Abstract
Men who have sex with men (MSM) and transgender women (TW) are a priority population for HIV prevention in Myanmar but report sub-optimal HIV testing frequency. Previous studies have shown that peer involvement in HIV testing can normalize stigmatized sexualities and reduce barriers to testing. We explored the acceptability of peer-delivered HIV testing among 425 undiagnosed MSM and TW in Yangon and Mandalay. An overwhelming majority of participants (86%) reported being ‘comfortable/very comfortable’ with peer-delivered HIV testing. Logistic regression identified reporting sexual identity as Apone [adjusted odds ratio (aOR) 3.8; 95% CI 1.2–11.7], recent HIV testing (aOR 3.1; 95% CI 1.4–6.5), reporting a high likelihood of HIV acquisition (aOR 3.6; 95% CI 1.7–7.6), and reporting ≥ 5 casual partners in the past 3 months (aOR 0.2; 95% CI 0.1–0.6) as associated with peer-delivered HIV testing acceptability. Given ongoing HIV vulnerability among MSM and TW in Myanmar, peer-delivered testing may offer prevention benefits by increasing testing rates and identifying undiagnosed infection earlier.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ambitious UN targets to virtually eliminate AIDS by 2030 are predicated on 90% of people with undiagnosed HIV infection knowing their HIV status [1]. Achieving this target is reliant on regular HIV testing among populations at risk of HIV infection. HIV testing offers important primary prevention opportunities through pre- and post-test discussions with providers and post-diagnosis reductions in risk behaviors [2], and facilitates secondary HIV prevention through early treatment access and viral suppression [3, 4].
Men who have sex with men and transgender women (hereafter referred to as MSM and TW for brevity) are a key population in the Asian HIV epidemic and are at substantially increased risk of HIV acquisition through risk behaviors such as unprotected anal intercourse with multiple sexual partners [5, 6]. In Myanmar, HIV prevalence among MSM and TW in 2015 increased to 11.6% from an estimated 6.6% in 2009, and the concentration of HIV reported among MSM and TW in the major cities of Yangon (26.6%) and Mandalay (21.6%) are among the highest seen across Asia-Pacific [7,8,9]. HIV infections among MSM and TW currently account for 13% of all incident cases in Myanmar; this is estimated to increase to 27% by 2021 in the absence of adequate interventions [10]. Consequently, MSM and TW are a priority for HIV control in Myanmar’s national response [11] and this concentrated focus has seen a rise in HIV prevention programs targeting this group [12].
The new national strategic plan for HIV highlights the need to strengthen the enabling environment for HIV prevention interventions among key populations [9]. Strategies such as expanding HIV testing service (HTS) models, strengthening affected communities’ involvement in service delivery, and the tailoring of community-based HIV services are identified as priority activities to reach 90% of MSM and TW by 2030 [9]. In part, these activities are designed to address low rates of HIV testing among MSM and TW in Myanmar [9], where the illegality of homosexual acts and discrimination and harassment of sexual minorities act as barriers to uptake of HTS [13,14,15,16]. In such settings, the involvement of MSM and TW peers in service delivery can enhance demand and uptake of HIV and sexual health services [13, 17,18,19] by creating environments in which stigmatized sexual identities are normalized and where MSM and TW can talk openly about same-sex behaviors [20]. When applied specifically to HIV testing, the involvement of peers in countries as diverse as Nigeria, Australia and France has demonstrated effectiveness in increasing diagnoses of HIV and linking more HIV-positive MSM to care compared to non- peer involved models [21,22,23].
Recent developments in Myanmar have expanded opportunities for new models of HTS, beyond those provided by government or private providers. In particular, the introduction of decentralized HTS in 2013, the introduction of HIV rapid point-of-care (RPOC) testing and increasing provision of HIV prevention services by domestic and international NGOs [24, 25] has enabled the expansion of HIV testing for MSM and TW into community settings. While there are some examples of the positive impact of MSM and TW peer-testing [26] and peer-involvement [27] on HIV testing rates in Asia, models that include the direct provision of HIV testing by MSM and TW remain relatively uncommon in this region. Moreover, the acceptability of peer-delivered models of testing among MSM and TW in Asia is also unknown; only one study has explored acceptability among key populations in Asia, revealing a high level of acceptance for peer-delivered testing among people who inject drugs in Thailand [28]. However, factors such as the perceived professionalism and skill of peer testers [29], boundaries between personal and professional relationships [30], and concerns for confidentiality [31] may affect the acceptability of peer-delivered testing and the extent to which such models can contribute to improved service engagement and rates of HIV testing among MSM and TW.
In 2014, we conducted a study among MSM and TW in Myanmar to: (1) determine the level of acceptability of peer- delivered HIV testing; and (2) identify factors associated with peer- delivered HIV testing acceptability.
