Abstract
Gay, bisexual, and other men who have sex with men (GBMSM) in Nigeria bear a disproportionately higher burden of HIV. Meyer’s minority stress theory posits that social stress due to the discrimination, violence, and stigma experienced by lesbian, gay, and bisexual men and women (LGBs)—due to their sexual orientation—may contribute to psychological problems, including mental health problems, substance use, and HIV sexual risk-taking. Between March and June 2019, we recruited 406 GBMSM from four states in Nigeria (Abuja, Delta, Lagos, and Plateau) to complete a cross-sectional survey at local community-based organizations. We utilized structural equation modeling to test whether psychological problems and substance use mediated the relationship between minority stress and HIV sexual risk-taking (condomless anal sex and number of sexual partners) among GBMSM in Nigeria. Minority stress (β = 0.60, 95% CI: 0.44–0.72, p ≤ .001), substance use (β = 0.43, 95% CI: 0.27–0.59, p = .004), and psychological problems (β = 0.35, 95% CI: 0.28–0.45 p = .012) had moderate associations with HIV sexual risk-taking. We found that psychological problems mediated the relationship between minority stress and HIV sexual risk-taking. Interventions focused on addressing psychological problems may help mitigate the effects of minority stress on HIV sexual risk-taking among GBMSM in Nigeria.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Nigeria has the fourth largest human immunodeficiency virus (HIV) epidemic in the world, with a prevalence of 1.4% among adults and an estimated 1.9 million people currently living with HIV (HIV/AIDS & UNAIDS, 2017). Gay, bisexual and other men who have sex with men (GBMSM) in Nigeria bear a disproportionately higher burden of HIV, with an estimated prevalence of 11–35% compared to 1.5% in the general population (Vu et al., 2013). HIV prevalence among GBMSM in Nigeria is increasing, from 14% in 2007 to 17% in 2010 and 23% in 2014 (Eluwa et al., 2019). A recent study found that increasing psychological problems was associated with risky sexual behavior among Nigerian men who have sex with men (MSM) (Oginni et al., 2019). Consequently, it is important to investigate intersecting factors that exacerbate risk of HIV infection among GBMSM in Nigeria, to better develop and implement interventions to reduce the burden of HIV in this vulnerable population.
Previous research has demonstrated that experiences of marginalization, discrimination, and violence, due to self-identifying or being perceived as a sexual minority (lesbian gay, bisexual, or transgender), contribute to psychological problems (i.e., depressive symptoms, anxiety, suicidal thoughts) and substance use (i.e., hazardous alcohol consumption and drug use) (Fingerhut, Peplau, & Gable, 2010; Lewis, Derlega, Griffin, & Krowinski, 2003; Meyer, 1995; Wong, Weiss, Ayala, & Kipke, 2010). Currently, homosexuality is criminalized in Nigeria through the passage of the Same-Sex Marriage Prohibition Act (SSMPA) in 2014, and lesbian, gay, bisexual, and transgender (LGBT) communities in Nigeria experience violations to their basic human rights on a regular basis (Okanlawon, 2018). A report found a total of 213 reported cases of battery, assault, arbitrary arrest/unlawful detention, mob attack, torture, threat to life, kidnap, and forced eviction, experienced by LGBT Nigerians between December 2017 and November 2018 (TIERS, 2019). Marginalization due to sexual minority identity and the resulting hostile and unsafe environment may contribute to lower quality of life and maladaptive coping strategies among LGBT communities in Nigeria (TIERS, 2019), which may have implications for their health status and access to healthcare services.
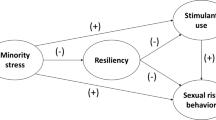
Meyer’s minority stress theory posits that social stress due to the discrimination, violence, and stigma experienced by the LGBT community—because of their sexual orientation and gender identity—may contribute to psychological problems including mental health problems, substance use, and HIV sexual risk-taking (Meyer, 2003; Newcomb & Mustanski, 2011). Prior research on LGBT individuals have provided empirical evidence in support of the proposed mechanism within the minority stress theory, where experiences of minority stress negatively impacts mental health outcomes (Frost, Lehavot, & Meyer, 2015; Hatzenbuehler, Nolen-Hoeksema, & Erickson, 2008; Lewis et al., 2003). Specifically, previous work has shown that psychosocial health might mediate the relationship between experiences of minority stress and sexual risk-taking among GBMSM. A longitudinal study of HIV-positive gay and bisexual men in New York City found that emotion dysregulation mediated the association between internalized stigma and sexual compulsivity and serodiscordant condomless anal sex (Rendina et al., 2017). Another study of 1817 young MSM in Texas showed that decreased resilience partially mediated the association of minority stress with sexual risk behavior (Storholm et al., 2019). The study also found that resilience was negatively associated with stimulant use (Storholm et al., 2019). Consequently, it is important to explore the pathway through which experiences of minority stress influences sexual risk-taking through psychosocial health and substance use among Nigerian GBMSM.
