Abstract
Impaired activity of galactose-1-phosphate uridyltransferase (GALT) causes galactosemia, an autosomal recessive disorder of galactose metabolism. Early initiation of a galactose-restricted diet can prevent or resolve neonatal complications. Despite therapy, patients often experience long-term complications including speech impairment, learning disabilities, and premature ovarian insufficiency in females. This study evaluates clinical outcomes in 34 galactosemia patients with markedly reduced GALT activity and compares outcomes between patients with different levels of mean galactose-1-phosphate in red blood cells (GAL1P) using logistic regression: group 1 (n = 13) GAL1P ≤1.7 mg/dL vs. group 2 (n = 21) GAL1P ≥ 2 mg/dL. Acute symptoms at birth were comparable between groups (p = 0.30) with approximately 50% of patients presenting with jaundice, liver failure, and failure-to-thrive. However, group 2 patients had significantly higher prevalence of negative long-term outcomes compared to group 1 patients (p = 0.01). Only one of 11 patients >3 yo in group 1 developed neurological and severe behavioral problems of unclear etiology. In contrast, 17 of 20 patients >3 yo in group 2 presented with one or more long-term complications associated with galactosemia. The majority of females ≥15 yo in this group also had impaired ovarian function with markedly reduced levels of anti-Müllerian hormone. These findings suggest that galactosemia patients with higher GAL1P levels are more likely to have negative long-term outcome. Therefore, evaluation of GAL1P levels on a galactose-restricted diet might be helpful in providing a prognosis for galactosemia patients with rare or novel genotypes whose clinical presentations are not well known.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Galactose-1-phosphate uridyltransferase (GALT) catalyzes the conversion of galactose-1-phosphate (GAL1P) and UDP-glucose to glucose-1-phosphate and UPD-galactose in the Leloir pathway (Holden et al. 2003). The enzyme is encoded by the GALT gene located on 9q13.3 and composed of 11 exons (Shih et al. 1984). Impaired activity of this enzyme causes galactosemia, an autosomal recessive disorder of galactose metabolism (OMIM#230400). More than 300 variants in the GALT gene have been identified in patients with galactosemia (ARUP galactosemia database: http://arup.utah.edu/database/GALT/GALT_welcome.php) and cause different degrees of enzyme activity impairment (Tyfield et al. 1999; Tyfield 2000). The most common pathogenic variants found in Caucasians are p.Q188R, p.K285N, and p.L195P (Elsas and Lai 1998; Tyfield et al. 1999; Berry 2014) while p.S135L or IVS2-2G are more frequent in individuals of African or Hispanic descent, respectively (Lai et al. 1996; Yang et al. 2002). A large 5.2 kb deletion has been reported in Ashkenazi Jews (Coffee et al. 2006; Goldstein et al. 2011). These homozygous or compound heterozygous genetic changes are associated with undetectable or markedly reduced GALT activity in red blood cells (RBC).
Classic galactosemia, characterized by markedly reduced GALT activity, leads to multiple neonatal and long-term complications (Berry 2014; Coelho et al. 2017). Galactosemia patients can present in the newborn period with jaundice, vomiting, failure to thrive, and diarrhea. These acute symptoms may be complicated by Gram-negative sepsis, progression to liver failure, septic shock, and even death if patients are left untreated. A galactose-restricted diet can prevent or resolve neonatal complications. However, even with therapy there can be long-term complications, such as cognitive and language impairments, developmental delays, and learning disabilities (Gitzelmann and Steinmann 1984; Waggoner et al. 1990; Schweitzer et al. 1993; Schweitzer-Krantz 2003). The majority of females with classic galactosemia also develop premature ovarian insufficiency (POI) (Berry 2014), and low concentrations of anti-Müllerian hormone (AMH), a cycle-independent marker of ovarian reserve, have been reported in these patients (Sanders et al. 2009; Fridovich-Keil et al. 2011; Spencer et al. 2013).
Several mechanisms have been implicated in the pathogenesis of galactosemia. It has been suggested that the accumulation of toxic metabolites, galactose, galactitol, and GAL1P could cause permanent damage to various tissues and organs in the prenatal and the postnatal periods (Chen et al. 1981; Bandyopadhyay et al. 2003; Lai et al. 2009; Coelho et al. 2017). The impact of abnormal glycosylation on the physiological function of different glycoproteins and glycolipids has been considered a contributing factor to galactosemia complications (Liu et al. 2012; Coss et al. 2014a, b). Recent in vitro and in vivo studies have also demonstrated the increase in oxidative stress and downregulation of PI3K/Akt pathway in response to the impaired GALT function (Jumbo-Lucioni et al. 2013; Balakrishnan et al. 2016), although the understanding of the complex interplay between these different mechanisms is still limited (Viggiano et al. 2017).
Genotype-phenotype correlations in galactosemia have been the subject of many studies in the past 30 years. Residual GALT activity is usually associated with milder clinical outcomes (Berry and Elsas 2011), with patients homozygous for p.S135L escaping many of the long-term complications of the disease (Lai et al. 1996; Elsas and Lai 1998). Patients carrying GALT alleles associated with <1% of normal enzymatic activity had higher incidence of long-term complications, such as ovarian dysfunction and learning deficits, compared to those with alleles retaining >1% WT activities (Ryan et al. 2013; Spencer et al. 2013). In addition, the risk of verbal dyspraxia has been associated with the rate of galactose oxidation to CO2 (the “breath test”) and mean GAL1P concentrations (Robertson et al. 2000; Webb et al. 2003). However, other studies found no correlation between biochemical phenotype and long-term outcomes in classic galactosemia patients (Waggoner et al. 1990; Walter et al. 1999; Shield et al. 2000; Schweitzer-Krantz 2003; Hughes et al. 2009).
