Abstract
This study examined associations of sleep and minutes spent in moderate-vigorous physical activity (MVPA) with C-reactive protein (CRP) and interleukin (IL)-6 among persons living with HIV. Cross-sectional analyses (n = 45) focused on associations of inflammatory outcomes (i.e., CRP and IL-6) with actigraph-derived sleep duration, latency, and efficiency; sleep onset; wake time; and wake-after-sleep-onset; as well as MVPA. Least square means for CRP and IL-6 by levels of sleep and MVPA were computed from general linear models. Individuals below the median of sleep duration, above the median for sleep onset, and below the median of MVPA minutes had higher CRP or IL-6 levels. Generally, individuals with both low MVPA and poor sleep characteristics had higher inflammation levels than those with more MVPA and worse sleep. Understanding the combined impact of multiple lifestyle/behavioral factors on inflammation could inform intervention strategies to reduce inflammation and therefore, chronic disease risk.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sleep is a physiological necessity. Disrupted sleep has been associated with a host of chronic physical and mental disorders, abnormal hormone and immune functioning, and mortality [1–4]. It is possible that mechanisms involving inflammatory pathways may partially explain the associations between sleep disruption and chronic disease. Chronic inflammation due to repeated insults or ‘injuries’ (e.g., tobacco use, chronic infection, chronic pain, repeated sleep disruption) is an underlying pathophysiological process that has been associated with numerous chronic conditions including cancer, diabetes, cardiovascular disease (CVD), obesity, metabolic syndrome, and mortality [5–7]. Systemic inflammation most likely involves a complex causal web involving many factors, including bio-behavioral influences [3].
The literature describing relationships between obstructive sleep apnea (OSA) and inflammation is extensive [8]. A recent meta-analysis including 51 studies found that, compared to controls, individuals with OSA had statistically greater C-reactive protein (CRP), tumor necrosis factor-α (TNF-α), and interleukin (IL)-6 [9]. Additionally, numerous experimental studies have indicated increased levels of white blood cells, TNF-α, IL-6 or CRP following sleep deprivation compared to normal sleeping conditions [10–12]. Most of the existing literature based on observational studies focusing on sleep and inflammation has been centered on sleep duration. Generally, short sleep or reduced sleep duration over time have been associated with increased inflammation [13–16]. For example, A study by Ferrie et al. [13] using the Whitehall II study participants, found that reduction in sleep duration of 1 h from the 1991/1994 to the 1997/1999 cycles was associated with an 8.1 % increase and 4.5 % increase in CRP and IL-6 (both p < 0.01), respectively. Long sleep duration also has been associated with inflammation [14, 15, 17, 18]. However, there is some inconsistency in definitions of short and long sleep duration, as well as statistical significance of findings between studies. Poor subjective sleep quality (as assessed by the Pittsburgh Sleep Quality Index), symptoms associated with worse sleep quality, and self-reported sleep debt also have been associated with elevated inflammation [19–24]. However, several studies have found no association between certain disrupted or inadequate sleep measures and inflammation [25–28]. Additionally, many of these previous studies have been limited to subjective measures of sleep [13–17, 19, 20, 22, 23, 27, 28].
Physical activity is one lifestyle factor that has been associated with both better sleep and reduced inflammation. Although intense bouts of physical activity have been shown to increase inflammation, long-term physical activity and greater cardiorespiratory fitness have been shown to lower levels of inflammation biomarkers [3, 29]. The effects of physical activity on sleep might be moderated by the duration, intensity, and timing of physical activity. However, in general, increased sleep and higher sleep quality have been associated with regular physical activity [30–32]. Of particular interest is the combined effect of sleep and physical activity on inflammation, which has yet to be fully elucidated among human populations. Using animal models, Zielinski et al. found reductions in IL-6 and TNF levels following 11 weeks of exercise training in wild-type mice under normal sleep conditions. However, exercise had no effect on IL-6 or TNF levels among sleep-restricted mice [33].
Persons living with HIV (PLWH) have often reported poor sleep quality and disruptions in routine sleeping habits that are believed to be caused by factors such as psychological distress, low socio-economic status, and viral and pharmacological side-effects (e.g. peripheral neuropathy resulting in chronic pain, migraines, nausea, insomnia) [34–36]. These sleep disruptions, in turn, have the potential to contribute to increased levels of fatigue and sedentary behavior. As least partly due to low levels of daily physical activity, drastic reductions in cardiorespiratory fitness (i.e. VO2max) have been found among HIV/AIDS patients [37–39], which have been consistently reported since the discovery of HIV both before and after the initiation of anti-retroviral therapy (ART) [40]. Thus, it seems that these reductions in fitness are a result of more than just HIV-related treatments.