Methods
Cross-sectional surveys were completed by self-identifying MSM and TW recruited in Yangon and Mandalay in November and December 2014. Participants were recruited by 12 trained MSM and TW peer workers selected from community-based NGO Myanmar Business Coalition on AIDS (MBCA). MBCA implements an MSM and TW-targeted outreach HIV education and prevention program which is coordinated by Burnet Institute as part of their HIV education and prevention program in Myanmar. This program has been operating since 2009 and provides condoms and lubricant distribution and HIV testing education and referral activities to MSM and TW through outreach activities and fixed-site drop in centres in five locations.
Recruitment
MSM and TW were recruited in Yangon and Mandalay. These are the two largest cities in Myanmar and were chosen based on high HIV prevalence among MSM and TW (26.6% in Yangon and 21.6% in Mandalay respectively; 9) and their subsequent centrality in Myanmar’s HIV prevention response.
Trained peer workers recruited participants using convenience and snowball sampling at known MSM/TW-hotspot locations. Following a short study description, MSM and TW expressing interest in participating were provided with a non-study identifying participation card containing a list of times and locations where they could participate in surveys. Participants that indicated they knew others in their peer network that might be interested in participating were provided with up to three participation cards to give to their peers. Eligible participants were biologically male, aged over 18 years, self-reported anal sex with another male in the past 1 year and had not previously participated in the study. We estimate that approximately 15% of eligible MSM and TW provided with a study card did not present at the agreed time and place for interview. All participants were required to provide informed written consent prior to participation and received 3000 Myanmar Kyat (MMK; approximately USD$2.20) for their time and travel expenses at the completion of the survey.
Data Collection
Surveys were researcher-administered using electronic, password-protected tablets at fixed-site locations selected on the basis of their confidentiality and safety. These included established drop in centres, the Burnet Institute office in Yangon, and locations where MSM and TW gather such as teahouses. Given the sensitivity of same-sex behaviors in Myanmar, no personally-identifying information was collected or recorded from participants during interviews. The survey was designed to inform ongoing HIV prevention and testing services for MSM and TW in Myanmar. The survey was conducted in the local language and explored a range of socio-demographic factors, sexual risk behaviors, HIV prevention practices, knowledge, attitudes and use of HIV/STI risk reduction strategies and self-perceived HIV risk among MSM and TW. Factors included in this analysis were: age, sexual identity (Apone, Apwint and Tha Nge; see below), highest level of education (primary, middle, secondary, tertiary), monthly income (equal or below median, above median), number of regular (none, 1, > 1) and casual (none, 1–5, > 5) male partners in past 3 months, condom use by partner type during the past 3 months (never, occasionally, often, always), any sex with female partners in past 3 months (yes, no), self-perceived risk of acquiring HIV (very unlikely, unlikely, neither unlikely or likely, likely, very likely), how serious participants considered HIV (not at all serious, not serious, neither serious nor unserious, serious, extremely serious), lifetime history of testing for HIV (yes, no) and time since last HIV test (past 6 months, 6 months–2 years, > 2 years, never).
Sexuality was defined using locally accepted the labels Apone, Apwint and Tha Nge that are commonly used in Myanmar to describe sub-groups of MSM and TW and have typically been indicative of sexual positioning, sexual behavior and power dynamics [32]. However these labels are equivocally defined [33, 34] and continue to evolve [34], particularly in response to increasing exposure to Western media and acceptance of sexual minorities in Myanmar. To reflect current understandings of male sexual identities in Myanmar we operationalized these terms in the following way: Apwint are biological males who are typically disclosing of same-sex preferences, and have a feminine presentation and/or may be regarded as transgendered. Apone are men who have a masculine presentation, and in some spheres or circumstances may disclose same-sex behavior and identify as gay, while in others are likely to conceal, or deny their same–sex preferences and are often referred to as ‘hidden’. Apwint and Apone are typically receptive partners in sexual positioning. Tha Nge are masculine, heterosexual-identifying men who conform to heteronormative expectations, and may engage in sexual relationships with women, while also engaging in incidental sex with other men and may also be referred to as ‘hidden’. Tha Nge typically partner with Apwint, often commercially, as well as Apone, and assume the insertive role in sexual partnerships [9, 13, 32, 33].