Research has found that GBMSM are at elevated risks for substance use related problems, compared to lesbian and bisexual women and heterosexual populations (Green & Feinstein, 2012). There exists a relationship between substance use, psychological problems, and sexual risk-taking among GBMSM. A pilot study of GBMSM in Lagos, Nigeria, found that individuals who reported alcohol dependence in the previous 3 month had five times the odds of reporting a history of post-traumatic stress disorder (Ogunbajo et al., 2020d). A longitudinal study of Black, Latino, and multiracial gay and bisexual men in New York City found that emotional regulation difficulty was associated with drug use (specifically methamphetamines, cocaine, ecstasy, and heroin) (English, Rendina, & Parsons, 2018). This provides some evidence of a significant association between substance use and psychological problems among gay and bisexual men, which can be bidirectional in nature (i.e., substance use facilitating occurrence of psychological problems and/or individuals dealing with existing psychological problems turning to using substance as a coping strategy). A qualitative study of GBMSM in Nigeria found that participants reported engaging in recreational drug use due to low self-esteem and to cope with difficulty emotional situations (Ogunbajo et al., 2020b). A large study of GBMSM in Kenya found that 51% of participants reported problematic substance use, 44% reported hazardous alcohol consumption, and 31% reported moderate-to-severe depressive symptoms (Korhonen et al., 2018). The study also found that condomless transactional sex with significantly associated with hazardous alcohol consumption (Korhonen et al., 2018), providing additional evidence of how substance use may influence sexual risk-taking among GBMSM in Africa. Other studies have found a strong association between substance use and condomless anal sex among MSM in the U.S. (Celentano et al., 2006; Ramirez-Valles, Garcia, Campbell, Diaz, & Heckathorn, 2008; Vosburgh, Mansergh, Sullivan, & Purcell, 2012).
There is limited research on how the minority stress model impacts HIV sexual risk-taking—specifically among GBMSM—within the African context. A qualitative study (N = 22) of South African GBMSM found that a majority of participants had experienced minority stress, which adversely affected their sexual partnerships (McAdams-Mahmoud et al., 2014). Specifically, participants discussed engaging in risky sex due to depression related to their sexual orientation (McAdams-Mahmoud et al., 2014). Another study found that increased levels of internalized homophobia were associated with lower reported quality of life (Oginni, Mapayi, Afolabi, Obiajunwa, & Oloniniyi, 2020) and depressive symptoms (Oginni, Mosaku, Mapayi, Akinsulore, & Afolabi, 2018) among MSM in Nigeria. The current study aims to fill this gap in knowledge by examining the processes through which minority stress impacts HIV sexual risk-taking among Nigerian GBMSM.
The current study investigated the potentially mediating effects of psychological problems and substance use on the relationship between minority stress and HIV sexual risk-taking among a multisite sample of GBMSM in Nigeria. We hypothesized a statistically significant positive direct relationship between minority stress and HIV sexual risk-taking. We also hypothesized statistically significant positive indirect pathways, in which the relationship between minority stress and HIV sexual risk-taking is mediated by psychological problems and substance use (Fig. 1).
Method
Participants and Procedure
Between March and June 2019, 406 GBMSM were recruited from Abuja (n = 107), Delta (n = 102), Lagos (n = 112), and Plateau (n = 85) through community-based organizations (CBOs) and snowball sampling. These four sites were selected due to existing relationships with the partner CBOs and to allow for geographical and ethnic group diversity in our sample. Peer educators, outreach workers, and key opinion leaders from CBOs based in the four study sites provided potential participants with information about the study during programmatic events (such as advocacy events, peer health education session, HIV testing and counseling outreach, etc.) Potential participants were provided with the study contact information to schedule a time for a brief screener to determine whether they were eligible to participate in the study. Individuals who contacted study staff were screened for eligibility. Eligibility criteria were: (1) 18 years of age or older; (2) currently residing in one of four Nigerian states (Abuja, Delta, Lagos or Plateau); (3) identify as cis-gender male (i.e., participants who were assigned male sex at birth and currently identify as men); and (4) any self-reported history of sex (oral or anal) with another male. Eligible participants were asked to provide members of their social network with information about the study.
Data collection occurred in the private offices of each CBO. Each participant provided verbal informed consent and completed the quantitative survey on a Tablet with the help of a trained research assistant. All research assistants were GBMSM living in Nigeria. The research assistant read through the survey instructions and questions with each participant. The survey took between 1 and 1.5 h to complete. Upon completion, each participant was compensated with 4,000 Naira (equivalent to 10 US dollars). All study procedures were approved by the Institutional Review Boards at Brown University and the Nigerian Institute of Medical Research.
Measures
Sociodemographics
Age was assessed by asking participants their current age in years. Relationship status was assessed as single versus not single (short-term relationship with a man or woman, long-term relationship with a man or woman, married to a man or woman, divorced, widowed, separated). Educational attainment was assessed by asking participants their level of school completion with the following response options: senior secondary school or lower (no formal education, primary school, junior secondary school, senior secondary school), some university or vocational school, university degree or higher (university degree, graduate/post-graduate degree), or other. Sexual orientation was assessed by asking participants to indicate their sexual identity: gay/homosexual, bisexual, straight/heterosexual, questioning, or other.
Monthly income was assessed by asking participants to provide their monthly income in Naira and the responses were categorized as: ₦0–₦10,000, ₦10,000–₦30,000, ₦30,000–₦50,000, ₦50,000–₦100,000, or ₦100,000 or more. Employment status was assessed as employed (working full-time, working part-time, self-employed) vs. unemployed (student, unemployed, looking for work, unemployed not looking for work). Financial hardship was assessed by asking participants: “How difficult is it for you to meet monthly payment on bills (rent, electricity, transportation, food, etc.)?” and dichotomized into high financial hardship (“somewhat difficult,” “very difficult,” “extremely difficult”) vs. low financial hardship (“not at all difficult,” “not very difficult”) (Tucker-Seeley, Mitchell, Shires, & Modlin, 2015). History of incarceration was assessed by asking participants: “Have you ever spent time in a prison, jail, or detention center?” with response options yes versus no.
