Abstract
Many Australian gay men do not get tested for HIV at the recommended frequency. Barriers to HIV testing may be reduced by the availability of home HIV self-testing (HHST). An online cross-sectional questionnaire was conducted with 2,306 Australian gay men during 2009. Multivariate logistic regression identified factors associated with being likely to increase testing frequency if HHST was available, among previously-tested and never-tested men. Among 2,018 non-HIV-positive men, 83.9 % had been tested. Two-thirds indicated they would test more often if HHST was available irrespective of previous testing history. In multivariate analysis, independent predictors of increased testing frequency with HHST included preferences for more convenient testing, not having to see a doctor when testing and wanting immediate results among all men, as well as not being from an Anglo-Australian background and recent unprotected anal sex with casual partners among previously-tested men only. The majority of gay men report that being able to test themselves at home would increase their frequency of HIV testing.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Two-thirds of newly diagnosed HIV infections in Australia are among gay men and other men who have sex with men (MSM) and the rate of new HIV diagnoses is not declining [1]. Clinical guidelines recommend at least annual HIV testing for all sexually active gay men, with 3–6 monthly testing for higher risk men [2, 3]. HIV testing allows men to be linked into care and treatment, and there can be a prevention benefit as many gay men are highly motivated to prevent onward transmission after a positive diagnosis [4–7]. Additionally, the viral load reduction that can be achieved through treatment can substantially lower the risk of transmission to sexual partners [8]. Regular HIV testing is essential for the effective use of non-condom-based risk reduction strategies, such as negotiated safety [9, 10], serosorting [10, 11], and strategic positioning [10, 12]. It is also important for men in relational circumstances placing them at higher risk, such as men in serodiscordant relationships.
Despite these benefits of HIV testing, many gay men in Australia do not test at the frequency recommended by Australian health authorities [2, 13, 14]. It has been estimated that 20–31 % of HIV infection in gay men may be undiagnosed [15, 16], and 23 % diagnosed late [17]. The most commonly reported barriers to frequent clinic-based HIV testing are: men not perceiving themselves to be at risk; having to return for HIV results; and lack of time [7, 18, 19]. Recent changes to the Australian National HIV Testing Policy allow HIV-negative test results to be given over the telephone [20], but it is not yet clear if this new policy has been widely implemented. Given that point-of-care rapid HIV testing (RHT) is not yet commonly used in Australia, and that many men are still asked to return to the clinic for their results about 1 week after testing [20, 21], many high-risk men would need eight clinic visits per year according to the testing guidelines. For most men there is a financial cost attached to each visit.
RHT may address some barriers to testing, enable some men to increase their frequency of HIV testing, and alleviate the problem not returning for results [21–23]. The current Australian National HIV Strategy identifies research on RHT among gay men as a priority [24], however, home HIV self-testing (HHST) is not supported by the strategy or HIV Testing Policy [20, 24]. Concerns over HHST include the longer window period for accurate diagnosis and lower test sensitivity [25–28]. Individuals may purchase HHST kits from overseas and import them for personal use, but it is not yet legal for manufacturers to sell HHST directly to consumers within Australia [20, 24, 29].
Internationally, there is little research published on gay men’s awareness and use of HHST. In France, 30 % of nearly 10,000 men were aware of HHST [5, 6]. Only a small minority had already purchased a home test kit online [6]. Among men who had not previously heard of HHST, 86.5 % were interested in using it. Higher risk men and those living their homosexual lives in secrecy were interested in HHST [5]. In the US, three-quarters of men who intended to have an HIV test in the next year were interested in HHST as compared to half of men who did not intend to have a test in the next year [30]. In Australia, the limited research indicates interest in HHST among gay men. In 2011, 46 % of non-HIV-positive men reported that they would be more likely to get tested for HIV if they could use a rapid test at home [31, 32]. In a study of gay men recruited from community events, 63 % of non-positive men reported they would be likely to use HHST and 61 % indicated they would test more frequently if HHST became available [21]. Of those never tested for HIV, 85 % reported they would be likely to use HHST. Men were interested in the privacy, immediacy, painlessness and convenience of HHST [21].
