Abstract
In Latin America, transgender women (transwomen or male to female transgenders) have been included in MSM research but without addressing their specific needs in terms of the HIV/AIDS. We present results of the first seroepidemiologic study designed for transwomen in Peru. We conducted a study using respondent driven sampling to recruit transwomen from Lima. Our survey explored sociodemographic characteristics, gender enhancement procedures and sexual behavior. In addition, we conducted laboratory based HIV, genital herpes (HSV2) and syphilis testing. A total of 450 transwomen were recruited between April and July 2009. HIV prevalence was 30%, HSV2: 79% and syphilis: 23%. Sex-work was the main economic activity (64%). Gender enhancement procedures were reported by 70% of the population. Multivariable analysis showed HIV infection to be associated with being older than 35 recent, syphilis infection and HSV2 infection. Transwomen are the group most vulnerable to HIV/AIDS in Peru.
Resumen
En Latinoamérica, las mujeres trans (personas trans de masculino a femenino) han sido incluídas en la investigación con población HSH sin abordar sus necesidades específicas en relación a la epidemia de VIH/SIDA. Presentamos los resultados del primer estudio sero-epidemiológico diseñado para mujeres trans en el Perú. Utilizamos un diseño transversal con respondent driven sampling (RDS). Las características socio-demográficas de la población, los procesos de transformación del cuerpo y las conductas sexuales fueron exploradas a través de una entrevista. Se realizaron pruebas de laboratorio para VIH, herpes genital (HSV2) y sífilis. Un total de 450 mujeres trans fueron enroladas en Lima entre abril y junio del 2009. La prevalencia de VIH encontrada fue de 30%, HSV2: 79% y sífilis: 23%. El trabajo sexual fue la principal actividad económica reportada (64%). Los procesos de modificación del cuerpo fueron reportados por el 70% de la población. El análisis mutivariable asoció la infección por VIH a una edad mayor a 35 años, la infección reciente por sífilis y la infección con HSV2. Este estudio muestra que las mujeres trans constituyen la población con mayor vulnerabilidad al VIH en el Perú.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
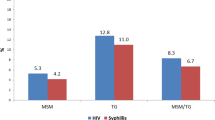
To date the HIV/AIDS epidemic in Peru and Latin America has been portrayed as being concentrated among men who have sex with men (MSM) [1–4]. However, the risk category, MSM, has also included populations that have gender identities other than male and who have different vulnerabilities for HIV infection. For example, surveillance studies among MSM in Peru have consistently shown a higher proportion of HIV infection among transwomen (persons who were born or assigned male gender at birth but identify as female, regardless of the initiation or completion of gender enhancement or transition procedures) compared to men who identify as gay or bisexual [3, 5]. These studies targeted high-risk MSM (including transwomen) but could have overestimated HIV prevalence among transwomen as they were not designed for this group alone and thus may not have achieved representative samples of this population. Several international studies have separated transwomen from MSM, conducting investigations specifically designed for this group [6–10]. To date no surveillance studies specific to this population have been conducted in Peru. Furthermore, there are no demographic and behavioral data from this population and consequently no prevention interventions have been specifically designed for transwomen in Peru [11, 12].
The risks for HIV infection among transwomen are linked to high rates of sex work and drug abuse, which are themselves linked to extreme marginalization and lack of other options for survival [13–16]. Social exclusion and violence are factors that also contribute to increased vulnerability [6, 17, 18]. Today, homophobia and transphobia are still prevalent in Peruvian society. Situations of marginalization and exclusion experienced by transwomen are common in everyday life [19]. Exploratory work conducted by the Unit of Health, Sexuality and Human Development at the Universidad Peruana Cayetano Heredia (UPCH) has found that transwomen in Peru suffer from lack of access to education, employment, and housing; are frequent victims of interpersonal and police violence; and have high rates of substance abuse [19]. A recent investigation conducted among a group of people living with HIV/AIDS from four cities in Peru showed that transwomen identity was associated with lower access to care [20]. In the past transwomen activists themselves have propelled the agenda in order to promote research and health interventions specifically designed for their community [21].