In addition to disturbances in sleep quality, PLWH also exhibit a state of chronic inflammation. The extent to which this is a result of HIV infection, ART toxicities, or daily lifestyle habits is not well understood; it is likely that a combination of factors is responsible [41]. Although ART has successfully halted viral replication and therefore viral load, PLWH receiving ART still exhibit increased levels of inflammation [41]. For example, a recent study by Brigham and colleagues compared a sample of men who were HIV-negative with two groups of HIV-positive men (those receiving ART and those who were not). They found that plasma levels of TNF-alpha and IL-6 were higher only in those who were HIV+ with moderate to severe OSA compared to those with no OSA or mild levels of OSA independent of HIV-related covariates or treatment [42]. Other studies have shown increased plasma levels of various cytokines and markers of inflammation among PLWH regardless of ART treatment [43, 44]. However, many of these studies did not incorporate sleep-related metrics that have been associated with inflammation in numerous non-HIV populations. Chronic conditions associated with inflammation such as CVD, type II diabetes, cancer, neurocognitive dysfunction, frailty, and many others, are often seen at higher-than-expected rates in elderly populations with HIV or AIDS [45]. Recently, it has become a top priority among healthcare professionals to discover new ways that may suppress immune system activation.
This current study was designed to examine the combined association of objectively measured physical activity and sleep with inflammatory levels among PLWH who had been recruited for a randomized controlled trial of exercise training [46]. We hypothesized that levels of CRP and IL-6 would be greater among individuals with ‘unhealthy’ sleep characteristics (e.g., later bed or wake times, short sleep duration, long sleep latency, low sleep efficiency, high wake-after-sleep-onset [WASO] minutes), which were objectively measured using BodyMedia’s SenseWear® physical activity armband. Additionally, we hypothesized that the combined effect of sleep and physical activity levels on inflammation would be greater than the effect of either exposure individually.
Methods
This cross-sectional study included baseline data from a larger home-based randomized control trial among PLWH. A complete description of the methodology, recruiting, and participant screening protocols for this home-based trial can be found elsewhere [46]. The research protocol was approved by the University of South Carolina Institutional Review Board. Written informed consent was obtained from all participants prior to any data collection.
Participants
Study participants were from a local sample of PLWH in the greater Columbia and Charleston, South Carolina areas. Participants were recruited from local healthcare providers, flyers posted at HIV support group centers, and word of mouth. Data were obtained from a total of 45 PLWH (26 males and 19 females) currently taking ART who had valid SenseWear® armband data.
Independent Variables: Sleep and Physical Activity Assessment
Sleep and physical activity patterns were assessed for 7–10 days with the SenseWear® armband, a commercially available lightweight physical activity monitor that is worn on the upper left arm halfway between the acromion and olecranon processes. The SenseWear® armband uses tri-axial accelerometry technology augmented by two heat sensors (a thermistor-based skin surface sensor and a heat flux sensor), and a galvanic skin response sensor. These four internal sensors turn on the monitor when detecting skin contact and measures total time the armband was worn, daily energy expenditure, step count, sleep, and the intensity, duration, and frequency of physical activity bouts [47, 48]. All armband data were analyzed by computer-based software using demographic information (sex and age), height and weight applied to proprietary algorithms. Moderate-vigorous physical activity (MVPA) minutes, measured by the SenseWear® armband, were defined as any activity ≥3 metabolic equivalent. Levels of MVPA were divided into two groups based on a median split (<70 vs. ≥70 minutes/day of MVPA).
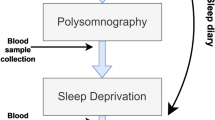
Using the latest proprietary algorithms from the SenseWear® software (SenseWear Professional software version 7.0; BodyMedia Inc.) each recorded minute-epoch has a sleep/wake designation. A few studies have indicated high correlation, percent agreement, or intraclass correlation between wrist actigraphy or polysomnography (PSG) and the SenseWear® armband for total sleep time, WASO, and sleep efficiency [49–52]. Only nighttime sleep was characterized. Participants did not record daytime activities during non-wear periods; therefore, making it difficult to reliably and fully discern daytime napping. Sleep onset was defined as the first of three consecutive minutes when the subject was asleep, in conjunction with at least 10 minutes lying down. Wake time was defined as the first of 90 consecutive minutes of wakefulness. After removing possible ‘daytime’ naps (i.e., sleep bouts <4 hours ending between noon and 10 p.m.), it was still possible that individuals had multiple sleep bouts for a single day. Multiple bouts per day were further reviewed and either combined to create one nighttime bout or considered naps that did not meet the standard definition of naps above. Total sleep time was the sum of all sleep minutes during the nighttime sleep bout. Sleep latency was the sum of minutes between lying down and falling asleep. WASO required subjects to be scored awake for two consecutive minutes after the onset of sleep and summed until the final wake time. Lastly, sleep efficiency was defined as total sleep time divided by the length of the nighttime sleep bout. Subjects had to have a least three nights of evaluable data to be included in the analyses. Due to the limited sample size (n = 45), a median split for each sleep metric was created instead of more standard cut-points (see Table 3 for cut-points).