The US Food and Drug Administration recently approved the first over-the-counter rapid HHST kit for sale in the US [25]. As Australian gay men may purchase and import HHST kits for personal use, the availability of HHST in the US is likely to have a direct impact in Australia among some gay men [29]. The aim of the current study was to explore which gay men would be more likely to increase the frequency of HIV testing if HHST was made available in Australia, and examine reasons for not testing among men who have never been tested.
Methods
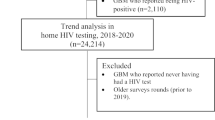
We used an anonymous, online, cross-sectional survey to investigate beliefs about the risks of HIV transmission among Australian gay men in a large sample recruited through gay community sources [33]. Ethics approval was obtained from the University of New South Wales and La Trobe University.
Participants
Men were eligible for the study if they were homosexually-identified or had had sex with another man in the previous year, and they lived in Australia. Participants were recruited to the anonymous online survey through promotional material at gay community events and venues, and through online promotion mainly via gay community associated websites and gay organisations. Of 2,306 men who provided useable complete responses, those who were not HIV-positive and who provided relatively complete responses were included in this analysis, resulting in a sample of 2,018 men.
Measures
The questionnaire included over 800 demographic, behavioural and attitudinal items. Men were asked about their most recent HIV test results and what they believed their current HIV serostatus to be. All men who indicated that they believed themselves to be HIV-negative or did not know their HIV status at the time of taking the questionnaire were asked if being able to take an HIV test at home would increase their frequency of HIV testing. Men who reported never having had an HIV test were asked their reasons for never testing. The questionnaire included items for several scales including: risk reduction beliefs, indicating extent of optimism about non-condom-based risk reduction strategies [33]; HIV viral load optimism, measuring extent of optimism about the effect of viral load on HIV transmission [34]; serosorting beliefs, measuring men’s belief in serosorting as an effective risk reduction strategy [35]; sexual sensation-seeking, indicating men’s interest in adventurous and risky sex [36]; and gay social engagement, assessing degree of social connection to other gay men [37].
Analysis
Data were analysed using SPSS™ software (Version 20, IBM). Demographic items, sexual behaviour items and attitudinal scales were included. The sample was divided into two groups: those who had previously been tested for HIV (“previously-tested”) and those who had not (“never-tested”). Descriptive statistics were used within each group to compare men who reported that HHST would increase their frequency of testing and those for whom it would not. Univariate analyses were conducted using Pearson’s Chi square test for categorical variables and between-groups analysis of variance for continuous variables. We used Type I error of 5 % for these analyses. Multivariate analysis to identify predictors of reporting that HHST would increase testing frequency was conducted using logistic regression models, generating adjusted odds ratios (AOR) and 95 % confidence intervals (CI).
Results
The mean age of all participants was 34.3 years (SD = 11.5). The majority of men identified as gay/homosexual (79.7 %), were Anglo-Australian (63.0 %), and were university educated (55.2 %). One-quarter of the men (26.2 %) had engaged in UAIC in the preceding 6 months. The majority of men (83.9 %) had been tested for HIV prior to completing the questionnaire (“previously-tested”) including 60.5 % who had been tested in the previous year. Approximately one-in-six men (16.1 %) had not been tested before (“never-tested”). Two-thirds (67.4 %) indicated that they would test more frequently if they could do the test themselves at home. Compared to never-tested men, previously-tested men were older (mean ages 35.4 [SD = 11.22] vs. 28.55 [SD = 11.50], F = 72.26, df1 = 1, df2 = 1,443, p < 0.001). There was no difference between previously-tested and never-tested men in the proportion who reported they would test more often if HHST was available (67.2 vs. 68.5 % respectively). Table 1 outlines the characteristics of both groups.
Men Previously Tested for HIV
In univariate analyses, socio-demographic factors associated with indicating the likelihood of increased testing frequency if HHST was available were: being younger, having a non-Anglo-Australian background, having a university-level education, and having higher gay social engagement scores (Table 2). Also, those who were likely to increase their testing frequency were somewhat younger than those who were unlikely to increase testing frequency (34.8 vs. 36.8 years; F = 8.65, df1 = 1, df2 = 1,211, p = 0.003). HIV testing factors included indicating they would test more frequently if testing was more convenient, if it did not have to involve consultation with a doctor, and if results were available immediately. Other behavioural and attitudinal factors associated with indicating they would test more often if HHST was available were: reported UAIC in the previous 6 months, higher scores on risk reduction beliefs, serosorting beliefs and sexual sensation-seeking.
