Abstract
Background
The position of the tip of a peripherally inserted central catheter (PICC) is crucial; malposition can lead to malfunction of the line or life-threatening events (e.g., arrhythmias, perforation).
Objective
To determine what factors other than arm position and accessed vein might influence the tip position of a PICC.
Materials and methods
Inclusion criteria were upper limb PICC placement, body weight <20 kg, intraoperative imaging with the arm in 0°, 45° and 90° abduction and an arm view marking the skin entry site relative to the shoulder. Evaluated variables included patient demographics, and PICC and insertion site characteristics. We measured central tip movement in rib units.
Results
We included 112 children who received a PICC (42 girls/70 boys, mean age 31±13 months, mean weight 6.5±4.9 kg). The overall range of central tip movement was -1 to +4 rib units (mean +0.8±0.7 rib units). Silicone PICCs moved significantly less than polyurethane PICCs (P<0.05). PICCs placed in the cephalic vein moved significantly less than those placed in other veins (P<0.05). Patient demographics and PICC characteristics (size, number of lumens, left or right arm accessed, length of the line) did not influence the range of central tip movement of a PICC (P>0.05).
Conclusion
Silicone PICCs and PICCs inserted into the cephalic vein move less than PICCs made of polyurethane and PICCs inserted into the brachial and basilic veins. These findings might assist operators in deciding which PICC to place in children in a given clinical context.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
An important consideration when placing a peripherally inserted central catheter (PICC), especially in infants and neonates, is the tip position. The optimal position for the tip of a PICC is close to the junction of the superior vena cava (SVC) and the right atrium (RA). In most children the SVC/RA junction is below the right main bronchus at the level of T6, two vertebrae below the carina [1–3]. However low PICC tip placement (i.e. deep within the right atrium) has been associated with cardiac arrhythmias and, in rare cases, cardiac perforation resulting in tamponade [4, 5]. On the other hand, if the tip of the PICC is too high (i.e. within the upper SVC), the catheter can flip into another vein (e.g., the contralateral brachiocephalic vein or ipsilateral jugular vein). In clinical practice, movement of the PICC is frequently encountered in small children and can result in the infusion of drugs into non-target vessels and potential erosion of the catheter into the pleura, soft tissues, lung parenchyma or bronchus [6, 7]. Hence great care is required when placing PICCs in young children to ensure optimal positioning of the tip.
Two previous studies have shown that the arm position and vein accessed in children influence the PICC tip position [8, 9]. For instance, elbow bending and adduction of the arm have been shown to move the PICC tip deeper into the chest when compared to straightening the arm or abducting it to 90°, especially when the PICC is placed below the elbow [9]. Another study, based on post-procedure radiographs, showed that PICCs placed in the cephalic vein moved away from the heart [8].
However no one has studied several other clinically relevant variables that might affect the movement of the PICC tip. These variables include the material from which the PICC is made, which ultimately influences the stiffness of the catheter (i.e. silicone vs. polyurethane); the size of the PICC (in French); the construction of the PICC (i.e. single or dual lumen); the internal length of the line (cm); distance from the PICC insertion point to the bending point (humeral head), and finally the biometric variables of the child. Our study therefore re-examines the effects of arm movement on the tip position, accounting for these other possible variables.
The hypothesis of this study was that arm positioning and vein accessed are not the sole factors influencing the tip position of a PICC. Understanding which variables affect PICC movement might influence operators in deciding location and type of PICC to place in a child in a given clinical context.
Materials and methods
We obtained institutional review board approval for this study. We reviewed and analyzed the clinical and imaging data from PICC insertion procedures performed over a 3-month period (Feb. 1–April 30, 2015) at a tertiary referral pediatric interventional radiology center. Inclusion criteria included (1) body weight under 20 kg, (2) upper limb access site and (3) availability of stored fluoroscopic images of PICC tip position in different arm positions. The prospectively acquired, fluoroscopically saved images include the PICC tip with the arm in abduction 90o, 45o and 0o, and of the arm showing PICC insertion site and shoulder. We included the following patient demographics: age, gender and body weight at the time of PICC insertion.