Minority Stress (Latent Construct)
Minority stress was assessed using the short-form version of the adapted LGBT Minority Stress measure (Ogunbajo et al., 2020a), a 50-item scale developed to measure the seven components of the minority stress model: prejudice events, victimization events, rejection anticipation, identity concealment, and internalized stigma, everyday discrimination, and community connectedness. We utilized the internalized stigma, rejection anticipation and victimization events subscales for the current study.
Internalized stigma was assessed using 3 items and scored on a 5-point Likert scale ranging from 1 “Strongly Disagree” to 5 “Strongly Agree” with a higher score indicating higher levels of internalized stigma. A sample question was: “If I could change from being LGBT to be straight, I would.” The items had adequate internal consistency (Cronbach’s alpha = 0.80) and were utilized as a composite score.
Rejection anticipation was assessed using four items and scored on a 5-point Likert scale ranging from 1 “Never Happens” to 5 “Happens all the time” with a higher sore indicating higher levels of rejection anticipation. A sample question was: “I expect that others will not accept me because I am LGBT.” The items had adequate internal consistency (Cronbach’s alpha = 0.72) and were utilized as a composite score.
Victimization events was assessed using three items and scored on a 5-point Likert scale ranging from 1 “Never Happens” to 5 “Happens all the time” with a higher sore indicating higher levels of self-reported experiences of victimization events. A sample question was: “Others have threatened to harm me because I am LGBT.” The items had adequate internal consistency (Cronbach’s alpha = 0.92) and were utilized as a composite score.
Psychological Problems (Latent Construct)
Anxiety
Anxiety was assessed using the Generalized Anxiety Disorder 7-item (GAD-7) scale (Spitzer, Kroenke, Williams, & Löwe, 2006), a validated scale that measures recent symptoms of generalized anxiety disorder on a 4-point Likert scale ranging from 0 “Not at all” to 3 “Nearly every day.” A sample question was: “Over the last two weeks, how often have you had trouble relaxing?” Scores were summed and higher score indicated greater anxiety. The items had high internal consistency (Cronbach’s alpha = 0.82) and were utilized as a composite score.
Depressive Symptoms
Depressive symptoms were assessed using the shortened CESD-R scale (Eaton, Smith, Ybarra, Muntaner, & Tien, 2004), a 20-item self-report scale used to screen for clinically significant depressive symptoms. The items were scored on a 4-point scale ranging from 0 “not at all or less than one day” to 3 “5–7 days or nearly every day.” A sample question was: “I didn’t have an appetite.” The items had high internal consistency (Cronbach’s alpha = 0.93) and were utilized as a composite score.
Substance Use (Latent Construct)
Alcohol Use
Alcohol use was assessed with the AUDIT-C (Bush, Kivlahan, McDonell, Fihn, & Bradley, 1998), a 3-item screening for heavy drinking or alcohol dependence. The AUDIT-C is scored on a scale of 0–12; a score of 4 or greater indicated hazardous drinking for men. A sample question was: “How often do you have a drink containing alcohol?” The items had adequate internal consistency (Cronbach’s alpha = 0.70) and were utilized as a composite score.
Drug Use
Drug use was assessed by asking participants how often they had ever used any of the following recreational drugs in the previous 3 months: cocaine and methamphetamines. These specific substances were chosen because they have been shown to be associated with sexual risk-taking among GBMSM (Vosburgh et al., 2012). The items were scored on a 5-point scale ranging from 1 “never” to 5 “daily or almost daily” and a higher score indicated more frequent drug use.
HIV Sexual Risk-Taking (Latent Construct)
Condom Use for Receptive Anal Sex Acts in Previous 3 Months
This was assessed by asking participants: “In the last 3 months, of the times you had receptive anal sex (bottom) with a male sexual partner how often were condoms used?” with response options “never” (5), “almost never” (4), “about half the time” (3), “almost always” (2), “always” (1), and “I didn't bottom in last 3 months” (0).
Condom Use for Insertive Anal Sex Acts in Previous 3 Months
This assessed by asking participants: “In the last 3 months, of the times you had insertive anal sex (top) with a male sexual partner how often were condoms used?” with response options “never” (5), “almost never” (4), “about half the time” (3), “almost always” (2), “always” (1), and “I didn't top in last 3 months” (0).
Number of Male Partners in Previous 3 Months
We asked participants: “How many male oral and anal sexual partners have you had in the past 3 months?” with an open-ended response option.
History of Prep Use
To assess history of PrEP use, participants were asked: “Have you ever taken PrEP to prevent HIV?” (yes/no).
Statistical Analyses
We utilized structural equation modeling (SEM) to assess the relationship between the four constructs: minority stress (internalized stigma, rejection anticipation, and victimization events), psychological problems (anxiety and depressive symptoms), substance use (alcohol use, cocaine, and methamphetamines), and HIV sexual risk-taking (condom use for receptive anal sex in previous 3 months, condom use for insertive anal sex in previous 3 months, and number of sexual partners in the previous 3 months). While we understand that the relationship between these variable can be bidirectional, we specified a directional path from minority stress to HIV sexual risk-taking to specifically test the minority stress mode. Additionally, we specified a directional path of psychological problems resulting in substance use to test due to prior work demonstrating substance use as a coping mechanism for psychological problems. The latent constructs were estimated by the structural model (Fig. 2). To assess fit of the model, we examined the root mean square error of approximation (RSMEA) values (< 0.06 considered excellent and < 0.08 considered good); comparative fit index (CFI) (< 0.95 considered excellent and < 0.90 considered good; and the standardized root mean square residual (SRMR) (< 0.08 considered good) (Brown, 2014; Marsh, Hau, & Wen, 2004). The relationship between the latent constructs was estimated by the structural model.
