Abstract
Purpose
This study aimed to evaluate the diagnostic performance of ultrasound to locate atresia/stenosis and other abdominal anomalies in pediatric patients with duodenal atresia/stenosis, including intestinal malrotation and annular pancreas.
Methods
We classified 36 retrospective cases of duodenal atresia/stenosis based on intestinal malrotation status, and evaluated the diagnostic performance of ultrasound/upper gastrointestinal contrast studies to locate atresia/stenosis and intestinal malrotation, as well as ultrasound for detecting additional anomalies such as annular pancreas. The incidence of annular pancreas was compared between groups using Fisher’s exact test.
Results
Atresia/stenosis was correctly located by ultrasound in 33 (91.7%) cases and by upper gastrointestinal contrast study in 36 (100%) cases. Of the eight cases with intestinal malrotation, five and two were correctly diagnosed by ultrasound and upper gastrointestinal contrast study, respectively. Ultrasound correctly diagnosed annular pancreas in 6/14 cases. The incidence of annular pancreas was significantly different between the groups (present/absent in groups with vs. without intestinal malrotation: 6/2 vs. 8/20, P = 0.036).
Conclusions
Ultrasound has a relatively high capability in locating atresia/stenosis. However, some cases are misdiagnosed. In clinical practice, upper gastrointestinal contrast studies should be used complementarily during diagnosis. Additional anomalies may not be detected by preoperative examinations; therefore, surgeons should carefully evaluate for additional anomalies during surgery, especially coexisting intestinal malrotation and annular pancreas.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Congenital duodenal atresia/stenosis is a common congenital anomaly induced by duodenal obstruction in neonates [1]. The surgical procedures for duodenal atresia/stenosis include diamond-shaped anastomosis—i.e., side-to-side duodenoduodenal anastomosis—and duodenojejunostomy [2,3,4,5]. The objective of these procedures is to reconstruct the patency of the duodenal lumen by bridging the location of atresia/stenosis. Therefore, adequate anastomotic sites are determined based on the location of the atresia/stenosis relative to the anal side of the intestine.
Duodenal atresia/stenosis is known to be accompanied by other anomalies [1, 3,4,5,6,7,8]. If additional abdominal anomalies, such as intestinal malrotation or jejunoileal atresia, are accompanied by duodenal atresia/stenosis, Ladd’s procedure or intestinal anastomosis might be required as additional surgical procedures [1, 5]. Therefore, preoperative examination to evaluate the presence or absence of intestinal malrotation and other anomalies would be useful for pediatric surgeons to plan surgical procedures.
Duodenal atresia/stenosis and intestinal malrotation are usually diagnosed using ultrasound and upper gastrointestinal contrast studies [1, 6, 8, 9]. A few reports focus on the incidence of anomalies accompanying duodenal atresia/stenosis; however, to the best of our knowledge, there have been no studies focusing on the diagnostic performance of these examinations for evaluating duodenal atresia/stenosis and accompanying abdominal anomalies [1, 3, 5]. Therefore, the purpose of this study was to evaluate the diagnostic performance of preoperative examinations, including ultrasound and upper gastrointestinal contrast studies, for determining the location of the atresia/stenosis and intestinal malrotation. In addition, we demonstrate the diagnostic performance of ultrasound scans for determining the presence or absence of additional abdominal anomalies, especially in annular pancreas in pediatric patients with duodenal atresia/stenosis. Intestinal malrotation is the most frequent intestinal anomaly in pediatric patients with duodenal atresia/stenosis [3, 5]; therefore, we compared the incidence of additional abdominal anomalies in pediatric patients with duodenal atresia/stenosis with and without intestinal malrotation.
Materials and methods
This study was performed in accordance with the tenets of the Declaration of Helsinki. The Ethics Committee of our institution approved this retrospective study, and the requirement for informed consent from the patients was waived.
Patients
The medical records from our hospital from April 2010 to May 2021 were reviewed and 46 pediatric patients who were surgically diagnosed with duodenal atresia/stenosis were identified. The exclusion criteria were as follows: (1) patients with two locations of atresia/stenosis in the duodenum due to a coexisting annular pancreas and membrane (n = 1), (2) patients in whom the surgical procedure was not performed in our hospital (n = 5), and (3) patients in whom neither ultrasound nor upper gastrointestinal contrast study was performed before surgical repair for duodenal atresia/stenosis (n = 4).
