Abstract
Purpose
The 21-gene recurrence score (RS) assay is increasingly utilized to predict the risk of recurrence in early stage estrogen receptor (ER)-positive breast cancer. We hypothesize that tumor grade and progesterone receptor (PR) status predict RS categorization.
Methods
We identified women between the ages of 18 and 74 years with stage I or II, ER-positive, invasive carcinoma of the breast from the Surveillance Epidemiology End-Results database from 2010 to 2013. Multivariable logistic regression was performed to determine factors associated with high-risk RS.
Results
We identified 42,530 patients that met inclusion criteria. Multivariable logistic regression demonstrated that grade I tumors [OR (odds ratio) 0.33, 95% CI (confidence interval) 0.31–0.37] and PR positive (PR+) status (OR 0.16, 95% CI 0.15–0.17) were significantly less likely to be associated with high-risk RS. Of patients with grade I PR+ tumors, 1% was in the high-risk group by the traditional cutoffs and 4% was in the high-risk group by the TAILORx cutoffs. The percentage of patients with high-risk RS remained low for grade I PR+ tumors regardless of age, race, tumor size, and lymph node status.
Conclusions
We found that grade I PR+ tumors are associated a < 5% probability of having high-risk RS regardless of other patient demographic or pathologic factors. This suggests that the histologic factors of grade and PR status should be taken into consideration before ordering the 21-gene recurrence score assay.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The 21-gene recurrence score (RS) assay (Oncotype Dx, Genomic Health, Redwood City, CA) provides a method of risk stratification for patients who have stage I or II, estrogen-receptor (ER)-positive, and human epidermal growth factor receptor 2 (HER2)-negative breast cancer. The assay evaluates the expression level of 21 genes in tumor cells and yields a RS from 0 to 100. The RS can estimate the risk of locoregional and distant recurrence over 10 years and predicts the benefit of adjuvant chemotherapy in reducing recurrence risk in both lymph node-negative and lymph node-positive patients [1,2,3,4,5,6]. Traditionally, patients have been stratified by RS into low-risk (RS < 18), intermediate-risk (RS 18–31), and high-risk (RS > 31) groups based on retrospective validation of this assay from multiple prospective trials evaluating the benefit of adjuvant chemotherapy [2]. The risk stratification cutoffs were modified to minimize under treatment of patients in an ongoing prospective trial, Trial Assigning IndividuaLized Options for Treatment (TAILORx). In this trial, low risk corresponds to a RS < 11, intermediate risk to a RS 11–25, and high risk to a RS > 25. The TAILORx study has provided early prospective data demonstrating the safety of omitting adjuvant chemotherapy in patients categorized as low-risk based on RS [3].
Since its approval for commercial use in 2004, the use of the RS assay has increased [7]. National studies using the National Cancer Database (NCDB), the Surveillance, Epidemiology, and End Results (SEER) program database, and SEER linked with Medicare show utility rates of 25 to 36% among women with early stage, hormone-receptor-positive breast cancer [7,8,9]. Several groups have correlated common clinicopathologic data with RS [10,11,12,13]. Early validation studies showed that high tumor grade significantly correlated with high-risk RS and risk of distant recurrence [1,2,3]. Institutional studies have demonstrated that progesterone (PR) negative status is associated with high RS and increased risk of recurrence over 10 years [14,15,16]. In addition, the PR status may be related to ER function and the response of the tumor to hormonal therapy [16, 17]. Multiple groups have developed nomograms or models which have correlated pathologic information such as tumor grade, ER status, PR status, and Ki-67 with RS [10,11,12,, 11, 18, 19]. These single institution studies are limited by the small size of the patient groups. With increasing rates of RS testing, identifying clinicopathologic features that can predict the probability of low- or high-risk RS can substantially improve the cost-effectiveness of the assay by precluding the need for RS testing.
Our objective was to determine if common clinicopathologic data could predict RS using the SEER database. We hypothesized that routinely reported pathological findings such as tumor grade and hormone receptor status can be used to identify early stage breast cancer patients for whom RS testing may have little benefit and can be avoided.
