Abstract
Purpose
The data of head-to-head comparisons of the anti-fracture efficacy of bone modifying agents (BMAs) in patients with hormone receptor-positive breast cancer receiving aromatase inhibitor (AI) are not available. Therefore, we conducted a network meta-analysis to compare the efficacy of different BMAs in patients with breast cancer receiving adjuvant AI.
Methods
We performed a network meta-analysis to compare the change of bone mineral densities (BMDs) and the risk of fracture in the selected studies using a random effect model. The primary outcomes are the change of BMD of lumbar spine (LS) and total hip (TH) from the baseline (ΔBMD, %) at 1 and 2 years and the risk of fracture.
Results
We identified and included a total of 16 randomized controlled trials for this analysis. All BMAs included (risedronate, zoledronate, and denosumab) were associated with a significant increase in BMD of LS and TH at 1 and 2 years compared with no upfront treatment group. Among BMAs, zoledronate and denosumab use resulted in significantly higher BMD of LS and TH at 1 and 2 years compared with risedronate. The risk of fracture was significantly lower in the patients who received denosumab or risedronate compared with the patients without upfront treatment (Relative risk (RR) [95% CI] 0.51 [0.38–0.67] and 0.54 [0.35–0.83], respectively).
Conclusion
Among the bisphosphonates, zoledronate increased BMD the most, but risedronate, not zoledronate, use was associated with lower risk of fracture. Denosumab increased BMD not only of LS but also of the cortical-bone-rich hip, and showed a significant reduction of fracture risk.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer is one of the most common cancer in women worldwide [1]. In the US, 279,100 people are estimated to be diagnosed with breast cancer, and 42,170 patients die of breast cancer in 2020 [2]. About 80% of all breast cancer is hormone receptor-positive [2], and adjuvant endocrine therapy including aromatase inhibitor (AI) is recommended to prevent recurring or developing new breast cancer in postmenopausal women with hormone-sensitive breast cancer without metastasis [3].
One of the major side effects of AI is a rapid bone loss by depleting residual estrogen in postmenopausal patients [4]. While postmenopausal women, generally speaking, lose bone mineral density (BMD) by about 1% per year [5], patients with AI use lose up to ~ 5% of BMD per year [6]. As expected, the risk of fracture almost doubles in those patients [7, 8]. Therefore, the current guidelines support using bone modifying agents (BMAs) such as bisphosphonates or denosumab to prevent the fracture [4].
However, head-to-head comparison of those medications in terms of the anti-fracture efficacy has not been conducted. Our aim of this study is to compare skeletal effect of each BMA based on BMD change and the incidence of fracture by a network meta-analysis.
Methods
All the studies investigating the skeletal impact of BMAs on the BMD changes or the risk of fracture in patients on AI were identified using a two-level search strategy. First, databases including PubMed, Cochrane library, and EMBASE were searched through August 11, 2019, using web-based search engines, as shown in Fig. 1. Second, relevant studies were identified through a manual search of secondary sources, including references of initially identified articles, reviews, and commentaries. All references were downloaded for consolidation, elimination of duplicates, and further analyses. Search terms included breast cancer or breast carcinoma or breast neoplasms; aromatase inhibitors or anastrozole or letrozole or exemestane; bisphosphonate or alendronate or risedronate or zoledronate or denosumab or diphosphonates; randomized. Two independent and blinded authors (HM and SS) reviewed the search results separately to select the studies based on inclusion and exclusion criteria. If there was lack of a consensus, a third author (TK) was consulted for final decision [9]. There was no language restriction. The references included in the studies were reviewed to minimize missing relevant studies. The study was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines [10].