Patients’ characteristics
The sex and age of the patients were recorded.
Diagnosis and location of duodenal atresia/stenosis and accompanying abdominal anomalies
Surgical results were used as the gold standard for diagnosing duodenal atresia/stenosis. The location of the atresia/stenosis was classified as the descending or transverse duodenum. Additional intra-abdominal anomalies—including intestinal malrotation, annular pancreas, Meckel’s diverticulum, and jejunoileal atresia—are also reported to be accompanied by duodenal atresia/stenosis [10,11,12,13,14]. Among these anomalies, Meckel’s diverticulum and jejunoileal atresia accompanying duodenal atresia/stenosis were of low incidence; therefore, these two anomalies were excluded [10,11,12,13,14]. Finally, the presence or absence of annular pancreas was also determined during surgery.
Preoperative examination
Ultrasound
Preoperative examinations were performed by four certified pediatric radiologists with 8, 8, 15, and 20 years of experience. All sonograms were obtained using linear or convex transducers (7–15 MHz) (LOGIQ 7, E9, S8, and E10; GE Healthcare, Waukesha, WI, USA). The atresia/stenosis was diagnosed as descending (Figs. 1, 2, 3, 4) or transverse (Figs. 5 and 6) based on the location of the dilated proximal duodenum. The following findings were used to diagnose additional abdominal anomalies: (a) intestinal malrotation, an inversion in the relative positions of the superior mesenteric artery and vein, and the absence of the retro-mesenteric transverse segment of the duodenum between the superior mesenteric vessels and the aorta (Fig. 3) [9, 15,16,17] and (b) annular pancreas, pancreatic tissue surrounding the duodenum (Fig. 1) [18, 19].
A 0-day-old male with duodenal atresia/stenosis caused by an annular pancreas. Surgical results indicated that the atresia/stenosis was located in the descending duodenum, and intestinal malrotation was absent. a An axial sonogram demonstrating a dilated proximal descending duodenum (arrow); therefore, the atresia/stenosis was located in the descending duodenum on ultrasound. The relative positions of the superior mesenteric artery (A) and vein (V) were normal. The duodenum was surrounded by pancreatic tissue (arrowheads). Annular pancreas was diagnosed via ultrasound (proven surgically as present). b The relative positions of the superior mesenteric artery (A) and vein (V) were normal. The transverse duodenum (arrowheads) was also seen in the transverse plane between the superior mesenteric artery and the aorta. Therefore, intestinal malrotation was diagnosed as absent (proven surgically as absent). c The anteroposterior view of the upper gastrointestinal contrast study showed the contrast in the proximal descending duodenum (arrow), and the distal side of the atresia/stenosis was not visualized due to obstruction
A 393-day-old male with Down syndrome and duodenal atresia/stenosis caused by a membrane. Surgical results indicated that the atresia/stenosis was located in the descending duodenum, and intestinal malrotation and annular pancreas were absent. a An axial sonogram demonstrated the dilated proximal descending duodenum (arrow). Therefore, the atresia/stenosis was located in the descending duodenum on ultrasound. The duodenum was surrounded by pancreatic tissue (arrowheads). Therefore, annular pancreas was suspected based on ultrasound (absent during surgery). b The relative positions of the superior mesentery artery (A) and vein (V) were normal, and the transverse duodenum was demonstrated between the superior mesentery artery and descending aorta (arrowheads). Therefore, intestinal malrotation was diagnosed as absent on ultrasound (proven surgically as absent). c The anteroposterior view in the upper gastrointestinal contrast study showed the contrast in the proximal descending duodenum (arrow), and the distal side of the atresia/stenosis was visualized. The duodenojejunal junction laid on the left side of the vertebrae (arrowheads). Therefore, intestinal malrotation was diagnosed as absent