Sleep metric categories were then combined with MVPA categories. For example, sleep efficiency and MVPA minutes were combined into the following categories: low sleep efficiency and low MVPA minutes (‘most unhealthy’ category), low sleep efficiency and high MVPA minutes, high sleep efficiency and low MVPA minutes, and high sleep efficiency and high MVPA minutes (‘healthiest’ category) with the comparison of interest being between the ‘healthiest’ and ‘most unhealthy’ categories (see Table 3, supplemental Table A displays the full results and p values for each category compared to the ‘healthiest’ category).
Outcomes: CRP and IL-6
Blood draws occurred in the early morning following a 12-h fast. Blood serum was separated via centrifuge and stored in a −80 °C freezer until analysis. CRP and IL-6 (higher values indicating greater systemic inflammation) were measured in duplicate by the LabCorp Clinical Trials Division using a standard protocol for immunochemiluminometric assays at a central location that undergoes rigorous quality assurance testing to deliver high accuracy and reliability.
Clinical Assessment and Self-Reported Measures
Clinical assessments included measures of resting blood pressure, waist and hip circumference, height, and weight. Waist-to-hip ratio and body mass index (BMI, kg/m2) were calculated. Basic demographic (e.g., race, gender, income, education) information was obtained, as well as sexual orientation, putative route of HIV infection, smoking status, and comorbidities. Numerous psychosocial and behavior questionnaires (e.g., social support for physical activity [53], decisional balance [54], perceived stress scale [55], Michigan alcohol screening test [56], process of change [57], and SF-36 [58]) also were examined as potential confounders.
Statistical Analyses
All analyses were performed using SAS® version 9.3 (Cary, NC, USA). Descriptive statistics for selected covariates and the sleep metrics were computed using frequencies or means for categorical and continuous variables, respectively. Variable selection began as a series of bivariate analyses (sleep metric + covariate). Covariates with a p value of ≤0.20 were added to a ‘full’ model. A backward elimination procedure was then used to develop ‘final’ models that included all variables that, when removed from the model, changed the beta coefficient of the sleep metric by at least 10 %. All statistically significant (p < 0.05) covariates also were kept in the model.
General linear models were used to compute least square means along with 95 % confidence intervals (95 % CI) for CRP and IL-6 among median splits of each sleep metric and MVPA minutes, and among the categories of the combined sleep and MVPA measures.
Results
Most participants (58 % male) had at least some college education (66 %), and were predominately single (78 %), black (82 %), current or former smokers (63 %), and overweight (mean BMI 29.9 ± 6.7 kg/m2). Additionally, a majority of the participants had an annual household income <$30,000 (67 %); 88 % had HIV (of which half were symptomatic), as opposed to having AIDS (which was based on self-report); and had relatively high crude baseline levels of CRP (5.5 ± 6.1 mg/L) and IL-6 (3.6 ± 1.8 pg/mL) (Table 1). The average age was 47.1 ± 9.4 years. The mean sleep onset and wake time were 12:00 a.m. and 7:32 a.m., respectively. Participants spent, on average, ≈7.5 hours in bed, but had an average sleep duration of only 5.5 hours. This was reflected by a high mean WASO of 85 minutes. Mean sleep efficiency was only 74 % (data not tabulated).
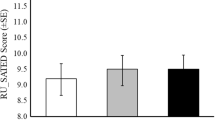
Results of analyses examining the relationship between each sleep metric or MVPA minutes and inflammation are shown in Table 2. Participants below the median of total sleep time (i.e., <339 minutes) had higher CRP values (6.9 vs. 2.0 mg/L, p = 0.05) compared to those above the median. For IL-6, those above the median of sleep onset (i.e., >11:46 p.m.; 4.8 vs. 3.7 pg/mL, p = 0.01) and those below the median of total sleep time (4.9 vs. 3.6 pg/mL, p = <0.01) had elevated values compared to those below the median of sleep onset and above the median of total sleep time, respectively. Participants performing at least 70 minutes of MVPA per day had lower CRP values compared to participants with <70 minutes of MVPA (1.6 vs. 4.6 mg/L, p = 0.04). However, no statistically significant association was observed between daily average MVPA minutes and IL-6 (Table 2).
