Abstract
Purpose
In patients on dialysis, the results of studies examining the association between sleep disorders and inflammation are controversial. We assessed the association between inflammatory markers and different sleep disorders in a large sample of kidney transplant recipients.
Methods
Cross-sectional study of 100 randomly selected kidney transplant patients who underwent one-night polysomnography (“sleep disorders evaluation in patients after kidney transplantation study”) to diagnose obstructive sleep apnea (OSA) and periodic limb movements in sleep (PLMS). Athens Insomnia Scale (AIS) was utilized to assess the prevalence of insomnia. Sociodemographic information and data about medication, comorbidity and laboratory parameters were collected. Levels of inflammatory markers, such as C-reactive protein, serum albumin, white blood cell count, interleukin-6 (IL-6) and tumor necrosis factor-α (TNF-α), were measured.
Results
The mean age was 51 ± 13 years, 43% were women, and the prevalence of diabetes was 19%. We found no significant difference in the levels of inflammatory markers between patients with versus without OSA and PLMS. Apnea–hypopnea index showed a significant association with white blood cell count (ρ = 0.23), and weak (ρ < |0.15|), non-significant correlation with the other inflammatory markers. PLM index showed weak (ρ < |0.15|), non-significant correlation with all markers of inflammation. The serum IL-6 level was significantly higher in patients with insomnia (AIS ≥ 10) than in non-insomniacs [median (IQR): 3.2(2.6–5.1) vs. 1.7(1.2–2.9) ng/l; P = 0.009]. The levels of other inflammatory markers were similar between insomniacs and non-insomniacs.
Conclusions
We did not find any association between the presence of objectively assessed sleep disorders and inflammatory markers in kidney transplant patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sleep disorders such as obstructive sleep apnea (OSA), periodic limb movements in sleep (PLMS) and insomnia are common in patients with end-stage renal disease (ESRD) [1–9]. These sleep disorders have been shown to contribute to the increased risk of morbidity, mortality and graft failure in ESRD patients [10–12].
Several lines of evidence suggest that there is an activated inflammatory state in patients with sleep disorders. Partial and sustained sleep deprivation induced an elevation in the levels of pro-inflammatory markers such as C-reactive protein (CRP), interleukin-6 (IL-6) and tumor necrosis factor-α (TNF-α) in healthy subjects [13–16]. Shearer et al. [17] reported an increase in the soluble TNF-α receptor 1 and IL-6 levels in healthy men after 4 days of sustained sleep deprivation. These results suggest a role for sleep deprivation as a pro-inflammatory factor. Most studies examining sleep-disordered patients have found higher levels of pro-inflammatory mediators in patients with OSA, compared with age- and body mass index (BMI)-matched controls [18–20]. Yue et al. [21] reported a moderate positive correlation between the serum level of soluble TNF-α receptor 1 and periodic limb movement–associated arousals. A recent trial has shown an association between increased IL-6 concentration in elderly individuals suffering from insomnia [22].
Inflammation is an important predictor of mortality in patients on maintenance dialysis [23] and kidney transplant recipients [24, 25]. In ESRD patients, the results of studies examining the association of sleep disorders with inflammation are controversial; however, most of these studies found some association. Yang et al. [26] reported higher serum interleukin-18 level in peritoneal dialysis patients with poorer sleep quality. In the study by Erten et al. [27], ESRD patients with sleep-related complaints had a trend for higher level of IL-6 and TNF-α as compared to those without sleep problems, although this difference failed to reach statistical significance. Higher CRP level was associated with poorer sleep quality in stable hemodialysis patients, as reported by Chiu et al. [28]; however, in the same study, other inflammatory markers, such as IL-6, TNF-α, albumin, ferritin and interleukin-1β, were similar between bad and good sleepers. Other studies also confirm these negative results, as the authors did not find any significant association between sleep disorders and inflammation markers such as IL-6, TNF-α and albumin in ESRD patients [26, 27].
Although a number of studies have examined the relationship between inflammation and sleep disorders in ESRD patients, most of them were carried out among dialyzed patients and sample sizes were usually small. Many of the previous studies reported the measurement of only one inflammatory marker, and none of them used polysomnography, but used only questionnaires. There is a complete lack of information in this field from kidney transplant patients. Therefore, we designed this cross-sectional study to examine the association between inflammatory markers and different sleep disorders such as OSA, PLMS and insomnia in a large, randomly selected sample of kidney transplant patients, using polysomnography. Based on the previously presented results reported by us or by other research groups, we hypothesized that the above-mentioned sleep disorders were associated with inflammatory markers.