Methods
Data
We utilized an augmented version of the National Cancer Institute’s SEER database. SEER is composed of 18 geographically based registries providing data on cancer surveillance reflecting 28% of the United States population. The SEER registries collect patient characteristics including age at diagnosis, race, type of surgical procedure performed, use of chemotherapy, use of radiation, vital status, and cause of death (per death certificate), along with tumor characteristics including primary site, laterality, histologic subtype, stage, size, lymph node status, grade, ER status, PR status, HER2 status, and diagnostic confirmation. By request, we received linked RS data that were available beginning in 2004. HER2 status has been available in SEER since 2010.
Patients
We restricted our cohort to women aged 18–74 years diagnosed with stage I or II, grade I to III, ER-positive breast cancer with RS available from January 2010 to December 2013. The breast cancer diagnoses were identified using the World Health Organization’s International Classification of Diseases, 3rd revision (Supplementary Table 1). We excluded negative or unknown ER status, unknown PR status, unknown lymph node status, grade IV tumors, and stage IV disease. Although the SEER database contains an entry for grade IV tumors, these patients were excluded as this classification in SEER does not correlate with the standard clinical grading system. The data that we used were deidentified; therefore, this study was exempt from review by the institutional review board of the University of Minnesota.
Statistical analysis
Patients were stratified into low-, intermediate-, and high-risk groups by both the traditional and the TAILORx RS cutoffs. We performed multivariable logistic regression to evaluate for factors associated with high-risk RS based on TAILORx cutoffs. The model included patient age, race, year of diagnosis, lymph node status, PR status, tumor size, and grade. Patients with grade I and PR positive tumors were then further stratified by lymph node status, age, race, and tumor size to evaluate the relationship of risk stratification. All statistical analysis was completed using SAS software, version 9.3 (SAS Institute, Cary, NC).
Results
Tumor and patient characteristics
We identified 42,530 patients with stage I or II, grade I to III, ER-positive, HER2-negative invasive breast cancer between 2010 and 2013 (Table 1). Most of the patients were in the 55–64 age group (n = 13,979; 33%) and were non-Hispanic whites (n = 31,463; 74%). Most tumors were < 2 cm (n = 29,676; 70%), PR positive (n = 38,890; 91%), grade II (n = 23,270; 55%), and lymph node negative (n = 36,139; 85%). The most common histologic subtype in this cohort was invasive ductal carcinoma (n = 32,030; 75%), followed by mixed ductal/lobular carcinoma (n = 4,723; 11%), and invasive lobular carcinoma (n = 4,671; 11%).
Overall, based on traditional RS cutoffs, 7% (n = 2882) were high risk, 35% (n = 14,844) were intermediate risk, and 58% (n = 24,804) were low risk. Based on TAILORx RS cutoffs, 26% (n = 11,232) were high risk, 60% (n = 25,374) were intermediate risk, and 14% (n = 5924) were low risk (Table 1).
Factors associated with high-risk RS
The TAILORx RS cutoffs are being evaluated in the current ongoing prospective clinical trial [3] and will likely be the cutoffs adopted into clinical practice. We therefore conducted a multivariable logistic regression model to identify the clinicopathologic factors associated with high-risk RS stratification based on the TAILORx cutoffs alone. We found that grade I (OR 0.33; 95% CI 0.30–0.37; compared to grade II) and PR+ (OR 0.16; 95% CI 0.15–0.17) tumors had the lowest odds of being stratified as high risk (Table 2). When controlling for other factors, Grade III tumors had the highest odds of a high-risk RS (OR 5.68; 95% CI 5.31–6.07; compared to grade II). Positive lymph node status (OR 0.86; 95% CI 0.79–0.94) and Spanish–hispanic–latino race (OR 0.88; 95% CI 0.79–0.98) were associated with decreased probability of high-risk RS (OR 0.86; 95% CI 0.79–0.94). Ages 45–54 (OR 1.82; 95% CI 1.13–1.43; compared to 18–44), ages 55–64 (OR 1.09; 95% CI 1.01–1.18; compared to 18–44), diagnosis in 2010 (OR 1.14; 95% CI 1.04–1.24; compared to 2013), diagnosis in 2011 (OR 1.13; 95% CI 1.04–1.23; compared to 2013), and tumor size 2–5 cm (OR 1.32; 95% CI of 1.24–1.41; compared to < 2 cm) were all associated with modest increased chance of high-risk RS.
