Abstract
Obese breast cancer patients have a higher risk of lymph node metastasis and a poorer prognosis compared to patients with normal weight. For obese women with node-positive breast cancer, an association between body weight and prognosis remains unclear. In this retrospective study, we analyzed patient data from the Phase-III ADEBAR trial, in which high-risk breast cancer patients (pT1–4, pN2–3, pM0) were randomized into a docetaxel-based versus epirubicin-based chemotherapy regimen. Patients were grouped according to their BMI value as underweight/normal weight (BMI < 25 kg/m2; n = 543), overweight (BMI 25–29.9 kg/m2; n = 482) or obese (BMI ≥ 30 kg/m2; n = 285). Overweight and obese patients were older, had larger tumors and were more likely to be postmenopausal at the time of diagnosis compared to underweight/normal-weight patients (all p < 0.001). Multivariate Cox regression analyses adjusting for age and histopathological tumor features showed that obese patients had a significantly shorter disease-free survival (DFS; HR 1.43; 95 % CI 1.11–1.86; p = 0.006) and overall survival (OS; HR 1.56; 95 % CI 1.14–2.14; p = 0.006) than non-obese patients. Subgroup analyses revealed that the differences in DFS and OS were significant for postmenopausal but not for premenopausal patients, and that the survival benefit of non-obese patients was more pronounced in women with hormone-receptor-positive disease. Obesity constitutes an independent, adverse prognostic factor in high-risk node-positive breast cancer patients, in particular for postmenopausal women and women with hormone-receptor-positive disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obesity is a major risk factor for morbidity throughout the world [1] and is associated with an increased risk of mortality due to diabetes and kidney diseases, coronary heart disease, and other cardiovascular ailments [2]. Obesity has also been linked to an increased incidence of cancer and cancer mortality [2, 3]. Several studies have investigated the association between body weight or body mass index (BMI) and breast cancer incidence, and there is convincing evidence that overweight or obese postmenopausal women have an increased risk of breast cancer as compared to normal-weight women [4, 5]. However, the available data for premenopausal women are less clear and several large studies or meta-analyses found no significant relationship between BMI and breast cancer risk or even an inverse association with overweight or obese premenopausal women having a reduced breast cancer risk [6].
In addition to other mechanistic links, it has been established that excess estrogen levels contribute to the development of breast cancer in obese women [7, 8], and multiple studies have shown that the association between obesity and breast cancer risk is especially pronounced for hormone-receptor-positive breast cancer. However, positive associations between obesity and breast cancer risk have also been demonstrated for triple-negative breast cancer [9, 10].
Overweight and obesity are not only linked to breast cancer incidence, but women that are obese at the time of breast cancer diagnosis also have worse outcomes compared to normal-weight patients in terms of recurrence and survival [11, 12]. However, most studies investigating the relationship between BMI and recurrence or survival are based on patients with either very heterogeneous tumor characteristics or early stage low-risk breast cancer, while very few data exist on the specific impact of obesity on prognosis for high-risk breast cancer patients. Therefore, we analyzed BMI and outcome data from node-positive breast cancer patients (pT1–4, pN2–3, pM0) that were recruited in a clinical trial involving exclusively women with high-risk breast cancer, the German ADEBAR trial. The aim of our study was to investigate the association between BMI at time of diagnosis, baseline histopathological tumor characteristics and outcome in terms of disease-free survival (DFS) and overall survival (OS). In addition, we performed subgroup analyses with respect to menopausal status and hormone receptor status, which are the two factors most likely to affect the relationship between BMI and outcome in breast cancer patients.
Patients and methods
The ADEBAR study is a prospective, randomized, multicenter Phase-III trial with the primary endpoint of DFS in high-risk breast cancer patients (defined as >4 cancerous lymph nodes). This study involves randomizing a sequential anthracycline-docetaxel regimen (Treatment arm A: EC-Doc: 4 cycles of epirubicin (E) 90 mg/m2 BSA plus cyclophosphamide (C) 600 mg/m2 BSA q21d, followed by 4 cycles of docetaxel (D) 100 mg/m2 BSA q21d) against an anthracycline-containing standard chemotherapy (Treatment arm B: FEC120: 6 cycles of E60 mg/m2 BSA d 1 + 8, 5- fluorouracil 500 mg/m2 BSA d 1 + 8 und C 75 mg/m2 BSA d 1−14, q28d). Secondary endpoints include OS, chemotherapy-toxicity, and quality of life.