Subjects and methods
Sample of patients and data collection
For this study [“sleep disorders evaluation in patients after kidney transplantation (SLEPT) study”], potentially eligible patients were selected from all prevalent adult transplant patients (“total clinic population”; n = 1,214) who were regularly followed at a single outpatient transplant center on December 31, 2006. After applying exclusion criteria (transplant received within less than 3 months, active and acute respiratory disorder, acute infection, hospitalization within 1 month, surgery within 3 months), 1,198 patients remained (“base population”; n = 1,198). From this “base population,” we randomly selected and approached 150 patients (“Tx study sample”) using the simple random sampling strategy offered by SPSS 15.0 (Figure S1). The creation of cohort has been described previously [3, 24, 25, 29–32].
Demographic data and details of medical history were collected at enrollment when information about age, gender and etiology of chronic kidney disease (CKD), transplantation-related data including immune suppressant medication use and comorbidities including the modified Charlson Comorbidity Index (CCI) [33] were obtained. Estimated glomerular filtration rate (eGFR) was calculated using the “4-variable” modification of diet in renal disease (MDRD) study formula [34].
Laboratory data
Laboratory data were extracted from the charts and from the electronic laboratory database of the hospital. The following laboratory parameters were tabulated: white blood cell count, hemoglobin (Hb), serum C-reactive protein (CRP), albumin, creatinine and blood urea nitrogen (BUN). Serum samples were also collected at the time of the baseline assessment and stored at −70°C for future use. From these samples, high-sensitivity interleukin-6 (IL-6) and tumor necrosis factor-α (TNF-α) levels were measured using immunoassay kits based on solid-phase sandwich enzyme-linked immunosorbent assay (ELISA) (R&D Systems, Minneapolis, MN, USA).
Comorbidities
We used the modified Charlson Comorbidity Index (CCI) [33, 35], which is a weighted scoring system based on the presence or absence of each of 17 variables. Earlier it has been reported that the CCI was a predictor of survival in kidney transplant patients [33]. Since one of the variables is the presence of moderate to severe renal disease, the minimum score for all patients with ESRD is 2. Thus, in patients with ESRD, scores range from two to a possible maximum of 33.
Polysomnography
Standard, attended overnight polysomnography was performed in acoustically isolated and video-monitored sleep laboratory with four individual suits in our sleep laboratory (SOMNOscreen™ PSG Tele, SOMNOmedics GmBH, Germany, CE0494). Recordings were manually scored by two somnologists (MZSM, AL). Sleep stages were determined in 30-s epochs according to Rechtschaffen and Kales [36].
Definition and classification of obstructive sleep apnea
Apnea was defined as the absence of airflow for more than 10 s; hypopnea was defined as a clearly discernible reduction in airflow for more than 10 s associated with an arousal and/or reduction in oxygen saturation greater than 3% [37]. The apnea–hypopnea index (AHI) was defined as the number of apneas and hypopneas per hour of sleep. “Average oxygen saturation” was calculated from the oxygen saturation values measured during sleep. Patients were defined apneic if: mild: 5 ≤ AHI < 15; moderate: 15 ≤ AHI < 30 and severe: AHI ≥ 30 [37]. Similarly to previous publications [38, 39], the term “OSA” refers to moderate or severe apnea (AHI ≥ 15) in this paper.
Definition and classification of periodic limb movements in sleep
PLMS was defined by the following criteria: limb movement (LM) duration: 0.5–5 s; inter-movement interval: 5–90 s; and separation criteria for LMs occurring in both legs: more than 5 s between onsets. A PLMS cycle consisted of at least four consecutive LMs. The periodic limb movement index (PLMI) was defined as the number of LMs per hours during sleep. We defined PLMS if PLMI ≥ 15 [40].
Assessment of insomnia
The Athens Insomnia Scale (AIS) was used to assess sleep complaints and identify possible cases of insomnia [41, 42]. The AIS consists of eight items (score range, 0–24, with higher scores indicating worse sleep). The first 5 items cover night-time symptoms of insomnia (difficulty initiating sleep; difficulty maintaining sleep; early morning awakening), and 3 items probe daytime consequences of disturbed sleep (well-being, functioning capacity and daytime sleepiness). Subjects were asked to grade the severity of these complaints (absent, mild, severe, very severe) only if the particular complaint occurred at least three times per week during the last month. A cutoff score of 10 has been suggested for epidemiological studies, providing acceptable sensitivity and specificity to detect clinically significant insomnia [42]. The English version of the AIS had been previously translated and validated by our group. Internal consistency of the Hungarian version of the AIS was excellent and test–retest validation showed good overall reproducibility [43].