Table 3 displays the results for combined sleep and MVPA. For CRP, participants with a later sleep onset and lower MVPA minutes compared to participants with earlier sleep onsets and higher MVPA minutes (CRP = 6.5 vs. 1.1 mg/L, p = 0.03) showed statistically significantly greater values. Similarly, those with lower total sleep time and lower MVPA minutes compared to higher total sleep and higher MVPA minutes (CRP = 6.7 vs. 1.0 mg/L, p = 0.01) had higher CRP values. The same was true for those with lower sleep efficiency (i.e., <73 %) and lower MVPA minutes compared to those with higher sleep efficiency and higher MVPA minutes (CRP = 7.8 vs. 1.3 mg/L, p = 0.02); and higher WASO (i.e., >85 minutes) and lower MVPA minutes compared to lower WASO and higher MVPA minutes (CRP = 3.9 vs. 1.0 mg/L, p = 0.04). For IL-6, participants with later bedtimes and lower MVPA minutes compared to earlier bedtimes and higher MVPA minutes (IL-6 = 5.0 vs. 3.4 pg/mL, p = 0.02); and participants with lower total sleep time and lower MVPA minutes compared to higher total sleep and higher MVPA minutes (IL-6 = 5.3 vs. 4.0, p = 0.02) had greater values.
Discussion
This study found that inflammation in PLWH was associated with various sleep metrics, especially later sleep onset and less total sleep time. Additionally, participants in the categories representing less MVPA and ‘less healthy’ sleep (i.e., later sleep onset, less total sleep time, lower sleep efficiency, and more WASO) had higher levels of CRP or IL-6. Generally, our findings of the associations of poor sleep with inflammation are consistent with previous literature, which indicates that disturbed or inadequate sleep is associated with inflammation [9–24, 59, 60]. However, this is one of the first studies to perform such an analysis among PLWH.
The present study expands on these previous findings by showing associations between inflammation markers and objectively measured sleep duration, as well as other measures including sleep onset and wake times, sleep efficiency and latency, and WASO. However, comparisons to previous studies, although possible, can be difficult due to differing definitions of sleep measures. This is especially true for sleep duration. The current study utilized median splits due to the limited sample size. Therefore, shorter and longer sleep duration was below and above 5.75 hours, respectively, which is typically a lower cut-point for sleep duration than other studies. It should be noted, however, that objectively measured sleep duration is often about 1 hour less than subjective sleep duration [61].
The literature indicates that the relationship between inflammation and sleep is most likely described by a complex model involving numerous demographic and behavioral factors with several different pathways [62–65]. Physical activity is associated with both sleep and inflammation [3, 30–32] and the combined impact of disturbed sleep and low levels of physical activity on inflammation may be stronger than either factor independently. In further support of combining the effect of sleep and physical activity, the current study observed that those in sleep metric categories indicative of ‘healthier’ sleep characteristics had between 16 and 55 % greater average daily MVPA minutes compared to those in ‘less healthy’ sleep categories (data not shown). We hypothesized that the combined influence of both sleep and physical activity would tend to modify the effect on inflammation. This was supported by our results and by similar previous findings using mouse models [33]. This model is an oversimplification of the true causal pathway describing the relationship between sleep, lifestyle factors, and inflammation. This is especially true among populations living with a chronic condition such as HIV or AIDS.
For example, it is possible that the relationships observed in this study were, in-part, mediated by unmeasured factors associated with chronic pain (including lower back), arthritis, and other bone/joint problems (known to be associated with inflammation), poor sleep quality, and sedentary behavior, which sometimes are observed among PLWH. Although sleep and physical activity may influence inflammation among PLWH, their effect on disease progression (e.g., viral load) and how that further influences inflammation is not well understood. However, disturbed sleep clearly has a negative effect on immunity. Reports have shown decreases in T-cells (e.g. CD4+, CD3+, etc.) in patients with poor sleep quality, as well as those with OSA [66–68]. However, these decrements in immunity due to sleep have not been shown to impact disease progression as indicated by HIV viral load. To our knowledge, the same is true for physical activity. The combined effect of reduced physical activity and disrupted sleep on inflammation, in conjunction with changes in disease progression among humans should be further explored, especially among those living with a chronic condition such as HIV or AIDS.
This study had several noteworthy strengths. Sleep and physical activity were both objectively measured using the SenseWear® armband. Several studies have used the summary sleep measures provided by the proprietary algorithms from the SenseWear® armband [52, 69, 70]. However, few have taken advantage of the capacity to calculate sleep-related parameters from the minute-by-minute sleep/wake designations, which are typically well correlated with other objective measures of sleep (e.g., PSG, wrist actigraphy) [49–51]. In addition to providing more evidence for an association between disturbed sleep and inflammation, this was one of the first studies to examine the combined effect of sleep and physical activity on inflammation using a population with a chronic condition (i.e., HIV or AIDS). Also, this study was able to examine numerous potential confounders, especially those related to psychosocial constructs.