This study presents an analysis of clinical, molecular, and biochemical data from 34 galactosemia patients with markedly reduced or undetectable GALT activity in RBC. The incidence of neonatal and long-term outcomes in these patients was evaluated and compared between patients with low and high concentrations of GAL1P. The results suggest an association between levels of GAL1P in red blood cells and long-term complications.
Methods
Subjects
All patients (16 females, 18 males) included in this study were diagnosed with galactosemia following an abnormal newborn screen result, and were followed at the Metabolic Clinic of the University of Utah and/or at outreach clinics. In this study, patients were divided into two groups based on their GAL1P levels obtained at ≥6 months of age with the exception of very young patients 3F and 6M, whose levels were obtained between 3 and 6 months of age. The mean GAL1P in group 1 and group 2 were ≤1.7 mg/dL (n = 13) and ≥2 mg/dL (n = 21), respectively (Fig. 1b and c). Patients 3F and 20F had only one GAL1P measurement; therefore, mean GAL1P was not calculated in these patients.
Concentrations of red blood cells galactose-1-phosphate in galactosemia patients. (a) GAL1P in all patients from birth to adulthood, (b) and (c) GAL1P in individual patients, ≥6 mo. The levels in patients 3F and 6M were obtained between 3 and 6 months of age. The white (group 1) and dark gray (group 2) boxes represent the first and the third quartiles of GAL1P range with whiskers defining min and max values. Total number of GAL1P measurements is shown above each box. Normal range (≤1 mg/dL) is shown as a light gray area, and dashed line represents the recommended GAL1P range on dietary treatment, <4 mg/dL
Clinical outcomes were compared between these two groups of patients. Symptoms at diagnosis included jaundice, liver failure, cataracts, sepsis, vomiting, and failure-to-thrive. Long-term outcomes included abnormal motor function, speech deficits, learning deficits, intellectual disability, developmental delays, neurologic deficits, premature ovarian insufficiency, and menstrual irregularities. Speech deficits and learning disabilities were assessed in all patients >3 yo. Reproductive function was evaluated in female patients ≥15 yo. To evaluate the growth of our patients, the Z-scores of the heights (or length in patients <2 yo), weight and BMI (or weight-to-length in patients <2 yo) for age were calculated using WHO growth charts for patients <2 years and CDC growth charts for patients ≥2 years. The patients’ socioeconomic status was not formally assessed in this study. This study was reviewed and approved by the Institutional Review Board at the University of Utah.
Standard treatment for all patients was the administration of lactose-free formula (soy-based or elemental) from the moment the diagnosis was suspected. Galactose-restriction is maintained for life, primarily restricting dairy products and fermented soy products with the exception of some aged cheeses. Fruits, vegetables, and legumes are no longer restricted based on new guidelines in recent years (Van Calcar et al. 2014). However, prior to these guidelines, patients were advised to restrict certain fruits, vegetables, and legumes with high concentrations of galactose. Our clinic allowed some diet liberalization in childhood, including introduction of tomatoes, their derivatives, legumes, and aged cheeses.
Patients with galactosemia are typically seen in the Metabolic Clinic every 3 months until 1 year of age, every 6 months between 1 and 3 years of age, and yearly thereafter. Laboratory testing depends on clinical status and can include red blood cells GAL1P, vitamin D, and liver function tests. Follicle-stimulating hormone (FSH), luteinizing hormone (LH), estradiol and, more recently, anti-Müllerian hormone are usually measured in female patients to evaluate their reproductive function. All female patients with abnormal ovarian function are referred to Obstetrics and Gynecology for hormone replacement therapy (HRT).
Biochemical and molecular testing
The GALT activity and galactose-1-phosphate in the majority of patients’ samples was measured at ARUP Laboratories (Salt Lake City, UT) using a spectrophotometric assay (Tietz 1995) and GC-MS/MS (Chen et al. 2002), respectively. The biochemical testing was also performed at Emory Genetic Laboratory (Atlanta, GA), Children’s Hospital of Philadelphia (Philadelphia, PA), Mayo Medical laboratories (Rochester, MN) and University Children’s Genetic Laboratory (Los Angeles, CA). All laboratories reported similar reference ranges for the enzyme activity and galactose-1-phosphate in red blood cells.
The levels of FSH, LH, estradiol, and AMH in galactosemia females were measured at ARUP Laboratories (Salt Lake City, UT) and LabCorp (Burlington, NC). DNA testing by targeted gene analysis or full gene sequencing was performed at ARUP laboratories (Salt Lake City, UT) or Emory Genetics laboratory (Atlanta, GA). All laboratory testing was performed according to standard procedures.