Transplantation- and donor-related data; immunosuppressive therapy
Transplantation-related information collected included current medications, transplant and dialysis “vintage” (i.e., time elapsed since transplantation or since the initiation of dialysis treatment), time spent on dialysis prior to transplantation, type of transplantation (deceased donor or living donor related), history of cumulative acute rejection, HLA mismatch, titer of pretransplant panel-reactive antibodies (PRA), cold ischemic time (CIT), age and gender of donor and history of delayed graft function. Time elapsed since the initiation of the first treatment for end-stage renal disease (ESRD) (cumulative ESRD time) was also calculated. Standard maintenance immunosuppressive therapy generally consisted of prednisolone, either cyclosporine A microemulsion formulation (CsA) or tacrolimus, combined with mycophenolate mofetil (MMF) or azathioprine, everolimus or sirolimus.
Ethical approval
The study was approved by the Ethics Committee of the Semmelweis University (4/2007). Before enrollment, patients received detailed verbal and written information about the aims and protocol of the study and signed an informed consent.
Statistical analysis
Statistical analyses were carried out using the STATA 11.1 software. Results are presented as percentage, mean ± (standard deviation, SD) or median (interquartile range, IQR). Continuous variables were compared using Student’s t test or the Mann–Whitney U test, and categorical variables were analyzed with chi-square test. Kruskal–Wallis test was used to analyze the relationship between continuous and categorical variables. Correlation analyses were performed using Spearman’s correlation. For multivariate analysis, logistic regressions were applied. Variables were included in the multivariate models based on theoretical considerations and also on the results of the bivariate analyses. Variance influence factors (VIF) were used to indicate colinearity between independent variables. In all statistics, two-sided test was used, and the results were considered statistically significant if P was less than 0.05.
As many of our results are negative, we had to make sure to avoid the type II error. Consequently, based on our clinical experience, we have defined the clinically minimally important difference in inflammatory markers: CRP at least 5 mg/l; IL-6 at least 1 ng/l; TNF-α at least 0.5 ng/l; serum albumin at least 1 g/l; and white blood cell count at least 1 × 103/l. We have performed sample size estimation to assess the number of patients needed to detect these minimally important differences (Table S1). All of these numbers are less than our sample size.
Results
Demographic data and baseline characteristics of the sample
Of the 150 eligible patients (“Tx study sample,” see methods), 50 individuals (33%) refused to participate. Consequently, the “final study population” included 100 Tx patients (participants) (Figure S1). There were no significant differences regarding age and gender between participants and those who refused to participate (not shown). The basic characteristics (age, gender, eGFR, hemoglobin, serum albumin) of the 100 participating Tx patients (“Tx study sample”) were similar to the characteristics of the “total clinic population” (not shown).
Table 1 shows the basic characteristics of the population. The mean age was 51 ± 13 years, 43% were women, and the prevalence of diabetes was 19%. The mean ± standard deviation (SD) or median (interquartile range (IQR)) of serum albumin and white blood cell count and the median and IQR of serum IL-6, serum CRP and TNF-α were 40.2 ± 3.4 g/l, 8.2 ± 2.4 × 103/l, 2.0 (1.2–3.2) ng/l, 3.5 (1.5–5.9) mg/l and 1.9 (1.4–2.7) ng/l, respectively. Eighty-five percent of the Tx patients were taking steroids, 43% were administered CsA, 71% were on MMF, 46% of the patients were administered tacrolimus, and 5% were on azathioprine. Only 1 and 12% of the patients took everolimus and sirolimus, respectively. Six percent of Tx patients had at least one previous transplantation.
Correlates of sleep apnea
Twenty-five percent of our patients had OSA. We found no significant difference in the levels of inflammatory markers between patients with versus without OSA (Table 2). The percentage of men was significantly higher in the OSA-positive group. Patients with OSA had significantly higher BMI and hemoglobin level. All other parameters were similar between the two groups. AHI showed a significant association with white blood cell count (ρ = 0.23), and weak (ρ < |0.15|), non-significant correlations with the other inflammatory markers (Table S2). In a sensitivity analysis, we have examined whether the gender has a modifying effect on our results. We found no association between inflammatory markers and OSA either in male or in female patients (not shown).