Analysis
The primary outcome of interest was acceptability of peer- delivered HIV testing. Participants were asked to respond to the following question: “How comfortable would you be with an appropriately trained peer counsellor providing you with HIV testing and counseling?” Those that reported being very comfortable or comfortable were classified as ‘accepting’ of peer-delivered HIV testing while those who reported being neither comfortable nor uncomfortable, uncomfortable, very uncomfortable were classified as ‘not accepting’ of peer-delivered testing. Analyses were restricted to those who provided a valid response to the primary outcome and who self-reported being HIV undiagnosed (either through reporting their last HIV test as negative or reporting their HIV status as unknown). Exposures were chosen a priori based on previous research on factors associated with testing uptake and knowledge of the local context. Socio-demographic characteristics, sexual risk behaviors, HIV prevention practices, barriers to HIV testing and self-perceived HIV risk were analyzed descriptively. Univariable and multivariable logistic regression identified significant associations between these variables and acceptability of HIV testing delivered by peers. A multivariable model was constructed retaining all variables analyzed in univariable analyses. Analyses were conducted using Stata (Version 13, Stata Corp., College Station, TX, USA). Statistical significance in all analysis was set at p ≤ 0.05.
Ethics
Ethics approval was granted by the Alfred Hospital Ethics Committee (Australia; #445/14) and the Department of Medical Research (Lower Myanmar) Ethical Review Committee (761 Ethics 2004).
Results
520 MSM and TW were recruited for this study. Ninety-five participants (18.3%) were excluded from analysis based on missing data on the primary outcome (n = 19) or HIV status (n = 10) or who self-reported an HIV-positive status (n = 66). Among the remaining 425 HIV-undiagnosed participants, 173 (40.7%) were recruited in Yangon and 252 (59.3%) in Mandalay. Three hundred and fifty four (83.5%) identified as male and 70 (16.5%) as TW. Two hundred and forty seven (58.3%) MSM and TW were aged under 25 and 210 (49.9%) identified as Tha Nge. Thirty seven percent of MSM and TW had completed secondary level education (equivalent to 11 years of schooling). The median monthly income was MMK 150,000 (approximately USD $190; IQR: 90,000–200,000).
Most MSM and TW reported anal sex with a regular male partner; 174 (40.9%) and 81 (19.1%) participants reported one, and more than one regular partner in the past 3 months, respectively. Among these 255 participants, 160 (69.9%) reported inconsistent condom use with their regular partner(s) during the past 3 months. Recent sex with casual partners was also common, with 199 (48.3%) and 88 (21.4%) participants reporting sex with 1–5 and more than 5 casual partners in the past 3 months, over half of whom (56.9%) reported inconsistent use of condoms. Thirty three percent of all participants reported both regular and casual partner(s) in the past 3 months. Sex with female partners was rare and reported by 64 (15.1%) participants.
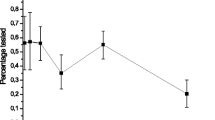
One hundred and ninety (46.0%) MSM and TW considered it ‘likely’ or ‘very likely’ they would acquire HIV in the future and 246 (58.7%) considered HIV ‘very serious’. HIV testing within the past 6 months was reported by 282 (66.8%) of participants. Three hundred and sixty-six (86.1%) indicated they were ‘comfortable/very comfortable’ with the idea of receiving HIV testing from a trained peer and classified as accepting of peer-delivered HIV testing (Table 1).
In unadjusted analyses, participants who identified as Apone (OR 3.6; 95% CI 1.5–8.9), who considered their risk of HIV acquisition as ‘likely/very likely’ (OR 3.0; 95% CI 1.6–5.7), who perceived HIV as ‘very serious’ (OR 2.3; 95% CI 1.3–4.1), and who reported their last HIV test within the past 6 months (OR 3.3; 95% CI 1.8–6.0) or between 6 months and 2 years (OR 4.6; 95% CI 1.5–14.1) were significantly more likely to find peer-delivered HIV testing acceptable. MSM and TW with more than five casual partners in the past 3 months were significantly less likely to accept peer- delivered HIV testing (OR 0.5; 95% CI 0.2–1.0) (Table 1).
In multivariable analysis, self-identifying as Apone (aOR 3.8; 95% CI 1.2–11.7), considering the risk of HIV acquisition as ‘likely/very likely’ (aOR 3.6; 95% CI 1.7–7.6), reporting an HIV test in the past 6 months (aOR 3.1; 95% CI 1.4–6.5) or between 6 months and 2 years ago (aOR 4.3; 95% CI 1.2–15.4) remained positively associated with acceptability of peer- delivered HIV testing. Reporting more than 5 casual partners in the past three months (aOR 0.2; 95% CI 0.1–0.6) also remained negatively associated with acceptance of peer- delivered HIV testing (Table 1).