Patients and recruitment
Between September 2001 and May 2005, 1493 women between the age of 18 and 70 years with completely resected, lymph node-positive primary breast cancer (pT1–4, pN2–3, pM0) were randomized (748 in treatment arm A and 745 in treatment arm B) in the ADEBAR trial after signing an informed consent form. Patients suffering from metastatic, inflammatory breast cancer or other primary malignancies were not included. Additionally, pregnant or lactating patients or those with known cardiac disorders or hypersensitivity to any of the study medications were excluded. Of the 218 registered study centers, 198 (91 %) actively participated in patient recruitment. Body weight was measured using a calibrated scale under standardized conditions, height was measured to the nearest 0.5 cm. BMI was calculated as weight in kg divided by the square of height in meter.
Endocrine treatment
Patients who had hormone-receptor-positive breast cancer (estrogen and/or progesterone receptor levels ≥10 %) received tamoxifen (20 mg/dpo), while postmenopausal patients with a contraindication to tamoxifen were given an anti-aromatase agent for 5 years. Patients with a positive hormone receptor status that were under 40 years of age, menstruated within 6 months after completing chemotherapy, or exhibited levels of LH < 20 mI U/ml, FSH < 20 mI U/ml and E2 > 20 pg/ml also received goserelin (3.6 mg q1 msc) for 2 years.
Data analysis
Overall, data on survival and BMI were available for 1310 of the 1493 randomized patients (see CONSORT diagram, Fig. 1). Data from both randomization arms were pooled for an explorative retrospective analysis to study the relationship between BMI at baseline and survival. Patients were grouped according to the following World Health Organization (WHO) criteria for BMI: underweight, <18.5 kg/m2 (n = 13); normal weight, 18.5–24.9 kg/m2 (n = 530); overweight, 25.0–29.9 kg/m2 (n = 482); and obese, ≥30.0 kg/m2 (n = 285). Due to the low number of patients with a BMI below 18.5, underweight and normal-weight patients were combined into one group for further analyses (underweight/normal weight, n = 543).
Patient outcome was analyzed in terms of both DFS (with local, contralateral, and distant disease recurrence as well as secondary primary tumors and death from any cause defined as event) and OS (with death from any cause defined as event). The time-to-event intervals were measured from the date of randomization to the date of the event. Data were censored at the date of the last adequate follow-up in case no event was reported. Median follow-up was 60.6 months.
Statistical analyses were performed using SPSS software, version 19 (SPSS Inc., Chicago, IL, USA). Descriptive statistics for categorical data were summarized using frequency tables presenting absolute and relative frequencies. Associations between BMI group and patient or tumor characteristics were evaluated using Chi Square tests. Survival estimates were obtained using the Kaplan–Meier product limit method and survival curves were compared using log-rank tests. Effects of multiple covariates on survival endpoints were calculated using Cox proportional hazards regression models. All statistical tests were two-sided, and p < 0.05 was considered statistically significant.
To analyze whether BMI group constitutes an independent prognostic factor for DFS and OS, we used Cox proportional hazards regression models adjusted for age class (≤40, 41–50, 51–60, >60), menopausal status (premenopausal, postmenopausal), tumor stage (pT1, pT2, pT3, pT4), nodal stage (pN2, pN3), histological grading (G1, G2, G3), histological type (ductal, lobular, other), hormone receptor status (positive, negative), Her2 status (positive, negative), and chemotherapy treatment (EC-Doc, FEC120). Effects of multiple covariates on survival endpoints were calculated using Cox proportional hazards regression models.
Results
Association of BMI with baseline patient and tumor characteristics
No significant differences were found between BMI groups (underweight/normal weight, overweight, obese) with regard to the histopathological tumor features nodal stage, tumor grade, histological subtype, hormone receptor status, and Her2 receptor status (see Table S1). In addition, patients in the three BMI groups were equally likely to receive either the EC-Doc or the FEC120 chemotherapy (Table S1). However, the BMI category was significantly associated with tumor size, age, and menopausal status. Both overweight and obese patients had larger tumors (more pT3 and pT4 tumors and less pT1 tumors) as compared to underweight/normal-weight patients (Table S1). Furthermore, overweight and obese patients were older at the time of primary diagnosis than underweight/normal-weight patients, as patients with a BMI exceeding 25.0 kg/m2 were more often 60 years or older and less often younger than 50 years compared to patients with a BMI under 25.0 kg/m2 (Table S1). Finally, the BMI groups differed significantly with regard to menopausal status. Nearly half of the women (47.3 %) in the underweight/normal-weight subgroup were premenopausal, whereas only 30.7 and 28.8 % of the women were premenopausal in the overweight and obese subgroup, respectively (Table S1).
