Abstract
Homoprejudiced violence is a type of aggression against an individual or a community based on their actual or perceived sexual orientation. It may be linked to risks of acquiring HIV/STI via psychosocial variables. This study explored the association between homoprejudiced violence experiences and high-risk sexual behaviors, and potential psychosocial mediators. Using cross-sectional survey data collected in China through Blued among men who have sex with men (MSM) in January 2021, this study conducted multiple mediation analyses. Standard instruments were used to collect data on depressive symptoms in the last two weeks (PHQ-9), recreational drug usage in the last three months, and ever experiencing homoprejudiced violence (12-item survey instrument). Dependent variables were having condomless anal sex and having three or more sexual partners in the last three months. Among 1828 MSM, nearly half (847, 46%) had experienced homoprejudiced violence. Twenty-three percent (427) reached a score that suggested moderate or severe depression and 35% (644) had used recreational drugs. In the last three months, 40% (731) had condomless anal sex and 34% (626) had three or more sexual partners. The indirect mediational coefficients through depression on condomless anal sex and multiple sexual partners were 0.04 (95% CI: [0.02, 0.07]) and 0.02 (95% CI: [0.001, 0.05]), respectively. The indirect mediational coefficient of homoprejudiced violence experience on multiple sexual partners through recreational drug use was 0.05 (95% CI: [0.03, 0.08]). These findings suggest that more comprehensive interventions are needed to address the syndemic of homoprejudiced violence, mental health issues, and HIV/STI-related risks.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Homoprejudiced violence is a type of aggression against an individual or a group based on actual or perceived sexual orientation (Wu et al., 2020). Homoprejudiced violence can manifest as physical, verbal, psychological, and cyber aggression against people who identify or are perceived as sexual minorities (Wu et al., 2020). The term “homoprejudice” was selected in place of the more commonly used term “homophobia,” as it more accurately characterized the nature of anti-homosexual responses (Logan, 1996; Schiffman et al., 2006).Footnote 1 While the term homophobia denoted an “irrational fear of tolerance of homosexuality” that is often pathological (Brooks et al., 2020), its true intention was to encompass various negative beliefs, attitudes, or actions against homosexual people which were found to stem from the realm of prejudice and discrimination (Jones & Sullivan, 2002; Logan, 1996). Homoprejudice is, therefore, a more appropriate term to describe such anti-homosexual responses (Schiffman et al., 2006). The minority stress theory argues that experienced prejudiced events can cause chronically elevated social stress among sexual minority groups, and these unique stressors can result in negative mental health outcomes (Meyer, 2003). Moreover, the psychological mediation framework suggests that such homoprejudice-related stress would cause emotion dysregulation and cognitive issues and thus lead to mental health problems such as depression and substance use among sexual minorities (Hatzenbuehler, 2009).
Numerous empirical studies have provided supporting evidence for the negative impact of homoprejudiced events on mental health including psychological distress, depression, anxiety, suicidal ideation, and substance usage (Baams et al., 2015; Bostwick et al., 2014; Lea et al., 2014; Meyer, 1995). A recent review reported consistent findings among lesbian, gay, bisexual, and transgender (LGBT) individuals with increased levels of depression compared to heterosexuals, possibly linked to stigma, victimization, and violence threats (Mongelli et al., 2019). LGBT populations are also more likely to use and/or abuse alcohol and substances as a form of maladaptive coping response to minority stressors (Goldbach et al., 2014; Lea et al., 2014; Mongelli et al., 2019). In addition to a higher prevalence of depression and substance use, sexual minorities also have higher rates of risky sexual behaviors associated with HIV/STI acquisition (Pitoňák, 2017). For example, previous studies have examined the effects of minority stress on sexual behavioral outcomes (Goldbach et al., 2014; Schwartz et al., 2016), including condomless anal sex (Hatzenbuehler et al., 2008), chemsex (Bourne et al., 2015), and having more sexual partners (Blake et al., 2001; Hamilton & Mahalik, 2009).
Additionally, links between victimization/bullying, poor mental health, substance use, and high-risk sexual behavior have been discussed (Burton et al., 2019; Finneran & Stephenson, 2014; Hamilton & Mahalik, 2009). Depression and drug use were reported to be associated with high-risk sexual behaviors (Agardh et al., 2012; Bourne et al., 2015; Colfax et al., 2005; Kiene et al., 2017; Pufall et al., 2018), and some work has shown that psychological factors might mediate the relationship between minority stress and risky sexual behaviors. One longitudinal study among gay and bisexual men living with HIV identified emotion dysregulation as a mediator between internalized stigma and condomless anal sex (Rendina et al., 2017), and another study among young men who have sex with men (MSM) found that decreased resilience mediated the association between minority stress and sexual risk behavior (Storholm et al., 2019).
However, these studies were mostly conducted in developed countries with the study populations being predominantly white (Pitoňák, 2017), leaving the mental and sexual health of sexual minorities under other cultural contexts insufficiently explored. Meanwhile, many studies that tested the minority stress model treated LGBT populations as one group (Goldbach et al., 2014; Mongelli et al., 2019), while subgroups may have different risks and health needs (Pitoňák, 2017), with MSM more vulnerable to acquiring HIV and other sexually transmitted infections (STIs) compared to lesbians (Dong et al., 2019). Chinese MSM, in particular, live in a heteronormative society where same-sex marriage is not lawful, and the collectivistic value of Chinese culture adds to their pressure to conform to social norms and conceal their sexual orientation (Logie et al., 2012; Sun et al., 2021). Although growing literature has been examining the associations between minority stress and health outcomes in MSM in China (Ding et al., 2020; Sun et al., 2020a, 2020b; Wang et al., 2022), the majority focused on internalized or perceived stigma (as an internal minority stressor) and mental health (Logie et al., 2012; Sun et al., 2020a, 2020b; Yang et al., 2020; Zheng et al., 2020). Studies exploring the pathways between homoprejudiced violence events (as an external minority stressor), mental health, and sexual behaviors in the Chinese context remain limited.
