Abstract
Lower-limb exoskeletons have the potential to improve mobility in individuals with movement disabilities, such as cerebral palsy (CP). The goal of this study was to assess the impact of plantar-flexor assistance from an untethered ankle exoskeleton on dynamic stability during unperturbed and perturbed walking in individuals with CP. Seven participants with CP (Gross Motor Function Classification System levels I-III, ages 6–31 years) completed a treadmill walking protocol under their normal walking condition and while wearing an ankle exoskeleton that provided adaptive plantar-flexor assistance. Pseudo-randomized treadmill perturbations were delivered during stance phase by accelerating one side of a split-belt treadmill. Treadmill perturbations resulted in a significant decrease in anteroposterior minimum margin-of-stability (− 32.1%, p < 0.001), and a significant increase in contralateral limb step length (8.1%, p = 0.005), integrated soleus activity during unassisted walking (23.4%, p = 0.02), and peak biological ankle moment (9.6%, p = 0.03) during stance phase. Plantar-flexor assistance did not significantly alter margin-of-stability, step length, soleus activity, or ankle moments during both unperturbed and perturbed walking. These results indicate that adaptive plantar-flexor assistance from an untethered ankle exoskeleton does not significantly alter dynamic stability maintenance during unperturbed and perturbed walking for individuals with CP, supporting future research in real-world environments.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cerebral palsy (CP) is a neurological disorder affecting one’s ability to move and maintain balance and posture.22 It is the most common cause of physical disability in children.5 CP can result in gait patterns that decrease walking efficiency and physical activity levels1,17,32 compared to typical development.15 Additionally, individuals with CP experience an elevated risk of falling, with 35% reporting daily falls and 30% reporting monthly or weekly falls.4 With a musculoskeletal system that is prone to low-energy fractures,26,35 falls pose a higher risk of injury for individuals with CP, which can exacerbate inactivity and subsequent declines in mobility. In addition, stability, activity levels, and overall mobility can worsen with age in CP, with many individuals requiring the use of a wheelchair or walker for ambulation later in life.3 Dynamic stability and fall risk, therefore, is an important therapeutic target for promoting increased physical activity and long-term functional mobility for individuals with CP.
There is evidence that children with CP walk with lower levels of dynamic stability versus their typically developing peers. One study18 found that children with CP require greater modulation of their stride characteristics (i.e., length and width) during overground walking relative to their typically developing peers to account for poorer dynamic gait stability. Two studies31,37 found that children with CP will take on a more conservative stepping strategy in the mediolateral plane during overground walking, hypothesizing this as a protective measure for the greater fall risk in this population. However, it was found that children with CP had no difference in their anteroposterior dynamic stability while walking overground compared to those without CP, meaning their stability in this direction was less conservative, putting them at a greater risk of falling.37 While no study has specifically evaluated dynamic stability during perturbed walking in CP, one can hypothesize that it would be affected based on the observed deficits in postural control and neuromuscular response to standing perturbations.40
Lower-limb exoskeletons have been developed to combat reduced mobility and augment muscle function.8,11,16,19,21,33,39 In individuals with CP, it has been demonstrated that untethered plantar-flexor assistance can improve over-ground and treadmill walking economy.10,20,21,29 However, before wearable exoskeletons can be confidently prescribed to augment mobility in free-living settings, it is important to understand the effect of these devices on walking stability and fall risk, particularly when used by individuals with neuromuscular impairments such as CP, given the aforementioned impairments in dynamic stability. Powered assistance may negatively influence stability, particularly assistance that does not adapt to de-stabilizing external perturbations (e.g., slips or bumps). Prior research has explored measures of stability in populations with physical disabilities who have a higher risk of falling,23,24,25,28,34,38 utilizing waist-belt perturbations, treadmill perturbations, moving platforms, and virtual reality “obstacles” to create dynamic perturbations. However, we are not aware of any study that has explored the impact of battery-powered ankle exoskeleton assistance on unperturbed and perturbed walking stability in individuals with CP or in any other patient population.