The included studies met the following criteria: the study was peer-reviewed by journals, the design was a randomized controlled trial of patients with different preventive strategies for bone loss and fracture (risedronate, zoledronate, denosumab), or no upfront treatment, the study had an end-result of at least one of the followings: BMD change from the baseline (ΔBMD,%) of lumbar spine (LS) or total hip (TH) at 1 year or 2 years, or the risk of fracture. We used the Cochrane risk of bias assessment to explore sources of bias [11]. According to this scale, we evaluated the risk of bias based on random sequence generation, allocation concealment, blinding of participants and researchers, blinding of outcome assessment, selective reporting and incomplete outcome data, and we categorized them as high, low or unclear. To assess the risk of publication bias, a visual estimation of the funnel plot was used. For each study, data regarding BMD and the incidence of fracture in each cohort were abstracted. We used mean difference of BMD adjusted with baseline factors (e.g., age, baseline T-score, or chemotherapy use) if they were reported. If the number of patients in each cohort were reported, we calculated the unadjusted difference of BMD. We performed network meta-analysis using “netmeta” 1.1–0 package (R Foundation for Statistical Computing, Vienna, Austria). We used the random effect model for the analysis. Within the framework, I2 statistics, which represent the proportion of total variation in study estimates due to heterogeneity, were used to quantify heterogeneity [12]. The I2 statistics represent the proportion of variability that is not attributable to chance. Lastly, we conducted sensitivity analyses by excluding a study with the largest number of patients and a study with the most heterogeneity.
Results
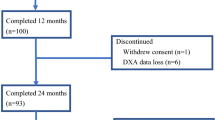
We identified 16 eligible studies [13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28], enrolling a total of 7699 patients receiving AI after surgical treatment for breast cancer [The number of patients: Risedronate (n = 312), Zoledronate (n = 1708), Denosumab (n = 1838), No upfront treatment (n = 3841)]. All 16 studies were randomized controlled trials comparing one of the medications with no upfront treatment. The analyzed studies are summarized in Table 1. The median age of the studies was similar. Of note, the studies of risedronate include exclusively patients with baseline T-score below − 1.0, while the studies of the other BMAs included all patients regardless of baseline BMD. Thirty-three percent of patients in the studies of zoledronic acid and 49% of patients in the studies of denosumab had baseline T-score less than − 1.0.
The characteristics of the network are shown in Fig. 2. Briefly, ten, eight, ten comparisons were included in the analysis for ΔBMD at 1 year, ΔBMD at 2 years and the incidence of fracture, respectively. The main outcomes are summarized in Table 1. The forest plots show the results of the meta-analysis of ΔBMD of LS at 1 year (Fig. 3). There was a significant heterogeneity in the analysis (I2 = 63.5%, p = 0.008). All treatment groups increased BMD significantly compared with no upfront treatment group at 1 year. At 2-year follow-up, BMDs at LS and TH further increased with all BMAs. Zoledronate and denosumab similarly increased BMD at LS (5.45% and 5.64% at 1 year, and 7.26% and 7.97% at 2 years, respectively), and at TH (3.34% and 4.65% at 1 year, and 3.75% and 5.31% at 2 years, respectively) (Supplementary Table 1, Supplementary Fig. 1A–C). The BMD gains by those two drugs were comparable except that denosumab gained significantly higher BMDs at TH at 2 years compared with zoledronate (0.66% [0.11– 1.21%]) (Supplementary Fig. 1C). In comparison with risedronate, zoledronate and denosumab showed significantly higher BMD increment at LS at 1 year (3.10% [2.23–3.98%] and 3.29% [2.29–4.29%], respectively), as shown in Fig. 3.
We performed a sensitivity analysis excluding a study with the most heterogeneity [17]. The analysis of ΔBMD of LS and TH showed consistent findings with the original analysis (Supplementary Fig. 2). The sensitivity analysis excluding a study with the largest number of patients [13] also showed similar results of BMD changes (Supplementary Fig. 3). However, the superior total hip BMD gain with denosumab at 2 years was not observed in the sensitivity analyses (Supplementary Figs. 2 and 3).