A cross-sectional study using respondent driven sampling (RDS) was designed to examine the HIV/AIDS epidemiologic profile among transwomen residing in Lima, and to describe the main sociodemographic and behavioral characteristics of this population in relation to the HIV epidemic. RDS is a method that has the potential to penetrate into networks of hidden/hard to reach populations, and has increasingly been used as a sampling method in populations with high vulnerability to HIV [22–26]. Overall, Lima represents 78% of all HIV/AIDS reported cases in Peru, and concentrates transwomen from other regions of the country that migrate there seeking economic improvement [21]. Our main study goals were to assess the seroepidemiology and prevalence of HIV, HSV2, syphilis, gather representative sociodemographic, gender enhancement procedure utilization and sexual risk data to understand how these factors relate to the HIV epidemic among transwomen in Peru. Secondary goals were to assess the acceptability and feasibility of using RDS to recruit transwomen in this country and to consider the implications of the findings for the design of appropriate HIV prevention interventions among this population.
Methods
Eligibility
A sociodemographic and sexual risk behavior survey including laboratory based testing for HIV, syphilis and HSV2 was conducted between April and July 2009. Eligibility criteria included identifying as a transwoman, age over 18, having a study coupon and being able to provide written informed consent. Being a transwoman was defined as been born male and identifying as female regardless of initiation or completion of gender enhancement procedures.
Formative Assessment
Both the formative phase and project implementation were carried out with the direct collaboration of Red Trans Peru, a community based organization and Peruvian branch of a Latin-American transgender network that includes local transgender leaders and activists. The study protocol was presented to the organization to elicit their feedback on its feasibility and acceptability. Once agreement to carry out the study was reached, the formative phase started. Four interviews and two focus groups (n = 8) with transwomen were conducted in order to determine the most suitable locations for study sites and operating hours. Six study offices were placed in six different districts giving the study wide coverage of metropolitan Lima. A fieldwork team was formed consisting of two interviewers, a laboratory technician and two counselors. Interviewers and the lab technician were all transwomen.
Concurrent with the formative phase, eight demographically diverse initial participants (seeds) were non-randomly selected with input from key informants to serve as the starting points for recruitment. Criteria for seed selection included leadership in the transwomen community, place of living or social interaction, age and type of work. After completing the interviewer- administered survey and specimen collection each seed was given three study coupons and instructed to invite three transgender acquaintances, who met the eligibility criteria, to participate in the study. Recruitment coupons provided a brief description of the project and the addresses and schedules of all study sites. Each coupon had a unique serial number, which was used as the participants’ identification code for the questionnaire, blood sample, results provision and to track further recruitment. Participation in the study was anonymous.
Measures
The study’s survey explored socio-demographic characteristics including age, educational level, work and region of birth: specifying the individual’s region of birth (Lima/Callao, other coastal cities, cities from the Highlands or Andean Region and cities from the Amazonian or Jungle Region) considering Lima as current city of residence. Gender enhancement/transition procedures were described considering if the respondent had undergone any type of process to appear more feminine. For those who had so we explored the type of procedure undergone (implants, sex reassignment, collagen injection, industrial silicone injection), where was it carried out (public or private health facility, acquaintance or the participants’ own home) and what part of the body was modified. Hormone use was described indicating the way it was administered (pills, injections, gel and patches), who indicated the hormones (health personnel, a friend or the individual by herself) and if there was any subsequent medical supervision. The questionnaire explored sexual behaviors by describing condom use, sexual role (insertive, receptive, both) type of partner (stable, casual, client and other) and drug/alcohol consumption on the last sexual encounter. Condom use in the last 6 months was explored considering usage with clients and with non-commercial partners as separate indicators. The survey was designed in collaboration with Red Trans Peru and personnel from a local STI clinic that offers care to transwomen sex workers. The instrument was piloted among 15 transwomen during the formative phase of the project. The final survey instrument was designed to take approximately 30 min to complete.
Procedures
Study staff explained the study process to eligible participants and obtained written consent before the face-to-face interview. Upon completing the interview, trained personnel offered participants free voluntary counseling and testing for HIV, syphilis and HSV2. A blood sample consisting of 10 ml was collected by a trained lab technician and stored for subsequent analysis. Results were delivered at study sites 1 week after specimen collection where individuals received post-test counseling. Individuals testing positive for HIV were assisted in enrolling at the National HIV/AIDS Program where HIV/AIDS care and treatment, including antiretrovirals, are provided free of charge. Individuals testing positive for syphilis were referred to the public health clinic in their home jurisdiction to receive treatment.
