Abstract
Osteosarcoma is the most common malignant bone tumor in children and characterized by aggressive biologic behavior of metastatic propensity to the lung. Change of treatment paradigm brings survival benefit; however, 5-year survival rate is still low in patients having metastastatic foci at diagnosis for a few decades. Metastasis-associated protein (MTA) family is a group of ubiquitously expressed coregulators, which influences on tumor invasiveness or metastasis. MTA1 has been investigated in various cancers including osteosarcoma, and its overexpression is associated with high-risk features of cancers. In this review, we described various molecular studies of osteosarcoma, especially associated with MTA1.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Osteosarcoma (OS) is the most common primary bone sarcoma, which tumor cells produce osteoid. It occurs most often in children and adolescents, accounting for 2.4 % of childhood cancers, making it the eighth most common malignancies in the childhood [1]. OS shows a bimodal age distribution with a peak in the second decade of life (at the age of 15–19 years) and a secondary peak in older adults age 60 to >85 years [2]. Approximately 900 new OS cases were diagnosed annually in the USA. It has a slight male predominance (male/female = 1.35:1) [3]. Although the cause of OS is uncertain, there are some preexisting conditions, such as Paget disease or radiation [4, 5]. OS is the most common radiation-induced sarcoma, and 1 % of Paget disease takes a sarcomatous transformation at the end. There are other assumed predisposing conditions, which are fibrous dysplasia, hereditary multiple exostosis, bone infarct sites, and chronic osteomyelitis [5, 6]. OS associated with predisposing conditions shows older age distribution. Some genetic predisposing conditions are also known, which are hereditary retinoblastoma, Li-Fraumeni syndrome, and Rothmund-Thomson syndrome [7, 8].
The goal of treatment is surgical removal of primary tumor and chemoprevention of metastasis. Local treatment is usually limb salvage wide resection, and chemotherapy is carried out preoperatively (neoadjuvant chemotherapy) or postoperatively (adjuvant chemotherapy). Telangiectatic OS is quitely chemosensitive [9]. Radiation therapy is used in an unresectable tumor [10]. Conventional OS shows locally aggressive growth and rapid hematogenous metastases, predominantly to the lung. The prognosis is influenced by age, sex, tumor size/volume, surgical margins, stage, and detectable metastases at diagnosis and response to preoperative chemotherapy [11–15]. Low-grade OS, including low-grade central OS, parosteal OS, and periosteal OS, reveals relatively favorable prognosis than conventional type [16, 17]. They show about 90 % overall survival at 5 years [17].
Metastasis-associated protein (MTA), a family of cancer progression-related genes, is a component of the nucleosome remodeling and histone deacetylation (NuRD) complex. It includes MTA1, MTA2, and MTA3 and functions as transcription regulation by ATP-dependent chromatin remodeling and histone deacetylation [18]. Recently, there have been some reports, which reveal other roles of MTA1 in DNA damage response, inflammation, and infectious agent-driven cancers [19]. MTA1 has a dual function as a transcriptional coactivator or corepressor of various oncogenes or tumor suppressor genes and influences on tumor invasion, epithelial-mesenchymal transition (EMT), and metastasis. MTA1 expression and its clinicopathologic and biologic relevance have been widely investigated in various cancers including breast cancer, gastrointestinal carcinoma, carcinoid, nonsmall cell lung carcinoma, ovarian cancer, prostatic cancer, as well as OS [20–27]. In most human cancers, overexpression of that is common and is associated with disease progression, prognosis, and metastasis.
A few decades ago, there was a change of treatment frame of OS from single surgery to combined therapy of surgery and chemotherapy [28]. Overall survival at 5 years increased to 70 % in extremity, nonmetastatic OS, and it has not been significantly changed up to days [29]. Although metastases at diagnosis are noted in 15–20 % of OS patients, overall survival at 5 years is still 37 %, and this level is not changed despite of more intensive chemotherapy protocol [29, 30]. There is a need to understand a mechanism of metastasis, which is most common cause of treatment failure. We describe here the genetic and molecular alterations of OS, especially associated with MTA1, which could be a new treatment target.
2 Genetic and molecular studies
2.1 MTA family
Molecular mechanisms of MTA1 in cancer have been demonstrated by various levels of cancer progression. Toh et al. identified a gene that is overexpressed in highly metastatic rat mammary adenocarcinoma cell lines than nonmetastatic cell lines and named mta1 [31]. Human counterpart was also cloned, and high expression of MTA1 mRNA was correlated with invasive property. In breast cancer, MTA1 could transform into more aggressive phenotype by repression of the estrogen receptor-α transactivation through chromatin deacetylation of ER-responsive gene. And, MTA1 also represses BRCA1 tumor suppressor gene in the same manner [32].
In addition to chromatin histones, MTA also deacetylates nonhistone proteins such as p53 and hypoxia-inducible factor-1α (HIF-1α). While acetylated HIF-1α is converted to deacetylated, and stable form by MTA1, which leads to angiogenesis, p53 protein is deacetylated by MTA1 or MTA2, resulting in inhibition of cell growth arrest and apoptosis [33].
MTA1 expression has been investigated in regard to angiogenesis in various cancers such as breast cancer, early-stage nonsmall lung cancer, prostate cancer, esophageal squamous cell cancer, and histologically node-negative gastric cancer [34–38]. Overexpression of MTA1 is usually correlated with intratumoral microvessel density. Kai et al. revealed that MTA1-expressing tumors secreted higher levels of vascular endothelial growth factor (VEGF) and silencing MTA1 suppressed the angiogenic activity in vivo [36].
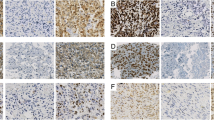
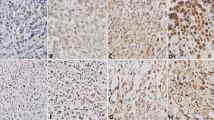
Park et al. reported that MTA1 is strongly expressed in high-grade OS tissue and metastatic lesion but not in low grade, and mRNA of MTA1 and MTA2 is increased in high-grade OS cell lines. MTA might be involved in the progression of high-grade OS, especially in metastasis of OS [27]. Other study using OS of the jaw revealed similar results that the high-grade tumors show higher positive rate of MTA expression [39].
2.2 Angiogenesis
Blood supply is required for delivery of oxygen and nutrients and removal of waste products via blood vessels in normal and neoplastic tissue. Cancer cells can induce neovascularization for the sustained growth and a way to systemic vasculature. Neovascularization is controlled by the balance between angiogenic factors and angiogenesis inhibitors. Angiogenic switch is induced when angiogenic factors are increased or angiogenesis inhibitors are decreased. Both intrinsic factors such as tumor cells themselves (oncogene activation or tumor suppressor gene inactivation) and tumor stromal cells and extrinsic factors like hypoxia, acidosis, and inflammation could lead to angiogenesis [40–42]. As tumor angiogenesis is a condition, which proangiogenic stimuli overwhelmed antiangiogenic factor, there could also be antiangiogenic factors such as angiostatin, endostatin, and thrombospondin as a counterpart [43–45]. There have been many reports, which show correlation between proangiogenic or antiangiogenic factors and clinicopathologic parameters [46–48].
HIF-1α is induced by tissue hypoxia, which is known to be associated with resistance to anticancer therapy, aggressive phenotype, and poor survival [49, 50]. It stimulates VEGF and acts as a potent proangiogenic factor. Some authors documented that MTA1 increases the stability and transcriptional activity of HIF-1α [51, 52]. It also enhances the expression of VEGF, which is a downstream target of HIF-1α. Recently, high expression of HIF-1α is associated with poor prognosis in various cancers such as ovarian cancer, breast cancer, and pancreatic cancer [53–55]. It is also highly expressed in OS cell lines than nonneoplastic osteoblasts in both normoxia and hypoxia conditions and functions as a protector of apoptosis [56]. High expression of HIF-1α is associated with significantly shorter overall survival and disease-free survival [50]. HIF-1α expression using prechemotherapy samples could be a good predictor of pathologic response of tumor cells (tumor necrosis) [57].
VEGF is one of the most important growth factors, which are involved in physiologic angiogenesis and tumor angiogenesis. It also interacts with various growth factors and signaling pathway, thereby enhancing angiogenesis or cell proliferation. Factors, which could upregulate VEGF, are transforming growth factor-α (TGF-α), basic fibroblast growth factor (bFGF), platelet-derived growth factor (PDGF), fibroblast growth factor 2 (FGF-2), TGF-β, and hepatocyte growth factor (HGF) [58, 59]. Lammli et al. presented that VEGF expression or level significantly increased in OS serum or tissues. They also showed that high expression of VEGF is associated with advanced clinical parameters such as frequent recurrence or metastasis [47]. However, prognostic value of VEGF is controversial [60, 61]. Recent study revealed that MTA1 is more potent angiogenesis inducer than VEGF in nonneoplastic and neoplastic lesions and upregulates VEGF and its receptor Flt-1 gene. VEGF also induces phosphorylation of endogenous MTA1, and this cross talk between them regulates angiogenesis and metastasis of tumor cells [62].
