Abstract
More than 30 years into the HIV epidemic, men who have sex with men (MSM) continue to be disproportionately impacted. It is estimated that worldwide nearly half of MSM infected with HIV are unaware of their status, making HIV testing along with early linkage to care crucial to HIV prevention efforts. However, there remain significant barriers to HIV testing among MSM, due largely to complex issues of layered stigma that deter MSM from accessing traditional, clinic-based testing. We conducted a review and synthesis of the literature on strategies to increase uptake of HIV testing among MSM. We found that social network-based strategies, community-based testing, HIV self-testing, and modifications to the traditional clinic-based model can effectively reach a subset of MSM, but success was often context-specific and there are significant gaps in evidence. We provide recommendations for increasing HIV testing rates and status awareness among MSM.
Resumen
Después de más de treinta años, los hombres que tienen sexo con hombres (HSH) continúan siendo afectados desproporcionadamente por el VIH. Se estima que, mundialmente, casi la mitad de los HSH infectados con el VIH desconocen su estado, haciendo que las pruebas de VIH junto con el vínculo temprano con la atención sean cruciales para los esfuerzos de prevención del VIH. Sin embargo, sigue habiendo barreras significativas para las pruebas de detección de VIH entre HSH, debido en gran parte a problemas complejos y cumulativos de estigma que impiden que los HSH accedan a las pruebas tradicionales basadas en la clínica. Se realizó una revisión y síntesis de la literatura sobre estrategias para aumentar las pruebas del VIH entre los HSH. Encontramos que las estrategias basadas en redes sociales, las pruebas basadas en la comunidad, las auto-pruebas del VIH y modificaciones al modelo clínico tradicional pueden llegar efectivamente a un subconjunto de HSH, pero el éxito suele ser específico al contexto y existen brechas significativas en la evidencia. Proporcionamos recomendaciones para aumentar las tasas de detección del VIH y la conciencia del estado entre los HSH.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Despite many public health successes in HIV prevention and treatment, the epidemic among men who have sex with men (MSM) continues to spread globally [1]. Much of the spread can be attributed to the large number of individuals who are unaware of their infection. The World Health Organization (WHO) estimates that nearly half of those infected with HIV worldwide are unaware of their status [2]. HIV testing and early linkage to care are critical for improving long-term individual health outcomes and preventing new HIV infections. Late-testing –presenting for testing late in the course of HIV infection—continues to fuel the epidemic as it leads to delayed treatment and thus increased transmission [3]. However, there remain significant individual, structural, and social barriers to HIV testing among MSM. Fear of knowing one’s status, low risk perception, anticipated stigma and discrimination, and conspiracy beliefs comprise individual barriers to testing uptake [4,5,6,7]; structurally, negative encounters with medical professionals, concerns about confidentiality, stigma, and medical distrust keep MSM from accessing clinics [6, 8, 9].
Increasing testing uptake and frequency among the most vulnerable groups, including MSM, is a critical to reaching the UNAIDS target that 90% of all persons living with HIV are aware of their status, and is the first step towards an world free of new HIV infections [10, 11]. Over the course of the epidemic, a number of strategies have been used to reach MSM and deliver HIV testing, including modifying clinic-based services, testing in the community setting, utilizing social marketing and social networks, and more recently HIV self-testing. The variety of initiatives and effectiveness of these strategies has varied across contexts, specifically geographic location, setting, and MSM community characteristics. To date, the evidence for these multiple strategies has not been distilled into recommendations intended to guide improved testing for HIV among MSM across different contexts. To fill this gap, we conducted a review and comprehensive synthesis of the published literature on strategies aimed at increasing HIV testing among MSM. Here we present our results and recommendations for effective and promising testing approaches.
Methods
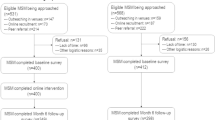
We searched PubMed, Web of Science, and Google Scholar using combinations of the following terms: MSM; gay and bisexual men; men who have sex with men; HIV; testing; uptake; strategies; HIV testing; and intervention. We limited our search to articles that were published in English, between 2005 and 2016 and that: (1) had MSM as the target population or included MSM as part of a larger sample and reported MSM-specific findings; (2) described strategies or interventions intended to increase testing among MSM and; (3) reported findings that included the number or proportion diagnosed with HIV, the testing profile of the MSM reached (i.e., time since last test), and/or whether there was an increase in testing uptake or recent testing. We excluded studies that only measured acceptability or participant satisfaction. We included articles published in peer reviewed journals, and excluded dissertations and conference abstracts. In total, we identified 1759 articles, of which 1172 were duplicates and 316 did not meet inclusion criteria, based on the title and abstract. The full text of 271 articles from six different regions around the world were downloaded for detailed review. A total of 78 articles met the above criteria for inclusion, including 34 from North America, 22 from Europe and Australia, 9 from Asia, 4 from Latin America, and 4 from Africa (Fig. 1).
Strategies to increase HIV testing could be sorted into two broad categories—test promotion (i.e., strategies to reach and recruit MSM) and test delivery. The evidence could be further subcategorized into four approaches for reach and recruitment: (1) internet strategies; (2) social marketing; (3) social networking strategies; (4) partner counseling and referral services; and three approaches for test delivery: (1) clinic-based strategies; (2) community-based testing; and (3) HIV self-testing (HIVST). It is worth noting that a number of the studies fall into multiple categories, though we categorized them based on the primary strategy being utilized. We offer examples in each category and key evidence is summarized in Table 1.
Results: Strategies for Test Promotion to MSM for Testing
Internet and Social Media
We identified nine articles reporting findings from interventions employing internet- and app-based strategies to encourage men to seek out HIV testing, either in clinic or community settings. These strategies range from banner ads on popular and/or MSM-specific websites, to engaging in chat rooms on existing sites, to creating new apps and intervention-specific websites. Overall, these strategies have demonstrated moderate effectiveness in reaching men across multiple contexts who do not test or test infrequently.
Evidence from the U.S. includes a repeated cross-sectional matched community randomized trial in the South, where the intervention consisted of promoting educational messages about the importance of HIV testing across multiple social media and partner-seeking websites (e.g. Adam4Adam; Black Gay Chat; Gay.com; Craigslist). Self-reported testing rates in the previous 12 months, which were similarly around 35% at baseline, increased significantly among intervention verses comparison participants (63.7% vs. 42%) [12]. In another study, trained interventionists promoted messages about the importance of testing in existing online chat rooms [13]. With this intervention, there was a significant increase in the odds of self-reported testing and a reduction in the proportion of men who had not tested in the previous 12 months from 55.5% at pretest to 40.6% at posttest. Lastly, investigators in the U.S. implemented a testing locator app, which tailored referrals to the demographics and testing barriers identified by participants [14]. Those in the control group had access to an online provider directory but no tailored content. While not statistically significant, for those who had never previously tested, a larger proportion of men that received the tailored locator reported having tested when compared to the control group.
Two studies in Peru also reported success in using technology to encourage MSM to attend clinics for testing. One study randomized gay and non-gay identified MSM to watch a 5-min online video focused on helping MSM overcome barriers to testing or to receive a standard public health text message from an ongoing HIV prevention campaign. Among the non-gay identified MSM, those exposed to the video were significantly more likely to attend the clinic for HIV testing, though findings were null among gay-identified men [15]. In the other study, peer health educators discussed prevention with participants in a Facebook group. Compared to the control group, who received standard care and joined a separate Facebook group for basic information, those in the intervention group were significantly more likely to get tested at a local clinic, which verified testing with study staff [16].
In Asia, advertisements and intervention websites to provide sexual health information and link men to HIV testing sites were used in a study in China in which 429 MSM were recruited through internet outreach, and 97.9% received HIV testing following the internet promotion efforts [17]. Of those, 52.1% had never tested before and 4.8% tested positive. In a study in Thailand [18], 15.5% of 1181 MSM recruited online and referred to an HIV testing clinic or private hospital received a positive diagnosis, demonstrating feasibility of accessing high risk MSM online. Lastly, in Taiwan, internet popular opinion leaders provided information, advice, and support to MSM in a study-specific, private Facebook group [19]. MSM were recruited through web banner ads and email messaging through Facebook. A control group was also recruited through a gay-specific social networking site but received no information about testing. At follow up, those in the Facebook group were significantly more likely to report having tested in the previous six months.
In summary, these data suggest that internet and social media strategies are promising for HIV test promotion among MSM that may not be accessible through more traditional gay venues, including men who do not identify as gay, who are not active participants in the gay community, or who have both male and female partners [13]. Social media and internet strategies can reach men where they are expressing their sexuality and may be most comfortable receiving these prevention messages [12]. These strategies can be an important tool in settings where the MSM community is dispersed and where recruitment venues (gay venues) are few or non-existent. For example, the public health department in a suburban county in California that lacked gay venues for traditional outreach saw a 1500% increase in the number of contacts they made with MSM by using Grindr, though testing outcomes were not reported [20]. Further, internet and social media strategies may be particularly useful for reaching MSM in settings with high levels of homophobia and HIV stigma, as noted in published studies from Peru [15], Thailand [18], and China [17] given the relative anonymity and social influence which online communities can provide [21]. Further, testing recommendations can be tailored to the specific participant-identified barriers, such as lack of knowledge of testing facilities or being afraid that testing staff will be judgmental [14]. There is a gap in the literature around use of internet-based strategies in Africa, where access to on-line media and apps is more restricted.
Social Marketing Campaigns
Social marketing, defined by Grier and Bryant as “the use of marketing to design and implement programs to promote socially beneficial behavior change” [22], has been employed to effect changes in HIV risk and testing behavior for decades [23, 24]. We found one randomized controlled trial and 11 evaluation studies exploring the effectiveness of social marketing campaigns to increase HIV testing; not all were specifically focused on MSM and the findings were mixed.