Participants who completed the interview received S/. 20 (approximately US $7), together with a box of 50 condoms and 5 lubricant sachets. Participants who recruited other eligible participants, i.e., referees who were eligible and completed the recruitment process received an additional 10 lubricants and 50 condoms for each of up to 3 possible recruits.
Sample Size
A sample size of 420 was calculated based on an expected HIV prevalence of 25% among transwomen with 95% power based on a precision of ±5% and a design effect of 2 [27].
Laboratory Procedures
HIV testing was performed following the Peruvian Ministry of Health algorithm consisting of enzyme immunoassay screening with Western Blot confirmation. HSV-2 antibody status was determined by type-specific enzyme immunoassay HerpeSelect 2 ELISA IgG (Focus Diagnostics, Cypress, CA). Syphilis infection was tested using rapid plasma reagin (RPR) test (RPR-nosticon II, BioMerieux, Boxtel, Netherlands) to demonstrate infection. To classify infection as chronic or recent (infection within the previous 6 months) RPR titers were observed and specimens with titers of 1:8 or greater were considered recent syphilis infections, in keeping with suggested diagnostic guidelines for delineation of primary and secondary syphilis from latent or cured [28].
Data Analysis
Point estimates and 95% confident intervals (95% CI) were calculated for variables of interest using Respondent Driven Sampling Analysis Tool 5.6 (RDSAT) (www.respondentdrivensampling.org). Estimates are generated by the software by adjusting for participants’ networks sizes and differential recruitment patterns. Demographic, behavioral and biological outcome variables were analyzed in relation to HIV status as the outcome of interest. RDSAT generated weights for the outcome variable were exported and used in multivariable analysis as suggested in the literature [23, 29, 30]. That is, the outcome of interest is analyzed in RDSAT and then individualized weights are exported and merged with the dataset. Further analyses, were weighted using this weight. Variables from the bivariate analysis with Chi square which had a moderate association (P < 0.2) with HIV infection were included in a multiple logistic regression model. Additionally, three multiple logistic regression models were fitted considering HIV (without adjusting for HSV2 and syphilis), HSV2, and syphilis infection (infected/not infected) as outcomes. Multivariable analysis was conducted using STATA 10.0 (College Station, TX). Ethical approval was granted by the Universidad Peruana Cayetano Heredia Human Research Committee.
Results
Sample Characteristics
A total of 450 transwomen were recruited between April and July 2009. Of these, 11 were seeds (8 initial seeds plus 3 additional seeds) and were excluded from the analysis. The coupon return rate was 56%. Table 1 shows the crude and adjusted proportions of key demographic variables. The majority of transwomen in Lima are under 35 years old (70.3%) and are born in Lima (70.5%) while migration stems mainly from the jungle region (18.3%). Most of the population has completed secondary education (44.7%) and 16.8% has higher education. Sex work is the main economic activity (63.9%) followed by hairdressing (27.9%). Basic needs coverage is available to 67.7% of population.
Gender enhancement procedures have been undertaken by 69.8% of the population as shown in Table 2. The commonest procedure is hormone use (82.7%) where the majority accomplishes this by injection (65.9%). Hormones are mainly indicated by a friend (66.7%) and have no medical follow up in 95.2% of individuals. The second most common procedure is the injection of industrial silicone, commonly known as airplane oil, occurring in 39.6% of those who underwent any gender enhancement procedure.
Table 3 shows the assessment of sexual behaviors and prevalence of HIV and other STIs. We describe the characteristics of last sex encounter (LSE): by partner, sex role, alcohol/drug use and condom use. Casual partners (42.3%) are the most common types of partners followed by commercial client (29.7%). Most transwomen engage in receptive anal sex (78.9%). Alcohol or drug use during sexual activity is common in the population (36.8%) while condom use is practiced by 75.1%. Consistent condom use in the last 6 months is higher with commercial clients (72.9%) than with non-commercial partners (51.9%).
