Abstract
Much research has examined the relationship between depressive symptoms and unprotected sex among men who have sex with men (MSM), but little is known about how depression is related to the sexual behavior of men who intentionally engage in unprotected anal intercourse, or bareback sex. In this study, we explored the extent to which depressive symptoms were associated with rates of unprotected sex among barebackers, and whether this relationship was dependent upon HIV serostatus. Using a sample of 120 MSM who engage in intentional condomless sex, we found that for HIV-negative participants, depressive symptoms were associated with the overall frequency of unprotected anal intercourse as well as unprotected anal intercourse with a serodiscordant partner. For HIV-positive participants, depressive symptoms were not associated unprotected intercourse. Additional research is needed to better understand depression among men who bareback and how interventions could be designed to address depression and reduce sexual risk behaviors.
Resumen
A pesar de la amplia investigación de la relación entre los síntomas depresivos y el sexo desprotegido entre hombres que tienen sexo con hombres (HSH), se sabe poco sobre cómo la depresión se relaciona con la conducta de los hombres que practican el sexo “bareback”, es decir, el coito anal intencionalmente desprotegido. En este estudio, exploramos si los síntomas depresivos estaban asociados a las tasas de sexo desprotegido entre un grupo de 120 hombres con episodios recientes de sexo “bareback” y si esta asociación dependía del estatus serológico por VIH. Encontramos que entre participantes VIH-negativos, los síntomas depresivos se asociaban tanto con la frecuencia global del coito anal desprotegido, como también con el coito anal desprotegido con una pareja serodiscordante. En cambio, para los participantes VIH-positivos, no hubo relación entre los síntomas depresivos y el coito anal desprotegido. Se requiere investigación adicional para comprender mejor el rol de la depresión entre hombres que practican el sexo “bareback” y para determinar cómo elaborar intervenciones que podrían enfocarse en la depresión y reducir conductas sexuales de riesgo.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
While some studies have failed to find a relationship between depressive symptoms and unprotected sex, much research has identified depression and negative affect as key factors in whether individuals engage in sex that carries the risk of infection with Human Immunodeficiency Virus [HIV; 1–9]. Among men who have sex with men (MSM), depressive symptoms and negative affective states have been associated with episodes of unprotected anal sex and occasional lapses in safer sex practices. What has been missing to date is an examination of the extent to which depressive symptoms are associated with rates of sexual activity among MSM who intentionally engage in condomless sexual activity in situations where there is risk of HIV transmission, referred to as “bareback sex”[10].
Research suggests that MSM engage in bareback sex for a variety of reasons, including enhanced intimacy with a partner, increased physical stimulation, defiance of popular norms regarding safer sex, and in some cases, fatigue with HIV-related concerns [11]. To what extent might depressive symptoms among MSM who bareback increase the frequency with which they engage in this sexual behavior? Intervention efforts often target depressive symptoms with the aim of reducing unprotected sex [12, 13]. Thus, addressing this question is critical to improve the effectiveness of these interventions with men who intentionally engage in condomless sex.
In this study, we explored the possible effect of depressive symptoms on rates of sexual activity among MSM who engage in intentional unprotected sex in risky contexts. In addition, given the differential motivations and health implications for unprotected sex depending on HIV serostatus, [11] we explored whether the relationship between depressive symptoms and rates of unprotected sex varied among barebackers based on their HIV serostatus. It is possible that depending on their serostatus, barebackers cope differently with depressive symptoms and consequently engage in distinct patterns of sexual risk taking. A recent study, for example, found that HIV-positive men were more likely than HIV-negative men to cope with psychosocial stressors through increased drug use which may lead to higher rates of unprotected sex [14].
Focusing on serostatus in examining the relationship between depressive symptoms and unprotected sex may be of additional relevance given that the research literature shows an inconsistent link between the two factors, with some studies finding evidence of increased sexual risk behavior during periods of depressed mood, [3, 4] and other studies failing to find such a relationship [15, 16]. In some cases, studies have reported decreased levels of sexual interest and activity during periods of depression [17]. This inconsistency may be accounted for to some extent by variations in study populations or depression measurement [1]. To what extent might it be attributed to differences based on serostatus?