Working to improve our understanding of safety and the risk–benefit ratio of ankle exoskeleton assistance in real-world settings, the goal of this feasibility study was to determine the effects of ankle exoskeleton assistance on dynamic stability during unperturbed and perturbed walking in individuals with CP. We hypothesized that adaptive plantar-flexor assistance, which could instantaneously respond to user input, would not significantly alter dynamic stability maintenance during unperturbed and perturbed walking. Participants were subjected to pseudo-randomized treadmill accelerations under their normal walking condition and while wearing an exoskeleton that provided plantar-flexor assistance. We utilized an adaptive exoskeleton control scheme that provided assistance proportional to the biological moment in real-time,10 intended to maintain stability by accounting for variability in the demand on the ankle. The minimum anteroposterior and mediolateral margins-of-stability, representing the greatest instability across the gait cycle,13 were assessed as primary outcome measures. Step length, step width, peak and average biological ankle moment, and soleus muscle activity were assessed as secondary outcome measures.
Materials and Methods
Participants
We recruited participants for this study using the following inclusion criteria: diagnosis of spastic CP, ages five–35 years, Gross Motor Function Classification System (GMFCS) I–III, and the ability to walk with or without a walker on a treadmill for at least ten minutes. Exclusion criteria included orthopedic surgery within the past six months, or any condition that would preclude safe participation. Seven participants with CP were enrolled for participation (Table 1). The study was approved by the Northern Arizona University Institutional Review Board (#986744) and completed at the Northern Arizona University—Flagstaff Campus (Flagstaff, AZ). Informed written consent was provided by a parent or legal guardian for each participant after the nature and possible consequences of the study were explained; participants provided verbal assent. Consent of any identifiable images or videos was also provided.
Instrumentation
A licensed physical therapist conducted a physical assessment and a technician took lower-body measurements for exoskeleton fitting. Participants were outfitted with a full-body 54-marker set to track motion of the head, trunk, upper limbs, pelvis, and lower limbs. A ten-camera motion capture system was used to record kinematic data (120 Hz, Vicon; Denver, CO, USA). Ground reaction forces were collected using an in-ground instrumented treadmill (980 Hz, Bertec; Columbus, OH, USA). Wireless, surface electromyography (EMG) sensors (980 Hz, Delsys; Natick, MA, USA) were placed bilaterally on the soleus muscles. Torque and state data simultaneously collected from the exoskeleton (100 Hz) was synchronized with the motion capture data using a triggered signal.
Ankle Exoskeleton
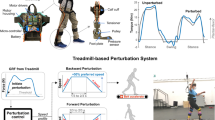
A previously validated, lower body exoskeleton was used to supply untethered ankle plantar-flexor assistance (Fig. 1).10 A detailed description on the design and files necessary for construction are reported in Ref. 20 In brief, the battery-powered exoskeleton consisted of a waist-mounted motor assembly that actuated pulleys on bilateral ankle assemblies via Bowden cable transmission (Fig. 1). Exoskeletons were customized to the participant’s height and leg length. A finite state machine informed by sensors embedded in the foot-plate insoles detected stance and swing phases of walking. During stance phase, the exoskeleton’s foot sensor measured the pressure between the fore-foot and the ground. Next, the real-time controller estimated the biological ankle moment through the regression equation reported in Ref. 10 Finally, a walking calibration procedure was completed so that torque was applied proportional to the biological ankle moment across the stance phase. The magnitude was set such that the controller provided 0.30 Nm/kg (nominally) of peak assistance during steady-state walking for all participants. This assistive torque setpoint was shown to maximize improvement in walking economy in a similar cohort of individuals with CP.29 The ankle exoskeleton controller was designed to automatically account for each participant’s gait pattern, stride-to-stride variability, and dynamic perturbations. The high-level control scheme was “closed-loop” in the sense that it instantaneously adapted to changes in pressure on the embedded fore-foot sensors, which, through calibration, reflect the instantaneous demand placed on the plantar-flexor muscles (Fig. 1); if a perturbation caused an increased in plantar-flexor activation, the control scheme responded by delivery an increase plantar-flexor torque, and vice versa.
Experimental setup. (a) Exoskeleton components worn by all participants during the assistance condition; (b) treadmill perturbation protocol, whereby participants outfitted with an exoskeleton device, reflective markers, and electromyography were subjected to 3 m/s2 accelerations for 25% increases in preferred speed, with random delivery of ‘Dummy’ perturbations to prevent anticipation; (c) adaptive control scheme, with assistive torque (blue dashed line) responding in real-time to user input.