RS stratification among grade I and PR-positive tumors
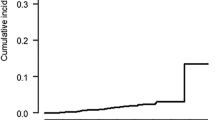
A total of 11,412 out of 42,530 patients were diagnosed with grade I PR+ breast cancer. Table 3 shows the distribution of RS in grade I PR+ patients, as stratified by the traditional and TAILORx cutoffs. With the traditional cutoffs, 1% (n = 62) of patients had high-risk RS; 25% (n = 2854) had intermediate-risk RS, and 74% (n = 8496) had low-risk RS. Using the TAILORx cutoffs, 3% (n = 334) of patients had high-risk RS; 36% (n = 4147) had intermediate-risk RS, and 61% (n = 6931) had low-risk RS.
Amongst patients with grade I PR− tumors, 17% were still categorized as high risk by TAILORx cutoffs (Table 4a). Amongst patients with grade I PR+ tumors, we further delineated the proportion of patients who received high-risk RS by categories of age, race, tumor size, and lymph node status (Table 4b). Regardless of demographic and pathologic characteristics, ≤ 5% of patients with grade I PR+ tumors were categorized as high risk.
Discussion
In this population-based study, we demonstrated that < 5% of patients with the combination of low tumor grade and PR positivity have a high-risk RS on the 21-gene RS assay. The lower odds of high-risk stratification persists regardless of other patient demographic or pathologic factors as well as method of RS stratification whether by Traditional or TAILORx cutoffs. This suggests that patients with stage I or II breast cancer with tumors that are grade I PR+ proportionally less likely of being categorized as either low or intermediate risk based on RS. For these patients, the addition of adjuvant chemotherapy would have minimal or equivocal benefit [2].
The findings of this study are consistent with other studies in which grade has been correlated with RS. After reexamination of the tissue samples from the National Surgical Adjuvant Breast and Bowel Project B-20 trial, Paik et al. demonstrated that only 5% of well-differentiated tumors had high-risk RS by the traditional cutoffs, while approximately 80% of these were low risk and 12–16% were intermediate risk [2]. Using NCDB data, Orucevic et al. examined clinicopathologic factors associated with low- or high-risk RS and found that grade I tumors were 49 times more likely to be associated with low-risk RS and that only 0.6% of these patients had high-risk RS [11]. Similarly, single institutional studies from Patin et al. and Chaudhary et al. showed that low tumor grade correlated with low RS using the traditional cutoffs [19, 14]. Our finding that low grade status was independently associated with a low likelihood of high-risk RS is consistent with previous finding and the difference in the biology of low- versus high-grade tumors. Nottingham grade is significantly associated with breast cancer-specific survival and disease-free survival, where patients with grade I tumors have the best prognosis [20]. The Nottingham grading system is derived from evaluation of mitotic index, nuclear pleomorphism, and differentiation. Microarrays of gene expression have demonstrated a difference in various cell differentiations, cell cycle progress, and proliferation genes between grade I and grade III tumors [21]. Chang et al. further demonstrated that the mitotic count component of the Nottingham grading system is associated with RS; tumors with high mitotic scores were more likely to have intermediate or high-risk RS. No patient with mitotic score of 1 had high-risk RS in this study [22]. Our study found that 1–3% of patients with grade I PR+ tumors had a high-risk RS. This may be related to the heterogeneity of the tumor subtypes included in this study, although 75% of the tumors were invasive ductal carcinoma. Additionally, Acs et al. have shown that increased presence of stroma and inflammatory cells in breast cancer samples are significantly correlated with intermediate or high RS [23]. The clinical significance of a high-risk RS in grade I PR+ tumors is uncertain, as we were unable to determine the overall survival in this study.