A network meta-analysis of the risk of fracture was also performed, as shown in Fig. 4. There was no significant heterogeneity (I2 = 0%, p = 0.784). Among all BMAs, denosumab and risedronate reduced the incidence of fracture significantly compared with no upfront treatment group (RR 0.51 [0.38–0.67] and RR 0.54 [0.35–0.83], respectively). In particular, denosumab was associated with a lower incidence of fracture compared with all the bisphosphonates including zoledronate (RR 0.60 [0.38–0.94]). Interestingly, zoledronate did not show significant anti-fracture efficacy, although it increased BMDs more than any other bisphosphonates.
We performed a subgroup analysis in the patients with a low baseline T-score (T-score < − 1.0). There was no heterogeneity in the studies (I2 = 0%, p = 0.525). Again, risedronate and denosumab use showed a significantly lower risk of fracture compared with no upfront treatment group (RR [95% CI] 0.54 [0.35–0.83] and 0.58 [0.42–0.81], respectively) (Supplementary Fig. 4).
Most studies in this analysis had a low risk of selective reporting, incomplete outcome data, and other risks. However, about half of the RCTs were open-label, which precludes the blinding of participants and researchers. Some RCTs did not specify the randomization protocol, which can lead to a bias in random sequence generation and allocation concealment (Fig. 5). Figure 6 shows the funnel plots for the outcomes that were assessed in this analysis. There was an obvious heterogeneity among the studies using zoledronate with BMD change (LS) as an end-result. Additionally, in the assessment of fracture risk, the studies on risedronate showed asymmetric distribution; the studies with large standard errors were associated with greater efficacy, suggesting the presence of publication bias.
Discussion
Our study is the first to analyze the skeletal effect of the different bisphosphonates and denosumab in postmenopausal patients receiving aromatase inhibitor as an adjuvant therapy for breast cancer The salient findings of our study are the following: (1) Our study showed that BMAs significantly increased the BMD of LS and TH at 1 and 2 years. (2) Zoledronate and denosumab were associated with significantly higher BMD gain among all the treatments. (3) Denosumab increased BMDs at cortical-bone-rich skeleton such as hip more than bisphosphonates. (4) Denosumab and risedronate demonstrated a significant fracture risk reduction. (5) Although zoledronate seemed as potent as denosumab in terms of increasing BMDs, the anti-fracture efficacy of zoledronate was unclear.
A previous meta-analysis showed that bisphosphonates (ibandronate, alendronate, risedronate and zoledronate) were associated with an increase in BMD in postmenopausal women receiving adjuvant AI for breast cancer [29]. However, they did not compare the skeletal effect of each medication. Among the bisphosphonates, our analysis found that zoledronate use was associated with significantly more BMD gain than the others. In patients with Crohn disease, zoledronate showed better efficacy as well [30]. However, a meta-analysis of patients with primary osteoporosis did not find a significant superiority of zoledronate in terms of BMD gain compared with the other bisphosphonates [31]. The distinct characteristics of the study subjects may explain this difference. The patients on aromatase inhibitors, like patients with Crohn disease, lose bone at a much higher rate than postmenopausal osteoporosis [6]. The efficacy of zoledronate, which is the most potent bisphosphonate, might appear more prominent in the setting of rapid bone decline.
In terms of fracture risk reduction, no previous study has shown a direct anti-fracture efficacy of bisphosphonates in this specific patient group. Although a large meta-analysis by Early Breast Cancer Trialists' Collaborative Group revealed that adjuvant bisphosphonates reduce fracture risk (RR 0·85 [0·75–0·97]) in patients with early breast cancer, the study group included both patients with and without receiving aromatase inhibitors, and the authors did not compare the anti-fracture efficacy of each bisphosphonate [32]. Another meta-analysis by O’Carrigan et al. analyzed 44 randomized controlled trials and found that bisphosphonates did not lower the risk of fracture regardless of the kind of bisphosphonates, the timing of bisphosphonate use (immediate vs. delayed) or patients’ AI use [33].