Overall HIV prevalence among transwomen in Lima is 29.6%. HSV2 infection is present in 79.4% of the population. RPR positivity for syphilis is 22.9% among transwomen in Lima and recent syphilis infection is 4.8%. HIV and HSV2 co-infection is present in 25.8% of the population. Syphilis (chronic) and HIV is present in 10.7% of transwomen and recent syphilis and HIV infection in 3.7%.
Bivariate Analyses
The exploration of factors associated with HIV infection was carried out starting with bivariate analysis using the Chi-square test. Significant bivariate predictors were chronic syphilis infection (P = 0.007), recent syphilis infection (P = 0.0006) and HSV2 infection (P = 0.025). No association was found between age (P = 0.185), education (P = 0.496), type of work (P = 0.74), having engaged in any gender enhancement/transition procedure (P = 0.48), hormone injection (P = 0.76), industrial silicone injection (P = 0.58), condom use in the last sexual encounter (P = 0.2) condom use with clients in the last 6 months (P = 0.19), condom use with non-commercial partners in the last 6 months (P = 0.14) and HIV infection.
Multivariable Analyses
Table 4 shows a multiple logistic regression analysis considering HIV as outcome (infected/not infected) including all variables with P < 0.2 in the bivariate association, and adjusting for education and type of work. The table also shows results of the bivariate regression analysis, which show calculated unadjusted odds ratios for risk factors. The multiple regression analysis showed increased odds of HIV infection associated with age older than 35 (adjusted odds ratio (AOR 4.7, P = 0.02 95% CI 1.3–17.4), recent syphilis infection (AOR 8.2, P = 0.009, 95% CI 1.7–39.4) and HSV2 infection (AOR 6.3, P = 0.042, 95% CI 1.1–36.2).
Additionally, three models were fitted having HSV2, syphilis and HIV (not including HSV2 and syphilis as covariates) as the outcome (infected/not infected) adjusting for age, educational level, type of work, condom use in the last sexual encounter, condom use in the last 6 months with clients and condom use in the last 6 months with non-commercial partners. Syphilis infection was associated with age 25–35 (OR 8.2, P = 0.007, 95% CI 1.8–37.3) and age > 35 (OR 9.8, P = 0.004, 95% CI 2.1–46.7). HSV2 infection was associated to having attained primary education (OR 13.5, P = 0.001, 95% CI 2.8–64.8). HIV infection was associated with age 25–35 (OR 3, P = 0.045, 95% CI 1.0–11.9) and age > 35 (OR 7.6, P = 0.002, 95% CI 2.1–27.7).
Discussion
The present study is the first quantitative study specifically designed to assess risk of HIV infection among transwomen in Peru, the first to use RDS in the country and to our knowledge one of the largest studies among transwomen in the region. It has allowed us to establish the epidemic profile of a heretofore under-studied population and to determine its demographic characteristics.
Our results when compared to HIV prevalence data among other populations confirm that transwomen in Lima are the group most highly affected by HIV/AIDS in Peru with almost one of every three transwomen infected. Our analysis found an association between HIV infection and HSV-2 infection, recent syphilis and age older than 35 years. Other factors explored in both bivariate and multivariable analysis (age, type of work, body transformation, among others) showed no significant association with HIV status.
The relation between STIs and HIV has been previously demonstrated, but without establishing causality [31–33]. We show elevated rates of concomitant HSV2/HIV and syphilis/HIV infection among transwomen. Other studies in Peru have described similar rates of genital herpes and an a higher rate of recent syphilis in MSM where HIV prevalence is on the order of 10% [34, 35]. In these studies syphilis and HSV2 infection was associated with age and HIV infection. In our study, age was a determinant of syphilis and HIV infection, but not of genital herpes. It is very hard to define a causal relation between HSV2, syphilis and HIV infection in this population. Nonetheless, from a public health perspective our results suggest that HIV and STI treatment and care services should be integrated for traswomen as it has been promoted in other settings [36]. The association of age and HIV infection as in other populations may be explained by accumulated probability of being exposed to the HIV virus over the lifecourse [37].
It becomes necessary to extend the conceptual framework to explain the vulnerability to the epidemic among this group [1, 38]. For transwomen this framework has to consider the interaction of factors that go from the structural level (such as exclusion, marginalization and transphobia) to the individual level (sexual behaviors, affirmation of identity) contributing to a dynamic process of increased vulnerability to HIV/AIDS among this group [7, 8, 39–44].