This study aims to fill this research gap by exploring possible pathways through which homoprejudiced violence experience impacts high-risk sexual behavior among Chinese MSM. Building on the minority stress theory, the psychological mediation framework, and previous evidence, we hypothesized that homoprejudiced violence experience might be associated with high-risk sexual behaviors through potential mediators of depressive symptoms and drug use, and performed mediation analysis to test this hypothesis.
Method
Participants and Procedure
Eligible participants of this study were Chinese MSM that met the following criteria: (1) assigned male at birth, (2) being 18 years old or above, (3) reported ever having anal sex with men, and (4) willing to provide online survey consent.
We conducted a cross-sectional online questionnaire survey which was distributed via Blued, the most popular gay social networking platform in China. Recruitment banner adverts were posted on Blued to recruit users in five provinces of southern China (Guangdong, Guangxi, Fujian, Hunan, and Jiangxi). MSM who clicked the banner posts would undergo an eligibility assessment using a set of pre-survey questions, and eligible participants completed an online baseline survey. All survey data were anonymous and confidential and each participant provided online consent (Lu et al., 2021). A total of 2150 eligible MSM finished the survey in January 2021. After omitting duplicates and invalid responses, the total sample size was 1828. An incentive of 3.5 USD (25 Chinese Yuan) was provided to each participant who completed the survey.
Measures
Sociodemographic and behavioral characteristics
The survey collected information about participants’ sociodemographic characteristics including age, occupation, marital status, monthly income, highest education obtained, gender identity (male, female, transgender, uncertain), sexual orientation (gay, heterosexual, bisexual, uncertain/other), sexual orientation disclosure to people other than their partner(s) (yes/no). It also collected information on participants’ sexual behaviors. Specifically, they were asked about their condom usage frequencies, recreational drug usage, and the number of sexual partners in the past three months.
Independent variable
Ever experienced homoprejudiced violence (1 = yes, 0 = no). Based on previous literature, a twelve-item instrument was used to capture information about prior experiences of homoprejudiced violence. The 12 items have been used in a previous survey with MSM in China (e.g., received name calling, spat on, threatened, or physically harmed due to one’s sexual orientation; see Supplementary Table 1 for the detailed items) (Wu et al., 2020). All 12 items used three responses: “yes,” “no,” and “do not want to tell,” with “yes” coded as 1 and “no” and “do not want to tell” coded as 0. Participants who responded “yes” to any of the 12 items were defined as having ever experienced homoprejudiced violence. The Kuder–Richardson 20 (KR-20) value was 0.89 indicating high reliability of the instrument.
Mediators
Depressive symptoms (1 = moderate or more severe depression, 0 = absence of depression). The Patient Health Questionnaire (PHQ-9) was used to measure the severity of depressive symptoms in the last two weeks. It has been validated for use among Chinese population as a screening instrument for depression (Wang et al., 2014). A PHQ-9 score ≥ 10 has a sensitivity of 88% and a specificity of 88% for major depressive disorder (Kroenke et al., 2001), and 10 was commonly used as a cutoff score to define whether the participant had risks of moderate or more severe depression in this study.
Recreational drug usage in the last three months (1 = yes, 0 = no). Participants were asked about the frequency they used amyl nitrite (Poppers), 5-MeO-DIPT (Foxy methoxy), gamma-butyrolactone (GBL), or other drugs (excluding medical use) in the last three months. These drugs were most commonly used among MSM in China to enhance their sex experience (Zhao et al., 2023). Those who reported “never” to all above drug use history were coded as 0 (no recreational drug use), while the rest who reported once or twice, every month, every week, or nearly every day use of any of the above drugs were coded as 1 (recreational drug use).
Dependent variables
Condomless anal sex with men in the last three months (1 = yes, 0 = no). Participants were asked the frequency of condom usage in the last three months when having anal sexual intercourse with men, and could respond “never,” “rarely,” “frequently,” “every time,” or “have not had anal sexual intercourse with men in the last three months.” Those who reported using condoms every time were coded as 0 (no condomless anal sex), while the rest were coded as 1 (condomless anal sex). Participants who reported no sex with males in the last three months were excluded from mediation analysis (Table 1).
Having multiple sexual partners in the last three months (1 = yes, 0 = no). This variable was newly generated by adding up two items: the number of different male sexual partners in the last three months, and the number of different female sexual partners in the last three months. The new variable was coded as 0 if the added number of sexual partners was smaller than three, otherwise it was coded as 1 (Chu et al., 2018; Feng et al., 2010; Lau et al., 2003).
Of note, given the existence of new technologies such as pre-exposure prophylaxis (PrEP), condomless anal sex or having multiple sexual partners does not necessarily increase HIV risk (Newcomb et al., 2018). However, at the time of the study, PrEP was not available in the Chinese market (Xu et al., 2020), and these sexual behaviors might still increase the risk of STI transmission.
Statistical Analysis
First, descriptive analysis was used to describe sample characteristics. Second, we used multivariable logistic regression models to test the relationship between homoprejudiced violence experience and depression, recreational drug use, as well as high-risk sexual behaviors (i.e., condomless anal sex and multiple sexual partners). We also tested the interaction effect of depression and recreational drug use on homoprejudiced violence experience. Variables including age, marital status, monthly income, highest education obtained, gender identity, sexual orientation, and sexual orientation disclosure were used to control for confounders.
Finally, mediation analysis was conducted to explore the indirect effect of depression and recreational drug use on the relationship between homoprejudiced violence experience and high-risk sexual behaviors. In the mediation model, homoprejudiced violence experience was the predictor variable, depression and drug use were two potential mediators, and HIV-related high-risk sexual behaviors in the last three months were the dependent variables. We separately performed multiple mediator analyses on the two dependent variables (VanderWeele & Vansteelandt, 2014). Model 1 examined condomless anal sex and Model 2 examined multiple sexual partners as the dependent variable. Probit regression models were used because both the mediators and the dependent variables were binary (Imai et al., 2010). The “lavaan” package in R Studio was used to conduct the mediation analysis and calculate the 95% confidence interval using 10,000 bootstrapping resamples (R version 4.0.2).