A 490-day-old female with Down syndrome and duodenal atresia/stenosis caused by a membrane. Surgical results indicated that the atresia/stenosis was located in the descending duodenum, intestinal malrotation was present, and other anomalies were absent. a The axial sonogram demonstrated a dilated proximal descending duodenum (arrow). Therefore, the atresia/stenosis was located in the descending duodenum on ultrasound. The duodenum was not surrounded by the pancreatic tissue; therefore, the ultrasound diagnosis indicated the absence of annular pancreas (proven surgically as absent). b The relative positions of the superior mesentery artery (A) and vein (V) were inversed. Therefore, intestinal malrotation was diagnosed as present (proven surgically as present). c Frontal view of the upper gastrointestinal contrast study showed the contrast in the proximal dilated descending duodenum. Therefore, the atresia/stenosis was located in the descending duodenum (arrow). The distal side of the atresia/stenosis was visualized and showed that the small bowel dropped away inferior to the descending duodenum (arrowheads). Therefore, intestinal malrotation was diagnosed as present
A 9-day-old female with Down syndrome and duodenal atresia/stenosis caused by a membrane. Surgical results showed that the atresia/stenosis was located in the descending duodenum, and intestinal malrotation was present, requiring the Ladd procedure. a The axial sonogram demonstrated a dilated proximal descending duodenum (arrow). Therefore, the atresia/stenosis was located in the descending duodenum on ultrasound. The relative positions of the superior mesentery artery (A) and vein (V) were normal. Therefore, intestinal malrotation was absent on ultrasound (present at surgery). The duodenum was surrounded by pancreatic tissue (arrowheads); therefore, annular pancreas was diagnosed as present on ultrasound (absent at surgery). b The frontal view of the upper gastrointestinal contrast study showed stenosis in the descending duodenum (arrow). Therefore, the atresia/stenosis was diagnosed as being located in the descending duodenum. c The anteroposterior view of the upper gastrointestinal contrast study showed that the duodenojejunal junction laid on the left side of the vertebrae (arrowheads). Therefore, intestinal malrotation was diagnosed as absent (detected during surgery)
A 0-day-old female with duodenal atresia/stenosis caused by a membrane. Surgical results indicated that the atresia/stenosis was located in the descending duodenum, and intestinal malrotation was absent. a A slightly dilated proximal transverse duodenum (arrow) and collapsed distal transverse duodenum. Therefore, the location of atresia/stenosis was misdiagnosed as the transverse duodenum on ultrasound. The duodenum was not surrounded by pancreatic tissue; therefore, annular pancreas was diagnosed as absent on ultrasound (proven surgically as absent). b The frontal view of the upper gastrointestinal contrast study showed the contrast in the proximal dilated descending duodenum (arrow). Therefore, the atresia/stenosis was diagnosed as being located in the descending duodenum
A 1-day-old female with duodenal atresia/stenosis caused by a membrane. Surgical results indicated that the atresia/stenosis was located in the transverse duodenum, and intestinal malrotation was absent. a The relative positions of the superior mesentery artery (A) and vein (V) were normal. The duodenum was not surrounded by pancreatic tissue. Therefore, annular pancreas was diagnosed as absent on ultrasound (proven surgically as absent). b The axial sonogram demonstrated a dilated proximal transverse duodenum and collapsed distal transverse duodenum. Therefore, the location of the atresia/stenosis was the transverse duodenum on ultrasound (arrow). The transverse duodenum (arrowheads) was also seen in the transverse plane between the superior mesenteric artery and the aorta. Therefore, intestinal malrotation was diagnosed as absent. c The oblique view of the upper gastrointestinal contrast study showed contrast in the proximal transverse duodenum (arrow). The distal side of the atresia/stenosis was not visualized due to obstruction
Upper gastrointestinal contrast study
All upper gastrointestinal contrast study techniques were used and combined with fluoroscopy and spot radiography with videotaping. Imaging was performed using one or two similar devices (Sonialvision G4 or C-vision Safire; Shimadzu, Kyoto, Japan). Patients were placed in the decubitus position with a nasogastric tube in the distal stomach. The contrast medium was injected into the tube, and the duodenal atresia/stenosis was located based on the location of the dilated proximal duodenum and stagnation of the contrast medium. The imaging findings were evaluated and intestinal malrotation was diagnosed if the duodenojejunal junction was inferior to the duodenal bulb (Fig. 3) [20].
