Abstract
Transgender female sex workers (TFSW) are highly affected by HIV, with a global prevalence of 27%. HIV self-testing (HIVST) to screen sexual partners has helped men who have sex with men and female sex workers make informed sexual decisions and avoid HIV exposure. This is the first report on TFSW’s experiences screening clients using HIVST. Ten TFSW were each given ten HIVST kits and returned after 3 months to complete an online questionnaire and undergo an interview. Eight of them reported using HIVST with potential partners. Among fifty potential partners who were asked in person to test, 42 (84%) were clients. Thirty-four out of fifty (68%) accepted and 16 (32%) refused. Very few violent incidents occurred, and participants felt empowered by offering HIVST to others. Nevertheless, HIVST market cost was prohibitive for future use. HIVST use with clients could be feasible for TFSW if the cost were lowered or subsidized.
Resumen
Globalmente, las trabajadoras sexuales transgéneros (TSTG) tienen un 27% de prevalencia VIH. El uso del autotest para VIH (HIVST) para examinar a parejas sexuales ha ayudado a los hombres que tienen relaciones sexuales con hombres y a las mujeres trabajadoras sexuales a tomar decisiones informadas sobre las relaciones sexuales y evitar exponerse al VIH. Éste es el primer reporte sobre las experiencias que tuvieron TSTG usando el HIVST para examinar a sus clientes. Diez TSTG recibieron diez equipos de prueba de HIVST cada una y regresaron después de tres meses para completar un cuestionario por Internet y ser entrevistadas. Ocho de ellas reportaron haber usado HIVST con posibles compañeros sexuales. De los cincuenta posibles compañeros sexuales que fueron invitados en persona a usar la prueba, 42 (84%) eran clientes. Treinta y cuatro de los cincuenta (68%) aceptaron usar la prueba y 16 (32%) se negaron. Hubo muy pocos incidentes de violencia, y las participantes se sintieron empoderadas al ofrecer HIVST a los demás. Sin embargo, las TSTG encontraron que el precio comercial del HIVST es una barrera para el uso futuro. El uso del HIVST con clientes podría ser factible para las TSTG si el costo fuera más bajo o fuera subvencionado.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Transgender female sex workers (TFSW) represent one of the populations most affected by HIV, with an estimated global prevalence of 27.3% [1,2,3,4,5]. Among TFSW, external factors such as limited coverage of healthcare services, criminalization of sex work, and competing priorities (e.g., securing stable housing and income), in addition to subjective factors such as discrimination, stigma, and mistrust of the healthcare system, all serve as primary barriers to accessing HIV prevention and testing services [6,7,8,9,10,11,12,13,14,15]. Therefore, targeted HIV prevention interventions to reduce TFSW’s risk of contracting or transmitting HIV, including increasing access to HIV testing, could prove beneficial [1, 14].
An emerging strategy for increasing access to HIV testing, HIV self-testing (HIVST), has been found to be highly acceptable among key populations, including TFSW [16], due to its convenience, privacy, painlessness, and ease of use [17]. Its use is supported by the World Health Organization, particularly for populations such as TFSW who have low healthcare service coverage, are at higher risk for HIV, and may not otherwise have access to HIV testing services [18]. The use of HIVST could also enable TFSW to operate at the margins of a healthcare system they often encounter as hostile. Research on the effects of HIVST found few instances of harm (i.e., suicide, self-harm, or intimate partner violence) attributable to self-testing; instead, HIVST was associated with increased uptake and testing frequency [19,20,21].
Furthermore, studies of the provision of HIVST to at-risk populations to screen sexual partners have demonstrated its feasibility as a risk reduction method that can increase testing rates and help testers avoid HIV exposure. A study in NY with men who have sex with men (MSM) found that participants who were given HIVST kits to screen partners reported that the intervention was acceptable and that they were able to avoid sexual intercourse with partners who had positive results [22]. Additionally, studies of HIVST for partner-testing among cisgender female sex workers (CFSW) showed that they were able to introduce tests to partners, including commercial sex clients, and could to make more informed sexual decisions [23], such as avoiding sex or using condoms in the case of a positive test result [24]. Despite the potential for violent interactions with clients in the context of sex work, studies to date have reported very low rates of violence following the provision of HIVST, ranging from 1-2% of participants [24, 25]. Although TFSW expressed concern in a previous study about hypothetical use of HIVST with clients due to a possible breach of confidentiality in the case of a positive test result and the potential for violent situations [26], no research to date has examined actual use of HIVST with clients among TFSW. This article will report on the experiences of TFSW in Puerto Rico (PR) and New York (NY) who used HIVST kits to screen clients, including strategies for using the test with clients, how they handled challenges such as violent situations or issues with confidentiality, and their likelihood of using HIVST in the future to prevent HIV.