Three studies in urban centers in North America showed positive effects on testing behavior. In Seattle in 2014, the Tu Amigo Pepe campaign, a small pilot evaluation among 50 men, saw increases in the proportion of men who had ever tested over the course of the campaign [25]. A campaign in Canada ran from 2011 to 2012, which was paired with extended clinic hours and additional testing sites, led to a 20 and 23% increase in testing among MSM in Toronto and Ottawa, respectively [26]. In Vancouver, two campaigns to increase diagnoses of acute HIV infection ran between 2009 and 2011. The campaigns were paired with pooled nucleic acid amplification testing (NAAT), which can detect HIV infection within 2 weeks of transmission, and testing at local clinics. Both the volume of HIV tests and the number of diagnoses of acute HIV infections increased significantly among MSM at the study clinics. However, the authors were unable to determine whether the NAAT testing itself or the social marketing campaigns were responsible for these increases [27].
In contrast, a number of studies found that social marketing campaigns were ineffective in increasing testing. One Australian study initially showed success in increasing HIV testing among MSM, but this effect could not be distinguished from an overall increasing trend in testing that started before the campaign [28, 29]. Similarly, five other studies in Europe and North America were unable to find a significant association between campaign exposure and increased testing among MSM [30,31,32,33,34,35].
The only randomized trial of a social marketing program, conducted in China, sought to compare the impact of a crowdsourced social marketing video with that of an evidence-based video on the testing behavior of MSM who had never been tested for HIV. The crowdsourced video was developed by community members through a public contest whereby videos submitted were judged by a panel of researchers, community, public health, and marketing experts. In both groups approximately one-third of participants got tested within 4 weeks of the campaign, suggesting that the more cost effective crowdsourced message was as effective as the evidence-based message developed by marketing and public health experts [36].
While social marketing campaigns have been widely used to promote testing among general populations, the existing evidence is insufficient to demonstrate consistent effectiveness targeting and increasing testing among MSM.
Partner Counseling and Referral Services
Partner counseling and referral services (PCRS) (also referred to as “partner services”, “partner notification”, and “partner referral”—all hereafter referred to as PCRS) has been utilized for STI prevention and treatment by health departments for many years [37]. A review of PCRS published in 2007 included nine studies, all published in the United States, and nearly all of which included MSM [37]. The review focused on the proportion of individuals receiving testing through PCRS and the proportion newly diagnosed. The authors found relatively consistent results in improving HIV testing outcomes across studies. On average, 67% of named partners were contacted, of which 63% were tested, and an average of 20% of tested partners were newly HIV infected. They conclude that PCRS is an important and effective strategy.
Our review yielded 13 additional studies that examined the efficacy of PCRS and drew similar conclusions. For example, two studies in San Francisco examined outcomes of third-party PCRS, in which a health department staff member notifies named partners. One found that between 2004 and 2006, 679 MSM identified 218 partners that were tested for HIV, and, of those, 10.5% were newly diagnosed with HIV [38]. Another study found that from 2004 to 2008, 200 MSM named partners were tested and 22% were newly diagnosed with HIV [39]. Similar programs in Seattle [40] and Edmonton [41] have reported rates of new diagnoses, among partners referred for testing, between 7.7 and 14%. In a study from the Netherlands, 15.3% of named partners of index patients were diagnosed with HIV [42]. Subsequently, training was implemented for STI professionals to improve PCRS, and a follow up study was conducted in which 21.2% of those referred by partners were diagnosed with HIV [43]. At two clinics in Barcelona, either the index patient or a public health worker contacted a total of 199 partners of HIV-positive MSM, of whom 141 were tested and 18.4% tested newly positive [44].
The only study of PCRS we identified outside of the US, Europe, and Australia was conducted in China [45]. Building on an HIV testing programs for MSM in two Chinese cities the authors compared PCRS testing outcomes for partners referred by newly diagnosed MSM index cases with those of partners referred by previously diagnosed MSM index cases. Partners who tested positive were also asked to refer their partners. The positivity rate was 10.1% in the first round of referrals and 28.6% in the second round. The positivity rate was higher among partners of newly diagnosed index cases compared to partners of previously diagnosed index cases.
Finally, a recent review of PCRS studies utilizing internet and text notifications to reach partners found that these strategies have largely been used as an addendum to existing, traditional PCRS services [46]. Two studies compared the effectiveness of these new strategies to traditional PCRS only. One study found contact rates were lower using internet/text (49.7% vs. 69%), as was the proportion of partners agreeing to be tested (80.7% vs 95.4%), though, the positivity rate was similar (26.8%) compared to traditional PCRS (29.9%) [47]. The other study found that the proportion of named partners contacted through text partner service (txPS) were higher (77%) than traditional PCRS or internet notification, though larger proportions of those notified through traditional PCRS were tested and newly diagnosed (13%) as compared to internet (10%) and text notification (5%) [48]. These strategies appear to be useful options for reaching partners that may not otherwise be reached.
PCRS is particularly well-situated to reach those who may not have otherwise tested due to any of the documented barriers to testing, including low risk perception or lack of symptoms. This is reflected in findings from the San Francisco PCRS program that 17% of those newly diagnosed with HIV had never tested, and 44% had not tested in the previous 2 years [49]. Further, 22% of those newly diagnosed reported that partner notification was the reason for their getting tested. Studies show good evidence of efficacy in urban centers in the US, Europe, and Australia. Arguably, this is due to the existence of large LGBT communities and well-resourced public health departments. In contrast, high levels of HIV-stigma and homophobia present substantial challenges to partner notification [45]. While this Chinese study demonstrated feasibility, there is no evaluative evidence of its effectiveness over time in China. In sum, the evidence suggests that PCRS is quite effective in resource-rich countries where health departments actively implement this strategy. We did not find any evidence of PCRS for MSM being evaluated in any Latin American or African countries, where provider–client ratios are lower and health departments have fewer resources.
Social Network Strategies
Social networks have increasingly been utilized to reach key populations for HIV testing. The underlying premise is that people in the same social networks likely have similar risk behaviors, and that they know and trust each other [50]. Social network strategies (SNS) typically consisted of recruiting “seeds,” an initial group of participants, who then recruit peers from their own social network to participate in the same study or testing campaign [51]. We found nine studies that employed SNS to reach MSM for HIV testing. For example, in a San Francisco study, ten African American MSM seeds each received three coupons, redeemable for testing at an HIV counseling and testing site, to distribute to members of their social networks [52]. Through multiple waves of recruitment in which testers were asked to recruit members of their own networks, a total of 256 MSM social network members were tested, of whom 5% tested newly positive. Nearly half of the testers in this study had not tested in the previous 12 months. Neither the seeds nor the social network members received incentives in this study. Three other U.S. studies conducted in urban centers were also successful at reaching MSM through their social networks [53,54,55,56]. However, unlike the first study, each of these studies provided incentives to peer recruiters and testers. The proportions of never-testers ranged from 6 to 68%, and the HIV positivity rate of those previously undiagnosed ranged from 4 to 11%. While PCRS studies show success in identifying undiagnosed infections, the positivity rates in these studies are lower than those of PCRS studies in the same urban centers.
Similar studies have been conducted to reach MSM in five African countries. In Ghana, MSM testing and support group clients were recruited to act as peer seeds [57]. Among the MSM social network members tested, 32.9% tested positive, 39.8% reported having never tested and 21.7% hadn’t tested in the previous year. In Soweto, South Africa, 378 MSM were tested through an SNS strategy, of which only 37.9% of the sample had ever tested, and 20.6% tested positive [58]. In another study conducted in Lesotho, Swaziland, and Malawi, 23 initial seeds accrued 982 MSM social network testers through successive waves of recruitment, in which testers in each wave were then recruited to act as seeds. The proportion that had never tested was between 19 and 40%, and positivity rate ranged from 15 to 31% [59]. In each of these studies seeds and social network testers received incentives.
Lastly, one study employed a peer educator strategy in three cities in China’s Anhui Province, where twelve seeds recruited network members to participate in an intervention intended to reduce HIV risk behavior and increase HIV testing among MSM [60]. A total of 218 social network members were recruited to the intervention. After the intervention, the rate of reported testing in the previous 2 months increased from 15.1 to 52.4%.
Each of these studies was effective in reaching MSM and demonstrates evidence for increasing testing among non- and infrequent testers, though it is difficult to separate the impact of incentives and the use of social connections. The SNS strategies did not yield as many new positives as PCRS in large urban settings, however, SNS appears quite successful in contexts where providers and programs have less ready access to the target population. The primary strength of the social networking strategy is its ability to reach those who are not likely to seek out testing and are not ready accessible to public health programs and providers, including those who have concerns about confidentiality, or have had negative experiences with the healthcare system. Being reached and encouraged to test by people in their own network whom they trust may neutralize some of the negative impact of HIV-stigma and homophobia on testing behaviors. Further, in Lesotho, with each subsequent wave of recruitment the proportion of MSM identifying as gay or homosexual decreased [59] suggesting that SNS can eventually reach deeper into networks and offer testing to those who are not “out”. These social networks exist throughout the world, with some more hidden than others, making social network testing appropriate in a broad array of settings, including sub-Saharan Africa and likely Latin America, though no studies were available to review in the Latin American context.