Discussion
This study revealed a high level of acceptance for peer-delivered HIV testing among MSM and TW in Myanmar. The acceptability of HIV peer-testing among key populations in Myanmar has not been previously investigated. Acceptability of peer-delivered HIV testing was high across all variables that characterized MSM and TW in our sample, demonstrating broad acceptability of peer-delivered HIV testing models. Acceptability of peer-delivered HIV testing was particularly high among MSM and TW identifying as Apone, those who reported recent HIV testing and perceived themselves as at high risk of acquiring HIV in the future. These findings have implications for future models of HTS in Myanmar and, given recent national recommendations for peer-involved models of service delivery, have immediate translational potential. Alongside new global guidelines supportive of lay HIV testing [35], MSM and TW peer-based HTS emerging in other countries [36, 37], nascent community mobilization and the increasing availability of RPOC HIV testing enhance the feasibility of new MSM and TW peer-based HIV testing models in Myanmar.
Our finding that Apone were more likely to accept peer-delivered HIV testing than heteronormative MSM self-identifying as Tha Nge likely reflects their relative level of comfort accessing peer-involved services more obviously tailored to MSM and TW. While over 80% of Tha Nge still considered peer-delivered testing as acceptable, ensuring these service models appeal to Tha Nge who may not identify as the intended target population of MSM and TW-specific services is crucially important to increase the reach and effectiveness of HTS in Myanmar. Across Asia, men who have sex with both men and women are less likely to test for HIV compared to men with exclusively male partners [38, 39], suggesting that heteronormative MSM are not adequately reached or served by existing models of HIV testing. However, while the avoidance of heteronormative men of HIV services that manifestly cater for MSM and TW may be expected, our finding that four in five Tha Nge were accepting of peer-delivered HIV testing suggests potential benefits of a peer-based model for this group. Mainstream health services in Asia have been identified as locations where HIV risk populations perceive and experience significant discrimination [15, 16, 40]. Mainstream health professionals in Asia have also been shown to exhibit highly stigmatizing attitudes to people at risk or living with HIV [41, 42]. Peer-based services can minimize reluctance to test associated with service-provider stigma [43, 44] by providing environments in which same-sex behaviors can be openly discussed with other MSM and TW, thereby ensuring that clients receive counseling and testing commensurate with their actual risk behaviors.
Our sample, recruited in the context of an existing community-based HIV prevention program, demonstrated a high level of existing engagement with HIV testing services. Two thirds of MSM and TW reported an HIV test in the past 6 months and the proportion reporting an HIV test in the past 12 months was one and a half times higher than the national average [9]. We found that MSM and TW with a more recent history of HIV testing were more likely to find peer-delivered HIV testing acceptable. This result is not surprising, given that MSM and TW who routinely engage with testing services are likely to have already overcome certain barriers to accessing HTS and may therefore be more willing to consider alternative models of testing. In recent studies, Chinese MSM who recently tested were more willing to consider couple-based HIV testing [45], while people who inject drugs in Thailand who reported recent avoidance of HIV testing were around three times less likely to accept peer- delivered HIV testing compared to those that did not [28]. Taken together, these findings highlight the need to consider specific strategies to identify and engage naïve and infrequent HIV testers to facilitate ongoing and routine engagement with HIV prevention services, including new and novel models of HIV testing. Innovative use of online technologies, for example, have demonstrated positive results in engaging MSM for HIV testing [46,47,48,49], including non-gay identified MSM [50], and are increasingly being used across Asia to reach hard to reach and hidden MSM and TW populations [51, 52]. Such approaches could be considered in Myanmar, particularly in light of the burgeoning information, communication and technology (ICT) environment [53] and increasing use of cyber networks among MSM and TW communities [54].
MSM and TW in this study who perceived they were at a greater risk of HIV acquisition were more accepting of peer-delivered HIV testing. In other studies, fear of a positive result has been identified as a barrier to HIV testing among MSM [55, 56]. Decisions to test among people at risk of HIV may be influenced by perceptions about the availability and quality of post-diagnosis support and HIV treatment and care following a positive result [55]. Our finding suggests that expectations among MSM and TW about the nature of post-diagnosis support provided by peers may similarly influence decisions to test and reflect a preference to be diagnosed by peers or by people with whom they have an existing relationship. This finding was potentially influenced by the recruitment of a sample through an established and peer-involved HIV education and prevention service. In any case, the common experiences and characteristics between peer workers and clients has been identified as a major benefit and appeal of peer-based services [57] and may help promote better engagement with HTS, particularly among those who consider themselves at high risk of HIV.
Somewhat contradictory of the positive relationship between acceptability of peer-delivered HIV testing and perceived risk of HIV acquisition, we found that those who reported a higher number of casual sex partners were less likely to find peer-delivered HIV testing acceptable. Others have reported peer-led models of HIV testing have attracted MSM and TW who report higher levels of sexual risk behavior compared to non-peer-based services [23, 58]. Our finding may reflect the context in which MSM and TW meet sex partners in Yangon and Mandalay mostly through a small number of public cruising areas, and concerns identified by others in relation to a potential overlap of social and sexual MSM and TW networks [59, 60]. While most MSM and TW reporting more than five sex partners in the past 3 months still found peer-delivered HIV testing acceptable, for some, concerns about privacy, confidentiality or fear of being judged by peers in relation to their risk behaviors or when receiving a positive diagnosis may present certain barriers [61]. While others have noted that peer-based models are perceived by MSM and TW as non-judgemental [31, 62], a perceived lack of confidentiality and potential for community gossip has been identified recently as a concern among MSM and TW in Myanmar regarding community-based HIV services [63].