The Notch signaling pathway is known to be involved in physiologic angiogenesis, tumor angiogenesis, and tumor metastasis [63]. In physiologic angiogenesis, Notch interacts with VEGF, thereby blocking excessive sprout formation. However, aberrant activation of Notch signaling has been associated with tumor progression or metastasis. Hughes demonstrated that high expression of Notch 1, Notch 2, Notch ligand DLL1, and Notch target gene Hes1 is observed in metastatic OS cell lines compared to normal human osteoblasts or nonmetastatic OS cell lines. In murine model of OS with pulmonary metastasis, inhibition of Hes1 and Notch signaling eliminated tumor spread from the primary tumor. Hes1 expression is inversely correlated with survival in OS tumor tissues [64]. In other study using murine OS cell lines, similar results are found that Notch gene and Notch downstream targets Hes1 and Stat3 are upregulated in metastatic cell line [65]. Won et al. suggested that microRNA-199b-5p is upregulated in OS cell lines and is associated with Notch signaling pathway. Under the microRNA-199b-5p inhibitor, components of Notch pathway expression were altered [66].
2.3 Invasion of extracellular matrix
Matrix metalloproteinases (MMPs), a family of zinc-dependent endopeptidases, primarily act on the extracellular matrix (ECM) and basement membrane components and degrade them. They take part in various physiologic and pathologic processes that require ECM or basement membrane remodeling such as morphogenesis, wound healing, tissue repair, tumor migration, invasion, and metastasis [67, 68]. In general, high expression of MMPs is associated with tumor progression such as invasion and metastasis or prognosis [69, 70]. MMP-9 is reported as a downstream target of MTA1 in esophageal squamous cell carcinoma and breast cancer cell lines MDA-MB-231 and MCF-7 [71, 72]. Forced downregulation of MTA1 reduces protein levels of MMP-9 and influences on the invasiveness. In OS, high-level expression of MMP-2 and MMP-9 is associated with increased risk of mortality and shorter overall survival, respectively [73, 74]. Jin J. et al. demonstrated that miR-218 is downregulated in OS tissues and cell line and functions as tumor suppressor gene by negatively regulating MMP-2 and MMP-9 [75]. MMP-1, a kind of collagenases, is overexpressed in OS cell line, especially which is highly metastatic. Forced downregulation of MMP-1 reduced an anchorage-independent growth in vitro and showed smaller primary tumors and decreased foci of lung metastases in vivo [76]. Recently, there have been a few reports that MMP-8 could be associated with antitumoral effect and protective function in breast and murine skin cancers [77, 78]. In OS, MMP-8 is expressed in primary tumors but not in metastatic foci. However, its expression could not predict patients’ survival [79].
The Wnt proteins, a family of secreted cysteine-rich glycoproteins, activate intracellular signaling cascades by binding to Frizzleds and LRP-5/6 on target cells. Both the canonical and noncanonical Wnt pathways are involved in various biologic processes, especially embryogenic development and oncogenesis [80]. MTA1 and MTA1s could play a role on cell proliferation, invasion, and epithelial-mesenchymal transition by stimulation of Wnt/β-catenin pathway [81–83]. In OS, expression of Wnt components is widely investigated, and overexpression of Wnt ligands and Frizzled and LRP receptors is commonly observed. Guo et al. showed that E-cadherin expression is upregulated in Saos-2 cells with a dominant-negative, soluble LRP-5 [84]. They also demonstrated that LRP-5 promotes tumor invasion and metastasis via expression of Slug and Twist, transcriptional repressor, and MMP-2 and MMP-14 [85]. Ma et al. presented that β-catenin is overexpressed in OS cell line Saos-2 cells and its expression level is correlated with invasiveness of OS. Pharmacologic inhibition of Wnt/β-catenin and Notch pathway increased the chemosensitivity of Saos-2 cells [86].
The Snail family, zinc finger-containing transcription factor, includes Snail1 and Snail2 (also known as Slug) and functions as transcriptional repressors. Snail/Slug is also involved in EMT by downregulating E-cadherin, which causes migration, invasion, and metastasis of tumor cells [87]. Cagatay et al. reported that MTA1 enhances the expression of Snail1 and Slug, and silencing of MTA1 results in decreased recruitment of Snail and Slug to the promoter of E-cadherin. They showed that overexpression of MTA1 in colorectal cancer cells enhances proliferation, migration, invasion, and anchorage-independent growth [88]. Yang et al. reported that overexpression of Snail1 is associated with OS invasion and metastasis through suppression of E-cadherin expression [89]. Snail2 expression was investigated in long bone OS and was significantly correlated with tumor grade [90]. Same group revealed that overexpression of Snail2 increase cell motility, remodeling of the actin cytoskeleton, cellular protrusions, and expression of promigratory noncanonical Wnt pathway components [91]. E-cadherin, which is a well-known adhesion molecule and a downstream target of Snail, has been investigated in association with MTA1. Downregulation of E-cadherin using small interfering RNA led to overexpression of MTA1, decreased cohesiveness, and enhanced motility and invasion in prostate adenocarcinoma cell lines [92]. Wang et al. showed that silencing of MTA1 using siRNA results in the upregulation of E-cadherin [93]. Contrary to MTA1, MTA3 functions as repressor of EMT by regulating Snail. Upregulation of MTA1 could repress MTA 3 expression, resulting in promotion of EMT.
Twist, a member of the basic helix-loop-helix transcription factor family, is involved in embryogenic skeletal development and remodeling as well as cancer biology, especially EMT [87, 94]. There are various signaling pathways associated with Twist in both upstream and downstream directions [94]. In OS, there are few reports that reveal association between Twist and other signaling pathways such as endothelin-1/endothelin A receptor and β-catenin signaling [95, 96]. Both pathways were associated with OS cell survival against cisplatin, which was decreased by Twist. Recent study also demonstrated that miR-33a promotes OS cell resistance to cisplatin by downregulating Twist [97]. Yin et al. showed that positive Twist expression has significantly poor overall survival and disease-free survival and independent prognostic factor in OS [98].
Src, a member of the Src family of kinases, is a nonreceptor tyrosine kinase encoded by the c-Src proto-oncogene. Src kinase activity is regulated by various tyrosine receptor kinases including epidermal growth factor receptor kinase, PDGF tyrosine kinase, and integrin receptor [99–101]. Src activation also affects downstream signaling pathways such as transcription factor STAT-3 and focal adhesion kinase (FAK) [102, 103]. Hingorani et al. revealed that dasatinib, a dual Src-Abl kinase inhibitor, effectively inhibits the adhesion and migration of OS cells. However, it does not inhibit the growth of primary tumor and pulmonary metastases even though Src activation is blocked in vivo. Although Src is involved in tumor progression such as invasion and metastasis, Src kinase activation is not a primary pathway for pulmonary metastasis [104].
2.4 Anoikis resistance
When cells lose contact with the adjacent cells or ECM, they undergo a specific cellular apoptosis termed anoikis. Although anoikis plays a role in regulating cell homeostasis during development or tissue remodeling, many transformed cells and tumor cell lines reveal anoikis resistance [105]. Tumor cells, entering into the circulation, should acquire the resistance to anoikis to survive and metastasize. Anoikis could be induced by transfection with Src oncogene or epidermal growth factor receptor (EGFR) activation [106–108], and inhibitors of Src and EGFR have been investigated [109]. Mahoney et al. reported that forced expression of MTA1 increases survival in forced suspension culture of immortalized keratinocytes, collaborating with EGFR [110]. Molecules or molecular pathways involved in anoikis resistance in OS are Src, PI3K/Akt signaling pathway, caveolin-1, c-met, and ezrin/β4 integrin interaction [111–113].
Integrin is a family of cell adhesion receptors, which are involved in important biologic processes such as adhesion, signaling, proliferation, and metastasis. Among them, β4 integrin is often upregulated in malignant tumors, and high expression level of that is sometimes associated with poor prognosis. β4 integrin is also highly expressed in OS cell lines and OS patient samples. Wan et al. presented that anchorage-independent growth is significantly decreased in β4 integrin shRNA cell line, and lung metastases are also markedly decreased in mice injected with β4 integrin-shRNA cells compared to the control-shRNA group. They also revealed that β4 integrin associates with ezrin, which is required for the maintenance of its expression at RNA and protein levels [113].
Caveolin-1 (Cav-1) is major protein of caveolae, which involves signaling pathway. Cav-1 functions as a tumor suppressor gene or an oncogene depending on the cell type. Its expression is decreased in met-transformed osteoblasts and OS tissues. Forced overexpression of Cav-1 inhibited anchorage-independent growth, migration, and invasion in OS cell lines by inhibiting c-Src activity and met signaling. In vivo, Cav-1 overexpression reduced the metastasis in experimental conditions [112]. Diaz-Montero et al. demonstrated that Src-dependent activation of the PI3K/Akt pathway is observed in anoikis-resistant SAOS-2 cells and pharmacologic inhibition of Src or PI3K/Akt activity recovers sensitivity to anoikis [111].
2.5 Homing of tumor cells, extravasation, and attachment
The lung is a preferential site for OS metastasis, which comprises more than 80 % [114]. This site-specific metastasis could be explained by chemokine axis such as C-X-C motif chemokine receptor 4 (CXCR4) and its ligand C-X-C-motif chemokine ligand 12 (CXCL12) [115–117]. CXCL12 is abundantly expressed in the lung and bone marrow and a potent chemoattractant for CXCR4 and CXCR7 expressing cells [118]. CXCR4 is highly expressed in malignant cells including prostatic cancer, breast cancer, and OS cells as a result of high expression of HIF-1α or VEGF [119, 120]. In OS, high mRNA expression of CXCR4 is adversely correlated to overall survival, event-free survival, and metastasis-free survival [115]. As interactions of CXCR4 or CXCR7 and CXCL12 make tumor cells to adhere and extravasate in pulmonary metastasis, CXCR4 and CXCR7 are considered as a target of an anticancer therapy [121]. Brennecke et al. presented CXCR4 antibody inhibits lung micrometastases in mice with intratibial human OS xenografts [122].
