Abstract
Previous studies on the association between mammography screening and stage at breast cancer (BC) diagnosis have limitations because they did not analyze persistence with mammography screening and did not distinguish screening from diagnostic mammograms. The objective of this study is to determine the association between persistence with mammography screening and stage at BC diagnosis among elderly women. A retrospective observational study of 39,006 women age ≥70 diagnosed with incident BC from 2005 to 2009 from the Surveillance, Epidemiology, and End Results (SEER)-Medicare dataset was conducted. A validated algorithm with high sensitivity and specificity was used to distinguish between screening and diagnostic mammograms. Persistence with mammography screening was measured as having at least three screening mammograms in five years before BC diagnosis. Multinomial logistic regressions were performed to analyze the association between persistence with mammography screening and stage at diagnosis, in a multivariate framework. Overall, 46 % of elderly women were persistent with mammography screening, 26 % were not persistent, and 28 % did not have any screening mammogram in five years before BC diagnosis. As compared to women who were not persistent with mammography screening, women who were persistent with mammography screening were significantly more likely to be diagnosed at earlier stages of BC. The adjusted odds ratios were 3.28, 2.37, and 1.60 for in situ, local, and regional stages, respectively. A lower proportion of elderly women was persistent with mammography and it was highly associated with earlier stages of BC diagnosis. Interventions designed to promote persistent mammography screening among elderly women are warranted.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Breast cancer (BC), the most common cancer is the second leading cause of cancer death in women in the United States (US). The incidence and mortality rates for BC vary significantly by age. Based on the 2005–2009 Surveillance, Epidemiology, and End Results (SEER) statistics, 41 % of the new BC cases, and 57.4 % of BC deaths occurred in women age 65 and above [1]. The overall incidence of BC was 82.97 per 100,000 women for those age below 65 years and was 421.30 per 100,000 women for those age 65 and above. The overall mortality from BC was 11.15 per 100,000 women for those below 65 years of age and was 98.64 per 100,000 women for those age 65 and above [1]. Also women age 65 and above have a greater burden of BC as tumor in these women is found at advanced stages and with larger sizes leading to poorer survival [2].
Even though mammography screening reduces BC-related mortality by 20–35 % in women age 40–69 years [3–7], it is yet not clear whether or not mammography screening is beneficial in women age 70 and above. This is because very few screening trials evaluating the benefits of mammography screening have included women aged 70 and above [8]. Although elderly women have a greater burden of BC since tumor is found at more advanced stages and with larger sizes [2], they are less likely to utilize mammography screening [9, 10]. About 64 % of women age 65 and above have had mammography screening within the previous 2 years as compared to 73 % among women age 50–64 years [11] in spite of the fact that annual mammography screenings are covered by both Medicare and Medicaid. This may be partly due to the uncertainty regarding the frequency and upper age limit for mammography screening as reflected in the BC screening guidelines. The US Preventive Service Task Force recommends biennial mammography screening for women in age group 69–74 years, but reported insufficient evidence for women above 74 years of age [12]. In contrast, the American Cancer Society recommends annual mammography screening with no set upper age limit for women till her life expectancy is at least 5 years [13]. In the absence of no direct evidence of beneficial effects of mammography screening and with its suggested potential and immediate harms in elderly women, this group encounters contrasting guidelines and recommendations for mammography screening which may ultimately affect their screening behavior and lead to poorer BC outcomes. Physicians have several mammography screening guidelines from which to choose for this expanding aging population, when most of the current guidelines have no upper age limit set up.
