Abstract
The purpose of the present study was to examine a new protocol involving the spontaneous correction of the misplaced tip of a peripherally inserted central catheter (PICC). Patients with PICCs misplaced in the jugular or contralateral subclavian veins were recruited. All patients underwent chest X-ray (CXR) after 3 days. In addition, those whose PICC tip still was misplaced and received another CXR after 4 days. The functions of the catheters, the subjective feelings of the patients, and local symptoms of the neck and upper anterior chest wall were recorded. Among 866 patients who had PICCs, we observed 22 PICC tips misplaced in the jugular, 3 tips misplaced in the contralateral subclavian vein, and 7 tips misplaced in other locations, which was confirmed by CXR. A total of 22 PICC tips automatically returned to the superior vena cava, which included all 3 tips in the contralateral subclavian vein and 19 tips in the jugular vein. All catheters functioned normally, and the patients had no complaints. In addition, we observed no local symptoms of the neck and upper anterior chest wall. For patients experiencing a PICC misplaced in the jugular and contralateral subclavian veins, there is no need to manually replace. In addition, the function of the catheter can remain normal.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The peripherally inserted central catheter (PICC) has been widely used to maintain reliable vascular access [1, 2]. Patients who undergo long-term cancer chemotherapy, total parenteral nutrition (TPN), antibiotic therapy, and dehydration treatment generally need PICC [3, 4]. From an anatomical perspective, PICCs do not cause serious complications, such as hemothorax and pneumothorax. However, there are strict requirements regarding the location of the PICC tip, which should be placed in the lower portion of the superior vena cava (SVC) after insertion. If the tip was misplaced, adjustments should be made to replace the tip [5,6,7]. In order to track the position of the PICC tip, several techniques have been recommended, which included: (1) inserting the PICC with the aid of image equipments so that the PICC tip position can be monitored simultaneously; (2) predicting the length of the PICC to ensure proper tip position before insertion [8]; (3) temporarily blocking the jugular vein during the procedure of PICC insertion [9]; (4) having the patients hold his or her breath in the procedure of PICC insertion [7]; (5) using a tracking system during the insertion procedure in order to track the position the PICC tip [4, 10]; and (6) adjusting the position of the PICC tip afterwards using a chest X-ray (CXR) [6]. The previous study has shown that, without adjusting the position of the PICC tip, the function of the PICC will be compromised [11].
Despite a variety of techniques and recommendations regarding the prevention and correction of misplaced PICC tips, many risk factors make it still very difficult for clinicians to ensure the correct position of PICC tips, which include: (1) venospasm [12]; (2) repeated catheterizations or catheter placement in seriously and chronically ill patients who require intermittent central venous access [12]; (3) acquired and congenital anatomical variations [13]; and et cetera. Therefore, PICC tip misplacement remains a persistent problem in the clinical practice, with a reported incidence rate of 7.87–35% [14,15,16]. The misplacement of PICC tip causes a variety of complications including phlebitis, infection, and thrombosis. The purpose of the present study was to examine a new protocol involving the spontaneous correction of the misplaced tip of a peripherally inserted central catheter (PICC).
Materials and methods
Participants
All studies have been performed in accordance with the Declaration of Helsinki and have been approved by the Xiangya Hospital Ethics Committee. Patients with malignancies in the Department of Radiotherapy at a comprehensive hospital in Changsha, Hunan, China were enrolled in the present study. All patients underwent a PICC between January 2013 and December 2015 using the new PICC care protocol. Inclusion criteria include (1) received the first non-surgical cancer treatment (e.g., chemotherapy, radiotherapy, dehydration therapy, immune regulation therapy, traditional Chinese medicine anti-tumor treatment, or comprehensive treatment) at the study site; (2) duration of the current hospitalization was no less than 60 days; (3) did not need an ADL or IADL assist during hospitalization. Exclusion criteria include (1) inability to perform CXR; (2) previous history of lower limb DVT; (3) patients who refused consent; and (4) patients who were not haemodynamically stable enough to have PICC performed.
Study protocol
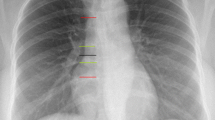
Under our new PICC care protocol, patients with a misplaced PICC in the jugular or contralateral subclavian vein were closely monitored for the consecutive 7 days without intervention. They were given a CXR after 3 days. Those patients whose PICC tips were still misplaced were given another CXR after 4 days (Fig. 1). If the PICC tip was misplaced in different locations, the PICC tips were immediately repositioned. These patients were given a CXR to confirm the position of the PICC tip [16].