Review process
Two radiologists (both with 8 years of clinical experience in pediatric radiology) retrospectively reviewed all images on a 1600 × 1200 picture archiving and communication system monitor (GE Healthcare) and evaluated the presence or absence of sonographic findings by consensus. During the review process, the radiologists were blinded to the patients’ physical findings, other imaging findings, and medical records.
Comparison of surgical results and preoperative imaging
After the review process, the preoperative diagnoses of the ultrasound and upper gastrointestinal contrast studies were judged based on the surgical results.
Statistical analyses
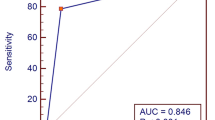
Data are presented as mean and standard deviation. The diagnostic performance for the location of duodenal atresia/stenosis and intestinal malrotation was evaluated via ultrasound and upper gastrointestinal contrast studies. In addition, the diagnostic performance for other abdominal anomalies, including annular pancreas, Meckel’s diverticulum, and jejunoileal atresia, was evaluated via ultrasound. The sensitivity, specificity, and accuracy, as well as the positive and negative predictive values of these diagnostic performances, were calculated. The 95% confidence intervals (95% CIs) were calculated using the Clopper–Pearson method to determine the accuracy of each sonographic finding. The patients' characteristics and sex, and the incidence of a congenital anomaly such as annular pancreas between patients with duodenal atresia/stenosis with and without intestinal malrotation were compared using Fisher’s exact test.
The significance level for all tests was set at 5% (two-sided). All data were analyzed using commercially available software (SPSS version 24; IBM, Armonk, NY, USA).
Results
Patients’ characteristics and surgical results of locating atresia/stenosis and additional abdominal anomalies
The characteristics of the patients with duodenal atresia/stenosis are summarized in Table 1. A total of 36 patients were included in this study. Seventeen patients were girls. The atresia/stenosis was located in the descending duodenum in 32 patients and the transverse duodenum in four patients. Of the 36 patients with duodenal atresia/stenosis, 8, 14, 2, and 1 were surgically diagnosed with intestinal malrotation, annular pancreas, Meckel’s diverticulum, and jejunoileal atresia, respectively. The incidences of Meckel’s diverticulum and jejunoileal atresia were too low to be statistically analyzed; therefore, these anomalies were excluded.
Preoperative imaging examination to locate duodenal atresia/stenosis and other abdominal anomalies (Table 2)
Of the 36 cases, 33 (91.7%) were correctly diagnosed with the location of the atresia/stenosis by ultrasound scans, while three cases that were misjudged to be in the transverse duodenum were actually in the descending duodenum (Fig. 5). All four cases with duodenal atresia/stenosis located in the transverse duodenum were correctly diagnosed (Fig. 6). In the upper gastrointestinal contrast study, all cases with duodenal atresia/stenosis located in the descending and transverse duodenum were correctly diagnosed.
On ultrasound, of the eight cases with intestinal malrotation, five (62.5%) were correctly diagnosed (Fig. 3). One case with heterotaxy was misdiagnosed as intestinal malrotation. In the upper gastrointestinal contrast study, two cases (25.0%) were correctly diagnosed. Although one case was misdiagnosed as absence of intestinal malrotation based on ultrasound and upper gastrointestinal contrast study (Fig. 4), an abnormal position of the ascending colon and Ladd band were detected during surgery. The various parameters in ultrasound for diagnosis of intestinal malrotation were as follows: sensitivity, 62.5% (5/8; 95% CI 24.5–91.5%); specificity, 96.4% (27/28; 95% CI 81.7–99.9%); accuracy, 88.9% (32/36; 95% CI 73.9–96.9%); positive predictive value (PPV), 83.3% (5/6; 95% CI 35.9–99.6%); and negative predictive value (NPV), 90% (27/30; 95% CI 73.5–97.9%) (Table 2).