Peripherally inserted central catheter placement
All PICCs were placed using US and fluoroscopic guidance in the Interventional Radiology department by an interventional radiologist or interventional nurse (n=10, 5 staff members, 4 fellows, 1 nurse practitioner). The type of PICC chosen was based on the clinical indication and size of the child, after discussion with the referring team. The PICCs employed in this study were 1.9 Fr, 2.6 Fr, 3 Fr, or 4 Fr and were made of silicone or polyurethane. Practice preference in this young cohort (<20 kg) was to place cuffed lines, so all were cuffed except the 1.9-Fr PICCs. Single- or double-lumen PICCs were placed. Veins were chosen with first preference being the basilic, above the elbow (as distant from the brachial artery and median nerve as possible, with a straight superficial anatomical course); however if access to this vein proved difficult, the brachial or cephalic vein was chosen (acknowledging their proximity to the brachial artery and acute angle of entry of the cephalic vein into the axillary vein). The right side was usually attempted first.
Insertion technique
We obtained informed consent from the parent/guardian. All PICC insertions were performed under strict sterile conditions in the interventional radiology suite, with the child supine, arm abducted 90o, and elbow straight. US-guided access into an upper arm vein was achieved and the distance from the entrance site to the superior cavoatrial junction was measured based on the access wire [8]. The measured PICC was inserted over the guidewire through a peel-away sheath. The cuff of the PICC was subcutaneously implanted. Before final securement, the central tip of the PICC was assessed after a small volume of contrast medium was injected into the arm while it was held in the three different positions. If PICC adjustment was required (i.e. if the length was too long or too short), this was performed using an over-the-wire technique. At the end of the procedure, a fluoroscopic image of the arm (with a radiopaque marker demonstrating the skin entrance site) during contrast medium injection was saved to exclude any leakage at the cuff, which would suggest catheter damage during cuff implantation. When a satisfactory position was confirmed, the entry site was closed with a single suture.
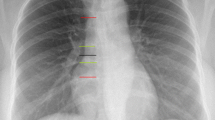
Calculation of PICC tip movement
Ribs were numbered from 1 to 12 and each tip position was given a number according to the level of the rib over which it was projected, similar to previously reported methods but without bending of the elbow [9]. The images were recorded as follows: Image 1, arm abducted 90°, position 1; Image 2: arm abducted 45°, position 2; Image 3: arm at side 0o, position 3; and Image 4: upper arm (abducted 90°) showing humeral head physis and a radiopaque marker at the skin entry site (to measure length of line to shoulder). One radiologist (R.G., with 6 years of experience) assessed all four post-procedural images. The movement of each PICC was calculated and documented in “rib units” (one rib unit describes the distance between the top of a rib to the top to the adjacent rib) with descent deeper into the chest given a positive value, and ascent cephalad into the SVC given a negative value. The maximum range of motion was calculated by the difference in tip location between position 1 and position 3. In addition, the distance from the PICC insertion site in the arm to the growth plate of the humeral head was estimated in centimeters, using the diameter of the PICC for distance calibration (the hypothesis being that the longer the straight component in the arm, the more anchored the PICC would be, i.e. less likely to move).
Statistical analysis
We used descriptive statistics to describe the sample. We used the Wilcoxon non-parametric test to compare the PICC movements between the left and right sides, single and double lumens, catheter material, and the effect of previously placed PICCs. We used non-parametric analysis of variance to compare the movement of the PICC tip in the three upper limb veins (basilic, brachial and cephalic) and the different sizes of the catheters. Spearman correlation was used to assess the correlation between continuous variables and PICC tip movement. We employed multivariate regression analysis using weight, vein and material as covariates, and PICC movement as outcome, on the full cohort. A further subset analysis was also performed (3-Fr single-lumen PICC, silicone and polyurethane) after adjusting for vein accessed and patient weight. We performed a chi-squared test to assess for power to detect differences in French size. The statistical package SAS 9.4 (SAS Institute, Cary, NC) was used for data analysis.