Statistical analysis
Data were summarized using descriptive statistics: mean and standard deviations for continuous variables and frequencies for dichotomous variables. Differences between groups were analyzed using Wilcoxon rank-sum tests for continuous variable and Fisher’s exact test or Kruskal-Wallis test for categorical variables. Logistic regression was used to predict the presence of one or more long-term clinical complications using mean Gal1P levels for each patient as a continuous variable after adjusting for age. Statistical analyses were conducted using Stata/IC 14.0. Significance was defined as a two-sided p value with alpha of 0.01 to account for multiple comparisons and reduce the risk of type I error.
A sample size of 32 (patients 3F and 6M excluded) with an allocation ratio of 1.9 between group 1 and group 2 was adequate to produce 80% power to detect a mean difference in the proportion of galactosemia patients with a negative long-term outcome of 0.55 (conservative estimation based on (Schweitzer et al. 1993; Jumbo-Lucioni et al. 2012; Frederick et al. 2017) with an alpha of 0.01 in a two-sided analysis.
Results
Biochemical findings
The majority of patients in this study had undetectable GALT activity in red blood cells, and 12 patients had markedly reduced GALT activity ranging from 0.2 to 1.7 μmol hr−1 g Hb−1 (Table 1). It is unclear if these non-zero values represent true residual activities or they reflect analytical limitations of the spectrometric method in measuring low enzymatic activity (Li et al. 2010, 2011). The repeat analysis of GALT activities by LC-MS/MS (Li et al. 2010, 2011) in four patients showed undetectable activity of the enzyme (values in parentheses in Table 1).
The measurements of red blood cell GAL1P were routinely performed at the clinic visits (see Methods). The highest GAL1P concentrations were observed at the time of diagnosis, and the levels stabilized after 4–6 months of galactose restriction (Fig. 1A) (Hutchesson et al. 1999; Walter et al. 1999). Overall, the intra-individual variability of GAL1P measurements in patients with abnormal GAL1P findings was <25% (Fig. 1b and c) suggesting a strong effect of the genotype and relative consistency in dietary galactose consumption. Significantly higher GAL1P levels were recorded on one occasion in patients 17M and 23F, probably reflecting higher than usual galactose intake (Fig. 1b and c). Based on GAL1P levels on dietary treatment patients were divided into two groups: group 1 with mean GAL1P <2-fold of the upper normal range (patients 1F-13M, mean GAL1P 0.3–1.7 mg/dL, n = 13) and group 2 with mean GAL1P ≥2-fold of the upper normal range (patients 14M-34F, mean GAL1P 2.0–4.9 mg/dL, n = 21) to compare biochemical, molecular and clinical findings (Tables 1 and 2).
Molecular findings
The most common pathogenic variant in the GALT gene in our cohort of patients was p.Q188R with 47.1% allele frequency: eight patients were homozygous and 13 patients were compound heterozygous for p.Q188R (Table 1). The frequencies of other common alleles, such as p.K285N, p.L195P, p.S135L, p.T138M, and p.D98N, were 2.9% each, while other variants were unique to individual families. Twelve variants were missense, two nonsense (p.W249X and p.Q212X), and one affected splicing (IVS2-2G). All 15 variants were previously reported in literature (Walter et al. 1999; Yang et al. 2002; Calderon et al. 2007; Tang et al. 2012). The results of molecular testing were not available for six patients (Table 1). In addition, targeted DNA analysis for the nine most common variants (Calderon et al. 2007; Jama et al. 2007) did not identify a second pathogenic allele in the GALT gene of four other patients (10M, 13M, 20F, and 21F).
The majority of patients in group 2 were homozygous or compound heterozygous for p.Q188R and other severe pathogenic variants, such as p.K285N and p.L195P (Tyfield et al. 1999). Interestingly, none of the group 1 patients who received genetic testing had Q188R/Q188R, Q188R/K285N or Q188R/L195P genotypes (Table 1) (Berry 2014). Instead, they carried variants characterized by residual activity in model organisms, such as p.D98N, p.T138M, p.R223S, p.I278N, and p.R201H (Riehman et al. 2001; Tang et al. 2012; Spencer et al. 2013), suggesting a correlation between accumulation of GAL1P and genotype.
Nutrition and growth
A galactose-restricted diet was initiated in all patients in the first weeks of life and, in general, all patients except 10M followed a galactose-restricted diet (Fig. 1b and c, Table 1). Despite consistent dietary recommendations for patients in group 1 and group 2 (see methods), growth deficiencies were more frequently observed in group 2 patients. Six out of 21 patients (29%) with mean GAL1P ≥2 mg/dL (group 2) were underweight (Z-score < −2), and four of them also had short stature (Z-scores < −2). In contrast, only one of 13 patients (patient 10M) with mean GAL1P levels ≤1.7 mg/dL (group 1) had Z-scores <2 SD below the 50th percentile for height and BMI (Fig. 2). Z-scores for weight were significantly lower in galactosemia patients in group 2 vs group 1 (p = 0.045; Fig. 2). Patient heights were not corrected for the mid-parental target heights, and unequal distribution of very tall or very short families in group 1 and group 2 could potentially influence the results.