As a first step, we have been able to describe at a population level some of these factors among transwomen in Lima. Socio-demographic characteristics show a young population mostly born in Lima with an important proportion of internal migrants. Migration can be associated with the search for improvement in standard of living (mainly through sex work), where Lima becomes a bridge for the eventual migration to other countries and/or access to methods to feminize their bodies [21].
The educational level among transwomen is higher than what has been described for MSM in the country [3, 35] and for transwomen of color in the USA [41]. However, this study did not explore whether access to education occurred before individuals started body feminization procedures or assumed gender identity by cross-dressing, which most probably would have decreased access by increasing discrimination. In any case, educational level should be reflected in various types of employment among transwomen. Nonetheless, sex work is the main economic activity in this group, followed by hairdressing, reflecting the lack of opportunities for transwomen in Lima which is consistent with other settings [13, 15, 40, 45, 46]. This finding is an indicator of what has been called secondary victimization: forms of discrimination/victimization (e.g., lack of working opportunities) resulting from processes of victimization that are legal or widely condoned (e.g., systematic rejection of transwomen by society) [47].
Several studies have shown that sex work among transwomen occurs mainly on the street and in a potentially violent environment [19, 42, 48] and is associated with substance use [17, 46]. At the individual level some transwomen may get involved in sex work as a way to affirm their identity [46]. This could be translated to unsafe sex, driven by fear or isolation, or lack of condom use if for example they feel physical attraction for the customer [17, 19, 44]. All this suggests that prevention interventions among transwomen sex workers should include activities such as education on rights, empowerment, self-esteem and strengthening the awareness of authorities to reduce systematic violence [21].
Body modification procedures are a potentially important part of transwomens’ identity affirmation through the pursuit of a body consistent with their gender identification and it has been described in different countries and cultural contexts [10, 21, 44]. We show the main features of these processes in the city of Lima, which have been seldom studied: Gender enhancement occurs outside the health system and could be seen as an expression of exclusion and marginalization. While hormones are the main substance used by transwomen as in most parts of the world [10, 49], in Lima, in the majority of cases these are provided by an acquaintance and use of which is not medically supervised. Studies in the USA have shown that hormone therapy provision may stimulate transwomen to access to health programs (including HIV prevention programs), and improve their quality of life [15, 50]. This is not the case for our context were no public medical facilities offer these services and where there is also a widespread use of industrial silicone injection as shown by our investigation. Other countries like Brazil have established harm reduction programs to provide clean needles to transwomen for hormone and silicone injection [51]. We consider that there is no evidence to promote such programs in our country: The deleterious effects of the use of industrial silicone have been previously described [52] and consistent with other studies [43, 53] we have not found an association between HIV infection and hormone or industrial silicone injection. We however did not collect data on needle sharing for hormone or silicone injection, a practice which could increase risk to HIV and other infections. Further research is needed in this area including the perceptions and beliefs of this population about gender enhancement processes. Efforts should be focused on implementing programs for transwomens’ health that go beyond STI control, and include proper conditions of gender enhancement procedures, a potentially neglected human right in this population.
Feasibility of RDS and Study Limitations
It is important to highlight the potential utility of RDS for surveillance studies among a population of transwomen in Peru. In a period of 3 months it was possible to reach a sample of 450 transwomen. The process produced the formation of different chains of participants from various areas of Lima and a number of waves (stages in the chain of recruitment) sufficient to ensure a sample with balanced demographic characteristics representing the full spectrum of transwomen in Lima. This method is, therefore, feasible for studies with this population and reinforces the need to use techniques to develop estimates with higher levels of representation in a group that constitutes a tight network than those methods based on convenience samples. However, it must be stressed that RDS is based on fixed assumptions about the functioning of social networks and interactions of individuals [22, 53]. These assumptions are not always met, and often remain in the realm of theory, which limits the validity of estimates obtained [54]. Furthermore, although there are publications that have used individualized weights generated by RDSAT for multivariate analysis [24, 30], estimates obtained have limitations for the interpretation of results. For example, weights only consider homphily of the outcome variable (HIV in this case) and not those of the other variables in the model.