Results
Of the 174 PICCs placed during the 3-month study period, 112 met the inclusion criteria. The gender distribution was 42 girls and 70 boys. The mean weight and age of the patients was 6.5±4.9 kg and 31±13 months, respectively. Eighteen children had at least one previous PICC inserted in the same arm (range 0–2). Of the PICCs placed, 32 were silicone and 80 polyurethane; sizes were 1.9 Fr (n=2), 2.6 Fr (n=8), 3 Fr (n=83) and 4 Fr (n=19); 25 PICCs were single lumen and 87 were double lumen (Table 1).
Maximum range of motion (i.e. from arm positions 1 to 3) in all 112 PICCs was mean 0.8 rib units, min -1, max +4. Adduction from positions 1 to 3 resulted in the PICC tip descending deeper into the thorax in 89/112 patients, irrespective of material, size and number of lumens. In 3/112 children (one cephalic and two brachial access; one silicone and two polyurethane PICCs) the PICC moved to a higher position when the arm was adducting, and in 20/112 children the PICC did not change position. There was a statistically significant difference in mean tip position among the three arm positions (position 1 mean at rib 5.3±0.73; position 2 mean at rib 5.8±0.79; and position 3 mean at rib 6.2±0.86) (P<0.05).
We conducted univariate analysis of all variables. Only PICC material and vein accessed significantly affected tip movement. Comparing silicone to polyurethane PICCs, the mean range of tip movement when the arm was moved from positions 1 to 2 was 0.3 rib units (silicone) and 0.5 rib units (polyurethane). From positions 2 to 3 the mean range of motion was 0.1 rib units (silicone) and 0.5 rib units (polyurethane); and from positions 1 to 3 the mean range was 0.4 and 1.0 rib units, respectively (P<0.05) (Fig. 1). The mean range of motion of the tip from arm positions 1 to 3 was 1.0 rib unit in uncuffed and 0.8 (±0.7) in cuffed PICCs. With respect to vein accessed, the mean range of movement for PICCs when the arm moved from positions 1 to 2 was 0.1 rib units for cephalic vein PICCs, 0.4 rib units for basilic vein PICCs and 0.5 rib units for brachial vein PICCs. The mean range of movement when the arm was moved from positions 2 to 3 was 0.3 rib units for cephalic vein PICCs, 0.4 for basilic vein PICCs and 0.3 for brachial vein PICCs. The mean range of movement when the arm was moved from positions 1 to 3 was 0.4 rib units for cephalic vein PICCs, 0.8 for basilic vein PICCs and 0.9 for brachial vein PICCs (P<0.05) (Fig. 2). These results show that silicone and cephalic vein PICCs moved least; however only three PICCs were both silicone and inserted into the cephalic vein in this patient cohort, and the mean range of motion among these three PICCs was (positions 1 to 3) 0.3 rib units, with one line moving away from the heart.
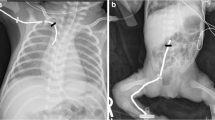
Differences in tip movement when comparing polyurethane (a, b) and silicone (c, d) PICCs. a Fluoroscopic image in a 4-year-old boy with a basilic vein polyurethane PICC (3 Fr, single lumen). Image with arm abducted 90o (position 1) shows PICC tip at rib V (arrow). b Fluoroscopic image in same boy with his arm abducted 0o (position 3) shows PICC tip moved two rib spaces to rib VII (arrow). c Fluoroscopic image in a 6-day-old boy with basilic vein silicone PICC (3 Fr, single lumen). Image with arm abducted 90o (position 1) shows PICC tip at the lower border of rib V (arrow). d Fluoroscopic image in the same boy with his arm abducted 0o (position 3) shows the tip remaining at the lower border of rib V (arrow), i.e. it did not move. PICC peripherally inserted central catheter
PICC inserted in the cephalic vein. a Typical anatomical course of the cephalic vein (arrow) in a 3-month-old girl with a 90° angle entering the subclavian vein. b, c After inserting the PICC (polyurethane, 3 Fr, single lumen) and moving the arm from (b) position 1 (tip at the level of rib VI, arrow) to (c) position 3 (tip at the level between ribs VI and VII, arrow), the central tip moves only 0.5 rib units. PICC peripherally inserted central catheter
The clinical variables (gender, age, weight) did not significantly affect tip movement. Other characteristics of the PICC such as its size, insertion side, number of lumens, length of PICC and length to growth plate did not significantly affect the central tip movement on arm adduction. Although no difference was found in tip movement comparing cuffed or uncuffed lines, our study only included two uncuffed lines.