Although reducing BC-related mortality is the ultimate goal of mammography screening, intermediate measures such as stage at diagnosis are useful to evaluate the utility of screening [14, 15]. Several studies have demonstrated the benefits of mammography screening on an important predictor of survival, stage at BC diagnosis, in elderly women. Two studies which used SEER-Medicare database reported that mammography screening decreased with advancing age at diagnosis, and elderly women who undergo regular mammography were diagnosed with an earlier stage of disease [16, 17]. However, these studies utilized the claims data from only 2 years before BC diagnosis, which failed to capture the effect of persistence with mammography screening. Also, one of these studies utilized SEER-Medicare data from only three registries which may limit the generalizability of the study findings [17]. A study which utilized 5 years claims data from entire SEER-Medicare focused only on women age 80 and above [18]. A systematic review of routine mammography screening demonstrated that regular mammography screening was associated with earlier stage and lower BC mortality, but it focused only on women over 74 years of age [19]. Hence, the studies evaluating the association between mammography screening and stage at BC diagnosis were conducted using data from either a few SEER-Medicare registries, or data for limited time period of 2 years before BC diagnosis, or among women age 80 and above. Moreover, the major limitation with all these studies is that the authors did not use any model or technique to distinguish screening from diagnostic mammograms which is one of the key issues with Medicare claims data. It is reported that challenges persist in distinguishing screening mammograms from the diagnostic ones with the Medicare claims data as many screening procedures may be billed as diagnostic procedures as the later are reimbursed at higher level [20]. The authors of a recently published study have developed and suggested a three-step algorithm with high sensitivity (99.7 %) and high positive predictive value (97.4 %) to distinguish between screening and diagnostic mammograms using Medicare data linked to a cancer registry [21]. Thus, overall there is a vital need to determine the association between persistence with mammography screening and stage at BC diagnosis among elderly women age 65 and above, which clearly distinguishes between screening and diagnostic mammograms, from entire SEER-Medicare population, with a longer follow-up time period before BC diagnosis to capture persistence with mammography screening.
Hence, the objective of the study is to determine the persistence with mammography screening in Medicare fee-for-service (FFS) women beneficiaries diagnosed with incident BC, and to determine the association between persistence with mammography screening and stage at BC diagnosis, after controlling for predisposing factors, enabling factors, need factors, healthcare use, and external healthcare environmental factors.
Methods
Study design, data source, and study cohort
This retrospective observational study utilized SEER-Medicare dataset which provides population-based information on cancer-related epidemiologic and health services research. The SEER-Medicare program collects information on newly diagnosed cancer cases from 18 population-based tumor registries which in turn collect information from several sources including hospitals, outpatient clinics, laboratories, private practitioners, laboratories, hospices, autopsy reports, and death certificates and covers approximately 26 % of the US population [22]. The details of the SEER-Medicare dataset are described elsewhere [22]. For this study, the Area Resource File (ARF) was linked to the SEER-Medicare dataset using the state and county Federal Information Processing Standards code for each beneficiary to extract the county level information on the availability of healthcare facilities.
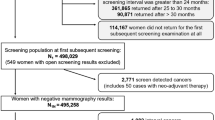
The study cohort consisted of women age 70 and above at the first primary diagnosis of incident BC between January 1, 2005 and December 31, 2009. Since mammography screening persistence during the period of five years before BC diagnosis was to be determined, women who were continuously enrolled in Medicare parts A/B for at least 60 months before BC diagnosis, and who were not enrolled in health maintenance organizations (HMO) at any time during the study period were included in the study. Women with any previous cancer diagnosis, unknown/missing BC stage information, and who were diagnosed via death certificate or autopsy were excluded from the study. BC diagnosis codes were based on the primary site and International Classification of Diseases, 9th edition (ICD-9) Clinical Modification codes 174.xx, 233.0x, 238.3x, and 239.3x. A total of 138,043 women were diagnosed with BC during 2005–2009. The following women were excluded: 68,872 women who were below 70 years at diagnosis, 3,548 women with previous cancer diagnosis, 864 women who were diagnosed with BC during death or autopsy, 1,865 women for whom BC stage information was missing or unknown, 3,865 women who were not continuously enrolled in Medicare parts A/B, and 19,023 women who were members of HMO at any time during the study follow-up period. The remaining 39,006 women were included in the study.
Measures
Dependent variable: Stage at diagnosis
SEER summary staging system which uses all the medical record information and which pools the most accurate clinical and pathological documentation of the extent of disease was used to determine the stage at BC diagnosis [23]. It was categorized as in situ, local, regional, and distant stages.