Correlates of periodic limb movements in sleep
Twenty-seven percent of our patients had PLMS. Patients with and without PLMS had similar values of all measured inflammatory markers (Table 3). The percentage of diabetic patients was significantly higher among patients with versus without PLMS. All other parameters were similar between the two groups. Additionally, PLM index showed weak (ρ < |0.15|), non-significant correlations with all markers of inflammation (Table S2). The association between inflammatory markers and PLMS was similar in men and women in a sensitivity analysis within gender strata (not shown).
Correlates of presence of insomnia
Sixteen percent of our patients suffered from insomnia symptoms. The serum IL-6 level was significantly higher in patients with insomnia (AIS ≥ 10 than in non-insomniacs [median (IQR): 3.2 (2.6–5.1) vs. 1.7 (1.2–2.9) ng/l; P = 0.009] (Table 4). The levels of other inflammatory markers were similar in the two groups. Insomniacs were older and had significantly higher CCI compared with patients without insomnia. The usage of the sleep pills was significantly higher in insomniacs than patients without insomnia. All other parameters were similar between the two groups. AIS showed a weak (ρ < |0.20|), non-significant correlation with all inflammatory markers (Table S2). Gender differences were examined, and IL-6 levels were higher [median (IQR): 4.3 (2.7–6.3) vs. 1.4 (1.0–2.4) ng/l; P = 0.02] and serum albumin levels (mean ± SD: 38.4 ± 3.1 vs. 40.8 ± 2.7 g/l; P = 0.03) were lower in women with insomnia versus without insomnia. Among men, we observed no such differences.
Logistic regression analysis
A logistic regression analysis was used to determine the associations between the presence of sleep disorders and inflammatory markers (Table 5a–c). The examined inflammatory markers were not associated with the presence of any of the three sleep disorders, neither in unadjusted nor in the fully adjusted binary logistic regression models.
Discussion
In this study, enrolling substantial number of kidney transplant patients, we found no association of inflammatory markers with obstructive sleep apnea, periodic limb movements in sleep and insomnia.
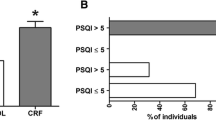
There is increasing evidence of elevated levels of inflammatory markers in different sleep disorders [18–22]. Similar association was found in ESRD patients [26–28, 44]. However, almost all of these studies used questionnaires instead of polysomnography [26–28, 44]. Erten et al. [27] examined nine hemodialysis patients with sleep complaints and another nine patients without sleep complaints. Patients with sleep complaints had higher IL-1β level; however, the IL-6 and TNF-α levels were similar between the two hemodialysis groups [27]. The study by Chiu et al. [28] disagrees with these results as they did not find any association between sleep quality and IL-1 β level in hemodialysis patients. Yang et al. [26] examined 57 peritoneal dialysis patients and reported higher IL-18 levels in “poor sleeper” patients versus “good sleepers” using the Pittsburgh Sleep Quality Index (PSQI). With the same questionnaire (PSQI), it was shown that serum CRP level was associated with “poor sleeper” status in hemodialysis patients [26, 44]. However, in these studies, other inflammatory markers such as ferritin, albumin, total iron-binding capacity, IL-6 and TNF-α were not associated with sleep quality [26, 28]. We found similar results in the case of IL-6, TNF-α and serum albumin. Contrary to a previous study, we did not find any difference in CRP levels in patients with and without sleep disorders. A potential explanation of this difference is that we used a gold standard method (polysomnography) to diagnose sleep disorders such as OSA and PLMS. All the other studies used the PSQI, a self-reported tool to measure general sleep disruption, which is not intended to give exact diagnosis. Another potential explanation of the difference is the dissimilarity of the examined cohorts. Kidney transplant patients have higher residual renal function compared with dialyzed patients, which might have an effect on the examined association. We are not aware of any study examining the relationship of inflammatory markers with specific sleep disorders in the CKD population.