Our sampling approach, which recruited MSM and TW engaged with an existing HIV prevention service in the two largest urban settings in Myanmar, may limit the generalizability of our findings to smaller cities or more rural locations. However, the findings are likely to be informative of attitudes among MSM and TW in the major cities of Yangon and Mandalay given that the MBCA-Burnet Institute outreach program through which the sample was recruited was among the most extensive (distributing approximately 1 million condoms per annum through outreach) of the MSM and TW peer-involved services operating in Yangon (four services) and Mandalay (three services) at the time of recruitment. MSM and TW included in this study reported rates of HIV testing higher than the national average [7] suggesting regular engagement with HIV prevention services. This frequent exposure to HIV services and health promotion may have contributed to the high level of acceptance for peer-delivered testing. Our sample was also relatively well educated and remunerated [64] and their preferences may not reflect those of MSM and TW who are more isolated, have less access to HIV services, or who are economically and socially-disadvantaged. However, the recruitment of MSM and TW being reached by an NGO HIV education and prevention program in outreach settings in Yangon and Mandalay enhances the translation potential of findings. As noted earlier, the new national strategic plan for HIV in Myanmar [9] emphasizes an expanded role for peers in HIV models of care. To our knowledge no HIV peer-delivered testing model has yet been implemented in Myanmar, with peer roles in testing typically restricted to pre-test counselling in NGO services. Soon after data collection was completed for this study the MBCA-Burnet Institute program introduced HIV testing, with peers involved in promoting testing services and in pre-test counselling and nurses delivering the RPOC tests. These services have since delivered on average 650 and 850 HIV tests per month to MSM and TW. Our findings showing high levels of acceptability for peer-delivered testing among MSM engaged with this NGO-delivered HIV program, suggest the direct provision of tests by peers (rather than nurses) would potentially enhance demand for testing even further and expand opportunities for prevention education.
MSM and TW in South and South-east Asia have low rates of HIV testing compared to other low- and middle-income countries [65]. Our findings demonstrate that peer-delivered HIV testing is highly acceptable and, given the low national rates of HIV testing and ongoing experiences of stigma and discrimination among MSM and TW in Myanmar, may help circumvent barriers to HIV testing and increase engagement of MSM and TW in HIV treatment and care. The current policy, regulatory and community context in Myanmar is conducive to the introduction of community-based models of HIV testing and the inclusion of peer-testing models [9] and our findings provide strong support for the integration of HIV testing by peers in community-based models. Further research is needed to understand implementation barriers to integrated peer-delivered HIV testing models across a range of community and clinical settings, including those associated with potential concerns for privacy and confidentiality among more sexually-active MSM and TW.
References
UNAIDS. 90- 90-90: An ambitious treatment target to help end the AIDS epidemic. Geneva, Switzerland: UNAIDS; 2014.
Fox J, White PJ, Macdonald N, Weber J, McClure M, Fidler S, et al. Reductions in HIV transmission risk behaviour following diagnosis of primary HIV infection: a cohort of high-risk men who have sex with men. HIV Med. 2009;10(7):432–8.
Sharma M, Ying R, Tarr G, Barnabas R. Systematic review and meta-analysis of community and facility-based HIV testing to address linkage to care gaps in sub-Saharan Africa. Nature. 2015;528(7580):S77–85.
Insight Start Study Group. Initiation of antiretroviral therapy in early asymptomatic HIV infection. N Engl J Med. 2015;373(9):795–807.
van Griensven F, Thienkrua W, McNicholl J, Wimonsate W, Chaikummao S, Chonwattana W, et al. Evidence of an explosive epidemic of HIV infection in a cohort of men who have sex with men in Thailand. AIDS. 2013;27(5):825–32.
Baral S, Sifakis F, Cleghorn F, Beyrer C. Elevated risk for HIV infection among men who have sex with men in low- and middle-income countries 2000–2006: a systematic review. PLoS Med. 2007;4(12):e339.
National AIDS Programme. Integrated bio-behavioural survey. Myanmar: Department of Health; 2009.
National AIDS Programme. Myanmar global AIDS response program report 2015. Myanmar: Department of Health; 2015.
National AIDS Programme. National strategic plan on HIV and AIDS: Myanmar 2016–2020. Myanmar: Department of Health; 2016.