Perturbation Control
We utilized treadmill perturbations, which allowed for an over-head harness system, to examine the effects of dynamic instabilities in a safe, controlled environment. Perturbation delivery was implemented every ten steps using remote control of a split-belt treadmill (Bertec). To compute the number of steps elapsed, gait transitions from a finite state machine were identified using force-sensitive resistors embedded in the shoe insoles. After ten gait cycles, a trigger signal was sent from the exoskeleton’s state machine via Bluetooth to activate a treadmill perturbation profile in MATLAB that induced a 25% increase or decrease in preferred speed by accelerating one side of the split-belt by 3 m/s2 during mid-stance phase of the selected limb (Fig. 1). “Dummy” perturbations inducing a 25% decrease of preferred speed (− 3 m/s2) were pseudo-randomized into the protocol to prevent anticipation of the fast (+ 25%) perturbations. The perturbations were applied to the limb that each participant indicated they would prefer to kick a ball with while standing (Supplementary Video 1). In developing the protocol, we found that an acceleration to 25% of the preferred speed was able produce a quantifiable destabilizing perturbation while minimizing the risk of a traumatic fall or injury, particularly for individuals with CP. We verified the magnitude and timing of the perturbation scheme by examining the stance-limb toe marker trajectory. We found perturbations were similar in magnitude (p = 0.37) and timing (p = 0.89) across the analyzed unassisted and assisted walking gait cycles (see Supplementary Material for further details).
Dynamic Stability Testing
Each participant’s preferred walking speed on the treadmill was determined by increasing and decreasing treadmill speed until a comfortable setting was reached. Participants were then outfitted with a full-bodyweight safety harness while they walked on the treadmill under the following two conditions in random order at their preferred speed: 1) Unassisted–shod walking (with ankle–foot orthoses if needed); and 2) Assisted–exoskeleton walking with plantar-flexor assistance. Participants walked under each condition until six perturbations were delivered per condition. We confirmed and analyzed the perturbations that were delivered during mid to late stance phase of the desired limb. A post-walking survey was conducted to determine if the participant preferred walking with or without exoskeleton assistance.
Data Analysis
Using OpenSim musculoskeletal modeling software (Stanford, CA,7), a generic musculoskeletal model was scaled to each participant using the marker trajectories from a standing calibration trial. Inverse kinematics and inverse dynamics analyses were used to calculate biological ankle moments. The anteroposterior and mediolateral margin-of-stability (MoS) was calculated as in Eq. (1) (13 modified for treadmill walking36):
where CoM is the position and VCoM is the velocity of the center of mass (CoM) in the transverse plane relative to the treadmill belt, which combine to make up the extrapolated CoM (xCoM). A participant’s vCoM was scaled to body size according to Ref. 12 where g is the gravitational constant 9.81 m/s2 and l is the pendulum length, defined as the instantaneous sagittal distance between the center of mass and ankle joint center. Finally, BoS is the position of the base of support boundary in the transverse plane. Please see Supplementary Fig. 1 for a diagram of these equation components. A positive margin-of-stability indicates a stable state and a negative value indicates an unstable state (Fig. 2).6,13 We chose to examine “margin-of-stability” as defined in Eq. (1), as it can be calculated across a gait cycle and results could be compared to existing dynamic stability analyses on individuals with CP.37
Perturbed gait cycles were identified and the minimum anteroposterior and mediolateral margin-of-stability were computed and averaged over the gait cycles before and during a perturbation, respectively. Please see Supplementary Fig. 2 for a diagram indicating before, during, and after perturbation gait cycle definitions, and Supplementary Fig. 3 for a representative participant’s (P1) time-series dataset of ankle angle and toe marker velocity data before, during, and after a perturbation. The minimum margin-of-stability represents the most unstable point during a dynamic activity, and typically occurs right before heel strike (Fig. 2). Step length, and step width data for the contralateral limb were computed and averaged over the cycles before and directly after a perturbation.
EMG data were band-pass filtered between 15 and 380 Hz, rectified, and low-pass filtered with a 7 Hz cutoff. The filtered signal was normalized to the average peak EMG observed during baseline walking. Final, average curves were calculated and resampled to percent of stance phase. The peak, normalized activity and work done by each muscle was then measured during the stance phase of the perturbed limb during each gait cycle before and during a perturbation. The work done by each muscle was calculated as the integrated EMG (iEMG) normalized to the average iEMG during baseline walking. As a supplementary analysis, the exoskeleton controller accuracy was measured during perturbed walking (see Supplementary Material for further details).