Methods
Sample
The ISUM (I’ll Show You Mine) study was a 5-year, randomized controlled trial in New York, NY and San Juan, PR that explored sexual risk behaviors among a population at high risk of HIV acquisition with access to rapid HIVST kits. Participants were HIV-uninfected, non-monogamous MSM and transgender women who never or seldom used condoms during anal intercourse (insertive and/or receptive). To be eligible, participants could not be taking pre-exposure prophylaxis (PrEP), and had to have reported at least three sexual occasions with a partner of discordant or unknown statust within the last 3 months.
Recruitment
Participants were recruited between 2014 and 2017. A total of 279 participants were enrolled, 22 (8%) of whom were transgender women who reported receiving money, goods, or other services in exchange for sex. A description of recruitment strategies has been previously published [27]. Briefly, participants were recruited in-person, online, and via word-of-mouth through other participants.
Procedures
Participants underwent a prescreen by phone to determine initial eligibility and then came to our office for a screening visit (Visit 1) in which they completed a baseline behavioral questionnaire via computer administered self-interview (CASI), completed rapid HIVST correctly without direction from staff (within two attempts), and were administered a confirmatory test by staff. Those who were eligible based on the questionnaire and the test results were invited to return for the enrollment visit (Visit 2) within 1 week. At the enrollment visit, a block-randomization strategy was used to assign participants to either the intervention group (n = 11 TFSW), in which they were given ten rapid oral HIV test kits to take home and viewed a video that included key points for consideration when using the tests to screen sexual partners or clients (https://www.youtube.com/watch?v=uq6Qb4BJLdM), or to the control group (n = 11 TFSW), in which they were not given tests to take home but were given condoms. During the 3-month study period, participants reported through daily SMS their sexual behavior and (for intervention group participants) the number of HIVST kits they had left; they could request additional kits. A description of the SMS system has been published previously [28]. After 3 months, participants returned for a follow-up visit (Visit 3), in which they completed an HIV test administered by staff and a follow-up CASI. In addition, participants in the intervention group underwent an in-depth interview (IDI, n = 10 TFSW). All procedures were reviewed and approved by the Institutional Review Boards at New York State Psychiatric Institute and the University of Puerto Rico Medical Sciences Campus.
Measures
The quantitative data reported in this manuscript come from the baseline (V1) and follow-up (V3) CASI questionnaires. The baseline included items on demographics and sexual behavior. The follow-up measured perceived ease or difficulty of discussing HIVST with partners; number of times HIVST was used to test self and partners; number of partners asked in person to use HIVST (including clients); ease or difficulty of determining whether a partner could become violent; number of partners who accepted, refused, got angry, or got violent when asked in person to test; frequency of asking partners to test via call, chat or text; and reasons for not discussing HIVST with partners. Given that this study was not designed to examine HIVST use among sex workers specifically, data on clients cannot be disaggregated from that of partners, except where noted.
The qualitative data are reported from the IDI. The IDI was conducted using a guide with open-ended questions and probes, which was developed by our team based on items tested in a prior study of HIVST use with partners. To explore participants’ experiences using the tests with clients, the guide focused on decision-making around testing clients, broaching the topic of the HIVST, client reactions, violent experiences and potential for violence, privacy and confidentiality concerns, and future use of HIVST.
Data Analysis
Given that this manuscript focuses on use of HIVST with clients, the data analysis was limited to the eleven participants in the intervention group (ten of whom returned for a follow-up visit). Frequencies were run on variables of interest from the CASI questionnaires using SPSS statistical program (v25) for data analysis. Percentages, means, and medians (where applicable) are reported. All audio files from IDIs were transcribed and checked for accuracy. A codebook which included code names and definitions was developed based on the IDI guide. The codebook was modified as needed after coding a set of five initial transcripts. Transcripts were loaded into the NVivo v.11 qualitative data analysis program, and each was coded by two independent coders, who subsequently met to discuss discrepancies until reaching consensus. The code for sex work involvement was examined for common themes, and then each transcript was content analyzed thoroughly by the first author to identify other salient themes. Quotes included from participants at the PR site were translated from Spanish to English by the first author. The primary study findings, along with secondary study findings, have been published elsewhere [29,30,31,32,33,34,35,36,37].
Results
Quantitative Findings
Demographics
Participants’ median age was 26 years old, and all were high school or college graduates. A majority self-identified as Hispanic/Latina and half self-identified as Black/African-American. Most self-identified as transgender, and the rest as women. Nearly half self-identified as gay/homosexual, with the rest considering themselves bisexual, heterosexual, or other. Most reported being employed part-time or unemployed, with a median annual income of $1600 (range = $0–$18,000). (See Table 1).