Some topics such as substance abuse or exposure to violence were not included in the present study. During the formative phase the research team realized that the time it took to complete the interview was a relevant issue to secure the participation of individuals. Therefore, some variables had to be excluded from the questionnaire to reduce interview length. These topics, along with investigations exploring the different levels of vulnerability (structural, environmental and individual) need to be included in future studies among this population.
Final Comments
It is most likely the complex interaction of several factors among transwomen that explains the extremely high HIV prevalence found. For many years the trend in public health when addressing vulnerable groups has explained risk for infection through individual behaviors such as not using condoms or high partner turnover [1]. While the literature has shown that these behaviors increase the risk of HIV and prevention programs should seek to reduce these risk behaviors, this approach is insufficient to explain the rate of HIV found among transwomen in our study. Future research should focus on the analysis of the environment, community and individual contexts in the lives of transwomen in our country in order to elucidate their vulnerability. From a public health perspective, there is a need to translate this approach into a comprehensive response to HIV among transwomen, while differentiating them from MSM and transcending the already known biomedical risk factors.
References
Caceres CF, Aggleton P, Galea JT. Sexual diversity, social inclusion and HIV/AIDS. AIDS. 2008;22(Suppl 2):S45–55.
Caceres CF. HIV among gay and other men who have sex with men in Latin America and the Caribbean: a hidden epidemic? AIDS. 2002;16(Suppl 3):S23–33.
Sanchez J, Lama JR, Kusunoki L, et al. HIV-1, sexually transmitted infections, and sexual behavior trends among men who have sex with men in Lima, Peru. J Acquir Immune Defic Syndr. 2007;44(5):578–85.
van Griensven F, de Lind van Wijngaarden JW, Baral S, Grulich A. The global epidemic of HIV infection among men who have sex with men. Curr Opin HIV AIDS. 2009;4(4):300–7.
Tabet S, Sanchez J, Lama J, et al. HIV, syphilis and heterosexual bridging among Peruvian men who have sex with men. AIDS. 2002;16(9):1271–7.
Clements-Nolle K, Marx R, Guzman R, Katz M. HIV prevalence, risk behaviors, health care use, and mental health status of transgender persons: implications for public health intervention. Am J Public Health. 2001;91(6):915–21.
Nemoto T, Operario D, Keatley J, Han L, Soma T. HIV risk behaviors among male-to-female transgender persons of color in San Francisco. Am J Public Health. 2004;94(7):1193–9.
Nuttbrock L, Hwahng S, Bockting W, et al. Lifetime risk factors for HIV/sexually transmitted infections among male-to-female transgender persons. J Acquir Immune Defic Syndr. 2009;52:417–21.
Pisani E, Girault P, Gultom M, et al. HIV, syphilis infection, and sexual practices among transgenders, male sex workers, and other men who have sex with men in Jakarta, Indonesia. Sex Transm Infect. 2004;80(6):536–40.
Herbst JH, Jacobs ED, Finlayson TJ, McKleroy VS, Neumann MS, Crepaz N. Estimating HIV prevalence and risk behaviors of transgender persons in the United States: a systematic review. AIDS Behav. 2008;12(1):1–17.
Caceres CF, Mendoza W, Konda K, Lescano A. Nuevas Evidencias para las políticas y programs de salud en VIH/SIDA e infecciones de transmisión sexual en el Perú. Lima: UPCH; 2007.
Caceres CF, Giron JM, Sandoval C, et al. Implementation effects of GFATM-supported HIV/AIDS projects on the health sector, civil society, affected communities in Peru–2007. Glob Public Health. 2004;13:1–19.
Melendez RM, Pinto R. ‘It’s really a hard life’: love, gender and HIV risk among male-to-female transgender persons. Cult Health Sex. 2007;9(3):233–45.
Ramirez-Valles J, Garcia D, Campbell RT, Diaz RM, Heckathorn DD. HIV infection, sexual risk behavior, and substance use among Latino gay and bisexual men and transgender persons. Am J Public Health. 2008;98(6):1036–42.
Sevelius JM, Reznick OG, Hart SL, Schwarcz S. Informing interventions: the importance of contextual factors in the prediction of sexual risk behaviors among transgender women. AIDS Educ Prev. 2009;21(2):113–27.
Wilson EC, Garofalo R, Harris DR, Belzer M. Sexual risk taking among transgender male-to-female youths with different partner types. Am J Public Health. 2010;100(8):1500–5.