In multivariate analysis, factors independently associated with indicating an increased frequency of testing with HHST were: being from a non-Anglo-Australian background (AOR 0.78; CI 0.61–0.99; p = 0.040), having engaged in UAIC in the previous 6 months (AOR 1.53; CI 1.17–2.01; p = 0.002), stating a preference for more convenient testing (AOR 1.93; CI 1.52–2.45; p < 0.001), stating a preference for not having to see a doctor when testing (AOR 4.24; CI 3.26–5.51; p < 0.001) and stating they would test more frequently if results were immediate (AOR 2.76; CI 2.13–3.59; p < 0.001).
Men Not Previously Tested for HIV
In univariate analyses among never-tested men, no socio-demographic factors were associated with increased testing if HHST was available. As with the previously-tested men, factors related to increased testing likelihood with HHST included: if testing was more convenient, if it did not involve consultation with a doctor, and if results were available immediately (Table 3). Attitudinal factors included higher scores on HIV viral load optimism and risk reduction beliefs.
Further univariate analyses with never-tested men related to their reasons for never having an HIV test (Table 4). The most common reason for not previously testing was that men believed themselves to be at low risk. A small proportion (15.6 %) of men who believed they were at low risk nonetheless reported having UAIC in the previous 6 months. Of the structural barriers to HIV testing generally, a little less than half reported not knowing where to get tested; and one-quarter found it difficult to get an appointment for testing. Also, one-in-five did not want to be seen at a sexual health clinic. Factors associated with a specific preference for HHST in univariate analyses included: difficulty in getting an appointment, not wanting to be seen at a sexual health clinic, costing too much, and not trusting the doctor’s confidentiality. That is, a greater proportion of those who stated that HHST would increase their frequency of testing also cited these as reasons for not having been tested.
In multivariate analysis, factors independently associated with indicating an increased frequency of testing with HHST were: stating a preference for not needing a doctor’s consultation when testing (AOR 3.54; CI 1.90–6.62; p < 0.001), stating they would test more frequently if results were immediate (AOR 1.87; CI 1.07–3.29; p = 0.029), and having higher optimism about the reduced transmission risk associated with undetectable viral load (AOR 1.47; CI 1.18–1.84; p = 0.001).
Discussion
Our findings indicate that gay men show a high degree of interest in HHST, with two-thirds of non-HIV-positive men stating that they would test more often if they could test themselves at home, regardless of previous testing history. In all men, reporting that HHST would increase the frequency of testing was associated with factors relating to testing convenience and a desire to avoid doctors’ consultations when testing. In previously-tested men, being from a non-Anglo-Australian background and reporting UAIC in the previous 6 months were also independently associated with interest in HHST.
Overall, the men in this sample were similar to other samples of Australian gay men [38]. Our findings were consistent with Australian and international studies on HHST in gay men as all studies have shown that a substantial proportion (and in some cases, the large majority) of gay men surveyed are interested in accessing HHST [5, 21, 30–32].
Although all gay men may benefit from the availability of HHST in Australia, it may be of particular benefit to some. First, men who need to test very frequently because of high-risk sexual behaviour may find the inconvenience of so many clinic visits the greatest barrier to more frequent testing [7]. For those men attending private clinics or general practitioners for testing, the potential cost of consultations, and time lost from the workplace, could also be a barrier. As HHST kits are not legally available for sale in Australia, the potential future cost of these kits is unknown. However, it is likely that they will be less expensive than the cost, including lost work time, of two doctor’s consultations. Second, men who have never been tested for HIV before may benefit from HHST [30] as they may not go to a clinic for conventional testing due to the inconvenience or difficulties in access (particularly in regional or rural areas), or because of particular concerns around confidentiality and privacy [5].
Four-fifths of our sample had ever been tested for HIV, which was slightly lower than the national self-reported rate of 85 % found in the Gay Community Periodic Surveys (GCPS). However, the proportion of non-HIV-positive men tested in the previous year was similar in our sample to the approximately 60 % in the GCPS [39]. The two samples, though, were broadly similar, and our findings were consistent with other studies comparing previously-tested and never-tested men [40, 41]. The mean age of the never-tested men was lower than the previously-tested men. Young men are less likely to have been tested, given that they have to commence testing at some point, but once they do test they then begin testing patterns similar to older men [40]. As has been previously found [41, 42], never-tested men were less socially engaged with other gay men than those who had previously been tested. Over two-thirds of men in both of these groups stated that having access to HHST would increase their frequency of testing.