Statistical Analysis
For each participant, outcome measures were averaged across perturbed and unperturbed gait cycles for each condition. Mean minimum anteroposterior margin-of-stability (margin-of-stabilityAP), mean minimum mediolateral margin-of-stability (margin-of-stabilityML), mean step length (SL), mean step width (SW), peak stance phase soleus EMG, and stance phase soleus iEMG during perturbed and unperturbed walking were compared during both unassisted and ankle-assisted conditions. Main effects of, and interaction between, treadmill condition (unperturbed or perturbed) and assistance condition (unassisted or assisted) were investigated using repeated measures two-way Analysis of Variance (ANOVA) with participant-level replicates. Post-hoc paired t tests were used to determine significant differences if a significant main effect or interaction was found. Significance was defined as α < 0.05 and p values were adjusted using Bonferroni correction to p < 0.025 for multiple comparisons of the two simple main effects if a significant interaction was found. Normality was assessed using a Kolmogorov–Smirnov test with a Lilliefors correction for small sample sizes. Non-normal distributions were manually assessed using Wilcoxon signed rank tests; only unassisted-unperturbed and unassisted-perturbed peak soleus EMG and assisted-perturbed soleus iEMG had non-normal distributions. Statistical analyses were conducted using SPSS software version 27. The adaptive performance of the exoskeleton controller was determined by calculating the correlation coefficient between the measured torque and the biological ankle moment during unperturbed and perturbed walking.
Results
All participants successfully completed the perturbation protocol without falling under all of the conditions. The exoskeleton control scheme provided adaptive assistance that was highly correlated to the biological ankle moment (r = 0.91 for both unperturbed and perturbed walking (additional details in Supplementary Material). Six of the seven participants preferred walking with assistance during the perturbation protocol (Table 1).
There was a significant main effect of treadmill condition (unperturbed or perturbed) on minimum margin-of-stabilityAP (p < 0.001, Fig. 3a, see Supplementary Fig. 4 for individual profiles). Pairwise comparisons revealed a 32.1% decrease in stability during perturbed walking compared to unperturbed walking (unperturbed minimum margin-of-stabilityAp = − 21.7% body height (%BH), perturbation minimum margin-of-stabilityAp = − 28.7%BH). No difference in minimum margin-of-stabilityAP due to assistance was found (p = 0.344). Minimum margin-of-stabilityML was similar across walking (p > 0.5) and assistance (p > 0.5) conditions (Fig. 3b). There was a significant main effect of treadmill condition on contralateral limb step length (p = 0.005, Fig. 4a). Pairwise comparisons showed an 8.11% increase in contralateral limb step length (unperturbed step length = 52.5% leg length, perturbed step length = 56.7% leg length), suggesting participants took longer steps to recover from the perturbation. Step length was unchanged due to exoskeleton assistance (p = 0.36). No difference in contralateral limb step width due to walking or assistance conditions was observed (p > 0.5 for both, Fig. 4b).
A significant interaction for peak soleus activity between treadmill and assistance conditions was found (p = 0.007). A significant simple effect of treadmill condition during the unassisted condition was found (p = 0.015), with peak soleus EMG increasing 42.1% during perturbations (Fig. 5a; see Supplementary Fig. 5 for individual soleus activation profiles). There was a significant interaction for soleus iEMG between treadmill and assistance conditions (p = 0.017). A significant simple effect of treadmill condition during the unassisted condition was found (p = 0.017), with soleus iEMG increasing 23.4% during perturbations (Fig. 5b). No other simple effects were significantly different. A significant main effect was found for peak biological ankle moment during stance phase (p = 0.036), resulting in 9.6% higher peaks during perturbations (Fig. 6a). No significant interactions or main effects of treadmill (p = 0.159) or assistance (p = 0.181) conditions were found regarding average biological ankle moment during stance phase (Fig. 6b; see Supplementary Fig. 6 for individual ankle moment profiles).
Plantar flexor muscle activity. (a) Peak and (b) average stance phase soleus activity during unperturbed and perturbated walking, with (blue) and without (gray) plantar flexion assistance; bracket indicates significant simple effect of perturbation on the unassisted condition, error bars indicate standard error of the mean.