Ezrin, a cytoskeleton linker membrane protein, mediates interaction of cells and surrounding microenvironment and facilitates signal transduction [123]. Khanna et al. presented that significantly diminished metastases could be induced by blocking ezrin with antisense ezrin or a dominant-negative inhibitor in murine OS models [124]. They also found that ezrin suppression results in decreased activity of Akt and MAPK. Akt signaling pathway is involved in OS metastasis through MMPs. High ezrin expression is associated with aggressiveness and a worse survival in OS patients [125–127]. MiR-183, markedly downregulated in OS cell lines and tissues, is inversely correlated with ezrin [128]. Combined miR-183 downregulation and ezrin upregulation were significantly associated with high tumor grade, poor response to chemotherapy, recurrence, and overall survival [129].
2.6 Inactivation of tumor suppressor genes
TP53 functions as a blocker of neoplastic transformation in various cancers. When DNA damage occurs, it binds to DNA and induces and maintains cell cycle arrest until DNA is repaired. Unless DNA is recovered, TP53 activates programmed cell death (apoptosis). MTA1 is also known as a DNA damage-responsive protein; it could control p53 stability by destabilizing constitutive photomorphogenic protein 1 (COP1) and mouse double minute 2 (MDM2), thereby regulating p53-dependent transcription of p53R2, a gene for supplying nucleotides for DNA repair [130]. It also transcriptionally suppresses p21WAF1, consequently leads to PCNA-dependent DNA repair in p53-independent mode [131]. Since MTA1 promoter has two p53 response elements, poly(ADP-ribosyl)ation of p53 could induce transcriptional repression of MTA1 [132]. TP53 mutation is a common genetic alteration in OS, and it is found in up to 50 % of OS patients [133–135]. Germline TP53 mutation is observed in Li-Fraumeni syndrome, which is known as a predisposing condition for OS, and shows higher incidence for OS. Some authors revealed that TP53 mutation is not a prognostic marker for chemotherapy response [136]. Recently, systematic review articles demonstrated that TP53 mutation is associated with poor overall survival and prognostically significant [137, 138]. TP53 function can be blocked by other mechanisms such as MDM2. MDM2 is frequently amplified, which is known as a major inhibitor of TP53 [139, 140]. It induces a degradation of TP53, and similar functional results as mutation. Amplification of MDM2 is commonly observed in low-grade OS, which usually does not have TP53 mutation [141].
RB1 gene is located on human chromosome 13q14, which is known as a common loss area by cytogenetics in OS tissue. Inactivation of RB1 gene is one of the most common genetic alterations in OS, which is found in up to 70 % of OS patients [142]. Patients with bilateral retinoblastoma have higher risk of subsequent OS [143], and both of them are associated with RB1 gene. RB1 gene is an important regulator of cell cycle, especially G1/S cell cycle transition. When there is a mitogenic signaling, RB1 is phosphorylated by cyclin D/CDK4, cylin D/CDK6, and cyclin E/CDK2 complexes, and it releases E2F transcription factors. Chromatin-remodeling proteins, such as histone deacetylases and histone methyltransferase, which are recruited at hypophosphylated RB state are also released, and promoters become more sensitive [144]. Functional loss of RB1 gene causes persistent transcriptional activation and tumorigenic effect. However, prognostic value of loss of heterozygosity at the RB gene is uncertain [145, 146]. P16 is cyclin-dependent kinase inhibitor and activator of RB dephosphorylation. Deletion of p16 was detected in 7∼16 % OS patients, and loss of p16 expression is correlated with decreased survival [147, 148]. Recently, Borys et al. demonstrated that p16 expression could be used as a predictor of chemotherapy response [149]. Cyclin-dependent kinase 4 (CDK4) and cyclin D1 are negative regulators of p16 [150]. CDK4 and MDM2 are coamplified or overexpressed in low-grade OS including parosteal OS and dedifferentiated type of high-grade OS [151, 152].
RECQL4 gene, a member of RecQ family DNA helicases, mutation is found in Rothmund-Thomson syndrome, which has a higher incidence in OS [8]. Deficiencies of RecQ family helicases result in increased levels of recombination and chromosomal aberrations [153]. However, RECQL4 gene mutation is not common in sporadic OS, and its prognostic value is also limited [154]. Some cytogenetic studies revealed recurrent deletion or loss of heterozygosity at 3q13 in OS, which contains LSAMP gene [155, 156]. Kresse SH et al. presented that low expression of LSAMP gene is associated with poor survival [157].
2.7 Activation of protooncogene
Activator protein-1 (AP-1) is a transcription factor complex containing c-jun, c-fos, and activating transcription factor family. Increased activity of AP-1 is observed in more aggressive OS cell line. Inhibition of AP-1 activity by TAM67, dominant-negative mutant of c-jun, suppresses the migration, invasion, and pulmonary metastasis in experimental murine OS [158]. c-jun and Fra-1, components of AP-1, regulate tumor invasion by controlling the matrix metalloproteinase (MMP)-1 in 143B OS cells [159]. c-fos also induce podoplanin and thereby control cell migration in OS cell lines [160].
Human epidermal growth factor receptor 2, also known as ErbB2/Her2/neu, is overexpressed in various tumors, including breast cancer [161]. In OS, there have been conflicting results of HER-2 status [162–164]. Recent papers suggested that HER2 amplification or overexpression is rarely observed in OS, and differences in the results between studies are due to interpretation of immunohistochemical results based on the poor methodology [165].
RUNX2, a member of transcription factor Runx family, is associated with osteoblast differentiation, and its expression is oscillates during the cell cycle [166, 167]. Although there are some reports of RUNX2 function, which is associated with RB, p53-MDM pathway, and cell cycle regulators, the role of that in OS is uncertain [168–170]. However, its level is elevated in OS cell lines and tissues, and increased expression is associated with metastases, poor response to chemotherapy, and poor prognosis [171, 172].
2.8 MicroRNAs in tumorigenesis
MicroRNAs, small noncoding RNAs, regulate gene expression posttranscriptionally. They function as a tumor suppressor or oncogene [173, 174]. There are several microRNA expression profiling studies, which compared nonneoplastic osteoblast and OS cells [175, 176]. Differentially expressed microRNAs could be involved in OS tumorigenesis and be therapeutic targets. Liu et al. reported that miR-125b is downregulated in OS cell lines and its upstream regulator is STAT3 [177]. MTA1 is known to be another upstream regulator of miR-125b, and it promotes the migration and invasion of nonsmall cell lung cancer cells. miR-199a-3p, miR-143, and miR-145 are also downregulated in OS cell lines and function as tumor suppressor [178–181]. miR-21 is overexpressed in OS tissues and negatively regulates RECK gene [182]. miR-199b-5p plays a role in Notch signaling in OS [66].
3 Conclusion
Despite of chemotherapeutic advance, survival rate of OS has stagnated for a few decades. New treatment strategies using molecular targets are required to patients who are unresponsive to current therapy. The aforementioned diverse molecular studies have advanced knowledge of OS pathogenesis and roles of MTA1 in OS. Since MTA1 influences on not only various levels of tumorigenesis or tumor progression, but also DNA damage repair, it could be a possible therapeutic target in high grade or metastatic OS. More comprehensive research and investigations are needed to refine and definitize MTA roles in OS pathogenesis.
References
Ottaviani, G., & Jaffe, N. (2009). The epidemiology of osteosarcoma. Cancer Treatment and Research, 152, 3–13.
Mirabello, L., Troisi, R. J., & Savage, S. A. (2009). Osteosarcoma incidence and survival rates from 1973 to 2004: data from the Surveillance, Epidemiology, and End Results Program. Cancer, 115(7), 1531–1543.
Siegel, R., Ma, J., Zou, Z., & Jemal, A. (2014). Cancer statistics, 2014. CA: A Cancer Journal for Clinicians, 64(1), 9–29.
Hansen, M. F., Seton, M., & Merchant, A. (2006). Osteosarcoma in Paget’s disease of bone. Journal of Bone and Mineral Research, 21(Suppl 2), 58–63.
Ottaviani, G., & Jaffe, N. (2009). The etiology of osteosarcoma. Cancer Treatment and Research, 152, 15–32.
Doganavsargil, B., Argin, M., Kececi, B., Sezak, M., Sanli, U. A., & Oztop, F. (2009). Secondary osteosarcoma arising in fibrous dysplasia, case report. Archives of Orthopaedic and Traumatic Surgery, 129(4), 439–444.
Carnevale, A., Lieberman, E., & Cardenas, R. (1997). Li-Fraumeni syndrome in pediatric patients with soft tissue sarcoma or osteosarcoma. Archives of Medical Research, 28(3), 383–386.
Wang, L. L., Gannavarapu, A., Kozinetz, C. A., Levy, M. L., Lewis, R. A., Chintagumpala, M. M., et al. (2003). Association between osteosarcoma and deleterious mutations in the RECQL4 gene in Rothmund-Thomson syndrome. Journal of the National Cancer Institute, 95(9), 669–674.