Poor sleeper status was associated with depression [44], which, in turn, is associated with higher levels of inflammatory markers [45]. In our study, we have assessed the depressive symptoms in this study using the “center for epidemiologic studies-depression (CESD)” questionnaire. However, in this paper, we focus on the association between sleep disorders and inflammation using gold standard diagnostic method to give exact diagnosis. All the other above-mentioned studies used the Pittsburgh Sleep Quality Index (PSQI), a self-reported tool to measure general sleep disruption, which is not designed to give an exact diagnosis. The higher level of CRP in these studies might have been the consequence of underlying depression and its association with inflammation. We have previously reported association between inflammatory markers and symptoms of depression using CESD score in our original large cohort [45]. However, we did not find any association between inflammatory markers and specific sleep disorders such as OSA and PLMS in this study. In our opinion, the results of the subjective sleep questionnaires such as PSQI are confounded by depression, and the association between PSQI and inflammatory markers is a marker of the depression–inflammation association. Unfortunately, studies using PSQI have not adjusted for depression; therefore, the independent association of PSQI with inflammatory markers is questionable. As in our study, we did not find any association between sleep disorders and inflammatory markers; therefore, we found it unnecessary to adjust for depressive symptoms.
We found an association between IL-6 level and symptoms of insomnia. However, this association disappeared after adjusting for several co-variables in our multivariate model. This association presents in women, but not in men. This observation might be a consequence of higher prevalence of depression in women [46]; hence, depression is associated with higher levels of inflammatory markers [45]. The duration of sleep appears to be slightly longer in women than in men; therefore, the presence of insomnia might have a stronger impact on health system in women than in men.
There are several potential explanations why there is no association between markers of inflammation and sleep disorders in kidney transplant recipients. The usage of immunosuppressive medication could have influenced the association of inflammatory markers with sleep disorders. The higher residual renal function is another potential modifying factor in this association.
We diagnosed sleep disorders with polysomnography, and in this regard, this is one of the largest studies among transplant patients. We collected a number of important co-variables and adjusted for these to make our analysis more reliable. A main strength of our study is the measurement of five different inflammatory markers and three different sleep disorders.
Limitations of this report should also be noted. First, we only examined a panel of inflammatory markers based on a single blood sample drawn at enrollment. The lack of association of certain inflammatory markers with sleep disorders might reflect the difficulty in accurately assessing the status of inflammation in kidney transplant recipients by a single cytokine measurement. A better design that involves multiple testing would be more ideal especially for certain cytokines, such as IL-6, which exhibits a circadian rhythm [47]. Second, determining sample size was driven mainly by feasibility, and no formal sample size calculations had been done prior to the study. Post hoc power calculations suggest that the study had sufficient power to detect a minimally important difference in different inflammatory markers (Table S1). However, there is a possibility that our study is unable to detect smaller differences. Third, we used one questionnaire to assess symptoms of insomnia instead of clinical interview or multiple questionnaires.
Patients from a single center were enrolled; therefore, our results are not to be generalized without further considerations. All laboratory and cytokine measurements were carried out one time at baseline, representing the actual cytokine levels and laboratory values. Finally, one-third of the approached transplant patients refused to participate. It is important to emphasize that we did not find any difference between participants and non-participants regarding the basic sociodemographic characteristics; therefore, it is unlikely that this would distort our conclusions significantly. Refusal rate was similar in other studies using PSG in ESRD populations [8, 48]. We also acknowledge that a potential selection bias cannot be excluded, which is also inherent in all studies of sleep disorders based on polysomnography: motivated or symptomatic patients are more likely to undergo polysomnography, whereas “good sleepers” may opt to avoid a test like this. Finally, we did not perform adaptation night before the actual PSG assessment, which might have an impact on our results.
In summary, this is the first report presenting data from a large number of transplant patients to assess the association between inflammatory markers and different sleep disorders such as OSA, PLMS and insomnia. We did not find any association between the presence of sleep disorders and inflammatory markers.