Structural model of minority stress. Psychological problems, substance use, and HIV sexual risk-taking among Nigerian GBMSM (N = 406). Variables in boxes are the measured indicator variable. Variables in circles are the latent constructs. Dashed lines are statistically insignificant associations (p > .05). Solid lines are statistically significant associations (p < .05). Standardized effect sizes with asterisks are statistically significant (p < .05). Paths that were significant (p < .05) are shown in solid lines and paths that were not significant (p > .05) are shown in dashed lines
We conducted SEM (specifically path analysis) utilizing maximum likelihood estimation with robust standard errors of model parameters using MPlus 8. Bootstrapping was used to estimate the significance of mediation effects (10,000 draws). We provide the standardized estimate (β), corresponding standard error (SE), and p-value for the estimated regression parameters. Statistical significance was assessed at 5% level (p < .05 statistically significant) and 95% confidence intervals (CIs) are provided for the direct and indirect effects (Muthén, 2011).
Model Fit Statistics
The measurement model had factor loadings that were moderate to high (0.39–0.88), indicating reasonable loading of the indicator variables on to latent constructs. We found acceptable fit for the structural equation model (χ2(62) = 174, p ≤ .0001; CFI = 0.90, RMSEA = 0.03 and SRMR = 0.03). The estimated paths for the mediation analysis are shown in Fig. 2. We present the factor loading values for the measurement model (latent constructs) and the standardized regression coefficients for the structural model.
Results
Demographic Characteristics
Participant demographics are presented in Table 1. Participants ranged in age from 18 to 60 years (mean = 29.2, SD = 5.8), the majority (n = 231, 59.7%) identified as bisexual, and 62.2% were single. Most (n = 238, 61.8%) participants reported experiencing high financial hardship and 22.3% reported a history of incarceration (n = 86).
Direct Effects
We found that HIV sexual risk-taking was significantly predicted by the hypothesized constructs within the minority stress model (Table 2). Minority stress (β = 0.60, 95% CI: 0.44–0.72, p ≤ .001), substance use (β = 0.43, 95% CI: 0.27–0.59, p = .004), and psychological problems (β = 0.35, 95% CI: 0.28–0.45 p = .012) had moderate associations with HIV sexual risk-taking.
Total Effects
We evaluated three unique pathways of the indirect effect of minority stress on HIV sexual risk-taking. The indirect pathways were: (I) the path where psychological problems mediated the association between minority stress and HIV sexual risk-taking, (II) the path where substance use mediated the association between minority stress and HIV sexual risk-taking, and (III) the path where psychological problems and substance use mediated the association between minority stress and HIV sexual risk-taking. The total effects of minority stress on HIV sexual risk-taking are summarized in Table 3. We found that the total combined effect of minority stress on HIV sexual risk-taking (direct and indirect) was significant (β = 0.71, 95% confidence interval (CI): 0.53–0.78, p ≤ .001). The total direct effect of minority stress on HIV sexual risk-taking was significant (β = 0.60, 95% CI: 0.44–0.72, p ≤ .001) , and the total indirect effect of minority stress on HIV sexual risk-taking was statistically significant (β = 0.12, 95% CI: 0.02–0.21, p = .02).
The first pathway showed the indirect effect of minority stress on HIV sexual risk-taking through psychological problems (paths A and F with βA = 0.67, 95% CI: 0.51–0.74, p ≤ .001 and βF = − 0.35, 95% CI: 0.28–0.45, p = .012). This suggests that greater minority stress was associated with higher psychological problems, which in turn was associated with higher HIV sexual risk-taking (overall indirect pathway β = 0.09, 95% CI: 0.04–0.12, p = .004).
The second pathway showed the indirect effect of minority stress on HIV sexual risk-taking through substance use (paths C and E with βC = − 0.08, 95% CI: − 0.12–0.17, p = .480 and βE = 0.43, 95% CI: 0.27–0.59, p = .004). This suggests that greater minority stress was not associated with substance use, which in turn was significantly associated with higher HIV sexual risk-taking (overall indirect pathway β = 0.04, 95% CI: 0.01–0.09, p = .051).
The third and final pathway showed the indirect effect of minority stress on HIV sexual risk-taking through psychological problems and substance use (paths A, D, and E with βA = 0.67, 95% CI: 0.51–0.74, p ≤ .001, βD = 0.22, 95% CI: − 0.06–0.29, p = .071, and βE = 0.43, 95% CI: 0.27–0.59, p = .004). This pathway suggests that higher minority stress was associated with higher psychological problems, which was not significantly associated with higher substance use; higher levels of substance use was significantly associated with higher HIV sexual risk-taking (overall indirect pathway β = 0.02, 95% CI: 0.01–0.05, p = .056).
Discussion
The current study used structural equation modeling to investigate the association between minority stress and HIV sexual risk-taking, while exploring the mediating role of psychological problems and substance use among GBMSM in Nigeria. Overall, minority stress had a statistically significant positive association with HIV sexual risk-taking. We found that minority stress had a positive association with psychological problems, which was associated with higher HIV sexual risk-taking. Our findings suggest that experiences of minority stress may result in more HIV sexual risk-taking among GBMSM in Nigeria and that relationship may be mediated by psychological problems. This is the first empirical study demonstrating the association between minority stress factors and HIV sexual risk behavior and partial mediation by psychological problems in GBMSM residing in a sub-Saharan African country.