In addition to the strengths, several limitations were present. As with other actigraphs, several reports indicate that the ability of the SenseWear® armband to differentiate between wakefulness and sleep becomes attenuated as sleep efficiency decreases [51, 52]. This is of particular concern considering that PLWH have been shown to report high levels of chronic fatigue and sleep disturbances [34]. Additionally, common side effects often reported among certain ART medications include sleep disturbances, such as insomnia and poor sleep efficiency [35]. Considering the entire study sample was comprised of PLWH currently on a stable ART regimen, we were not only able to adjust for any potential ART-related differences, but it is suspected that any error would be non-differential in nature, therefore, biasing results towards the null. Although, this study had examined numerous confounders, potential residual confounding or lack of adjustment for unmeasured covariates cannot be completely ruled out. One of those covariates could potentially be chronic pain experienced by HIV-related peripheral neuropathy, a common comorbidity among PLWH [71, 72]. We cannot overlook this as a potential cause of the increased markers of inflammation, as well as the sleep disturbances within our study sample.
Other limitations include the limited sample size (n = 45 for CRP; n = 42 for IL-6) which may partially explain the lack of statistical significance for some results. The small sample size precluded comparisons by other factors, such as sex. Previous studies have found that the relationship between sleep and inflammation differs by sex, although there is some inconsistency [14, 15, 17, 19, 23, 24, 28]. For example, one study found the odds of a CRP value above 3.0 mg/L was greater among long sleepers [odds ratio (OR) 1.50, 95 % confidence interval (95 % CI) 1.05–2.14] or those with greater sleep disturbance (OR 1.29, 95 % CI 1.05–1.59), but only among men [17]. However, Suarez et al. [23] found that, among women, sleep problems (i.e., overall poor sleep quality and increased sleep latency) were associated with elevated CRP. It would have been optimal to provide more categories of the sleep parameters or to perform a sensitivity analysis to examine cut-point bias; the limited sample size made this difficult. However, this study still demonstrated numerous statistically significant relationships between sleep and inflammation. Also, we observed lower levels of adjusted CRP among those in the upper median of MVPA minutes compared to the lower median, providing further support for use of a median split for MVPA minutes. Lastly, causation is difficult to establish due to the cross-sectional nature of this study. It is possible that adverse effects of ART treatments or other factors associated with HIV could have influenced inflammation, which in turn affected sleep quality or ability to participate in physical activity [30].
Conclusion
Reducing inflammation is an important step in diminishing the risk and burden of chronic disease, as well as moderating the risk of comorbidities among those currently living with a chronic disease. Proper sleep maintenance and participation in regular physical activity may help to reduce the risk of inflammation, thereby, reducing the risk of several chronic diseases [3, 10, 29]. Future studies with larger populations are necessary to further elucidate the combined effects of sleep and physical activity on inflammation, as well as to incorporate other lifestyle factors, such as diet. Determining which combination of these lifestyle factors is most strongly associated with inflammation could aid health care providers and researchers in developing lifestyle intervention and treatment programs that would be most effective in reducing systemic inflammation levels. This is especially true among PLWH who suffer from numerous sleep complaints [34–36] and increased inflammation, even when effectively undergoing ART treatment [42]. Therefore, future treatment or intervention studies among PLWH should incorporate components for sleep improvement and participation in physical activity to investigate avenues to reduce inflammation or disease progression (e.g., viral load).
References
Breslau N, Roth T, Rosenthal L, Andreski P. Sleep disturbance and psychiatric disorders: a longitudinal epidemiological study of young adults. Biol Psychiatry. 1996;39(6):411–8.
Parish JM. Sleep-related problems in common medical conditions. Chest. 2009;135(2):563–72.
O’Connor MF, Irwin MR. Links between behavioral factors and inflammation. Clin Pharmacol Ther. 2010;87(4):479–82.
Gallicchio L, Kalesan B. Sleep duration and mortality: a systematic review and meta-analysis. J Sleep Res. 2009;18(2):148–58.
Keibel A, Singh V, Sharma MC. Inflammation, microenvironment, and the immune system in cancer progression. Curr Pharm Des. 2009;15(17):1949–55.
Libby P. Inflammatory mechanisms: the molecular basis of inflammation and disease. Nutr Rev. 2007;65(12 Pt 2):S140–6.
Ahmadi-Abhari S, Luben RN, Wareham NJ, Khaw KT. Seventeen year risk of all-cause and cause-specific mortality associated with C-reactive protein, fibrinogen and leukocyte count in men and women: the EPIC-Norfolk study. Eur J Epidemiol. 2013;28(7):541–50.