In our analysis, we found that risedronate significantly decreased the risk of fracture in breast cancer patients receiving AIs compared with no upfront treatment group. When we analyzed patients with low BMD (T-score < − 1.0), risedronate still demonstrated a significant fracture risk reduction. However, the most potent zoledronate with a superior BMD gain over risedronate, did not show expected anti-fracture efficacy. This might be a reflection of the trials of zoledronate in our analysis, which included patients with all BMDs, whereas the trials of risedronate exclusively studied patients with low BMDs (T-score < − 1.0). Only 33% of patients receiving zoledronate had T-score < − 1.0 at the baseline. Therefore, the low incidence of fracture in studies of zoledronate might lead to an insufficient power to detect anti-fracture efficacy.
Denosumab is a relatively new anti-resorptive agent, and so far, there have been two meta-analyses, which examined the effect of denosumab in patients with osteoporosis [34] and postmenopausal women with a high risk of fracture [35]. Both studies showed that denosumab increased BMD significantly more than the other BMAs. In our study, we also observed consistent findings in this specific group of patients. Of note, a recent meta-analysis compared the effect of denosumab and zoledronate in the same patient group as ours, using both fixed and random effect models. In this analysis, different models resulted in inconsistent findings where a fixed effect model showed a significantly better fracture risk reduction at 36 months with denosumab, but a random effect model did not show any difference in two treatment groups [36]. With a larger number of studies in our analysis, we noted that denosumab use was associated with a significant lower risk of fracture in a random effect model as well.
In terms of potential side effects of long-term use of anti-resorptives, atypical femur fracture (AFF) is particularly concerning as anti-resorptives tend to accumulate in active resorptive areas like skeletal metastasis. The study from MD Anderson reported a very low incidence of AFF (0.05 cases per 100,000 person-year) with bisphosphonate use [37]. In terms of denosumab, a retrospective study reported a higher incidence of AFF (5 cases in 277 patients with a median of 10 doses), but the study was very small and 4 out of 5 cases had been exposed to bisphosphonate prior [38].
To our knowledge, this is the first network meta-analysis comparing different treatments for bone loss in patients with adjuvant AI for breast cancer, comprising of all the currently available studies. The larger number of patients were included (n = 7699). The consistent results from sensitivity analyses and previous meta-analyses support the validity of the findings. The effects of BMAs on BMD were analyzed on the different axial skeletal sites (LS and TH) and different time points (1 year and 2 years). Additionally, our analysis is the first to report the anti-fracture efficacy of risedronate in this specific patient population. The limitation of our study is the heterogeneous characteristics of patients at baseline among the trials, which may impact the effect size of each treatment.
Conclusion
Currently, we do not have a specific recommendation for a particular BMA for postmenopausal breast cancer patients receiving an AI. Our finding revealed that BMAs, especially denosumab and zoledronate, significantly increased the BMD in LS and TH. Notably, denosumab might generate more BMD gain in cortical-bone-rich hip bone than zoledronate. Both risedronate and denosumab reduced the risk of fracture, but the anti-fracture efficacy of zoledronate, the most potent bisphosphonate, remains uncertain. In conclusion, our finding suggests denosumab might be a better option for preserving BMD and preventing fracture in postmenopausal patients receiving AI, as adjuvant therapy for breast cancer.