Liu, J. J., Liu, S., Wang, J. G., Zhu, W., Hua, Y. Q., Sun, W., et al. (2013). Telangiectatic osteosarcoma: a review of literature. OncoTargets and Therapy, 6, 593–602.
DeLaney, T. F., Park, L., Goldberg, S. I., Hug, E. B., Liebsch, N. J., Munzenrider, J. E., et al. (2005). Radiotherapy for local control of osteosarcoma. International Journal of Radiation Oncology, Biology, Physics, 61(2), 492–498.
Davis, A. M., Bell, R. S., & Goodwin, P. J. (1994). Prognostic factors in osteosarcoma: a critical review. Journal of Clinical Oncology, 12(2), 423–431.
Bieling, P., Rehan, N., Winkler, P., Helmke, K., Maas, R., Fuchs, N., et al. (1996). Tumor size and prognosis in aggressively treated osteosarcoma. Journal of Clinical Oncology, 14(3), 848–858.
Bacci, G., Bertoni, F., Longhi, A., Ferrari, S., Forni, C., Biagini, R., et al. (2003). Neoadjuvant chemotherapy for high-grade central osteosarcoma of the extremity. Histologic response to preoperative chemotherapy correlates with histologic subtype of the tumor. Cancer, 97(12), 3068–3075.
Lee, J. A., Kim, M. S., Kim, D. H., Lim, J. S., Yoo, J. Y., Koh, J. S., et al. (2008). Relative tumor burden predicts metastasis-free survival in pediatric osteosarcoma. Pediatric Blood & Cancer, 50(2), 195–200.
Bacci, G., Longhi, A., Versari, M., Mercuri, M., Briccoli, A., & Picci, P. (2006). Prognostic factors for osteosarcoma of the extremity treated with neoadjuvant chemotherapy: 15-year experience in 789 patients treated at a single institution. Cancer, 106(5), 1154–1161.
Han, I., Oh, J. H., Na, Y. G., Moon, K. C., & Kim, H. S. (2008). Clinical outcome of parosteal osteosarcoma. Journal of Surgical Oncology, 97(2), 146–149.
Revell, M. P., Deshmukh, N., Grimer, R. J., Carter, S. R., & Tillman, R. M. (2002). Periosteal osteosarcoma: a review of 17 cases with mean follow-up of 52 months. Sarcoma, 6(4), 123–130.
Toh, Y., & Nicolson, G. L. (2009). The role of the MTA family and their encoded proteins in human cancers: molecular functions and clinical implications. Clinical & Experimental Metastasis, 26(3), 215–227.
Li, D. Q., Pakala, S. B., Nair, S. S., Eswaran, J., & Kumar, R. (2012). Metastasis-associated protein 1/nucleosome remodeling and histone deacetylase complex in cancer. Cancer Research, 72(2), 387–394.
Martin, M. D., Fischbach, K., Osborne, C. K., Mohsin, S. K., Allred, D. C., & O’Connell, P. (2001). Loss of heterozygosity events impeding breast cancer metastasis contain the MTA1 gene. Cancer Research, 61(9), 3578–3580.
Toh, Y., Ohga, T., Endo, K., Adachi, E., Kusumoto, H., Haraguchi, M., et al. (2004). Expression of the metastasis-associated MTA1 protein and its relationship to deacetylation of the histone H4 in esophageal squamous cell carcinomas. International Journal of Cancer, 110(3), 362–367.
Toh, Y., Oki, E., Oda, S., Tokunaga, E., Ohno, S., Maehara, Y., et al. (1997). Overexpression of the MTA1 gene in gastrointestinal carcinomas: correlation with invasion and metastasis. International Journal of Cancer, 74(4), 459–463.
Kidd, M., Modlin, I. M., Mane, S. M., Camp, R. L., Eick, G., & Latich, I. (2006). The role of genetic markers—NAP1L1, MAGE-D2, and MTA1—in defining small-intestinal carcinoid neoplasia. Annals of Surgical Oncology, 13(2), 253–262.
Sasaki, H., Moriyama, S., Nakashima, Y., Kobayashi, Y., Yukiue, H., Kaji, M., et al. (2002). Expression of the MTA1 mRNA in advanced lung cancer. Lung Cancer, 35(2), 149–154.
Dannenmann, C., Shabani, N., Friese, K., Jeschke, U., Mylonas, I., & Bruning, A. (2008). The metastasis-associated gene MTA1 is upregulated in advanced ovarian cancer, represses ERbeta, and enhances expression of oncogenic cytokine GRO. Cancer Biology & Therapy, 7(9), 1460–1467.
Hofer, M. D., Kuefer, R., Varambally, S., Li, H., Ma, J., Shapiro, G. I., et al. (2004). The role of metastasis-associated protein 1 in prostate cancer progression. Cancer Research, 64(3), 825–829.
Park, H. R., Jung, W. W., Kim, H. S., Bacchini, P., Bertoni, F., & Park, Y. K. (2005). Overexpression of metastatic tumor antigen in osteosarcoma: comparison between conventional high-grade and central low-grade osteosarcoma. Cancer Research and Treatment, 37(6), 360–364.
Ferrari, S., Smeland, S., Mercuri, M., Bertoni, F., Longhi, A., Ruggieri, P., et al. (2005). Neoadjuvant chemotherapy with high-dose Ifosfamide, high-dose methotrexate, cisplatin, and doxorubicin for patients with localized osteosarcoma of the extremity: a joint study by the Italian and Scandinavian Sarcoma Groups. Journal of Clinical Oncology, 23(34), 8845–8852.
Ta, H. T., Dass, C. R., Choong, P. F., & Dunstan, D. E. (2009). Osteosarcoma treatment: state of the art. Cancer Metastasis Reviews, 28(1–2), 247–263.
Briccoli, A., Rocca, M., Salone, M., Guzzardella, G. A., Balladelli, A., & Bacci, G. (2010). High grade osteosarcoma of the extremities metastatic to the lung: long-term results in 323 patients treated combining surgery and chemotherapy, 1985–2005. Surgical Oncology, 19(4), 193–199.
Toh, Y., Pencil, S. D., & Nicolson, G. L. (1995). Analysis of the complete sequence of the novel metastasis-associated candidate gene, mta1, differentially expressed in mammary adenocarcinoma and breast cancer cell lines. Gene, 159(1), 97–104.
Molli, P. R., Singh, R. R., Lee, S. W., & Kumar, R. (2008). MTA1-mediated transcriptional repression of BRCA1 tumor suppressor gene. Oncogene, 27(14), 1971–1980.
Yoo, Y. G., Na, T. Y., Seo, H. W., Seong, J. K., Park, C. K., Shin, Y. K., et al. (2008). Hepatitis B virus X protein induces the expression of MTA1 and HDAC1, which enhances hypoxia signaling in hepatocellular carcinoma cells. Oncogene, 27(24), 3405–3413.
Jang, K. S., Paik, S. S., Chung, H., Oh, Y. H., & Kong, G. (2006). MTA1 overexpression correlates significantly with tumor grade and angiogenesis in human breast cancers. Cancer Science, 97(5), 374–379.
Li, S. H., Tian, H., Yue, W. M., Li, L., Li, W. J., Chen, Z. T., et al. (2011). Overexpression of metastasis-associated protein 1 is significantly correlated with tumor angiogenesis and poor survival in patients with early-stage non-small cell lung cancer. Annals of Surgical Oncology, 18(7), 2048–2056.
Kai, L., Wang, J., Ivanovic, M., Chung, Y. T., Laskin, W. B., Schulze-Hoepfner, F., et al. (2011). Targeting prostate cancer angiogenesis through metastasis-associated protein 1 (MTA1). Prostate, 71(3), 268–280.
Li, S. H., Tian, H., Yue, W. M., Li, L., Gao, C., Li, W. J., et al. (2012). Metastasis-associated protein 1 nuclear expression is closely associated with tumor progression and angiogenesis in patients with esophageal squamous cell cancer. World Journal of Surgery, 36(3), 623–631.
Deng, X., Du, L., Wang, C., Yang, Y., Li, J., Liu, H., et al. (2013). Close association of metastasis-associated protein 1 overexpression with increased angiogenesis and poor survival in patients with histologically node-negative gastric cancer. World Journal of Surgery, 37(4), 792–798.
Park, H. R., Cabrini, R. L., Araujo, E. S., Paparella, M. L., Brandizzi, D., & Park, Y. K. (2009). Expression of ezrin and metastatic tumor antigen in osteosarcomas of the jaw. Tumori, 95(1), 81–86.
Choi, K. S., Bae, M. K., Jeong, J. W., Moon, H. E., & Kim, K. W. (2003). Hypoxia-induced angiogenesis during carcinogenesis. Journal of Biochemistry and Molecular Biology, 36(1), 120–127.
Ito, T. K., Ishii, G., Chiba, H., & Ochiai, A. (2007). The VEGF angiogenic switch of fibroblasts is regulated by MMP-7 from cancer cells. Oncogene, 26(51), 7194–7203.
Figueras, A., Arbos, M. A., Quiles, M. T., Vinals, F., Germa, J. R., & Capella, G. (2013). The impact of KRAS mutations on VEGF-A production and tumour vascular network. BMC Cancer, 13, 125.