Comparative Studies
We also identified several studies that compared the effectiveness of different strategies to promote HIV testing among MSM. Three studies in North America compared the social networking strategy (SNS), PCRS, and alternative venue testing (AVT) (e.g., testing in bars, sex clubs, street corners, community centers, which is included in our review as a test delivery strategy) to reach African American MSM for testing. In a New York City study, the SNS and PCRS strategies had 3.6 times and 2.5 times greater odds, respectively, of identifying a new positive result when compared to AVT [61]. In another study in Washington, DC, MSM reached through AVT and SNS were less likely to have tested previously when compared to men reached through PCRS [62]. However, in this study, the greatest proportion of newly diagnosed positives was found among those tested through PCRS (11%), followed by SNS (10%), and AVT (5%). In contrast to the New York and Washington DC studies, which were conducted by community-based organizations, a study conducted by the Baltimore City Health Department used a stepwise approach, where those tested through AVT were then assigned to act as peers in SNS, or to become a PCRS index partner [63]. The new positivity rate in the AVT sample was 9.2%. No new positives were identified by the social networking or PCRS strategies. The authors posit that this finding may be due to very small sample sizes in the PCRS and SNS strategies, and a difficulty in getting positive MSM to participate in notification and referrals. Overall, these comparative studies further bolster the findings of the SNS and PCRS studies that, for MSM, particularly urban African American MSM, using a social network approach is an effective way of reaching those that are non- or infrequent testers and may be undiagnosed.
Results: Strategies to Deliver HIV Testing
Clinic-Based Strategies
Testing in clinical settings has been the mainstay of HIV diagnosis. Numerous strategies have been employed to increase testing uptake among MSM in clinical settings and to improve the efficiency of case finding. Most clinic strategies fall under two categories—altering or expanding services or establishing MSM-friendly services.
Altering or Expanding Existing Services
Opt-out testing in all healthcare settings has been recommended by the CDC [64] and the United Stated Prevention Services Task Force [65]. A number of jurisdictions have employed this strategy in an effort to increase testing among key populations, noting large increases in HIV testing uptake as compared to previous rates when testing was offered upon request. In Arizona, the STD clinic replaced referrals for HIV testing to an opt-out HIV testing strategy, resulting in a huge increase in HIV testing—from 10 to 68.1% of STD patients. In the first 18 months, a total of 643 MSM tested, of which 41 (6.4%) tested positive [66]. Public health programs in Washington State implemented opt-out HIV testing and PCRS for all MSM with a new STI diagnosis [67], yielding increases in test delivery but no significant increase in HIV case detection. Success has also been documented in the Netherlands, where implementing opt out testing resulted in increases in testing uptake from 82–84% to 97–98% of MSM attending STI clinics [68, 69].
Implementing counseling and testing services tailored to key populations has also improved HIV testing uptake in Madrid [70], where one program in seven primary care clinics achieved a positivity rate of HIV among MSM of 6.3%, with 21.3 percent of MSM having never previously tested. In Melbourne, Australia, a public primary care clinic serving mostly MSM employed a sexual health practice nurse to focus on HIV/STD services [71]. Within the clinic implementing the public health nurse intervention, there was a significant increase (from 52 to 57%) in the proportion of MSM receiving HIV tests compared to the period preceding the introduction of the sexual practice nurse and an equivalent decrease in testing in a comparison clinic with no sexual health practice nurse.
Creating MSM-Friendly Testing Environments
In a study in three French cities (Paris, Nice, and Marseille), after-hours testing, conducted by community members from a local community based organization (CBO), was offered in volunteer counseling and testing centers [72] and compared to outcomes from the standard clinic setting during normal business hours. The positivity rate was lower (1.4% compared to 2.5%) in the after hours, community-based program, though MSM in the community-based program were less frequent testers. In Ottawa, Canada, “Gay Zone”, an MSM specific clinic was established one evening per week within an existing clinic to provide HIV and STI testing and treatment free of charge [73]. While the HIV test positivity rates in Gay Zone were not higher than those at the community level, the clinic accounted for between 8.1% (2011) and 19.2% (2012) of diagnoses citywide.
The “Checkpoint” MSM clinic model has been implemented in several European countries. Similar to GayZone, these clinics are generally open during specific hours each week and offer HIV and STI testing and treatment primarily targeting MSM on a walk-in basis. Staffing includes some combination of community agents, peer counselors, and physicians and nurses that are familiar with and accepting of gay male sexuality. Based on data in a Checkpoint clinic in Geneva, the number of HIV tests and HIV diagnoses doubled from 2005 to 2009, and on average, 2.0% tested positive per year. [74] This model was also implemented in Zurich [75], Barcelona [76], Copenhagen [77], and Quebec [78]. Each of these studies reported increases in the number of tests among MSM overall, and positivity was between 1 and 3.9%. Furthermore, between 5.5 and 19.4% of participants were first time testers, and these clinics accounted for large proportions (11–56%) of all positive HIV tests among MSM in their respective cities.
These studies expanding clinic programs generally reported increased testing rates and demonstrate that MSM are receptive to MSM-targeted clinic spaces in urban North American and European settings. These clinic-based strategies can address a number of barriers to testing. Opt out can address fear and low risk perception [68, 69] by allowing more time at the beginning of the counseling session to address personal barriers. A number of studies in our review addressed stigma by creating MSM-specific medical facilities or MSM-specific hours, to offer HIV testing as well as psychological and general medical care in a setting staffed by culturally competent, MSM-friendly medical professionals [73, 75,76,77, 79].
Overall, however, it is not clear whether collectively these findings represent an actual increase in testing among MSM or if these strategies simply create spaces MSM, who would have tested with or without the intervention, prefer over their previous testing options and where they may not have disclosed as MSM. Additional studies are needed to determine whether these specialized clinics lead to increased testing among MSM who may not have otherwise tested and whether these expanded programs are feasible outside of high resource countries or where a high level of stigma exists.
Community-Based Strategies
Community-based strategies have been used around the world to deliver HIV testing outside of the clinical setting. Three systematic reviews have explored the use of these strategies to test for HIV among MSM. First, focusing on resource-rich countries, Thornton et al. found that comparisons of positivity rates between community-based (including mobile testing) and clinic-based settings were not consistent across studies [80]. Though, only five of the 44 studies in their review included a comparison group. In a review of studies from Africa, America, Europe, Asia, and Australia, Suthar et al., found that testing uptake was higher in community-based sites, and in all but one study, first-time testers were more likely to be tested in community-based settings than in facility-based testing [81]. However, findings regarding positivity rates were inconclusive. Lastly, Sharma and colleagues conducted a systematic review and meta-analysis of studies in Nigeria and the Democratic Republic of Congo [82]. Collectively, these three reviews found that community-based testing resulted in 24% of MSM testing positive and more than 83% of those in the programs had never tested. More recent studies have highlighted successes of three particular community-based strategies: mobile testing, testing in MSM-specific venues, and pharmacy testing.
Mobile Testing
Three studies in Spain and one in Lima, Peru have noted successes in reaching a large number of new or infrequent MSM testers. For example, 3004 MSM tested in mobile vans in Madrid over three separate time periods. A total of 26.3% had never tested and 3.9% tested positive [83]. Other mobile testing initiatives in Spain have reported similar rates of new testers (24.2%) [84], and slighly lower positivity (2.76%) [85]. The proportion of those being diagnosed at a later stage of disease was lower, indicating earlier diagnosis [85]. Similarly, in Lima, Peru, a mobile testing study reached a greater proportion of MSM who had never tested for HIV (48%) compared to a fixed clinic (41.3%). The positivity rate was 12.6% and 4.7% among gay and bisexual men, respectively [86]. These data suggest that, while case finding is greater among men who seek out testing in clinics, mobile testing may be effective in finding new testers and increase early diagnoses in these diverse urban environments.
Venue-Based Testing
Seven studies described testing efforts in community venues, some of which were MSM-specific. In Belgium, of MSM recruited from cruising venues, gay clubs, and young MSM venues, 6% tested positive, with the highest positivity found at cruising venues (14.5%) [87]. In Estonia, the country with the highest HIV prevalence in Europe, testing at a gay bar, a gay sauna, and at a gay and lesbian information center [88] found no positive results, though just under half of participants (48.4%) had no HIV testing history. The authors suggest that this strategy reached men who were openly gay and attend gay establishments, but could miss a potential hidden epidemic among those who are closeted. In Hamburg, Germany, a community space for MSM including a drop-in center, information on gay life, outreach, and testing was established [89]. Between 2011 and 2012, 1413 MSM were tested for HIV, and 3.3% were newly infected.
Among MSM testing at Gay pride events in 13 U.S. cities in 2009 and 2010, about a third of MSM had either never tested (21.7%) or hadn’t tested in the past year (11.9%), and the positivity rate was 7.2% [90]. Additional findings from this study suggest that testing at gay pride events is particularly effective in reaching MSM of color and those who have never tested. Another analysis evaluated HIV testing among young MSM in non-healthcare settings in the U.S. including bars, clubs, and adult entertainment venues; partner services field visits; and syringe exchange programs [91, 92]. Positivity was 2.8, 74% of which were newly diagnosed.
In China, MSM community members recruited MSM who had never tested from gay bars, clubs, bathhouses, cruising areas and hotels [93]. A total of 512 MSM first time testers participated, and 10.4% tested positive. In India, MSM were recruited from public sex environments (e.g., parks, bathrooms) and CBO-organized drop-in centers [94], and offered field-based video counseling as well as testing with a counselor. Of the 298 MSM tested in the study, 41.3% had never tested and the overall positivity rate among MSM was 26.1%. These findings suggest that across regions, conducting HIV testing at venues frequented by MSM is effective at reaching MSM who have never tested, are undiagnosed, and who may not attend a clinic for testing otherwise.
In-pharmacy Testing
Three studies reported on testing programs in pharmacies. In Spain, 3482 MSM were tested at pharmacies offering testing during business hours [95]. Just under a third (31.8%) had never tested, 26.9% hadn’t tested in the previous year, and 3.4% tested positive. In New York City, public health advocates (PHAs) approached visitors at participating pharmacies and offered them a free HIV rapid test [96]. A total of 795 MSM tested, of which three (0.3%) tested positive. A small study in Michigan also demonstrated high rates of first time testers in a pharmacy program [97]. Overall, these studies provide evidence that testing in pharmacies may be a promising strategy for identifying people who have not tested previously. However, these studies were not MSM-specific, and this strategy may not be appropriate for targeting MSM outside of largely gay neighborhoods. Furthermore, there is little evidence regarding in-pharmacy testing outside of resource rich countries.