Results
Descriptive Outcomes
A total of 1828 MSM were enrolled in the survey, of whom 73% self-identified as gay men, 46% ever experienced homoprejudiced violence (i.e., experienced any one of the 12 items). Nearly a quarter (427, 23%) reached a PHQ-9 cutoff score of 10 that suggested risks of moderate or more severe depression, and 644 (35%) ever used recreational drugs in the last three months. In terms of high-risk sexual behaviors, 693 (48%) had condomless anal sex with male partners in the last three months, and 847 (46%) reported having multiple sexual partners in the last three months. Over one-fifth (398, 22%) reported no sex with a man in the last three months and were excluded from mediation analysis, leaving the sample size of 1430.
Multivariable Regression Analysis Results
Table 2 shows that college level education (aOR = 0.73, 95% CI: [0.57, 0.93]), monthly income of higher than 8000 CNY (aOR = 0.61, 95% CI: [0.40, 0.93]), and bisexual identity (aOR = 0.73, 95% CI: [0.54, 0.97]) were found to be associated with lower odds of moderate or severe depression. Being 30 years old or older (aOR = 0.67, 95% CI: [0.51, 0.86]) was associated with lower odds of recreational drug usage. College level education (aOR = 1.36, 95% CI: [1.09, 1.70]), monthly income of higher than 8000 CNY (aOR = 1.83, 95% CI: [1.28, 2.63]), and sexual orientation disclosure (aOR = 1.31, 95% CI: [1.07, 1.61]) were associated with higher odds of recreational drug usage.
Ever experiencing homoprejudiced violence was significantly associated with higher odds of moderate or severe depression (aOR = 2.17, 95% CI: [1.73, 2.14]), and higher odds of recreational drug usage (aOR = 1.39, 95% CI: [1.14, 1.70]). In addition, depression was associated with higher odds of condomless anal sex with males (aOR = 1.74, 95% CI: [1.23, 2.48]), and recreational drug usage was associated with higher odds of both condomless anal sex with males (aOR = 1.43, 95% CI: [1.00, 2.05]) and having three or more sexual partners in the last 3 months (aOR = 2.33, 95% CI: [1.80, 3.02]). No interaction was found between depression and recreational drug usage. Homoprejudiced violence experience was not directly associated with recent high-risk sexual behaviors (i.e., condomless anal sex with males and having multiple sexual partners in the last 3 months) (Table 2).
Mediation Analysis Results
Table 3 shows the coefficients of three mediation models. For Model 1, the coefficients of the a1-path (homoprejudiced violence ⋄ depression) and b1-path (depression ⋄ condomless anal sex) were both significant at the 95% confidence interval. The indirect effect of the homoprejudiced violence experience on condomless anal sex with males via depression was 0.04 (95% CI: [0.02, 0.07]), suggesting that experiencing homoprejudiced violence was associated with greater risks of depression, which was associated with increased recent condomless anal sex behaviors. The coefficient a2 (homoprejudiced violence ⋄ drug use) was significant but b2 (drug use ⋄ condomless anal sex) was nonsignificant, and the indirect mediation effect through recreational drug use was nonsignificant (a2b2 = 0.01, 95% CI: [− 0.002, 0.03]). The direct effect (c′-path) of homoprejudiced violence experience on condomless anal sex with males was nonsignificant (c′ = − 0.13, 95% CI: [− 0.27, 0.03]). (Fig. 1) For Model 2, the coefficients of a1 (homoprejudiced violence ⋄ depression), b1 (depression ⋄ multiple sex partners), a2 (homoprejudiced violence ⋄ drug use), and b2 (drug use ⋄ multiple sex partners) were all significant at the 95% confidence interval. The mediation effect of homoprejudiced violence experience on having multiple sexual partners through depression was 0.02 (95% CI: [0.001, 0.05]) and that through recreational drug usage was 0.05 (95% CI: [0.03, 0.08]), suggesting that experiencing homoprejudiced violence may add to the risk of depression and the risk of using recreation drugs, and then depression and recreational drug usage may increase the risk of having multiple sexual partners. The direct effect, nevertheless, was nonsignificant. (c’ = − 0.01, 95% CI: [− 0.16, 0.14]).
Discussion
Our understanding remains limited of how prior experience of homoprejudiced violence among MSM may be associated with high-risk sexual behaviors via psychosocial mediators. The findings presented here extend the minority stress literature by testing the model in the Chinese MSM context, examining the influence of homoprejudiced violence experience as a specific type of minority stressor, and exploring potential psychological pathways through which homoprejudiced violence may impact sexual risk behaviors. In our sample, although no direct associations between homoprejudiced violence experience and high-risk sexual behaviors were identified, they may be linked via depression and recreational drug use. Our findings have public health implications for HIV/STI risk reduction campaigns that aim to decrease high-risk sexual behaviors by focusing on key factors that are amenable to psychological interventions.
Homoprejudiced violence experience was not directly associated with high-risk sexual behaviors among Chinese MSM, which was inconsistent with prior studies that identified significant, positive associations in other populations with different cultural backgrounds (Arnold et al., 2013; Damschroder et al., 2009; Hamilton & Mahalik, 2009; Hatzenbuehler et al., 2008). However, our results identified a full mediation effect through depression and recreational drug use, which was in line with a recent study in South Africa that found the association between homophobia and risk-taking sexual behavior was not always straightforward, and the best model fit was when the relationship was fully mediated by depression and self-efficacy (Tucker et al., 2014). Another study among Nigerian MSM also reported similar findings, where they identified a partial mediation effect of depressive symptoms on the relationship between minority stress and sexual risk-taking behaviors (Ogunbajo et al., 2021). Our finding of a full mediation effect within the Chinese MSM population suggested the necessity of exploring psychosocial factors to capture the complexities in the potential relationships between homoprejudiced experience and high-risk sexual behaviors. It also highlights the importance of considering the previously understated associations of prejudice-based violence with HIV/STI infection among MSM in China and other countries with similar heteronormative cultures and a lack of law protection.