To exclude any possible selection bias we conducted a multivariate regression analysis. A subset analysis of all 3-Fr single-lumen PICCs was also performed (52 polyurethane and 31 silicone). After adjusting for vein accessed and the weight of the child, multivariate regression analysis showed that with arm movement 3-Fr silicone PICCs moved a mean of 0.61 rib spaces less than 3-Fr polyurethane PICCs (P<0.0001) (Fig. 3). Similarly, the subset multivariate regression analysis showed a significant difference in movement among accessed veins (PICCs inserted in the basilic vein moved 0.95 rib units more and PICCs inserted in the brachial vein moved 1.0 rib units more than PICCs inserted into the cephalic vein (P<0.0001).
Comparison of materials in a single child, a 4-year-old boy. Initially a 3-Fr single-lumen polyurethane line (a, b) was inserted through the basilic vein. Because the tip moved too far into the right atrium when adducting the arm, we exchanged the line with a 3-Fr single-lumen silicone line (c, d) during the same procedure. a Polyurethane line. Fluoroscopic image with arm abducted 90o (position 1) shows the tip between ribs V and VI (arrow). b Polyurethane line. Fluoroscopic image with arm abducted 0o (position 3) shows tip moved 1.5 rib spaces to rib VII (arrow). c Silicone line. Fluoroscopic image in the same boy after exchanging the PICC to a silicone line, with arm abducted 90o (position 1), shows tip at the lower border of rib VI (arrow). d Silicone line. Fluoroscopic image with arm abducted 0o (position 3) shows tip moved 1 rib unit less than that of the polyurethane line, between ribs VI and VII (arrow). PICC peripherally inserted central catheter
Discussion
This study reaffirms that PICCs move with arm position, and importantly shows that tip movement is affected by the characteristics of the catheter material and the vein accessed. Interestingly it shows that patient characteristics (i.e. age, weight, gender, prior PICCs) and PICC characteristics (length, distance from insertion site to humeral head, French size, number of lumens) do not affect tip movement. This suggests that when minimizing movement is important (e.g., in infants or neonates, in patients with underlying structural or electrophysiological cardiac disease, in cases of cavo-pulmonary anastomosis or left SVC), choice of a silicone PICC or a cephalic access may be preferred to prevent the tip of the PICC from moving too deep into the right atrium, pulmonary artery or coronary sinus with arm movement. However the combination of silicone PICC and cephalic access (n=3) did not reduce range of motion any further.
In general, PICCs are made from two materials, silicone and polyurethane. While silicone has been used since the 1960s and is preferred for children who require an ethanol lock [10], polyurethane is a newer product and has been used in various formulations in clinical practice since the 1990s. In ex vivo experiments polyurethane has been shown to be stiffer when compared to silicone, giving it the advantage of ease of insertion over a guidewire without bunching up [11]. Furthermore, polyurethane has a thinner wall construction and hence has a lower profile when compared to a silicone PICC of the same inner luminal size. Polyurethane is also a stronger material and is therefore less likely to break or fracture [12]. In contrast, silicone PICCs are softer and more likely to absorb any applied translational vectors, making movements of the catheter tip less likely during arm abduction as demonstrated in the present study.
The different veins (i.e. basilic, brachial and cephalic) are relevant to PICC tip movement. Nadroo and colleagues [8] in a retrospective review of chest radiographs showed that PICCs inserted in the cephalic vein tend to move upward in the SVC on adduction. However, in that study the PICCs were placed with their tips positioned higher in the SVC (second posterior intercostal space, confluence of the right brachiocephalic vein and the SVC), enabling the tip to easily move up into the subclavian vein. Connolly et al. [9], in a prospective study of PICC tip movement at the time of insertion, showed that arm movement affects the tip position but these authors could not find any significant difference regarding vein accessed. However in that study “a variety of PICCs were inserted” of unspecified material [9]. The results of our study differ from both of these earlier reports by showing that the tip of a PICC moves significantly less when the catheter is inserted in the cephalic vein compared to the basilic or brachial. One hypothesis is that as each upper limb vein takes a different anatomical course, the PICC is subjected to different translational vectors when the arm is moved. The cumulative sum of all the vectors during arm movement then determines the amount of movement translated to the tip of the PICC. Hence as the cephalic vein travels higher in the upper arm and enters the axillary vein at a steep angle, this may disperse some of the translational vectors applied to it, resulting in less forward movement being transferred to the tip [13]. Only three PICCs in our cohort moved cephalad in the SVC, and no variable was predictive of this direction of movement.