As was found in an earlier Australian study [21], factors related to convenience of testing were important for both previously-tested and never-tested men. In both groups, men who indicated a desire not to see a doctor for HIV testing were approximately four times more likely to report that HHST would increase testing frequency. This may be related mostly to increasing convenience, or alternatively, men may specifically be interested in not having to see a doctor when being tested, perhaps because of a desire not to engage in a discussion with a doctor about risky sex. Those reporting that their testing would increase if results were immediate were nearly three times more likely to also state HHST would increase their testing in the previously-tested group, and nearly two times more likely in the never-tested group. For all men, but particularly those never tested before, having convenient, accessible home test kits available for purchase may increase their willingness to be tested.
Recent UAIC has been associated with interest in HHST among gay men [5]. In our study, UAIC in the previous 6 months was independently associated with interest in HHST in the previously-tested group, although not in the never-tested group. In these higher-risk men, our analysis indicates substantial interest in HHST: Three-quarters of those who had engaged in UAIC in the previous 6 months were likely to increase their frequency of testing with HHST; a smaller proportion of those who reported no UAIC indicated that HHST would increase their testing frequency. The higher-risk men may be seeking ways to decrease their risk of HIV infection while also maximising and prioritising the pursuit of pleasure through practicing UAIC [43–45]. They may view HHST as a technology that could aid in making non-condom-based risk reduction strategies safer, given that knowing one’s HIV status is imperative to the effectiveness of many of these strategies. Indeed, research with gay men in New York City has explicitly explored the notion that HHST may be used by gay men to screen sexual partners before engaging in UAIC [44, 46], that is, as a form of ‘enhanced serosorting’. Mathematical modeling of such a scenario has indicated that concerns over the increased window period of HHST and the risk for transmission due to false-negative results notwithstanding, there is a potential population decrease in HIV transmission through use of such a strategy [26]. If HHST becomes available in Australia, it will be important to educate higher-risk men about the increased window period and potential for false-negative test results. However, although testing sexual partners using HHST kits may not eliminate the risk of UAIC, it may still reduce the risk. Further exploration regarding the potential impact of HHST on frequency of HIV testing in high-risk men is warranted.
In never-tested men, there was an independent association between higher optimism about the reduced transmission risk associated with undetectable viral load and an interest in HHST. Never-tested men are typically less connected to gay community and less knowledgeable about HIV risk, so this may suggest the need to further explore these men’s understandings of HIV risk in the context of undetectable viral load.
Given that HHST is currently not supported by the National HIV Testing Policy and that no HHST kit has been approved, it is premature to discuss the implementation of home testing in Australia. However, if HHST does become available in the future, and given the broad interest in HHST among gay men in our study, it would perhaps be best to promote the kits’ availability and convenience benefits to all gay men. However, within this broad approach, higher-risk men and never-tested men stand out as important subgroups that could benefit from tailored social marketing and educational messages. Higher-risk men may benefit from detailed education regarding the window period of the tests and the potential for false-negative results. Such information could be incorporated into educational campaigns about how to increase the effectiveness of non-condom-based risk reduction strategies such as serosorting. Never-tested gay men are perhaps a more difficult subgroup to target, given that they are typically less connected to gay community [41, 42]. However, factors relating to convenience and confidentiality are clearly important to these men, and promoting these aspects of HHST could be an effective means to encourage these men to test themselves.
The present study had the strength of being community-based and participants can be considered broadly representative of gay men who are involved in the gay community in Australia. As an anonymous, online survey, men were unlikely to have concerns about confidentiality. The main limitations of this study arose because HHST was not the primary focus of the questionnaire. Men were not asked about their knowledge of HHST, its availability within Australia, or previous use. They were also not asked explicitly whether they would ever use HHST—the question was framed solely in terms of whether HHST would increase their frequency of testing. For those who stated that HHST would indeed increase their testing frequency, we did not explicitly ask why this may be the case. Finally, clinic-based and community-based RHT is not yet widely available in Australia, and this may have influenced the men’s stated interest in HHST.