Key independent variable: Persistence with mammography screening
There is ambiguity regarding the ability of Medicare claims data to distinguish screening from diagnostic mammograms. Appropriately distinguishing screening mammograms from diagnostic mammograms is very crucial when assessing screening utilization using claims-based database [24]. A recently published three-step algorithm with high sensitivity (99.7 %) and high positive predictive value (97.4 %) of a screening designation was utilized to classify the claims for screening mammograms from those of the diagnostic mammograms [21]. The sequential steps to identify the screening mammograms from the Medicare claims are described elsewhere [21]. Based on the number of screening mammograms a woman had in five years prior to BC diagnosis, the study cohort was categorized as non-users (no screening mammograms), non-persistent users (with 1–2 screening mammograms), and persistent users (with three or more screening mammograms). Also, elderly women have similar risk of advanced stage of BC with either biennial or annual mammography screening [25]. Hence, persistent users represented a population who have had annual to biennial mammography screening before BC diagnosis.
Other independent variables
For this study, Andersen behavioral model for healthcare services utilization was used [26, 27]. Based on this model, the independent variables were grouped into predisposing factors, enabling factors, need-related factors, factors associated with healthcare use, and external healthcare environmental factors.
Predisposing factors included age at BC diagnosis (70–74, 75–79, 80+), race (white, black, other), while enabling factors included marital status (married/partnered; single/divorced/widowed), census tract median annual household income (≤$25,000; $25,001–50,000; $50,001–75,000; >$75,000), and census tract percentage of people age ≥25 years with at least four years of college education divided into four quartiles based on the median value (0–13.29, 13.30–22.83, 22.84–38.55, ≥38.56). Need-related factor included co-occurring chronic conditions which were identified from Medicare files using the ICD-9 diagnosis codes. Comorbidity scores were calculated using Charlson comorbidity index [28–30] and were categorized as 0 (no comorbidity), 1, and 2+. Healthcare use factors included number of primary care physicians (PCP) visits in 5 years prior to BC diagnosis derived from National Claims History file using the Medicare provider specialty field [31], and were categorized into four quartiles based on its median value (0–10, 11–21, 22–34, ≥35). External healthcare environmental factors included location of residence (metro, non-metro), SEER regions (Northeast, South, North Central, West), and the number of hospitals with BC screening/mammography services in the area of residence for each woman derived from ARF file, categorized into four quartiles based on its median value (0–1, 2–3, 4–7, ≥8).
Statistical analyses
Chi-square statistics were used to determine significant differences between persistence with mammography screening categories across all the independent variables. Multinomial logistic regression was performed to determine the association between persistence with mammography screening and early stages of disease, after controlling for predisposing factors, enabling factors, need-related factor, healthcare use, and external healthcare environmental factors. To control for selection bias, the post-hoc sub-group analysis was also conducted to determine significant differences on stage at diagnosis between persistent and non-persistent users. In both the regressions, “distant stage” was used as the reference group for the dependent variable. The parameter estimates were transformed to odds ratios and their corresponding 95 % confidence intervals (CI) were examined and the findings that were significant with p values≤0.05 levels are discussed. All analyses were conducted within statistical analysis systems software SAS 9.4 (SAS® version 9.4, SAS Institute Inc., Cary, NC, USA).
Results
The left column of Table 1 describes the study cohort of 39,006 women age 70 years and older, diagnosed with first primary incident BC in 2005–2009. Overwhelming 56 % of elderly women were diagnosed with local stage BC followed by 23 % with regional stage and 15 % at an in situ stage. Only 6 % women were diagnosed at distant stage BC. Forty percent of the study cohort was age 80 and above, while 31 % were in the age group 70–74 years. A majority of the study cohort was white (88 %), single or divorced or widowed (61 %), had census tract income of $50,000 or less (57 %), resided in metro areas (83 %), and had no co-occurring chronic condition (53 %).