BMI and outcome
Overall, 362 (27.6 %) patients showed disease recurrence, and median DFS was 105.1 months (95 % CI 101.9–108.3 months). There were significant differences in DFS among the three BMI groups (log-rank test; p = 0.004; see Fig. 2a). Median DFS was 104.5 months (95 % CI 100.0–109.1 months) for underweight/normal-weight patients (140 events, 25.8 %) and 77.2 months (95 % CI 69.0–85.3 months) for obese patients (98 events, 34.4 %), while median DFS was not reached in our study for overweight patients (124 events, 25.7 %). Pairwise comparisons using log-rank tests revealed that both underweight/normal-weight patients (p = 0.004) and overweight patients (p = 0.003) had better survival prospects in terms of prolonged DFS as compared to obese patients, while there was no significant difference regarding DFS between underweight/normal-weight and overweight patients (p = 0.788). Based on these results, we combined all patients with a BMI below 30 (non-obese) and performed a multivariate Cox regression analysis to test whether the parameter BMI group (obese vs. non-obese) had prognostic relevance for DFS independently from other well-known prognostic factors. The multivariate analysis confirmed that obesity was an independent prognostic factor for poor DFS, with a hazard ratio (HR) of 1.43 (95 % CI 1.11–1.86; p = 0.006; see Table S2).
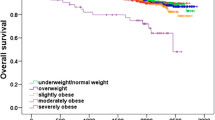
225 patients died during follow-up. Similar to DFS, there were significant differences in OS among BMI groups (log-rank test; p = 0.004; see Fig. 2b). Again, both underweight/normal-weight patients and overweight patients had significantly prolonged OS as compared to obese patients (p = 0.001 and 0.019, respectively), while there was no significant difference regarding OS between underweight/normal-weight and overweight patients (p = 0.345). A multivariate Cox regression showed that obesity (obese vs. non-obese) was an independent predictor of poor OS (HR 1.56; 95 % CI 1.14–2.14; p = 0.006; see Table S3).
Effect of menopausal status
We performed separate analyses to compare DFS and OS between obese and non-obese patients for premenopausal and postmenopausal women. The corresponding survival plots are shown in Fig. 3. Both DFS and OS were significantly different between obese and non-obese postmenopausal patients (log-rank test; p = 0.002 and 0.001, respectively), while there were no significant differences regarding DFS and OS between obese and non-obese premenopausal patients (log-rank test; p = 0.325 and 0.524, respectively). The results of these univariate analyses were confirmed by multivariate Cox regressions adjusting for age, and histopathological tumor characteristics. Obese postmenopausal patients had a significantly shorter DFS (HR 1.56; 95 % CI 1.15–2.12; p = 0.004) and OS (HR 1.79; 95 % CI 1.25–2.58; p = 0.002) than non-obese postmenopausal women. In contrast, the multivariate Cox regression revealed no differences in DFS or OS between obese and non-obese premenopausal patients (DFS: HR 1.06; 95 % CI 0.63–1.76; p = 0.84; OS: HR 0.94; 95 % CI 0.46–1.89; p = 0.853).
Effect of hormone receptor status
To assess whether the association between BMI and outcome was affected by hormone receptor status, we compared DFS and OS between obese and non-obese women separately for patients with a hormone-receptor-positive and patients with a hormone-receptor-negative tumor. Kaplan–Meier survival plots are shown in Fig. 4.
Log-rank tests revealed that obese women with hormone-receptor-positive breast cancer had a significantly worse DFS and OS compared to non-obese women with hormone-receptor-positive breast cancer (p = 0.001 and 0.003, respectively). Multivariate Cox regressions confirmed these results for DFS (HR 1.53; 95 % CI 1.12–2.09; p = 0.007), but failed to show a significant prolonged OS in non-obese as compared to obese women with hormone-receptor-positive tumors, though the hazard ratio was similar as for DFS and statistical significance was borderline (HR 1.48; 95 % CI 0.99–2.21; p = 0.057).