Abbreviations
- AI:
-
Aromatase inhibitor
- BMA:
-
Bone modifying agent
- BMD:
-
Bone mineral density
- ΔBMD:
-
BMD change from baseline (%)
- CI:
-
Confidence interval
- RR:
-
Relative risk
- LS:
-
Lumbar spine
- TH:
-
Total hip
References
Siegel RL, Miller KD, Jemal A (2020) Cancer statistics, 2020. CA Cancer J Clin 70:7–30. https://doi.org/10.3322/caac.21590
American Cancer Society Facts & Figures. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2018/cancer-facts-and-figures-2018.pdf. Accessed 18 Jan 2019
Burstein HJ, Lacchetti C, Anderson H et al (2016) Adjuvant Endocrine therapy for women with hormone receptor-positive breast cancer: American society of clinical oncology clinical practice guideline update on ovarian suppression. J Clin Oncol 34:1689–1701. https://doi.org/10.1200/JCO.2015.65.9573
Hadji P, Aapro MS, Body JJ et al (2017) Management of aromatase inhibitor-associated bone loss (AIBL) in postmenopausal women with hormone sensitive breast cancer: joint position statement of the IOF, CABS, ECTS, IEG, ESCEO IMS, and SIOG. J Bone Oncol 7:1–12
Osteoporosis International Consensus Development Statement (1997) Who are candidates for prevention and treatment for osteoporosis? Osteoporos Int 7(1):1–6. https://doi.org/10.1007/bf01623453
Hadji P (2009) Aromatase inhibitor-associated bone loss in breast cancer patients is distinct from postmenopausal osteoporosis. Crit Rev Oncol Hematol 69:73–82. https://doi.org/10.1016/j.critrevonc.2008.07.013
Howell A, Cuzick J, Baum M et al (2005) Results of the ATAC (Arimidex, Tamoxifen, Alone or in Combination) trial after completion of 5 years’ adjuvant treatment for breast cancer. Lancet 365:60–62. https://doi.org/10.1016/S0140-6736(04)17666-6
Kanis JA, Johnell O, Oden A et al (2001) Ten year probabilities of osteoporotic fractures according to BMD and diagnostic thresholds. Osteoporos Int 12:989–995. https://doi.org/10.1007/s001980170006
Kuno T, Takagi H, Sugiyama T et al (2019) Antithrombotic strategies after transcatheter aortic valve implantation: Insights from a network meta-analysis. Catheter Cardiovasc Interv. https://doi.org/10.1002/ccd.28498
Liberati A, Altman DG, Tetzlaff J et al (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. https://doi.org/10.1371/journal.pmed.1000100
Higgins JPT, Altman DG, Gøtzsche PC et al (2011) The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. https://doi.org/10.1136/bmj.d5928
Rücker G (2012) Network meta-analysis, electrical networks and graph theory. Res Synth Methods 3:312–324. https://doi.org/10.1002/jrsm.1058
Gnant M, Pfeiler G, Dubsky PC et al (2015) Adjuvant denosumab in breast cancer (ABCSG-18): a multicentre, randomised, double-blind, placebo-controlled trial. Lancet 386:433–443. https://doi.org/10.1016/S0140-6736%2815%2960995-3
Sestak I, Blake GM, Patel R et al (2019) Comparison of risedronate versus placebo in preventing anastrozole-induced bone loss in women at high risk of developing breast cancer with osteopenia. Bone 124:83–88. https://doi.org/10.1016/j.bone.2019.04.016
Greenspan SL, Vujevich KT, Brufsky A et al (2015) Prevention of bone loss with risedronate in breast cancer survivors: a randomized, controlled clinical trial. Osteoporos Int 26:1857–1864. https://doi.org/10.1007/s00198-015-3100-7
Coleman R, De Boer R, Eidtmann H et al (2013) Zoledronic acid (zoledronate) for postmenopausal women with early breast cancer receiving adjuvant letrozole (ZO-FAST study): final 60-month results. Ann Oncol 24:398–405. https://doi.org/10.1093/annonc/mds277
Brufsky AM, Harker WG, Beck JT et al (2012) Final 5-year results of Z-FAST trial: adjuvant zoledronic acid maintains bone mass in postmenopausal breast cancer patients receiving letrozole. Cancer 118:1192–1201. https://doi.org/10.1002/cncr.26313