The right end columns of Table 1 describe the group differences in persistence with mammography screening by stage at BC diagnosis and all the independent variables. Approximately 46 % of women were persistent with mammography screening, while 26 % were not persistent with mammography screening and 28 % did not have any screening mammogram in five years prior to BC diagnosis. In the bivariate analyses, all the subgroups were significant in Chi-square analyses, at the 0.05 % level. Women with BC who were persistent with mammography screening were age 70–74 years, white, married, or partnered, with 11–34 PCP visits, residing in areas with higher proportion of individuals with at least 4 years of college education and with household income >$75,000, resided in West region and with no co-occurring chronic conditions.
Figure 1 describes disease stage by persistence with mammography screening. Among women who had no mammography screening, 45 % were diagnosed with BC at local stage, 35 % were diagnosed with regional stage, 16 % were diagnosed at distant stage, and only 4 % were diagnosed at an in situ stage. Among women who were not persistent with mammography screening, 60 % were diagnosed with local stage, 22 % were diagnosed at regional stage, 3 % were diagnosed at distant stage, and 15 % were diagnosed at an in situ stage. However, among women who were persistent with mammography screening, only 15 and 1 % were diagnosed at regional and distant stages, respectively, while 62 % were diagnosed at local stage and 22 % were diagnosed at an in situ stage.
Table 2 describes the results from the multinomial logistic regression. After controlling for all the factors, women who were persistent with mammography screening were 3.28 times more likely to be diagnosed at an in situ stage (Adjusted odds ratio (AOR) = 3.28, 95 % confidence interval (CI) = 2.75–3.91), 2.37 times more likely to be diagnosed at the local stage (AOR = 2.37, 95 % CI = 2.00–2.81), and two times more likely to be diagnosed at the regional stage (AOR = 1.60, 95 % CI = 1.35–1.91) as compared to those who were not persistent with mammography screening. Women who did not have any screening mammogram in the five years before BC diagnosis were 93 % less likely to be diagnosed at an in situ stage (AOR = 0.07, 95 % CI = 0.06–0.08), 83 % less likely to be diagnosed at the local stage (AOR = 0.17, 95 % CI = 0.15–0.19), and 63 % less likely to be diagnosed at the regional stage (AOR = 0.37, 95 % CI = 0.33–0.42) as compared to those who were not persistent with mammography screening. Women who were age 80 and above were 21 % less likely to be diagnosed at an in situ stage (AOR = 0.79, 95 % CI = 0.69–0.90) as compared to those in the age group 70–74 years. African–American women were significantly less likely to be diagnosed at local and regional stages of BC as compared to white women. However, women belonging to the ‘other’ race/ethnicity were significantly more likely to be diagnosed at in situ (AOR = 1.84) and local (AOR = 1.47) stages of BC as compared to white women. Also, women who were married or partnered were highly likely to be diagnosed at earlier stages of BC as compared to those who were single or divorced. The AORs were 1.21 for in situ stage, 1.26 for local stage, and 1.21 for regional stage of BC. Also women with census tract income >$75,000 had higher likelihood of being diagnosed at in situ (AOR = 1.49, 95 % CI = 1.11–2.01) and local (AOR = 1.42, 95 % CI = 1.10–1.84) stages of BC, as compared to those with income of $25,000 or less. In addition, women who resided in geographic area with higher percentage of people with at least some college education demonstrated higher amounts of early stages of disease. Women who had at least 11 PCP visits were significantly more likely to be diagnosed at in situ, local, and regional stages of BC as compared to those with visits in the first quartile. The AORs ranged from 1.43 to 1.71. Women who resided in North East and North Central SEER-Medicare regions were significantly less likely to be diagnosed at local and regional stages of BC as compared to those who resided in the West SEER-Medicare region.