Discussion
The primary goal of this study was to examine the effect of providing adaptive plantar-flexor assistance on dynamic stability maintenance during unperturbed and perturbed walking in CP. Prior studies have examined the effect of waist-belt, treadmill, and visual perturbations on dynamic stability, but we are not aware of any that have investigated the effects of powered assistive devices on either unperturbed or perturbed walking stability.14,23,24,25,28,34,38 Our findings confirm our hypothesis that an ankle exoskeleton device providing adaptive plantar-flexor assistance would not significantly alter dynamic stability during unperturbed and perturbed walking. To fulfill the purpose of the study, we developed and evaluated the novel protocol that delivers perturbations during walking at a magnitude capable of safely, but significantly altering dynamic stability for individuals with CP; the prescribed perturbations resulted in statistically significant changes in anteroposterior stability, but resulted in no falls or injuries for our participants with CP who were GMFCS levels I–III. Our protocol may be utilized in future studies interested in investigating dynamic stability during walking with perturbations for this population, both with and without assistive exoskeletons.
During walking, the least stable moment in anteroposterior direction across the gait cycle occurs right before heel strike and is considered a crucial moment in gait stability.27 We observed a significant change in anteroposterior dynamic stability during the treadmill perturbation condition, indicating a significant departure from unperturbed walking. During the perturbed treadmill condition, however, no difference was observed between unassisted and assisted conditions, suggesting that the plantar-flexor assistance appropriately adapted to the perturbations and did not impair stability (Fig. 3a, Supplemental Table 1). This finding provides confidence in the safety of adaptive ankle exoskeleton assistance to accommodate destabilizing situations, like unexpected changes in terrain or surface, and suggests that walking with adaptive exoskeleton assistance may not exacerbate fall risk, which is essential for patient populations like CP that are prone to an elevated risk of falling and low-energy fractures.4,26,35
We investigated step length and step width of the contralateral limb to further evaluate the effects of adaptive plantar-flexor assistance on stability and recovery from a perturbation. Our results indicated that participants took a significantly longer step directly after experiencing the treadmill perturbation (Fig. 4a), which was an expected recovery method associated with the reduction in the anteroposterior stability (Fig. 3a). Conversely, no differences in step width due to perturbations or ankle assistance were observed, which was expected because the perturbations were only delivered in the anteroposterior direction (Fig. 4b). Step length and step width were unchanged during walking with vs. without adaptive plantar-flexor assistance. This was an important finding in regards to fall risk, because step length after a perturbation is a significant indicator of recovery success, with shorter steps associated with failed responses (i.e., a fall).30
We observed a significant increase in peak soleus EMG and average soleus iEMG during the perturbed limb stance phase during unassisted walking (Fig. 5a and 5b), indicating increased recruitment and work by the plantar-flexor muscles relative to unperturbed walking. Increased recruitment of the soleus muscle following a perturbation likely contributed to the observed increase in peak biological ankle moment during stance phase (Fig. 6a). We did not find an increase in soleus iEMG during assisted perturbed walking relative to assisted unperturbed walking, suggesting that the adaptive assistance may have mitigated the need for increased soleus recruitment as during unassisted walking. The observed relationships between perturbations, soleus muscle activity, and ankle moment yield potential for longer-term perturbation training to examine existing trends seen in this preliminary study. There is broad clinical consensus that plantar-flexor dysfunction is a primary contributor to slow, inefficient, and crouched walking patterns in CP.2 Perturbed walking protocols that can increase plantar-flexor activation functionally during walking may hold potential as a rehabilitation tool to target selective control of this important muscle group.
Individuals must perceive a benefit from assistive devices like lower-limb exoskeletons for their successful adoption in free-living settings, which motivated our user experience survey. Six out of the seven participants expressed a preference for adaptive plantar-flexor assistance over shod walking. Patients perceived a “noticeable difference” between unassisted and ankle-assistance during perturbed walking. Specifically, one participant claimed walking “felt easier” with ankle-assistance. Multiple participants described the feeling of ankle-assistance as “helping” propel them during a perturbation, perceiving higher stability while wearing the exoskeleton with assistance. This perceived increase in stability suggests the device’s control strategy noticeably adapted to perturbations to the satisfaction of the user, despite no quantifiable differences in minimum margin-of-stability between unassisted and assisted conditions.