Comparative Studies
One study in Sydney, Australia, compared three HIV test delivery venues [98]. Patients attended either: a sexual health clinic (n = 646) [99]; a LGBT Health focused community based organization (CBO) (n = 587); or a temporary shopfront in a gay neighborhood (n = 471). MSM at the CBO were more likely to have never tested, a higher proportion of those at the sexual health clinic were infrequent testers and identified as bisexual, and the positivity rate was highest at the shopfront (2.37%) compared to the CBO (1.04%) and the sexual health clinic (1.02%).
In Nigeria, three strategies to increase testing among MSM and men who inject drugs were compared [100]. In each strategy, community key opinion leaders (KOLs) conducted outreach and either (1) provided referrals to friendly counseling and testing sites, (2) were paired with HIV counselors and testers who could provide HIV testing in the community, or (3) were themselves trained to conduct the HIV testing and counseling. Uptake was the highest in strategy 3 (98.88%), followed by S1 (92.61%), and S2 (77%). Similarly, positivity was highest in strategy 3 (12.67%), followed by S1 (9.05%) and S2 (3.27). Thus, while all three strategies showed high uptake, the strategy in which testers only interacted with community KOLs and were tested in the community was most effective These findings suggest that, in high-stigma contexts, having MSM conduct outreach and deliver testing may be a critical strategy for reaching those who would likely not seek out testing in community clinics on their own.
These community based strategies and comparative studies reveal the strength of offering testing in community settings where MSM feel comfortable. Further, inconvenient locations and hours are barriers to testing [101]. Mobile testing and testing at night in locations more convenient to the target population are effective strategies for overcoming these and other barriers [102]. It is worth noting that gay-venue-based strategies are primarily feasible in urban areas with an established gay community and will be less likely to reach those MSM who do not identify as gay or bisexual, or who do not frequent those establishments. Lastly, while there are few studies of pharmacy based testing, the data suggest that offering testing in a health-related space that is not specific to MSM may be effective in destigmatizing testing, and reaching those who may not be willing to test in an MSM-specific venue.
HIV Self-testing (HIVST)
HIV self-test kits have been recently employed as a strategy to deliver HIV testing to MSM. HIVST kits were approved for over the counter sales in the U.S. in 2012 [103] and are currently available in approximately 23 countries [104]. Much of the published literature prior to approval and since has focused on feasibility, and acceptability, with several previously published reviews of this literature [105,106,107] and subsequent studies [e.g. 108–113] finding moderate to high acceptability of HIVST among MSM. As of our review, there were nine published studies specifically focused on the use of HIVST among MSM. These studies used several different strategies to distribute HIVST to MSM, including venue-based settings, CBO-based voucher distribution, internet strategies (on-line requests), and through peer distribution.
Studies conducted in the West include one in Los Angeles where vouchers redeemable for HIVST from a participating national pharmacy (Walgreens), were distributed by community based organizations [114]. Thirty percent of those testing and completing a survey had not tested in the past year, and 6.1% tested positive. While the sample was not exclusively MSM, MSM did account for the majority (66%) of the sample. A study in San Francisco distributed HIVST to patrons of a local bathhouse [115]. A quarter of those accepting HIVST had not tested in the previous year and 7% had never tested. In New York, 27 MSM distributed test kits to their sex partners and acquaintances [116]. Of 101 kits distributed, 6 tested newly positive. Additional studies in Los Angeles reached MSM through online social network sites [117] or banner ads [118] to offer HIVST. In the study using social network sites, 36 kits were mailed. Just under half (48%) of requesters had not tested in the previous 6 months, and 11% had not tested in the previous 3 years. In the study utilizing banner ads on a partner seeking site, 333 tests were requested, of which 29% of MSM had last tested over 1 year ago, and 9% had never tested.
A longitudinal study conducted in Lima, Peru and Rio de Janeiro, Brazil distributed test kits at a local health research center, trained MSM to use the kits, and asked them to test monthly during their 3-month study participation [119]. Nearly all participants (98%) reported using the test at the first monthly follow up visit, as well as the last study visit (97%). Forty-five percent had not tested in the previous year and 16% had never tested.
In two Chinese studies, MSM completed an online survey and paid a deposit, refundable after participants reported test results, to have tests mailed to them. In Beijing, 220 MSM paid a $10 deposit. Just over half of their sample (N = 220) had never tested and 15% tested positive. [120]. And in Guangzhou, China, 198 MSM paid a $23 USD deposit to have a HIV and Syphilis self-test kits mailed to them. Just over a quarter (27.8%) had never tested before and the positivity rate was 4.5% [121].
The findings of these studies confirm the high acceptability of HIVST among MSM wherever deployed and attest to the variety of methods to reach MSM for HIVST delivery. Home HIVST kits can reduce barriers to testing by making the testing process private, confidential, and in the control of the tester [114], removing the need to go to a physical testing facility for those uncomfortable in the clinic setting. Indeed, a number of the studies we review suggested that HIVST is a particularly effective way to overcome the barriers of sexual minority stigma, HIV stigma, and lack of privacy, particularly among MSM of color (in the U.S.) [114, 117, 118, 120]. Further, studies have found that men are willing to test more often if self-testing is available [122, 123]. It seems clear that MSM will utilize HIVST, however, optimal methods for HIVST distribution are as of yet unclear, being geographically and culturally dependent and contingent upon local policy, as HIVST is not regulated or legal in some contexts [124]. Reach will likely require greater levels of anonymity (e.g., mail delivery; peer distribution vs. clinic-based distribution) in more stigmatized cultural contexts.
Discussion
Over the course of the HIV epidemic, a number of strategies has been employed to reach MSM and deliver HIV testing to MSM. Our synthesis of the evidence from the past decade suggests that there are long-standing strategies, such as standard in-clinic testing and PCRS approaches, that remain effective for MSM in spaces where the population is less hidden and services are MSM-friendly, but for MSM in highly stigmatized environments, newer approaches are needed. To date, the evidence base for most strategies to reach and deliver HIV testing to MSM in Africa and Latin America is under-developed (see Fig. 2 for a summary of the available evidence by geographic regions), with unanswered questions regarding efficacy and feasibility.
Numerous barriers to testing for MSM are well documented, globally. In some settings, identifying as a man who have sex with men comes with significant risk. For example, in a number of countries represented in this review, including Ghana, Swaziland, Malawi, and Nigeria, homosexuality is highly stigmatized and illegal [125]. Such criminalization and sexual stigma are associated with lower access to testing [126]. In other locales, where gay identity or behaviors are not themselves criminalized, HIV non-disclosure criminalization laws have also been associated with some believing that it is better to remain unaware of one’s status and less likelihood of testing [127, 128]. Other negative influences on testing include internalized homophobia, lack of access to testing, lack of social support, poor accessibility of health services, and living in low-resourced communities (vs. urban centers), among others [129,130,131,132,133].
Among the most versatile strategies with the strongest global evidence base to address these barriers, social network-based approaches are particularly effective in reaching MSM, including African American MSM in the US, who are infrequent testers or have never tested [52,53,54,55,56,57,58,59,60,61,62, 100, 134, 135], as well as MSM in Africa and Asia. In communities where social, structural, and political barriers make it less likely that clinic-based strategies can be successful at serving those at most need of HIV services, reaching MSM through their networks, on-line or otherwise, can reach those in need. Importantly, these efforts are particularly effective at delivering testing in communities where HIV and homosexuality are stigmatized and criminalized, and where MSM venues are hidden or uncommon [136,137,138,139]. Comparative studies support the success of this approach in identifying those men who are less likely to have tested previously and are undiagnosed. Strategies employing community members and social networks have been effective in large urban cities in the U.S. [52, 54, 55], as well as in China [60], and Sub-Saharan Africa [57, 58] where reaching and offering testing to MSM through trusted key opinion leaders or peers was effective in overcoming some of the fear and mistrust that MSM have due to the possibility of legal jeopardy or physical harm [100]. PCRS has been used to identify undiagnosed STIs for many decades [37] and continues to be consistently effective in reaching a portion of previously undiagnosed MSM with HIV. Among those who perceive themselves to be low risk and choose not to seek testing, PCRS is a particularly useful strategy for reaching those who may be unaware that they have HIV-positive partners. However, the implementation of this approach has been limited to North America, Europe, Australia, and one study in China. Thus, there is a gap in knowledge around the potential effectiveness of PCRS for reaching undiagnosed MSM in countries where surveillance programs are likely under resourced, particularly the African continent and Central and South America. There are likely multiple challenges to both identifying MSM and eliciting partner referrals in areas where same sex behavior is criminalized or highly stigmatized. Exploring PCRS in Africa and Latin America in select contexts (e.g., MSM-friendly clinics) is certainly warranted; however, it is not yet clear whether this approach would be feasible based on current evidence.
Internet and social media strategies appear to be useful in locations where MSM venues are scarce [20], where there are high levels of HIV stigma [17], and where the internet is widely accessed [16]. These strategies are relatively inexpensive to implement and are also effective in reaching MSM who identify as straight or bisexual and thus less likely to be recruited at MSM-specific venues [12, 15]. However, it is worth noting that evidence with these strategies is currently limited to urban and suburban areas of the United States, Asia, and one study in Peru. We could not identify similar research from other Asian or Latin American countries or any African countries, though programming exists that has not been evaluated in these contexts. Fortunately, internet access is also growing exponentially in these locations [140], providing critical opportunities to reach MSM. Lastly, most of these studies were demonstration or feasibility studies that did not employ rigorous experimental design. As a result, conclusions regarding whether these strategies can reach new testers or increase testing frequency as compared to traditional strategies are still speculative.