Llombart A, Frassoldati A, Paija O et al (2012) Immediate administration of zoledronic acid reduces aromatase inhibitor-associated bone loss in postmenopausal women with early breast cancer: 12-month analysis of the E-ZO-FAST trial. Clin Breast Cancer 12:40–48. https://doi.org/10.1016/j.clbc.2011.08.002
Takahashi S, Iwase T, Kohno N et al (2012) Efficacy of zoledronic acid in postmenopausal Japanese women with early breast cancer receiving adjuvant letrozole: 12-month results. Breast Cancer Res Treat 133:685–693. https://doi.org/10.1007/s10549-012-1973-0
Van Poznak C, Hannon RA, Mackey JR et al (2010) Prevention of aromatase inhibitor-induced bone loss using risedronate: the SABRE trial. J Clin Oncol 28:967–975. https://doi.org/10.1200/JCO.2009.24.5902
Ellis GK, Bone HG, Chlebowski R et al (2009) Effect of denosumab on bone mineral density in women receiving adjuvant aromatase inhibitors for non-metastatic breast cancer: subgroup analyses of a phase 3 study. Breast Cancer Res Treat 118:81–87. https://doi.org/10.1007/s10549-009-0352-y
Greenspan SL, Brufsky A, Lembersky BC et al (2008) Risedronate prevents bone loss in breast cancer survivors: a 2-year, randomized, double-blind, placebo-controlled clinical trial. J Clin Oncol 26:2644–2652. https://doi.org/10.1200/JCO.2007.15.2967
Monda V, Lupoli GA, Messina G et al (2017) Improvement of bone physiology and life quality due to association of risedronate and anastrozole. Front Pharmacol. https://doi.org/10.3389/fphar.2017.00632
Sun S, Wang F, Dou H et al (2016) Preventive effect of zoledronic acid on aromatase inhibitor-associated bone loss for postmenopausal breast cancer patients receiving adjuvant letrozole. Onco Targets Ther 9:6029–6036. https://doi.org/10.2147/OTT.S115058
Nuzzo F, Gallo C, Lastoria S et al (2012) Bone effect of adjuvant tamoxifen, letrozole or letrozole plus zoledronic acid in early-stage breast cancer: the randomized phase 3 HOBOE study. Ann Oncol 23:2027–2033. https://doi.org/10.1093/annonc/mdr600
Safra T, Bernstein-Molho R, Greenberg J et al (2011) The protective effect of zoledronic acid on bone loss in postmenopausal women with early breast cancer treated with sequential tamoxifen and letrozole: a prospective, randomized, phase II trial. Oncology 81:298–305. https://doi.org/10.1159/000334456
Markopoulos C, Tzoracoleftherakis E, Polychronis A et al (2010) Management of anastrozole-induced bone loss in breast cancer patients with oral risedronate: results from the ARBI prospective clinical trial. Breast Cancer Res 12:R24. https://doi.org/10.1186/bcr2565
Wagner-Johnston ND, Sloan JA, Liu H et al (2015) 5-year follow-up of a randomized controlled trial of immediate versus delayed zoledronic acid for the prevention of bone loss in postmenopausal women with breast cancer starting letrozole after tamoxifen: n03CC (Alliance) trial. Cancer 121:2537–2543. https://doi.org/10.1002/cncr.29327
Su G, Xiang Y, He G et al (2014) Bisphosphonates may protect against bone loss in postmenopausal women with early breast cancer receiving adjuvant aromatase inhibitor therapy: results from a meta-analysis. Arch Med Res 45:570–579. https://doi.org/10.1016/j.arcmed.2014.10.007
Zhao X, Zhou C, Chen H et al (2017) Efficacy and safety of medical therapy for low bone mineral density in patients with Crohn disease. Medicine 96:e6378
Sanderson J, Martyn-St James M, Stevens J et al (2016) Clinical effectiveness of bisphosphonates for the prevention of fragility fractures: a systematic review and network meta-analysis. Bone 89:52–58. https://doi.org/10.1016/j.bone.2016.05.013
Early Breast Cancer Trialists’ Collaborative Group (EBCTCG) (2015) Adjuvant bisphosphonate treatment in early breast cancer: meta-analyses of individual patient data from randomised trials. Lancet 386:1353–1361. https://doi.org/10.1016/S0140-6736(15)60908-4