Depression is an important risk factor that links prior adverse life events such as homoprejudiced violence experience with recent high-risk sexual behaviors. This is consistent with the majority of evidence from MSM in high-income countries that depression was associated with condomless sex (Alvy et al., 2011), and sex with any transmission risk partner (defined as having multiple partners, casual partners, or partners living with HIV or with an unknown HIV status) (Fendrich et al., 2013; Safren et al., 2009), although some subgroup analysis suggested that the association between depression and high-risk sexual behaviors only existed in HIV-negative MSM (Houston et al., 2012). The underlying mechanisms may be explained by maladaptive coping patterns in response to minority stressors, which may decrease one’s self-efficacy, the perceived capacity for oneself to take control of one’s life, and thus lead to depression (Maciejewski et al., 2000). Reduced self-efficacy may lead to less effort to adhere to safe sex practices (Miltz et al., 2020), and some individuals may engage in high-risk sexual practices driven by escapism (i.e., escape from rational cognition of HIV threat) because they feel powerless and incapable of keeping the threat under control when depressed (Alvy et al., 2011). Yet, depression and high-risk sexual behaviors may also be concurrent or interactive (Jie et al., 2012), so we need to be cautious of drawing any causal inference. Our regression results also found that bisexual identity was associated with lower odds of depression compared to gay, different from Western literature that reported bisexual individuals as particularly vulnerable to depression (Pakula et al., 2016). The inconsistency may be due to cultural variations where bisexuality faces dual exclusion from gay and heterosexual communities in Western society (Molina et al., 2015), while bisexual men in China have less pressure from family and society since they can still conform to heterosexual norms (Shi et al., 2020).
Additionally, recreational drug usage was another potential mediator and compared to people who have not used recreational drugs in the last 3 months, people who reported recreational drug use were more likely to have multiple sexual partners. Our results were consistent with previous findings among Chinese MSM that drug use was positively associated with condomless anal sex and multiple sex partners (Duan et al., 2017). Some limited evidence suggests that drug usage and depression may have interaction effects on condomless anal sex with casual sexual partners (Nöstlinger et al., 2020), but our regression analysis did not find such significant interactions. While recreational drug usage was reported to increase HIV infection risk partly through having more sexual partners (Xu et al., 2014), our study extends by disentangling a potentially more significant effect among MSM who experienced homoprejudiced violence and used recreational drugs. One possible explanation is that using recreational drugs was a coping strategy that meant inclusion and belonging in the MSM community, to overcome loneliness and emotional traumas from adverse life events. A previous study mentioned MSM with internalized homophobia would engage in substance use as it enabled them to express suppressed desires and overcome shame for having sex with men (Tan et al., 2021). Qualitative evidence from MSM using chemsex mentioned that the legacy of childhood isolation and marginalization experiences drove them to have chemsex in search for feelings of bonding and acceptance (Pollard et al., 2018). However, participants also acknowledged that chemsex was a barrier to nurturing relationships, indicating that sexual relationships were mostly transient and hard to maintain, which may explain why recreational drug users were more likely to have multiple sexual partners (Melendez-Torres & Bourne, 2016).
These findings have important public health and research implications. For practice, comprehensive interventions are needed to address the syndemic of homoprejudiced violence, psychosocial problems, and HIV/STI-related risks among MSM. For initiatives to reduce high-risk sexual behaviors to be effective, interventional components to address psychosocial issues may be especially important for men who experienced homoprejudiced violence and developed depression and/or had drug usage history. Some interventions have been found effective to reduce depressive symptoms and drug usage in MSM (Coulter et al., 2019), such as cognitive behavioral therapy (Safren et al., 2011) and group-based counseling interventions (Petersen et al., 2014). Two pilot trials also reported reduced sexual risk behavior through psychotherapies (Pachankis, 2014; Smith et al., 2017). These measures might be worth integrating into existing safe sex promotion programs targeting the subset of individuals with lived experiences of homoprejudiced violence. For researchers, public health research often tends to study the prevalence and characteristics of high-risk behaviors of MSM without further investigating why certain behaviors occur. But prior adverse life events such as homoprejudiced violence experience can significantly impact psycho-socio-behaviors and health outcomes (Cange et al., 2015). Our study adds a psychosocial lens to understand potential reasons for high-risk sexual behaviors.
Limitations
Some limitations need to be noted. First, our measurement of homoprejudiced violence experience was twelve items adapted from previous literature, but it was not a validated scale (Evans & Chapman, 2014; Hinduja & Patchin, 2011; Wu et al., 2020). Although the instruments covered different domains of violence such as physical assault and verbal aggression, our analysis operationalized it as a binary variable for exploratory purposes. This did not capture how the extent of homoprejudiced violence experience is associated with high-risk sexual behaviors and may account for the lack of direct associations in our mediational analyses. Yet, our study provided a starting point for future research to assess and evaluate the scale validity of measuring homoprejudiced violence (Boateng et al., 2018) and to further explore how such experience may be linked to sexual risks. Second, our mediation analysis identified associations based on cross-sectional data and therefore was unable to infer causal relationships. We used PHQ-9, a measurement of depressive symptoms within two weeks as a proxy of depression, so there were possibilities of comorbidity or inverse causation. Additionally, a recent meta-analytic study showed that this score may overestimate depression compared to structured clinical interviews (Levis et al., 2020). Further longitudinal data are needed to support the hypothesis of mediation effects. Moreover, how the mediators come into play remains unknown and requires qualitative assessment to understand the underlying mechanisms. Third, our study sample is an online convenience sample from a gay dating app. This sample may not be representative of the broader population of gay, bisexual, and other MSM population in China. The high-risk sexual behavior patterns among Chinese MSM who do not visit online gay dating apps may be different from our survey participants. Further studies should reach out to more marginalized groups of MSM communities to validate these findings. Nonetheless, our study has a large sample size from five provinces that cover a big geographical area in China, and the online recruitment helped us to reach MSM whom we might not be able to reach otherwise. Last, our study focused on prior homoprejudiced violence experience, which only involved one of the main stressors faced by sexual minorities (Meyer, 1995). Other minority stressors such as the expectation of rejection and discrimination, concealment of sexual orientation, and internalized homophobia may also come into play when shaping mental and sexual health for sexual minorities (Meyer, 2003; Mongelli et al., 2019). Future research should operationalize the minority stressors by developing a more comprehensive measurement to have a complete understanding of how sexual minority community-related stressors may impact health and behavioral outcomes.
