinical impact. Cancer Treat Rev 39:947–957
Dieci MV, Barbieri E, Piacentini F et al (2013) Discordance in receptor status between primary and recurrent breast cancer has a prognostic impact: a single-institution analysis. Ann Oncol 24:101–108
Amir E, Miller N, Geddie W et al (2012) Prospective study evaluating the impact of tissue confirmation of metastatic disease in patients with breast cancer. J Clin Oncol 30:587–592
Thompson AM, Jordan LB, Quinlan P et al (2010) Prospective comparison of switches in biomarker status between primary and recurrent breast cancer: the Breast Recurrence in Tissues Study (BRITS). Breast Cancer Res 12:R92
NCCN Clinical Practice Guidelines in Oncology, Breast Cancer Version 3.2014. Available at http://www.nccn.org/professionals/physician_gls/pdf/breast.pdf
Liedtke C, Broglio K, Moulder S et al (2009) Prognostic impact of discordance between triple-receptor measurements in primary and recurrent breast cancer. Ann Oncol 20:1953–1958
Feng Y, Sun B, Li X et al (2007) Differentially expressed genes between primary cancer and paired lymph node metastases predict clinical outcome of node-positive breast cancer patients. Breast Cancer Res Treat 103:319–329
Aitken SJ, Thomas JS, Langdon SP et al (2010) Quantitative analysis of changes in ER, PR and HER2 expression in primary breast cancer and paired nodal metastases. Ann Oncol 21:1254–1261
Pusztai L, Viale G, Kelly CM et al (2010) Estrogen and HER-2 receptor discordance between primary breast cancer and metastasis. Oncologist 15:1164–1168
Bertos NR, Park M (2011) Breast cancer––one term, many entities? J Clin Invest 121:3789–3796
Wu JM, Fackler MJ, Halushka MK et al (2008) Heterogeneity of breast cancer metastases: comparison of therapeutic target expression and promoter methylation between primary tumors and their multifocal metastases. Clin Cancer Res 14:1938–1946
Mittendorf EA, Wu Y, Scaltriti M et al (2009) Loss of HER2 amplification following trastuzumab-based neoadjuvant systemic therapy and survival outcomes. Clin Cancer Res 15:7381–7388
Pectasides D, Gaglia A, Arapantoni-Dadioti P et al (2006) HER-2/neu status of primary breast cancer and corresponding metastatic sites in patients with advanced breast cancer treated with trastuzumab-based therapy. Anticancer Res 26:647–653
Wilking U, Karlsson E, Skoog L et al (2011) HER2 status in a population-derived breast cancer cohort: discordances during tumor progression. Breast Cancer Res Treat 125:553–561
Lower EE, Glass E, Blau R et al (2009) HER-2/neu expression in primary and metastatic breast cancer. Breast Cancer Res Treat 113:301–306
Falck AK, Ferno M, Bendahl PO et al (2010) Does analysis of biomarkers in tumor cells in lymph node metastases give additional prognostic information in primary breast cancer? World J Surg 34:1434–1441
Botteri E, Disalvatore D, Curigliano G et al (2012) Biopsy of liver metastasis for women with breast cancer: impact on survival. Breast 21:284–288
Acknowledgments
This study was supported by a Grant-in-Aid from the Ministry of Education, Culture, Sports, Science and Technology, Japan.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Matsumoto, A., Jinno, H., Murata, T. et al. Prognostic implications of receptor discordance between primary and recurrent breast cancer. Int J Clin Oncol 20, 701–708 (2015). https://doi.org/10.1007/s10147-014-0759-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10147-014-0759-2