Growth in galactosemia patients. Z-scores for (a) weight, (b) height or length (for patients <2yo), and (c) BMI or WL (weight to length, for patients <2 yo) were calculated using WHO growth charts for patients <2 years and CDC growth charts for patients ≥2 years. Left panels show the average of the three most recent Z-scores for individual patients aligned with the age of the latest measurement. Right panels demonstrate the range of the average Z-scores in group 1 (in white) vs group 2 (in gray) patients. Fisher’s exact test was used to evaluate the differences in Z-scores between group 1 and 2
Clinical findings
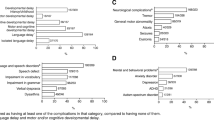
The clinical findings in our galactosemia patients are summarized in Fig. 3, Tables 1 and 2. Long-term outcomes were not assessed for patients 3F and 6M due to very young age. In 27 out of 34 patients, galactose restricted diet was initiated within the first ten days of life. Dietary treatment in three patients in group 1 (4M, 5M, and 7F) and four patients in group 2 (18M, 27F, 33F, and 34F) started between 11 and 21 days of life. Approximately half of the patients presented at birth with neonatal complications, such as jaundice, liver failure, vomiting, and failure to thrive. The acute symptoms resolved shortly after starting a galactose-free diet. These early manifestations were observed with similar frequencies among the two groups, 46% in group 1 and 52% in group 2 (p = 0.30, Table 2). The presence of long-term complications did not correlate with participant sex and GALT activity in RBC (Table 2). The comparison of the long-term outcomes in early treated (≤ 10 days of age) vs late treated (11–21 days of age) infants also did not demonstrate any significant effect (p = 1.0). However, higher mean GAL1P levels were associated with a 2.53-fold increase in the odds of having one or more long-term complications associated with galactosemia after controlling for age (95% CI 1.24–5.16, p = 0.010). Only patient 10M among 11 patients >3 yo in group 1 had neurological and severe behavioral problems of unclear etiology (Table 1). In contrast, 17 out of 20 patients >3 yo in group 2 (85%) presented with one or more negative outcomes (Tables 1 and 2). Speech impairment and learning disabilities were the most frequent galactosemia-related complications observed in group 2 for both males and females (Table 2). The difference in the prevalence of speech deficits between group 1 and group 2 was statistically significant (p < 0.01).
Clinical findings in 34 galactosemia patients. Patients are presented in order of mean GAL1P increase. Vertical dashed lines mark individual patients. “r” reproductive function was not evaluated in females <15 yo; “S” speech deficits and learning disabilities were not evaluated in patients <3 yo. Abbreviations: LF– liver failure; J– jaundice; HM– hepatomegaly; DD– developmental delays; LD– learning deficits; AMF– abnormal motor function; SD– speech deficits; POI– premature ovarian insufficiency; MI– menstrual irregularities
The number of galactosemia females ≥15 yo was too small for the comparison of reproductive outcomes between group 1 and group 2 patients. However, six out of nine females ≥15 yo in group 2 experienced menstrual cycle irregularities and four of them were later diagnosed with premature ovarian insufficiency (Table 1, Fig. 3). These patients demonstrated elevated levels of follicle-stimulating hormone and luteinizing hormone in combination with low estradiol consistent with their poor ovarian outcomes (Fig. 4). Notably, patients 20F and 27F, both presenting with multiple galactosemia-related complications, had successful spontaneous pregnancies (Table 1, Fig. 3). Interestingly, several FSH, LH, and estradiol measurements in patient 27F taken before pregnancy were in the postmenopausal range (Fig. 4) demonstrating limited utility of the measurement of these hormones for fertility assessment (Committee on Gynecologic Practice 2015).
Five patients ≥15 yo in group 2 had persistently low AMH, a cycle-independent marker of ovarian reserve, suggesting decreased ovarian function (Fig.4). AMH levels were also evaluated in three very young pre-pubescent patients, 7F, 15F and 34F, and the results showed markedly reduced AMH levels in patients 15F and 34F (group 2) and normal AMH in patient 7F (group 1). Patient 34F was only 6 months of age when the first AMH measurement was taken (Fig. 4) and a prolonged longitudinal assessment of ovarian function is necessary to define the prognostic value of early AMH measurements.
Discussion
In this study we present clinical, molecular, and biochemical findings from 34 classic galactosemia patients. All patients were identified by newborn screening and started on galactose-free formula in the first weeks of life. Despite early diagnosis and dietary treatment, the majority of our patients developed one or more long-term complications, including speech deficits and mild to moderate learning disabilities (Tables 1 and 2), as reported by many other investigators (Waggoner et al. 1990; Schweitzer et al. 1993; Waisbren et al. 2012). Interestingly, approximately one third of our patients with markedly reduced or undetectable red blood cell GALT activity have not developed long-term compilations associated with galactosemia (Table 1), which prompted further investigation into differences in biochemical and molecular findings between galactosemia patients with normal long-term outcomes vs negative long-term outcomes.
The measurement of GALT activity in patients’ red blood cells was not sufficient to predict the severity of clinical phenotype, as previously reported (Viggiano et al. 2015). Enzymatic testing is also method-dependent (Li et al. 2010, 2011). In this study, re-analysis of GALT activity in four galactosemia patients by LC-MS/MS did not detect the presence of low residual activity previously measured by spectrometry in these patients (Table 1), although the results obtained with both methods were consistent with classic galactosemia. Importantly, undetectable red blood cell GALT activity does not exclude residual GALT activity in other tissues and organs as seen in patients homozygous for the p.S135L mutation (Lai et al. 1996; Lai and Elsas 2001).