Research indicates that the clinical features of depression differ based on serostatus, [18] thus adding to the importance of examining HIV serostatus in understanding the mixed findings between unprotected sex and depressive symptoms. While numerous psychosocial, genetic, and behavioral factors may spur depressive symptoms among men regardless of serostatus, [19, 20] depressive symptoms among HIV-positive men may also be triggered or exacerbated by the physical impact of this medical condition. Differential clinical features may affect whether the individual engages in inhibitory (i.e., reduced sexual activity) versus excitatory behavior (i.e., increased sexual activity) in response to negative mood. Such an explanation would be supported by the “dual control” hypothesis posited by Bancroft and colleagues [21–23]. By failing to note differences in clinical features, we may be unable to accurately identify cases when mood does matter and depressive symptoms among MSM are associated with escalations in unprotected sex.
Using a sample of 120 MSM who engage in intentional condomless sex, we employed the Beck Depression Inventory-II (BDI-II) to assess depressive symptoms. The BDI-II is one of the most widely used self-report measures in research and clinical practice to screen or assess individuals for depressive symptoms. The BDI contains two subscales: the cognitive-affective subscale and the somatic subscale. In this exploratory study, we examined depressive symptoms as assessed by both of the BDI’s subscales since for HIV-positive men, items related to somatic symptoms may reflect the impact of their medical condition rather than the mood disturbance. By examining both subscales, we employed an assessment approach utilized in previous research involving individuals with medical conditions.
Method
Sample and Recruitment
The current study is based on data collected in Frontiers in prevention (FIP), a four-year study that focused on MSM who meet sexual partners through the Internet to intentionally engage in condomless anal intercourse. Between April 2005 and March 2006, men were recruited who met the following criteria: (1) were at least 18 years old; (2) lived in New York City or within commuting distance; (3) reported using the Internet to meet men at least twice per month; (4) self-identified as a barebacker or as someone who practices barebacking [“Are you into bareback or do you consider yourself a barebacker”]; (5) had intentional, condomless anal intercourse during the previous two months with a man met over the Internet; and (6) used at least one of the six most popular internet sites identified in the first phase of the study. Approximately equal numbers of European Americans, African Americans, Latinos, and Asian Pacific Islanders were recruited. For more details of on this study, see Carballo-Diéguez et al. [10, 24].
Procedure
After being administered informed consent, participants completed a structured questionnaire in the research office through a Computer Assisted Self-Interview [CASI; 25]. Participants were compensated with $50 for their time upon completing the interview. This study was reviewed and approved by the Institutional Review Board at the New York State Psychiatric Institute.
Measures
Demographic Characteristics
Respondents were asked to report their age, highest year of school completed, annual income, current occupational status (including whether participants were on disability), and ethnic and racial group membership.
Sexual Behavior
Respondents were asked to report their sexual behavior with men and women during the previous 2 months using a modified version of the Sexual practices assessment schedule (SPAS) [26]. Questions were posed both in formal language and vernacular (in italics) to increase comprehension. Of relevance for the present report are three questions on sexual behavior with men in the past 2 months: (a) “How many times did a male partner put his penis in your rectum? (How many times did you get fucked in the ass?)”; (b) “How many times did a male partner put his penis in your rectum without a condom? (How many times did you get fucked in the ass without a condom?)”; and c) “How many men put their penis in your rectum without a condom? (How many men fucked you in the ass without a condom?).”
HIV Status
Participants were asked whether they had been tested for HIV, if they had received their test result, and whether they were HIV seropositive. No actual HIV tests were administered as part of this study.