Sexual Behavior
At baseline, the median number of times participants reported receiving money, goods or services in exchange for sex in the 3 months prior was 50 (range = 1–700), with a median of 45 sexual partners and 15 occasions of receptive anal intercourse, most of them condomless (median = 10). (See Table 1)
HIVST Use
Eight of the ten participants reported using the HIVST to test themselves at least once during the study (median = 2.0 times, range = 0–20). Also, eight reported using the HIVST to test at least one potential sexual partner (median = 6.5 times, range = 0–20). Regarding asking partners to test, most reported finding it very easy (N = 4) or fairly easy (N = 2), while some found it fairly hard (N = 4). Six of the ten participants reported asking at least one partner in person to use the kits. Table 2 summarizes the experiences and partner reactions reported by these six participants. In total, they asked 50 partners to use the kits, 42 (84%) of whom were clients (median = 5.0 clients, range = 1–20). Out of those 50 partners, 34 (68%) agreed to test (median = 4.5, range = 0–15) and 16 (32%) refused (median = 1.5, range = 0–8). Four participants reported that a total of sixteen partners (32%) got angry or upset due to the request (median = 3, range = 0–8). Five people reported finding it very easy (N = 1) or fairly easy (N = 4) to judge whether a partner could become violent, while three others found it fairly hard and one very hard. Violent reactions were uncommon, but two participants reported a total of eight partners (16%) who got physically violent due to the request (median = 0, range = 0–7). Finally, one participant reported that four partners disclosed their HIV positive status, and none of the partners who tested received HIV positive results.
Two participants did not ask anyone to test in person, but did report asking potential partners to test via chat, call, or text. The most common reasons given by the eight participants who did not discuss the test with at least one potential partner included feeling the person might react negatively (50%), feeling uncomfortable bringing it up (38%), not wanting to risk ending the encounter (38%), or not having the test kit on hand (38%) (See Table 3).
Qualitative Findings
Decision to Test Clients
Participants’ decisions to propose the HIVST to clients were based on calculations of risk, whether that of the sexual encounter itself or that of possible client reactions. To reduce the risk of the sexual encounter, the HIVST was used as a risk reduction alternative with clients who did not want to use condoms:
They have to do the test with me if they want to be intimate without protection. (ID 058, 21 yo, PR)
However, if an encounter was seen as low risk, based on planned condom use or level of familiarity with the client, they did not feel the need to test:
Because I’ve known him for a long time and I always use condoms [with him], that’s why I didn’t ask him to test. (ID 164, 35 yo, PR)
To reduce the risk of unpleasant interactions, participants used their judgment to avoid introducing HIVST to those who might have bad reactions:
There’s a particular type of attitude that certain people who contact me have. It’s this very sort of aggressive alpha male type of mentality and people who had that type of attitude, I didn’t offer it to… I assumed that they’d say no and further assumed that they might say no in an aggressive, unpleasant way. (ID 190, 24 yo, NY)
Some felt safer asking only clients they already knew, not first-time clients:
If it was someone who I was meeting for the first time, I wouldn’t bring it up with them, because I – even for me, that seems a little uncomfortable. (Participant ID 045, 24 years old, NY)
In sum, the decision whether to propose HIVST to clients required participants to weigh the risk of HIV transmission during the sexual encounter against the risk of an aggressive reaction from a client.
Broaching the Topic of HIVST
Participants developed techniques for broaching the topic of testing to maximize client acceptability of the HIVST and reduce negative reactions by considering timing and context. A few explained to clients that they were in a study and had been given tests to use with others:
I’m like, “You know, I’m a part of this study and I have these HIV kits, so now, you know, you put the Q-tip in your mouth, just simple.” (ID 045, 24 yo, NY)
Many found it easier to introduce the test right at the start of an interaction:
Every time a client comes over, I say, “Come to my bedroom,” I look for the tests and take them out, we go to the bedroom and I say, “Look my dear, I’m going to test you for HIV. All you have to do is open your mouth and I will pass this swab over your gums.” (ID 009, 23 yo, PR)
Others routinely discussed the importance of safe sex with clients, so they incorporated the HIVST into this conversation:
At the point when I was bringing up issues of protection and issues of –and the health issues that could potentially arise … I was like, “Well, I have these kits that I get for free from this study that I’m doing. They take 20 min, and you know really quickly, so that would make you feel more safe.” (ID 190, 24 yo, NY)
Participants found that broaching the topic became easier with time and practice:
The first time, with the first one, it was difficult. But by the second one, it wasn’t. I didn’t have any qualms. (ID 088, 39 yo, PR)
In sum, introducing the HIVST to clients was a matter of practice, but useful techniques included explaining the context of the study, bringing it up at the start of the interaction, and incorporating into routine safe sex conversations.