Further analysis of clinical findings with respect to biochemical data showed that patients with higher mean Gal1P were more likely to develop one or more long-term symptoms than patients with mildly increased GAL1P levels (group 1 vs group 2, p = 0.01), whereas acute neonatal symptoms were observed with similar frequencies in both groups (p = 0.30). It should be noted that patients in group 1 were overall younger than in group 2 (Tables 1 and 2), and although we accounted for age in the logistic regression model, the long-term symptoms in group 1 patients may become more apparent with increasing age. One previous study found no correlation between Gal1P levels and neurological outcome (Hughes et al. 2009). However, levels of GAL1P described in these patients were mostly above 2 mg/dL (96–397 μmol/L) (Hughes et al. 2009), and we also did not observe increased frequency of negative outcomes among group 2 patients with higher GAL1P. The same study reported borderline low IQ (73 and 74 on a Wechsler Intelligence Scale) in two classic galactosemia siblings with GAL1P values <1 mg/dL (23–30 μmol/L) on dietary treatment suggesting poor association between GAL1P and neurological outcomes at least in some galactosemia patients. Additional possible causes of low intellectual functioning were not explored in these two siblings with persistently low GAL1P levels despite a severe genotype, making it difficult to evaluate the contribution of other genetic or environmental factors to clinical outcome. Other studies have also demonstrated association of higher GAL1P levels >2.7 mg/dL and >3.5 mg/dL with verbal dyspraxia and premature ovarian failure, respectively (Guerrero et al. 2000; Webb et al. 2003). In our limited population, such a correlation could not be established.
The socioeconomic status of patients could have a significant effect on clinical outcomes (Shulman et al. 1991; MacDonald et al. 2010; Stockler et al. 2012) and this was not formally assessed in our study. However, a recent study of 231 patients with classic galactosemia (Frederick et al. 2017) showed no association between family income or parent education level and rigor of child dietary galactose restriction as well as between rigor of non-dairy galactose restriction and long-term outcomes, including growth.
The majority of galactosemia females ≥15 yo in group 2 exhibited varying degrees of ovarian function impairment from menstrual irregularities to premature ovarian insufficiency/infertility, and demonstrated abnormal levels of reproductive hormones including AMH (Fig. 4). In classic galactosemia, AMH levels are lower and correlate with antral follicle counts ascertained by ultrasound (Spencer et al. 2013). Markedly reduced AMH is associated with diminished ovarian reserve and poor response to ovarian stimulation, but low measurements in the general population are not considered predictive of failure to conceive (Committee on Gynecologic Practice 2015), a recommendation shared for patients with galactosemia (Welling et al. 2017). It would be important to continue longitudinal evaluation of reproductive function in young galactosemia females with various AMH and GAL1P levels (for example, patients 2F and 7F in group 1 vs patients 15F, 32F and 33F in group 2, Fig. 4) to further assess the correlation between GAL1P accumulation, AMH measurements, and the degree of ovarian function impairment. Since the number of females with galactosemia followed up by a single metabolic clinic is usually small, a multi-center study might be necessary to address this question.
Previous studies showed suboptimal growth in some galactosemia patients (Waggoner et al. 1990; Schweitzer et al. 1993; Panis et al. 2007), and growth restriction in a mouse model of classic galactosemia (Tang et al. 2014). Growth deficiencies (Z-scores < −2 for weight, height or both) were also observed in eight patients in this study (Fig. 2). Only one male patient in group 1 (patient 10M with essentially normal GAL1P, 1.1 ± 0.2 mg/dL) was underweight in addition to having significant neurological and behavioral problems (Table 1, Figs. 2 and 3). It is unclear if the negative outcomes observed in this patient are related to untreated galactosemia (patient did not follow diet for many years) or secondary to other diagnoses causing severe behavioral issues (autism and ADHD, patient lives in a group home) or both. Increased risk of malnutrition in autistic individuals has been reported in previous studies (Hyman et al. 2012; Phillips et al. 2014; Mari-Bauset et al. 2017). All other patients with growth deficiencies in this study had mean GAL1P ≥ 2 mg/dL, suggesting that patients with higher GAL1P levels were more likely to be underweight and/or have short stature (Fig. 2). In our study, the patient height was not corrected for the mid-parental target height and, therefore, unequal distribution of very tall or very short families in group 1 and group 2 could have potentially influenced our results.
A decreased bone mass has been reported in patients with classic galactosemia (Batey et al. 2013). This was not assessed in our study. It must be noted that a recent meta-analysis found only a limited reduction in bone mineral density in patients with classic galactosemia (Z-score − 0.7) indicating overall only a mild bone involvement (van Erven et al. 2017).