We found that experiences of minority stress (internalized stigma, rejection anticipation, and victimization events) had a significant positive association with HIV sexual risk-taking. This is in line with prior studies that have found minority stress to be associated with HIV sexual risk-taking among MSM in South Africa and the U.S. (Icard et al., 2020; Jeffries, Marks, Lauby, Murrill, & Millett, 2013; Storholm et al., 2019). The direct effect of minority stress on HIV sexual risk-taking was greater than the direct effect of psychological problems and substance use on HIV sexual risk-taking. This finding underscores the importance of considering the effects of prejudices, discrimination, and state-sanctioned homophobic laws on risk of HIV infection among GBMSM in Nigeria and other low and middle income country with similar laws. This highlights the possible individual level effects of unjust and cruel public policy. A study of 174,209 MSM across 38 European countries found that MSM living in countries with higher levels of discriminatory laws—on the basis of sexual orientation—had higher odds of sexual risk-taking, unmet HIV prevention needs, and not using HIV testing services, compared to MSM living in countries with less discriminatory laws (Pachankis et al., 2015). Consequently, it is important that public health researchers and practitioners collaborate with local community-based organizations to devise interventions to help GBMSM in Nigeria engage in active self-preservation, develop coping strategies, and build resiliency, as resilience has been demonstrated to be associated with decreased HIV sexual risk-taking among MSM (Storholm et al., 2019). Specifically, it is also important to explore how the public health research agenda in Nigeria can be informed to collect empirical data that might aid the repeal of the SSMPA. It is important to note that also factors such as HIV prevention and care health service utilization, transactional sex, and online-sex seeking behaviors, amongst other possible factors, may account for the residual effect of minority stress on HIV sexual risk-taking and more studies (particularly longitudinal studies) are needed to elucidate those possible pathways.
The only observed statistically significant mediation pathway was the indirect pathway of minority stress on HIV sexual risk-taking through psychological problems. The strongest effect in the entire model is the association between minority stress and psychological problems. This finding is in line with previous research that has shown experiences of minority stress to be significantly associated with negative mental health outcomes among MSM in the U.S. (Bruce, Harper, & Bauermeister, 2015; Choi, Paul, Ayala, Boylan, & Gregorich, 2013; Wong, Schrager, Holloway, Meyer, & Kipke, 2014). This suggests that the internalization of negative messages and experiences of violence and prejudice—due to one’s sexual minority status—can lead to a state of stress, which has negative consequences for the psychological health of GBMSM, especially in a hostile environment such as Nigeria. This can influence sexual risk behaviors that might put GBMSM in Nigeria at heightened risk of HIV infection. Consequently, it is important to develop mental health interventions that are tailored to the unique circumstances and experiences of GBMSM in Nigeria and other countries with similar punitive laws. These interventions should be developed and implemented in conjunction with local community-based organizations and should not be mere adaptation of programs demonstrated to be effective in western countries. On a structural level, there is a need for more trained mental health providers in the healthcare workforce in Nigeria, a country which has only 200 licensed psychiatrists to its population of over 170 million (Gureje et al., 2015). Additionally, provision of mental health services has the potential to influence HIV sexual risk-taking among this vulnerable population. Specifically, it might increase uptake of innovative HIV prevention strategies, such as HIV pre-exposure prophylaxis, which has been demonstrated to be acceptable among MSM in various African countries including Nigeria (Ogunbajo et al., 2019b, 2020c, d).
Substance use was significantly and directly associated with HIV sexual risk-taking. This finding is consistent with existing literature that has found alcohol dependence and substance use to be associated with elevated sexual risk-taking among MSM both in the U.S. and Nigeria (McCarty-Caplan, Jantz, & Swartz, 2014; Ogunbajo et al., 2020d; Vosburgh et al., 2012). This finding underscores the need for substance use cessation programs that are tailored to the types of substance utilized by Nigerian GBMSM and the contexts in which substance use behavior is occurring. Conversely, we found that substance use was not a statistically significant mediator of the relationship between minority stress and HIV sexual risk-taking. It is possible that substance use may not be as widely utilized among GBMSM in Nigeria compared to the U.S. and Europe due to price and cultural context in which substance use occurs. Previous studies (Ogunbajo et al., 2019a, b, c, 2020a, b, c, d) have shown that Nigerian GBMSM engage in substance use within the context of risky sexual behaviors which was corroborated by our study, however minority stress was not a significant predictor of substance use. Another possible explanation might be that substance use may not be utilized as a coping strategy for GBMSM experiencing minority stress in Nigeria. Consequently, more research is needed to elucidate the context and motivators of substance use among GBMSM.
Experiencing psychological problems were marginally associated with substance use. These findings align with previous research that have demonstrated an association between substance use and mental health among sexual minority men in Nigeria and the U.S. (Batchelder et al., 2019; Ogunbajo et al., 2019a, 2020d; Reisner et al., 2009). A possible explanation for this observed effect is that GBMSM might be engage in substance use as a coping strategy for minority stress. Consequently, it is important to devise GBMSM-affirming mental health and substance use cessation intervention programs specifically designed by and tailored for GBMSM in Nigeria. These interventions should be rooted in the core tents of community-based participatory research, with transparent and honest collaborations between public health practitioners/researchers, community-based organizations and community members. No known studies have been published on the formulation, implementation, and evaluation of any mental health or substance use cessation intervention among GBMSM in Nigeria and this work is desperately needed.