Our findings that PR positivity is inversely correlated with high-risk RS is also consistent with the current literature. Single institutional studies from Chaudhary et al. and Onoda et al. found that patients with PR- tumors tend to have high-risk RS [14, 15]. Furthermore, ER+ PR− tumors have been shown to have more aggressive clinical phenotype, with greater chance of positive lymph nodes and larger tumor size [24, 25]. In addition, this subset of tumors has greater genomic instability and greater proliferative rate [25]. The molecular crosstalk between PR and its regulator, ER, may also explain the difference in phenotype of PR− tumors; the loss of PR may reflect decreased responsiveness to ER− directed therapy or the presence of hyperactive growth factor pathways that downregulate PR [16, 25].
Other models to predict RS from histopathological factors have been proposed. Orucevic et al. derived nomograms involving age, tumor size, grade, PR status, lymphovascular invasion, and histologic subtype to predict the probability of low- and high-risk RS [11]. Based on single institution results, other groups have derived and validated models which use only ER and/or PR status and tumor grade [10, 12,13,14]. Kim et al. derived an online RS calculator based on ER status, PR status, Ki-67, HER2 status, and grade, that have been validated at 5 institutions [18]. Using the same histologic features of the tumor, Klein et al. have demonstrated the utility and correlation of the Magee equations, a set of equations based on immunohistologic characters of tumors, to predict RS [26]. While several analyses have found the 21-gene assay to be cost-effective [27,28,29], determining patient or tumor factors that can predict high-risk RS or low-risk RS stratification can identify patients where RS testing can be safely omitted and improve cost-effectiveness. One analysis using the Magee equations showed that if tumors with low or high-risk RS were not sent for the 21-gene assay, the estimated cost savings could be up to $2 million [30]. Our results suggest that for stage I and II, ER + breast cancer patients, grade I PR+ tumors are rarely stratified as high-risk. Further analyses will help to determine if avoiding the 21-gene RS assay in this population of patients would be cost-effective.
We acknowledge several limitations of our study. SEER is a national database consisting of patients from numerous local registries, and tumor grade information relies on the histopathological evaluation of each participating institution. Consequently, there is no central or consistent validation of pathology and grade. Studies have shown the greatest amount of inter-observer variability and pathologic discordance in tumors categorized as grade II (moderately differentiated), compared to grade I (well-differentiated), or to grade III (poorly differentiated) [1, 31, 32]. Nonetheless, complete agreement has been shown to be 75–84% in grade I tumors [31]. The SEER database also does not specify the degree of PR positivity, which may differentially impact the likelihood of high-risk RS. As HER2 status has only been available in SEER since 2010, insufficient time has passed to analyze breast cancer-specific survival. Lastly, since the design of this study is retrospective, inherent selection bias with preferential ordering of the 21-gene assay may exist in this subset. For example, in the multivariate analysis, in addition to grade I tumors, positive lymph node status was associated with a lower likelihood of a high RS. This may be attributable to selection bias of obtaining a RS in patients with positive nodal status but with otherwise low-risk clinicopathological features, as chemotherapy would otherwise have been recommended without the 21-gene assay if the patient also had other high-risk features. Despite these limitations, we believe that our analysis is robust due to large patient size and reflects the current literature regarding clinicopathologic features and RS testing.
Conclusion
Our study demonstrates that in early stage breast cancer, grade I PR+ tumors are independently predictive of having high-risk RS, regardless of patient demographics and other tumor characteristics by both traditional and TAILORx cutoffs for RS. Histologic characteristics such as tumor grade and PR status should be taken into consideration prior to obtaining 21-gene RS assay on early stage ER+ breast cancer patients. Avoiding unnecessary spending on RS testing could mean a significant reduction in the economic burden of breast cancer treatment. However, further studies will be needed to delineate the clinical significance of high-risk RS in the setting of low-grade tumors and the cost effectiveness of genomic testing.