Conclusions
Overall, the majority of non-HIV-positive men in Australia report that being able to test themselves at home for HIV would increase their frequency of HIV testing, irrespective of whether they had ever been tested before or not. Men in this study would like HIV testing to be more convenient. Men who had both been previously tested and who had never tested were also interested in testing more if HIV testing was made more convenient, immediate, and did not necessarily involve a doctor’s consultation. Previous studies have found that gay men report significant barriers to HIV testing and these need to be addressed if the rate of testing is to be increased, especially among high-risk men who may need four or more HIV tests per year to meet current guidelines. While there are some reasonable concerns around the introduction of HHST into Australia, these concerns must be balanced against gay men’s clear interest in ways to increase the convenience of testing in general, and in home testing in particular. Furthermore, the results of our study demonstrate that for men who had previously been tested for HIV, UAIC was associated with an interest in HHST. That is, men at greater risk of HIV infection are even more likely than other gay men to be interested in using HHST to increase their frequency of testing. These findings indicate that Australian gay men are seeking strategies to make HIV testing easier. Despite the evidence indicating that gay men are interested in using HHST to increase their testing frequency, and despite the approval of home testing in the United States, such a policy change in Australia is currently not forthcoming (nor does it appear to be elsewhere in the world). However, these data demonstrate clearly that gay men’s interest in HHST is strong, and provide support for the continued evaluation and introduction of HHST as a means of increasing frequency and accessibility of HIV testing in Australia. Policy makers need to consider data such as these demonstrating the widespread and strong support for HHST amongst gay men in their determinations about its introduction.
References
Kirby Institute. HIV, viral hepatitis and sexually transmissible infections in Australia: Annual surveillance report 2011. Sydney, NSW: The Kirby Institute, University of New South Wales, 2011. www.kirby.unsw.edu.au/sites/hiv.cms.med.unsw.edu.au/files/hiv/resources/2011AnnualSurvReport_0.pdf. Accessed 17 Sept 2012.
Guy R, Goller JL, Spelman T, et al. Does the frequency of HIV and STI testing among men who have sex with men in primary care adhere with Australian guidelines? Sex Transm Infect. 2010;86:371–6.
STIs in Gay Men Action Group. STI testing guidelines for men who have sex with men (MSM). Sydney, NSW: STIs in Gay Men Action Group; 2010. www.stigma.net.au/resources/STIGMA_MSM_Testing_Guidelines_2010.pdf. Accessed 8 Aug 2012.
Crepaz N, Marks G, Liau A, et al. Prevalence of unprotected anal intercourse among HIV-diagnosed MSM in the United States: a meta-analysis. AIDS. 2009;23:1617–29.
Greacen T, Friboulet D, Blachier A, et al. Internet-using men who have sex with men would be interested in accessing authorised HIV self-tests available for purchase online. AIDS Care. 2012. doi:10.1080/09540121.2012.687823.
Greacen T, Friboulet D, Fugon L, et al. Access to and use of unauthorised online HIV self-tests by internet-using French-speaking men who have sex with men. Sex Trans Infect. 2012;88:368–74.
Prestage G, Brown G, Keen P. Barriers to HIV testing among Australian gay men. Sex Health. 2012;9(5):453–8.
Cohen MS, Chen YQ, McCauley M, et al. Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med. 2011;365:493–505.
Crawford JM, Rodden P, Kippax S, et al. Negotiated safety and other agreements between men in relationships: risk practice redefined. Int J STD AIDS. 2001;12:164–70.
Jin F, Crawford JM, Prestage G, et al. Unprotected anal intercourse, risk reduction behaviours, and subsequent HIV infection in a cohort of homosexual men. AIDS. 2009;23:243–52.
Zablotska IB, Imrie J, Prestage G, et al. Gay men’s current practice of HIV seroconcordant unprotected anal intercourse: serosorting or seroguessing? AIDS Care. 2009;21:501–10.
Jin F, Jansson J, Law M, et al. Per-contact probability of HIV transmission in homosexual men in Sydney in the era of HAART. AIDS. 2010;24:907–13.
Prestage G, McCann PD, Hurley M, et al. Pleasure and Sexual Health: The PASH Study. Sydney, NSW: National Centre in HIV Epidemiology and Clinical Research, University of New South Wales, 2009. www.kirby.unsw.edu.au/sites/hiv.cms.med.unsw.edu.au/files/hiv/attachment/PASH2009-final.pdf. Accessed 14 Sept 2012.