Table 3 describes the results from the sub-group analysis among users of mammography screening. As compared to women who were not persistent with mammography screening, women who were persistent with mammography screening were significantly more likely to be diagnosed at earlier stages of BC. The AORs were 3.21 (95 % CI = 2.69–3.83) for in situ stage, 2.32 (95 % CI = 1.96–2.75) for local stage, and 1.56 (95 % CI = 1.31–1.86) for regional stage of BC. To evaluate the effect of overdiagnosis, another regression was performed that excluded women with an in situ stage. There were no changes in the directions and significance of the study findings even after adjusting for overdiagnosis (data not shown).
Discussion
As per the literature to date, this is the first study which evaluated the association between persistence with mammography screening and stage at BC diagnosis among elderly women from the SEER-Medicare data after appropriately identifying screening mammograms using an algorithm with high sensitivity and positive predictive value. This study found significant associations between persistence with mammography screening and earlier stages of BC. The study findings highlight the beneficial effects of regular mammography screening on stage of breast tumor in elderly women age 70 and above. These results are consistent with the previous studies which reported that regular mammography screening or having had a mammography screening in one to two years before BC diagnosis was associated with earlier disease stage representation [16–19]. However, rates of persistence with mammography screening in the elderly women are low. Less than half of the elderly women diagnosed with BC were persistent to mammography screening, while 26 % were not persistent with mammography screening in five years prior to their BC diagnosis. One of the striking findings of the study was that a significant proportion of elderly women (28 %) did not have a single screening mammogram in the five years prior to their BC diagnosis even though these women are more likely to be diagnosed with larger tumor sizes at more advanced stages [2]. Thus, increasing awareness among both PCP and elderly women about the importance of mammography screening in this elderly group for whom there are contrasting guidelines, may help improve persistence with mammography screening.
Among predisposing factors, older age of 80 and above and being African American resulted in a lower likelihood of being diagnosed at an in situ, local, or regional stages, which were consistent with previous studies [18, 32–34]. This implies that persistence with mammography screening did not eliminate the differences in stage representation between African American and white women and there may other factors such as family history, genetic composition, and other lifestyle factors, and quality of breast cancer care [35, 36] contributing to these disparities. However, women belonging to ‘other’ race/ethnicity were significantly more likely to be diagnosed with earlier stages after controlling for all the factors in contrast to the results of the previous studies [18, 32]. This suggests that women belonging to ‘other’ races may have protective factors such as individual characteristics, behavioral factors, biological characteristics, and lack of family history of BC which may be protecting them from being diagnosed at distant stages.
A major strength of this study is the utilization of the recently published algorithm with a high sensitivity and positive predictive value for identifying screening mammograms in the Medicare claims files [21]. Distinguishing screening from diagnostic mammograms when evaluating screening utilization from claims-based data has been reported as a major limitation by several previous studies [16–19]. The results of the study also aids in understanding the benefits of persistence with mammography screening for elderly women for whom there are no clear recommended guidelines for mammography screening. The study utilized the very recent (2005–2009) SEER-Medicare data to provide recent estimates and also utilized a comprehensive list of the covariates in the analyses to minimize any confounding.
There are several limitations worth stating when interpreting the results of this study. Some women of the study may have been recipients of free mammograms which will not be captured in the Medicare data. However, this may not be considered a major limitation as Medicare is the primary health insurer for the older adult population. Certain variables such as annual household income, education level, and access to total of BC screening centers at patient level are not available and hence census tract information for these variables were utilized [37]. Lastly, the SEER-Medicare data tend to include more urban and affluent individuals and fewer white individuals as compared to the US population [22]. Regardless of these limitations, SEER-Medicare database provides data on large US population which is utilized in studying important issues related to screening in the older population. Also, the findings of the study are generalizable only to elderly women age 70 and above.
In conclusion, a lower proportion of elderly women with BC was persistent with mammography screening and it was significantly associated with earlier stages of BC, thereby supporting the use of regular mammography in these women. Interventions and targeted strategies to promote persistence with mammography screening among elderly women are warranted.