O’Reilly, M. S., Holmgren, L., Shing, Y., Chen, C., Rosenthal, R. A., Moses, M., et al. (1994). Angiostatin: a novel angiogenesis inhibitor that mediates the suppression of metastases by a Lewis lung carcinoma. Cell, 79(2), 315–328.
O’Reilly, M. S., Boehm, T., Shing, Y., Fukai, N., Vasios, G., Lane, W. S., et al. (1997). Endostatin: an endogenous inhibitor of angiogenesis and tumor growth. Cell, 88(2), 277–285.
Tsuchida, R., Osawa, T., Wang, F., Nishii, R., Das, B., Tsuchida, S., et al. (2014). BMP4/Thrombospondin-1 loop paracrinically inhibits tumor angiogenesis and suppresses the growth of solid tumors. Oncogene, 33(29), 3803–3811.
Kim, H. S., Lim, S. J., & Park, Y. K. (2009). Anti-angiogenic factor endostatin in osteosarcoma. APMIS, 117(10), 716–723.
Lammli, J., Fan, M., Rosenthal, H. G., Patni, M., Rinehart, E., Vergara, G., et al. (2012). Expression of vascular endothelial growth factor correlates with the advance of clinical osteosarcoma. International Orthopaedics, 36(11), 2307–2313.
Rastogi, S., Kumar, R., Sankineani, S. R., Marimuthu, K., Rijal, L., Prakash, S., et al. (2012). Role of vascular endothelial growth factor as a tumour marker in osteosarcoma: a prospective study. International Orthopaedics, 36(11), 2315–2321.
Roncuzzi, L., Pancotti, F., & Baldini, N. (2014). Involvement of HIF-1alpha activation in the doxorubicin resistance of human osteosarcoma cells. Oncology Reports, 32(1), 389–394.
Yang, Q. C., Zeng, B. F., Dong, Y., Shi, Z. M., Jiang, Z. M., & Huang, J. (2007). Overexpression of hypoxia-inducible factor-1alpha in human osteosarcoma: correlation with clinicopathological parameters and survival outcome. Japanese Journal of Clinical Oncology, 37(2), 127–134.
Yoo, Y. G., Kong, G., & Lee, M. O. (2006). Metastasis-associated protein 1 enhances stability of hypoxia-inducible factor-1alpha protein by recruiting histone deacetylase 1. EMBO Journal, 25(6), 1231–1241.
Moon, H. E., Cheon, H., Chun, K. H., Lee, S. K., Kim, Y. S., Jung, B. K., et al. (2006). Metastasis-associated protein 1 enhances angiogenesis by stabilization of HIF-1alpha. Oncology Reports, 16(4), 929–935.
Birner, P., Schindl, M., Obermair, A., Breitenecker, G., & Oberhuber, G. (2001). Expression of hypoxia-inducible factor 1alpha in epithelial ovarian tumors: its impact on prognosis and on response to chemotherapy. Clinical Cancer Research, 7(6), 1661–1668.
Schindl, M., Schoppmann, S. F., Samonigg, H., Hausmaninger, H., Kwasny, W., Gnant, M., et al. (2002). Overexpression of hypoxia-inducible factor 1alpha is associated with an unfavorable prognosis in lymph node-positive breast cancer. Clinical Cancer Research, 8(6), 1831–1837.
Shibaji, T., Nagao, M., Ikeda, N., Kanehiro, H., Hisanaga, M., Ko, S., et al. (2003). Prognostic significance of HIF-1 alpha overexpression in human pancreatic cancer. Anticancer Research, 23(6C), 4721–4727.
El Naggar, A., Clarkson, P., Zhang, F., Mathers, J., Tognon, C., & Sorensen, P. H. (2012). Expression and stability of hypoxia inducible factor 1alpha in osteosarcoma. Pediatric Blood & Cancer, 59(7), 1215–1222.
Chen, Y., Yang, Y., Yuan, Z., Wang, C., & Shi, Y. (2012). Predicting chemosensitivity in osteosarcoma prior to chemotherapy: an investigational study of biomarkers with immunohistochemistry. Oncology Letters, 3(5), 1011–1016.
McMahon, G. (2000). VEGF receptor signaling in tumor angiogenesis. The Oncologist, 5(Suppl 1), 3–10.
Dong, G., Chen, Z., Li, Z. Y., Yeh, N. T., Bancroft, C. C., & Van Waes, C. (2001). Hepatocyte growth factor/scatter factor-induced activation of MEK and PI3K signal pathways contributes to expression of proangiogenic cytokines interleukin-8 and vascular endothelial growth factor in head and neck squamous cell carcinoma. Cancer Research, 61(15), 5911–5918.
Yu, X. W., Wu, T. Y., Yi, X., Ren, W. P., Zhou, Z. B., Sun, Y. Q., et al. (2014). Prognostic significance of VEGF expression in osteosarcoma: a meta-analysis. Tumour Biology, 35(1), 155–160.
Qu, J. T., Wang, M., He, H. L., Tang, Y., & Ye, X. J. (2012). The prognostic value of elevated vascular endothelial growth factor in patients with osteosarcoma: a meta-analysis and systemic review. Journal of Cancer Research and Clinical Oncology, 138(5), 819–825.
Nagaraj, S. R., Shilpa, P., Rachaiah, K., & Salimath, B. P. (2013). Crosstalk between VEGF and MTA1 signaling pathways contribute to aggressiveness of breast carcinoma. Molecular Carcinogenesis. doi:10.1002/mc.22104.
Garcia, A., & Kandel, J. J. (2012). Notch: a key regulator of tumor angiogenesis and metastasis. Histology and Histopathology, 27(2), 151–156.
Hughes, D. P. (2009). How the NOTCH pathway contributes to the ability of osteosarcoma cells to metastasize. Cancer Treatment and Research, 152, 479–496.
Mu, X., Isaac, C., Greco, N., Huard, J., & Weiss, K. (2013). Notch signaling is associated with ALDH activity and an aggressive metastatic phenotype in murine osteosarcoma cells. Frontiers in Oncology, 3, 143.
Won, K. Y., Kim, Y. W., Kim, H. S., Lee, S. K., Jung, W. W., & Park, Y. K. (2013). MicroRNA-199b-5p is involved in the Notch signaling pathway in osteosarcoma. Human Pathology, 44(8), 1648–1655.
Morley, M. E., Riches, K., Peers, C., & Porter, K. E. (2007). Hypoxic inhibition of human cardiac fibroblast invasion and MMP-2 activation may impair adaptive myocardial remodelling. Biochemical Society Transactions, 35(Pt 5), 905–907.
Jodele, S., Blavier, L., Yoon, J. M., & DeClerck, Y. A. (2006). Modifying the soil to affect the seed: role of stromal-derived matrix metalloproteinases in cancer progression. Cancer Metastasis Reviews, 25(1), 35–43.
Wang, G., Wang, W., Zhou, J., & Yang, X. (2013). Correlation between telomerase activity and matrix metalloproteinases 2 expression in gastric cancer. Cancer Biomarkers, 13(1), 21–28.
Zhao, S., Ma, W., Zhang, M., Tang, D., Shi, Q., Xu, S., et al. (2013). High expression of CD147 and MMP-9 is correlated with poor prognosis of triple-negative breast cancer (TNBC) patients. Medical Oncology, 30(1), 335.
Jiang, Q., Zhang, H., & Zhang, P. (2011). ShRNA-mediated gene silencing of MTA1 influenced on protein expression of ER alpha, MMP-9, CyclinD1 and invasiveness, proliferation in breast cancer cell lines MDA-MB-231 and MCF-7 in vitro. Journal of Experimental & Clinical Cancer Research, 30, 60.
Weng, W., Yin, J., Zhang, Y., Qiu, J., & Wang, X. (2014). Metastasis-associated protein 1 promotes tumor invasion by downregulation of E-cadherin. International Journal of Oncology, 44(3), 812–818.
Wen, X., Liu, H., Yu, K., & Liu, Y. (2014). Matrix metalloproteinase 2 expression and survival of patients with osteosarcoma: a meta-analysis. Tumour Biology, 35(1), 845–848.
Li, H., Zhang, K., Liu, L. H., Ouyang, Y., Bu, J., Guo, H. B., et al. (2014). A systematic review of matrix metalloproteinase 9 as a biomarker of survival in patients with osteosarcoma. Tumour Biology, 35(6), 5487–5491.
Jin, J., Cai, L., Liu, Z. M., & Zhou, X. S. (2013). miRNA-218 inhibits osteosarcoma cell migration and invasion by down-regulating of TIAM1, MMP2 and MMP9. Asian Pacific Journal of Cancer Prevention, 14(6), 3681–3684.
Husmann, K., Arlt, M. J., Muff, R., Langsam, B., Bertz, J., Born, W., et al. (2013). Matrix metalloproteinase 1 promotes tumor formation and lung metastasis in an intratibial injection osteosarcoma mouse model. Biochimica et Biophysica Acta, 1832(2), 347–354.
Decock, J., Long, J. R., Laxton, R. C., Shu, X. O., Hodgkinson, C., Hendrickx, W., et al. (2007). Association of matrix metalloproteinase-8 gene variation with breast cancer prognosis. Cancer Research, 67(21), 10214–10221.