References
Molnar MZ, Szentkiralyi A, Lindner A, Czira ME, Szabo A, Mucsi I, Novak M (2007) High prevalence of patients with a high risk for obstructive sleep apnoea syndrome after kidney transplantation—association with declining renal function. Nephrol Dial Transplant 22:2686–2692
Novak M, Molnar MZ, Ambrus C, Kovacs AZ, Koczy A, Remport A, Szeifert L, Szentkiralyi A, Shapiro CM, Kopp MS, Mucsi I (2006) Chronic insomnia in kidney transplant recipients. Am J Kidney Dis 47:655–665
Molnar MZ, Lazar AS, Lindner A, Fornadi K, Czira ME, Dunai A, Zoller R, Szentkiralyi A, Rosivall L, Shapiro CM, Novak M, Mucsi I (2010) Sleep apnea is associated with cardiovascular risk factors among kidney transplant patients. Clin J Am Soc Nephrol 5:125–132
Lindner A, Fornadi K, Lazar AS, Czira ME, Dunai A, Zoller R, Veber O, Szentkiralyi A, Kiss Z, Toronyi E, Mucsi I, Novak M, Molnar MZ (2011) Periodic limb movements in sleep are associated with stroke and cardiovascular risk factors in patients with renal failure. J Sleep Res. doi: 10.1111/j.1365-2869.2011.00956.x
Hanly PJ, Gabor JY, Chan C, Pierratos A (2003) Daytime sleepiness in patients with CRF: impact of nocturnal hemodialysis. Am J Kidney Dis 41:403–410
Jurado-Gamez B, Martin-Malo A, Alvarez-Lara MA, Munoz L, Cosano A, Aljama P (2007) Sleep disorders are under diagnosed in patients on maintenance hemodialysis. Nephron 105:c35–c42
Rijsman RM, de Weerd AW, Stam CJ, Kerkhof GA, Rosman JB (2004) Periodic limb movement disorder and restless legs syndrome in dialysis patients. Nephrology (Carlton) 9:353–361
Unruh ML, Sanders MH, Redline S, Piraino BM, Umans JG, Hammond TC, Sharief I, Punjabi NM, Newman AB (2006) Sleep apnea in patients on conventional thrice-weekly hemodialysis: comparison with matched controls from the Sleep Heart Health study. J Am Soc Nephrol 17:3503–3509
Merlino G, Piani A, Dolso P, Adorati M, Cancelli I, Valente M, Gigli GL (2006) Sleep disorders in patients with end-stage renal disease undergoing dialysis therapy. Nephrol Dial Transplant 21:184–190
Szentkiralyi A, Czira ME, Molnar MZ, Kovesdy CP, Remport A, Szeifert L, Vamos EP, Juhasz J, Turanyi CZ, Mucsi I, Novak M (2011) High risk of obstructive sleep apnea is a risk factor of death censored graft loss in kidney transplant recipients: an observational cohort study. Sleep Med 12:267–273
Benz RL, Pressman MR, Hovick ET, Peterson DD (2000) Potential novel predictors of mortality in end-stage renal disease patients with sleep disorders. Am J Kidney Dis 35:1052–1060
Jung HH, Lee JH, Baek HJ, Kim SJ, Lee JJ (2010) Nocturnal hypoxemia and periodic limb movement predict mortality in patients on maintenance hemodialysis. Clin J Am Soc Nephrol 5:1607–1613
Meier-Ewert HK, Ridker PM, Rifai N, Regan MM, Price NJ, Dinges DF, Mullington JM (2004) Effect of sleep loss on C-reactive protein, an inflammatory marker of cardiovascular risk. J Am Coll Cardiol 43:678–683
Vgontzas AN, Zoumakis E, Bixler EO, Lin HM, Follett H, Kales A, Chrousos GP (2004) Adverse effects of modest sleep restriction on sleepiness, performance, and inflammatory cytokines. J Clin Endocrinol Metab 89:2119–2126
Irwin MR, Wang M, Campomayor CO, Collado-Hidalgo A, Cole S (2006) Sleep deprivation and activation of morning levels of cellular and genomic markers of inflammation. Arch Intern Med 166:1756–1762
Haack M, Sanchez E, Mullington JM (2007) Elevated inflammatory markers in response to prolonged sleep restriction are associated with increased pain experience in healthy volunteers. Sleep 30:1145–1152
Shearer WT, Reuben JM, Mullington JM, Price NJ, Lee BN, Smith EO, Szuba MP, Van Dongen HP, Dinges DF (2001) Soluble TNF-alpha receptor 1 and IL-6 plasma levels in humans subjected to the sleep deprivation model of spaceflight. J Allergy Clin Immunol 107:165–170
Hatipoglu U, Rubinstein I (2003) Inflammation and obstructive sleep apnea syndrome pathogenesis: a working hypothesis. Respiration; international review of thoracic diseases 70:665–671