On ultrasound, of the 14 cases with annular pancreas, six (42.9%) were correctly diagnosed (Fig. 1). The parameters were as follows: sensitivity, 42.9% (6/14; 95% CI 17.7–71.1%); specificity, 81.8% (18/22; 95% CI 59.7–94.8%); accuracy, 66.7% (24/36; 95% CI 49.0–81.4%); PPV, 60.0% (6/10; 95% CI 26.2–87.8%); and NPV, 69.2% (18/26; 95% CI 48.2–87.0%) (Table 2).
Comparison of patients’ characteristics between duodenal atresia/stenosis patients with and without intestinal malrotation
No significant differences were observed in terms of sex (female/male in groups with vs. without intestinal malrotation: 6/2 vs. 11/17, respectively; P = 0.114).
Comparison of the incidence of other accompanying anomalies between duodenal atresia/stenosis patients with and without intestinal malrotation
There was a significant difference in the incidence of annular pancreas between pediatric patients with duodenal atresia/stenosis with and without intestinal malrotation (number of cases with annular pancreas present/absent in groups with vs. without intestinal malrotation: 6/2 vs. 8/20, respectively; P = 0.036).
Discussion
We demonstrated that ultrasound exhibited relatively high diagnostic performance for determining the location of atresia/stenosis; however, the location was misdiagnosed in a few cases. In contrast, an upper gastrointestinal contrast study could correctly diagnose the location of duodenal atresia/stenosis. Therefore, in clinical practice, upper gastrointestinal contrast studies are used complementarily to compensate for this limitation in ultrasound. Since ultrasound did not demonstrate sufficient diagnostic performance for additional abdominal anomalies, surgeons should carefully evaluate any additional anomalies during surgery, especially coexisting intestinal malrotation and annular pancreas.
During surgery, surgeons carefully evaluated the location of duodenal atresia/stenosis. The hepatic flexure of the colon was mobilized by reflecting it downwards; subsequently, the descending duodenum was exposed. The descending duodenum was then adequately mobilized by Kocher's maneuver [2,3,4,5, 21]. Although reconstruction of duodenal atresia/stenosis located in the descending duodenum was performed using this procedure, atresia/stenosis located in the transverse duodenum behind the posterior layer of the transverse mesocolon needed additional evaluation. In addition, the abnormal location of the transverse duodenum usually occurred in cases with intestinal malrotation; therefore, before surgery, this information could prove to be useful for surgeons in planning the surgical procedure and help them explain the surgery to the parents.
On ultrasound, atresia/stenosis in the descending duodenum was misdiagnosed as being in the transverse duodenum. The location of atresia/stenosis could not be visualized with ultrasound because of the excessively dilated proximal descending duodenum or variation in the amount of intraluminal air during ultrasound examination (Fig. 5). In addition, since the transition portion between the descending and horizontal duodenum might originally be a dilated area, this dilation can be misdiagnosed as being due to duodenal atresia/stenosis at the transverse duodenum.
The relationship of the superior mesenteric artery to the vein is important in diagnosing intestinal malrotation (Fig. 3); however, in a few cases with this anomaly, the positions of the vessels could appear normal (Fig. 4) [22]. One case with heterotaxy was misdiagnosed as intestinal malrotation, because various relative positions of the superior mesenteric artery and vein have been reported [23]. Demonstrating the transverse duodenum between the superior mesenteric vessels and the aorta is also important for diagnosing intestinal malrotation [15,16,17]. However, in cases with duodenal atresia/stenosis, the distal side of the atresia/stenosis collapses and makes it difficult to detect the transverse duodenum using ultrasound. In the upper gastrointestinal contrast study, information about the distal side of the atresia/stenosis was dependent on complete obstruction. In addition, as shown in Fig. 4, with a few exceptions, the location of the duodenojejunal junction is important in the diagnosis of intestinal malrotation on upper gastrointestinal contrast examination [24]. Cecum malposition could be noted in cases with intestinal malrotation; therefore, contrast enema would provide useful information about the location of the ascending colon and improve the misdiagnosis of this condition [25, 26]. Furthermore, ultrasound might be able to evaluate the location of the ascending colon.