Our findings should be interpreted in light of several limitations. The cross-sectional nature of the research design precludes us from drawing any conclusions related to causation, especially within the framework of structural equation modeling and path analysis. Also, some of the recreational drugs participants could choose from may not be commonly used in Nigeria, but participants were provided a write-in option. We also recognize that utilizing the number of male sexual partners in the previous 3 months as a measurement of sexual risk is flawed, especially if condoms were utilized with all those partners. In addition, participants were mainly recruited through GBMSM community-based organizations and GBMSM social networks, thus limiting our ability to generalize our findings to GBMSM who do not seek services at these organizations or who are outside of the social networks sampled. However, the sample is comprised of individuals from various different geographical locations, age, ethnic groups, religious affiliation, and socioeconomic status. Also, we did not analyze findings from gay self-identified participants separately from bisexual-identified participants, which is an area for exploration in future research projects. Further, as participants completed assessments with the help of trained research staff, social desirability may have influenced participant responses.
Conclusion
This is among the first known studies to investigate the relationship between minority stress, psychological problems, substance use, and HIV sexual risk-taking among Nigerian GBMSM. Overall, minority stress had a statistically significant positive association with HIV sexual risk-taking. We also found that psychological problems mediated the relationship between minority stress and HIV sexual risk-taking. Given the associations between minority stress, psychological problems, substance use, and HIV sexual risk-taking, it is critical to further investigate the potentially long-term detrimental mental, physical and chronic health effects they may have on GBMSM in Nigeria. Specifically, there is a need for longitudinal, cohort studies to investigate possible causal pathways through which these factors negatively impact the health and wellness of this vulnerable population. Interventions that aim to address to improve mental health as well as reduce substance use and HIV sexual risk-taking among this group are needed.
References
Batchelder, A. W., Choi, K., Dale, S. K., Pierre-Louis, C., Sweek, E. W., Ironson, G., et al. (2019). Effects of syndemic psychiatric diagnoses on health indicators in men who have sex with men. Health Psychology, 38(6), 509–517.
Brown, T. A. (2014). Confirmatory factor analysis for applied research. New York: Guilford Publications.
Bruce, D., Harper, G. W., & Bauermeister, J. A. (2015). Minority stress, positive identity development, and depressive symptoms: Implications for resilience among sexual minority male youth. Psychology of Sexual Orientation and Gender Diversity, 2(3), 287–296.
Bush, K., Kivlahan, D. R., McDonell, M. B., Fihn, S. D., & Bradley, K. A. (1998). The AUDIT alcohol consumption questions (AUDIT-C): An effective brief screening test for problem drinking. Archives of Internal Medicine, 158(16), 1789–1795.
Celentano, D. D., Valleroy, L. A., Sifakis, F., MacKellar, D. A., Hylton, J., Thiede, H., et al. (2006). Associations between substance use and sexual risk among very young men who have sex with men. Sexually Transmitted Diseases, 33(4), 265–271.
Choi, K.-H., Paul, J., Ayala, G., Boylan, R., & Gregorich, S. E. (2013). Experiences of discrimination and their impact on the mental health among African American, Asian and Pacific Islander, and Latino men who have sex with men. American Journal of Public Health, 103(5), 868–874.
Eaton, W. W., Smith, C., Ybarra, M., Muntaner, C., & Tien, A. (2004). Center for Epidemiologic Studies Depression Scale: Review and revision (CESD and CESD-R). In M. E. Maruish (Ed.), The use of psychological testing for treatment planning and outcomes assessment: Instruments for adults (Vol. 1, pp. 363–377). Lawrence Erlbaum Associates Publishers.
Eluwa, G. I., Adebajo, S. B., Eluwa, T., Ogbanufe, O., Ilesanmi, O., & Nzelu, C. (2019). Rising HIV prevalence among men who have sex with men in Nigeria: A trend analysis. BMC Public Health, 19(1), 1201. https://doi.org/10.1186/s12889-019-7540-4.
English, D., Rendina, H. J., & Parsons, J. T. (2018). The effects of intersecting stigma: A longitudinal examination of minority stress, mental health, and substance use among Black, Latino, and multiracial gay and bisexual men. Psychology of Violence, 8(6), 669–679.
Fingerhut, A. W., Peplau, L. A., & Gable, S. L. (2010). Identity, minority stress and psychological well-being among gay men and lesbians. Psychology and Sexuality, 1(2), 101–114.
Frost, D. M., Lehavot, K., & Meyer, I. H. (2015). Minority stress and physical health among sexual minority individuals. Journal of Behavioral Medicine, 38(1), 1–8.
Green, K. E., & Feinstein, B. A. (2012). Substance use in lesbian, gay, and bisexual populations: An update on empirical research and implications for treatment. Psychology of Addictive Behaviors, 26(2), 265–278.
Gureje, O., Abdulmalik, J., Kola, L., Musa, E., Yasamy, M. T., & Adebayo, K. (2015). Integrating mental health into primary care in Nigeria: Report of a demonstration project using the mental health gap action programme intervention guide. BMC Health Services Research, 15(1), 1–8. https://doi.org/10.1186/s12913-015-0911-3.
Hatzenbuehler, M. L., Nolen-Hoeksema, S., & Erickson, S. J. (2008). Minority stress predictors of HIV risk behavior, substance use, and depressive symptoms: Results from a prospective study of bereaved gay men. Health Psychology, 27(4), 455–462.