Social marketing studies have used a variety of strategies to reach large numbers of people, however, findings are mixed on the effectiveness of social marketing to promote HIV testing specifically in MSM. All studies were conducted in urban areas of the United States, Canada, Australia, England, and China, and only about half of these studies were effective in increasing testing rates [25,26,27] and findings are inconclusive as to whether the successful campaigns engaged new MSM in testing or simply encouraged more testing among existing regular testers. Lastly, MSM-targeted social marketing depends on the availability and accessibility of testing services and is unlikely to be effective in rural, low-resource, or high HIV-stigma communities. Based on our review, social marketing is not a recommended strategy for targeting MSM in most circumstances. Targeted media approaches (dating apps and MSM internet sites) are more appropriate.
When examining approaches for delivering HIV testing to MSM, success in high-income settings has been achieved by altering or extending clinic environments and also by moving testing out of the clinic and into the community. Making clinics MSM-friendly (e.g., opt-out testing, after-hours testing) has resulted in increased testing and reductions in test refusal among MSM. Similarly, interventions in gay venues (e.g., bars, clubs, bathhouses, gay pride events, and cruising areas) [87, 88, 90, 93, 94], mobile testing studies [83, 84, 86], and in-pharmacy studies [95, 97] have shown success in delivering tests to new testers. Based on the available evidence, providing testing in community venues is likely effective for increasing testing among MSM. It is important to highlight, however, that gay-specific HIV testing spaces require gay community venues or neighborhoods [89]. In locations where MSM are largely closeted, it is less likely that MSM would present in a gay venue for testing [88]. Some models of clinic-based HIV testing will be more effective in reaching these and other subgroups of MSM populations. For example, bisexual men were more likely to get tested in the sexual health clinic compared to the Shopfront or the LGBT health-focused CBO [98]. Knowing the profile of those least likely to be reached and those most at risk in each context will shape programming.
Finally, research on HIV self-testing has been growing steadily in recent years. Most evidence indicates that self-testing holds promise as an effective strategy for reaching MSM who have not tested recently or have never tested, including those at greater risk of infection and those who are not predisposed to access clinics or venue-based testing. Indeed, the World Health Organization recently published extensive guidelines and recommendations on the implementation of self-testing strategies [124]. The proportion of MSM in HIVST studies reporting not having tested in the previous year ranged from 25 to 45% [114,115,116, 118,119,120,121], including in a study from China that reported that over half of participants had never tested [120]. While the studies cited were limited to five countries—the United States, Peru, Brazil, the UK, and China—additional studies are underway, including many in lower and middle-income countries [141,142,143,144,145,146]. Given the successes, particularly in China where HIV and MSM are highly stigmatized, HIVST should be pursued to determine if positive findings remain consistent in broader geographical contexts and if newer self-tests coming to market offer further advantages. Burgeoning research into combined reach and delivery strategies using peers and the internet to disseminate HIVST shows great potential to access hard to reach MSM across the globe.
There are important discussions around HIV testing for MSM that our review cannot address. First, we used the current CDC and WHO recommendations that sexually active MSM get tested once a year to guide our review [2, 147]. While the recommendation for those at high risk is every 6 months, for most of the studies in our review, we were unable to distinguish which MSM would be classified as high risk. Therefore, our focus was limited to those studies that reported success in reaching this goal. However, it is worth noting that there is great variation in the relationship status, identities, and sexual risk behaviors which should determine the frequency of testing for different groups of MSM. We were unable to determine the extent to which the risk profile of the men in these studies differed and required different testing frequencies. Second, in addition to reaching those who have never tested or have not recently tested, there is also a need for strategies to establish regular and consistent testing patterns for MSM. This was not the focus of this review but should be explored in future studies and reviews of the literature.
As we move forward in the effort to reach the UNAIDS 90–90–90 targets, combinations of existing strategies, along with those yet to be developed, continue to be needed to encourage HIV testing among MSM. Cultural, socio-economic, racial, and political contexts will determine which approaches are feasible at the local level, however, based on our review, only a small number of approaches have been studied (and published) in most contexts. Almost all studies we found were conducted in urban areas, making the findings potentially less relevant in rural settings, where stigma may be greater, prevention information less available, and testing facilities scarcer. A great deal more research is needed to understand the most effective means of improving early and frequent HIV testing for MSM, particularly in lower and middle-income countries. Fortunately, the universe of MSM HIV testing strategies is expanding and a variety of interventions hold promise for helping to end the epidemic. Additional comparative research around HIV testing uptake and earlier diagnosis, particularly utilizing combinations of recommended reach and delivery approaches, is warranted.
References
Beyrer C, Baral SD, van Griensven F, Goodreau SM, Chariyalertsak S, Wirtz AL, et al. Global epidemiology of HIV infection in men who have sex with men. Lancet. 2012;380(9839):367–77.
WHO. Consolidated guidelines on HIV testing services. Geneva: WHO; 2015.
Mukolo A, Villegas R, Aliyu M, Wallston KA. Predictors of late presentation for HIV diagnosis: a literature review and suggested way forward. AIDS Behav. 2013;17(1):5–30.
Golub SA, Gamarel KE. The impact of anticipated HIV stigma on delays in HIV testing behaviors: findings from a community-based sample of men who have sex with men and transgender women in New York City. AIDS Patient Care STDS. 2013;27(11):621–7.
Jürgensen M, Tuba M, Fylkesnes K, Blystad A. The burden of knowing: balancing benefits and barriers in HIV testing decisions. a qualitative study from Zambia. BMC Health Serv Res. 2012;12(1):1.
Prestage G, Brown G, Keen P. Barriers to HIV testing among Australian gay men. Sex Health. 2012;9(5):453–8.
Schwarcz S, Richards TA, Frank H, Wenzel C, Chin Hsu L, Chin C-SJ, et al. Identifying barriers to HIV testing: personal and contextual factors associated with late HIV testing. AIDS Care. 2011;23(7):892–900.
Logie CH, Lacombe-Duncan A, Brien N, Jones N, Lee-Foon N, Levermore K, et al. Barriers and facilitators to HIV testing among young men who have sex with men and transgender women in Kingston, Jamaica: a qualitative study. J Int AIDS Soc. 2017;20(1):21385.
Malebranche DJ, Peterson JL, Fullilove RE, Stackhouse RW. Race and sexual identity: perceptions about medical culture and healthcare among Black men who have sex with men. J Natl Med Assoc. 2004;96(1):97.
Joint UN Programme on HIV/AIDS. 90–90–90 an ambitious treatment target to help end the AIDS epidemic. 2014. http://www.unaids.org/sites/default/files/media_asset/90-90-90_en_0.pdf. Accessed 15 Nov 2016.
Wainberg M, Hull M, Girard P, Montaner J. Achieving the 90–90–90 target: incentives for HIV testing. Comment. Lancet Infect Dis. 2016;16:1215–6.
Rhodes SD, McCoy TP, Tanner AE, Stowers J, Bachmann LH, Nguyen AL, et al. Using social media to increase HIV testing among gay and bisexual men, other MSM, and transgender persons: outcomes from a randomized community trial. Clin Infect Dis. 2016;62(11):1450–3.
Rhodes SD, Vissman AT, Stowers J, Miller C, McCoy TP, Hergenrather KC, et al. A CBPR partnership increases HIV testing among men who have sex with men (MSM): outcome findings from a pilot test of the CyBER/testing internet intervention. Health Educ Behav. 2011;38(3):311–20.
Bauermeister JA, Pingel ES, Jadwin-Cakmak L, Harper GW, Horvath K, Weiss G, et al. Acceptability and preliminary efficacy of a tailored online HIV/STI testing intervention for young men who have sex with men: the get connected! program. AIDS Behav. 2015;19(10):1860–74.
Blas MM, Alva IE, Carcamo CP, Cabello R, Goodreau SM, Kimball AM, et al. Effect of an online video-based intervention to increase HIV testing in men who have sex with men in Peru. PLoS ONE. 2010;5(5):e10448.
Young SD, Cumberland WG, Nianogo R, Menacho LA, Galea JT, Coates T. The HOPE social media intervention for global HIV prevention in Peru: a cluster randomised controlled trial. Lancet HIV. 2015;2(1):e27–32.
Zou H, Wu Z, Yu J, Li M, Ablimit M, Li F, et al. Internet-facilitated, voluntary counseling and testing (VCT) clinic-based HIV testing among men who have sex with men in China. PLoS ONE. 2013;8(2):e51919.
Anand T, Nitpolprasert C, Ananworanich J, Pakam C, Nonenoy S, Jantarapakde J, et al. Innovative strategies using communications technologies to engage gay men and other men who have sex with men into early HIV testing and treatment in Thailand. J Virus Erad. 2015;1:111–5.
Ko N-Y, Hsieh C-H, Wang M-C, Lee C, Chen C-L, Chung A-C, et al. Effects of Internet popular opinion leaders (iPOL) among Internet-using men who have sex with men. J Med Internet Res. 2013;15(2):e40.
Lampkin D, Crawley A, Lopez TP, Mejia CM, Yuen W, Levy V. Reaching suburban men who have sex with men for STD and HIV services through online social networking outreach: a public health approach. JAIDS. 2016;72(1):73–8.
Garett R, Smith J, Young SD. A review of social media technologies across the global HIV care continuum. Curr Opin Psychol. 2016;9:56–66.
Grier S, Bryant CA. Social marketing in public health. Annu Rev Public Health. 2005;26:319–39.
Noar SM, Palmgreen P, Chabot M, Dobransky N, Zimmerman RS. A 10-year systematic review of HIV/AIDS mass communication campaigns: have we made progress? J Health Commun. 2009;14(1):15–42.