Conclusion
Homoprejudiced violence experience is positively associated with depression and recreational drug usage. Moreover, depression and drug use appear to be potential mediators that added to the odds of high-risk sexual behavior among Chinese MSM. The results indicated the importance of comprehensive interventions to address the syndemic of homoprejudiced violence, psychosocial issues, and HIV/STI-related risks among MSM. Further studies are needed to verify the mediation effect and to better understand the psychosocial mechanisms of HIV/STI-related risks.
Notes
We use the term “homoprejudice” instead of the regularly used term “homophobia” out of the following considerations. First, in China, same-sex sexual orientation and relationships are still not widely accepted by the society, and homophobic behaviors, either intentional or unintentional, are still a quite sensitive topic to be openly discussed. Second, as elaborated in the paper, homoprejudice can better capture the nature of the issue. Third, we hope to catalyze changes in the society by adopting a socially more acceptable term to spur more open discussions in the Chinese setting.
References
Agardh, A., Cantor-Graae, E., & Östergren, P.-O. (2012). Youth, sexual risk-taking behavior, and mental health: A study of university students in Uganda. International Journal of Behavioral Medicine, 19(2), 208–216.
Alvy, L. M., McKirnan, D. J., Mansergh, G., Koblin, B., Colfax, G. N., Flores, S. A., & Hudson, S. (2011). Depression is associated with sexual risk among men who have sex with men, but is mediated by cognitive escape and self-efficacy. AIDS and Behavior, 15(6), 1171–1179.
Arnold, M. P., Struthers, H., McIntyre, J., & Lane, T. (2013). Contextual correlates of per partner unprotected anal intercourse rates among MSM in Soweto, South Africa. AIDS and Behavior, 17(1), 4–11.
Baams, L., Grossman, A. H., & Russell, S. T. (2015). Minority stress and mechanisms of risk for depression and suicidal ideation among lesbian, gay, and bisexual youth. Developmental Psychology, 51(5), 688–696.
Blake, S. M., Ledsky, R., Lehman, T., Goodenow, C., Sawyer, R., & Hack, T. (2001). Preventing sexual risk behaviors among gay, lesbian, and bisexual adolescents: The benefits of gay-sensitive HIV instruction in schools. American Journal of Public Health, 91(6), 940–946.
Boateng, G. O., Neilands, T. B., Frongillo, E. A., Melgar-Quiñonez, H. R., & Young, S. L. (2018). Best practices for developing and validating scales for health, social, and behavioral research: A primer. Frontiers in Public Health, 6. https://doi.org/10.3389/fpubh.2018.00149
Bostwick, W. B., Boyd, C. J., Hughes, T. L., West, B. T., & McCabe, S. E. (2014). Discrimination and mental health among lesbian, gay, and bisexual adults in the United States. American Journal of Orthopsychiatry, 84(1), 35–45.
Bourne, A., Reid, D., Hickson, F., Torres-Rueda, S., & Weatherburn, P. (2015). Illicit drug use in sexual settings (‘chemsex’) and HIV/STI transmission risk behaviour among gay men in South London: Findings from a qualitative study. Sexually Transmitted Infections, 91(8), 564–568.
Brooks, A. S., Luyt, R., Zawisza, M., & McDermott, D. T. (2020). Ambivalent homoprejudice towards gay men: Theory development and validation. Journal of Homosexuality, 67(9), 1261–1289.
Burton, C. L., Wang, K., & Pachankis, J. E. (2019). Psychotherapy for the spectrum of sexual minority stress: Application and technique of the ESTEEM treatment model. Cognitive and Behavioral Practice, 26(2), 285–299.
Cange, C. W., LeBreton, M., Billong, S., Saylors, K., Tamoufe, U., Papworth, E., Yomb, Y., & Baral, S. (2015). Influence of stigma and homophobia on mental health and on the uptake of HIV/sexually transmissible infection services for Cameroonian men who have sex with men. Sexual Health, 12(4), 315–321.
Chu, Z., Xu, J., Zhang, Y., Zhang, J., Hu, Q., Yun, K., Wang, H., Jiang, Y., Geng, W., & Shang, H. (2018). Poppers use and sexual partner concurrency increase the HIV incidence of MSM: A 24-month prospective cohort survey in Shenyang, China. Scientific Reports, 8(1), 1–10. https://doi.org/10.1038/s41598-017-18127-x
Colfax, G., Coates, T. J., Husnik, M. J., Huang, Y., Buchbinder, S., Koblin, B., Chesney, M., & Vittinghoff, E. (2005). Longitudinal patterns of methamphetamine, popper (amyl nitrite), and cocaine use and high-risk sexual behavior among a cohort of San Francisco men who have sex with men. Journal of Urban Health, 82(1), i62–i70. https://doi.org/10.1093/jurban/jti025
Coulter, R. W., Egan, J. E., Kinsky, S., Friedman, M. R., Eckstrand, K. L., Frankeberger, J., Folb, B. L., Mair, C., Markovic, N., & Silvestre, A. (2019). Mental health, drug, and violence interventions for sexual/gender minorities: A systematic review. Pediatrics, 144(3), 1–20. https://doi.org/10.1542/peds.2018-3367
Damschroder, L. J., Aron, D. C., Keith, R. E., Kirsh, S. R., Alexander, J. A., & Lowery, J. C. (2009). Fostering implementation of health services research findings into practice: A consolidated framework for advancing implementation science. Implementation Science, 4(1), 1–15. https://doi.org/10.1186/1748-5908-4-50
Ding, C., Chen, X., Wang, W., Yu, B., Yang, H., Li, X., Deng, S., Yan, H., & Li, S. (2020). Sexual minority stigma, sexual orientation concealment, social support and depressive symptoms among men who have sex with men in China: A moderated mediation modeling analysis. AIDS and Behavior, 24(1), 8–17.