Strategic Information and Monitoring and Evaluation Working Group Technical and Strategy Group on AIDS. HIV estimates and projections: asian epidemiological model Myanmar 2010–2015. Myanmar: Department of Health.
National AIDS Programme. Myanmar National Strategic Plan on HIV and AIDS 2011–2015. Myanmar: Department of Health.
National AIDS Programme. Global AIDS response progress report. Myanmar: Department of Health; 2014.
Chua LJG, Glibert D. Sexual orientation and gender identity minorities in transition: LGBT rights and activism in Myanmar. Hum Rights Q. 2015;37:1–28.
Logie CH, Newman PA, Weaver J, Roungkraphon S, Tepjan S. HIV-related stigma and HIV prevention uptake among young men who have sex with men and transgender women in Thailand. AIDS Patient Care STDs. 2016;30(2):92–100.
Wei C, Cheung DH, Yan H, Li J, Shi LE, Raymond HF. The impact of homophobia and HIV Stigma on HIV testing uptake among Chinese men who have sex with men: a mediation analysis. J Acquir Immune Defic Syndr. 2015;71(1):87–93.
Wei C, Yan H, Yang C, Raymond HF, Li J, Yang H, et al. Accessing HIV testing and treatment among men who have sex with men in China: a qualitative study. AIDS Care. 2014;26(3):372–8.
Scott HM, Pollack L, Rebchook GM, Huebner DM, Peterson J, Kegeles SM. Peer social support is associated with recent HIV testing among young black men who have sex with men. AIDS Behav. 2014;18(5):913–20.
Young SD, Cumberland WG, Nianogo R, Menacho LA, Galea JT, Coates T. The HOPE social media intervention for global HIV prevention: a cluster randomized controlled trial in Peru. Lancet HIV. 2015;2(1):e27–32.
Williamson LM, Hart GJ, Flowers P, Frankis JS, Der GJ. The Gay Men’s Task Force: the impact of peer education on the sexual health behaviour of homosexual men in Glasgow. Sex Transm Infect. 2001;77(6):427–32.
Trapence G, Collins C, Avrett S, Carr R, Sanchez H, Ayala G, et al. From personal survival to public health: community leadership by men who have sex with men in the response to HIV. Lancet. 2012;380(9839):400–10.
Adebajo S, Eluwa G, Njab J, Oginni A, Ukwuije F, Ahonsi B, et al. Evaluating the effect of HIV prevention strategies on uptake of HIV counselling and testing among male most-at-risk-populations in Nigeria; a cross-sectional analysis. Sex Transm Infect. 2015;91(8):555–60.
Minas BC, Giele CM, Laing SC, Bastian L, Burry AW, Sales KJ, et al. Early diagnosis of HIV among men who have sex with men in Western Australia: impact of a peer-led sexually transmissible infection testing service. Sex Health. 2015;12(4):360–3.
Lorente N, Preau M, Vernay-Vaisse C, Mora M, Blanche J, Otis J, et al. Expanding access to non-medicalized community-based rapid testing to men who have sex with men: an urgent HIV prevention intervention (The ANRS-DRAG Study). PLoS ONE. 2013;8(4):e61225.
National AIDS Programme. Joint Rapid Assessment of HIV Treatment in Myanmar: Final Report September 2013. Myanmar: Department of Health, 2013.
Oo HN, Hone S, Fujita M, Maw-Naing A, Boonto K, Jacobs M, et al. Evolution of the health sector response to HIV in Myanmar: progress, challenges and the way forward. J Virus Erad. 2016;2(Suppl 4):20–6.
Pawa D, Firestone R, Ratchasi S, Dowling O, Jittakoat Y, Duke A, et al. Reducing HIV risk among transgender women in Thailand: a quasi-experimental evaluation of the sisters program. PLoS ONE. 2013;8(10):e77113.
USAID. Linkages Thailand: using peer mobilizers to increase uptake of HIV testing and counseling 3 July 2017. https://www.usaid.gov/what-we-do/global-health/hiv-and-aids/success-stories/linkages-thailand-using-peer-mobilizers.
Ti L, Hayashi K, Kaplan K, Suwannawong P, Wood E, Montaner J, et al. Willingness to access peer-delivered HIV testing and counseling among people who inject drugs in Bangkok, Thailand. J Community Health. 2013;38(3):427–33.
Njau B, Ostermann J, Brown D, Muhlbacher A, Reddy E, Thielman N. HIV testing preferences in Tanzania: a qualitative exploration of the importance of confidentiality, accessibility, and quality of service. BMC Public Health. 2014;14:838.
Repper J, Carter T. A review of the literature on peer support in mental health services. J Mental Health. 2011;20(4):392–411.