Client Reactions
Most clients were initially surprised, but overall they reacted well to being asked to take an HIV test:
They were like, “Wow, how do you have this?” It was something really surprising to them. (ID 095, 37 yo, PR)
Even some who initially refused often changed their minds as they considered the test:
They refused, but then they said, “OK, I’ll do it, I don’t have a choice, now I’m dying to know.” (ID 058, 21 yo, PR)
However, some did refuse to test. A few became suspicious, asking participants if they had HIV:
The first thing they’re going to think is, “She has something. She has HIV.”…I had to start by telling them that this had nothing to do with my personal character. (ID 088, 39 yo, PR)
Others were simply disinterested or did not want to wait 20 min for the result:
Some people I offered it to said no, that we could use a condom, and let’s go because it’s late. (ID 164, 35 yo, PR)
Finally, a few became angry, but subsequently calmed down:
I was surprised that some of them who I knew already, when I brought it up, they started to get angry…I am such a calm person that I know how to say things so that they are not misinterpreted…so I didn’t have any problems. (ID 095, 37 yo, PR)
In sum, participants described a variety of client reactions, ranging from surprise to curiosity, from suspicion or impatience to anger. Nevertheless, a majority of those who were asked to test agreed, and participants were able to handle a range of client reactions skillfully.
Violent Experiences and the Potential for Violence
Violent experiences were not very common, although they did occur. Whether or not participants’ clients reacted violently, all TFSW interviewed recognized the potential for violence and had a plan for dealing with it if it did occur. Only one participant described in the interview a violent interaction when proposing the test to a client after he offered her more money if she agreed not to use condoms:
I asked him if he wanted to do the OraQuick test with me, and he got violent. He threw the kits on the floor and he said…why the hell would he want to do that test, why the hell did I bring those tests… he grabbed my arm and dragged me… I left, grabbed the two kits… it was hard to leave because he didn’t want me to leave and he said, “I paid you and you came here to fulfill my fantasy, and we’re doing it without a condom right now,” but I was able to get around him and leave. (ID 058, 21 yo, PR)
Participants described that working on the streets could lead TFSW to interact with a variety of personalities, and they recognized the potential for violence:
It’s concerning because some women who work on the streets doing sex work are exposed to many crazy people. They aren’t very selective. And sometimes the streets are very tough, it’s bad, they leave with any crazy person, and just imagine proposing the test. (ID 083, 32 yo, PR)
Nevertheless, participants offered recommendations for avoiding violent situations, such as:
Do it somewhere – not, like, in public, but like, if you’re working out of a hotel, I would say do it in a setting like that. Somewhere where you can be assisted. (ID 045, 24 yo, NY)
If the partner is using [drugs or alcohol], there is a greater likelihood of some kind of violence if test use is proposed. (ID 083, 32 yo, PR)
A few mentioned that people in their line of work are used to dealing with all types of situations. One stated she felt confident she could handle any situation:
They know they’re going to get it when they try to kill me or something. I’m violent too, and I don’t hit like a girl. (ID 009, 23 yo, PR)
In sum, TFSW were aware of the potential for violence when proposing HIVST use to clients, but had strategies for avoiding such situations or handling them effectively if they occurred.
Privacy and Confidentiality Concerns When Testing with Clients
Given the potential for privacy concerns and breach of confidentiality when testing oneself for HIV with another person, participants were asked whether they tested themselves in front of clients. Four reported testing themselves in front of a client at least once. One stated that this helped her clients feel more comfortable:
I did one myself so that they would feel they could trust me, and so they would say “well, she is going to do it, so I will do it too.” So, I did it with them and I told them step-by-step how to test themselves. (ID 058, 21 yo, PR)
Among those who tested themselves in front of clients, none mentioned feeling concerned about a possible breach of confidentiality if clients were to see a positive result, as they were confident in their negative status. However, one participant believed that her client refused to test because he did not want her to see the result:
I’m not his girlfriend or his wife… we just have business together… maybe that’s something he might want to conquer on his own. (ID 045, 24 yo, NY)
While privacy was not a big concern in this sample, participants recognized that it could influence clients’ acceptability of the HIVST in the context of sex work.
Empowerment
Seven of those interviewed described feeling empowered by using the HIVST with clients. They felt they were in a position of authority since they could administer the tests for others:
If I have the test…like, someone depends on you. So, it’s like, if you find out someone’s positive by doing an at-home test, it’s like, then this person kind of looks to you for comfort. And then if you find out it’s negative, it’s still, like, you know, that suspense and they still kind of depend on you throughout. (ID 045, 24 yo, NY)
This dynamic allowed TFSW to educate clients about the importance of HIV testing and the availability of an oral HIVST:
It’s learning to be aware of it, if they didn’t know about it or they didn’t know how to protect themselves. And at least with a test like this… well, some people thought it had to be with a syringe, taking a blood sample. (ID 083, 32 yo, PR)
Having the kits enabled them to build awareness among clients that they, too, are at risk for HIV:
It was a new experience for me to be able to tell them, “Look, you should do the test,” because as transsexuals and sex workers, they always tell us, “No, you have to take care of yourself, I have to be careful because of what you do.” It’s like they blame us and point fingers at us, and this allowed me to show them that, no, this is an issue for everyone. (ID 095, 37 yo, PR)
In addition, having HIVST led some to feel that their status was elevated before clients:
They were like, “Oh, this is so professional.”… It made people think that I was less desperate, for lack of a better word. Beggars can’t be choosers, and because I was doing something to allow me to choose, it meant that it reduced my perception as a beggar in their minds. (ID 190, 24 yo, NY)
Overall, possession of the HIVST kits empowered TFSW to take control of testing and to educate their clients about HIV risk.
