Abstract
Objective
To evaluate outcome of laparoscopic subtotal hysterectomy (LASH) performed in women with large uteri using a modified five port technique.
Design
Prospective Cohort Study (Canadian Task Force classification III).
Setting
Advanced laparoscopic Unit at the Whipps Cross University Hospital, London, UK.
Inclusion criteria
(1) All women with symptomatic and large uteri undergoing LASH, (2) previous three normal cervical smears and consent for future smears as protocol, (3) patient consent for the procedure.
Methods
Prospectively collected database was analysed statistically for 29 women with enlarged uteri weighing more than 300 g who underwent LASH using the modified five port technique, during the time period of 24 months from Jan 2007 to Jan 2009. This technique demonstrates that the port placement facilitates the procedure.
Results
The mean age of the patients was 47 ± 4 years. Median BMI was 29 (range 22–41), Most common indication of surgery was menorrhagia in 90% of cases followed by palpable lump in 67% of cases. Median size of uterus was 18 weeks (range 12–30). Mean operative time was 84 ± 42 min. Median blood loss was 200 ml (range 100–800 ml).There was only one case with major complication such as bladder injury which was diagnosed and repaired intraoperatively. Mean hospital stay was 2 ± 1 day. None of the cases needed conversion to laparotomy.
Conclusion
Modified five port technique of LASH for large uteri provides optimal exposure of the operative field to increase the efficiency and ease of the procedure and has its added cosmetic benefits.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Laparoscopic subtotal hysterectomy (LASH) was developed during the 1990s [1, 2]. It is a minimally invasive procedure that is quick, results in reduced operating time, blood loss and quicker return to normal activity. This makes it a popular choice amongst women requiring hysterectomy for benign conditions [3, 4]. Most studies set uterine size of 16 weeks gestation as the upper limit, as larger uteri allow for limited access and exposure to the engorged vascular pedicles due to anatomic distortion resulting in a potentially prolonged operating time and a higher complication rate. To overcome these limitations we introduced this modified five port technique for LASH.
Objective
To evaluate short-term outcome of LASH performed in women with large uteri using a modified five port technique.
Materials and methods
It is a prospective cohort study of 29 women with enlarged uteri weighing more than 300 g who underwent LASH for benign gynaecological conditions using a modified five port technique during the time period of 24 months from Jan 2007 to Jan 2009. All cases were performed at the advanced laparoscopy unit at the Whipps Cross University Hospital, London, UK. Inclusion criteria were benign uterine disorders with a uterine size of 12 weeks gestation or more, patient’s consent for the procedure and previous three normal cervical smears and willingness to continue on the cervical screening programme. Women with malignancy or pelvic floor prolapse were excluded.
All patients underwent pre-operative clinical evaluation of uterine size and mobility, pelvic ultrasonography and when indicated endometrial sampling with or without hysteroscopy.
Operative technique
All patients underwent the procedure under general anaesthesia with endotracheal intubation and in modified lithotomy position. Bladder was catheterised and a Clearview™ (Clinical innovations) uterine manipulator was inserted through the cervix for manipulation of the uterus.
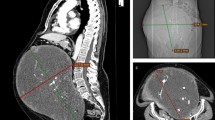
Pneumoperitoneum was created by Veress needle at the left subcostal region 2 cm below the costal margin in the mid-clavicular line, i.e. Palmers point, a 5 mm port was then inserted at this point. A zero degree 5 mm laparoscope was used to inspect the abdomen and for the duration of the operation. A second 5 mm port was placed on the contralateral side, in the right hypochondrium and two other ancillary (5 mm) ports were inserted laterally at the level of the umbilicus depending upon the size of the uterus, above the level of the ovarian ligaments lateral to the epigastric vessels and a 10 mm suprapubic port 4 cm above the pubic symphysis in the midline (Fig. 1). The right side of the procedure was carried out with the laparoscope in the right subcostal port and likewise the left side was carried out with the laparoscope in the left subcostal port. Bipolar diathermy forceps were used for coagulation and harmonic scalpel was used for coagulation and cutting the pedicles. On both sides the infundibulopelvic or ovarian ligament with the tube and round ligaments were coagulated and divided, the uterovesical fold was then opened and bladder reflected downwards (this is important especially where there is a large fibroid at the level of isthmus of the uterus). On both sides the uterine arteries were skeletonised, coagulated and divided. Then the uterus was transected from the cervix using the laploop™ (Roberts Surgical). Endocervical canal was cored out to destroy any remnant endometrial tissue. A Morcellex™ (Gynecare) tissue morcellator was then used to remove the uterine specimen from the abdominal cavity. Operative time was calculated from the insertion of the Veress needle to skin closure of the last port site.
Results
The mean age of the patients was 47 years (standard deviation of ±4 years). Most of the women were either overweight or obese with a median BMI of 29 (range 22–41). There was an overlap of symptoms and the most common indication for surgery was menorrhagia in 90% (25/29) of women, coupled with a palpable mass in 67% (19/29) of women. Pressure symptoms were present in 34% (10/29) of women. The median size of the uterus was 18 weeks (range 12–30). The median uterine weight was 575 g (range 310–1,200 g). The mean operative time was 84 ± 42 min.
The median blood loss was 200 ml (range 100–800 ml). There was a significant difference in operating times in women with uteri >500 g and those below 500 g (<500 g = 65 min, >500 g = 103 min, P = 0.007).