Icard, L. D., Zhang, J., Jemmott, J. B., Sandfort, T. G., Rutledge, S. E., Van Greunen, D., & Martinez, O. (2020). The effects of three types of sexual orientation victimization on HIV sexual risk behavior among black south African men who have sex with men (MSM). Journal of Homosexuality, 67, 513–527.
Jeffries, W. L., Marks, G., Lauby, J., Murrill, C. S., & Millett, G. A. (2013). Homophobia is associated with sexual behavior that increases risk of acquiring and transmitting HIV infection among black men who have sex with men. AIDS and Behavior, 17(4), 1442–1453.
Korhonen, C., Kimani, M., Wahome, E., Otieno, F., Okall, D., Bailey, R. C., et al. (2018). Depressive symptoms and problematic alcohol and other substance use in 1476 gay, bisexual, and other MSM at three research sites in Kenya. AIDS, 32(11), 1507–1515.
Lewis, R. J., Derlega, V. J., Griffin, J. L., & Krowinski, A. C. (2003). Stressors for gay men and lesbians: Life stress, gay-related stress, stigma consciousness, and depressive symptoms. Journal of Social and Clinical Psychology, 22(6), 716–729.
Marsh, H. W., Hau, K.-T., & Wen, Z. (2004). In search of golden rules: Comment on hypothesis-testing approaches to setting cutoff values for fit indexes and dangers in overgeneralizing Hu and Bentler’s (1999) findings. Structural Equation Modeling, 11(3), 320–341.
McAdams-Mahmoud, A., Stephenson, R., Rentsch, C., Cooper, H., Arriola, K. J., Jobson, G., et al. (2014). Minority stress in the lives of men who have sex with men in Cape Town, South Africa. Journal of Homosexuality, 61(6), 847–867.
McCarty-Caplan, D., Jantz, I., & Swartz, J. (2014). MSM and drug use: A latent class analysis of drug use and related sexual risk behaviors. AIDS and Behavior, 18(7), 1339–1351.
Meyer, I. H. (1995). Minority stress and mental health in gay men. Journal of Health and Social Behavior, 36, 38–56.
Meyer, I. H. (2003). Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence. Psychological Bulletin, 129(5), 674–697.
Muthén, B. (2011). Applications of causally defined direct and indirect effects in mediation analysis using SEM in Mplus. Los Angeles: Citeseer.
Newcomb, M. E., & Mustanski, B. (2011). Moderators of the relationship between internalized homophobia and risky sexual behavior in men who have sex with men: A meta-analysis. Archives of Sexual Behavior, 40(1), 189–199.
Oginni, O. A., Mapayi, B. M., Afolabi, O. T., Ebuenyi, I. D., Akinsulore, A., & Mosaku, K. S. (2019). Association between risky sexual behavior and a psychosocial syndemic among Nigerian men who have sex with men. Journal of Gay and Lesbian Mental Health, 23(2), 168–185.
Oginni, O. A., Mapayi, B. M., Afolabi, O. T., Obiajunwa, C., & Oloniniyi, I. O. (2020). Internalized homophobia, coping, and quality of life among Nigerian gay and bisexual men. Journal of Homosexuality, 67, 1447–1470.
Oginni, O. A., Mosaku, K. S., Mapayi, B. M., Akinsulore, A., & Afolabi, T. O. (2018). Depression and associated factors among gay and heterosexual male university students in Nigeria. Archives of Sexual Behavior, 47(4), 1119–1132.
Ogunbajo, A., Anyamele, C., Restar, A. J., Dolezal, C., & Sandfort, T. G. (2019a). Substance use and depression among recently migrated African gay and bisexual men living in the United States. Journal of Immigrant and Minority Health, 21(6), 1224–1232.
Ogunbajo, A., Iwuagwu, S., Williams, R., Biello, K. B., Kahler, C. W., Sandfort, T., & Mimiaga, M. J. (2020a). Validation of depressive symptoms, social support, and minority stress scales among gay, bisexual, and other men who have with men (GBMSM) in Nigeria, Africa: A mixed methods approach. BMC Public Health, 20, 1–12. https://doi.org/10.1186/s12889-020-09127-0.
Ogunbajo, A., Iwuagwu, S., Williams, R., Biello, K. B., Kahler, C. W., Sandfort, T. G., & Mimiaga, M. J. (2020b). Experiences of minority stress among gay, bisexual, and other men who have sex with men (GBMSM) in Nigeria, Africa: The intersection of mental health, substance use, and HIV sexual risk behavior. Global Public Health, 20. https://doi.org/10.1080/17441692.2020.1834598.
Ogunbajo, A., Iwuagwu, S., Williams, R., Biello, K., & Mimiaga, M. J. (2019b). Awareness, willingness to use, and history of HIV PrEP use among gay, bisexual, and other men who have sex with men in Nigeria. PLoS ONE, 14(12), e0226384.
Ogunbajo, A., Kang, A., Shangani, S., Wade, R. M., Onyango, D. P., Odero, W. W., & Harper, G. W. (2019c). Awareness and acceptability of pre-exposure prophylaxis (PrEP) among gay, bisexual and other men who have sex with men (GBMSM) in Kenya. AIDS Care, 31, 1185–1192.
Ogunbajo, A., Leblanc, N. M., Kushwaha, S., Boakye, F., Hanson, S., Smith, M. D., & Nelson, L. E. (2020c). Knowledge and acceptability of HIV pre-exposure prophylaxis (PrEP) among men who have sex with men (MSM) in Ghana. AIDS Care, 32, 330–336.