Pedrana A, Koester K, Stewart W, Gibson S, Powell S, Stoove M. Editor Community-based rapid HIV point-of-care testing with contrasting health systems: a tale of two cities from San Francisco and Melbourne. 20th International AIDS Conference 2014 July 20–25, 2014; Melbourne, Australia.
Aung T, McFarland W, Paw E, Hetherington J. Reaching men who have sex with men in Myanmar: population characteristics, risk and preventive behavior, exposure to health programs. AIDS Behav. 2013;17(4):1386–94.
UNESCO Bangkok and Department of Medical Research MoH, Myanmar. Multi-level risk and protective factors and HIV-related risk behaviours among young men who have sex with men (YMSM) in Myanmar. Paris, France: UNESCO Bangkok and Department of Medical Research, Ministry of Health, Myanmar; 2015.
Gilbert D. Categorizing gender in queer Yangon. Sojourn. 2013;28(2):241–71.
WHO. Consolidated guidelines on HIV testing services. 5Cs: consent, confidentiality, counseling, correct results and connection Geneva, Switzerland WHO; 2015.
Zhang DP, Han L, Li CM, Meng SN, Leng ZW, Li F, et al. The impact of community-based organizations in HIV testing mobilization among men who have sex with men. Zhonghua Yu Fang Yi Xue Za Zhi. 2013;47(5):431–4.
Ryan KE, Wilkinson AL, Leitinger D, El-Hayek C, Ryan C, Pedrana A, et al. Characteristics of gay, bisexual and other men who have sex with men testing and retesting at Australia. Sex Health. 2016;13(6):560–7.
Bowring AL, Veronese V, Doyle JS, Stoove M, Hellard M. HIV and sexual risk among men who have sex with men and women in Asia: a systematic review and meta-analysis. AIDS Behav. 2016;20(10):2243–65.
Guadamuz TE, Cheung DH, Wei C, Koe S, Lim SH. Young, online and in the dark: scaling up HIV testing among MSM in ASEAN. PLoS ONE. 2015;10(5):e0126658.
Churcher S. Stigma related to HIV and AIDS as a barrier to accessing health care in Thailand: a review of recent literature. WHO South East Asia J Public Health. 2013;2(2):12–22.
Chan KY, Yang Y, Li ZR, Stoove MA, Reidpath DD. Interrelationships between HIV/AIDS and risk behavior prejudice among medical students in Southern China. Curr HIV Res. 2009;7(6):601–11.
Chan KY, Stoove MA, Reidpath DD. Stigma, social reciprocity and exclusion of HIV/AIDS patients with illicit drug histories: a study of Thai nurses’ attitudes. Harm Reduct J. 2008;5:28.
Ayala G, Makofane K, Santos GM, Beck J, Do TD, Hebert P, et al. Access to basic HIV-related services and PrEP acceptability among men who have sex with men worldwide: barriers, facilitators, and implications for combination prevention. J Sex Transm Dis. 2013;2013:953123.
Meehan SA, Leon N, Naidoo P, Jennings K, Burger R, Beyers N. Availability and acceptability of HIV counselling and testing services. A qualitative study comparing clients’ experiences of accessing HIV testing at public sector primary health care facilities or non-governmental mobile services in Cape Town, South Africa. BMC Public Health. 2015;15:845.
Wei C, Muessig KE, Bien C, Yang L, Meng R, Han L, et al. Strategies for promoting HIV testing uptake: willingness to receive couple-based and collective HIV testing among a cross-sectional online sample of men who have sex with men in China. Sex Transm Infect. 2014;90(6):469–74.
Rhodes SDVA, Stowers J, Miller C, McCoy TP, Hergenrather KC, Wilkin AM, Reece M, Bachmann LH, Ore A, Ross MW, Hendrix E, Eng E. A CBPR partnership increases HIV testing among men who have sex with men (MSM): outcome findings from a pilot test of the CyBER/testing internet intervention. Health Educ Behav. 2011;38(3):311–20.
Zou H, Wu Z, Yu J, Li M, Ablimit M, Li F, et al. Internet-facilitated, voluntary counseling and testing (VCT) clinic-based HIV testing among men who have sex with men in China. PloS ONE. 2013;8(2):e51919.
Lampkin D, Crawley A, Lopez TP, Mejia CM, Yuen W, Levy V. Reaching suburban men who have sex with men for STD and HIV services through online social networking outreach: a public health approach. J Acquir Immune Defic Syndr. 2016;72(1):73–8.
Schnall R, Travers J, Rojas M, Carballo-Dieguez A. eHealth interventions for HIV prevention in high-risk men who have sex with men: a systematic review. Journal Med Internet Res. 2014;16(5):e134.
Blas MM, Alva IE, Carcamo CP, Cabello R, Goodreau SM, Kimball AM, et al. Effect of an online video-based intervention to increase HIV testing in men who have sex with men in Peru. PLoS ONE. 2010;5(5):e10448.