Yun AJ, Lee PY, Bazar KA (2004) Autonomic dysregulation as a basis of cardiovascular, endocrine, and inflammatory disturbances associated with obstructive sleep apnea and other conditions of chronic hypoxia, hypercapnia, and acidosis. Med Hypotheses 62:852–856
Harsch IA, Koebnick C, Wallaschofski H, Schahin SP, Hahn EG, Ficker JH, Lohmann T, Konturek PC (2004) Resistin levels in patients with obstructive sleep apnoea syndrome–the link to subclinical inflammation? Med Sci Monit 10:CR510–CR515
Yue HJ, Mills PJ, Ancoli-Israel S, Loredo JS, Ziegler MG, Dimsdale JE (2009) The roles of TNF-alpha and the soluble TNF receptor I on sleep architecture in OSA. Sleep Breath (Schlaf Atmung) 13:263–269
Okun ML, Reynolds CF 3rd, Buysse DJ, Monk TH, Mazumdar S, Begley A, Hall M (2011) Sleep variability, health-related practices, and inflammatory markers in a community dwelling sample of older adults. Psychosomatic Med 73:142–150
Rambod M, Bross R, Zitterkoph J, Benner D, Pithia J, Colman S, Kovesdy CP, Kopple JD, Kalantar-Zadeh K (2009) Association of malnutrition-inflammation score with quality of life and mortality in hemodialysis patients: a 5-year prospective cohort study. Am J Kidney Dis 53:298–309
Molnar MZ, Czira ME, Rudas A, Ujszaszi A, Lindner A, Fornadi K, Kiss I, Remport A, Novak M, Kennedy SH, Rosivall L, Kovesdy CP, Mucsi I (2011) Association of the malnutrition-inflammation score with clinical outcomes in kidney transplant recipients. Am J Kidney Dis 58(1):101–108
Molnar MZ, Keszei A, Czira ME, Rudas A, Ujszaszi A, Haromszeki B, Kosa JP, Lakatos P, Sarvary E, Beko G, Fornadi K, Kiss I, Remport A, Novak M, Kalantar-Zadeh K, Kovesdy CP, Mucsi I (2010) Evaluation of the malnutrition-inflammation score in kidney transplant recipients. Am J Kidney Dis 56:102–111
Yang JY, Huang JW, Chiang CK, Pan CC, Wu KD, Tsai TJ, Chen WY (2007) Higher plasma interleukin-18 levels associated with poor quality of sleep in peritoneal dialysis patients. Nephrol Dial Transplant 22:3606–3609
Erten Y, Kokturk O, Yuksel A, Elbeg S, Ciftci TU, Pasaoglu H, Ozkan S, Bali M, Arinsoi T, Sindel S (2005) Relationship between sleep complaints and proinflammatory cytokines in haemodialysis patients. Nephrology (Carlton) 10:330–335
Chiu YL, Chuang YF, Fang KC, Liu SK, Chen HY, Yang JY, Pai MF, Peng YS, Wu KD, Tsai TJ (2009) Higher systemic inflammation is associated with poorer sleep quality in stable haemodialysis patients. Nephrol Dial Transplant 24:247–251
Molnar MZ, Czira ME, Rudas A, Ujszaszi A, Haromszeki B, Kosa JP, Lakatos P, Beko G, Sarvary E, Varga M, Fornadi K, Novak M, Rosivall L, Kiss I, Remport A, Goldsmith DJ, Kovesdy CP, Mucsi I (2011) Association between the malnutrition-inflammation score and post-transplant anaemia. Nephrol Dial Transplant 26(6):2000–2006
Kovesdy CP, Czira ME, Rudas A, Ujszaszi A, Rosivall L, Novak M, Kalantar-Zadeh K, Molnar MZ, Mucsi I (2010) Body mass index, waist circumference and mortality in kidney transplant recipients. Am J Transplant 10:2644–2651
Kovesdy CP, Molnar MZ, Czira ME, Rudas A, Ujszaszi A, Rosivall L, Szathmari M, Covic A, Keszei A, Beko G, Lakatos P, Kosa J, Mucsi I (2010) Associations between serum leptin level and bone turnover in kidney transplant recipients. Clin J Am Soc Nephrol 5:2297–2304
Kovesdy CP, Mucsi I, Czira ME, Rudas A, Ujszaszi A, Rosivall L, Kim SJ, Wolf M, Molnar MZ (2011) Association of serum phosphorus level with anemia in kidney transplant recipients. Transplantation 91:875–882
Jassal SV, Schaubel DE, Fenton SS (2005) Baseline comorbidity in kidney transplant recipients: a comparison of comorbidity indices. Am J Kidney Dis 46:136–142
Levey A, Greene T, Kusek J, Beck G, Group MS (2000) A simplified equation to predict glomerular filtration rate from serum creatinine {Abstract}. J Am Soc Nephrol 11:155A
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40:373–383