Future Use of HIVST
Those who used the tests with clients liked the idea of continuing to use them in the future, and HIVST use to screen clients was seen as a good option for the TFSW community. As one participant stated:
In the case of the trans community, it’s clear, once they have this information, once you tell them that this is here, that they can come get tests, I think that they are going to use them and they are going to approach their clients. Because most of them are going to feel empowered, like, “Yes, they prepared me to do this test, and I have it in my purse, I have it at home, whatever. When my clients come, I am going to use it.” (ID 088, 39 yo, PR)
Nevertheless, price was a significant concern for all of them, particularly those with a large volume of clients:
If I have ten clients lined up, at $40 per test, that’s $400! (ID 045, 24 yo, NY)
Most felt that they could pay up to around $10 per test, and that anything more would be too much of a financial burden:
I’m not going to pay for a test if it means I can’t buy food. (ID 088, 39 yo, PR)
Still, one participant recognized the possibility of passing the cost to the client:
I can improve my business because I can charge a little more just for doing the test. (ID 009, 23 yo, PR)
In sum, participants liked the idea of continuing to use HIVST for prevention; nevertheless, market cost was prohibitive and strategies to reduce or mitigate the cost would be necessary for future use.
Discussion
This study demonstrated that the use of the HIVST to screen clients was feasible and acceptable among a sample of TFSW in NY and PR who reported rarely using condoms. A majority of participants who were given the HIVST kits were able to propose the tests to clients. For the most part, participants were able to determine whom they could approach and how to broach the topic safely. Although a few potential partners became angry or acted violently, most had favorable reactions and eventually agreed to test, despite initial surprise or refusal.
In a prior study, a similar sample presented with the hypothetical possibility of using HIVST with clients reported concerns about privacy and confidentiality of HIVST with clients [26]. Yet, in this sample even those who tested themselves in front of clients were unconcerned. It is possible that having access to the test kits, which they could use to test themselves as frequently as necessary, alleviated their concerns about their own HIV status. These findings are consistent with those of several other studies that point to privacy and confidentiality as primary benefits of HIVST use [38,39,40,41,42,43]. In particular, transgender women may associate clinic-based testing with stigma and lack of privacy [38, 41], and possession of the HIVST may increase their sense of control over the testing process [39].
Another concern mentioned by participants in our previous study was the potential for violence. Fortunately, this sample reported very few instances of violence, which is consistent with findings from the overall study sample [30]. Participants recognized that proposing HIVST use with clients could lead to violent situations. Nevertheless, most felt prepared, by virtue of the nature of sex work, to handle such instances when they occurred. They had several strategies for minimizing the likelihood of violence, such as only testing familiar clients, using the test in a public place where help could be readily available, and avoiding proposing the tests to clients who had consumed alcohol or drugs. Similar strategies have been reported by CFSW when presenting HIVST to clients [23].
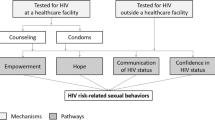
During the interviews, participants also spontaneously articulated a sense of empowerment when using HIVST with clients. Other studies have found empowerment to be a benefit of using HIVST [38, 42,43,44]. In one study, transgender women reported feeling empowered by the use of HIVST as it gave them a level of control over testing and status awareness, particularly in the context of stigmatized clinical interactions and unequal power dynamics in personal relationships [38]. Among sex workers, research has also found increased levels of personal confidence through participation in HIV-prevention peer education programs which allow them to take on the role of experts in their communities and increase skills for workplace autonomy and negotiation [45, 46]. Although this study was not designed as a peer education program, participants in the intervention arm were taught how to use the HIVST and given a chance to self-administer the test. They were also shown a video at enrollment with vignettes collected from participants in a prior study of HIVST with partners, discussing scenarios they had encountered when using the tests, one of whom was a TFSW. These findings on empowerment via HIVST use and HIV-prevention peer education programs, coupled with our findings on TFSW’s sense of empowerment when using HIVST as an HIV-prevention method with clients, merit continued research to evaluate best practices for building TFSW’s confidence and skills around using HIVST as a tool for HIV prevention with clients.