Vrints H, Shivalkar B, Hilde H, et al. Cardiovascular mechanisms and consequences of obstructive sleep apnoea. Acta Clin Belg. 2013;68(3):169–78.
Nadeem R, Molnar J, Madbouly EM, et al. Serum inflammatory markers in obstructive sleep apnea: a meta-analysis. J Clin Sleep Med. 2013;9(10):1003–12.
Solarz DE, Mullington JM, Meier-Ewert HK. Sleep, inflammation and cardiovascular disease. Front Biosci (Elite Ed). 2012;4:2490–501.
Chennaoui M, Sauvet F, Drogou C, et al. Effect of one night of sleep loss on changes in tumor necrosis factor alpha (TNF-alpha) levels in healthy men. Cytokine. 2011;56(2):318–24.
Pejovic S, Basta M, Vgontzas AN, et al. Effects of recovery sleep after one work week of mild sleep restriction on interleukin-6 and cortisol secretion and daytime sleepiness and performance. Am J Physiol Endocrinol Metab. 2013;305(7):E890–6.
Ferrie JE, Kivimaki M, Akbaraly TN, et al. Associations between change in sleep duration and inflammation: findings on C-reactive protein and interleukin 6 in the Whitehall II Study. Am J Epidemiol. 2013;178(6):956–61.
Grandner MA, Buxton OM, Jackson N, Sands-Lincoln M, Pandey A, Jean-Louis G. Extreme sleep durations and increased C-reactive protein: effects of sex and ethnoracial group. Sleep. 2013;36(5):769E–79E.
Wiener RC, Zhang R, Shankar A. Elevated serum C-reactive protein and markers of sleep disordered breathing. Int J Vasc Med. 2012;2012:914593.
Matthews KA, Zheng H, Kravitz HM, et al. Are inflammatory and coagulation biomarkers related to sleep characteristics in mid-life women?: study of women’s health across the nation sleep study. Sleep. 2010;33(12):1649–55.
Jackowska M, Kumari M, Steptoe A. Sleep and biomarkers in the english longitudinal study of ageing: associations with C-reactive protein, fibrinogen, dehydroepiandrosterone sulfate and hemoglobin. Psychoneuroendocrinology. 2013;38(9):1484–93.
Patel SR, Zhu X, Storfer-Isser A, et al. Sleep duration and biomarkers of inflammation. Sleep. 2009;32(2):200–4.
Prather AA, Epel ES, Cohen BE, Neylan TC, Whooley MA. Gender differences in the prospective associations of self-reported sleep quality with biomarkers of systemic inflammation and coagulation: findings from the heart and soul study. J Psychiatr Res. 2013;47(9):1228–35.
Main LC, Dawson B, Heel K, Grove JR, Landers GJ, Goodman C. Relationship between inflammatory cytokines and self-report measures of training overload. Res Sports Med. 2010;18(2):127–39.
Prather AA, Marsland AL, Hall M, Neumann SA, Muldoon MF, Manuck SB. Normative variation in self-reported sleep quality and sleep debt is associated with stimulated pro-inflammatory cytokine production. Biol Psychol. 2009;82(1):12–7.
Okun ML, Coussons-Read M, Hall M. Disturbed sleep is associated with increased C-reactive protein in young women. Brain Behav Immun. 2009;23(3):351–4.
Suarez EC. Self-reported symptoms of sleep disturbance and inflammation, coagulation, insulin resistance and psychosocial distress: evidence for gender disparity. Brain Behav Immun. 2008;22(6):960–8.
Liukkonen T, Rasanen P, Ruokonen A, et al. C-reactive protein levels and sleep disturbances: observations based on the Northern Finland 1966 Birth Cohort study. Psychosom Med. 2007;69(8):756–61.
Taheri S, Austin D, Lin L, Nieto FJ, Young T, Mignot E. Correlates of serum C-reactive protein (CRP)—no association with sleep duration or sleep disordered breathing. Sleep. 2007;30(8):991–6.
Fornadi K, Lindner A, Czira ME, et al. Lack of association between objectively assessed sleep disorders and inflammatory markers among kidney transplant recipients. Int Urol Nephrol. 2012;44(2):607–17.
Dowd JB, Goldman N, Weinstein M. Sleep duration, sleep quality, and biomarkers of inflammation in a Taiwanese population. Ann Epidemiol. 2011;21(11):799–806.
Miller MA, Kandala NB, Kivimaki M, et al. Gender differences in the cross-sectional relationships between sleep duration and markers of inflammation: Whitehall II study. Sleep. 2009;32(7):857–64.