Partner Serodiscordance
Participants who reported having had unprotected anal intercourse (UAI) with one or more partners were asked the following two questions, “Of those men, how many had actually told you they were HIV-negative and you had no reason to doubt it?” and “Of those men, how many do you know to be HIV-positive?” The difference in wording between the two questions was based on our interest to know if the participant had actually been expressly told by the partner that he was HIV-negative (as opposed of assuming seronegativity given that the partner “looked healthy”), and our acknowledgement that someone may find out a partner’s HIV-positive status without actually discussing it (e.g., finding HIV prescription drugs in his medicine cabinet). Those partners who were neither included in the HIV-negative nor HIV-positive counts were considered of unknown status. Among HIV-negative participants, having a serodiscordant partner was operationalized as having one or more partners who were HIV-positive or of unknown status. Among HIV-positive participants, a serodiscordant partner was operationalized as having one or more partners who were HIV-negative or of unknown status.
Depressive Symptoms
The presence of depressive symptoms during the previous 2 weeks was assessed using the BDI-II. The BDI-II is a 21-item self-report questionnaire assessing depressive symptomatology. Each item is scored on a four-point scale, ranging from 0 (absence of the symptom) to three (severe symptom). Scores of 0–13 are indicative of minimal depression; scores of 14–19 correspond to mild depression; scores of 20 to 28 indicate moderate depression; and scores of ≥29 correspond to severe symptoms [27]. The BDI contains two subscales: the cognitive-affective (items 1–14) and somatic (items 15–21) subscale.
Data Analytic Strategy
Data analysis was performed using the Predictive Analytics Software 18.0 (PASW, also known as SPSS) [28]. Due to the non-normal distribution of the data, we used nonparametric statistical methods. We divided the sample into two groups based on HIV serostatus and tested demographic differences between HIV-negative and HIV-positive participants using the χ2 statistic. We examined the relationship between depressive symptoms, frequency of unprotected anal intercourse, and numbers of sexual partners using Spearman’s rho correlation. To compare differences in depressive symptoms and these sexual behaviors between participants based on HIV serostatus, we used the Mann–Whitney U test. We also used the Mann–Whitney U test and conducted logistic regression analyses to compare levels of depressive symptoms between participants based on whether they engaged in unprotected serodiscordant sex. The significance level for all statistical tests was set at 95% (α = .05).
Results
Sample Description
Participants (N = 120) reported a mean age of approximately 34 years (SD = 9.6 years), an average of 14.8 years of education (SD = 2.9), and mean income of $27,948 (SD = 23,890). Close to two-thirds of the sample (63%; n = 76) reported having a part-time or full-time job. Thirty-one men (26%) reported being HIV-positive (Table 1). Compared with HIV-negative men, HIV-positive men were older by an average of about 6 years and earned less income. HIV-positive participants were more likely to be underemployed or work fewer hours than HIV-negative participants, χ2 (2) = 20.84; p < .01. In addition, 11 of the 13 men that reported being on disability were HIV-positive, χ2 (1) = 25.98; p < .01. We found no statistically significant differences in education or race/ethnicity by HIV status.
Depressive Symptoms
The mean BDI score for the sample was 11.2 (SD = 10.6). Thirty percent of participants (n = 36) had BDI scores in the moderate to severe range while 15% (n = 18) had mild symptom levels. HIV-positive participants garnered slightly higher scores than HIV-negative participants for the full BDI as well as the cognitive-affective and somatic subscales (see Table 1). These differences, however, were not statistically significant.
Sexual Risk Behaviors
As Table 1 shows, we compared sexual risk behaviors reported by HIV-negative and HIV-positive participants in the 2 months prior to the interview. Overall, 96% of the sample (n = 115) reported having engaged in UAI during this time frame on at least one occasion. The median number of times participants reported having UAI was six (IQR = 11) occasions. HIV seropositive participants engaged in UAI more times during a two-month period than HIV seronegative participants (Mdns = 10 vs. 5; Z = 2.538; p = .013).
More than half of the participants engaged in UAI with potentially serodiscordant partners (53%, n = 64). Nearly 50% of the HIV-negative men (n = 44) and 64.5% of the HIV-positive men (n = 20) reported having had one or more serodiscordant partners during the previous two months.