Abbreviations
- BC:
-
Breast cancer
- US:
-
United States
- SEER:
-
Surveillance, epidemiology, and end results
- FFS:
-
Fee-for-service
- ARF:
-
Area resource file
- ICD-9:
-
International classification of diseases 9th edition
- PCP:
-
Primary care physicians
- AOR:
-
Adjusted odds ratio
- CI:
-
Confidence interval
References
Howlader N, Noone A, Krapcho M, et al (2012) SEER cancer statistics review, 1975–2009 (Vintage 2009 Populations), National Cancer Institute. Bethesda, MD. Based on November 2011 SEER data submission http://seer.cancer.gov/csr/1975_2009_pops09/. Accessed 15 Aug 2014
Hillner BE, Penberthy L, Desch CE, McDonald MK, Smith TJ, Retchin SM (1996) Variation in staging and treatment of local and regional breast cancer in the elderly. Breast Cancer Res Treat 40(1):75–86
Fletcher SW, Elmore JG (2003) Clinical practice. Mammographic screening for breast cancer. N Engl J Med 348(17):1672–1680
Nystrom L, Andersson I, Bjurstam N, Frisell J, Nordenskjold B, Rutqvist LE (2002) Long-term effects of mammography screening: updated overview of the Swedish randomised trials. Lancet 359(9310):909–919
Smith-Bindman R, Kerlikowske K, Gebretsadik T, Newman J (2000) Is screening mammography effective in elderly women? Am J Med 108(2):112–119
Tabar L, Dean PB (2003) Mammography and breast cancer: the new era. Int J Gynaecol Obstet 82(3):319–326
Hellquist BN, Duffy SW, Abdsaleh S, Bjorneld L, Bordas P, Tabar L et al (2011) Effectiveness of population-based service screening with mammography for women ages 40–49 years: evaluation of the Swedish mammography screening in young women (SCRY) cohort. Cancer 117(4):714–722
Walter LC, Covinsky KE (2001) Cancer screening in elderly patients: a framework for individualized decision making. JAMA 285(21):2750–2756
Caplan LS, Haynes SG (1996) Breast cancer screening in older women. Public Health Rev 24(2):193–204
Use of mammography services by women aged ≥65 years enrolled in Medicare-united states, 1991–1993 (1995) MMWR Morb Mortal Wkly Report; Report No. 44;777–781
American Cancer Society (2013) Breast cancer facts and figures 2013–2014. Atlanta, GA http://www.cancer.org/acs/groups/content/@research/documents/document/acspc-040951.pdf. Accessed 15 Aug 2014
US Preventive Services Task Force (2009) Screening for breast cancer: US preventive services task force recommendation statement. Ann Intern Med 151(10):716–726, W-236
Smith RA, Manassaram-Baptiste D, Brooks D, Cokkinides V, Doroshenk M, Saslow D et al (2014) Cancer screening in the United States, 2014: a review of current American Cancer Society guidelines and current issues in cancer screening. CA Cancer J Clin 64(1):30–51
Day NE (1989) Quantitative approaches to the evaluation of screening programs. World J Surg 13(1):3–8
Sant M, Allemani C, Capocaccia R, Hakulinen T, Aareleid T, Coebergh JW et al (2003) Stage at diagnosis is a key explanation of differences in breast cancer survival across Europe. Int J Cancer 106(3):416–422
Randolph WM, Goodwin JS, Mahnken JD, Freeman JL (2002) Regular mammography use is associated with elimination of age-related disparities in size and stage of breast cancer at diagnosis. Ann Intern Med 137(10):783–790
McCarthy EP, Burns RB, Freund KM, Ash AS, Shwartz M, Marwill SL et al (2000) Mammography use, breast cancer stage at diagnosis, and survival among older women. J Am Geriatr Soc 48(10):1226–1233
Badgwell BD, Giordano SH, Duan ZZ, Fang S, Bedrosian I, Kuerer HM et al (2008) Mammography before diagnosis among women age 80 years and older with breast cancer. J Clin Oncol 26(15):2482–2488
Galit W, Green MS, Lital KB (2007) Routine screening mammography in women older than 74 years: a review of the available data. Maturitas 57(2):109–119