Finally, most participants reported that, while they would like to continue using the HIVST to screen clients, cost was a significant prohibitive factor. Although the test is available for sale over-the-counter in drug stores and pharmacies in both NY and PR for approximately $40USD, this is clearly too expensive for regular use by TFSW, who may have a high volume of clients for whom they would need tests. Research has shown that cost is a significant barrier to HIVST use [38,39,40,41,42,43], particularly since those with the highest prevalence of undiagnosed HIV are often those with the lowest socioeconomic status [40]. Studies that have assessed willingness to pay for HIVST kits among populations at risk for HIV have widely demonstrated that a majority cannot pay more than $10–$20 per test kit [17, 38, 43], which is consistent with our findings.
Policies that facilitate test kit subsidization and convenient methods of test kit distribution could mitigate the cost and increase uptake of HIVST by TFSW, given that our study demonstrated that TFSW are willing and able to use the HIVST with clients. Studies have offered numerous ideas for convenient and/or low cost test kit distribution including: offering free self-tests at health departments or community organizations [39], making them available at pharmacies without interaction with a pharmacist [40], sale through vending machines (401), home delivery via mail [40], offering HIVST through private and public insurance programs [40], and packaging kits in pairs to allow a single purchase to cover two partners [38] Because participants in our study informed their clients of the test’s availability and taught them how to use it, policies of this sort could deliver benefits to both groups at risk for HIV, TFSW and their clients.
Limitations
This study had some limitations. First, the study was not designed specifically to evaluate the use of the kits among sex workers; therefore, attitudes towards the use of kits with clients was not systematically assessed in the questionnaires. Second, although we were able to recruit a sample of twenty-two TFSW between two study sites, due to the study design only eleven of them, those in the intervention arm, were given test kits to use with clients during the study; thus, our small sample does not provide generalizable data. Nevertheless, we were able to gather valuable information from the first TFSW to use the HIVST as an HIV prevention tool and demonstrate its feasibility, acceptability, potential for scale-up, and limitations.
Conclusions
TFSW were willing and able to use HIVST to screen clients, and overall favorable reactions by clients led to expanded access to testing in populations that may be unaware of their status and less likely to be reached by traditional HIV testing outreach. As such, this HIV prevention strategy merits future study to determine its expanded feasibility and acceptability, to develop guidelines for effective and safe use among TFSW and their clients, and to inform policies that can mitigate cost and facilitate convenient HIVST distribution.
References
Operario D, Soma T, Underhill K. Sex work and HIV status among transgender women: systematic review and meta-analysis. JAIDS. 2008;48:97–103.
Baral SD, Poteat T, Stromdahl S, Wirtz AL, Guadamuz TE, Beyrer C. Worldwide burden of HIV in transgender women: a systematic review and meta-analysis. Lancet Infect Dis. 2013;13:214–22.
dos Ramos Farías MS, Garcia MN, Reynaga E, et al. First report on sexually transmitted infections among trans (male to female transvestites, transsexuals, or transgender) and male sex workers in Argentina: high HIV, HPV, HBV, and syphilis prevalence. Int J Infect Dis. 2011;15:e635–40.
Silva-Santisteban A, Raymond HF, Salazar X, et al. Understanding the HIV/AIDS epidemic in transgender women of Lima, Peru: results from a sero-epidemiologic study using respondent driven sampling. AIDS Behav. 2012;16:872–81.
Silva-Santisteban A, Eng S, de la Iglesia G, Falistocco C, Mazin R. HIV prevention among transgender women in Latin America: implementation, gaps and challenges. J Int AIDS Soc. 2016;19:20799.
Shannon K, Strathdee SA, Shoveller J, Rusch M, Kerr T, Tyndall MW. Structural and environmental barriers to condom use negotiation with clients among female sex workers: implications for HIV-prevention strategies and policy. Am J Public Health. 2009;99:659–65.
Budhwani H, Hearld KR, Hasbun J, et al. Transgender female sex workers’ HIV knowledge, experienced stigma, and condom use in the Dominican Republic. PLoS ONE. 2017;12:e0186457.
Wood SM, Lee S, Barg FK, Castillo M, Dowshen N. Young transgender women’s attitudes toward HIV pre-exposure prophylaxis. J Adolesc Health. 2017;60:549–55.
Zalazar V, Arístegui I, Kerr T, et al. High willingness to use HIV pre-exposure prophylaxis among transgender women in Argentina. Transgend Health. 2016;1:266–73.
Beyrer C, Crago AL, Bekker LG, et al. An action agenda for HIV and sex workers. Lancet. 2015;385:287–301.
Poteat T, Wirtz AL, Radix A, et al. HIV risk and preventive interventions in transgender women sex workers. Lancet. 2015;385:274–86.
Scorgie F, Nakato D, Harper E, et al. ‘We are despised in the hospitals’: sex workers’ experiences of accessing health care in four African countries. Cult Health Sex. 2013;15:450–65.
Beattie TS, Bhattacharjee P, Suresh M, Isac S, Ramesh BM, Moses S. Personal, interpersonal and structural challenges to accessing HIV testing, treatment and care services among female sex workers, men who have sex with men and transgenders in Karnataka state, South India. J Epidemiol Commun Health. 2012;66(2):242–8.