It is important to note that this study had several limitations that should be considered. First, the sample size for this study is relatively small for a patient population that is highly heterogenous, with only one individual at a functional level of GMFCS level III. The heterogeneity of our cohort should be carefully considered when interpreting or generalizing the results. Still, this study serves as an important, preliminary assessment of the impact of untethered ankle exoskeleton assistance on walking stability, and provides details on a walking perturbation protocol that was feasible for all of our participants. Second, the calf cuff of the exoskeleton device prevented recording activity of the gastrocnemii. While it is possible that the gastrocnemius would respond differently than the soleus to a perturbation, and should be explored in future iterations of this protocol, both muscles generally serve to plantar-flex the ankle during walking. A previously untested level of perturbation (25% speed increase) was used to induce a dynamically unstable state for our participants, and was successful in doing so. It is possible, however, that perturbation profiles with larger magnitudes would yield results that differ from our findings here, and should be tested in future investigations. Finally, only one level of nominal ankle assistance was assessed (0.3 Nm/kg). This level was chosen because it resulted in the maximum decrease in metabolic cost of transport for a similar cohort of participants, but it is possible that a different level would be more beneficial for perturbation recovery, which should be explored in future investigations.
To the best of our knowledge, this study is one of the first to evaluate how a lower-limb exoskeleton affects stability during unperturbed and perturbed walking for participants with a neurological disease. Our results suggest that adaptive plantar-flexor assistance from an untethered ankle exoskeleton does not decrease dynamic stability during unperturbed and perturbed walking in individuals with CP. Additionally, the reported treadmill perturbation protocol may be useful for future studies exploring the effects of lower-body exoskeletons on dynamic stability, spatiotemporal gait parameters, and neuromuscular response during perturbed walking across a range of neurological disorders. Our findings contribute to the growing body of evidence in support of future research on the use of ankle exoskeleton assistance for use in free-living settings.
Abbreviations
- CP:
-
Cerebral palsy
- GMFCS:
-
Gross Motor Function Classification System
- EMG:
-
Electromyography
- MoS:
-
Margin-of-stability
- AP:
-
Anteroposterior
- ML:
-
Mediolateral
- CoM:
-
Center of mass
- BoS:
-
Base of support
- g :
-
Gravity
- l :
-
Pendulum length
- iEMG:
-
Integrated EMG
- SL:
-
Step length
- SW:
-
Step width
- ANOVA:
-
Analysis of variance
References
Armand, S., G. Decoulon, and A. Bonnefoy-Mazure. Gait analysis in children with cerebral palsy. EFORT Open Rev. 1:448–460, 2016.
Arnold, A. S., F. C. Anderson, M. G. Pandy, and S. L. Delp. Muscular contributions to hip and knee extension during the single limb stance phase of normal gait: a framework for investigating the causes of crouch gait. J. Biomech. 38:2181–2189, 2005.
Bjornson, K. F., B. Belza, D. Kartin, R. Logsdon, and J. F. McLaughlin. Ambulatory physical activity performance in youth with cerebral palsy and youth who are developing typically. Phys. Ther. 87(3):248–257, 2007.
Boyer, E. R., and A. Patterson. Gait pathology subtypes are not associated with self-reported fall frequency in children with cerebral palsy. Gait Posture 63:189–194, 2018.
Boyle, C. A., S. Boulet, L. A. Schieve, R. A. Cohen, S. J. Blumberg, M. Yeargin-Allsopp, S. Visser, and M. D. Kogan. Trends in the prevalence of developmental disabilities in US children, 1997-2008. Pediatrics 127:1034–1042, 2011.
Bruijn, S. M., O. G. Meijer, P. J. Beek, and J. H. Van Dieen. Assessing the stability of human locomotion: a review of current measures. J. R. Soc. Interface 10(83):20120999, 2013.
Delp, S. L., F. C. Anderson, A. S. Arnold, P. Loan, A. Habib, C. T. John, E. Guendelman, and D. G. Thelen. OpenSim: open-source software to create and analyze dynamic simulations of movement. IEEE Trans. Biomed. Eng. 54:1940–1950, 2007.
Esquenazi, A., M. Talaty, A. Packel, and M. Saulino. The ReWalk powered exoskeleton to restore ambulatory function to individuals with thoracic-level motor-complete spinal cord injury. Am. J. Phys. Med. Rehabil. 91:911–921, 2012.
Gage, J. R., M. H. Schwartz, S. E. Koop, and T. F. Novacheck. The Identification and Treatment of Gait Problems in Cerebral Palsy. London: Mac Keith Press, 2009.