Balbin, M., Fueyo, A., Tester, A. M., Pendas, A. M., Pitiot, A. S., Astudillo, A., et al. (2003). Loss of collagenase-2 confers increased skin tumor susceptibility to male mice. Nature Genetics, 35(3), 252–257.
Korpi, J. T., Hagstrom, J., Lehtonen, N., Parkkinen, J., Sorsa, T., Salo, T., et al. (2011). Expression of matrix metalloproteinases-2, −8, −13, −26, and tissue inhibitors of metalloproteinase-1 in human osteosarcoma. Surgical Oncology, 20(1), e18–e22.
Cai, Y., Cai, T., & Chen, Y. (2014). Wnt pathway in osteosarcoma, from oncogenic to therapeutic. Journal of Cellular Biochemistry, 115(4), 625–631.
Kumar, R., Balasenthil, S., Pakala, S. B., Rayala, S. K., Sahin, A. A., & Ohshiro, K. (2010). Metastasis-associated protein 1 short form stimulates Wnt1 pathway in mammary epithelial and cancer cells. Cancer Research, 70(16), 6598–6608.
Yan, D., Avtanski, D., Saxena, N. K., & Sharma, D. (2012). Leptin-induced epithelial-mesenchymal transition in breast cancer cells requires beta-catenin activation via Akt/GSK3- and MTA1/Wnt1 protein-dependent pathways. Journal of Biological Chemistry, 287(11), 8598–8612.
Lu, Y., Wei, C., & Xi, Z. (2014). Curcumin suppresses proliferation and invasion in non-small cell lung cancer by modulation of MTA1-mediated Wnt/beta-catenin pathway. In Vitro Cellular & Developmental Biology. Animal. doi:10.1007/s11626-014-9779-5.
Guo, Y., Rubin, E. M., Xie, J., Zi, X., & Hoang, B. H. (2008). Dominant negative LRP5 decreases tumorigenicity and metastasis of osteosarcoma in an animal model. Clinical Orthopaedics and Related Research, 466(9), 2039–2045.
Guo, Y., Zi, X., Koontz, Z., Kim, A., Xie, J., Gorlick, R., et al. (2007). Blocking Wnt/LRP5 signaling by a soluble receptor modulates the epithelial to mesenchymal transition and suppresses met and metalloproteinases in osteosarcoma Saos-2 cells. Journal of Orthopaedic Research, 25(7), 964–971.
Ma, Y., Ren, Y., Han, E. Q., Li, H., Chen, D., Jacobs, J. J., et al. (2013). Inhibition of the Wnt-beta-catenin and Notch signaling pathways sensitizes osteosarcoma cells to chemotherapy. Biochemical and Biophysical Research Communications, 431(2), 274–279.
Yang, G., Yuan, J., & Li, K. (2013). EMT transcription factors: implication in osteosarcoma. Medical Oncology, 30(4), 697.
Tuncay Cagatay, S., Cimen, I., Savas, B., & Banerjee, S. (2013). MTA-1 expression is associated with metastasis and epithelial to mesenchymal transition in colorectal cancer cells. Tumour Biology, 34(2), 1189–1204.
Yang, H., Zhang, Y., Zhou, Z., Jiang, X., & Shen, A. (2014). Transcription factor Snai1-1 induces osteosarcoma invasion and metastasis by inhibiting E-cadherin expression. Oncology Letters, 8(1), 193–197.
Sharili, A. S., Allen, S., Smith, K., Hargreaves, J., Price, J., & McGonnell, I. (2011). Expression of Snail2 in long bone osteosarcomas correlates with tumour malignancy. Tumour Biology, 32(3), 515–526.
Sharili, A. S., Allen, S., Smith, K., Price, J., & McGonnell, I. M. (2013). Snail2 promotes osteosarcoma cell motility through remodelling of the actin cytoskeleton and regulates tumor development. Cancer Letters, 333(2), 170–179.
Fan, L., Wang, H., Xia, X., Rao, Y., Ma, X., Ma, D., et al. (2012). Loss of E-cadherin promotes prostate cancer metastasis via upregulation of metastasis-associated gene 1 expression. Oncology Letters, 4(6), 1225–1233.
Wang, H., Fan, L., Wei, J., Weng, Y., Zhou, L., Shi, Y., et al. (2012). Akt mediates metastasis-associated gene 1 (MTA1) regulating the expression of E-cadherin and promoting the invasiveness of prostate cancer cells. PloS One, 7(12), e46888.
Khan, M. A., Chen, H. C., Zhang, D., & Fu, J. (2013). Twist: a molecular target in cancer therapeutics. Tumour Biology, 34(5), 2497–2506.
Zhou, Y., Zang, X., Huang, Z., & Zhang, C. (2013). TWIST interacts with endothelin-1/endothelin A receptor signaling in osteosarcoma cell survival against cisplatin. Oncology Letters, 5(3), 857–861.
Wu, J., Liao, Q., He, H., Zhong, D., & Yin, K. (2014). TWIST interacts with beta-catenin signaling on osteosarcoma cell survival against cisplatin. Molecular Carcinogenesis, 53(6), 440–446.
Zhou, Y., Huang, Z., Wu, S., Zang, X., Liu, M., & Shi, J. (2014). miR-33a is up-regulated in chemoresistant osteosarcoma and promotes osteosarcoma cell resistance to cisplatin by down-regulating TWIST. Journal of Experimental & Clinical Cancer Research, 33, 12.
Yin, K., Liao, Q., He, H., & Zhong, D. (2012). Prognostic value of Twist and E-cadherin in patients with osteosarcoma. Medical Oncology, 29(5), 3449–3455.
Egloff, A. M., & Grandis, J. R. (2008). Targeting epidermal growth factor receptor and SRC pathways in head and neck cancer. Seminars in Oncology, 35(3), 286–297.
Mori, S., Ronnstrand, L., Yokote, K., Engstrom, A., Courtneidge, S. A., Claesson-Welsh, L., et al. (1993). Identification of two juxtamembrane autophosphorylation sites in the PDGF beta-receptor; involvement in the interaction with Src family tyrosine kinases. EMBO Journal, 12(6), 2257–2264.
Playford, M. P., & Schaller, M. D. (2004). The interplay between Src and integrins in normal and tumor biology. Oncogene, 23(48), 7928–7946.
Cheranov, S. Y., Karpurapu, M., Wang, D., Zhang, B., Venema, R. C., & Rao, G. N. (2008). An essential role for SRC-activated STAT-3 in 14,15-EET-induced VEGF expression and angiogenesis. Blood, 111(12), 5581–5591.
Brunton, V. G., & Frame, M. C. (2008). Src and focal adhesion kinase as therapeutic targets in cancer. Current Opinion in Pharmacology, 8(4), 427–432.
Hingorani, P., Zhang, W., Gorlick, R., & Kolb, E. A. (2009). Inhibition of Src phosphorylation alters metastatic potential of osteosarcoma in vitro but not in vivo. Clinical Cancer Research, 15(10), 3416–3422.
Strauss, S. J., Ng, T., Mendoza-Naranjo, A., Whelan, J., & Sorensen, P. H. (2010). Understanding micrometastatic disease and Anoikis resistance in ewing family of tumors and osteosarcoma. The Oncologist, 15(6), 627–635.
Frisch, S. M., & Francis, H. (1994). Disruption of epithelial cell-matrix interactions induces apoptosis. Journal of Cell Biology, 124(4), 619–626.
Jost, M., Huggett, T. M., Kari, C., & Rodeck, U. (2001). Matrix-independent survival of human keratinocytes through an EGF receptor/MAPK-kinase-dependent pathway. Molecular Biology of the Cell, 12(5), 1519–1527.
Jost, M., Huggett, T. M., Kari, C., Boise, L. H., & Rodeck, U. (2001). Epidermal growth factor receptor-dependent control of keratinocyte survival and Bcl-xL expression through a MEK-dependent pathway. Journal of Biological Chemistry, 276(9), 6320–6326.
Sakuma, Y., Yamazaki, Y., Nakamura, Y., Yoshihara, M., Matsukuma, S., Nakayama, H., et al. (2012). WZ4002, a third-generation EGFR inhibitor, can overcome anoikis resistance in EGFR-mutant lung adenocarcinomas more efficiently than Src inhibitors. Laboratory Investigation, 92(3), 371–383.
Mahoney, M. G., Simpson, A., Jost, M., Noe, M., Kari, C., Pepe, D., et al. (2002). Metastasis-associated protein (MTA)1 enhances migration, invasion, and anchorage-independent survival of immortalized human keratinocytes. Oncogene, 21(14), 2161–2170.
Diaz-Montero, C. M., Wygant, J. N., & McIntyre, B. W. (2006). PI3-K/Akt-mediated anoikis resistance of human osteosarcoma cells requires Src activation. European Journal of Cancer, 42(10), 1491–1500.
Cantiani, L., Manara, M. C., Zucchini, C., De Sanctis, P., Zuntini, M., Valvassori, L., et al. (2007). Caveolin-1 reduces osteosarcoma metastases by inhibiting c-Src activity and met signaling. Cancer Research, 67(16), 7675–7685.
Wan, X., Kim, S. Y., Guenther, L. M., Mendoza, A., Briggs, J., Yeung, C., et al. (2009). Beta4 integrin promotes osteosarcoma metastasis and interacts with ezrin. Oncogene, 28(38), 3401–3411.