Relationship Between Depressive Symptoms and Risk Behaviors
We wanted to determine whether increases in depressive symptoms as measured by the BDI were associated with increases in the following risk behaviors: (1) numbers of sexual partners; (2) frequency of overall UAI; and, (3) frequency of UAI with serodiscordant sexual partners (all during a two-month period). We also sought to determine whether the cognitive-affective subscale rather than the somatic subscale of the BDI would be associated with risk behaviors among HIV seropositive men due to the potential impact of health-related symptoms among these participants. To examine the relationship between HIV risk behaviors and depressive symptoms, we calculated correlations between risk behaviors, the BDI total scores, and subscale scores for the cognitive-affective (BDI-Cog) and somatic (BDI-Somatic) components.
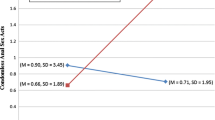
Neither the full BDI nor either of its subscales was associated with risk taking in the overall sample. Table 2 shows the relationship between depressive symptoms and sexual risk behavior according to participant HIV serostatus. Among HIV-negative participants, total BDI scores showed a significant correlation with the number of times these men engaged in UAI with a potentially serodiscordant partner during the prior two months (Spearman’s rho = .23, p < .05). Similarly, depressive symptoms as assessed by the cognitive-affective subscale were also correlated with UAI occasions with serodiscordant partners (Spearman’s rho = .24, p < .05). There were no significant correlations between serodiscordant UAI occasions and BDI-somatic subscale scores (Spearman’s rho = .17, p = .12). For HIV-positive participants, we found no significant correlations between risk behaviors and depressive symptoms as measured by the BDI or either of its two subscales.
To further test the relationship between risk behaviors and measures of depressive symptoms, we directly compared participants who reported engaging in any UAI with a serodiscordant partner versus those who did not report having had unprotected sex with a serodiscordant partner. For the entire sample, we found significant differences in depressive symptoms between men who engaged in serodiscordant UAI versus those who did not based on the cognitive-affective subscale (Z = −2.309; p = .029). We found no significant relationship between serodiscordant sex and depressive symptoms based on either the full BDI or the somatic subscale for the overall sample. Among HIV-negative participants, those who engaged in discordant UAI experienced greater levels of depressive symptoms than HIV-negative participants who did not based on the full BDI (Ms = 13.5 vs. 7.9, Z = −2.183; p = .027). There was also a similar difference in depressive symptoms between the two groups of HIV-negative men measured by the cognitive-affective subscale (Z = −2.418; p = .016). There was no significant effect based on the somatic subscale. Among HIV-positive participants, there were no statistically significant differences in depressive symptoms based on whether they engaged in discordant UAI.
Controlling for demographic factors, such as race/ethnicity, income, and education, we further examined the significant relationships between risk behaviors and depressive. Consistent with our earlier analysis for the entire sample, we found that based on the cognitive-affective subscale, men who engaged in serodiscordant UAI were significantly more likely to report greater depressive symptoms, Wald (1, n = 120) = 4.85, p = .028. In addition, we found that for HIV-negative men, those who engaged in serodiscordant UAI were more likely to report elevated depressive symptoms, Wald (1, n = 83) = 4.49, p = .034. Similarly, these HIV-negative participants reported significantly greater’s depressive symptoms based on the cognitive-affective subscale, Wald (1, n = 83) = 4.62, p = .032.