Salazar, X. Resultados de los grupos focales con trabajadoras sexuales travestis sobre el trabajo sexual y los clientes. Lima, 2008.
De Santis JP. HIV infection risk factors among male-to-female transgender persons: a review of the literature. J Assoc Nurses AIDS Care. 2009;20(5):362–72.
Silva-Santisteban A, Salazar X. Informe final de mapeo y encuesta sociodemográfica del trabajo sexual en cuatro ciudades del Perú. Lima: UNFPA; 2009.
Caceres CF, Segura E, Silva-Santisteban A, et al. Non-conforming gender identification as determinant of lower HIV care access among people living with HIV in Peru: the HIV, economic flows and globalization study [WEPE0766]. Presented at AIDS 2010—XVIII International AIDS Conference.
Salazar X, Villayzan J. Outlines for multisectorial work with transgender populations, human rights, sex work and HIV/AIDS. Lima: IEESDEH, UNFPA; 2010.
Heckathorn DD. Respondent driven sampling: a new approach to the study of hidden populations. Soc Probl. 1997;44(2):174–99.
Johnston LG, Khanam R, Reza M, et al. The effectiveness of respondent driven sampling for recruiting males who have sex with males in Dhaka, Bangladesh. AIDS Behav. 2008;12(2):294–304.
Lane T, Raymond HF, Dladla S, et al. High HIV prevalence among men who have sex with men in Soweto, South Africa: results from the Soweto men’s study. AIDS Behav. 2011;15(3):626–34.
Malekinejad M, Johnston LG, Kendall C, Kerr LR, Rifkin MR, Rutherford GW. Using respondent-driven sampling methodology for HIV biological and behavioral surveillance in international settings: a systematic review. AIDS Behav. 2008;12(4 Suppl):S105–30.
Magnani R, Sabin K, Saidel T, Heckathorn D. Review of sampling hard-to-reach and hidden populations for HIV surveillance. AIDS. 2005;19(Suppl 2):S67–72.
Salganik MJ. Variance estimation, design effects, and sample size calculations for respondent-driven sampling. J Urban Health. 2006;83(6 Suppl):i98–112.
Larsen SA, Steiner BM, Rudolph AH. Laboratory diagnosis and interpretation of tests for syphilis. Clin Microbiol Rev. 1995;8(1):1–21.
Heckathorn D. Extensions of respondent-driven sampling: analyzing continuous variables and controlling for differential recruitment. Sociol Methodol. 2007;37:151–207.
Ruan S, Yang H, Zhu Y, et al. Rising HIV prevalence among married and unmarried among men who have sex with men: Jinan, China. AIDS Behav. 2009;13(4):671–6.
Corey L, Wald A, Celum CL, Quinn TC. The effects of herpes simplex virus-2 on HIV-1 acquisition and transmission: a review of two overlapping epidemics. J Acquir Immune Defic Syndr. 2004;35(5):435–45.
Lama JR, Lucchetti A, Suarez L, et al. Association of herpes simplex virus type 2 infection and syphilis with human immunodeficiency virus infection among men who have sex with men in Peru. J Infect Dis. 2006;194(10):1459–66.
Zetola NM, Bernstein KT, Wong E, Louie B, Klausner JD. Exploring the relationship between sexually transmitted diseases and HIV acquisition by using different study designs. J Acquir Immune Defic Syndr. 2009;50(5):546–51.
Snowden JM, Konda KA, Leon SR, et al. Recent syphilis infection prevalence and risk factors among male low-income populations in coastal Peruvian cities. Sex Transm Dis. 2010;37(2):75–80.
Konda KA, Klausner JD, Lescano AG, et al. The epidemiology of herpes simplex virus type 2 infection in low-income urban populations in coastal Peru. Sex Transm Dis. 2005;32(9):534–41.
Centers for Disease Control and Prevention. Program collaboration and service integration: enhancing the prevention and control of HIV/AIDS, viral hepatitis, sexually transmitted diseases, and tuberculosis in the United States. Atlanta: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; 2009.
Hall HI, An Q, Hutchinson AB, Sansom S. Estimating the lifetime risk of a diagnosis of the HIV infection in 33 states, 2004–2005. J Acquir Immune Defic Syndr. 2008;49(3):294–7.