Vidanapathirana J, Abramson MJ, Forbes A, Fairley C. Mass media interventions for promoting HIV testing. Cochrane Database Syst Rev. 2005;3:4775.
Solorio R, Norton-Shelpuk P, Forehand M, Montaño D, Stern J, Aguirre J, et al. Tu Amigo Pepe: evaluation of a multi-media marketing campaign that targets young Latino immigrant MSM with HIV testing messages. AIDS Behav. 2016;20:1973–88.
Adam BD, Gardner S, Major C, Campbell D, Light L, Globerman J. Promoting HIV testing for gay and bisexual men an evaluation of the 2011–2012 campaign in Toronto and Ottawa. Health Promot Pract. 2015;17:40–7.
Gilbert M, Cook D, Steinberg M, Kwag M, Robert W, Doupe G, et al. Targeting screening and social marketing to increase detection of acute HIV infection in men who have sex with men in Vancouver, British Columbia. AIDS. 2013;27(16):2649–54.
Pedrana A, Hellard M, Guy R, El-Hayek C, Gouillou M, Asselin J, et al. Stop the drama Downunder: a social marketing campaign increases HIV/sexually transmitted infection knowledge and testing in Australian gay men. Sex Transm Dis. 2012;39(8):651–8.
Wilkinson AL, Pedrana AE, El-Hayek C, Vella AM, Asselin J, Batrouney C, et al. The Impact of a social marketing campaign on HIV and sexually transmissible infection testing among men who have sex with men in Australia. Sex Transm Dis. 2016;43(1):49–56.
Guy R, Goller J, Leslie D, Thorpe R, Grierson J, Batrouney C, et al. No increase in HIV or sexually transmissible infection testing following a social marketing campaign among men who have sex with men. J Epidemiol Community Health. 2009;63(5):391–6.
Hickson F, Tomlin K, Hargreaves J, Bonell C, Reid D, Weatherburn P. Internet-based cohort study of HIV testing over 1 year among men who have sex with men living in England and exposed to a social marketing intervention promoting testing. Sex Transm Infect. 2015;91(1):24–30.
Prati G, Mazzoni D, Cicognani E, Albanesi C, Zani B. Evaluating the persuasiveness of an HIV mass communication campaign using gain-framed messages and aimed at creating a superordinate identity. Health Commun. 2016;31(9):1097–104.
Olshefsky AM, Zive MM, Scolari R, Zuñiga M. Promoting HIV risk awareness and testing in Latinos living on the US-Mexico border: the Tu No Me Conoces social marketing campaign. AIDS Educ Prev. 2007;19(5):422.
Martínez-Donate AP, Zellner JA, Fernández-Cerdeño A, Sañudo F, Hovell MF, Sipan CL, et al. Hombres Sanos: exposure and response to a social marketing HIV prevention campaign targeting heterosexually identified Latino men who have sex with men and women. AIDS Educ Prev. 2009;21(Suppl B):124.
Martínez-Donate AP, Zellner JA, Sañudo F, Fernandez-Cerdeño A, Hovell MF, Sipan CL, et al. Hombres Sanos: evaluation of a social marketing campaign for heterosexually identified Latino men who have sex with men and women. Am J Public Health. 2010;100(12):2532–40.
Tang W, Han L, Best J, Zhang Y, Mollan K, Kim J, et al. Crowdsourcing HIV test promotion videos: a noninferiority randomized controlled trial in China. Clin Infect Dis. 2016;62:1436–42.
Hogben M, McNally T, McPheeters M, Hutchinson AB. Services TFoCP. The effectiveness of HIV partner counseling and referral services in increasing identification of HIV-positive individuals: a systematic review. Am J Prev Med. 2007;33(2):S89–100.
Ahrens K, Kent CK, Kohn RP, Nieri G, Reynolds A, Philip S, et al. HIV partner notification outcomes for HIV-infected patients by duration of infection, San Francisco, 2004 to 2006. JAIDS. 2007;46(4):479–84.
Marcus JL, Bernstein KT, Klausner JD. Updated outcomes of partner notification for human immunodeficiency virus, San Francisco, 2004–2008. AIDS. 2009;23(8):1024–6.
Golden MR, Stekler J, Kent JB, Hughes JP, Wood RW. An evaluation of HIV partner counseling and referral services using new disposition codes. Sex Transm Dis. 2009;36(2):95–101.
Bergman J, Gratrix J, Pillay T, Houston S, Cooper R, Charlton CL, et al. Intensive HIV partner notification is effective in identifying new and previously diagnosed HIV infections in Edmonton, Canada. AIDS Patient Care STDS. 2015;29(8):419–22.
van Aar F, Schreuder I, van Weert Y, Spijker R, Götz H, de Coul EO. Current practices of partner notification among MSM with HIV, gonorrhoea and syphilis in the Netherlands: an urgent need for improvement. BMC Infect Dis. 2012;12(1):114.
van Aar F, van Weert Y, Spijker R, Götz H, de Coul EOP. Partner notification among men who have sex with men and heterosexuals with STI/HIV: different outcomes and challenges. Int J STD AIDS. 2015;26(8):565–73.
De Olalla PG, Molas E, Barberà MJ, Martín S, Arellano E, Gosch M, et al. Effectiveness of a pilot partner notification program for new HIV cases in Barcelona, Spain. PLoS ONE. 2015;10(4):e0121536.
Fu X, Qi J, Hu Y, Pan X, Li Y, Liu H, et al. Partner notification in cooperation with community-based organizations among HIV-positive men who have sex with men in two Chinese cities. Int J STD AIDS. 2016;27(10):821–31.
Hochberg CH, Berringer K, Schneider JA. Next-generation methods for HIV partner services: a systematic review. Sex Transm Dis. 2015;42(9):533.
Vest JR, Valadez AM, Hanner A, Lee JH, Harris PB. Using e-mail to notify pseudonymous e-mail sexual partners. Sex Transm Dis. 2007;34(11):840–5.
Udeagu C-CN, Bocour A, Shah S, Ramos Y, Gutierrez R, Shepard CW. Bringing HIV partner services into the age of social media and mobile connectivity. Sex Transm Dis. 2014;41(10):631–6.
Chen M-J, Pipkin S, Marcus JL, Bernstein KT, Scheer S. Using HIV testing history to measure the success of HIV partner services. Sex Transm Dis. 2013;40(5):419–21.
CDC. Social network strategy (SNS) for HIV testing recruitment. https://effectiveinterventions.cdc.gov/en/HighImpactPrevention/PublicHealthStrategies/SocialNetworkStrategy.aspx. Accessed 24 July 2017.
Heckathorn DD. Respondent-driven sampling: a new approach to the study of hidden populations. Soc Probl. 1997;44(2):174–99.
Fuqua V, Chen Y-H, Packer T, Dowling T, Ick TO, Nguyen B, et al. Using social networks to reach Black MSM for HIV testing and linkage to care. AIDS Behav. 2012;16(2):256–65.
CDC. Use of social networks to identify persons with undiagnosed HIV infection—seven US cities, October 2003–September 2004. MMWR. 2005;54(24):601.
Kimbrough LW, Fisher HE, Jones KT, Johnson W, Thadiparthi S, Dooley S. Accessing social networks with high rates of undiagnosed HIV infection: the social networks demonstration project. Am J Public Health. 2009;99(6):1093–9.
Golden MR, Gift TL, Brewer DD, Fleming M, Hogben M, Lawrence JSS, et al. Peer referral for HIV case-finding among men who have sex with men. AIDS. 2006;20(15):1961–8.
McCree DH, Millett G, Baytop C, Royal S, Ellen J, Halkitis PN, et al. Lessons learned from use of social network strategy in HIV testing programs targeting African American men who have sex with men. Am J Public Health. 2013;103(10):1851–6.
Girault P, Green K, Clement NF, Rahman YAA, Adams B, Wambugu S. Piloting a social networks strategy to increase HIV testing and counseling among men who have sex with men in Greater Accra and Ashanti Region, Ghana. AIDS Behav. 2015;19(11):1990–2000.
Lane T, Raymond HF, Dladla S, Rasethe J, Struthers H, McFarland W, et al. High HIV prevalence among men who have sex with men in Soweto, South Africa: results from the Soweto men’s study. AIDS Behav. 2011;15(3):626–34.
Stahlman S, Johnston LG, Yah C, Ketende S, Maziya S, Trapence G, et al. Respondent-driven sampling as a recruitment method for men who have sex with men in southern sub-Saharan Africa: a cross-sectional analysis by wave. Sex Transm Infect. 2016;92(4):292–8.
Zhang H, Wu Z, Zheng Y, Wang J, Zhu J, Xu J. A pilot intervention to increase condom use and HIV testing and counseling among men who have sex with men in Anhui, China. JAIDS. 2010;53:S88–92.
Halkitis PN, Kupprat SA, McCree DH, Simons SM, Jabouin R, Hampton MC, et al. Evaluation of the relative effectiveness of three HIV testing strategies targeting African American men who have sex with men (MSM) in New York City. Ann Behav Med. 2011;42(3):361–9.
Baytop C, Royal S, Hubbard McCree D, Simmons R, Tregerman R, Robinson C, et al. Comparison of strategies to increase HIV testing among African-American gay, bisexual, and other men who have sex with men in Washington, DC. AIDS Care. 2014;26(5):608–12.
Ellen J, McCree D, Muvva R, Chung S, Miazad R, Arrington-Sanders R, et al. Recruitment approaches to identifying newly diagnosed HIV infection among African American men who have sex with men. Int J STD AIDS. 2013;24(5):335–9.
Branson BM, Handsfield HH, Lampe MA, Janssen RS, Taylor AW, Lyss SB, et al. Revised recommendations for HIV testing of adults, adolescents, and pregnant women in health-care settings. MMWR. 2006;55(14):1–4.
Moyer VA. Screening for HIV: US preventive services task force recommendation statement. Ann Intern Med. 2013;159(1):51–60.