There were two patients who bled more than 500 ml intraoperatively but neither of them needed blood transfusion. There was one case of bladder injury which was recognised intraoperatively during reflection of the bladder over a large anterior isthmic fibroid which was repaired laparoscopically and managed with an indwelling catheter for 10 days as an outpatient followed by cystogram to ensure complete healing of the bladder. The mean hospital stay was 2 ± 1 day. None of the cases needed conversion to laparotomy. Histopathological diagnosis included 27 cases of benign leiomyoma (93%) and 2 cases of adenomyosis (7%).There were no malignancies.
Discussion
Laparoscopic subtotal hysterectomy is a minimally invasive procedure accepted as a safe and efficient way of managing benign conditions of the uterus in women who require hysterectomy [2, 5]. This operation was first performed in the 1990s [5]. Laparoscopic technique has well-known advantages to the patient by reducing trauma, blood loss, post-operative pain, shorter hospital stay and quicker return to normal activity resulting in financial benefits not only to the patient but also the society [2, 6, 7]. Many laparoscopists set the upper limit for uterine size equivalent to 16 weeks’ gestation [8] and suggest that very large uteri should be treated by laparotomy [8].
Despite the development of treatments providing a potential alternative to hysterectomy, the incidence of hysterectomy does not appear to be declining [9], it would thus be important to the majority of women if they can benefit from the known advantages of minimally invasive laparoscopic hysterectomy.
Others have tried to overcome the problems of operating on women with large uteri [3, 10–12] by introducing different techniques. These techniques, however, have a few disadvantages; such as (1) the need for seven trocars and increased cost of high trocar placement technique [10, 11], (2) the use of intra or supraumbilical ports, which are not without risk of uterine laceration when the size of the uterus is 20 weeks or more [10–12], (3) large diameter ports used above the bikini line adversely affect the cosmetic effect [10–12]. All these techniques were devised for either laparoscopic assisted vaginal hysterectomy or total laparoscopic hysterectomy where there is the vaginal outlet for the uterine specimen.
There are various limitations posed by the size and limited mobility of the enlarged uterus at the time of LASH such as limited access to hypertrophic uterine vascular pedicles, poor exposure resulting in higher risk of complications such as haemorrhage and injury to bowel, bladder, ureter, absence of vaginal outlet for the specimen and prolonged operation time. In order to overcome these difficulties and to improve the operative field we suggest this modified five port technique for LASH. It is our particular placement of the ports that enabled us to remove large uteri satisfactorily. The advantage of this technique is that the exposure of both the pelvic side walls is good despite the large uterus as the laparoscope can be placed on the left side for left sided pedicles and likewise on the right side for the right sided pedicles. Operation on the right side does not tend to be more complicated. By avoiding an umbilical and supraumbilical port the risk of laceration of the uterus is minimised and using a 0° laparoscope from the subcostal region gives a better view of the pelvic side wall, and the assistant can concentrate on exposing the field rather than also having to concentrate on the angle of the laparoscope that sometimes happens with 30° laparoscopes. Placement of the lateral ports at the level of the umbilicus allows access to the uterine vascular pedicles easily. This technique has added cosmetic benefits as all the ports above the bikini line are small (5 mm) and symmetrical.
Conclusion
The use of this modified five port technique for LASH for large uteri provides optimal exposure of the operative field, thus facilitating the procedure in women who otherwise would have had open surgery; it also provides good cosmetic effect.
References
Semm K (1991) Hysterectomy via laparotomy or pelviscopy. A new CASH method without colpotomy. Geburtshilfe Frauenheilkd 51:996–1003
Donnez J, Nisolle M (1993) Laparoscopic supracervical (subtotal) hysterectomy (LASH). J Gynecol Surg 9:91–94
Lyons TL, Adolph AJ, Winer WK (2004) Laparoscopic supracervical hysterectomy for the large uterus. J Am Assoc Gynecol Laparosc 11:170–174
Morrison JE Jr, Jacobs VR (2001) 437 classic intrafascial supracervical hysterectomies in 8 years. J Am Assoc Gynecol Laparosc 8:558–567
Jenkins TR (2004) Laparoscopic supracervical hysterectomy. Am J Obstet Gynecol 191:1875–1884
Bojahr B, Raatz D, Schonleber G, Abri C, Ohlinger R (2006) Perioperative complication rate in 1706 patients after a standardized laparoscopic supracervical hysterectomy technique. J Minim Invasive Gynecol 13:183–189
Diab AE, Abdul-Latif EE, Eldash M, Mahdy MS, Shalaby H, Shafik M (2008) Laparoscopic supracervical hysterectomy compared with total abdominal hysterectomy. Saudi Med J 29:1597–1600
Switala I, Cosson M, Lanvin D, Querleu D, Crepin G (1998) Is vaginal hysterectomy important for large uterus of more than 500 g? Comparison with laparotomy. J Gynecol Obstet Biol Reprod (Paris) 27:585–592
Garry (2005) The future of hysterectomy. BJOG 112:133–139
Lee YS (2001) Benefits of high epigastric port placement for removing the very large uterus. J Am Assoc Gynecol Laparosc 8:425–428
Wattiez A, Soriano D, Fiaccavento A, Canis M, Botchorishvili R, Pouly J et al (2002) Total laparoscopic hysterectomy for very enlarged uteri. J Am Assoc Gynecol Laparosc 9:125–130
Choi JS, Kyung YS, Kim KH, Lee KW, Han JS (2006) The four-trocar method for performing laparoscopically-assisted vaginal hysterectomy on large uteri. J Minim Invasive Gynecol 13:276–280
Conflict of interest statement
We declare that we have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shahid, A., Sankaran, S. & Odejinmi, F. Laparoscopic subtotal hysterectomy for large uteri using modified five port technique. Arch Gynecol Obstet 283, 79–81 (2011). https://doi.org/10.1007/s00404-009-1322-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-009-1322-7