Rechtschaffen A, Kales A (1968) A manual of standardized terminology, techniques and scoring system for sleep stages of human subjects. Brain Information Service/Brain Research Institute, University of California, Los Angeles
(1999) Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. The report of an American academy of sleep medicine task force. Sleep 22:667–689
Nakashima H, Katayama T, Takagi C, Amenomori K, Ishizaki M, Honda Y, Suzuki S (2006) Obstructive sleep apnoea inhibits the recovery of left ventricular function in patients with acute myocardial infarction. Eur Heart J 27:2317–2322
Hanly PJ, Pierratos A (2001) Improvement of sleep apnea in patients with chronic renal failure who undergo nocturnal hemodialysis. N Engl J Med 344:102–107
American Academy of Sleep Medicine (2005) International classification of sleep disorders, 2nd ed.: diagnostic and coding manual. American Academy of Sleep Medicine, Westchester
Soldatos CR, Dikeos DG, Paparrigopoulos TJ (2000) Athens Insomnia Scale: validation of an instrument based on ICD-10 criteria. J Psychosom Res 48:555–560
Soldatos CR, Dikeos DG, Paparrigopoulos TJ (2003) The diagnostic validity of the Athens Insomnia Scale. J Psychosom Res 55:263–267
Novak M, Mucsi I, Shapiro CM, Rethelyi J, Kopp MS (2004) Increased utilization of health services by insomniacs–an epidemiological perspective. J Psychosom Res 56:527–536
Bilgic A, Akgul A, Sezer S, Arat Z, Ozdemir FN, Haberal M (2007) Nutritional status and depression, sleep disorder, and quality of life in hemodialysis patients. J Ren Nutr 17:381–388
Czira ME, Lindner AV, Szeifert L, Molnar MZ, Fornadi K, Kelemen A, Laszlo G, Mucsi I, Keszei AP, Kennedy SH, Novak M (2011) Association between the malnutrition-inflammation score and depressive symptoms in kidney transplanted patients. Gen Hosp Psychiatry 33:157–165
Szeifert L, Molnar MZ, Ambrus C, Koczy AB, Kovacs AZ, Vamos EP, Keszei A, Mucsi I, Novak M (2010) Symptoms of depression in kidney transplant recipients: a cross-sectional study. Am J Kidney Dis 55:132–140
Sothern RB, Roitman-Johnson B, Kanabrocki EL, Yager JG, Fuerstenberg RK, Weatherbee JA, Young MR, Nemchausky BM, Scheving LE (1995) Circadian characteristics of interleukin-6 in blood and urine of clinically healthy men. In vivo (Athens, Greece) 9:331–339
Unruh ML, Sanders MH, Redline S, Piraino BM, Umans JG, Chami H, Budhiraja R, Punjabi NM, Buysse D, Newman AB (2008) Subjective and objective sleep quality in patients on conventional thrice-weekly hemodialysis: comparison with matched controls from the sleep heart health study. Am J Kidney Dis 52:305–313
Acknowledgments
The authors thank the patients and the staff in the Department of Transplantation and Surgery, Semmelweis University, Budapest. MZM received grants from the National Developmental Agency (KTIA-OTKA-EU 7KP-HUMAN-MB08-A-81231) from the Research and Technological Innovation Fund and was also supported by Hungarian Kidney Foundation. This study was supported by the Hungarian Kidney Foundation, Hungarian Society of Hypertension, Hungarian Society of Nephrology and the Foundation for Prevention in Medicine. This paper was also supported by the János Bolyai Research Scholarship of the Hungarian Academy of Sciences (Marta Novak and Miklos Zsolt Molnar). Katalin Fornadi is recipient of the Hungarian Eötvös Scholarship. The research of M. Novak has been supported by an unrestricted research grant from Canadian Home Healthcare Inc., and the Center for Integrative Mood Research, Toronto, Canada.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Fornadi, K., Lindner, A., Czira, M.E. et al. Lack of association between objectively assessed sleep disorders and inflammatory markers among kidney transplant recipients. Int Urol Nephrol 44, 607–617 (2012). https://doi.org/10.1007/s11255-011-0095-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-011-0095-7