Higher GAL1P levels have been associated with poor dietary compliance of galactosemia patients (Guerrero et al. 2000; Robertson et al. 2000). All our patients, with the exception of patient 10M, followed a galactose-restricted diet (as repeatedly verified by 3-day diet records) and recommendations for dietary galactose restriction were similar in groups 1 and 2. Therefore, lower GAL1P accumulation in group 1 individuals might reflect the presence of residual GALT activity in their tissues and organs (not in red blood cells), which could alleviate phenotype severity. As an example, the mild clinical and biochemical phenotype in S135L/S135L individuals on treatment has been attributed to the residual activity of the S135L allele in liver and intestine (Lai et al. 1996; Elsas and Lai 1998; Palmieri et al. 1999). Similarly, the presence of variants p.D98N, p.T138M, p.R223S, p.I278N, and p.R201H, all characterized by ≥5% wild type residual activity in model organisms (Riehman et al. 2001; Tang et al. 2012; Spencer et al. 2013), in group 1 patients might explain their normal clinical outcomes as well as low GAL1P accumulation. In contrast, homozygosity or compound heterozygosity for p.Q188R and other severe variants with <1% wild type residual activity, such as p.K285N and p.L195P (Riehman et al. 2001; Ryan et al. 2013; Berry 2014), was unique to group 2 patients (Table 1). Global impairment of GALT activity would be expected to dysregulate many physiological pathways through various pathogenic mechanisms, including aberrant glycosylation and abnormal activation of signaling pathways (Lebea and Pretorius 2005; Liu et al. 2012; Jumbo-Lucioni et al. 2013; Coss et al. 2014a, b; Balakrishnan et al. 2016; Coelho et al. 2017), although normal outcomes were still observed in several patients with severe genotypes in this study (Table 1, Fig. 3).
In summary, the results of our study suggest that higher mean GAL1P levels are associated with poorer long-term outcomes in galactosemia patients. Therefore, evaluation of GAL1P levels on dietary treatment might be used in estimating the risk of developing long-term complications in patients with markedly reduced or undetectable red blood cell GALT activity. Considering wide genotypic heterogeneity of galactosemia patients, GAL1P levels might be especially helpful in providing a prognosis for patients with rare or novel genotypes whose clinical presentations are not well known. As for many other rare disorders, our conclusions are based on a small cohort of galactosemia patients, and, therefore, additional studies on a larger pool of patients with various genotypes and older age are necessary to corroborate predictive values of GAL1P and genotype-phenotype association.
References
Balakrishnan B, Chen W, Tang M et al (2016) Galactose-1 phosphate uridylyltransferase (GalT) gene: a novel positive regulator of the PI3K/Akt signaling pathway in mouse fibroblasts. Biochem Biophys Res Commun 470:205–212
Bandyopadhyay S, Chakrabarti J, Banerjee S et al (2003) Prenatal exposure to high galactose adversely affects initial gonadal pool of germ cells in rats. Hum Reprod 18:276–282
Batey LA, Welt CK, Rohr F et al (2013) Skeletal health in adult patients with classic galactosemia. Osteoporo Int : J Estab Result Coop Between Europe Found Osteoporo Natl Osteoporo Found USA 24:501–509
Berry GT (2014) Classic Galactosemia and clinical variant Galactosemia. In: Pagon RA, Adam MP, Ardinger HH et al (eds). GeneReviews, Seattle
Berry GT, Elsas LJ (2011) Introduction to the Maastricht workshop: lessons from the past and new directions in galactosemia. J Inherit Metab Dis 34:249–255
Calderon FR, Nelson L, Dobrowolski P et al (2007) Combination of enzyme analysis, allele-specific PCR and sequencing to detect mutations in the GALT gene. J Inherit Metab Dis 30:818
Chen J, Yager C, Reynolds R, Palmieri M, Segal S (2002) Erythrocyte galactose 1-phosphate quantified by isotope-dilution gas chromatography-mass spectrometry. Clin Chem 48:604–612
Chen YT, Mattison DR, Feigenbaum L, Fukui H, Schulman JD (1981) Reduction in oocyte number following prenatal exposure to a diet high in galactose. Science 214:1145–1147
Coelho AI, Rubio-Gozalbo ME, Vicente JB, Rivera I (2017) Sweet and sour: an update on classic galactosemia. J Inherit Metab Dis 40:325–342
Coffee B, Hjelm LN, DeLorenzo A, Courtney EM, Yu C, Muralidharan K (2006) Characterization of an unusual deletion of the galactose-1-phosphate uridyl transferase (GALT) gene. Genet Med 8:635–640
Committee on Gynecologic Practice (2015) Committee opinion no. 618: ovarian reserve testing. Obstet Gynecol 125:268–273
Coss KP, Hawkes CP, Adamczyk B et al (2014a) N-glycan abnormalities in children with galactosemia. J Proteome Res 13:385–394
Coss KP, Treacy EP, Cotter EJ et al (2014b) Systemic gene dysregulation in classical Galactosaemia: is there a central mechanism? Mol Genet Metab 113:177–187
Elsas LJ 2nd, Lai K (1998) The molecular biology of galactosemia. Genet Med : Off J Am College Med Genet 1:40–48