Lopresti AL, Hood SD, Drummond PD. A review of lifestyle factors that contribute to important pathways associated with major depression: diet, sleep and exercise. J Affect Disord. 2013;148(1):12–27.
Santos RV, Tufik S, De Mello MT. Exercise, sleep and cytokines: is there a relation? Sleep Med Rev. 2007;11(3):231–9.
Youngstedt SD. Effects of exercise on sleep. Clin Sports Med. 2005;24(2):355–65 xi.
Youngstedt SD, Kline CE. Epidemiology of exercise and sleep. Sleep Biol Rhythm. 2006;4:215–21.
Zielinski MR, Davis JM, Fadel JR, Youngstedt SD. Influence of chronic moderate sleep restriction and exercise on inflammation and carcinogenesis in mice. Brain Behav Immun. 2012;26(4):672–9.
Robbins JL, Phillips KD, Dudgeon WD, Hand GA. Physiological and psychological correlates of sleep in HIV infection. Clin Nurs Res. 2004;13(1):33–52.
Gallego L, Barreiro P, del Rio R, et al. Analyzing sleep abnormalities in HIV-infected patients treated with Efavirenz. Clin Infect Dis. 2004;38(3):430–2.
Blanch J, Martinez E, Rousaud A, et al. Preliminary data of a prospective study on neuropsychiatric side effects after initiation of efavirenz. J Acquir Immune Defic Syndr. 2001;27(4):336–43.
Hand GA, Phillips KD, Dudgeon WD, William Lyerly G, Larry Durstine J, Burgess SE. Moderate intensity exercise training reverses functional aerobic impairment in HIV-infected individuals. AIDS Care. 2008;20(9):1066–74.
Bopp CM, Phillips KD, Fulk LJ, Hand GA. Clinical implications of therapeutic exercise in HIV/AIDS. J Assoc Nurs AIDS Care. 2003;14(1):73–8.
Yahiaoui A, McGough EL, Voss JG. Development of evidence-based exercise recommendations for older HIV-infected patients. J Assoc Nurs AIDS Care. 2012;23(3):204–19.
Hand GA, Lyerly GW, Jaggers JR, Dudgeon WD. Impact of aerobic and resistance exercise on the health of HIV-infected persons. Am J Lifestyle Med. 2009;3(6):489–99.
Deeks SG, Lewin SR, Havlir DV. The end of AIDS: HIV infection as a chronic disease. Lancet. 2013;382(9903):1525–33.
Brigham EP, Patil SP, Jacobson LP, et al. Association between systemic inflammation and obstructive sleep apnea in men with or at risk for HIV infection. Antivir Ther. 2014. doi:10.3851/IMP2745.
Appay V, Sauce D. Immune activation and inflammation in HIV-1 infection: causes and consequences. J Pathol. 2008;214(2):231–41.
Deeks SG. HIV infection, inflammation, immunosenescence, and aging. Annu Rev Med. 2011;62:141–55.
Hunt PW. HIV and inflammation: mechanisms and consequences. Curr HIV/AIDS Rep. 2012;9(2):139–47.
Jaggers JR, Dudgeon W, Blair SN, et al. A home-based exercise intervention to increase physical activity among people living with HIV: study design of a randomized clinical trial. BMC Public Health. 2013;13:502.
Welk GJ, McClain JJ, Eisenmann JC, Wickel EE. Field validation of the MTI Actigraph and BodyMedia armband monitor using the IDEEA monitor. Obesity (Silver Spring). 2007;15(4):918–28.
St-Onge M, Mignault D, Allison DB, Rabasa-Lhoret R. Evaluation of a portable device to measure daily energy expenditure in free-living adults. Am J Clin Nutr. 2007;85(3):742–9.
Peterson BT, Chiao P, Pickering E, et al. Comparison of actigraphy and polysomnography to assess effects of zolpidem in a clinical research unit. Sleep Med. 2012;13(4):419–24.
Soric M, Turkalj M, Kucic D, Marusic I, Plavec D, Misigoj-Durakovic M. Validation of a multi-sensor activity monitor for assessing sleep in children and adolescents. Sleep Med. 2013;14(2):201–5.
O’Driscoll DM, Turton AR, Copland JM, Strauss BJ, Hamilton GS. Energy expenditure in obstructive sleep apnea: validation of a multiple physiological sensor for determination of sleep and wake. Sleep Breath. 2013;17(1):139–46.
Sharif MM, Bahammam AS. Sleep estimation using BodyMedia’s sensewear armband in patients with obstructive sleep apnea. Ann Thorac Med. 2013;8(1):53–7.
Sallis JF, Grossman RM, Pinski RB, Patterson TL, Nader PR. The development of scales to measure social support for diet and exercise behaviors. Prev Med. 1987;16(6):825–36.