Results
Among a total of 866 patients (average age 48 years; range 9–88 years) who underwent PICCs, 808 candidates were administered with a 4F single-lumen, silicone elastomer PICC with a distal-valve (Bard, Salt Lake City, UT), and 58 candidates were administered with a 4F single-lumen, polyurethane PICC with no valve (Medcomp, Harleysville, PA). A total of 32 cases (3.7%, two of them were Medcomp) had misplaced PICC tips, which comprised 22 in the jugular vein (Fig. 2a; including one medcomp), three in the contralateral subclavian vein (Fig. 2b), and seven in other positions: five in an axillary vein (including one medcomp), one in a chest wall vein, and one in a brachial vein as detected by CXR after insertion.
Among a total of 32 cases of misplaced PICC tips, 25 spontaneously returned to the SVC including 22 in the jugular vein and three in the contralateral subclavian vein. Among the 25 cases, a total of 19 spontaneously returned to the SVC three days after the insertion as confirmed by the CXR. In two of the remaining three cases, the PICC tip spontaneously returned to the SVC 7 days after insertion confirmed by the CXR (Fig. 3). For the remaining one case, the PICC tip position was unable to be tracked by the CXR. The function of the PICCs in all 25 patients was normal, and these patients not only reported no complaints, but also experienced no catheter-related complications during the period of observation.
Discussion
PICCs have been widely used in clinical practice for several decades and have been shown to be a safe and convenient means of administering chemical drugs and parenteral hyperalimentation [17, 18]. When the catheter does not reach the appropriate location within the vena cava, it is considered to be misplaced. This complication is very common in clinical practice. If the catheter is difficult to thread or to insert to the premeasured depth, blood withdrawal is difficult, the catheter flushes with resistance or removal of the stylet is difficult, this is an indication that malpositioning may have occurred [19]. An X-ray examination following PICC insertion is necessary to identify whether the catheter is misplaced.
The clinical skill and experience of the healthcare professional is important to ensure successful catheter placement. Furthermore, a knowledge of venous anatomy, which may aid in the selection of a suitable vein and a suitable catheter for insertion, is essential. It is also important for the catheter to be inserted slowly, to allow the blood returning to the heart to carry the catheter to the vena cava. Rapid threading of the catheter may increase the risk of malposition. In addition, the position of the patient may impact the PICC insertion, with misplacement potentially occurring if it is not possible to position the patient’s jaw close to the shoulder.
In the present study, a total of 32 PICC tip malposition cases of 866 patients (3.7%) were observed, which is much lower than previous reports (e.g., 7.87% [15], 11.4% [20], and 35% [16]). The possible reasons are the clinicians in the present study who performed the PICCs were highly experienced [21] and all patients in the present study had no communication barriers, therefore fully cooperated with the clinician during the procedures.
Wu et al. [22] and Prabaharan et al. [23] reported that PICC tips placed in the SVC would spontaneously move to the jugular vein. In addition, Rastogi et al. [24] reported that misplaced PICCs can reorient themselves within a day without any adjustment. It is reported that the misplaced catheters are usually taken out and replaced in many centers, which may increase the risk and impose great stress to critical ill patients, especially for infant cases [24]. The spontaneous correction of PICC tip may be suggested for avoiding the risk and stress of catheters replacement. Thus, leaving the misplaced catheters in place may be safer than replacement.
The results from the present study showed that, in 19 cases of malposition in the jugular vein and three cases of malposition in the contralateral subclavian vein, the PICC tips spontaneously repositioned themselves to the SVC 3 days after insertion. In addition, in two cases of malposition in the jugular vein, the PICC tips spontaneously repositioned themselves to the SVC 7 days after insertion. In these cases, the functions of the catheters remained normal, and none of the complications reported in other studies (e.g., Kundra et al. [25]) occurred.
The reasons underlying the PICC tip misplaced in the jugular or contralateral subclavian veins spontaneously reposition to SVC may be as follows. The jugular vein does not have valves. This blood flow vibrations from not only the walking of independent patients but also the movement of their limbs could facilitate the PICC tip within the contralateral subclavian vein to reposition itself to SVC.
In conclusion, for patients experiencing a PICC misplaced in the jugular and contralateral subclavian veins, there is no need for adjustment and repositioning. The PICC tips will spontaneously reposition themselves to SVC. In addition, the function of PICC remains normal during the whole process.