UNDP. Towards universal access: examples of municipal HIV programming for men who have sex with men and transgendered people in six Asian cities Bangkok, Thailand: UNDP; 2011.
Lau JTF, Lau M, Cheung A, Tsui HY. A randomized controlled study to evaluate the efficacy of an Internet-based intervention in reducing HIV risk behaviors among men who have sex with men in Hong Kong. AIDS Care. 2008;20(7):820–8.
On device research. Myanmar: the final frontier for the mobile internet. On device research 2014. https://ondeviceresearch.com/blog/myanmar-mobile-internet-report
Lin KS, Van der Putten M. Identities in motion: cyberspace and Myanmar men have sex with men. Res Humaniti Soc Sci. 2012;2(4):36–48.
Lorenc T, Marrero-Guillamón I, Llewellyn A, Aggleton P, Cooper C, Lehmann A, et al. HIV testing among men who have sex with men (MSM): systematic review of qualitative evidence. Health Educ Res. 2011;26(5):834–46.
Deblonde J, De Koker P, Hamers FF, et al. Barriers to HIV testing in Europe: a systematic review. Eur J Public Health. 2010;20:422–32.
Simoni JM, Nelson KM, Franks JC, Yard SS, Lehavot K. Are peer interventions for HIV efficacious? A systematic review. AIDS Behav. 2011;15(8):1589–95.
Yan H, Zhang R, Wei C, Li J, Xu J, Yang H, et al. A peer-led, community-based rapid HIV testing intervention among untested men who have sex with men in China: an operational model for expansion of HIV testing and linkage to care. Sex Transm Infect. 2014;90(5):388–93.
Peterson JL, Rothenberg R, Kraft JM, Beeker C, Trotter R. Perceived condom norms and HIV risks among social and sexual networks of young African American men who have sex with men. Health Educ Res. 2009;24(1):119–27.
Choi K-H, Ning Z, Gregorich SE, Pan QC. The influence of social and sexual networks in the spread of HIV and syphilis among men who have sex with men in Shanghai, China. J Acquir Immune Defic Syndr. 2007;45(1):77–84.
Flowers P, Duncan B, Frankis J. Community, responsibility and culpability: HIV-risk management among Scottish gay men. J Community Appl Soc Psychol. 2000;10:285–300.
Sempe S, Coquelin V, Rios L, Pelletier V, Stranz R. Editor Peer testing: how queer! How satisfying? Evaluating the immediate satisfaction and self-perceived effects of peer prevention interventions, including HIV rapid testing, in gay cruising areas and sex clubs. 19th International AIDS Conference 2012; Washington D.C., USA.
Vaughan M. MSM community’s perception of HTC service models for MSM 2015.
World Bank. Gross national income by capita 2015 (atlas method and PPP): World Bank; 2015 http://databank.worldbank.org/data/download/GNIPC.pdf.
Adam PCG, de Wit JBF, Toskin I, Mathers BM, Nashkhoev M, Zablotska I, et al. Estimating levels of HIV testing, HIV prevention coverage, HIV knowledge, and condom use among men who have sex with men (MSM) in low-income and middle-income countries. J Acquir Immune Defic Syndr. 2009;52:S143–51.
Acknowledgements
The authors gratefully acknowledge the work of the peer researchers from MBCA who were involved in this study as well as the participants who generously provided their time and information. The data collection was funded through program funds allocated to evaluate the Myanmar Business Coalition on AIDS (MBCA) HIV prevention outreach program and internal funds from the Burnet Institute. The Burnet Institute receives support from the Victorian Operational Infrastructure Support Program. VV is supported by a National Health and Medical Research Council (NHMRC) PhD scholarship. AP is supported by a NHMRC Early Career Fellowship. MS is supported by a National Health and Medical Research Council (Australia) Career Development Fellowship.
Funding
This study was supported by internal programme funding from the Burnet Institute. The Burnet Institute receives support from the Victorian Operational Infrastructure Support Program. This work forms part of the PhD of VV, who is supported by an NHMRC Postgraduate scholarship through Monash University.
Author information
Authors and Affiliations
Contributions
ZMO, ZWT, PPA, CH, CR and MS all contributed to the development of the data collection tools, training of peer educators to recruit participants, oversight of recruitment, data collection, and interpretation of results. VV, BLD and MS led the data cleaning and analysis process. VV led the writing of the manuscript. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Veronese, V., Oo, Z.M., Thein, Z.W. et al. Acceptability of Peer-Delivered HIV Testing and Counselling Among Men Who Have Sex with Men (MSM) and Transgender Women (TW) in Myanmar. AIDS Behav 22, 2426–2434 (2018). https://doi.org/10.1007/s10461-017-2022-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-017-2022-0