Frederick AB, Cutler DJ, Fridovich-Keil JL (2017) Rigor of non-dairy galactose restriction in early childhood, measured by retrospective survey, does not associate with severity of five long-term outcomes quantified in 231 children and adults with classic galactosemia. J Inherit Metab Dis 40:813-821
Fridovich-Keil JL, Gubbels CS, Spencer JB, Sanders RD, Land JA, Rubio-Gozalbo E (2011) Ovarian function in girls and women with GALT-deficiency galactosemia. J Inherit Metab Dis 34:357–366
Gitzelmann R, Steinmann B (1984) Galactosemia: how does long-term treatment change the outcome? Enzyme 32:37–46
Goldstein N, Cohen Y, Pode-Shakked B et al (2011) The GALT rush: high carrier frequency of an unusual deletion mutation of the GALT gene in the Ashkenazi population. Mol Genet Metab 102:157–160
Guerrero NV, Singh RH, Manatunga A, Berry GT, Steiner RD, Elsas LJ 2nd (2000) Risk factors for premature ovarian failure in females with galactosemia. J Pediatr 137:833–841
Holden HM, Rayment I, Thoden JB (2003) Structure and function of enzymes of the Leloir pathway for galactose metabolism. J Biol Chem 278:43885–43888
Hughes J, Ryan S, Lambert D et al (2009) Outcomes of siblings with classical galactosemia. J Pediatr 154:721–726
Hutchesson AC, Murdoch-Davis C, Green A et al (1999) Biochemical monitoring of treatment for galactosaemia: biological variability in metabolite concentrations. J Inherit Metab Dis 22:139–148
Hyman SL, Stewart PA, Schmidt B et al (2012) Nutrient intake from food in children with autism. Pediatrics 130(Suppl 2):S145–S153
Institute CaLS (2010) Defining, Establishing, and Verifying Reference Intervals in the Clinical Laboratory; Approved Guideline - 3rd Edition (C28-A3)
Jama M, Nelson L, Pont-Kingdon G, Mao R, Lyon E (2007) Simultaneous amplification, detection, and analysis of common mutations in the galactose-1-phosphate uridyl transferase gene. J Molec Diagnos 9:618–623
Jumbo-Lucioni PP, Garber K, Kiel J et al (2012) Diversity of approaches to classic galactosemia around the world: a comparison of diagnosis, intervention, and outcomes. J Inherit Metab Dis 35:1037–1049
Jumbo-Lucioni PP, Hopson ML, Hang D, Liang Y, Jones DP, Fridovich-Keil JL (2013) Oxidative stress contributes to outcome severity in a Drosophila Melanogaster model of classic galactosemia. Dis Model Mech 6:84–94
Lai K, Elsas LJ (2001) Structure-function analyses of a common mutation in blacks with transferase-deficiency galactosemia. Mol Genet Metab 74(1–2):264–272
Lai K, Elsas LJ, Wierenga KJ (2009) Galactose toxicity in animals. IUBMB Life 61:1063–1074
Lai K, Langley SD, Singh RH, Dembure PP, Hjelm LN, Elsas LJ 2nd (1996) A prevalent mutation for galactosemia among black Americans. J Pediatr 128:89–95
Lebea PJ, Pretorius PJ (2005) The molecular relationship between deficient UDP-galactose uridyl transferase (GALT) and ceramide galactosyltransferase (CGT) enzyme function: a possible cause for poor long-term prognosis in classic galactosemia. Med Hypotheses 65:1051–1057
Li Y, Ptolemy AS, Harmonay L, Kellogg M, Berry GT (2010) Quantification of galactose-1-phosphate uridyltransferase enzyme activity by liquid chromatography-tandem mass spectrometry. Clin Chem 56:772–780
Li Y, Ptolemy AS, Harmonay L, Kellogg M, Berry GT (2011) Ultra fast and sensitive liquid chromatography tandem mass spectrometry based assay for galactose-1-phosphate uridylyltransferase and galactokinase deficiencies. Mol Genet Metab 102:33–40
Liu Y, Xia B, Gleason TJ et al (2012) N- and O-linked glycosylation of total plasma glycoproteins in galactosemia. Mol Genet Metab 106:442–454
MacDonald A, Gokmen-Ozel H, van Rijn M, Burgard P (2010) The reality of dietary compliance in the management of phenylketonuria. J Inherit Metab Dis 33:665–670
Mari-Bauset S, Llopis-Gonzalez A, Zazpe I, Mari-Sanchis A, Morales Suarez-Varela M (2017) Comparison of nutritional status between children with autism spectrum disorder and typically developing children in the Mediterranean region (Valencia, Spain). Autism 21:310–322
Palmieri M, Mazur A, Berry GT et al (1999) Urine and plasma galactitol in patients with galactose-1-phosphate uridyltransferase deficiency galactosemia. Metab Clin Exp 48:1294–1302
Panis B, Gerver WJ, Rubio-Gozalbo ME (2007) Growth in treated classical galactosemia patients. Eur J Pediatr 166:443–446
Phillips KL, Schieve LA, Visser S et al (2014) Prevalence and impact of unhealthy weight in a national sample of US adolescents with autism and other learning and behavioral disabilities. Matern Child Health J 18:1964–1975
Riehman K, Crews C, Fridovich-Keil JL (2001) Relationship between genotype, activity, and galactose sensitivity in yeast expressing patient alleles of human galactose-1-phosphate uridylyltransferase. J Biol Chem 276:10634–10640
Robertson A, Singh RH, Guerrero NV, Hundley M, Elsas LJ (2000) Outcomes analysis of verbal dyspraxia in classic galactosemia. Genet Med 2:142–148