Jeffree, G. M., Price, C. H., & Sissons, H. A. (1975). The metastatic patterns of osteosarcoma. British Journal of Cancer, 32(1), 87–107.
Laverdiere, C., Hoang, B. H., Yang, R., Sowers, R., Qin, J., Meyers, P. A., et al. (2005). Messenger RNA expression levels of CXCR4 correlate with metastatic behavior and outcome in patients with osteosarcoma. Clinical Cancer Research, 11(7), 2561–2567.
Sun, X., Cheng, G., Hao, M., Zheng, J., Zhou, X., Zhang, J., et al. (2010). CXCL12/CXCR4/CXCR7 chemokine axis and cancer progression. Cancer Metastasis Reviews, 29(4), 709–722.
Kaplan, R. N., Psaila, B., & Lyden, D. (2006). Bone marrow cells in the ‘pre-metastatic niche’: within bone and beyond. Cancer Metastasis Reviews, 25(4), 521–529.
Ando, K., Mori, K., Verrecchia, F., Marc, B., Redini, F., & Heymann, D. (2012). Molecular alterations associated with osteosarcoma development. Sarcoma, 2012, 523432.
Balkwill, F. (2004). Cancer and the chemokine network. Nature Reviews Cancer, 4(7), 540–550.
Zagzag, D., Lukyanov, Y., Lan, L., Ali, M. A., Esencay, M., Mendez, O., et al. (2006). Hypoxia-inducible factor 1 and VEGF upregulate CXCR4 in glioblastoma: implications for angiogenesis and glioma cell invasion. Laboratory Investigation, 86(12), 1221–1232.
Brennecke, P., Arlt, M. J., Muff, R., Campanile, C., Gvozdenovic, A., Husmann, K., et al. (2013). Expression of the chemokine receptor CXCR7 in CXCR4-expressing human 143B osteosarcoma cells enhances lung metastasis of intratibial xenografts in SCID mice. PloS One, 8(9), e74045.
Brennecke, P., Arlt, M. J., Campanile, C., Husmann, K., Gvozdenovic, A., Apuzzo, T., et al. (2014). CXCR4 antibody treatment suppresses metastatic spread to the lung of intratibial human osteosarcoma xenografts in mice. Clinical & Experimental Metastasis, 31(3), 339–349.
Zhang, Y., Zhang, L., Zhang, G., Li, S., Duan, J., Cheng, J., et al. (2014). Osteosarcoma metastasis: prospective role of ezrin. Tumour Biology, 35(6), 5055–5059.
Khanna, C., Wan, X., Bose, S., Cassaday, R., Olomu, O., Mendoza, A., et al. (2004). The membrane-cytoskeleton linker ezrin is necessary for osteosarcoma metastasis. Nature Medicine, 10(2), 182–186.
Ferrari, S., Zanella, L., Alberghini, M., Palmerini, E., Staals, E., & Bacchini, P. (2008). Prognostic significance of immunohistochemical expression of ezrin in non-metastatic high-grade osteosarcoma. Pediatric Blood & Cancer, 50(4), 752–756.
Li, H., Min, D., Zhao, H., Wang, Z., Qi, W., Zheng, S., et al. (2013). The prognostic role of ezrin immunoexpression in osteosarcoma: a meta-analysis of published data. PloS One, 8(6), e64513.
Lun, D. X., Hu, Y. C., Xu, Z. W., Xu, L. N., & Wang, B. W. (2014). The prognostic value of elevated ezrin in patients with osteosarcoma. Tumour Biology, 35(2), 1263–1266.
Zhu, J., Feng, Y., Ke, Z., Yang, Z., Zhou, J., Huang, X., et al. (2012). Down-regulation of miR-183 promotes migration and invasion of osteosarcoma by targeting Ezrin. American Journal of Pathology, 180(6), 2440–2451.
Mu, Y., Zhang, H., Che, L., & Li, K. (2014). Clinical significance of microRNA-183/Ezrin axis in judging the prognosis of patients with osteosarcoma. Medical Oncology, 31(2), 821.
Li, D. Q., Divijendra Natha Reddy, S., Pakala, S. B., Wu, X., Zhang, Y., Rayala, S. K., et al. (2009). MTA1 coregulator regulates p53 stability and function. Journal of Biological Chemistry, 284(50), 34545–34552.
Li, D. Q., Pakala, S. B., Reddy, S. D., Ohshiro, K., Peng, S. H., Lian, Y., et al. (2010). Revelation of p53-independent function of MTA1 in DNA damage response via modulation of the p21 WAF1-proliferating cell nuclear antigen pathway. Journal of Biological Chemistry, 285(13), 10044–10052.
Lee, M. H., Na, H., Kim, E. J., Lee, H. W., & Lee, M. O. (2012). Poly(ADP-ribosyl)ation of p53 induces gene-specific transcriptional repression of MTA1. Oncogene, 31(49), 5099–5107.
Birch, J. M., Alston, R. D., McNally, R. J., Evans, D. G., Kelsey, A. M., Harris, M., et al. (2001). Relative frequency and morphology of cancers in carriers of germline TP53 mutations. Oncogene, 20(34), 4621–4628.
Gokgoz, N., Wunder, J. S., Mousses, S., Eskandarian, S., Bell, R. S., & Andrulis, I. L. (2001). Comparison of p53 mutations in patients with localized osteosarcoma and metastatic osteosarcoma. Cancer, 92(8), 2181–2189.
Tsuchiya, T., Sekine, K., Hinohara, S., Namiki, T., Nobori, T., & Kaneko, Y. (2000). Analysis of the p16INK4, p14ARF, p15, TP53, and MDM2 genes and their prognostic implications in osteosarcoma and Ewing sarcoma. Cancer Genetics and Cytogenetics, 120(2), 91–98.
Pakos, E. E., Kyzas, P. A., & Ioannidis, J. P. (2004). Prognostic significance of TP53 tumor suppressor gene expression and mutations in human osteosarcoma: a meta-analysis. Clinical Cancer Research, 10(18 Pt 1), 6208–6214.
Jiang, L., Tao, C., & He, A. (2013). Prognostic significance of p53 expression in malignant bone tumors: a meta-analysis. Tumour Biology, 34(2), 1037–1043.
Fu, H. L., Shao, L., Wang, Q., Jia, T., Li, M., & Yang, D. P. (2013). A systematic review of p53 as a biomarker of survival in patients with osteosarcoma. Tumour Biology, 34(6), 3817–3821.
Florenes, V. A., Maelandsmo, G. M., Forus, A., Andreassen, A., Myklebost, O., & Fodstad, O. (1994). MDM2 gene amplification and transcript levels in human sarcomas: relationship to TP53 gene status. Journal of the National Cancer Institute, 86(17), 1297–1302.
Miller, C. W., Aslo, A., Won, A., Tan, M., Lampkin, B., & Koeffler, H. P. (1996). Alterations of the p53, Rb and MDM2 genes in osteosarcoma. Journal of Cancer Research and Clinical Oncology, 122(9), 559–565.
Mejia-Guerrero, S., Quejada, M., Gokgoz, N., Gill, M., Parkes, R. K., Wunder, J. S., et al. (2010). Characterization of the 12q15 MDM2 and 12q13-14 CDK4 amplicons and clinical correlations in osteosarcoma. Genes, Chromosomes & Cancer, 49(6), 518–525.
Wadayama, B., Toguchida, J., Shimizu, T., Ishizaki, K., Sasaki, M. S., Kotoura, Y., et al. (1994). Mutation spectrum of the retinoblastoma gene in osteosarcomas. Cancer Research, 54(11), 3042–3048.
Eng, C., Li, F. P., Abramson, D. H., Ellsworth, R. M., Wong, F. L., Goldman, M. B., et al. (1993). Mortality from second tumors among long-term survivors of retinoblastoma. Journal of the National Cancer Institute, 85(14), 1121–1128.
Brehm, A., Miska, E. A., McCance, D. J., Reid, J. L., Bannister, A. J., & Kouzarides, T. (1998). Retinoblastoma protein recruits histone deacetylase to repress transcription. Nature, 391(6667), 597–601.
Feugeas, O., Guriec, N., Babin-Boilletot, A., Marcellin, L., Simon, P., Babin, S., et al. (1996). Loss of heterozygosity of the RB gene is a poor prognostic factor in patients with osteosarcoma. Journal of Clinical Oncology, 14(2), 467–472.
Heinsohn, S., Evermann, U., Zur Stadt, U., Bielack, S., & Kabisch, H. (2007). Determination of the prognostic value of loss of heterozygosity at the retinoblastoma gene in osteosarcoma. International Journal of Oncology, 30(5), 1205–1214.
Patino-Garcia, A., & Sierrasesumaga, L. (1997). Analysis of the p16INK4 and TP53 tumor suppressor genes in bone sarcoma pediatric patients. Cancer Genetics and Cytogenetics, 98(1), 50–55.
Maitra, A., Roberts, H., Weinberg, A. G., & Geradts, J. (2001). Loss of p16(INK4a) expression correlates with decreased survival in pediatric osteosarcomas. International Journal of Cancer, 95(1), 34–38.
Borys, D., Canter, R. J., Hoch, B., Martinez, S. R., Tamurian, R. M., Murphy, B., et al. (2012). P16 expression predicts necrotic response among patients with osteosarcoma receiving neoadjuvant chemotherapy. Human Pathology, 43(11), 1948–1954.