In clinical practice, the choice of a PICC depends on several clinical factors (patient needs, vein size, number of lumens required) and is a balance of risk to benefit, with available evidence unclear and even conflicting at times. PICCs come in a variety of sizes (i.e. 1.9 Fr, 2.6 Fr, 3 Fr and 4 Fr) and with a different number of lumens (i.e. single and double). The choice of size of the PICC inserted must be balanced against the size of the vein because total occupancy of the cross-sectional area by the catheter impedes flow, predisposing the vein to thrombosis. The catheter size needs to be chosen to prevent total occupancy of the vein, to facilitate insertion, and to reduce damage to the vein. The cephalic vein is a smaller vein in diameter and has lower flow compared to the basilic or brachial veins. However a direct relation between ratio of catheter size and vein size, and thrombosis and vein cannulated has not been proved. In fact Dubois et al. [14] showed less thrombosis in cephalic vein PICCs. The risk-to-benefit balance is more complex in children with impaired renal function. The future need for arteriovenous fistulae for renal dialysis would suggest lower-limb PICCs be favored over upper-limb PICCs, and especially that the cephalic vein be avoided. Counter to this is the need to preserve the iliac veins for future renal transplantation. To minimize risks, our practice is to place any subsequent PICCs on the ipsilateral arm side and preserve the venous system of the contralateral upper limb. Depending on the planned administration of medication, a single- or double-lumen PICC is chosen (e.g., incompatible medications require a double lumen to avoid chemical precipitation [15]). On the one hand, no significant difference was demonstrated in tip movement with overall catheter size, length of the line or the number of lumens in this study. On the other hand, it has been previously shown that the material, number of lumens and catheter diameter contribute to the perforating potential of a central venous line [16]. Furthermore univariate and multivariate analyses showed that patient biometric data (age, gender, weight) and the insertion site distance from the growth plate of the humeral head did not affect the relative tip movement of a PICC.
We measured PICC tip movement in rib units. This provides a meaningful relevant assessment as compared to absolute numbers (in mm or cm) because it accounts for patient size and is independent of magnification. Furthermore, in practice the central tip position is judged on a radiograph from its relation to the anatomical landmarks of ribs and bronchus. In the pediatric population an arbitrary movement of 1 cm is clinically more significant in younger children compared to older children. Arm position is important when interpreting central PICC tip position on any subsequent radiographs [8, 9, 17]. Hence radiographic findings need to be clinically correlated and optimized to the child’s usual nursing or sleeping position and the underlying disease.
There are several limitations to this study. All the images were obtained with the child in a supine position, and inspiration/expiration was not accounted for. Because of the retrospective nature of the study, some children were excluded because the full set of images was not available. In addition, measurements were obtained immediately after the PICC insertion, and PICC material might not have fully warmed to body temperature. It is known that polyurethane softens under body temperature after insertion [11]. In addition, there were unequal numbers of certain types of lines used in this study cohort, but statistical assessment confirmed sufficient power for analysis. The study population was limited to children with a body weight of less than 20 kg because the impact of PICC motion is clinically more relevant in smaller children, but this could be considered a limitation. Despite this, the use of rib units as the unit of measure would minimize any such limitation because the actual size of the rib unit increases with patient weight and age. Although most lines in this cohort were cuffed, which might have some impact on movement, these results remain meaningful for other programs because all PICCs are secured by using a combination of one or more methods: suture, securement devices, dressings or cuff.