Ryan EL, Lynch ME, Taddeo E, Gleason TJ, Epstein MP, Fridovich-Keil JL (2013) Cryptic residual GALT activity is a potential modifier of scholastic outcome in school age children with classic galactosemia. J Inherit Metab Dis 36:1049–1061
Sanders RD, Spencer JB, Epstein MP et al (2009) Biomarkers of ovarian function in girls and women with classic galactosemia. Fertil Steril 92:344–351
Schweitzer-Krantz S (2003) Early diagnosis of inherited metabolic disorders towards improving outcome: the controversial issue of galactosaemia. Eur J Pediatr 162(Suppl 1):S50–S53
Schweitzer S, Shin Y, Jakobs C, Brodehl J (1993) Long-term outcome in 134 patients with galactosaemia. Eur J Pediatr 152:36–43
Shield JP, Wadsworth EJ, MacDonald A et al (2000) The relationship of genotype to cognitive outcome in galactosaemia. Arch Dis Child 83:248–250
Shih LY, Suslak L, Rosin I, Searle BM, Desposito F (1984) Gene dosage studies supporting localization of the structural gene for galactose-1-phosphate uridyl transferase (GALT) to band p13 of chromosome 9. Am J Med Genet 19:539–543
Shulman S, Fisch RO, Zempel CE, Gadish O, Chang PN (1991) Children with phenylketonuria: the interface of family and child functioning. J Dev Behav Pediatr : JDBP 12:315–321
Spencer JB, Badik JR, Ryan EL et al (2013) Modifiers of ovarian function in girls and women with classic galactosemia. J Clin Endocrinol Metab 98:E1257–E1265
Stockler S, Moeslinger D, Herle M, Wimmer B, Ipsiroglu OS (2012) Cultural aspects in the management of inborn errors of metabolism. J Inherit Metab Dis 35:1147–1152
Tang M, Facchiano A, Rachamadugu R et al (2012) Correlation assessment among clinical phenotypes, expression analysis and molecular modeling of 14 novel variations in the human galactose-1-phosphate uridylyltransferase gene. Hum Mutat 33:1107–1115
Tang M, Siddiqi A, Witt B et al (2014) Subfertility and growth restriction in a new galactose-1 phosphate uridylyltransferase (GALT) - deficient mouse model. Europe J Human Genet 22:1172–1179
Tietz NW (1995) Clinical guide to laboratory tests, 3rd edn. Saunders, Philadelphia, pp 268–273
Tyfield L, Reichardt J, Fridovich-Keil J et al (1999) Classical galactosemia and mutations at the galactose-1-phosphate uridyl transferase (GALT) gene. Hum Mutat 13:417–430
Tyfield LA (2000) Galactosaemia and allelic variation at the galactose-1-phosphate uridyltransferase gene: a complex relationship between genotype and phenotype. Eur J Pediatr 159(Suppl 3):S204–S207
Van Calcar SC, Bernstein LE, Rohr FJ, Scaman CH, Yannicelli S, Berry GT (2014) A re-evaluation of life-long severe galactose restriction for the nutrition management of classic galactosemia. Mol Genet Metab 112:191–197
van Erven B, Welling L, van Calcar SC et al (2017) Bone health in classic Galactosemia: systematic review and meta-analysis. JIMD Rep 35:87–96
Viggiano E, Marabotti A, Burlina AP et al (2015) Clinical and molecular spectra in galactosemic patients from neonatal screening in northeastern Italy: structural and functional characterization of new variations in the galactose-1-phosphate uridyltransferase (GALT) gene. Gene 559:112–118
Viggiano E, Marabotti A, Politano L, Burlina A (2017) Galactose-1-phosphate Uridyltransferase deficiency: a literature review of the putative mechanisms of short and long-term complications and allelic variants. Clin Genet. doi: 10.1111/cge.13030
Waggoner DD, Buist NR, Donnell GN (1990) Long-term prognosis in galactosaemia: results of a survey of 350 cases. J Inherit Metab Dis 13:802–818
Waisbren SE, Potter NL, Gordon CM et al (2012) The adult galactosemic phenotype. J Inherit Metab Dis 35:279–286
Walter JH, Collins JE, Leonard JV (1999) Recommendations for the management of galactosaemia. UK Galactosaemia Steering Group. Arch Disease Childhood 80:93–96
Webb AL, Singh RH, Kennedy MJ, Elsas LJ (2003) Verbal dyspraxia and galactosemia. Pediatr Res 53:396–402
Welling L, Bernstein LE, Berry GT et al (2017) International clinical guideline for the management of classical galactosemia: diagnosis, treatment, and follow-up. J Inherit Metab Dis 40:171–176
Yang YP, Corley N, Garcia-Heras J (2002) Molecular analysis in newborns from Texas affected with galactosemia. Hum Mutat 19:82–83
Funding
This work was supported by the ARUP Institute for Clinical and Experimental Pathology®. The authors confirm independence from the sponsors; the content of the article has not been influenced by the sponsors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All authors were compliant and followed the ethical guidelines, according to the requirements of the Institutional Review Board of the University of Utah.
Conflict of interests
None.
Animal rights
This article does not contain any studies with animal subjects.
Additional information
Communicated by: William Ross Wilcox
Rights and permissions
About this article
Cite this article
Yuzyuk, T., Viau, K., Andrews, A. et al. Biochemical changes and clinical outcomes in 34 patients with classic galactosemia. J Inherit Metab Dis 41, 197–208 (2018). https://doi.org/10.1007/s10545-018-0136-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10545-018-0136-9