Wei, G., Lonardo, F., Ueda, T., Kim, T., Huvos, A. G., Healey, J. H., et al. (1999). CDK4 gene amplification in osteosarcoma: reciprocal relationship with INK4A gene alterations and mapping of 12q13 amplicons. International Journal of Cancer, 80(2), 199–204.
Wunder, J. S., Eppert, K., Burrow, S. R., Gokgoz, N., Bell, R. S., & Andrulis, I. L. (1999). Co-amplification and overexpression of CDK4, SAS and MDM2 occurs frequently in human parosteal osteosarcomas. Oncogene, 18(3), 783–788.
Yoshida, A., Ushiku, T., Motoi, T., Beppu, Y., Fukayama, M., Tsuda, H., et al. (2012). MDM2 and CDK4 immunohistochemical coexpression in high-grade osteosarcoma: correlation with a dedifferentiated subtype. American Journal of Surgical Pathology, 36(3), 423–431.
Nakayama, H. (2002). RecQ family helicases: roles as tumor suppressor proteins. Oncogene, 21(58), 9008–9021.
Nishijo, K., Nakayama, T., Aoyama, T., Okamoto, T., Ishibe, T., Yasura, K., et al. (2004). Mutation analysis of the RECQL4 gene in sporadic osteosarcomas. International Journal of Cancer, 111(3), 367–372.
Yen, C. C., Chen, W. M., Chen, T. H., Chen, W. Y., Chen, P. C., Chiou, H. J., et al. (2009). Identification of chromosomal aberrations associated with disease progression and a novel 3q13.31 deletion involving LSAMP gene in osteosarcoma. International Journal of Oncology, 35(4), 775–788.
Pasic, I., Shlien, A., Durbin, A. D., Stavropoulos, D. J., Baskin, B., Ray, P. N., et al. (2010). Recurrent focal copy-number changes and loss of heterozygosity implicate two noncoding RNAs and one tumor suppressor gene at chromosome 3q13.31 in osteosarcoma. Cancer Research, 70(1), 160–171.
Kresse, S. H., Ohnstad, H. O., Paulsen, E. B., Bjerkehagen, B., Szuhai, K., Serra, M., et al. (2009). LSAMP, a novel candidate tumor suppressor gene in human osteosarcomas, identified by array comparative genomic hybridization. Genes, Chromosomes & Cancer, 48(8), 679–693.
Leaner, V. D., Chick, J. F., Donninger, H., Linniola, I., Mendoza, A., Khanna, C., et al. (2009). Inhibition of AP-1 transcriptional activity blocks the migration, invasion, and experimental metastasis of murine osteosarcoma. American Journal of Pathology, 174(1), 265–275.
Kimura, R., Ishikawa, C., Rokkaku, T., Janknecht, R., & Mori, N. (2011). Phosphorylated c-Jun and Fra-1 induce matrix metalloproteinase-1 and thereby regulate invasion activity of 143B osteosarcoma cells. Biochimica et Biophysica Acta, 1813(8), 1543–1553.
Kunita, A., Kashima, T. G., Ohazama, A., Grigoriadis, A. E., & Fukayama, M. (2011). Podoplanin is regulated by AP-1 and promotes platelet aggregation and cell migration in osteosarcoma. American Journal of Pathology, 179(2), 1041–1049.
Slamon, D. J., Clark, G. M., Wong, S. G., Levin, W. J., Ullrich, A., & McGuire, W. L. (1987). Human breast cancer: correlation of relapse and survival with amplification of the HER-2/neu oncogene. Science, 235(4785), 177–182.
Akatsuka, T., Wada, T., Kokai, Y., Kawaguchi, S., Isu, K., Yamashiro, K., et al. (2002). ErbB2 expression is correlated with increased survival of patients with osteosarcoma. Cancer, 94(5), 1397–1404.
Anninga, J. K., van de Vijver, M. J., Cleton-Jansen, A. M., Kristel, P. M., Taminiau, A. H., Nooij, M., et al. (2004). Overexpression of the HER-2 oncogene does not play a role in high-grade osteosarcomas. European Journal of Cancer, 40(7), 963–970.
Somers, G. R., Ho, M., Zielenska, M., Squire, J. A., & Thorner, P. S. (2005). HER2 amplification and overexpression is not present in pediatric osteosarcoma: a tissue microarray study. Pediatric and Developmental Pathology, 8(5), 525–532.
Baumhoer, D., Smida, J., Specht, K., Bink, K., Quintanilla-Martinez, L., Rosemann, M., et al. (2011). Aberrant expression of the human epidermal growth factor receptor 2 oncogene is not a common feature in osteosarcoma. Human Pathology, 42(6), 859–866.
Yoshida, C. A., Furuichi, T., Fujita, T., Fukuyama, R., Kanatani, N., Kobayashi, S., et al. (2002). Core-binding factor beta interacts with Runx2 and is required for skeletal development. Nature Genetics, 32(4), 633–638.
Galindo, M., Pratap, J., Young, D. W., Hovhannisyan, H., Im, H. J., Choi, J. Y., et al. (2005). The bone-specific expression of Runx2 oscillates during the cell cycle to support a G1-related antiproliferative function in osteoblasts. Journal of Biological Chemistry, 280(21), 20274–20285.
van Harn, T., Foijer, F., van Vugt, M., Banerjee, R., Yang, F., Oostra, A., et al. (2010). Loss of Rb proteins causes genomic instability in the absence of mitogenic signaling. Genes & Development, 24(13), 1377–1388.
Lengner, C. J., Steinman, H. A., Gagnon, J., Smith, T. W., Henderson, J. E., Kream, B. E., et al. (2006). Osteoblast differentiation and skeletal development are regulated by Mdm2-p53 signaling. Journal of Cell Biology, 172(6), 909–921.
Thomas, D. M., Johnson, S. A., Sims, N. A., Trivett, M. K., Slavin, J. L., Rubin, B. P., et al. (2004). Terminal osteoblast differentiation, mediated by runx2 and p27KIP1, is disrupted in osteosarcoma. Journal of Cell Biology, 167(5), 925–934.
Won, K. Y., Park, H. R., & Park, Y. K. (2009). Prognostic implication of immunohistochemical Runx2 expression in osteosarcoma. Tumori, 95(3), 311–316.
Sadikovic, B., Thorner, P., Chilton-Macneill, S., Martin, J. W., Cervigne, N. K., Squire, J., et al. (2010). Expression analysis of genes associated with human osteosarcoma tumors shows correlation of RUNX2 overexpression with poor response to chemotherapy. BMC Cancer, 10, 202.
Zhang, B., Pan, X., Cobb, G. P., & Anderson, T. A. (2007). microRNAs as oncogenes and tumor suppressors. Developmental Biology, 302(1), 1–12.
Shenouda, S. K., & Alahari, S. K. (2009). MicroRNA function in cancer: oncogene or a tumor suppressor? Cancer Metastasis Reviews, 28(3–4), 369–378.
Zhou, G., Shi, X., Zhang, J., Wu, S., & Zhao, J. (2013). MicroRNAs in osteosarcoma: from biological players to clinical contributors, a review. Journal of International Medical Research, 41(1), 1–12.
Miao, J., Wu, S., Peng, Z., Tania, M., & Zhang, C. (2013). MicroRNAs in osteosarcoma: diagnostic and therapeutic aspects. Tumour Biology, 34(4), 2093–2098.
Liu, L. H., Li, H., Li, J. P., Zhong, H., Zhang, H. C., Chen, J., et al. (2011). miR-125b suppresses the proliferation and migration of osteosarcoma cells through down-regulation of STAT3. Biochemical and Biophysical Research Communications, 416(1–2), 31–38.
Duan, Z., Choy, E., Harmon, D., Liu, X., Susa, M., Mankin, H., et al. (2011). MicroRNA-199a-3p is downregulated in human osteosarcoma and regulates cell proliferation and migration. Molecular Cancer Therapeutics, 10(8), 1337–1345.
Zhang, H., Cai, X., Wang, Y., Tang, H., Tong, D., & Ji, F. (2010). microRNA-143, down-regulated in osteosarcoma, promotes apoptosis and suppresses tumorigenicity by targeting Bcl-2. Oncology Reports, 24(5), 1363–1369.
Osaki, M., Takeshita, F., Sugimoto, Y., Kosaka, N., Yamamoto, Y., Yoshioka, Y., et al. (2011). MicroRNA-143 regulates human osteosarcoma metastasis by regulating matrix metalloprotease-13 expression. Molecular Therapy, 19(6), 1123–1130.
Tang, M., Lin, L., Cai, H., Tang, J., & Zhou, Z. (2013). MicroRNA-145 downregulation associates with advanced tumor progression and poor prognosis in patients suffering osteosarcoma. OncoTargets and Therapy, 6, 833–838.
Ziyan, W., Shuhua, Y., Xiufang, W., & Xiaoyun, L. (2011). MicroRNA-21 is involved in osteosarcoma cell invasion and migration. Medical Oncology, 28(4), 1469–1474.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Kim, S.S., Park, YK. Significance of MTA1 in the molecular characterization of osteosarcoma. Cancer Metastasis Rev 33, 981–991 (2014). https://doi.org/10.1007/s10555-014-9523-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10555-014-9523-3