Gasparri, G. M., J. Luque, and Z. F. Lerner. Proportional joint-moment control for instantaneously adaptive ankle exoskeleton assistance. IEEE Trans. Neural Syst. Rehabil. Eng. 27:751–759, 2019.
Griffin, R., T. Cobb, T. Craig, M. Daniel, N. van Dijk, J. Gines, K. Kramer, S. Shah, O. Siebinga, J. Smith, and P. Neuhaus. Stepping forward with exoskeletons: team IHMC?s design and approach in the 2016 cybathlon. IEEE Robot. Autom. Mag. 24:66–74, 2017.
Hof, A. L. Scaling gait data to body size. Gait Posture 4:222–223, 1996.
Hof, A. L., M. G. J. Gazendam, and W. E. Sinke. The condition for dynamic stability. J. Biomech. 2005. https://doi.org/10.1016/j.jbiomech.2004.03.025.
Ilmane, N., S. Croteau, and C. Duclos. Quantifying dynamic and postural balance difficulty during gait perturbations using stabilizing/destabilizing forces. J. Biomech. 48:441–448, 2015.
Johnson, D. L., F. Miller, P. Subramanian, and C. M. Modlesky. Adipose tissue infiltration of skeletal muscle in children with cerebral palsy. J. Pediatr. 154:715–720, 2009.
Kang, J., D. Martelli, V. Vashista, I. Martinez-Hernandez, H. Kim, and S. K. Agrawal. Robot-driven downward pelvic pull to improve crouch gait in children with cerebral palsy. Sci. Robot. 2:eaan2634, 2017.
Kerr, C., J. Parkes, M. Stevenson, A. P. Cosgrove, and B. C. Mcdowell. Energy efficiency in gait, activity, participation, and health status in children with cerebral palsy. Dev. Med. Child Neurol. 50:204–210, 2008.
Kurz, M. J., D. J. Arpin, and B. Corr. Differences in the dynamic gait stability of children with cerebral palsy and typically developing children. Gait Posture 36:600–604, 2012.
Lee, S., J. Kim, L. Baker, A. Long, N. Karavas, N. Menard, I. Galiana, and C. J. Walsh. Autonomous multi-joint soft exosuit with augmentation-power-based control parameter tuning reduces energy cost of loaded walking. J. Neuroeng. Rehabil. 15:66, 2018.
Lerner, Z. F., G. M. Gasparri, M. O. Bair, J. L. Lawson, J. Luque, T. A. Harvey, and A. T. Lerner. An untethered ankle exoskeleton improves walking economy in a pilot study of individuals with cerebral palsy. IEEE Trans. Neural Syst. Rehabil. Eng. 26:1985–1993, 2018.
Lerner, Z. F., T. A. Harvey, and J. L. Lawson. A battery-powered ankle exoskeleton improves gait mechanics in a feasibility study of individuals with cerebral palsy. Ann. Biomed. Eng. 2019. https://doi.org/10.1007/s10439-019-02237-w.
Liao, H.-F., and A.-W. Hwang. Relations of balance function and gross motor ability for children with cerebral palsy. Percept. Mot. Skills 96:1173–1184, 2003.
Martelli, D., J. Kang, and S. K. Agrawal. A perturbation-based gait training with multidirectional waist-pulls generalizes to split-belt treadmill slips. In: IEEE/RAS-EMBS International Conference on Biomedical Robotics and Biomechatronics (BioRob), 2018.
Martelli, D., L. Luo, J. Kang, U. J. Kang, S. Fahn, and S. K. Agrawal. Adaptation of stability during perturbed walking in Parkinson’s disease. Sci. Rep. 7:1–11, 2017.
McAndrew Young, P. M., J. M. Wilken, and J. B. Dingwell. Dynamic margins of stability during human walking in destabilizing environments. J. Biomech. 45:1053–1059, 2012.
Modlesky, C. M., S. A. Kanoff, D. L. Johnson, P. Subramanian, and F. Miller. Evaluation of the femoral midshaft in children with cerebral palsy using magnetic resonance imaging. Osteoporos. Int. 20:609–615, 2009.
Ohtsu, H., S. Yoshida, T. Minamisawa, T. Takahashi, S. Yomogida, and H. Kanzaki. Investigation of balance strategy over gait cycle based on margin of stability. J. Biomech. 95:2019.
Okubo, Y., M. A. Brodie, D. L. Sturnieks, C. Hicks, H. Carter, B. Toson, and S. R. Lord. Exposure to trips and slips with increasing unpredictability while walking can improve balance recovery responses with minimum predictive gait alterations. PLoS ONE 13:2018.