Parker R, Aggleton P. HIV and AIDS-related stigma and discrimination: a conceptual framework and implications for action. Soc Sci Med. 2003;57(1):13–24.
Kosenko KA. Contextual influences on sexual risk-taking in the transgender community. J Sex Res. 2010;24:1–12.
Lombardi EL, Wilchins RA, Priesing D, Malouf D. Gender violence: transgender experiences with violence and discrimination. J Homosex. 2001;42(1):89–101.
Lombardi E. Varieties of transgender/transsexual lives and their relationship with transphobia. J Homosex. 2009;56(8):977–92.
Infante C, Sosa-Rubi SG, Cuadra SM. Sex work in Mexico: vulnerability of male, travesti, transgender and transsexual sex workers. Cult Health Sex. 2009;11(2):125–37.
Nuttbrock L, Hwahng S, Bockting W, et al. Lifetime risk factors for HIV/sexually transmitted infections among male-to-female transgender persons. J Acquir Immune Defic Syndr. 2009;52(3):417–21.
Bockting WO, Robinson BE, Rosser BR. Transgender HIV prevention: a qualitative needs assessment. AIDS Care. 1998;10(4):505–25.
Garofalo R, Deleon J, Osmer E, Doll M, Harper GW. Overlooked, misunderstood and at-risk: exploring the lives and HIV risk of ethnic minority male-to-female transgender youth. J Adolesc Health. 2006;38(3):230–6.
Nemoto T, Operario D, Keatley J, Villegas D. Social context of HIV risk behaviours among male-to-female transgenders of colour. AIDS Care. 2004;16(6):724–35.
Berrill KT, Herek GM. Primary and secondary victimization in anti-gay hate crimes: official response and public policy. J Interpers Violence. 1990;5:401–13.
Operario D, Soma T, Underhill K. Sex work and HIV status among transgender women: systematic review and meta-analysis. J Acquir Immune Defic Syndr. 2008;48(1):97–103.
Wimonsate W, Naorat S, Varangrat A, et al. Risk behavior, hormone use, surgical history and HIV infection among transgendered persons (TG) in Thailand, 2005 [MOPE0349]. Presented at AIDS 2006—XVI International AIDS Conference.
Newfield E, Hart S, Dibble S, Kohler L. Female-to-male transgender quality of life. Qual Life Res. 2006;15(9):1447–57.
Gagizi E, Ferreira E, Abbate MC. Biosecurity on using industrial liquid silicon and female sexual hormones by transvestis and transgenders in São Paulo City, Brazil [CDC1677]. Presented at AIDS 2006—XVI International AIDS Conference.
Hage JJ, Kanhai RC, Oen AL, van Diest PJ, Karim RB. The devastating outcome of massive subcutaneous injection of highly viscous fluids in male-to-female transsexuals. Plast Reconstr Surg. 2001;107(3):734–41.
Heckathorn DD. Respondent driven sampling II: deriving valid population estimates from chain-referral samples of hiddenpopulations. Soc Probl. 2002;49(1):11–34.
Burt RD, Hagan H, Sabin K, Thiede H. Evaluating respondent-driven sampling in a major metropolitan area: comparing injection drug users in the 2005 Seattle area national HIV behavioral surveillance system survey with participants in the RAVEN and Kiwi studies. Ann Epidemiol. 2010;20(2):159–67.
Acknowledgments
This study was conducted in all its phases in collaboration with Red Trans Peru, an organization that brings together transwomen from across the country and performs important work to pursue the fulfillment of rights of transwomen. It would not have been possible to design the instrument or the logistics of a feasible study without the participation of the population, demonstrating the important synergy obtained in a horizontal work between academia and grassroots organizations in research processes. Study funded by amfAR, American Foundation for AIDS Research (Grant no. 107266-44-IAMM).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Silva-Santisteban, A., Raymond, H.F., Salazar, X. et al. Understanding the HIV/AIDS Epidemic in Transgender Women of Lima, Peru: Results from a Sero-Epidemiologic Study Using Respondent Driven Sampling. AIDS Behav 16, 872–881 (2012). https://doi.org/10.1007/s10461-011-0053-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-011-0053-5