In women with hormone-receptor-negative tumors, both univariate log-rank tests and multivariate Cox regressions showed no difference in DFS between obese and non-obese women (log-rank test: p = 0.193; Cox regression: HR 0.87; 95 % CI 0.53–1.44; p = 0.597). For OS, a slight and barely significant survival benefit in non-obese women revealed by a univariate log-rank test (p = 0.047; see Fig. 4c) was not confirmed by multivariate Cox regression (HR 1.23; 95 % CI 0.70–2.16; p = 0.468).
Discussion
Our data show that obesity constitutes an independent, adverse risk factor in patients with node-positive high-risk primary breast cancer. Women who were obese (BMI ≥ 3 0 kg/m2) at the time of breast cancer diagnosis had a significantly shorter DFS and OS as compared to women who were non-obese (BMI < 30 kg/m2) at the time of primary diagnosis. No differences in DFS or OS were found between overweight (BMI 25–29.9 kg/m2) and underweight/normal-weight (BMI < 25 kg/m2) patients. Subgroup analyses showed that the association of obesity with poor DFS and OS was significant for postmenopausal patients, while no such association was found for premenopausal patients. Furthermore, a significant inverse relationship between obesity and outcome was found for patients with hormone-receptor-positive breast cancer, but not for patients with hormone-receptor-negative disease.
The association between obesity and breast cancer risk is well known, and two recent large meta-analyses have confirmed that obesity constitutes a risk factor for breast cancer recurrence and poor survival [13, 14]. Obese women with breast cancer are typically diagnosed late in life, have large primary tumors and a high number of lymph node metastases [15–17]. Thus, the advanced or potentially more aggressive disease of women with a high BMI at diagnosis might contribute to the worse prognosis found in obese breast cancer patients. We investigated whether obese patients had also more advanced tumors at the time of primary diagnosis in our pre-selected study sample of patients with high-risk node-positive disease (pT1–4, pN2–3, pM0). While we found no differences regarding grading, hormone receptor status or Her2 status, overweight and obese patients were diagnosed at an older age, had larger tumors and were more likely to be postmenopausal than underweight/normal-weight patients. However, our results showed that BMI significantly affects DFS and OS independently from other well-known prognostic tumor characteristics, in accordance with several other studies that have demonstrated the prognostic role of BMI for recurrence and/or survival independently from histopathological tumor features [12, 18, 19].
To our knowledge, there are only two other studies that explicitly investigated the effect of obesity on DFS and OS in node-positive breast cancer patients based on data collected in randomized clinical trials. A retrospective analysis of patients enrolled in the randomized Phase-III BIG 02-98 trial reported that obesity was associated with poorer outcome independently from other prognostic factors [19]. In contrast, a recent pooled analysis of two randomized French trials found no significant influence of obesity on DFS or OS after adjusting for tumor characteristics [20]. Both studies differed from our study with regard to the number of positive lymph nodes of patients included; while the majority of patients in these two studies had only 1–3 positive lymph nodes, our study comprised only high-risk patients with more than 3 positive lymph nodes. Nevertheless, the reason for the lack of a significant negative effect of obesity on breast cancer prognosis in the French population remains unclear, and the authors could only speculate that local dietary habits and/or types and intensities of adjuvant chemotherapies might reduce the negative impact of obesity [20].
Similar to menopausal status, evidence for an effect of hormone receptor status on the association between obesity and survival in breast cancer patients is equivocal. Some studies found that obesity was associated with poor survival independently from hormone receptor status [21, 22], while other studies reported that the association between obesity and inferior outcome was more pronounced for patients with hormone-receptor-positive breast cancer [17, 23].
Most recently, the Early Breast Cancer Trialists’ Collaborative Group (EBCTCG) presented the results of a large study comprising 80,000 women enrolled in 70 clinical trials [24]. Quite surprisingly, obesity significantly increased the risk of breast cancer-related mortality in premenopausal women with estrogen-receptor-positive breast cancer compared to normal-weight patients, but had little effect on breast cancer-related mortality in postmenopausal women with estrogen-receptor-positive disease. No effect of obesity on breast cancer-related mortality in women with estrogen-receptor-negative disease was found.
Overall, the conflicting results regarding the effect of menopausal and hormone receptor status on the association between obesity and outcome in breast cancer patients, which might partly be due to differences with regard to patient cohorts and received treatments, show that currently the mechanisms underlying the link between obesity and prognosis are complex and far from being completely understood. Studies that found an association between obesity and outcome in premenopausal and/or hormone-receptor-negative breast cancer patients suggest that molecular mechanisms not related to sex hormone levels play an important role, at least in particular subgroups. Clearly, both more basic research on the molecular mechanisms and carefully designed clinical trials are needed to increase our understanding of the apparently complex link between obesity and breast cancer.