References
Paik S, Shak S, Tang G et al (2004) A multigene assay to predict recurrence of tamoxifen-treated, node-negative breast cancer. N Engl J Med 351:2817–2826
Paik S, Tang G, Shak S et al (2006) Gene expression and benefit of chemotherapy in women with node-negative, estrogen receptor-positive breast cancer. J Clin Oncol 24:3726–3734
Sparano JA, Gray RJ, Makower DF et al (2015) Prospective validation of a 21-gene expression assay in breast cancer. N Engl J Med 373:2005–2014
Albain KS, Barlow WE, Shak S et al (2010) Prognostic and predictive value of the 21-gene recurrence score assay in postmenopausal women with node-positive, oestrogen-receptor-positive breast cancer on chemotherapy: a retrospective analysis of a randomised trial. Lancet Oncol 11:55–65
Mamounas EP, Tang G, Fisher B, Paik S, Shak S, Constantino J, Watson D, Geyer CE, Wickerham DL, Wolmack N (2010) Association between the 21-gene recurrence score and the risk of locoreginal recurrence in node-negative, estrogen receptor-positive breast cancer: Results from NSABP B-14 and NSABP B-20. J Clin Oncol 28:1677–1683
Mamounas EP, Liu Q, Paik S, Baehner F, Tang G, Jeong JH et al (2017) 21-gene recurrence score and locoregional recurrence in node-positive/ER-positive breast cancer treated with chemo-endocrine therapy. J Natl Cancer Inst 109:1–8
Enewold L, Geiger AM, Zujewski J, Harlan LC (2015) Oncotype Dx assay and breast cancer in the United States: usage and concordance with chemotherapy. Breast Cancer Res Treat 151:149–156
Orucevic A, Heidel RE, Bell JL (2016) Utilization and impact of 21-gene recurrence score assay for breast cancer in clinical practice across the United States: lessons learned from the 2010 to 2012 National Cancer Data Base analysis. Breast Cancer Res Treat 157:427–435
Dinan MA, Mi X, Reed SD, Hirsch BR, Lyman GH, Curtis LH (2015) Initial trends in the use of the 21-gene recurrence score assay for patients with breast cancer in the medicare population, 2005–2009. JAMA Oncol 1:158–166
Gage MM, Rosman M, Mylander WC et al (2015) A validated model for identifying patients unlikely to benefit from the 21-gene recurrence score assay. Clin Breast Cancer 15:467–472
Orucevic A, Bell JL, McNabb AP, Heidel RE (2017) Oncotype DX breast cancer recurrence score can be predicted with a novel nomogram using clinicopathologic data. Breast Cancer Res Treat 163:51–61
Allison KH, Kandalaft PL, Sitlani CM, Dintzis SM, Gown AM (2012) Routine pathologic parameters can predict oncotype DX recurrence scores in subsets of ER positive patients: who does not always need testing? Breast Cancer Res Treat 131:413–424
Mattes MD, Mann JM, Ashamalla H, Tejwani A (2013) Routine histopathologic characteristics can predict oncotype DX(TM) recurrence score in subsets of breast cancer patients. Cancer Invest 31:604–606
Chaudhary LN, Jawa Z, Szabo A, Visotcky A, Chitambar CR (2016) Relevance of progesterone receptor immunohistochemical staining to Oncotype DX recurrence score. Hematol Oncol Stem Cell Ther 9:48–54
Onoda T, Yamauchi H, Yagata H et al (2015) The value of progesterone receptor expression in predicting the Recurrence Score for hormone-receptor positive invasive breast cancer patients. Breast Cancer 22:406–412
Cui X, Schiff R, Arpino G, Osborne CK, Lee AV (2005) Biology of progesterone receptor loss in breast cancer and its implications for endocrine therapy. J Clin Oncol 23:7721–7735
Viale G, Regan MM, Maiorano E, Mastropasqua MG, Dell’Orto P, Rasmussen BB et al (2007) Prognostic and predictive value of centrally reviewed expression of estrogen and progesterone receptors in a randomized trial comparing letrozole and tamoxifen adjuvant therapy for postmenopausal early breast cancer: BIG 1–98. J Clin Oncol 25:3846–3852