Orekhov, G., Y. Fang, J. Luque, and Z. F. Lerner. Ankle exoskeleton assistance can improve over-ground walking economy in individuals with cerebral palsy. IEEE Trans. Neural Syst. Rehabil. Eng. 28:461–467, 2020.
Owings, T. M., M. J. Pavol, and M. D. Grabiner. Mechanisms of failed recovery following postural perturbations on a motorized treadmill mimic those associated with an actual forward trip. Clin. Biomech. 16:813–819, 2001.
Rethwilm, R., H. Böhm, M. Haase, D. Perchthaler, C. U. Dussa, and P. Federolf. Dynamic stability in cerebral palsy during walking and running: predictors and regulation strategies. Gait Posture 84:329–334, 2021.
Rose, J., J. G. Gamble, A. Burgos, J. Medeiros, and W. L. Haskell. Energy expenditure index of walking for normal children and for children with cerebral palsy. Dev. Med. Child Neurol. 32:333–340, 1990.
Sawicki, G. S., and D. P. Ferris. Mechanics and energetics of level walking with powered ankle exoskeletons. J. Exp. Biol. 211:1402–1413, 2008.
Sessoms, P. H., M. Wyatt, M. Grabiner, J. D. Collins, T. Kingsbury, N. Thesing, and K. Kaufman. Method for evoking a trip-like response using a treadmill-based perturbation during locomotion. J. Biomech. 47:277–280, 2014.
Stevenson, R. D., M. Conaway, J. W. Barrington, S. L. Cuthill, G. Worley, and R. C. Henderson. Fracture rate in children with cerebral palsy. Pediatr. Rehabil. 9:396–403, 2006.
Süptitz, F., K. Karamanidis, M. M. Catalá, and G. P. Brüggemann. Symmetry and reproducibility of the components of dynamic stability in young adults at different walking velocities on the treadmill. J. Electromyogr. Kinesiol. 22:301–307, 2012.
Tracy, J. B., D. A. Petersen, J. Pigman, B. C. Conner, H. G. Wright, C. M. Modlesky, F. Miller, C. L. Johnson, and J. R. Crenshaw. Dynamic stability during walking in children with and without cerebral palsy. Gait Posture 72:182–187, 2019.
Van Dijsseldonk, R. B., L. A. F. De Jong, B. E. Groen, M. V. Van Der Hulst, A. C. H. Geurts, and N. L. W. Keijsers. Gait stability training in a virtual environment improves gait and dynamic balance capacity in incomplete spinal cord injury patients. Front. Neurol. 9:1–12, 2018.
Vouga, T., R. Baud, J. Fasola, M. Bouri, and H. Bleuler. TWIICE—a lightweight lower-limb exoskeleton for complete paraplegics. In: The IEEE International Conference on Rehabilitation Robotics, vol. 1000, pp. 1639–1645, 2017. https://doi.org/10.1109/icorr.2017.8009483.
Woollacott, M. H., and A. Shumway-Cook. Postural dysfunction during standing and walking in children with cerebral palsy: what are the underlying problems and what new therapies might improve balance? Neural Plasticity 12:211–219, 2005.
Acknowledgments
This research was supported in part by the Eunice Kennedy Shriver National Institute of Child Health & Human Development of the National Institutes of Health under Award Number R15HD099664. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. This work was also supported in part by the University of Arizona College of Medicine – Phoenix MD/PhD Program. The authors would like to thank James Babers and Leah Liebelt for their assistance with device manufacturing. The authors would also like to thank the participants and their families for their involvement in the study.
Competing interest
ZFL is a named inventor on pending utility patent applications that describe the exoskeleton utilized in the study. ZFL is a co-founder of a company seeking to commercialize the device. The other authors declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Associate Editor Stefan M Duma oversaw the review of this article.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Video 1 Representative perturbations during unassisted and assisted conditions (MP4 8606 kb)
Rights and permissions
About this article
Cite this article
Harvey, T.A., Conner, B.C. & Lerner, Z.F. Does Ankle Exoskeleton Assistance Impair Stability During Walking in Individuals with Cerebral Palsy?. Ann Biomed Eng 49, 2522–2532 (2021). https://doi.org/10.1007/s10439-021-02822-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10439-021-02822-y