Conclusion
Our findings show that silicone PICCs and PICCs inserted into the cephalic vein move less than PICCs inserted into the brachial and basilic veins and PICCs made of polyurethane. Although cephalic access can be more challenging for the interventional radiologist, this vein should be considered in children where the central tip placement is crucial and position of the tip should remain stable regardless of the child's arm movement. Other clinical and material factors were not significant variables. These findings might influence interventional radiologists when they are choosing the type of PICC and which vein to access.
References
Connolly B, Mawson JB, MacDonald CE et al (2000) Fluoroscopic landmark for SVC-RA junction for central venous catheter placement in children. Pediatr Radiol 30:692–695
NAoVA Networks (1998) NAVAN position statement. J Vasc Access Devices 3:8–10
Baskin KM, Jimenez RM, Cahill AM et al (2008) Cavoatrial junction and central venous anatomy: implications for central venous access tip position. J Vasc Interv Radiol 19:359–365
Darling JC, Newell SJ, Mohamdee O et al (2001) Central venous catheter tip in the right atrium: a risk factor for neonatal cardiac tamponade. J Perinatol 21:461–464
Murray BH, Cohle SD, Davison P (1996) Pericardial tamponade and death from Hickman catheter perforation. Am Surg 62:994–997
Puel V, Caudry M, Le Métayer P et al (1993) Superior vena cava thrombosis related to catheter malposition in cancer chemotherapy given through implanted ports. Cancer 72:2248–2252
Racadio JM, Doellman DA, Johnson ND et al (2001) Pediatric peripherally inserted central catheters: complication rates related to catheter tip location. Pediatrics 107:E28
Nadroo AM, Glass RB, Lin J et al (2002) Changes in upper extremity position cause migration of peripherally inserted central catheters in neonates. Pediatrics 110:131–136
Connolly B, Amaral J, Walsh S et al (2006) Influence of arm movement on central tip location of peripherally inserted central catheters (PICCs). Pediatr Radiol 36:845–850
Crnich CJ, Halfmann JA, Crone WC et al (2005) The effects of prolonged ethanol exposure on the mechanical properties of polyurethane and silicone catheters used for intravascular access. Infect Control Hosp Epidemiol 26:708–714
Walder T (2013) Thermoplastic polyurethanes as medical grade thermoplastic elastomer. 1–7. http://files.eventsential.org/61198b3c-1544-484a-a2b1-01ec6810ec04/event-58/29265646-Walder%20Paper%20Material%20101513[1]-thermoplastic.pdf. Accessed 5 May 2016
Moran BJ, Sutton GL, Karran SJ (1992) Clinical evaluation of percutaneous insertion and long-term usage of a new cuffed polyurethane catheter for central venous access. Ann R Coll Surg Engl 74:426–429
Young MD, Streicher MC, Beck RJ et al (2012) Simulation of lower limb axial arterial length change during locomotion. J Biomech 45:1485–1490
Dubois J, Rypens F, Garel L et al (2007) Incidence of deep vein thrombosis related to peripherally inserted central catheters in children and adolescents. CMAJ 177:1185–1190
Collins JL, Lutz RJ (1991) In vitro study of simultaneous infusion of incompatible drugs in multilumen catheters. Heart Lung 20:271–277
Gravenstein N, Blackshear RH (1991) In vitro evaluation of relative perforating potential of central venous catheters: comparison of materials, selected models, number of lumens, and angles of incidence to simulated membrane. J Clin Monit 7:1–6
Forauer AR, Alonzo M (2000) Change in peripherally inserted central catheter tip position with abduction and adduction of the upper extremity. J Vasc Interv Radiol 11:1315–1318
Acknowledgments
Author Ralph Gnannt was supported by EMDO (Emily Dorothy Lageman) Foundation and Helmut-Hartweg Funds. We thank the Image-Guided Therapy team at the Hospital for Sick Children for assisting with recording and labeling of all the images used for our data analysis.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None
Rights and permissions
About this article
Cite this article
Gnannt, R., Connolly, B.L., Parra, D.A. et al. Variables decreasing tip movement of peripherally inserted central catheters in pediatric patients. Pediatr Radiol 46, 1532–1538 (2016). https://doi.org/10.1007/s00247-016-3648-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-016-3648-1