Kim HS, Umbricht CB, Illei PB et al (2016) Optimizing the use of gene expression profiling in early-stage breast cancer. J Clin Oncol 34:4390–4397
Partin JF, Mamounas EP (2011) Impact of the 21-gene recurrence score assay compared with standard clinicopathologic guidelines in adjuvant therapy selection for node-negative, estrogen receptor-positive breast cancer. Ann Surg Oncol 18:3399–3406
Rakha EA, El-Sayed ME, Lee AH et al (2008) Prognostic significance of Nottingham histologic grade in invasive breast carcinoma. J Clin Oncol 26:3153–3158
Sotiriou C, Wirapati P, Loi S et al (2006) Gene expression profiling in breast cancer: understanding the molecular basis of histologic grade to improve prognosis. J Natl Cancer Inst 98:262–272
Chang JM, McCullough AE, Dueck AC, Kosirek HE, Ocal IT et al (2015) Back to basics: traditional Nottingham grade mitotic counts alone are significant in predicting survival in invasive breast carcinoma. Ann Surg Oncol suppl3:S509–515
Acs G, Esposito NN, Kiluk J, Loftus L, Laronga C (2012) A mitotically active, cellular tumor stroma and/or inflammatory cells associated with tumor cells may contribute to intermediate or high Oncotype DX Recurrence Scores in low-grade invasive breast carcinomas. Mod Path 25:556–566
Arpino G, Weiss H, Lee AV et al (2005) Estrogen receptor-positive, progesterone receptor-negative breast cancer: Association with growth factor receptor expression and tamoxifen resistance. J Natl Cancer Inst 97:1254–1261
Thakkar JP, Mehta DG (2011) A review of an unfavorable subset of breast cancer: estrogen receptor positive progesterone receptor negative. Oncologist 16:276–285
Klein ME, Dabbs DJ, Shuai Y, Brufsky A, Jankowitz R, Puhalla SL, Bhargava R (2013) Prediction of the Oncotype DX recurrence score: use of pathology-generated equations derived by linear regression analysis. Mod Path 26:658–664
Smyth L, Watson G, Walsh EM et al (2015) Economic impact of 21-gene recurrence score testing on early-stage breast cancer in Ireland. Breast Cancer Res Treat 153:573–582
Lyman GH, Cosler LE, Kuderer NM, Hornberger J (2007) Impact of a 21-gene RT-PCR assay on treatment decisions in early-stage breast cancer: an economic analysis based on prognostic and predictive validation studies. Cancer 109:1011–1018
Lamond NW, Skedgel C, Rayson D, Lethbridge L, Younis T (2012) Cost-utility of the 21-gene recurrence score assay in node-negative and node-positive breast cancer. Breast Cancer Res Treat 133:1115–1123
Turner BM, Skinner KA, Tang P et al (2015) Use of modified Magee equations and histologic criteria to predict the Oncotype DX recurrence score. Mod Pathol 28:921–931
Bueno-de-Mesquita JM, Nuyten DS, Wesseling J, van Tinteren H, Linn SC, van de Vijver MJ (2010) The impact of inter-observer variation in pathological assessment of node-negative breast cancer on clinical risk assessment and patient selection for adjuvant systemic treatment. Ann Oncol 21:40–47
Robbins PPS, de Klerk N, Dawkins H, Harvey J, Sterrett G, Ellis I, Elston C (1995) Histologic grading of breast carcinomas: a study of interobserver agreement. Hum Pathol 26:873–879
Bardou VJ, Arpino G, Elledge RM et al (2003) Progesterone receptor status significantly improves outcome prediction over estrogen receptor status alone for adjuvant endocrine therapy in two large breast cancer databases. J Clin Oncol 21:1973–1979
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Huang, J.L., Kizy, S., Marmor, S. et al. Tumor grade and progesterone receptor status predict 21-gene recurrence score in early stage invasive breast carcinoma. Breast Cancer Res Treat 172, 671–677 (2018). https://doi.org/10.1007/s10549-018-4955-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-018-4955-z