Discussion
This study is the first to our knowledge that examines the relationship between depressive symptoms and sexual behavior using a sample of MSM who deliberately engage in bareback sex. While previous research has focused on MSM who may depart from their sexual safety intentions in response to depressive symptoms, this study contributes to the literature on the depression-risk taking relationship by directing attention to men who have no such intentions. There are limitations to this investigation that deserve mention. Given that our findings were based on a cross-sectional design, we are unable to test or make any statements about a causal relationship between depressive symptoms and risk taking. The measure used to assess depressive symptoms asked participants to rate items based on the previous 2 weeks whereas the measure of sexual risk behavior covered the previous 2 months. In addition, the small sample size of the study may have hindered our ability to detect a significant effect of depressive symptoms on the sexual behavior of HIV-positive participants. Future studies should be conducted with larger samples. These limitations notwithstanding, this study is novel and makes an important contribution to understanding of how depressed mood may affect sexual behavior among MSM, particularly among MSM who engage in bareback sex.
The current study addressed the question of whether depressive symptoms among barebackers had any effect on sexual behavior, particularly sexual behavior that has been associated with HIV transmission risk. Our findings showed that for HIV-negative men who bareback, there was a direct relationship between depressive symptoms and sexual risk taking, with greater depressive symptoms corresponding to an increased frequency of engaging in unsafe behaviors. In contrast, among HIV-positive men, there was no significant relationship between depressive symptoms and unprotected sex. More research is needed to help us better understand the nature of depression among HIV-negative men in contrast to depression among HIV-positive men, and how this information may be used in the development of interventions designed to reduce their infection risk.
Findings presented here might have additional relevance given previous research which shows inconsistency in the link between depressive symptoms and risk taking. The current study suggests that some of this inconsistency may be attributed to differences in study populations. Men who deliberately seek unprotected sexual encounters in risky contexts may represent a distinct group of MSM whose sexual behaviors may be affected (albeit not fully explained) by mood disturbance when serostatus is taken into account. Such a pattern has been found in other research showing a relationship between HIV serostatus and differential patterns of coping with psychological distress and maladaptive or potentially harmful behavior, such as heightened drug use [14]. This finding is critical in that it shows the importance of directing attention to an individual’s HIV serostatus when trying to assess the likelihood of sexual risk behaviors. It is possible that such divergent patterns based on HIV serostatus existed in other studies but were not examined, thereby adding to the inconsistency between depressive symptoms and risk taking found in the literature.
Given that this sample of MSM represents men who intentionally engage in condomless sex, it may be helpful to distinguish their behavior from that of other MSM. Much of the literature that has focused on MSM who engage in unprotected sex has identified depression as a factor in the slips or departures from intentions to follow sexual safety guidelines. The current study consisted only of men who reported that they deliberately sought out unprotected sex and, furthermore, did it in circumstances that involved HIV risk. It is possible that the relationship between depressive symptoms and sexual behavior among men in this sample differed due to variations in the health consequences of unprotected sex they faced based on serostatus and the meaning they attached to these consequences. Due to these differences in potential consequences and meanings, risk taking could also be viewed as reflecting attenuation in their ability to avoid harmful behavior. Evidence suggests that individuals with depressive symptoms are more likely to engage in behaviors which have an adverse or harmful effect on their health, including poor nutrition, inadequate physical activity, substance use, cigarette smoking, irregular sleep, and failure to take medications as prescribed [29–32].
For HIV-positive men, the potential consequences of being less likely to avoid this harmful behavior include sexually transmitted infections or exposure to a drug-resistant strain of HIV. HIV-negative men, however, face exposure to both HIV as well as sexually transmitted infections. Our findings suggest that increases in existing sexual risk behavior (i.e., unprotected anal intercourse) may occur among HIV-negative men with escalations in depressive symptoms. These men may more frequently engage in risk taking for reasons similar to those found in other studies examining the relationship between depression and unprotected sex among HIV-negative men [9]. These reasons include fatalistic beliefs about maintaining their HIV-negative serostatus and those related to fatigue with HIV safety. Risk taking among HIV-negative men may be related to a marked need for intimacy and the comfort derived from this personal connection [33]. In addition, HIV-negative men may engage in intentional unprotected sex in risky contexts as a way of relieving depressive symptoms by “letting go.” In contrast, HIV-positive men may have concerns not present among those who are seronegative that cancel out any potential respite from depressive symptoms (e.g., transmitting the virus to a partner). Additional research is needed to better understand how depressive symptoms affect sexual activity among men who intentionally engage in potentially harmful sexual behaviors.