Annular pancreas usually occurred at the descending duodenum, and pancreatic tissue size and extent were variable in cases with annular pancreas, with some such cases being known to have fibrous pancreatic tissue [18, 19, 27]. In addition, the dilated descending duodenum was located above the annular pancreas. Therefore, it might be difficult to visualize the annular pancreas using ultrasound (Fig. 2).
Two major etiologies of duodenal atresia/stenosis are known—recanalization or annular pancreas [5, 28]. During the first 4–8 weeks of normal embryonic development, the dorsal and ventral pancreatic buds rotate and fuse, and the small bowel rotates in a counterclockwise direction around the superior mesenteric artery axis. Annular pancreas occurs because of the failure of ventral bud rotation [11, 12, 19]. Rotations of the ventral pancreatic buds and intestines occur during the same developmental period and may be associated with each other. Therefore, surgeons should carefully evaluate the presence or absence of intestinal malrotation in cases with duodenal atresia/stenosis caused by an annular pancreas.
We showed the sonographic findings needed to diagnose intestinal malrotation and annular pancreas accompanying duodenal atresia/stenosis (Table 3). The diagnostic performance of ultrasound for these anomalies was not so good, but the combination of upper gastrointestinal contrast study, contrast enema, and the location of duodenal atresia/stenosis could provide additional information for correct diagnosis.
Despite the benefits of ultrasound identified in this cohort, our study had some limitations. First, the number of patients included was small. Thus, future studies with more patients are required to confirm our preliminary findings. Second, this was a retrospective study. Therefore, during the review process, the two reviewers could only review images that had already been scanned and stored, and could not detect additional findings that had not been demonstrated during the original examination.
Conclusions
Ultrasound had a relatively high capability in locating atresia/stenosis. However, some cases were misdiagnosed. In clinical practice, upper gastrointestinal contrast studies should be used complementarily during diagnosis. Our results indicate that ultrasound does not have adequate diagnostic performance for detection of the accompanying anomalies of duodenal atresia/stenosis. Surgeons should carefully evaluate any additional anomalies during surgery, especially coexisting intestinal malrotation and annular pancreas.
References
Chen QJ, Gao ZG, Tou JF, et al. Congenital duodenal obstruction in neonates: a decade’s experience from one center. World J Pediatr. 2014;10:238–44.
Kimura K, Tsugawa C, Ogawa K, et al. Diamond-shaped anastomosis for congenital duodenal obstruction. Arch Surg. 1977;112:1262–3.
Bethell GS, Long AM, Knight M, et al. The impact of trisomy 21 on epidemiology, management, and outcomes of congenital duodenal obstruction: a population-based study. Pediatr Surg Int. 2020;36:477–83.
Gfroerer S, Theilen TM, Fiegel HC, et al. Comparison of outcomes between complete and incomplete congenital duodenal obstruction. World J Gastroenterol. 2019;25:3787–97.
Bethell GS, Long AM, Knight M, et al. Congenital duodenal obstruction in the UK: a population-based study. Arch Dis Child Fetal Neonatal Ed. 2020;105:178–83.
Carroll AG, Kavanagh RG, Ni Leidhin C, et al. Comparative effectiveness of imaging modalities for the diagnosis of intestinal obstruction in neonates and infants: a critically appraised topic. Acad Radiol. 2016;23:559–68.
Miscia ME, Lauriti G, Lelli Chiesa P, et al. Duodenal atresia and associated intestinal atresia: a cohort study and review of the literature. Pediatr Surg Int. 2019;35:151–7.
Hosokawa T, Yamada Y, Tanami Y, et al. Sonography for an imperforate anus: approach, timing of the examination, and evaluation of the type of imperforate anus and associated anomalies. J Ultrasound Med. 2017;36:1747–58.
Hosokawa T, Hosokawa M, Tanami Y, et al. Use of ultrasound findings to predict bowel ischemic changes in pediatric patients with intestinal volvulus. J Ultrasound Med. 2020;39:683–92.
Guerra A, De Gaetano AM, Infante A, et al. Imaging assessment of portal venous system: pictorial essay of normal anatomy, anatomic variants and congenital anomalies. Eur Rev Med Pharmacol Sci. 2017;21:4477–86.