However, despite the limited knowledge regarding the mechanistic link, it seems clear that obesity plays a significant role for prognosis at least in some breast cancer patients. Thus, dietary and lifestyle interventions resulting in weight loss have been suggested to reduce recurrence rates in addition to providing secondary benefits [25]. Several studies have shown that interventions based on controlling dietary quality and/or physical activity patterns can be successful in reducing body weight of breast cancer patients [26–28]. Two large clinical trials, the Women’s Intervention Nutrition Study (WINS) and women’s healthy eating and living (WHEL) have investigated the effect of dietary interventions on disease recurrence in early stage breast cancer patients [29, 30]. A reduction in dietary fat and modest average weight loss was associated with a reduced recurrence of breast cancer in the WINS trial [29]. This result, however, was not confirmed in the WHEL trial, in which dietary intervention neither resulted in weight loss nor changed breast cancer prognosis in patients [30]. SUCCESS C [31], DIANA-5 [32] and ENERGY [33] are three large ongoing randomized lifestyle intervention trials on breast cancer patients that assess the effect of an intervention aimed at increased physical activity combined with dietary counseling on breast cancer recurrence and survival. The results of these studies will hopefully shed light on the question of whether lifestyle interventions in breast cancer patients targeting body weight and physical activity can indeed influence recurrence and survival.
In conclusion, our study showed that obesity constitutes an independent, adverse prognostic factor in high-risk node-positive breast cancer patients, in particular for postmenopausal women and women with hormone-receptor-positive disease. Obese high-risk breast cancer patients might benefit from adhering to a healthy lifestyle aiming at body weight control as part of a comprehensive oncologic therapy.
References
Guh DP, Zhang W, Bansback N, Amarsi Z, Birmingham CL, Anis AH (2009) The incidence of co-morbidities related to obesity and overweight: a systematic review and meta-analysis. BMC Public Health 9:88
Flegal KM, Graubard BI, Williamson DF, Gail MH (2007) Cause-specific excess deaths associated with underweight, overweight, and obesity. JAMA 298(17):2028–2037
Renehan AG, Tyson M, Egger M, Heller RF, Zwahlen M (2008) Body-mass index and incidence of cancer: a systematic review and meta-analysis of prospective observational studies. Lancet 371(9612):569–578
Cheraghi Z, Poorolajal J, Hashem T, Esmailnasab N, Doosti Irani A (2012) Effect of body mass index on breast cancer during premenopausal and postmenopausal periods: a meta-analysis. PLoS One 7(12):e51446
Suzuki R, Orsini N, Saji S, Key TJ, Wolk A (2009) Body weight and incidence of breast cancer defined by estrogen and progesterone receptor status—a meta-analysis. Int J Cancer 124(3):698–712
Ursin G, Longnecker MP, Haile RW, Greenland S (1995) A meta-analysis of body mass index and risk of premenopausal breast cancer. Epidemiology 6(2):137–141
Simpson ER, Brown KA (2013) Minireview: obesity and breast cancer: a tale of inflammation and dysregulated metabolism. Mol Endocrinol 27(5):715–725
Key TJ, Appleby PN, Reeves GK, Roddam A, Dorgan JF, Longcope C, Stanczyk FZ, Stephenson HE Jr, Falk RT, Miller R, Schatzkin A, Allen DS, Fentiman IS, Wang DY, Dowsett M, Thomas HV, Hankinson SE, Toniolo P, Akhmedkhanov A, Koenig K, Shore RE, Zeleniuch-Jacquotte A, Berrino F, Muti P, Micheli A, Krogh V, Sieri S, Pala V, Venturelli E, Secreto G, Barrett-Connor E, Laughlin GA, Kabuto M, Akiba S, Stevens RG, Neriishi K, Land CE, Cauley JA, Kuller LH, Cummings SR, Helzlsouer KJ, Alberg AJ, Bush TL, Comstock GW, Gordon GB, Miller SR (2003) Body mass index, serum sex hormones, and breast cancer risk in postmenopausal women. J Natl Cancer Inst 95(16):1218–1226