Wand H, Yan P, Wilson D, et al. Increasing HIV transmission through male homosexual and heterosexual contact in Australia: results from an extended back-projection approach. HIV Med. 2010;11:395–403.
Pedrana AE, Hellard ME, Wilson K, et al. High rates of undiagnosed HIV infections in a community sample of gay men in Melbourne Australia. JAIDS. 2012;59:94–9.
Birrell F, Staunton S, Debattista J, et al. Pilot of non-invasive (oral fluid) testing for HIV within a community setting. Sex Health. 2010;7:11–6.
Lemoh C, Guy R, Yohannes K, et al. Delayed diagnosis of HIV infection in Victoria 1994 to 2006. Sex Health. 2009;6:117–22.
De Wit J, Adam P. To test or not to test: psychosocial barriers to HIV testing in high-income countries. HIV Med. 2008;9:20–2.
Koelmeyer R, Grierson J, Pitts M. Motivations for and barriers to HIV testing in Australia. Melbourne, Victoria: Australian Research Centre in Sex, Health and Society, La Trobe University, 2011. www.ashm.org.au/images/arv_guidelines/arcshs_motivations_for_and_barriers_to_hiv_testing_report.pdf. Accessed 17 Sept 2012.
Department of Health and Ageing. National HIV Testing Policy. Canberra, ACT: Commonwealth of Australia; 2010. www.testingportal.ashm.org.au/resources/Australian_National_HIV_Testing_Policy_v1-1.pdf. Accessed 16 Sept 2012.
Chen MY, Bilardi JE, Lee D, et al. Australian men who have sex with men prefer rapid oral HIV testing over conventional blood testing for HIV. Int J STD AIDS. 2010;21:428–30.
Healey LM, O’Connor CC, Templeton DJ. HIV result giving. Is it time to change our thinking? Sex Health. 2010;7:8–10.
Pedrana AE, Guy R, Bowring A, et al. Community models of HIV testing for men who have sex with men (MSM): Systematic review 2011. Melbourne, Victoria: Report commissioned by ACON; 2011. www.ashm.org.au/images/pdfs/national%20strategies/hiv/acon_literature_review_final_version.pdf. Accessed 17 Sept 2012.
Department of Health and Ageing. Sixth National HIV Strategy 2010–2013. Canberra, ACT: Commonwealth of Australia, 2010. http://www.health.gov.au/internet/main/publishing.nsf/Content/ohp-national-strategies-2010-hiv/$File/hiv.pdf. Accessed 1 Sept 2012.
US Food and Drug Administation. FDA approves first over-the-counter home-use rapid HIV test (press release). Silver Spring, MD: US Food and Drug Administration; 2012. www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm310542.htm. Accessed 4 July 2012.
Ventuneac A, Carballo-Diéguez A, Leu CS, et al. Use of a rapid HIV home test to screen sexual partners: an evaluation of its possible use and relative risk. AIDS Behav. 2009;13:731–7.
Haddow L, Robinson A. A case of a false positive result on a home HIV test kit obtained on the internet. Sex Transm Infect. 2005;81:359–60.
Chen MY, Estcourt CS. Time to roll out rapid testing for HIV? Yes, but with appropriate safeguards. Sex Health. 2009;6:1–3.
Therapeutic Goods Administration. The use of rapid tests for HIV in Australia. Canberra ACT: Therapeutic Goods Administration. www.tga.gov.au/consumers/information-devices-hiv-rapid-tests.htm. Accessed 17 August 2012.
MacKellar DA, Hou SI, Whalen CC, et al. Reasons for Not HIV Testing, Testing Intentions, and Potential Use of an Over-the-Counter Rapid HIV Test in an Internet Sample of Men Who Have Sex With Men Who Have Never Tested for HIV. Sex Trans Dis. 2011;38:419–28.
Hull P, Holt M, Mao L, et al. Gay Community Periodic Survey: Sydney, February 2011. Sydney, NSW: National Centre in HIV Social Research, The University of New South Wales, 2011. http://nchsr.arts.unsw.edu.au/media/File/GCPS_2011_Sydney_February_Report.pdf. Accessed 3 August 2012.