Freeman JL, Klabunde CN, Schussler N, Warren JL, Virnig BA, Cooper GS (2002) Measuring breast, colorectal, and prostate cancer screening with Medicare claims data. Med Care 40(8 Suppl):IV, 36–42
Fenton JJ, Zhu W, Balch S, Smith-Bindman R, Fishman P, Hubbard RA (2014) Distinguishing screening from diagnostic mammograms using Medicare claims data. Med Care 52(7):e44–e51
Warren JL, Klabunde CN, Schrag D, Bach PB, Riley GF (2002) Overview of the SEER-Medicare data: content, research applications, and generalizability to the United States elderly population. Med Care 40(8 Suppl):IV,3–18
Young JL Jr, Roffers SD, Ries LAG, Fritz AG, Hurlbut AA (2001) SEER summary staging manual-2000: Codes and coding instructions, National Cancer Institute, NIH Pub. No. 01-4969, Bethasda
Randolph WM, Mahnken JD, Goodwin JS, Freeman JL (2002) Using medicare data to estimate the prevalence of breast cancer screening in older women: comparison of different methods to identify screening mammograms. Health Serv Res 37(6):1643–1657
Braithwaite D, Zhu W, Hubbard RA, O’Meara ES, Miglioretti DL, Geller B et al (2013) Screening outcomes in older US women undergoing multiple mammograms in community practice: does interval, age, or comorbidity score affect tumor characteristics or false positive rates? J Natl Cancer Inst 105(5):334–341
Andersen RM (1995) Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav 36(1):1–10
Andersen R, Newman JF (1973) Societal and individual determinants of medical care utilization in the United States. Milbank Mem Fund Q Health Soc 51(1):95–124
Klabunde CN, Potosky AL, Legler JM, Warren JL (2000) Development of a comorbidity index using physician claims data. J Clin Epidemiol 53(12):1258–1267
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40(5):373–383
National cancer institute (2013) SEER-Medicare: Calculation of comorbidity weights. http://healthservices.cancer.gov/seermedicare/program/comorbidity.html. Accessed 15 Aug 2014
Yu X, McBean AM, Virnig BA (2007) Physician visits, patient comorbidities, and mammography use among elderly colorectal cancer survivors. J Cancer Surviv 1(4):275–282
McCarthy EP, Burns RB, Coughlin SS, Freund KM, Rice J, Marwill SL et al (1998) Mammography use helps to explain differences in breast cancer stage at diagnosis between older black and white women. Ann Intern Med 128(9):729–736
Li CI, Malone KE, Daling JR (2003) Differences in breast cancer stage, treatment, and survival by race and ethnicity. Arch Intern Med 163(1):49–56
Jacobellis J, Cutter G (2002) Mammography screening and differences in stage of disease by race/ethnicity. Am J Public Health 92(7):1144–1150
Smedley B, Stith A, Nelson A (2002) Unequal treatment-confronting racial and ethnic disparities in health care. Institute of Medicine, National Academy Press, Washington, DC
McDougall JA, Li CI (2010) Trends in distant-stage breast, colorectal, and prostate cancer incidence rates from 1992 to 2004: potential influences of screening and hormonal factors. Horm Cancer 1(1):55–62
Krieger N (1992) Overcoming the absence of socioeconomic data in medical records: validation and application of a census-based methodology. Am J Public Health 82(5):703–710
Acknowledgments
This project was supported by AHRQ Grant (R24HS018622-03) and National Institute of General Medicine Sciences Grant (U54GM104942). The content is solely the responsibility of the authors and does not necessarily represent the official views of AHRQ and NIH.
Disclosures
No conflict of interest and no disclosures.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Vyas, A., Madhavan, S. & Sambamoorthi, U. Association between persistence with mammography screening and stage at diagnosis among elderly women diagnosed with breast cancer. Breast Cancer Res Treat 148, 645–654 (2014). https://doi.org/10.1007/s10549-014-3204-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-014-3204-3