Ogunbajo, A., Oke, T., Jin, H., Rashidi, W., Iwuagwu, S., Harper, G. W., et al. (2020d). A syndemic of psychosocial health problems is associated with increased HIV sexual risk among Nigerian gay, bisexual, and other men who have sex with men (GBMSM). AIDS Care, 32, 337–343.
Okanlawon, K. (2018). Cultures of public intervention regarding LGBTQ issues after Nigeria’s same-sex marriage prohibition act (SSMPA). College Literature, 45(4), 641–651.
Pachankis, J. E., Hatzenbuehler, M. L., Hickson, F., Weatherburn, P., Berg, R. C., Marcus, U., & Schmidt, A. J. (2015). Hidden from health: Structural stigma, sexual orientation concealment, and HIV across 38 countries in the European MSM internet survey. AIDS, 29(10), 1239–1246.
Ramirez-Valles, J., Garcia, D., Campbell, R. T., Diaz, R. M., & Heckathorn, D. D. (2008). HIV infection, sexual risk behavior, and substance use among Latino gay and bisexual men and transgender persons. American Journal of Public Health, 98(6), 1036–1042.
Reisner, S. L., Mimiaga, M. J., Skeer, M., Bright, D., Cranston, K., Isenberg, D., et al. (2009). Clinically significant depressive symptoms as a risk factor for HIV infection among black MSM in Massachusetts. AIDS and Behavior, 13(4), 798–810.
Rendina, H. J., Gamarel, K. E., Pachankis, J. E., Ventuneac, A., Grov, C., & Parsons, J. T. (2017). Extending the minority stress model to incorporate HIV-positive gay and bisexual men’s experiences: A longitudinal examination of mental health and sexual risk behavior. Annals of Behavioral Medicine, 51(2), 147–158.
Spitzer, R. L., Kroenke, K., Williams, J. B., & Löwe, B. (2006). A brief measure for assessing generalized anxiety disorder: the GAD-7. Archives of Internal Medicine, 166(10), 1092–1097.
Storholm, E. D., Huang, W., Siconolfi, D. E., Pollack, L. M., Carrico, A. W., Vincent, W., et al. (2019). Sources of resilience as mediators of the effect of minority stress on stimulant use and sexual risk behavior among young black men who have sex with men. AIDS and Behavior, 23(12), 3384–3395.
TIERS. (2019). Report on human rights violations based on real or perceived sexual orientation and gender identity in Nigeria (Vol. 4, pp. 1–37). The Initiative for Equal Rights Publications.
Tucker-Seeley, R. D., Mitchell, J. A., Shires, D. A., & Modlin, C. S. (2015). Financial hardship, unmet medical need, and health self-efficacy among African American men. Health Education and Behavior, 42(3), 285–292.
UNAIDS. (2017). UNAIDS Data 2017 (Vol. 1, No. 1, pp. 1–323). UNAIDS Publications.
Vosburgh, H. W., Mansergh, G., Sullivan, P. S., & Purcell, D. W. (2012). A review of the literature on event-level substance use and sexual risk behavior among men who have sex with men. AIDS and Behavior, 16(6), 1394–1410.
Vu, L., Adebajo, S., Tun, W., Sheehy, M., Karlyn, A., Njab, J., et al. (2013). High HIV prevalence among men who have sex with men in Nigeria: Implications for combination prevention. JAIDS Journal of Acquired Immune Deficiency Syndromes, 63(2), 221–227.
Wong, C. F., Schrager, S. M., Holloway, I. W., Meyer, I. H., & Kipke, M. D. (2014). Minority stress experiences and psychological well-being: The impact of support from and connection to social networks within the Los Angeles house and ball communities. Prevention Science, 15(1), 44–55.
Wong, C. F., Weiss, G., Ayala, G., & Kipke, M. D. (2010). Harassment, discrimination, violence, and illicit drug use among young men who have sex with men. AIDS Education and Prevention, 22(4), 286–298.
Acknowledgements
We will like to thank all the participants of the study for their time and efforts. We would also like to thank the staff at Centre for Right to Health (Abuja) Equality Triangle Initiative (Delta), Improved Sexual Health and Rights Advocacy Initiative (ISHRAI, Lagos) and Hope Alive Health Awareness Initiative (Plateau). We also extend our gratitude to Olubiyi Oludipe (ISHRAI), Bala Mohammed Salisu (Hope Alive Health Awareness Initiative), Chucks Onuoha, Prince Bethel, Eke Chukwudi, Tochukwu Okereke, Josiah Djagvidi, Victor Brownson, and Odi Iorfa Agev, for providing logistical support to the Project.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
This study was supported by a R36 dissertation grant from the National Institute on Drug Abuse [DA047216] (principal investigator [PI]: Adedotun Ogunbajo) and by the Robert Wood Johnson Foundation Health Policy Research Scholars Program, for which the first author is a scholar but the foundation did not provide direct Project support.
Ethical Approval
The study protocols were approved by the institutional review boards at Brown University and the Nigerian Institute of Medical Research.
Informed Consent
Each participant provided verbal informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ogunbajo, A., Iwuagwu, S., Williams, R. et al. Psychological Problems Mediate the Relationship Between Minority Stress and HIV Sexual Risk Among Nigerian Men Who Have Sex with Men: Testing the Minority Stress Model. Arch Sex Behav 50, 3163–3174 (2021). https://doi.org/10.1007/s10508-021-01943-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10508-021-01943-8