References
Johansson E, Hammarskjöld F, Lundberg D, Arnlind MH (2013) Advantages and disadvantages of peripherally inserted central venous catheters (PICC) compared to other central venous lines: a systematic review of the literature. Acta Oncol 52(5):886
Merrell SW, Peatross BG, Grossman MD, Sullivan JJ, Harker WG (1994) Peripherally inserted central venous catheters. Low-risk alternatives for ongoing venous access. West J Med 160(1):25
Kumar M, Amin M (2004) The peripherally inserted central venous catheter; friend or foe? Int J Oral Maxillofac Surg 33(2):201–204
Bidgood C (2016) Improving the patient experience with real-time PICC placement confirmation. Br J Nurs 25(10):539
Dale M, Higgins A, Carolanrees G (2016) Sherlock 3CG® tip confirmation system for placement of peripherally inserted central catheters: A NICE medical technology guidance. Appl Health Econ Health Policy 14(1):41–49
Jin JF, Zhao RY, Shentu YQ (2012) The effect of clinical practice in manual reduction on patients with malposition of PICC. Chin J Nurs 47:160–161
Yuan L, Lu QM, Wang CL, Xu RF (2014) Application of breathing coordination in reducing catheter tip malposition during PICC inserting. Chin J Nurs 49:498–502
Jeon EY, Koh SH, Lee IJ, Ha HI, Park BJ (2015) Useful equation for proper estimate of left side peripherally inserted central venous catheter length in relation to the height. J Vasc Access 16(1):42–46
Qian HU, Song M, Xue-Yu LI, Liu HY, Zheng ZD, Xie XD, Zhou LJ (2013) Comparison on the effect of three different methods on preventing PICC ectopic in jugular veins. Chin J Nurs 178(s 1–4):241–255
Lelkes V, Kumar A, Shukla PA, Contractor S, Rutan T (2013) Analysis of the Sherlock II tip location system for inserting peripherally inserted central venous catheters. Clin Imaging 37(5):917
Wei S, Wang A, Zhao S (2011) Discussion of PICC ectopic adjustment method. Chin J Nurs Train 26:1620–1622
Kay C, Alicia D, Renee OM (2016) Complications & interventions. In: Josie S (ed) Study guide for vascular access certification, 2nd edn. Association for Vascular Access, Herriman, pp 30–48
Lisa G, Lynn H, Mary H, Mary M, Marsha O, Darcy D (2016) Central vascular access device (CVAD) malposition. In: Alexander M (ed) Infusion therapy standards of practice, 1st edn. Infusion Nurses Society, Norwood, pp 79–87
Song L, Hui LI (2013) Malposition of peripherally inserted central catheter: experience from 3,012 patients with cancer. Exp Ther Med 6(4):891–893
Song LP, Li XS, Guo YY, Ye M, Ma YL, Guo M et al (2014) Malposition of peripherally inserted central catheter: experience from 3012 cancer patients. Int J Nurs Pract 20(4):446
Minkovich L, Djaiani G, Mccluskey SA, Mitsakakis N, Gilbert RW, Beattie WS (2011) Frequent malpositions of peripherally inserted central venous catheters in patients undergoing head and neck surgery. Can J Anaesth 58(8):709–713
Geng T, Yan Z, Li Q, Guo F, Xu H (2010) Efficacy of multifaceted interventions in reducing complications of peripherally inserted central catheter in adult oncology patients. Support Care Cancer 18(10):1293–1298
Cunningham RS, Ravikumar TS (1995) A review of peripherally inserted central venous catheters in oncology patients. Surg Oncol Clin N Am 4(3):429
Aladangady N, Roy R, Costeloe KL (2005) The cobweb sign: percutaneous silastic long line tip placement in tributaries of superficial veins. J Perinatol 25(10):671–673
Mitrović Z et al (2014) The use of peripherally inserted central catheter (PICC) in patients with hematological malignancies—a single center experience. Lijec Vjesn 136(6):136–140
Chen WF, Deng HY, Shen LF, Qin M, He LX (2014) A comprehensive intervention program on the long-term placement of peripherally inserted central venous catheters. J Cancer Res Ther 10:359–362
Wu PY, Yeh YC, Huang CH, Lau HP, Yeh HM (2005) Spontaneous migration of a port-a-cath catheter into ipsilateral jugular vein in two patients with severe cough. Ann Vasc Surg 19(5):734–736
Prabaharan B, Thomas S (2014) Spontaneous migration of central venous catheter tip following extubation. Saud J Anaesth 8(1):131
Sweeney R (1998) Spontaneous correction of the malpositioned percutaneous central venous line in infants. Pediatr Radiol 28(9):694
Kundra P, Chandran BVS, Subbarao KSVK. (2009) Unanticipated complication of a malpositioned central venous catheter. J Anesth 23(2):275–277
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest. Informed consent: Informed consent was obtained from all individual participants included in the study.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Mijung Park—co-corresponding author.
Rights and permissions
About this article
Cite this article
Chen, W., He, L., Yue, L. et al. Spontaneous correction of misplaced peripherally inserted central catheters. Int J Cardiovasc Imaging 34, 1005–1008 (2018). https://doi.org/10.1007/s10554-018-1321-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-018-1321-5