Schulden JD, Song B, Barros A, et al. Rapid HIV testing in transgender communities by community-based organizations in three cities. Public Health Rep. 2008;123:101–14.
Bockting WO, Robinson BE, Rosser BR. Transgender HIV prevention: a qualitative needs assessment. AIDS Care. 1998;10:505–25.
Pal K, Ngin C, Tuot S, et al. Acceptability study on HIV self-testing among transgender women, men who have sex with men, and female entertainment workers in Cambodia: a qualitative analysis. PLoS ONE. 2016;11:e0166129.
Figueroa C, Johnson C, Verster A, Baggaley R. Attitudes and acceptability on HIV self-testing among key populations: a literature review. AIDS Behav. 2015;19:1949–65.
World Health Organization. Guidelines on HIV self-testing and partner notification. 2016. http://apps.who.int/iris/bitstream/10665/251655/1/9789241549868-eng.pdf?ua=1. Accessed 13 March 2019.
Johnson CC, Kennedy C, Fonner V, et al. Examining the effects of HIV self-testing compared to standard HIV testing services: a systematic review and meta-analysis. J Int AIDS Soc. 2017;20:21594.
Kelvin EA, George G, Mwai E, et al. A randomized controlled trial to increase HIV testing demand among female sex Workers in Kenya through Announcing the availability of HIV self-testing via text message. AIDS Behav. 2019;23:116–25.
Veronese V, Oo ZM, Thein ZW, et al. Acceptability of peer-delivered HIV testing and counselling among men who have sex with men (MSM) and transgender women (TW) in Myanmar. AIDS Behav. 2018;22:2426–34.
Carballo-Diéguez A, Frasca T, Balan I, Ibitoye M, Dolezal C. Use of a rapid HIV home test prevents HIV exposure in a high risk sample of men who have sex with men. AIDS Behav. 2012;16:1753–60.
Maman S, Murray KR, Mavedzenge SN, et al. A qualitative study of secondary distribution of HIV self-test kits by female sex workers in Kenya. PLoS ONE. 2017;12:e0174629.
Thirumurthy H, Masters SH, Mavedzenge SN, Maman S, Omanga E, Agot K. Promoting male partner HIV testing and safer sexual decision making through secondary distribution of self-tests by HIV-negative female sex workers and women receiving antenatal and post-partum care in Kenya: a cohort study. Lancet HIV. 2016;3:e266–74.
Ortblad K, Musoke DK, Ngabirano T, et al. Direct provision versus facility collection of HIV self-tests among female sex workers in Uganda: a cluster-randomized controlled health systems trial. PLoS Med. 2017;14:e1002458.
Giguere R, Frasca T, Dolezal C, Febo I, Cranston RD, Mayer K, McGowan I, Carballo-Diéguez A. Acceptability of three novel HIV prevention methods among young male and transgender female sex workers in Puerto Rico. AIDS Behav. 2016;20(10):2192–202.
Iribarren SJ, Ghazzawi A, Sheinfil AZ, Frasca T, Brown W, Lopez-Rios J, Rael CT, Balán IC, Crespo R, Dolezal C, Giguere R. Mixed-method evaluation of social media-based tools and traditional strategies to recruit high-risk and hard-to-reach populations into an HIV prevention intervention study. AIDS Behav. 2018;22(1):347–57.
Brown W 3rd, Sheinfil A, Lopez-Rios J, Giguere R, Dolezal C, Frasca T, Lentz C, Balán IC, Rael C, Cruz Torres C, Crespo R, Febo I, Carballo-Diéguez A. Methods, system errors, and demographic differences in participant errors using daily text message-based short message service computer-assisted self-interview (SMS-CASI) to measure sexual risk behavior in a RCT of HIV self-test use. mHealth. 2019;18:5.
Carballo-Diéguez A, Giguere R, Balán IC, Brown W, Dolezal C, Leu C-S, Lopez Rios J, Sheinfil AZ, Frasca T, Rael CT, Lentz C, Crespo R, Iribarren S, Cruz Torres C, Febo I. Use of rapid HIV self-test to screen potential sexual partners: Results of the ISUM study. Under review.
Carballo-Diéguez A, Giguere R, Balán IC, Dolezal C, Brown W, Lopez Rios J, Sheinfil A, Frasca T, Rael CT, Lentz C, Crespo R, Cruz Torres C, Leu C-S, Febo I. Few aggressive or violent incidents are associated with the use of HIV self-tests to screen sexual partners among key populations. Under review.
Brown W, Lopez Rios J, Sheinfil A, Frasca T, Cruz Torres C, Crespo R, Dolezal C, Giguere R, Lentz C, Balán I, Rael C, Febo I, Carballo-Diéguez A. Text messaging and disaster preparedness aids engagement, re-engagement, retention and communication among Puerto Rican participants in an HIV self-testing study after Hurricanes Irma and Maria. Disaster Medicine and Public Helath Preparedness. In press.