O’Carrigan B, Wong MHF, Willson ML et al (2017) (2017) Bisphosphonates and other bone agents for breast cancer. Cochrane Database Syst, Rev
Beaudoin C, Jean S, Bessette L et al (2016) Denosumab compared to other treatments to prevent or treat osteoporosis in individuals at risk of fracture: a systematic review and meta-analysis. Osteoporos Int 27:2835–2844
Brown JP, Roux C, Ho PR et al (2014) Denosumab significantly increases bone mineral density and reduces bone turnover compared with monthly oral ibandronate and risedronate in postmenopausal women who remained at higher risk for fracture despite previous suboptimal treatment with an oral bisphosphonate. Osteoporos Int 25:1953–1961. https://doi.org/10.1007/s00198-014-2692-7
Abdel-Rahman O (2016) Denosumab versus zoledronic acid to prevent aromatase inhibitors-associated fractures in postmenopausal early breast cancer; a mixed treatment meta-analysis. Expert Rev Anticancer Ther 16:885–891. https://doi.org/10.1080/14737140.2016.1192466
Edwards BJ, Sun M, West DP et al (2016) Incidence of atypical femur fractures in cancer patients: the MD Anderson Cancer Center experience. J Bone Miner Res 31:1569–1576. https://doi.org/10.1002/jbmr.2818
Takahashi M, Ozaki Y, Kizawa R et al (2019) Atypical femoral fracture in patients with bone metastasis receiving denosumab therapy: a retrospective study and systematic review. BMC Cancer. https://doi.org/10.1186/s12885-019-6236-6
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflicts of interest
Hirotaka Miyashita declares that he has no conflict of interest. Sera Satoi declares that she has no conflict of interest. Toshiki Kuno declares that he has no conflict of interest. Christina Cruz declares that she has no conflict of interest. Stephen Malamud declares that he has no conflict of interest. Se-Min Kim declares that he has no conflict of interest.
Research involving human participants and/or animals
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
10549_2020_5640_MOESM1_ESM.pdf
Supplementary Figure 1A: Forrest plot comparing the BMD change (%, lumbar spine) with each BMA at 2 year (MD: mean difference, CI: confidence interval). Supplementary Figure 1B: Forrest plot comparing the BMD change (%, total hip) with each BMA at 1 year (MD: mean difference, CI: confidence interval). Supplementary Figure 1C: Forrest plot comparing the BMD change (%, total hip) with each BMA at 2 year (MD: mean difference of ΔBMD, CI: confidence interval). Supplementary Figure 2: Forrest plot comparing the BMD change (%) of lumbar spine (2A and 2B) and of total hip (2C and 2D) with each BMA at 1 and 2 year after excluding a study with the greatest heterogeneity (MD: mean difference, CI: confidence interval). Supplementary Figure 3: Forrest plot comparing the BMD change (%) of lumbar spine (3A and 3B) and of total hip (3C and 3D) with each BMA at 1 and 2 year after excluding a study with the largest number of patients (MD: mean difference, CI: confidence interval). Supplementary Figure 4: Forrest plot comparing the risk of fracture with each BMA in patients with low BMD at baseline (T score < -1.0) (RR: relative risk of fracture, CI: confidence interval). Supplementary file1 (PDF 751 kb)
Rights and permissions
About this article
Cite this article
Miyashita, H., Satoi, S., Kuno, T. et al. Bone modifying agents for bone loss in patients with aromatase inhibitor as adjuvant treatment for breast cancer; insights from a network meta-analysis. Breast Cancer Res Treat 181, 279–289 (2020). https://doi.org/10.1007/s10549-020-05640-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-020-05640-3