Maiti B, Kundranda MN, Spiro TP, Daw HA (2009) The association of metabolic syndrome with triple-negative breast cancer. Breast Cancer Res Treat 121(2):479–483
Pierobon M, Frankenfeld CL (2012) Obesity as a risk factor for triple-negative breast cancers: a systematic review and meta-analysis. Breast Cancer Res Treat 137(1):307–314
Calle EE, Rodriguez C, Walker-Thurmond K, Thun MJ (2003) Overweight, obesity, and mortality from cancer in a prospectively studied cohort of U.S. adults. N Engl J Med 348(17):1625–1638
Ewertz M, Jensen MB, Gunnarsdottir KA, Hojris I, Jakobsen EH, Nielsen D, Stenbygaard LE, Tange UB, Cold S (2011) Effect of obesity on prognosis after early-stage breast cancer. J Clin Oncol 29(1):25–31
Protani M, Coory M, Martin JH (2010) Effect of obesity on survival of women with breast cancer: systematic review and meta-analysis. Breast Cancer Res Treat 123(3):627–635
Chan DS, Vieira AR, Aune D, Bandera EV, Greenwood DC, McTiernan A, Navarro Rosenblatt D, Thune I, Vieira R, Norat T (2014) Body mass index and survival in women with breast cancer-systematic literature review and meta-analysis of 82 follow-up studies. Ann Oncol 25(10):1901–1914
Biglia N, Peano E, Sgandurra P, Moggio G, Pecchio S, Maggiorotto F, Sismondi P (2012) Body mass index (BMI) and breast cancer: impact on tumor histopathologic features, cancer subtypes and recurrence rate in pre and postmenopausal women. Gynecol Endocrinol 29(3):263–267
Haakinson DJ, Leeds SG, Dueck AC, Gray RJ, Wasif N, Stucky CC, Northfelt DW, Apsey HA, Pockaj B (2012) The impact of obesity on breast cancer: a retrospective review. Ann Surg Oncol 19(9):3012–3018
Majed B, Moreau T, Senouci K, Salmon RJ, Fourquet A, Asselain B (2008) Is obesity an independent prognosis factor in woman breast cancer? Breast Cancer Res Treat 111(2):329–342
Berclaz G, Li S, Price KN, Coates AS, Castiglione-Gertsch M, Rudenstam CM, Holmberg SB, Lindtner J, Erien D, Collins J, Snyder R, Thurlimann B, Fey MF, Mendiola C, Werner ID, Simoncini E, Crivellari D, Gelber RD, Goldhirsch A (2004) Body mass index as a prognostic feature in operable breast cancer: the International Breast Cancer Study Group experience. Ann Oncol 15(6):875–884
de Azambuja E, McCaskill-Stevens W, Francis P, Quinaux E, Crown JP, Vicente M, Giuliani R, Nordenskjold B, Gutierez J, Andersson M, Vila MM, Jakesz R, Demol J, Dewar J, Santoro A, Lluch A, Olsen S, Gelber RD, Di Leo A, Piccart-Gebhart M (2009) The effect of body mass index on overall and disease-free survival in node-positive breast cancer patients treated with docetaxel and doxorubicin-containing adjuvant chemotherapy: the experience of the BIG 02-98 trial. Breast Cancer Res Treat 119(1):145–153
Kamineni A, Anderson ML, White E, Taplin SH, Porter P, Ballard-Barbash R, Malone K, Buist DS (2012) Body mass index, tumor characteristics, and prognosis following diagnosis of early-stage breast cancer in a mammographically screened population. Cancer Causes Control 24(2):305–312
Niraula S, Ocana A, Ennis M, Goodwin PJ (2012) Body size and breast cancer prognosis in relation to hormone receptor and menopausal status: a meta-analysis. Breast Cancer Res Treat 134(2):769–781
Pajares B, Pollan M, Martin M, Mackey JR, Lluch A, Gavila J, Vogel C, Ruiz-Borrego M, Calvo L, Pienkowski T, Rodriguez-Lescure A, Segui MA, Tredan O, Anton A, Ramos M, Camara Mdel C, Rodriguez-Martin C, Carrasco E, Alba E (2013) Obesity and survival in operable breast cancer patients treated with adjuvant anthracyclines and taxanes according to pathological subtypes: a pooled analysis. Breast Cancer Res 15(6):R105