Rael CT, Giguere R, Lopez Rios J, Lentz C, Balán IC, Sheinfil A, Dolezal C, Brown W, Frasca T, Cruz Torres C, Crespo R, Iribarren S, Leu C-S, Febo I, Carballo-Diéguez A. Transgender women’s experiences using a home HIV-testing kit for self- and partner-testing. Under review.
Balán IC, Lopez Rios J, Giguere R, Lentz C, Dolezal C, Cruz Torres C, Brown W, Crespo R, Sheinfil A, Rael CT, Febo I, Carballo-Diéguez A. Then we looked at his results: What happens when a sexual partner’s HIV self-test result is positive? Under review.
Sheinfil AZ, Giguere R, Dolezal C, Lopez Rios J, Iribarren S, Brown W, Rael C, Lentz C, Balán I, Frasca T, Cruz Torres C, Crespo R, Febo I, Carballo-Diégeuz A. Applying the Information-Motivation-Behavioral Skills model to predict HIV serostatus awareness among a population of high-risk men who have sex with men and transgender women. Under review.
Lentz C, et al. Broaching the topic of HIV self-testing kit use with potential sexual partners among men who have sex with men (MSM) and transgender women (TGW) in New York and Puerto Rico. In progress.
Dolezal C, et al. Substance use and testing partners using HIV rapid home tests. In progress.
Iribarren S, et al. HIV self-test considerations: Preferences, cost considerations, issues using, and future plans for use in high-risk populations. In progress.
Lippman SA, Moran L, Sevelius J, et al. Acceptability and feasibility of HIV self-testing among transgender women in San Francisco: a mixed methods pilot study. AIDS Behav. 2016;20:928–38.
Frye V, Wilton L, Hirshfield S, et al. “Just because it’s out there, people aren’t going to use it.” HIV self-testing among young, Black MSM, and transgender women. AIDS Patient Care STDs. 2015;29(11):617–24.
Estem KS, Catania J, Klausner JD. HIV self-testing: a review of current implementation and fidelity. Curr HIV AIDS Rep. 2016;13:107–15.
Bustamante MJ, Konda KA, Joseph Davey D, et al. HIV self-testing in Peru: questionable availability, high acceptability but potential low linkage to care among men who have sex with men and transgender women. Int J STD AIDS. 2017;28:133–7.
Napierala Mavedzenge S, Baggaley R, Corbett EL. A review of self-testing for HIV: research and policy priorities in a new era of HIV prevention. Clin Infect Dis. 2013;57:126–38.
Wood BR, Ballenger C, Stekler JD. Arguments for and against HIV self-testing. HIV AIDS. 2014;6:117–26.
Martinez O, Carballo-Diéguez A, Ibitoye M, et al. Anticipated and actual reactions to receiving HIV positive results through self-testing among gay and bisexual men. AIDS Behav. 2014;14:2485–95.
Campbell C, Mzaidume Z. Grassroots participation, peer education, and HIV prevention by sex workers in South Africa. Am J Public Health. 2001;91:1978–86.
Swenderman D, Basu I, Das S, Jana S, Rotheram-Borus MJ. Empowering sex workers in India to reduce vulnerability to HIV and sexually transmitted diseases. Soc Sci Med. 2009;69:1157–66.
Acknowledgements
The authors wish to thank the participants who shared their time and thoughts about using HIVST kits with clients. This project was supported by a grant from the NICHD (R01-HD076636; PI: Carballo-Diéguez, PhD). This work was also supported by a Center Grant from the NIMH to the HIV Center for Clinical and Behavioral Studies at New York State Psychiatric Institute and Columbia University (P30-MH43520; PI: Remien, PhD). William Brown III was supported by the National Library of Medicine (NLM) [grant numbers R01-LM012355 PI: Schillinger, T15-LM007079 PI: Hripcsak, R01-LM013045 PI: Lyles], the National Institute on Minority Health and Health Disparities (NIMHD) [grant number P60-MD006902 PI: Bibbins-Domingo], the Agency for Healthcare Research and Quality (AHRQ) [grant number K12-HS026383], and the National Center for Advancing Translational Sciences (NCATS) of the NIH [UCSF-CTSI grant number KL2-TR001870] during various stages of the research and/or preparation of the article. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Funding
This study was funded by a grant from the NICHD (R01-HD076636; PI: Carballo-Diéguez, PhD).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Giguere, R., Lopez-Rios, J., Frasca, T. et al. Use of HIV Self-Testing Kits to Screen Clients Among Transgender Female Sex Workers in New York and Puerto Rico. AIDS Behav 24, 506–515 (2020). https://doi.org/10.1007/s10461-019-02730-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-019-02730-2