Dong, M.-J., Peng, B., Liu, Z.-F., Ye, Q., Liu, H., Lu, X.-L., Zhang, B., & Chen, J.-J. (2019). The prevalence of HIV among MSM in China: A large-scale systematic analysis. BMC Infectious Diseases, 19(1). https://doi.org/10.1186/s12879-019-4559-1
Duan, C., Wei, L., Cai, Y., Chen, L., Yang, Z., Tan, W., Gan, Y., Au, W. W., & Zhao, J. (2017). Recreational drug use and risk of HIV infection among men who have sex with men: A cross-sectional study in Shenzhen, China. Drug and Alcohol Dependence, 181, 30–36.
Evans, C. B., & Chapman, M. V. (2014). Bullied youth: The impact of bullying through lesbian, gay, and bisexual name calling. American Journal of Orthopsychiatry, 84(6), 644–652.
Fendrich, M., Avci, O., Johnson, T. P., & Mackesy-Amiti, M. E. (2013). Depression, substance use and HIV risk in a probability sample of men who have sex with men. Addictive Behaviors, 38(3), 1715–1718.
Feng, Y., Wu, Z., Detels, R., Qin, G., Liu, L., Wang, X., Wang, J., & Zhang, L. (2010). HIV/STD prevalence among MSM in Chengdu, China and associated risk factors for HIV infection. Journal of Acquired Immune Deficiency Syndromes, 53(Suppl 1), S74-80. https://doi.org/10.1097/QAI.0b013e3181c7dd16
Finneran, C., & Stephenson, R. (2014). Intimate partner violence, minority stress, and sexual risk-taking among US men who have sex with men. Journal of Homosexuality, 61(2), 288–306.
Goldbach, J. T., Tanner-Smith, E. E., Bagwell, M., & Dunlap, S. (2014). Minority stress and substance use in sexual minority adolescents: A meta-analysis. Prevention Science, 15, 350–363.
Hamilton, C. J., & Mahalik, J. R. (2009). Minority stress, masculinity, and social norms predicting gay men’s health risk behaviors. Journal of Counseling Psychology, 56(1), 132–141.
Hatzenbuehler, M. L. (2009). How does sexual minority stigma “get under the skin”? A psychological mediation framework. Psychological Bulletin, 135(5), 707–730.
Hatzenbuehler, M. L., Nolen-Hoeksema, S., & Erickson, S. J. (2008). Minority stress predictors of HIV risk behavior, substance use, and depressive symptoms: Results from a prospective study of bereaved gay men. Health Psychology, 27(4), 455–462.
Hinduja, S., & Patchin, J. W. (2011). Cyberbullying research summary: Bullying, cyberbullying, and sexual orientation. Cyberbullying Research Center. https://cyberbullying.org/cyberbullying_sexual_orientation_fact_sheet.pdf
Houston, E., Sandfort, T., Dolezal, C., & Carballo-Diéguez, A. (2012). Depressive symptoms among MSM who engage in bareback sex: Does mood matter? AIDS and Behavior, 16(8), 2209–2215.
Imai, K., Keele, L., Tingley, D., & Yamamoto, T. (2010). Causal mediation analysis using R. In H. D. Vinod (Ed.), Advances in social science research using R (pp. 129–154). Springer. https://doi.org/10.1007/978-1-4419-1764-5_8
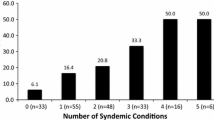
Jie, W., Ciyong, L., Xueqing, D., Hui, W., & Lingyao, H. (2012). A syndemic of psychosocial problems places the MSM (men who have sex with men) population at greater risk of HIV infection. PLoS ONE, 7(3). https://doi.org/10.1371/journal.pone.0032312
Jones, M. K., & Sullivan, G. (2002). Psychiatric disorder or straight prejudice? The role of education in overcoming homophobia. Journal of Gay & Lesbian Social Services, 14(2), 95–105.
Kiene, S. M., Lule, H., Sileo, K. M., Silmi, K. P., & Wanyenze, R. K. (2017). Depression, alcohol use, and intimate partner violence among outpatients in rural Uganda: Vulnerabilities for HIV, STIs and high risk sexual behavior. BMC Infectious Diseases, 17(88). https://doi.org/10.1186/s12879-016-2162-2
Kroenke, K., Spitzer, R. L., & Williams, J. B. W. (2001). The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine, 16(9), 606–613. https://doi.org/10.1046/j.1525-1497.2001.016009606.x
Lau, J. T., Kim, J. H., Lau, M., & Tsui, H. Y. (2003). Prevalence and risk behaviors of Chinese men who seek same-sex partners via the internet in Hong Kong. AIDS Education and Prevention, 15(6), 516–528.
Lea, T., de Wit, J., & Reynolds, R. (2014). Minority stress in Lesbian, Gay, and Bisexual young adults in Australia: Associations with psychological distress, suicidality, and substance use. Archives of Sexual Behavior, 43(8), 1571–1578. https://doi.org/10.1007/s10508-014-0266-6
Levis, B., Benedetti, A., Ioannidis, J. P., Sun, Y., Negeri, Z., He, C., Wu, Y., Krishnan, A., Bhandari, P. M., & Neupane, D. (2020). Patient Health Questionnaire-9 scores do not accurately estimate depression prevalence: Individual participant data meta-analysis. Journal of Clinical Epidemiology, 122(115–128), e1. https://doi.org/10.1016/j.jclinepi.2020.02.002
Logan, C. R. (1996). Homophobia? No, homoprejudice. Journal of Homosexuality, 31(3), 31–53.
Logie, C. H., Newman, P. A., Chakrapani, V., & Shunmugam, M. (2012). Adapting the minority stress model: Associations between gender non-conformity stigma, HIV-related stigma and depression among men who have sex with men in South India. Social Science & Medicine, 74(8), 1261–1268.
Lu, Y., Ni, Y., Wang, Q., Jing, F., Zhou, Y., He, X., Huang, S., Dai, W., Wu, D., & Tucker, J. D. (2021). Effectiveness of sexual health influencers identified by an ensemble machine learning model in promoting secondary distribution of HIV self-testing among men who have sex with men in China: Study protocol for a quasi-experimental trial. BMC Public Health, 21(1). https://doi.org/10.1186/s12889-021-11817-2
Maciejewski, P. K., Prigerson, H. G., & Mazure, C. M. (2000). Self-efficacy as a mediator between stressful life events and depressive symptoms: Differences based on history of prior depression. British Journal of Psychiatry, 176(4), 373–378.