Harnoss JM, Harnoss JC, Diener MK, et al. Portal annular pancreas: a systematic review of a clinical challenge. Pancreas. 2014;43:981–6.
Joseph P, Raju RS, Vyas FL, et al. Portal annular pancreas. A rare variant and a new classification. JOP. 2010;11:453–5.
Kanazawa H, Nosaka S, Miyazaki O, et al. The classification based on intrahepatic portal system for congenital portosystemic shunts. J Pediatr Surg. 2015;50:688–95.
Chen Q, Gao Z, Zhang L, et al. Multifaceted behavior of Meckel’s diverticulum in children. J Pediatr Surg. 2018;53:676–81.
Yousefzadeh DK, Kang K, Tessicini L. Assessment of retromesenteric position of the third portion of the duodenum: an US feasibility study in 33 newborns. Pediatr Radiol. 2010;40:1476–84.
Yousefzadeh DK. The position of the duodenojejunal junction: the wrong horse to bet on in diagnosing or excluding malrotation. Pediatr Radiol. 2009;39(Suppl 2):S172–7.
Menten R, Reding R, Godding V, et al. Sonographic assessment of the retroperitoneal position of the third portion of the duodenum: an indicator of normal intestinal rotation. Pediatr Radiol. 2012;42:941–5.
Piglia E, Penna CRR, Tobias J, et al. The main radiologic findings in annular pancreas. Radiol Bras. 2019;52:275–6.
Sandrasegaran K, Patel A, Fogel EL, et al. Annular pancreas in adults. AJR Am J Roentgenol. 2009;193:455–60.
Sizemore AW, Rabbani KZ, Ladd A, et al. Diagnostic performance of the upper gastrointestinal series in the evaluation of children with clinically suspected malrotation. Pediatr Radiol. 2008;38:518–28.
Mentessidou A, Saxena AK. Laparoscopic repair of duodenal atresia: systematic review and meta-analysis. World J Surg. 2017;41:2178–84.
Taylor GA. CT appearance of the duodenum and mesenteric vessels in children with normal and abnormal bowel rotation. Pediatr Radiol. 2011;41:1378–83.
Choi KS, Choi YH, Cheon JE, et al. Intestinal malrotation in patients with situs anomaly: Implication of the relative positions of the superior mesenteric artery and vein. Eur J Radiol. 2016;85:1695–700.
McVay MR, Kokoska ER, Jackson RJ, et al. Jack Barney Award. The changing spectrum of intestinal malrotation: diagnosis and management. Am J Surg. 2007;194:712–7.
Xiong Z, Shen Y, Morelli JN, et al. CT facilitates improved diagnosis of adult intestinal malrotation: a 7-year retrospective study based on 332 cases. Insights Imaging. 2021;12:58.
Steiner GM. The misplaced caecum and the root of the mesentery. Br J Radiol. 1978;51:406–13.
Nagpal SJS, Peeraphatdit T, Sannapaneni SK, et al. Clinical spectrum of adult patients with annular pancreas: Findings from a large single institution cohort. Pancreatology. 2019;19:290–5.
Sadler TW. Langman’s medical embryology (English edition). 14th ed. Philadelphia: Wolters Kluwer Health; 2018.
Acknowledgements
We would like to thank Editage for English language editing.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Takahiro Hosokawa, Yutaka Tanami, Yumiko Sato, Tetsuya Ishimaru, Hiroshi Kawashima, and Eiji Oguma declare that they have no financial or personal relationships that could lead to a conflict of interest.
Research involving human subjects
This research was performed in accordance with the tenets of the Declaration of Helsinki.
Informed consent
This retrospective study was approved by the ethics committee of our institution, and informed consent was waived.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Hosokawa, T., Tanami, Y., Sato, Y. et al. The diagnostic accuracy of ultrasound and upper gastrointestinal contrast studies for locating atresia/stenosis and intestinal malrotation and detecting annular pancreas in pediatric patients with duodenal atresia/stenosis. J Med Ultrasonics 49, 299–309 (2022). https://doi.org/10.1007/s10396-021-01176-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10396-021-01176-1