Campos-Outcalt D, Mickey T, Weisbuch J, Jones R. Integrating routine HIV testing into a public health STD clinic. Public Health Rep. 2006;121(2):175–80.
Katz DA, Dombrowski JC, Kerani RP, Aubin MR, Kern DA, Heal DD, et al. Integrating HIV testing as an outcome of STD partner services for men who have sex with men. AIDS Patient Care STDS. 2016;30(5):208–14.
Dukers-Muijrers NH, Niekamp A-M, Vergoossen MM, Hoebe CJ. Effectiveness of an opting-out strategy for HIV testing: evaluation of 4 years of standard HIV testing in a STI clinic. Sex Transm Infect. 2009;85(3):226–30.
Heijman R, Stolte I, Thiesbrummel H, van Leent E, Coutinho R, Fennema J, et al. Opting out increases HIV testing in a large sexually transmitted infections outpatient clinic. Sex Transm Infect. 2009;85(4):249–55.
Esteban-Vasallo MD, Morán-Arribas M, García-Riolobos C, Domínguez-Berjón MF, Rico-Bermejo J, Collado-González S, et al. Targeted rapid HIV testing in public primary care services in Madrid. Are we reaching the vulnerable populations? Int J Infect Dis. 2014;19:39–45.
Snow AF, Vodstrcil LA, Fairley CK, El-Hayek C, Cummings R, Owen L, et al. Introduction of a sexual health practice nurse is associated with increased STI testing of men who have sex with men in primary care. BMC Infect Dis. 2013;13(1):298.
Lorente N, Preau M, Vernay-Vaisse C, Mora M, Blanche J, Otis J, et al. Expanding access to non-medicalized community-based rapid testing to men who have sex with men: an urgent HIV prevention intervention (the ANRS-DRAG study). PLoS ONE. 2013;8(4):e61225.
O’Byrne P, MacPherson P, Ember A, Grayson M-O, Bourgault A. Overview of a gay men’s STI/HIV testing clinic in Ottawa: clinical operations and outcomes. Can J Public Health. 2014;105(5):389–94.
Gumy C, Jeannin A, Balthasar H, Huissoud T, Jobin V, Häusermann M, et al. Five-year monitoring of a gay-friendly voluntary counselling and testing facility in Switzerland: who got tested and why? BMC Public Health. 2012;12(1):422.
Schwappach DL, Bruggmann P. An integrated model of care to counter high incidence of HIV and sexually transmitted diseases in men who have sex with men—initial analysis of service utilizers in Zurich. BMC Public Health. 2008;8(1):180.
Meulbroek M, Ditzel E, Saz J, Taboada H, Pérez F, Pérez A, et al. BCN Checkpoint, a community-based centre for men who have sex with men in Barcelona, Catalonia, Spain, shows high efficiency in HIV detection and linkage to care. HIV Med. 2013;14(S3):25–8.
Qvist T, Cowan SA, Graugaard C, Helleberg M. High linkage to care in a community-based rapid HIV testing and counseling project among men who have sex with men in Copenhagen. Sex Transm Dis. 2014;41(3):209–14.
Engler K, Rollet K, Lessard D, Thomas R, Lebouché B. Ability of a rapid HIV testing site to attract and test vulnerable populations: a cross-sectional study on Actuel sur Rue. Int J STD AIDS. 2015;27:973–7.
Munro HL, Lowndes CM, Daniels DG, Sullivan AK, Robinson AJ. National study of HIV testing in men who have sex with men (MSM) attending genitourinary (GUM) clinics in the UK. Sex Transm Infect. 2007;84(4):265–70.
Thornton A, Delpech V, Kall M, Nardone A. HIV testing in community settings in resource-rich countries: a systematic review of the evidence. HIV Med. 2012;13(7):416–26.
Suthar AB, Ford N, Bachanas PJ, Wong VJ, Rajan JS, Saltzman AK, et al. Towards universal voluntary HIV testing and counselling: a systematic review and meta-analysis of community-based approaches. PLoS Med. 2013;10(8):e1001496.
Sharma M, Ying R, Tarr G, Barnabas R. Systematic review and meta-analysis of community and facility-based HIV testing to address linkage to care gaps in sub-Saharan Africa. Nature. 2015;528(7580):S77–85.
Belza M, Hoyos J, Fernandez-Balbuena S, Diaz A, Bravo M, de la Fuente L. Assessment of an outreach street-based HIV rapid testing programme as a strategy to promote early diagnosis: a comparison with two surveillance systems in Spain, 2008–2011. Eurosurveillance. 2015;20(14):23–33.
Fernández-Balbuena S, de la Fuente L, Hoyos J, Rosales-Statkus ME, Barrio G, Belza M-J, et al. Highly visible street-based HIV rapid testing: is it an attractive option for a previously untested population? A cross-sectional study. Sex Transm Infect. 2013;90(2):112–8.
De la Fuente L, Delgado J, Hoyos J, Belza M, Alvarez J, Gutierrez J, et al. Increasing early diagnosis of HIV through rapid testing in a street outreach program in Spain. AIDS Patient Care STDS. 2009;23(8):625–9.
Lipsitz MC, Segura ER, Castro JL, Smith E, Medrano C, Clark JL, et al. Bringing testing to the people–benefits of mobile unit HIV/syphilis testing in Lima, Peru, 2007–2009. Int J STD AIDS. 2014;25(5):325–31.
Berghe WV, Nöstlinger C, Buve A, Beelaert G, Fransen K, Laga M. A venue-based HIV prevalence and behavioural study among men who have sex with men in Antwerp and Ghent, Flanders, Belgium, October 2009 to March 2010. Eurosurveillance. 2011;16(28):19914.
RüüTel K, Ustina V, Parker RD. Piloting HIV rapid testing in community-based settings in Estonia. Scand J Public Health. 2012;40:629–33.
Marcus U, Ort J, Grenz M, Eckstein K, Wirtz K, Wille A. Risk factors for HIV and STI diagnosis in a community-based HIV/STI testing and counselling site for men having sex with men (MSM) in a large German city in 2011–2012. BMC Infect Dis. 2015;15(1):14.
Mdodo R, Thomas PE, Walker A, Chavez P, Ethridge S, Oraka E, et al. Rapid HIV testing at gay pride events to reach previously untested MSM: US, 2009–2010. Public Health Rep. 2014;129(4):328–34.
Seth P, editor. CDC-funded HIV testing, HIV positivity, and linkage to HIV medical care among young MSM in the United States, 2013. In: 2015 APHA Annual Meeting & Expo (Oct 31–Nov 4, 2015); 2015: APHA.
Seth P, Wang G, Collins NT, Belcher L. Identifying new positives and linkage to HIV medical care—23 testing site types, United States, 2013. MMWR. 2015;64(24):663–7.
Yan H, Zhang R, Wei C, Li J, Xu J, Yang H, et al. A peer-led, community-based rapid HIV testing intervention among untested men who have sex with men in China: an operational model for expansion of HIV testing and linkage to care. Sex Transm Infect. 2014;90(5):388–93.
Snyder H, Yeldandi VV, Prem Kumar G, Liao C, Lakshmi V, Gandham SR, et al. Field-based video pre-test counseling, oral testing, and telephonic post-test counseling: implementation of an HIV field testing package among high-risk Indian men. AIDS Educ Prev. 2012;24(4):309–26.
Fernández-Balbuena S, Belza MJ, Zulaica D, Martinez JL, Marcos H, Rifá B, et al. Widening the access to HIV testing: the contribution of three in-pharmacy testing programmes in Spain. PLoS ONE. 2015;10(8):e0134631.
Calderon Y, Cowan E, Rhee JY, Brusalis C, Leider J. Counselor-based rapid HIV testing in community pharmacies. AIDS Patient Care STDS. 2013;27(8):467–73.
Darin KM, Klepser ME, Klepser DE, Klepser SA, Reeves A, Young M, et al. Pharmacist-provided rapid HIV testing in two community pharmacies. J Am Pharm Assoc. 2015;55(1):81–8.
Knight V, Wand H, Gray J, Keen P, McNulty A, Guy R. Convenient HIV testing service models are attracting previously untested gay and bisexual men; a cross-sectional study. JAIDS. 2015;69:e147–55.
Knight V, Ryder N, Guy R, Lu H, Wand H, McNulty A. New Xpress sexually transmissible infection screening clinic improves patient journey and clinic capacity at a large sexual health clinic. Sex Transm Dis. 2013;40(1):75–80.
Adebajo S, Eluwa G, Njab J, Oginni A, Ukwuije F, Ahonsi B, et al. Evaluating the effect of HIV prevention strategies on uptake of HIV counselling and testing among male most-at-risk-populations in Nigeria; a cross-sectional analysis. Sex Transm Infect. 2015;91(8):555–60.
Morin SF, Khumalo-Sakutukwa G, Charlebois ED, Routh J, Fritz K, Lane T, et al. Removing barriers to knowing HIV status: same-day mobile HIV testing in Zimbabwe. JAIDS. 2006;41(2):218–24.
Obermeyer CM, Osborn M. The utilization of testing and counseling for HIV: a review of the social and behavioral evidence. Am J Public Health. 2007;97(10):1762–74.
US Food and Drug Administration. Consumer health information. First rapid home-use HIV kit approved for self-testing. US Food and Drug Administration, 2012.
World Health Organization. HIV self-testing 2017. http://www.who.int/hiv/topics/self-testing/en/.
Figueroa C, Johnson C, Verster A, Baggaley R. Attitudes and acceptability on HIV self-testing among key populations: a literature review. AIDS Behav. 2015;19(11):1949–65.
Krause J, Subklew-Sehume F, Kenyon C, Colebunders R. Acceptability of HIV self-testing: a systematic literature review. BMC Public Health. 2013;13(1):1.