Melendez-Torres, G. J., & Bourne, A. (2016). Illicit drug use and its association with sexual risk behaviour among MSM: More questions than answers? Current Opinion in Infectious Diseases, 29(1), 58–63.
Meyer, I. H. (1995). Minority stress and mental health in gay men. Journal of Health and Social Behavior, 36(1), 38–56. https://doi.org/10.2307/2137286
Meyer, I. H. (2003). Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence. Psychological Bulletin, 129(5), 674–697.
Miltz, A. R., Rodger, A. J., Lepri, A. C., Sewell, J., Nwokolo, N. C., Allan, S., Scott, C., Ivens, D., Lascar, M., & Speakman, A. (2020). Investigating conceptual models for the relationship between depression and condomless sex among gay, bisexual, and other men who have sex with men: Using structural equation modelling to assess mediation. AIDS and Behavior, 24(6), 1793–1806.
Molina, Y., Marquez, J. H., Logan, D. E., Leeson, C. J., Balsam, K. F., & Kaysen, D. L. (2015). Current intimate relationship status, depression, and alcohol use among bisexual women: The mediating roles of bisexual-specific minority stressors. Sex Roles, 73, 43–57.
Mongelli, F., Perrone, D., Balducci, J., Sacchetti, A., Ferrari, S., Mattei, G., & Galeazzi, G. M. (2019). Minority stress and mental health among LGBT populations: An update on the evidence. Minerva Psichiatrica, 60(1), 27–50. https://doi.org/10.23736/S0391-1772.18.01995-7
Newcomb, M. E., Moran, K., Feinstein, B. A., Forscher, E., & Mustanski, B. (2018). Pre-exposure prophylaxis (PrEP) use and condomless anal sex: Evidence of risk compensation in a cohort of young men who have sex with men. Journal of Acquired Immune Deficiency Syndromes, 77(4), 358–364.
Nöstlinger, C., Reyniers, T., Smekens, T., Apers, H., Laga, M., Wouters, K., & Vuylsteke, B. (2020). Drug use, depression and sexual risk behaviour: A syndemic among early pre-exposure prophylaxis (PrEP) adopters in Belgium? AIDS Care, 32(sup2), 57–64. https://doi.org/10.1080/09540121.2020.1739218
Ogunbajo, A., Iwuagwu, S., Williams, R., Biello, K., Kahler, C. W., Sandfort, T. G., & Mimiaga, M. J. (2021). Psychological problems mediate the relationship between minority stress and HIV sexual risk among Nigerian men who have sex with men: Testing the minority stress model. Archives of Sexual Behavior, 50, 3163–3174.
Pachankis, J. E. (2014). Uncovering clinical principles and techniques to address minority stress, mental health, and related health risks among gay and bisexual men. Clinical Psychology: Science and Practice, 21(4), 313–330.
Pakula, B., Carpiano, R. M., Ratner, P. A., & Shoveller, J. A. (2016). Life stress as a mediator and community belonging as a moderator of mood and anxiety disorders and co-occurring disorders with heavy drinking of gay, lesbian, bisexual, and heterosexual Canadians. Social Psychiatry and Psychiatric Epidemiology, 51, 1181–1192.
Petersen, I., Hancock, J. H., Bhana, A., & Govender, K. (2014). A group-based counselling intervention for depression comorbid with HIV/AIDS using a task shifting approach in South Africa: A randomized controlled pilot study. Journal of Affective Disorders, 158, 78–84.
Pitoňák, M. (2017). Mental health in non-heterosexuals: Minority stress theory and related explanation frameworks review. Mental Health & Prevention, 5, 63–73. https://doi.org/10.1016/j.mhp.2016.10.002
Pollard, A., Nadarzynski, T., & Llewellyn, C. (2018). Syndemics of stigma, minority-stress, maladaptive coping, risk environments and littoral spaces among men who have sex with men using chemsex. Culture, Health & Sexuality, 20(4), 411–427.
Pufall, E. L., Kall, M., Shahmanesh, M., Nardone, A., Gilson, R., Delpech, V., Ward, H., Group, P. V. S., Hart, G., & Anderson, J. (2018). Sexualized drug use (‘chemsex’) and high-risk sexual behaviours in HIV-positive men who have sex with men. HIV Medicine, 19(4), 261–270.
Rendina, H. J., Gamarel, K. E., Pachankis, J. E., Ventuneac, A., Grov, C., & Parsons, J. T. (2017). Extending the minority stress model to incorporate HIV-positive gay and bisexual men’s experiences: A longitudinal examination of mental health and sexual risk behavior. Annals of Behavioral Medicine, 51(2), 147–158.
Safren, S. A., Blashill, A. J., & O’Cleirigh, C. M. (2011). Promoting the sexual health of MSM in the context of comorbid mental health problems. AIDS and Behavior, 15(1), 30–34.
Safren, S. A., Thomas, B. E., Mimiaga, M. J., Chandrasekaran, V., Menon, S., Swaminathan, S., & Mayer, K. H. (2009). Depressive symptoms and human immunodeficiency virus risk behavior among men who have sex with men in Chennai, India. Psychology, Health & Medicine, 14(6), 705–715.
Schiffman, J. B., DeLucia-Waack, J. L., & Gerrity, D. A. (2006). An examination of the construct of homophobia: Prejudice or phobia? Journal of LGBT Issues in Counseling, 1(1), 75–93.
Schwartz, D. R., Stratton, N., & Hart, T. A. (2016). Minority stress and mental and sexual health: Examining the psychological mediation framework among gay and bisexual men. Psychology of Sexual Orientation and Gender Diversity, 3(3), 313–324. https://doi.org/10.1037/sgd0000180
Shi, X., Xu, W., & Zheng, Y. (2020). Heterosexual marital intention: Effects of internalized homophobia, homosexual identity, perceived family support, and disclosure among Chinese gay and bisexual men. Journal of Homosexuality, 67(4), 452–467.
Smith, N. G., Hart, T. A., Kidwai, A., Vernon, J. R., Blais, M., & Adam, B. (2017). Results of a pilot study to ameliorate psychological and behavioral outcomes of minority stress among young gay and bisexual men. Behavior Therapy, 48(5), 664–677.