References
Alvy LM, McKirnan DJ, Mansergh G, et al. Depression is associated with sexual risk among men who have sex with men, but is mediated by cognitive escape and self-efficacy. AIDS Behav. 2001;15(6):1171–9.
Beck A, McNally I, Petrak J. Psychosocial predictors of HIV/STI risk behaviours in a sample of homosexual men. Sex Transm Infect. 2003;79(2):142–6.
Bradley MV, Remien RH, Dolezal C. Depression symptoms and sexual HIV risk behavior among serodiscordant couples. Psychosom Med. 2008;70(2):186–91.
Koblin BA, Husnik MJ, Colfax G, Huang Y, Madison M, Mayer K. Risk factors for HIV infection among men who have sex with men. AIDS. 2006;20:731–9.
Parsons JT, Halkitis PN, Wolitski RJ, Gomez CA. Correlates of sexual risk behaviors among HIV-positive men who have sex with men. AIDS Educ Prev. 2003;15(5):383–400.
Perdue T, Hagan H, Thiede H, Valleroy L. Depression and HIV risk behavior among seattle-area injection drug users and young men who have sex with men. AIDS Educ Prev. 2003;15(1):81–92.
Rogers G, Curry M, Oddy J, Pratt N, Beilby J, Wilkinson D. Depressive disorders and unprotected casual anal sex among Australian homosexually active men in primary care. HIV Med. 2003;4(3):271–5.
Stall R, Mills TC, Williamson J, Hart T, Greenwood G, Paul J, et al. Association of co-occurring psychosocial health problems and increased vulnerability to HIV/AIDS among urban men who have sex with men. Am J Public Health. 2003;93(6):939–42.
Yi H, Sandfort TGM, Shidlo A. Effects of disengagement coping with HIV risk on unprotected sex among HIV-negative gay men in New York City. Health Psychol. 2010;29(2):205–14.
Carballo-Diéguez A, Ventuneac A, Bauermeister J, Dowsett GW, Dolezal C, Remien RH, et al. Is ‘bareback’ a useful construct in primary HIV-prevention? Definitions, identity, and research. Cult Health Sex. 2009;11(1):51–65.
Carballo-Diéguez A, Bauermeister J. “Barebacking”: intentional condomless anal sex in HIV-risk contexts. Reasons for and against it. J Homosex. 2004;47(1):1–16.
McKirnan DJ, Tolou-Shams M, Courtenay-Quirk C. The treatment advocacy program: a randomized controlled trial of a peer-led safer sex intervention for HIV-infected men who have sex with men. J Consult Clin Psychol. 2010;78(6):952–63.
Stein MD, Anderson BJ, Solomon DA, Herman DS, Ramsey SE, Brown RA, et al. Reductions in HIV risk behaviors among depressed drug injectors. Am J Drug Alcohol Abuse. 2005;31(3):417–32.
Hampton MC, Halkitis PN, Mattis JS. Coping, drug use, and religiosity/spirituality in relation to HIV serostatus among gay and bisexual men. AIDS Educ Prev. 2010;22(5):417–29.
Dolezal C, Carballo-Diéguez A, Nieves-Rosa L, Diaz F. Substance use and sexual risk behavior: understanding their association among four ethnic groups of Latino men who have sex with men. J Subst Abuse. 2000;11(4):323–36.
Levounis P, Galanter M, Dermatis H, Hamowy A, De Leon G. Correlates of HIV transmission risk factors and considerations for interventions in homeless, chemically addicted and mentally ill patients. J Addict Disord. 2002;21(3):61–72.
Kennedy SH, Dickens SE, Eisfeld BS, Bagby RM. Sexual dysfunction before antidepressant therapy in major depression. J Affect Disord. 1999;56(2–3):201–8.