Lee E, Holt M, Mao L, et al. Gay Community Periodic Survey: Melbourne, February 2011. Sydney, NSW: National Centre in HIV Social Research, The University of New South Wales, 2011. http://nchsr.arts.unsw.edu.au/media/File/1_GCPS_2011_Melbourne.pdf. Accessed 3 August 2012.
Prestage G, Down IA, Bradley J, et al. Is optimism enough? Gay men’s beliefs about HIV and their perspectives on risk and pleasure. Sex Transm Dis. 2012;39:167–72.
Prestage G, Brown G, Down IA, et al. “It’s hard to know what is a risky or not a risky decision”: gay men’s beliefs about risk during sex. AIDS Behav. 2012. doi:10.1007/s10461-012-0180-7.
Kalichman SC, Eaton L, White D, et al. Beliefs about treatments for HIV/AIDS and sexual risk behaviors among men who have sex with men, 1997–2006. J Behav Med. 2007;30:497–503.
Kalichman SC, Weinhardt L, DiFonzo K, et al. Sensation seeking and alcohol use as markers of sexual transmission risk behavior in HIV-positive men. Ann Behav Med. 2002;24:229–35.
Prestage G, Mao L, McGuigan D, et al. HIV risk and communication between regular partners in a cohort of HIV-negative gay men. AIDS Care. 2006;18:166–72.
Holt M, Lee E, Prestage G, et al. The converging and diverging characteristics of HIV-positive and HIV-negative gay men in the Australian Gay Community Periodic Surveys, 2000–2009. 2012. doi:10.1080/09540121.2012.686598.
Holt M, Mao L, Prestage G, et al. Gay Community Periodic Surveys: National Report 2010. Sydney, NSW: National Centre in HIV Social Research, The University of New South Wales, 2010. http://nchsr.arts.unsw.edu.au/media/File/GCPS_2010_National_report.pdf. Accessed 8 Sept 2012.
Zablotska IB, Holt M, de Wit J, et al. Gay men who are not getting tested for HIV. AIDS Behav. 2012. doi: 10.1007/s10461-012-0184-3.
Jin FY, Prestage G, Law MG, et al. Predictors of recent HIV testing in homosexual men in Australia. HIV Med. 2002;3:271–6.
Van de Ven P, Prestage G, Knox S, et al. Gay men in Australia who do not have HIV test results. Int J STD AIDS. 2000;11:456–60.
Balán IC, Carballo-Diéguez A, Ventuneac A, et al. Are HIV-negative men who have sex with men and who bareback concerned about HIV infection? Implications for HIV risk reduction interventions. Arch Sex Behav. 2012. doi:10.1007/s10508-011-9886-2.
Carballo-Diéguez A, Frasca T, Dolezal, C, et al. Will gay and bisexually active men at high risk of infection use over-the-counter rapid HIV tests to screen sexual partners? J Sex Res. 2012. doi:10.1080/00224499.2011.647117.
Carballo-Diéguez A, Ventuneac A, Dowsett GW, et al. Sexual pleasure and intimacy among men who engage in “bareback sex”. AIDS Behav. 2011;15:57–65.
Carballo-Diéguez A, Frasca T, Balán IC, et al. Use of a rapid HIV home test prevents HIV exposure in a high risk sample of men who have sex with men. AIDS Behav. 2012. doi:10.1007/s10461-012-0274-2.
Acknowledgments
The authors would like to thank the participants and the many people and organisations that assisted with recruitment and referral of potential participants to the study. This study was commissioned and funded by the Departments of Health in the states of New South Wales, Victoria, South Australia and Western Australia. Indirect support was also provided by the Queensland Health Department. The Kirby Institute is affiliated with the Faculty of Medicine, University of New South Wales. The Australian Research Centre in Sex Health and Society (ARCSHS) is affiliated with the Faculty of Health Sciences, La Trobe University. The Kirby Institute and ARCSHS receive funding from the Commonwealth of Australia Department of Health and Ageing.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bavinton, B.R., Brown, G., Hurley, M. et al. Which Gay Men Would Increase Their Frequency of HIV Testing with Home Self-testing?. AIDS Behav 17, 2084–2092 (2013). https://doi.org/10.1007/s10461-013-0450-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-013-0450-z