Storholm, E. D., Huang, W., Siconolfi, D. E., Pollack, L. M., Carrico, A. W., Vincent, W., Rebchook, G. M., Huebner, D. M., Wagner, G. J., & Kegeles, S. M. (2019). Sources of resilience as mediators of the effect of minority stress on stimulant use and sexual risk behavior among young black men who have sex with men. AIDS and Behavior, 23, 3384–3395.
Sun, S., Budge, S., Shen, W., Xu, G., Liu, M., & Feng, S. (2020a). Minority stress and health: A grounded theory exploration among men who have sex with men in China and implications for health research and interventions. Social Science & Medicine, 252, 1–10. https://doi.org/10.1016/j.socscimed.2020.112917
Sun, S., Hoyt, W. T., Tarantino, N., Pachankis, J. E., Whiteley, L., Operario, D., & Brown, L. K. (2021). Cultural context matters: Testing the minority stress model among Chinese sexual minority men. Journal of Counseling Psychology, 68(5), 526–537.
Sun, S., Pachankis, J. E., Li, X., & Operario, D. (2020b). Addressing minority stress and mental health among men who have sex with men (MSM) in China. Current HIV/AIDS Reports, 17(1), 35–62.
Tan, R. K. J., Phua, K., Tan, A., Gan, D. C. J., Ho, L. P. P., Ong, E. J., & See, M. Y. (2021). Exploring the role of trauma in underpinning sexualised drug use (‘chemsex’) among gay, bisexual and other men who have sex with men in Singapore. International Journal of Drug Policy, 97. https://doi.org/10.1016/j.drugpo.2021.103333
Tucker, A., Liht, J., de Swardt, G., Jobson, G., Rebe, K., McIntyre, J., & Struthers, H. (2014). Homophobic stigma, depression, self-efficacy and unprotected anal intercourse for peri-urban township men who have sex with men in Cape Town, South Africa: A cross-sectional association model. AIDS Care, 26(7), 882–889.
VanderWeele, T., & Vansteelandt, S. (2014). Mediation analysis with multiple mediators. Epidemiologic Methods, 2(1), 95–115.
Wang, W., Bian, Q., Zhao, Y., Li, X., Wang, W., Du, J., Zhang, G., Zhou, Q., & Zhao, M. (2014). Reliability and validity of the Chinese version of the Patient Health Questionnaire (PHQ-9) in the general population. General Hospital Psychiatry, 36(5), 539–544.
Wang, Y., Lao, C. K., Wang, Q., & Zhou, G. (2022). The impact of sexual minority stigma on depression: The roles of resilience and family support. Sexuality Research and Social Policy, 19(2), 442–452.
Wu, D., Yang, E., Huang, W., Tang, W., Xu, H., Liu, C., Baral, S., Day, S., & Tucker, J. D. (2020). Homoprejudiced violence among Chinese men who have sex with men: A cross-sectional analysis in Guangzhou, China. BMC Public Health, 20(1), 1–7. https://doi.org/10.1186/s12889-020-08540-9
Xu, J.-J., Qian, H.-Z., Chu, Z.-X., Zhang, J., Hu, Q.-H., Jiang, Y.-J., Geng, W.-Q., Zhang, C. M., & Shang, H. (2014). Recreational drug use among Chinese men who have sex with men: A risky combination with unprotected sex for acquiring HIV infection. BioMed Research International, 2014, 1–9. https://doi.org/10.1155/2014/725361
Xu, J., Tang, W., Zhang, F., & Shang, H. (2020). PrEP in China: Choices are ahead. The Lancet HIV, 7(3), e155–e157. https://doi.org/10.1016/S2352-3018(19)30293-0
Yang, X., Li, X., Qiao, S., Li, L., Parker, C., Shen, Z., & Zhou, Y. (2020). Intersectional stigma and psychosocial well-being among MSM living with HIV in Guangxi, China. AIDS Care, 32(sup2), 5–13. https://doi.org/10.1080/09540121.2020.1739205
Zhao, T., Chen, G., Sun, C., Gong, X., Li, H., & Fu, G. (2023). The epidemic of HIV and syphilis and the correlation with substance abuse among men who have sex with men in China: A systematic review and meta-analysis. Frontiers in Public Health, 11, 1–19. https://doi.org/10.3389/fpubh.2023.1082637
Zheng, L., Hart, T. A., Noor, S. W., & Wen, G. (2020). Stressors based on sexual orientation and mental health among lesbian, gay, and bisexual individuals in China: Minority stress and perceived pressure to get married. Archives of Sexual Behavior, 49, 1769–1782.
Acknowledgements
We would like to thank all participants who were willing to complete the survey.
Funding
This work was supported by National Nature Science Foundation of China (82304257 to DW), Nanjing Medical University Career Development Grant (NMUR20230008 to DW), Jiangsu Provincial Professorship Development Grant (KY103R202309), the Key Technologies Research and Development Program (2022YFC2304900-4 to WT), National Institute of Health (R34MH119963 to WT), National Nature Science Foundation of China (81903371 to WT), and CRDF Global (G-202104–67775 to WT). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
Wu and Yan contributed to the study conception. Material preparation and data collection were performed by Ni, Lu, and Wang. Data analysis was performed by Yan and assisted by Ni. The first draft of the manuscript was written by Yan and all authors commented on previous versions of the manuscript and revised it critically. Wu and Tang acquired the fundings for the study. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare no competing interests.
Ethical Approval
The study obtained the ethical approval of the Dermatology Hospital of Southern Medical University Office of Medical Ethics Institutional Review Board (IRB) # 2019020 (R3).
Informed Consent
Informed consent was obtained from all participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yan, X., Ni, Y., Lu, Y. et al. Homoprejudiced Violence Experiences and High-Risk Sexual Behaviors among Chinese Men Who Have Sex with Men: Depression Severity and Recreational Drug Usage as Potential Mediators. Arch Sex Behav 53, 1265–1276 (2024). https://doi.org/10.1007/s10508-023-02775-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10508-023-02775-4