Akena DH, Musisi S, Kinyanda E. A comparison of the clinical features of depression in HIV-positive and HIV-negative patients in Uganda. Afr J Psychiatry (Johannesbg). 2010;13(1):43–51.
Newcomb ME, Mustanski B. Internalized homophobia and internalizing mental health problems: a meta-analytic review. Clin Psychol Rev. 2010;30(8):1019–29.
Meyer I. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychol Bull. 2003;129(5):674–97.
Bancroft J, Janssen E, Strong D, Carnes L, Vukadinovic Z, Long JS. The relation between mood and sexuality in heterosexual men. Arch Sex Behav. 2003;32(3):217–30.
Bancroft J, Janssen E, Strong D, Vukadinovic Z. The relation between mood and sexuality in gay men. Arch Sex Behav. 2003;32(3):231–42.
Bancroft J, Janssen E. The dual control model of male sexual response: a theoretical approach to centrally mediated erectile dysfunction. Neurosci Biobehav Rev. 2000;24(5):571–9.
Carballo-Diéguez A, Dowsett G, Ventuneac A, Remien R, Balan I, Dolezal C, et al. Cybercartography of popular Internet sites used by New York City men who have sex with men interested in bareback sex. AIDS Educ Prev. 2006;18(6):475–89.
Couper M, Rowe B. Evaluation of a computer-assisted self-interview component in a computer-assisted interview survey. Public Opin Q. 1996;60(1):89–105.
Carballo-Diéguez A, Remien RH, Dolezal C, Wagner G. Reliability of sexual behavior self-reports in male couples of discordant HIV-status. J Sex Res. 1999;38(2):152–8.
Beck A, Steer R, Brown G. The Beck Depressive Inventory—Second Edition Manual. San Antonio: The Psychological Corporation; 1996.
SPSS Inc. PASW 18.0 for Windows, Release 18.0. Chicago: SPSS Inc., 1996.
John U, Meyer C, Rumpf HJ, Hapke U. Self-efficacy to refrain from smoking predicted by major depression and nicotine dependence. Addict Behav. 2004;29(5):857–66.
Lin EH, Katon W, Von Korff M, Rutter C, Simon GE, Oliver M, et al. Relationship of depression and diabetes self-care, medication adherence, and preventive care. Diabetes Care. 2004;27(9):2154–60.
Odegard PS, Capoccia K. Medication taking and diabetes: a systematic review of the literature. Diabetes Educ. 2007;33(6):1014–29.
Allgöwer A, Wardle J, Steptoe A. Depressive symptoms, social support, and personal health behaviors in young men and women. Health Psychol. 2001;20(3):223–7.
Carballo-Diéguez A, Ventuneac A, Dowsett GW, Balan I, Bauermeister J, Remien RH, et al. Sexual pleasure and intimacy among men who engage in “bareback sex”. AIDS Behav. 2011;15(Suppl 1):S57–65.
Acknowledgments
Dr. Houston is supported by a training grant from the National Institute of Mental Health (T32 MH019139; Behavioral Sciences Research in HIV Infection; Principal Investigator, Theodorus Sandfort, Ph.D.). This research was supported by Grant R01 MH69333 from the NIMH to the HIV Center for Clinical and Behavioral Studies at New York State Psychiatric Institute and Columbia University (Alex Carballo-Diéguez, Ph.D., Principal Investigator). The content is solely the responsibility of the authors and does not necessarily represent the official views of NIMH or the NIH. The authors would like to thank Theresa Exner, Timothy Frasca, Rebecca Giguere, Susie Hoffman, Marina Mabragaña, John Markowitz, Tsitsi Masvaure, Judith Rabkin, and Ray Smith for their assistance and support in completing this report.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Houston, E., Sandfort, T., Dolezal, C. et al. Depressive Symptoms Among MSM Who Engage in Bareback Sex: Does Mood Matter?. AIDS Behav 16, 2209–2215 (2012). https://doi.org/10.1007/s10461-012-0156-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-012-0156-7