Sparano JA, Wang M, Zhao F, Stearns V, Martino S, Ligibel JA, Perez EA, Saphner T, Wolff AC, Sledge GW Jr, Wood WC, Fetting J, Davidson NE (2012) Obesity at diagnosis is associated with inferior outcomes in hormone receptor-positive operable breast cancer. Cancer 118(23):5937–5946
Pan H, Gray R (2014) Effect of obesity in premenopausal ER+ early breast cancer: EBCTCG data on 80,000 patients in 70 trials. In: ASCO annual meeting abstract 503 present 31 May 2014
Chlebowski RT (2013) Nutrition and physical activity influence on breast cancer incidence and outcome. Breast 22(Suppl 2):S30–S37
Goodwin PJ, Segal RJ, Vallis M, Ligibel JA, Pond GR, Robidoux A, Blackburn GL, Findlay B, Gralow JR, Mukherjee S, Levine M, Pritchard KI (2014) Randomized trial of a telephone-based weight loss intervention in postmenopausal women with breast cancer receiving letrozole: the LISA trial. J Clin Oncol 32(21):2231–2239
Morey MC, Snyder DC, Sloane R, Cohen HJ, Peterson B, Hartman TJ, Miller P, Mitchell DC, Demark-Wahnefried W (2009) Effects of home-based diet and exercise on functional outcomes among older, overweight long-term cancer survivors: renew: a randomized controlled trial. JAMA 301(18):1883–1891
Reeves MM, Terranova CO, Eakin EG, Demark-Wahnefried W (2014) Weight loss intervention trials in women with breast cancer: a systematic review. Obes Rev 15(9):749–768
Chlebowski RT, Blackburn GL, Thomson CA, Nixon DW, Shapiro A, Hoy MK, Goodman MT, Giuliano AE, Karanja N, McAndrew P, Hudis C, Butler J, Merkel D, Kristal A, Caan B, Michaelson R, Vinciguerra V, Del Prete S, Winkler M, Hall R, Simon M, Winters BL, Elashoff RM (2006) Dietary fat reduction and breast cancer outcome: interim efficacy results from the women’s intervention nutrition study. J Natl Cancer Inst 98(24):1767–1776
Pierce JP, Natarajan L, Caan BJ, Parker BA, Greenberg ER, Flatt SW, Rock CL, Kealey S, Al-Delaimy WK, Bardwell WA, Carlson RW, Emond JA, Faerber S, Gold EB, Hajek RA, Hollenbach K, Jones LA, Karanja N, Madlensky L, Marshall J, Newman VA, Ritenbaugh C, Thomson CA, Wasserman L, Stefanick ML (2007) Influence of a diet very high in vegetables, fruit, and fiber and low in fat on prognosis following treatment for breast cancer: the women’s healthy eating and living (WHEL) randomized trial. JAMA 298(3):289–298
Rack B, Andergassen U, Neugebauer J, Salmen J, Hepp P, Sommer H, Lichtenegger W, Friese K, Beckmann MW, Hauner D, Hauner H, Janni W (2010) The German SUCCESS C study—the first european lifestyle study on breast cancer. Breast Care (Basel) 5(6):395–400
Villarini A, Pasanisi P, Traina A, Mano MP, Bonanni B, Panico S, Scipioni C, Galasso R, Paduos A, Simeoni M, Bellotti E, Barbero M, Macellari G, Venturelli E, Raimondi M, Bruno E, Gargano G, Fornaciari G, Morelli D, Seregni E, Krogh V, Berrino F (2012) Lifestyle and breast cancer recurrences: the DIANA-5 trial. Tumori 98(1):1–18
Rock CL, Byers TE, Colditz GA, Demark-Wahnefried W, Ganz PA, Wolin KY, Elias A, Krontiras H, Liu J, Naughton M, Pakiz B, Parker BA, Sedjo RL, Wyatt H (2012) Reducing breast cancer recurrence with weight loss, a vanguard trial: the exercise and nutrition to enhance recovery and good health for you (ENERGY) trial. Contemp Clin Trials 34(2):282–295
Conflict of interest
All authors declare that there is no conflict of interest. W. Janni holds a consulting and advisory function at Sanofi-Aventis and Amgen.
Author information
Authors and Affiliations
Corresponding author
Additional information
Christoph Scholz and U. Andergassen have contributed equally.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Scholz, C., Andergassen, U., Hepp, P. et al. Obesity as an independent risk factor for decreased survival in node-positive high-risk breast cancer. Breast Cancer Res Treat 151, 569–576 (2015). https://doi.org/10.1007/s10549-015-3422-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-015-3422-3