Marcus BH, Rakowski W, Rossi JS. Assessing motivational readiness and decision making for exercise. Health Psychol. 1992;11(4):257–61.
Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385–96.
Skinner HA, Sheu WJ. Reliability of alcohol use indices. The lifetime drinking history and the MAST. J Stud Alcohol. 1982;43(11):1157–70.
Marcus BH, Rossi JS, Selby VC, Niaura RS, Abrams DB. The stages and processes of exercise adoption and maintenance in a worksite sample. Health Psychol. 1992;11(6):386–95.
McHorney CA, Ware JE Jr, Lu JF, Sherbourne CD. The MOS 36-item Short-Form Health Survey (SF-36): III. Tests of data quality, scaling assumptions, and reliability across diverse patient groups. Med Care. 1994;32(1):40–66.
Trotti LM, Rye DB, De Staercke C, Hooper WC, Quyyumi A, Bliwise DL. Elevated C-reactive protein is associated with severe periodic leg movements of sleep in patients with restless legs syndrome. Brain Behav Immun. 2012;26(8):1239–43.
Zhang J, Lamers F, Hickie IB, He JP, Feig E, Merikangas KR. Differentiating nonrestorative sleep from nocturnal insomnia symptoms: demographic, clinical, inflammatory, and functional correlates. Sleep. 2013;36(5):671–9.
Kline CE, Zielinski MR, Devlin TM, Kripke DF, Bogan RK, Youngstedt SD. Self-reported long sleep in older adults is closely related to objective time in bed. Sleep Biol Rhythm. 2010;8(1):42–51.
Mullington JM, Simpson NS, Meier-Ewert HK, Haack M. Sleep loss and inflammation. Best Pract Res Clin Endocrinol Metab. 2010;24(5):775–84.
Youngstedt SD, Jean-Louis G, Bootzin RR, et al. Chronic moderate sleep restriction in older long sleepers and older average duration sleepers: a randomized controlled trial. Contemp Clin Trials. 2013;36(1):175–86.
Youngstedt SD, Kripke DF. Long sleep and mortality: rationale for sleep restriction. Sleep Med Rev. 2004;8(3):159–74.
Golombek DA, Casiraghi LP, Agostino PV, et al. The times they’re a-changing: effects of circadian desynchronization on physiology and disease. J Physiol Paris. 2013;107(4):310–22.
Besedovsky L, Lange T, Born J. Sleep and immune function. Pflugers Arch. 2012;463(1):121–37.
Ferrando S, Evans S, Goggin K, Sewell M, Fishman B, Rabkin J. Fatigue in HIV illness: relationship to depression, physical limitations, and disability. Psychosom Med. 1998;60(6):759–64.
Cruess DG, Antoni MH, Gonzalez J, et al. Sleep disturbance mediates the association between psychological distress and immune status among HIV-positive men and women on combination antiretroviral therapy. J Psychosom Res. 2003;54(3):185–9.
Bahammam AS, Alaseem AM, Alzakri AA, Sharif MM. The effects of Ramadan fasting on sleep patterns and daytime sleepiness: an objective assessment. J Res Med Sci. 2013;18(2):127–31.
Al Otair H, Al-Shamiri M, Bahobail M, Sharif MM, BaHammam AS. Assessment of sleep patterns, energy expenditure and circadian rhythms of skin temperature in patients with acute coronary syndrome. Med Sci Monit. 2011;17(7):CR397–403.
Pardo CA, McArthur JC, Griffin JW. HIV neuropathy: insights in the pathology of HIV peripheral nerve disease. J Peripher Nerv Syst. 2001;6(1):21–7.
Wulff EA, Wang AK, Simpson DM. HIV-associated peripheral neuropathy: epidemiology, pathophysiology and treatment. Drugs. 2000;59(6):1251–60.
Acknowledgments
We thank all participants who volunteered their time for this project. Drs. Jaggers, Dudgeon, and Hand were supported by an NIH/NINR Grant (1R21NRO11281). Drs. Hand and Blair are supported by unrestricted funding from The Coca-Cola Company. Dr. Hébert is supported by an Established Investigator Award in Cancer Prevention and Control from the Cancer Training Branch of the National Cancer Institute (K05 CA136975). Dr. Youngstedt is supported by an NIH Grant (R01HL095799).
Conflict of interest
The authors have no conflicts of interest to declare.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Wirth, M.D., Jaggers, J.R., Dudgeon, W.D. et al. Association of Markers of Inflammation with Sleep and Physical Activity Among People Living with HIV or AIDS. AIDS Behav 19, 1098–1107 (2015). https://doi.org/10.1007/s10461-014-0949-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-014-0949-y