Pai NP, Sharma J, Shivkumar S, Pillay S, Vadnais C, Joseph L, et al. Supervised and unsupervised self-testing for HIV in high-and low-risk populations: a systematic review. PLoS Med. 2013;10(4):e1001414.
Bustamante MJ, Konda KA, Davey DJ, León SR, Calvo GM, Salvatierra J, et al. HIV self-testing in Peru: questionable availability, high acceptability but potential low linkage to care among men who have sex with men and transgender women. Int J STD AIDS. 2016;28:133–7.
Eaton LA, Driffin DD, Smith H, Conway-Washington C, White D, Cherry C. Black men who have sex with men, sexual risk-taking, and willingness to use rapid home HIV tests. Prev Sci. 2015;16(2):321–9.
Lippman SA, Périssé AR, Veloso VG, Sullivan PS, Buchbinder S, Sineath RC, et al. Acceptability of self-conducted home-based HIV testing among men who have sex with men in Brazil: data from an on-line survey. Cad Saude Publ. 2014;30(4):724–34.
Myers JE, Bodach S, Cutler BH, Shepard CW, Philippou C, Branson BM. Acceptability of home self-tests for HIV in New York City, 2006. Am J Public Health. 2014;104(12):e46–8.
Oldenburg CE, Biello KB, Perez-Brumer AG, Rosenberger J, Novak DS, Mayer KH, et al. HIV testing practices and the potential role of HIV self-testing among men who have sex with men in Mexico. Int J STD AIDS. 2016;28:242–9.
Pérez GM, Cox V, Ellman T, Moore A, Patten G, Shroufi A, et al. ‘I know that i do Have HIV but nobody saw me’: oral HIV self-testing in an informal settlement in South Africa. PLoS ONE. 2016;11(4):e0152653.
Marlin RW, Young SD, Bristow CC, Wilson G, Rodriguez J, Ortiz J, et al. Piloting an HIV self-test kit voucher program to raise serostatus awareness of high-risk African Americans, Los Angeles. BMC Public Health. 2014;14(1):1.
Woods WJ, Lippman SA, Agnew E, Carroll S, Binson D. Bathhouse distribution of HIV self-testing kits reaches diverse, high-risk population. AIDS Care. 2016;28(sup1):111–3.
Carballo-Diéguez A, Frasca T, Balan I, Ibitoye M, Dolezal C. Use of a rapid HIV home test prevents HIV exposure in a high risk sample of men who have sex with men. AIDS Behav. 2012;16(7):1753–60.
Chiu CJ, Young SD. Correlates of requesting home HIV self-testing kits on online social networks among African-American and Latino men who have sex with men. AIDS Care. 2016;28(3):289–93.
Rosengren AL, Huang E, Daniels J, Young SD, Marlin RW, Klausner JD. Feasibility of using Grindr™ to distribute HIV self-test kits to men who have sex with men in Los Angeles, California. Sex Health. 2016;13:389–92.
Volk JE, Lippman SA, Grinsztejn B, Lama JR, Fernandes NM, Gonzales P, et al. Acceptability and feasibility of HIV self-testing among men who have sex with men in Peru and Brazil. Int J STD AIDS. 2015;27:531–6.
Tao J, M-y Li, Qian H-Z, Wang L-J, Zhang Z, Ding H-F, et al. Home-based HIV testing for men who have sex with men in China: a novel community-based partnership to complement government programs. PLoS ONE. 2014;9(7):e102812.
Zhong F, Tang W, Cheng W, Lin P, Wu Q, Cai Y, et al. Acceptability and feasibility of a social entrepreneurship testing model to promote HIV self-testing and linkage to care among men who have sex with men. HIV Med. 2016;18:376–82.
Bavinton BR, Brown G, Hurley M, Bradley J, Keen P, Conway DP, et al. Which gay men would increase their frequency of HIV testing with home self-testing? AIDS Behav. 2013;17(6):2084–92.
Chen M, Bilardi J, Lee D, Cummings R, Bush M, Fairley C. Australian men who have sex with men prefer rapid oral HIV testing over conventional blood testing for HIV. Int J STD AIDS. 2010;21(6):428–30.
WHO. Guidelines on HIV Self-Testing and Partner Notification: Supplement to Consolidated Guidelines on HIV Testing Services. 2016.
Carroll A. State-sponsored homophobia: a world survey of sexual orientation laws: criminalisation, protection and recognition. In: Mendos LR, editor. 12 ed. Geneva: International Lesbian, Gay, Bisexual, Trans and Intersex Association; 2017.
Arreola S, Santos G-M, Beck J, Sundararaj M, Wilson PA, Hebert P, et al. Sexual stigma, criminalization, investment, and access to HIV services among men who have sex with men worldwide. AIDS Behav. 2015;19(2):227–34.
O’Byrne P, Bryan A, Roy M. HIV criminal prosecutions and public health: an examination of the empirical research. Med Humanit. 2013;39(2):85–9.
O’Byrne P, Willmore J, Bryan A, Friedman DS, Hendriks A, Horvath C, et al. Nondisclosure prosecutions and population health outcomes: examining HIV testing, HIV diagnoses, and the attitudes of men who have sex with men following nondisclosure prosecution media releases in Ottawa, Canada. BMC Public Health. 2013;13:94.
Berg RC, Ross MW, Weatherburn P, Schmidt AJ. Structural and environmental factors are associated with internalised homonegativity in men who have sex with men: findings from the European MSM Internet Survey (EMIS) in 38 countries. Soc Sci Med. 2013;78:61–9.
Deblonde J, De Koker P, Hamers FF, Fontaine J, Luchters S, Temmerman M. Barriers to HIV testing in Europe: a systematic review. Eur J Public Health. 2010;20(4):422–32.
Knox J, Sandfort T, Yi H, Reddy V, Maimane S. Social vulnerability and HIV testing among South African men who have sex with men. Int J STD AIDS. 2011;22(12):709–13.
Leblanc NM, Flores DD, Barroso J. Facilitators and barriers to HIV screening: a qualitative meta-synthesis. Qual Health Res. 2016;26(3):294–306.
Mayer KH, Wheeler DP, Bekker L-G, Grinsztejn B, Remien RH, Sandfort TG, et al. Overcoming biological, behavioral and structural vulnerabilities: New directions in research to decrease HIV transmission in men who have sex with men. J. Acquir Immune Defic Syndr. 2013;63(02):S161.
Elliot E, Rossi M, McCormack S, McOwan A. Identifying undiagnosed HIV in men who have sex with men (MSM) by offering HIV home sampling via online gay social media: a service evaluation. Sex Transm Infect. 2016;92(6):470–3.
Lau JT, Tsui HY, Lau MM. A pilot clustered randomized control trial evaluating the efficacy of a network-based HIV peer-education intervention targeting men who have sex with men in Hong Kong, China. AIDS Care. 2013;25(7):812–9.
Andrinopoulos K, Hembling J, Guardado ME, de Maria Hernández F, Nieto AI, Melendez G. Evidence of the negative effect of sexual minority stigma on HIV testing among MSM and transgender women in San Salvador, El Salvador. AIDS Behav. 2015;19(1):60–71.
Mannheimer S, Wang L, Wilton L, Tieu H, Del Rio C, Buchbinder S, et al. Infrequent HIV testing and late HIV diagnosis are common among a cohort of Black men who have sex with men (BMSM) in six US cities. J Acquir Immune Defic Syndr. 2014;67(4):438.
Solorio R, Forehand M, Simoni J. Attitudes towards and beliefs about HIV testing among Latino immigrant MSM: a comparison of testers and nontesters. AIDS Res Treat. 2013;2013:563537.
Walensky RP, Paltiel AD. Rapid HIV testing at home: does it solve a problem or create one? Ann Intern Med. 2006;145(6):459–62.
Poushter J. Smartphone ownership and internet usage continues to climb in emerging economies. Washington, DC: Pew Research Center; 2016.
van der Elst EM, Shally M, Odour C, Chirro O, Ibrahim F, Kombo B, et al. Peer-led oral HIV SELF testing finds undiagnosed HIV among MSM in Malindi, Kenya. In: Conference of Retroviruses and Opportunistic Infections, Seattle, WA; 2017.
Catania J. HIV self-testing in Afican American young MSM: a formative translational study. NIH Reporter. https://www.projectreporternihgov/.
Frye V, Wilton L. Testing an intervention to increase HIV self-testing among young, black MSM. NIH Reporter. https://www.projectreporternihgov/.
Tun W, Sekoni A. Assessing the acceptability, feasibility, and a potential distribution model of HIV oral self-testing (HST) among men who have sex with men (MSM) in Lagos, Nigeria. NIH Reporter. https://www.projectreporternihgov/.
Wei C. Development of an HIV self-testing intervention to reduce HIV risks among MSM: taking the guess out of the seroguessing. NIH Reporter. https://www.projectreporternihgov/.
Lippman SA. Self-conducted HIV tests—improving HIV prevention in key populations. NIH Reporter. https://www.projectreporternihgov/.
DiNenno EA. Recommendations for HIV screening of gay, bisexual, and other men who have sex with men—United States, 2017. MMWR. 2017;66:830.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Mr. Chadwick Campbell declares that he has no conflict of interest. Dr. Sheri Lippman declares that she has no conflict of interest. Dr. Nicholas Moss declares that he has no conflict of interest. Dr. Marguerita Lightfoot declares that she has no conflict of interest.
Ethical Approval
This article does not contain any studies with human participants performed by any of the authors.
Rights and permissions
About this article
Cite this article
Campbell, C.K., Lippman, S.A., Moss, N. et al. Strategies to Increase HIV Testing Among MSM: A Synthesis of the Literature. AIDS Behav 22, 2387–2412 (2018). https://doi.org/10.1007/s10461-018-2083-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-018-2083-8